Exercise-Based Muscle Development Programmes and Their Effectiveness in the Functional Recovery of Rotator Cuff Tendinopathy: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
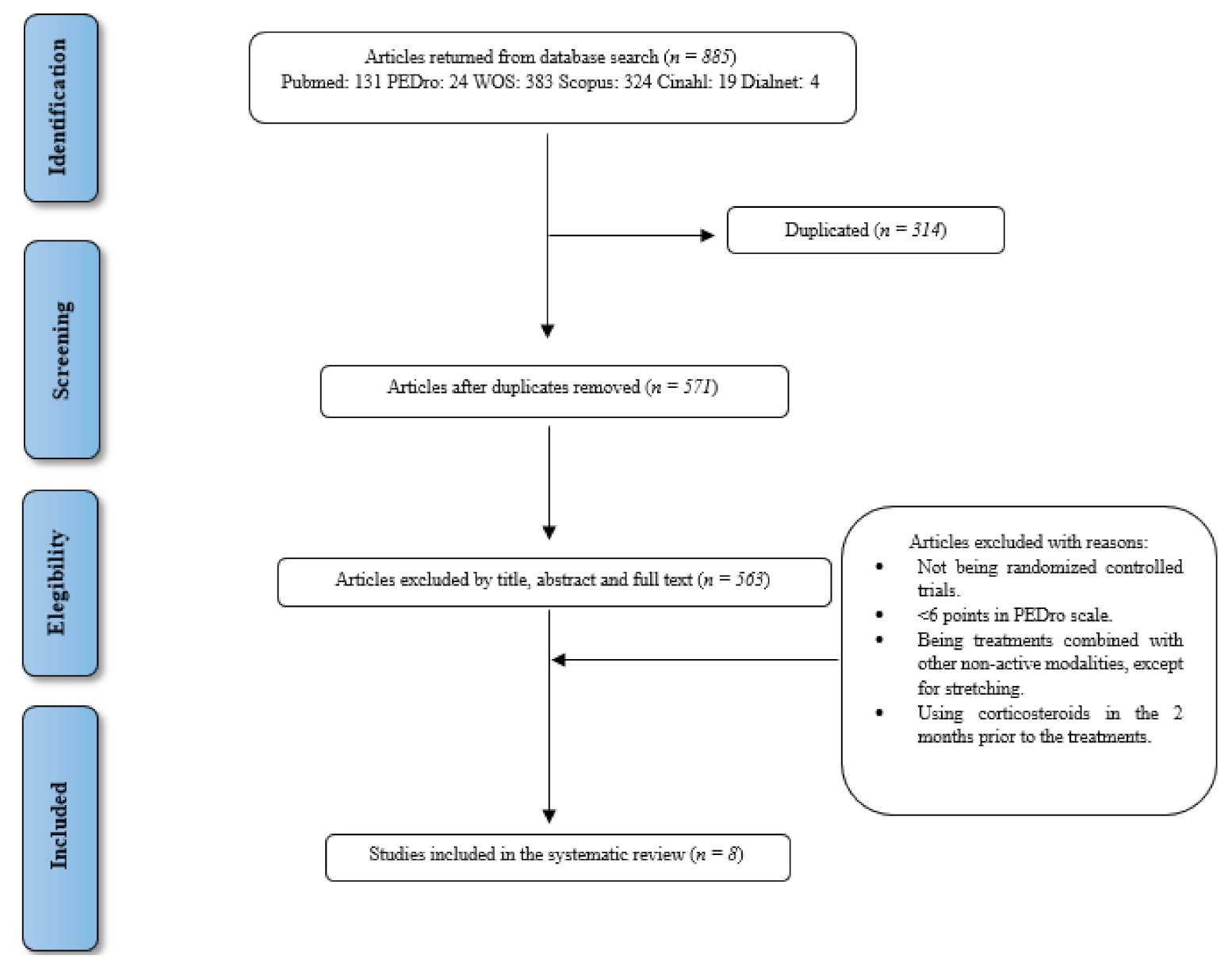
2.2. Study Selection and Inclusion Criteria
- Participants: Adults (≥18 years) with signs and symptoms compatible with RC tendinopathy in the absence of other shoulder diagnoses (ruptures/tears RC, frozen shoulder, shoulder instability).
- Intervention/comparison: Studies that include and compare programmes of active physical exercise involving gravity-resistance, either actively and freely or with an extra load applied (dumbbells, elastic bands, pulleys, etc.). Programmes consisting exclusively of active exercises (excluding manual therapy, electrotherapy, pharmacology, etc.) were allowed. Two exceptions are considered: passive stretching, as we understand that they usually form part of these programmes for final relaxation purposes; and the use of corticosteroids up to 2 months before the intervention, since most studies allowed this.
- Measurements: Studies that include measurements of shoulder strength and ROM, as well as of patients’ perception, i.e., “Patient Reported Outcome Measures” (PROMs), of pain and function by means of functional assessment scales.
- Study design: Randomised Clinical Trials (RCTs) with a minimum of 6 points on the PEDro scale [30].
- Language: English.
2.3. Data Extraction
2.4. Methodological Quality Analysis
3. Results
3.1. Literature Search and Selection
3.2. Characteristics of Included Studies
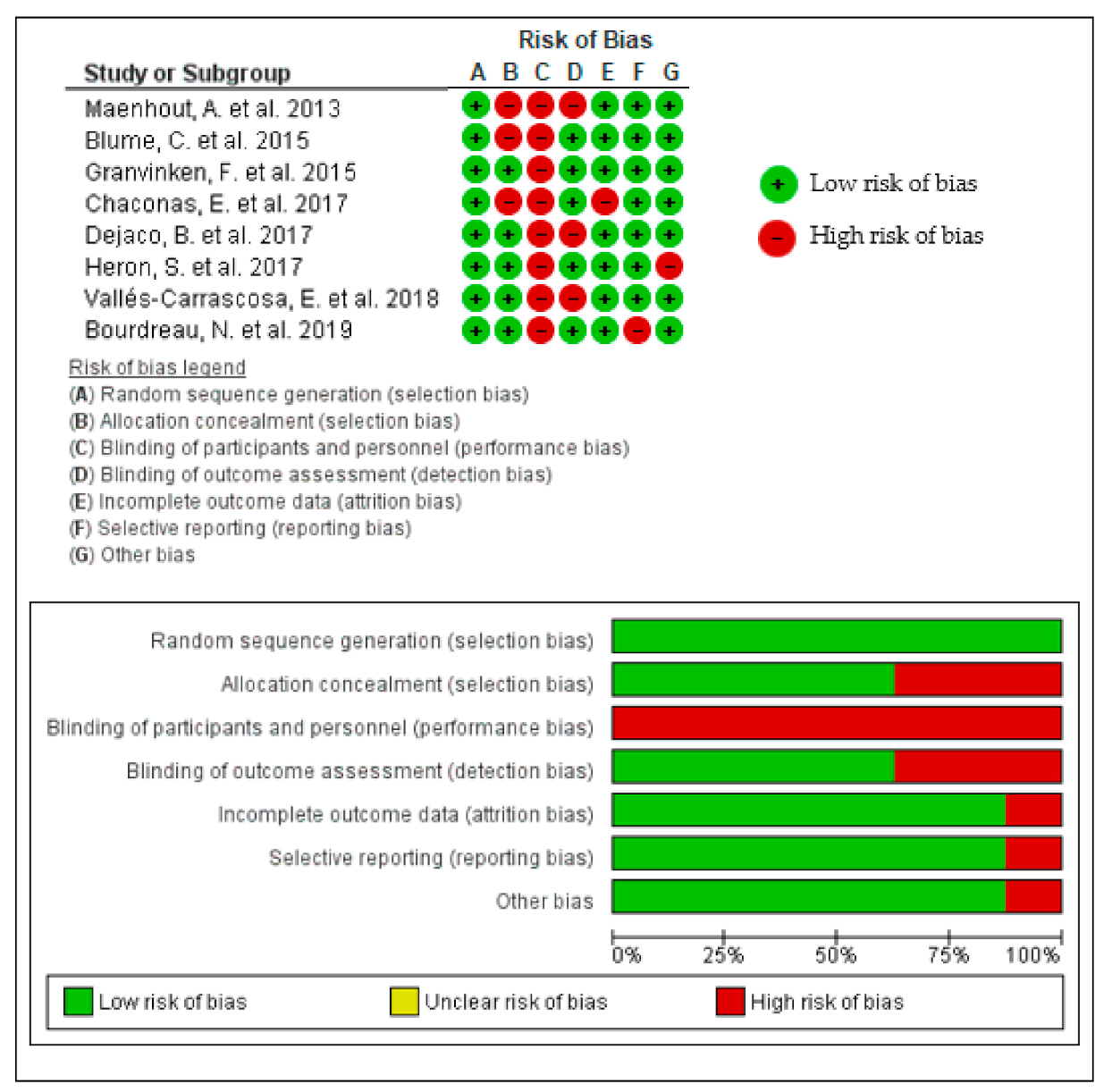
3.3. Assessment of Methodological Quality
3.4. Participant Characteristics
3.5. Characteristics of the Interventions
3.6. Outcome Measures of the Selected Studies
3.7. Narrative Synthesis of the Results of the Selected Studies
- Concentric vs. eccentric training
- Open kinetic chain vs. closed kinetic chain vs. mobility exercises
- Exercises with vs. without co-activation of glenohumeral musculature
- Exercises with pain vs. without pain
- Eccentric training vs. conventional therapeutic exercises
- Exercises with vs. without high eccentric load
- Supervised exercises vs. exercises at home:
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ABD | Abduction |
| AHD | Acromio-Humeral Distance |
| AROM | Active Range of Motion |
| CI | Confidence Interval |
| CM | Constant Murlay |
| CROB | Cochrane Risk of Bias |
| DASH | Disabilities of Arm, Shoulder and Hand |
| EMG | Electromyography |
| ER | External Rotation |
| FABQ | Fear Avoidance Beliefs Questionnaire |
| GROC | Global Rating of Change |
| IR | Internal Rotation |
| MeSH | Medical Subject Headings |
| MR | Maximum Repetition |
| MD | Mean Difference |
| MDC | Minimum Detectable Change |
| MDP | Muscle Development Program |
| NPRS | Numeric Pain Rating Scale |
| OCEBM | Oxford Centre for Evidence-Based Medicine |
| OSI | Ocupational Stress Indicator |
| PROMs | Patient Related Outcome Measures |
| RC | Rotator Cuff |
| RCT | Randomized Controlled Trial |
| RHB | Rehabilitation |
| ROM | Range of Motion |
| SD | Standard Desviation |
| SE | Standard Error |
| SMD | Standarized Mean Difference |
| SPADI | Shoulder Pain and Disabilities Index |
| UQYBT | Upper Quarter Y-Balance test |
| VAS | Visual Analogue Scale |
| WORC | Western Ontario Rotator Cuff Index |
Appendix A
| MeSH Terms * and Others | Identifier |
|---|---|
| tendinopathy or tendonopathy or tendinosis or tendinoses or tendonosis or tendonoses or tendinitis or tendinitides or tendonitis or tendonitides or “shoulder tendinopathy” or “shoulder impingement syndrome” or “shoulder impingement” or “subacromial impingement syndrome” or “subacromial bursitis” | 1 |
| “rotator cuff” or supraspinatus or infraspinatus or subscapularis or “teres minor” or “long head of biceps” | 2 |
| “isometric contraction” or “isotonic contraction” or concentric* or eccentric * or exercise* or resistance* or load * | 3 |
| “randomized controlled trial” | 4 |
Appendix B
| Database | Search Strategy | Identifier |
|---|---|---|
| Pubmed | (tendin * or tendon * or “shoulder tendinopathy” or “shoulder impingement *” or “shoulder burs *” or “subacromial impingement” or “subacromial impingement *” or “subacromial bursitis”) and (“rotator cuff” or supraspinatus or infraspinatus or subscapularis or “teres minor” or “long head of bíceps”) and (isometric * or isotonic * or concentric* or eccentric * or exercise * or “resistance training” or load *) Filter: “clinical trial” | 1, 2 and 3 |
| WOS | (tendin * or tendon * or “shoulder tendinopathy” or “shoulder impingement *” or “shoulder burs*” or “subacromial impingement” or “subacromial impingement*” or “subacromial bursitis”) and (“rotator cuff” or supraspinatus or infraspinatus or subscapularis or “teres minor” or “long head of biceps”) and (isometric * or isotonic * or concentric* or eccentric * or exercise * or resistance * or load *) and random * Filter: “article” | 1, 2, 3 and 4 |
| PEDro | “rotator cuff tend *” and “strength training” and pain and “upper arm, shoulder or shoulder girdle” and musculoskeletal and “clinical trial” | 1 and 2 * |
| Cinahl | (tendin * or tendon * or “shoulder tendinopathy” or “shoulder impingement *” or “shoulder burs*” or “subacromial impingement” or “subacromial impingement*” or “subacromial bursitis”) and (“rotator cuff” or supraspinatus or infraspinatus or subscapularis or “teres minor” or “long head of bíceps”) and (isometric * or isotonic * or concentric* or eccentric * or exercise * or “resistance training” or load *) Filter: “clinical trial” | 1, 2 and 3 |
| Scopus | (tendin * or tendon * or “shoulder tendinopathy” or “shoulder impingement *” or “shoulder burs*” or “subacromial impingement” or “subacromial impingement*” or “subacromial bursitis”) and (“rotator cuff” or supraspinatus or infraspinatus or subscapularis or “teres minor” or “long head of biceps”) and (isometric* or isotonic * or concentric* or eccentric* or exercise * or “resistance training” or load *) and random * Filter: “article” | 1, 2, 3 and 4 |
| Dialnet ** | (tendin * or tendon * or “shoulder tendinopathy” or “shoulder impingement *” or “shoulder burs *” or “subacromial impingement” or “subacromial impingement*” or “subacromial bursitis”) AND (isometric * or isotonic * or concentric * or eccentric * or exercise * or “resistance training” or load *) and random * (“rotator cuff” or supraspinatus or infraspinatus or subscapularis or “teres minor” or “long head of biceps”) and (isometric * or isotonic * or concentric * or eccentric * or exercise* or “resistance training” or load *) and random * Filter: “artículos de revista” | 1,2,3 and 4 |
References
- Littlewood, C. Contractile Dysfunction of the Shoulder (Rotator Cuff Tendinopathy): An Overview. J. Man. Manip. Ther. 2012, 20, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Pope, D.P.; Croft, P.R.; Pritchard, C.M.; Silman, A.J. Prevalence of Shoulder Pain in the Community: The Influence of Case Definition. Ann. Rheum. Dis. 1997, 56, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Van der Windt, D.A.; Koes, B.W.; de Jong, B.A.; Bouter, L.M. Shoulder Disorders in General Practice: Incidence, Patient Characteristics, and Management. Ann. Rheum. Dis. 1995, 54, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Redondo-Alonso, L.; Chamorro-Moriana, G.; Jimenez-Rejano, J.J.; Lopez-Tarrida, P.; Ridao-Fernandez, C. Relationship between Chronic Pathologies of the Supraspinatus Tendon and the Long Head of the Biceps Tendon: Systematic Review. BMC Musculoskelet. Disord. 2014, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Loppini, M.; Marineo, G.; Khan, W.S.; Maffulli, N.; Denaro, V. Tendinopathy of the Tendon of the Long Head of the Biceps. Sports Med. Arthrosc. Rev. 2021, 19, 321–332. [Google Scholar] [CrossRef]
- Gimbel, J.A.; Van Kleunen, J.P.; Mehta, S.; Perry, S.M.; Williams, G.R.; Soslowsky, L.J. Supraspinatus Tendon Organizational and Mechanical Properties in a Chronic Rotator Cuff Tear Animal Model. J. Biomech. 2004, 37, 739–749. [Google Scholar] [CrossRef]
- Cook, J.L.; Purdam, C.R. Is Tendon Pathology a Continuum? A Pathology Model to Explain the Clinical Presentation of Load-Induced Tendinopathy. Br. J. Sports Med. 2009, 43, 409–416. [Google Scholar] [CrossRef]
- Scott, A.; Squier, K.; Alfredson, H.; Bahr, R.; Cook, J.L.; Coombes, B.; De Vos, R.J.; Fu, S.N.; Grimaldi, A.; Lewis, J.S.; et al. ICON 2019: International Scientific Tendinopathy Symposium Consensus: Clinical Terminology. Br. J. Sports Med. 2020, 54, 260–262. [Google Scholar] [CrossRef]
- Linaker, C.H.; Walker-Bone, K. Shoulder Disorders and Occupation. Best Pract. Res. Clin. Rheumatol. 2015, 19, 405–423. [Google Scholar] [CrossRef]
- Bartolozzi, A.; Andreychik, D.; Ahmad, S. Determinants of Outcome in the Treatment of Rotator Cuff Disease. Clin. Orthop. Relat. Res. 1994, 308, 90–97. [Google Scholar] [CrossRef]
- Lewis, J.S. Rotator Cuff Tendinopathy. Br. J. Sports Med. 2009, 43, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.S. Rotator Cuff Tendinopathy: A Model for the Continuum of Pathology and Related Management. Br. J. Sports Med. 2010, 44, 918–923. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.L.; Rio, E.; Purdam, C.R.; Docking, S.I. Revisiting the Continuum Model of Tendon Pathology: What Is Its Merit in Clinical Practice and Research? Br. J. Sports Med. 2016, 50, 1187–1191. [Google Scholar] [CrossRef] [PubMed]
- Croisier, J.L.; Foidart-Dessalle, M.; Tinant, F.; Crielaard, J.M.; Forthomme, B. An Isokinetic Eccentric Programme for the Management of Chronic Lateral Epicondylar Tendinopathy. Br. J. Sports Med. 2007, 41, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Wilson, F.; Walshe, M.; O’Dwyer, T.; Bennett, K.; Mockler, D.; Bleakley, C. Exercise, Orthoses and Splinting for Treating Achilles Tendinopathy: A Systematic Review with Meta-Analysis. Br. J. Sports Med. 2018, 52, 1564–1574. [Google Scholar] [CrossRef]
- Lim, H.Y.; Wong, S.H. Effects of Isometric, Eccentric, or Heavy Slow Resistance Exercises on Pain and Function in Individuals with Patellar Tendinopathy: A Systematic Review. Physiother. Res. Int. 2018, 23, e1721. [Google Scholar] [CrossRef] [PubMed]
- Littlewood, C.; Ashton, J.; Chance-Larsen, K.; May, S.; Sturrock, B. Exercise for Rotator Cuff Tendinopathy: A Systematic Review. Physiotherapy 2012, 98, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, J.E. Exercise in the Treatment of Rotator Cuff Impingement: A Systematic Review and a Synthesized Evidence-Based Rehabilitation Protocol. J. Shoulder Elb. Surg. 2009, 18, 138–160. [Google Scholar] [CrossRef]
- Hanratty, C.E.; McVeigh, J.G.; Kerr, D.P.; Basford, J.R.; Finch, M.B.; Pendleton, A.; Sim, J. The Effectiveness of Physiotherapy Exercises in Subacromial Impingement Syndrome: A Systematic Review and Meta-Analysis. Semin. Arthritis Rheum. 2012, 42, 297–316. [Google Scholar] [CrossRef]
- Desmeules, F.; Boudreault, J.; Dionne, C.E.; Frémont, P.; Lowry, V.; MacDermid, J.C.; Roy, J.S. Efficacy of Exercise Therapy in Workers with Rotator Cuff Tendinopathy: A Systematic Review. J. Occup. Health 2016, 58, 389–403. [Google Scholar] [CrossRef]
- Ingwersen, K.G.; Vobbe, J.W.; Pedersen, L.L.; Sørensen, L.; Wedderkopp, N. Effect of Psychomotricity in Combination With 3 Months of Active Shoulder Exercises in Individuals with Chronic Shoulder Pain: Primary Results From an Investigator-Blinded, Randomized, Controlled Trial. Arch. Phys. Med. Rehabil. 2019, 100, 2136–2143. [Google Scholar] [CrossRef]
- Vallés-Carrascosa, E.; Gallego-Izquierdo, T.; Jiménez-Rejano, J.J.; Plaza-Manzano, G.; Pecos-Martín, D.; Hita-Contreras, F.; Achalandabaso-Ochoa, A. Pain, Motion and Function Comparison of Two Exercise Protocols for the Rotator Cuff and Scapular Stabilizers in Patients with Subacromial Syndrome [with Consumer Summary]. J. Hand Ther. 2018, 31, 227–237. [Google Scholar] [CrossRef]
- Heron, S.R.; Woby, S.R.; Thompson, D.P. Comparison of Three Types of Exercise in the Treatment of Rotator Cuff Tendinopathy/Shoulder Impingement Syndrome: A Randomized Controlled Trial. Physiotherapy 2017, 103, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Dejaco, B.; Habets, B.; van Loon, C.; van Grinsven, S.; van Cingel, R. Eccentric versus Conventional Exercise Therapy in Patients with Rotator Cuff Tendinopathy: A Randomized, Single Blinded, Clinical Trial. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 2051–2059. [Google Scholar] [CrossRef]
- Desmeules, F.; Côté, C.H.; Frémont, P. Therapeutic Exercise and Orthopedic Manual Therapy for Impingement Syndrome: A Systematic Review. Clin. J. Sport Med. 2003, 13, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Grant, H.J.; Arthur, A.; Pichora, D.R. Evaluation of Interventions for Rotator Cuff Pathology: A Systematic Review. J. Hand Ther. 2004, 17, 274–299. [Google Scholar] [CrossRef] [PubMed]
- Johansson, K.; Öberg, B.; Adolfsson, L.; Foldevi, M. A Combination of Systematic Review and Clinicians’ Beliefs in Interventions for Subacromial Pain. Br. J. Gen. Pract. 2002, 52, 145–152. [Google Scholar]
- Kelly, S.M.; Wrightson, P.A.; Meads, C.A. Clinical Outcomes of Exercise in the Management of Subacromial Impingement Syndrome: A Systematic Review. Clin. Rehabil. 2010, 24, 99–109. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Grp, P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement (Reprinted from Annals of Internal Medicine). Phys. Ther. 2009, 89, 873–880. [Google Scholar] [CrossRef]
- Yamato, T.P.; Maher, C.; Koes, B.; Moseley, A. The PEDro Scale Had Acceptably High Convergent Validity, Construct Validity, and Interrater Reliability in Evaluating Methodological Quality of Pharmaceutical Trials. J. Clin. Epidemiol. 2017, 86, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, A.P.; De Vet, H.C.W.; De Bie, R.A.; Kessels, A.G.H.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi List: A Criteria List for Quality Assessment of Randomized Clinical Trials for Conducting Systematic Reviews Developed by Delphi Consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343. [Google Scholar] [CrossRef] [PubMed]
- Maenhout, A.G.; Mahieu, N.N.; De Muynck, M.; De Wilde, L.F.; Cools, A.M. Does Adding Heavy Load Eccentric Training to Rehabilitation of Patients with Unilateral Subacromial Impingement Result in Better Outcome? A Randomized, Clinical Trial. Knee Surg. Sport. Traumatol. Arthrosc. 2013, 21, 1158–1167. [Google Scholar] [CrossRef] [PubMed]
- Blume, C.; Wang-Price, S.; Trudelle-Jackson, E.; Ortiz, A. Comparison of eccentric and concentric exercise interventions in adults with subacromial impingement syndrome. Int. J. Sports Phys. Ther. 2015, 10, 441–455. [Google Scholar] [PubMed]
- Granviken, F.; Vasseljen, O. Home Exercises and Supervised Exercises Are Similarly Effective for People with Subacromial Impingement: A Randomised Trial. J. Physiother. 2015, 61, 135–141. [Google Scholar] [CrossRef]
- Chaconas, E.J.; Kolber, M.J.; Hanney, W.J.; Daugherty, M.L.; Wilson, S.H.; Sheets, C. Shoulder external rotator eccentric training versus general shoulder exercise for subacromial pain syndrome: A randomized controlled trial. Int. J. Sports Phys. Ther. 2017, 12, 1121–1133. [Google Scholar] [CrossRef]
- Boudreau, N.; Gaudreault, N.; Roy, J.-S.S.; Bédard, S.; Balg, F.F.F.; Bedard, S.; Balg, F.F.F. The Addition of Glenohumeral Adductor Coactivation to a Rotator Cuff Exercise Program for Rotator Cuff Tendinopathy: A Single-Blind Randomized Controlled Trial. J. Orthop. Sport. Phys. Ther. 2019, 49, 126. [Google Scholar] [CrossRef]
- Manterola, C.; Asenjo-Lobos, C.; Otzen, T. Hierarchy of Evidence. Levels of Evidence and Grades of Recommendation from Current Use. Rev. Chil. Infectol. 2014, 31, 705–718. [Google Scholar] [CrossRef]
- Martins, L.V.; Marziale, M.H.P. Assessment of Proprioceptive Exercises in the Treatment of Rotator Cuff Disorders in Nursing Professionals: A Randomized Controlled Clinical Trial. Braz. J. Phys. Ther. 2012, 16, 502–509. [Google Scholar] [CrossRef]
- Smythe, A.; White, J.; Littlewood, C.; Bury, J.; Haines, T.; Malliaras, P. Physiotherapists Deliver Management Broadly Consistent with Recommended Practice in Rotator Cuff Tendinopathy: An Observational Study. Musculoskelet. Sci. Pract. 2020, 47, 102132. [Google Scholar] [CrossRef]
- Rio, E.; Van Ark, M.; Docking, S.; Moseley, G.L.; Kidgell, D.; Gaida, J.E.; Van Den Akker-Scheek, I.; Zwerver, J.; Cook, J. Isometric Contractions Are More Analgesic than Isotonic Contractions for Patellar Tendon Pain: An in-Season Randomized Clinical Trial. Clin. J. Sport Med. 2017, 27, 253–259. [Google Scholar] [CrossRef]
- Rio, E.; Kidgell, D.; Purdam, C.; Gaida, J.; Moseley, G.L.; Pearce, A.J.; Cook, J. Isometric Exercise Induces Analgesia and Reduces Inhibition in Patellar Tendinopathy. Br. J. Sports Med. 2015, 49, 1277–1283. [Google Scholar] [CrossRef]
- Gravare Silbernagel, K.; Vicenzino, B.T.; Rathleff, M.S.; Thorborg, K. Isometric Exercise for Acute Pain Relief: Is It Relevant in Tendinopathy Management? Br. J. Sports Med. 2019, 53, 1330–1331. [Google Scholar] [CrossRef]
- Littlewood, C.; Malliaras, P.; Chance-Larsen, K. Therapeutic Exercise for Rotator Cuff Tendinopathy: A Systematic Review of Contextual Factors and Prescription Parameters. Int. J. Rehabil. Res. 2015, 38, 95–106. [Google Scholar] [CrossRef]
- Langberg, H.; Ellingsgaard, H.; Madsen, T.; Jansson, J.; Magnusson, S.P.; Aagaard, P.; Kjær, M. Eccentric Rehabilitation Exercise Increases Peritendinous Type I Collagen Synthesis in Humans with Achilles Tendinosis. Scand. J. Med. Sci. Sport. 2007, 17, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Shalabi, A.; Kristoffersen-Wilberg, M.; Svensson, L.; Aspelin, P.; Movin, T. Eccentric Training of the Gastrocnemius-Soleus Complex Ion Chronic Achilles Tendinopathy Results in Decreased Tendon Volume and Intratendinous Signal as Evaluated by MRI. Am. J. Sports Med. 2004, 32, 1286–1296. [Google Scholar] [CrossRef] [PubMed]
- Öhberg, L.; Lorentzon, R.; Alfredson, H. Eccentric Training in Patients with Chronic Achilles Tendinosis: Normalised Tendon Structure and Decreased Thickness at Follow Up. Br. J. Sports Med. 2004, 38, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Öhberg, L.; Alfredson, H. Effects on Neovascularisation behind the Good Results with Eccentric Training in Chronic Mid-Portion Achilles Tendinosis? Knee Surg. Sport. Traumatol. Arthrosc. 2004, 12, 465–470. [Google Scholar] [CrossRef]
- Roos, E.M.; Engström, M.; Lagerquist, A.; Söderberg, B. Clinical Improvement after 6 Weeks of Eccentric Exercise in Patients with Mid-Portion Achilles Tendinopathy—A Randomized Trial with 1-Year Follow-Up. Scand. J. Med. Sci. Sport. 2004, 14, 286–295. [Google Scholar] [CrossRef] [PubMed]
- De Mattos, F.; Leite, N.; Pitta, A.; Bento, P.C.B. Effects of Aquatic Exercise on Muscle Strength and Functional Performance of Individuals with Osteoarthritis: A Systematic Review. Rev. Bras. Reumatol. Engl. Ed. 2016, 56, 530–542. [Google Scholar] [CrossRef]
- Williams, M.A.; Williamson, E.M.; Heine, P.J.; Nichols, V.; Glover, M.J.; Dritsaki, M.; Adams, J.; Dosanjh, S.; Underwood, M.; Rahman, A.; et al. Strengthening and Stretching for Rheumatoid Arthritis of the Hand (SARAH). A Randomised Controlled Trial and Economic Evaluation. Health Technol. Assess. (Rockv). 2015, 19, 221. [Google Scholar] [CrossRef] [PubMed]
- de Lorena, S.B.; de Lima, M.d.C.C.; Ranzolin, A.; Duarte, Â.L.B.P. Effects of Muscle Stretching Exercises in the Treatment of Fibromyalgia: A Systematic Review. Revista Bras. Reumatol. 2015, 55, 167–173. [Google Scholar] [CrossRef][Green Version]
- Mine, K.; Nakayama, T.; Milanese, S.; Grimmer, K. Effectiveness of Stretching on Posterior Shoulder Tightness and Glenohumeral Internal-Rotation Deficit: A Systematic Review of Randomized Controlled Trials. J. Sport Rehabil. 2017, 26, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Docking, S.I.; Cook, J. How Do Tendons Adapt? Going Beyond Tissue Responses to Understand Positive Adaptation and Pathology Development: A Narrative Review—PubMed. J. Musculoskelet. Neuronal Interact. 2019, 19, 300–310. [Google Scholar] [PubMed]
- Mascaró, A.; Cos, M.À.; Morral, A.; Roig, A.; Purdam, C.; Cook, J. Load Management in Tendinopathy: Clinical Progression for Achilles and Patellar Tendinopathy. Apunt. Med. L’esport 2018, 53, 19–27. [Google Scholar] [CrossRef]
- Cloke, D.J.; Watson, H.; Purdy, S.; Steen, I.N.; Williams, J.R. A Pilot Randomized, Controlled Trial of Treatment for Painful Arc of the Shoulder. J. Shoulder Elb. Surg. 2008, 17, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, K.S. Subacromial Impingement Syndrome of the Shoulder: A Musculoskeletal Disorder or a Medical Myth? Malays. Orthop. J. 2019, 13, 1–7. [Google Scholar]
- Hegedus, E.J.; Goode, A.; Campbell, S.; Morin, A.; Tamaddoni, M.; Moorman, C.T.; Cook, C. Physical Examination Tests of the Shoulder: A Systematic Review with Meta-Analysis of Individual Tests. Br. J. Sports Med. 2008, 42, 80–92. [Google Scholar] [CrossRef]
- Papadonikolakis, A.; McKenna, M.; Warme, W.; Martin, B.I.; Matsen, F.A. Published Evidence Relevant to the Diagnosis of Impingement Syndrome of the Shoulder. J. Bone Jt. Surg. Ser. A 2011, 93, 1827–1832. [Google Scholar] [CrossRef]
- Kelly, B.T.; Kadrmas, W.R.; Speer, K.P. The Manual Muscle Examination for Rotator Cuff Strength: An Electromyographic Investigation. Am. J. Sports Med. 1996, 24, 581–588. [Google Scholar] [CrossRef]
- Salamh, P.; Lewis, J. It Is Time to Put ‘Special Tests’ for Rotator Cuff Related Shoulder Pain Out to Pasture. J. Orthop. Sport. Phys. Ther. 2020, 50, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.M.; Harryman, D.T. Tendons, Ligaments, and Capsule of the Rotator Cuff. Gross and Microscopic Anatomy—PubMed. J. Bone Jt. Surg. 1992, 74, 713–725. [Google Scholar] [CrossRef]
- Boettcher, C.E.; Ginn, K.A.; Cathers, I. The “empty Can” and “Full Can” Tests Do Not Selectively Activate Supraspinatus. J. Sci. Med. Sport 2009, 12, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Keung, W.W.; Yan, L.I.M.; Patrick, Y.; Hang, S.; Teng, L.H. The Effect of Psychological Factors on Pain, Function and Quality of Life in Patients with Rotator Cuff Tendinopathy: A Systematic Review. Musculoskelet. Sci. Pract. 2020, 102173. [Google Scholar] [CrossRef]
- Holmgren, T.; Bjornsson Hallgren, H.; Oberg, B.; Adolfsson, L.; Johansson, K. Effect of Specific Exercise Strategy on Need for Surgery in Patients with Subacromial Impingement Syndrome: Randomised Controlled Study. BMJ 2012, 344, e787. [Google Scholar] [CrossRef] [PubMed]
- Dilek, B.; Gulbahar, S.; Gundogdu, M.; Ergin, B.; Manisali, M.; Ozkan, M.; Akalin, E. Efficacy of Proprioceptive Exercises in Patients with Subacromial Impingement Syndrome. Am. J. Phys. Med. Rehabil. 2016, 95, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Struyf, F.; Nijs, J.; Mollekens, S.; Jeurissen, I.; Truijen, S.; Mottram, S.; Meeusen, R. Scapular-Focused Treatment in Patients with Shoulder Impingement Syndrome: A Randomized Clinical Trial. Clin. Rheumatol. 2013, 32, 73–85. [Google Scholar] [CrossRef]
- Hallgren, H.C.B.; Holmgren, T.; Öberg, B.; Johansson, K.; Adolfsson, L.E. A Specific Exercise Strategy Reduced the Need for Surgery in Subacromial Pain Patients. Br. J. Sports Med. 2014, 48, 1431–1436. [Google Scholar] [CrossRef]
- Bae, Y.H.; Lee, G.C.; Shin, W.S.; Kim, T.H.; Lee, S.M. Effect of Motor Control and Strengthening Exercises on Pain, Function, Strength and the Range of Motion of Patients with Shoulder Impingement Syndrome. J. Phys. Ther. Sci. 2011, 23, 687–692. [Google Scholar] [CrossRef]
- Subasi, V.; Toktas, H.; Demirdal, U.S.; Turel, A.; Cakir, T.; Kavuncu, V. Water-Based versus Land-Based Exercise Program for the Management of Shoulder Impingement Syndrome. Turk. Fiz. Tip Ve Rehabil. Derg. Turk. J. Phys. Med. Rehabil. 2012, 58, 79–84. [Google Scholar]
- Başkurt, Z.; Başkurt, F.; Gelecek, N.; Özkan, M.H. The Effectiveness of Scapular Stabilization Exercise in the Patients with Subacromial Impingement Syndrome. J. Back Musculoskelet. Rehabil. 2011, 24, 173–179. [Google Scholar] [CrossRef]
- Moseley, A.M.; Rahman, P.; Wells, G.A.; Zadro, J.R.; Sherrington, C.; Toupin-April, K.; Brosseau, L. Agreement between the Cochrane Risk of Bias Tool and Physiotherapy Evidence Database (PEDro) Scale: A Meta-Epidemiological Study of Randomized Controlled Trials of Physical Therapy Interventions. PLoS ONE 2019, 14, e0222770. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Fuentes, J.; Ospina, M.; Saltaji, H.; Hartling, L. Inconsistency in the Items Included in Tools Used in General Health Research and Physical Therapy to Evaluate the Methodological Quality of Randomized Controlled Trials: A Descriptive Analysis. Bmc Med. Res. Methodol. 2013, 13, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Herbert, R.D.; Maher, C.G.; Moseley, A.M. PEDro. A Database of Randomized Trials and Systematic Reviews in Physiotherapy. Man. Ther. 2000, 5, 223–226. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, B.R.; Hilfiker, R.; Egger, M. PEDro’s Bias: Summary Quality Scores Should Not Be Used in Meta-Analysis. J. Clin. Epidemiol. 2013, 66, 75–77. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S. Quality Scores Are Useless and Potentially Misleading Reply to “Re: A Critical Look at Some Popular Analytic Methods”. Am. J. Epidemiol. 1994, 140, 300–301. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Training. Available online: https://training.cochrane.org/handbook/current (accessed on 4 March 2021).
- Vase, L.; Wartolowska, K. Pain, Placebo, and Test of Treatment Efficacy: A Narrative Review. Br. J. Anaesth. 2019, 123, e254–e262. [Google Scholar] [CrossRef]
- De Deyn, P.P.; D’Hooge, R. Placebos in Clinical Practice and Research. J. Med. Ethics 1996, 22, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Savović, J.; Jones, H.E.; Altman, D.G.; Harris, R.J.; Jüni, P.; Pildal, J.; Als-Nielsen, B.; Balk, E.M.; Gluud, C.; Gluud, L.L.; et al. Influence of Reported Study Design Characteristics on Intervention Effect Estimates from Randomized, Controlled Trials. Ann. Intern. Med. 2012, 157, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.; Egger, M.; Gluud, L.L.; Schulz, K.F.; Jüni, P.; Altman, D.G.; Gluud, C.; Martin, R.M.; Wood, A.J.G.; Sterne, J.A.C. Empirical Evidence of Bias in Treatment Effect Estimates in Controlled Trials with Different Interventions and Outcomes: Meta-Epidemiological Study. BMJ 2008, 336, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Boone, D.C.; Azen, S.P.; Lin, C.M.; Spence, C.; Baron, C.; Lee, L. Reliability of Goniometric Measurements. Phys. Ther. 1978, 58, 1355–1360. [Google Scholar] [CrossRef] [PubMed]
- Mullaney, M.J.; McHugh, M.P.; Johnson, C.P.; Tyler, T.F. Reliability of Shoulder Range of Motion Comparing a Goniometer to a Digital Level. Physiother. Theory Pract. 2010, 26, 327–333. [Google Scholar] [CrossRef]
- Damas, F.; Phillips, S.M.; Lixandrão, M.E.; Vechin, F.C.; Libardi, C.A.; Roschel, H.; Tricoli, V.; Ugrinowitsch, C. Early Resistance Training-Induced Increases in Muscle Cross-Sectional Area Are Concomitant with Edema-Induced Muscle Swelling. Eur. J. Appl. Physiol. 2016, 116, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Brook, M.S.; Wilkinson, D.J.; Mitchell, W.K.; Lund, J.N.; Szewczyk, N.J.; Greenhaff, P.L.; Smith, K.; Atherton, P.J. Skeletal Muscle Hypertrophy Adaptations Predominate in the Early Stages of Resistance Exercise Training, Matching Deuterium Oxide-Derived Measures of Muscle Protein Synthesis and Mechanistic Target of Rapamycin Complex 1 Signaling. FASEB J. 2015, 29, 4485–4496. [Google Scholar] [CrossRef]
- Fridén, J. Changes in Human Skeletal Muscle Induced by Long-Term Eccentric Exercise. Cell Tissue Res. 1984, 236, 365–372. [Google Scholar] [CrossRef]
- Mosher, Z.A.; Ewing, M.A.; Collins, C.S.; Young, P.G.; Brabston, E.W.; Momaya, A.M.; Tashjian, R.Z.; Ponce, B.A. Usage Trends of Patient-Reported Outcome Measures in Shoulder Literature. J. Am. Acad. Orthop. Surg. 2019, 24, 1–8. [Google Scholar] [CrossRef]
- Jawad Hashim, M. Patient-Centered Communication: Basic Skills. Am. Fam. Physician 2017, 95, 29–34. [Google Scholar]
- Babatunde, F.; MacDermid, J.; MacIntyre, N. Characteristics of Therapeutic Alliance in Musculoskeletal Physiotherapy and Occupational Therapy Practice: A Scoping Review of the Literature. Bmc Health Serv. Res. 2017, 17, 1–23. [Google Scholar]
- Thong, I.S.K.; Jensen, M.P.; Miró, J.; Tan, G. The Validity of Pain Intensity Measures: What Do the NRS, VAS, VRS, and FPS-R Measure? Scand. J. Pain 2018, 18, 99–107. [Google Scholar] [CrossRef]
- Breckenridge, J.D.; McAuley, J.H. Shoulder Pain and Disability Index (SPADI). J. Physiother. 2011, 57, 197. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Muriel, A.; Medina, J.M.; Abraira, V.; Castillo Sánchez, M.D.; Jaúregui, J.O. Psychometric Characteristics of the Spanish Version of the FAB Questionnaire. Spine (Phila. Pa. 1976) 2006, 31, 104–110. [Google Scholar] [CrossRef] [PubMed]
| Characteristics of Studies | |||
|---|---|---|---|
| Study/Objective | Characteristics of Participants | Intervention/Comparison | Outcome Measures/Results |
| Maenhout, A. et al., 2013 [33] Study objective: To investigate superior value of adding heavy load eccentric training to conservative treatment in patients with subacromial impingement. Level of evidence: Therapy, 2b (OCEBM) | n = 61 Sex: 25 men/36 women Age (Mean ± SD):
Exclusion criteria: partial/full RC ruptures; shoulder surgery, fracture, dislocation; traumatic onset of the pain; osteoarthritis; frozen shoulder, traumatic glenohumeral instability; shoulder nerve injuries; concomitant disorders (cervical pathology or systemic musculoskeletal disease); physiotherapy and/or corticosteroids within 2 months of the intervention. | Heavy-load eccentric exercises Both groups:
| Variables evaluation at 6 and 12 weeks. Main variables evaluated with:
|
| Blume, C. et al., 2015 [34] Study objective: To compare the effectiveness of an eccentric progressive resistance exercise intervention to a concentric progressive resistance exercise intervention in adults with subacromial impingement syndrome. Level of evidence: Therapy, 1b (OCEBM) | n= 34 Sex: 14 men/20 women Age (mean ± SD): 49.4 ± 15.6 years Inclusion criteria: ≥18 years; at least 1 of 3 positive tests (Neer, Hawkins-Kennedy and coracoid ADD impingement tests); 1 negative RC tear test. Exclusion criteria: shoulder, cervical, or thoracic surgeries; shoulder dislocation; fracture; labral tear; full-thickness RC tear; adhesive capsulitis; rheumatic disease; pregnancy or medical condition that precluded them from performing resisted exercises. | Eccentric vs. concentric exercises Both groups:
Lifting portion of the exercises with the therapist repositioning the weight to the start position to avoid resistance in the lowering (eccentric) portion of the exercise. Group 2—Eccentric progressive resistance exercises (n = 16): Lowering portion of the exercises with the therapist repositioning the weight to the starting position to avoid resistance during the lifting (concentric) portion of each exercise. | Valiables evaluation at 5 and 8 weeks. Variables evaluated with (does not specify which is the primary variable):
Significant improvements were found for all variables up to week 5 (p < 0.05) regardless of group assignment. All measures except arm elevation ROM (p = 0.302) continued to show significant improvement from week 5 to week 8 (p < 0.05). |
| Granviken, F. et al., 2013 [35] Study objective: To compare the different effects of home exercise and supervised exercise on pain and disability for patients with subacromial impingement. Level of evidence: Therapy, 1b (OCEBM) | n = 46 Sex: 24 men/22 women Age (mean ± SD):
Exclusion criteria: Glenohumeral instability; acromioclavicular joint pathology; labrum pathology on imaging; full-thickness RC tears; glenohumeral osteoarthritis; undergone shoulder surgery; insufficient language capability; cervical spine problems; rheumatoid arthritis;other physical or serious mental illness. | Home vs. supervised exercise Both groups:
Parameters: 3 × 30 rep. Group 1—Home exercises (n = 23):
Group 2—Supervised exercises (n = 23):10 supervised treatments + home exercises. | Variables evaluated at 6 and 26 weeks Main variable evaluated with:
There were no significant differences between groups in pain, physical activity, or work on the FABQ and ROM. No participant reported full recovery in terms of perceived benefit. One subject was dissatisfied with treatment. |
| Chaconas, E. J. et al., 2017 [36] Study objective: To compare outcomes, for individuals diagnosed with subacromial pain syndrome, performing a 6-week protocol of eccentric training of the shoulder external rotators compared to a general exercise protocol. Level of evidence: Therapy, 2b (OCEBM) | n = 48 Sex: 28 men/20 women Age (mean ± SD): 46.8 ± 17.29 years Inclusion criteria: ≥3 positives tests of: Neer, Hawkins-Kennedy and the empty can test; pain with resisted ER; palpable tenderness at the insertion of the supraspinatus or infraspinatus; painful arc between 60–120° active ABD; shoulder pain ≥3 months duration Exclusion criteria: Red flags; full thickness supraspinatus or infraspinatus tendon; adhesive capsulitis and history of shoulder surgery. | Eccentric vs. general shoulder exercises: Both groups: Diary exercise.
Group 1—Eccentric exercises (n = 25): Eccentric exercises with scapular retraction + posterior shoulder stretching.
| Variables evaluated at 3, 6 weeks and 6 months. Main variables evaluated with:
|
| Heron, S. et al., 2017 [23] Study objective: To assess the efficacy of three different exercise programmes in treating RC tendinopathy/shoulder impingement syndrome. Level of evidence: Therapy, 1b (OCEBM) | n = 120 Sex: 71 men/49 women Age (mean): 49, 9 years Inclusion criteria: shoulder pain for ≥3 months; no passive limitation of ROM suggestive of adhesive capsulitis; pain on isometric RC testing; pain on Hawkins–Kennedy or empty can tests; able to read and write English. Exclusion criteria: symptoms of cervical radiculopathy; diagnosed inflammatory disorder; neurological disorder; widespread pain condition; complete RC tear (positive drop arm test and/or Oxford scale grade II and/or less strength of the RC); history of shoulder sugery. | Open kinetic chain vs. closed kinetic chain vs. mobility exercises All groups:
ER, IR and ABD exercises with a resistance elastic band. Group 2—Closed kinetic chain exercises (n = 40): Double-arm wall press up, quadrupedal press up and a seated position and pressed their hands into the chair, as if trying to lift their body. Group 3—Mobility exercises) (n = 40): IR, ER and ABD exercises from self-passive mobility to free active mobility. | Variables evaluated at 6 weeks. Main variable evaluated with:
Change of intra-group mean in SPADI; (Effect size). Group 1: 12; p = 0.0001 (0.56); Group 2: 9; p = 0.0002 (0.63); Group 3: 9; p = 0.0002 (0.49). There were no significant differences between groups. (Kruskal-Wallis test): Change in SPADI mean (95% CI): Group 1: −3.5 (−5, 12); Group 2: −0.5 (−3, 15); Group 3: −4.0 (−5, 17). There were no clinically significant differences in SPADI during follow-up. |
| Dejaco, B. et al., 2017 [24] Study objective: To investigate the effectiveness of isolated eccentric versus conventional exercise therapy in patients with RC tendinopathy. Level of evidence: Therapy, 1b (OCEBM) | n= 36 Sex= 19 men/17 women Age (mean ± SD)
Exclusion criteria: Subjective feeling of instability and positive apprehension sign; positive scapular assistance and/or resistance test; partial/full ruptures of RC; calcifications >4 mma; acromion type III (according to Bigliani criteria); bursitis; history of shoulder fracture and/or shoulder surgery; cervical radiculopathy; adhesive capsulitis; systemic diseases; corticosteroid injection 3 months prior to inclusion. | Eccentric vs. conventional exercises Both groups: 1 session of physiotherapy per week (during the first 6 weeks) and 3 sessions per week (during the last 6 weeks)
Group 2—Conventional exercises (n = 16): 8 differents exercises 1 time/day
| Variables evaluated at 6, 12 and 26 weeksMain variable evaluated with:
Secondary variables evaluated with:
|
| Vallés-Carrascosa, E. et al., 2018 [22] Study objective: To compare the effect on pain, active ROM and shoulder function of an exercise protocol performed with pain <40 mm Visual Analogue Scale and without pain, in patients with subacromial syndrome. Level of evidence: Therapy, 2b (OCEBM) | n = 22 Sex: 10 men/12 women Age (mean (1st quartile; 3rd quartile))
Exclusion criteria: RC tears; shoulder surgery in the last 3 months; frozen shoulder; shoulder prosthesis; fibromyalgia; malignant neoplasm; history of rheumatic or chronic inflammatory disease. | With vs. withouth pain Both groups:
Group 2—Without pain (n = 11): Exercises without pain (0 mm on VAS scale). | Variables evaluated at 4 weeks Main variables evaluated with:
There were no significant differences between groups (p > 0.05). |
| Bourdreau, N. et al., 2019 [37] Study objective: To compare the short-term efficacy of adding glenohumeral adductor coactivation to a RC strengthening program to improve function, reduce symptoms and increase acromiohumeral distance in adults with RC tendinopathy. Level of evidence: Therapy, 1b (OCEBM) | n = 42 Sex: 20 men/22 women Age (mean ± SD):
Exclusion criteria: Full-thickness RC tear; shoulder surgery; shoulder capsulitis, osteoarthritis or traumatic instability; rheumatoid arthritis; systemic inflammatory or neurologic condition; corticosteroid injections in the affected shoulder within the past 6 weeks. | Exercises with co-activation of glenohumeral musculature vs. without it Both groups:
Group 2—Withouth co-activation of glenohumeral muscles (n = 21): Glenohumeral muscles exercises without recruitment of minor pectoral and latissimus dorsi, with visual feedback (EMG). The rest of exercises were done in the same way. | Variables evaluated at 3 and 6 weeks Main variable evaluated with:
|
| Study | Criteria | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Maenhout, A. et al. [33] | √ | √ | X | √ | X | X | X | √ | √ | √ | √ | 6 |
| Blume, C. et al. [34] | √ | √ | √ | √ | X | X | √ | √ | √ | √ | √ | 8 |
| Granvinken, F. et al. [35] | √ | √ | √ | √ | X | X | √ | √ | √ | √ | √ | 8 |
| Chaconas, E. J. et al. [36] | X | √ | X | √ | X | X | √ | √ | X | √ | √ | 6 |
| Heron, S. et al. [23] | √ | √ | √ | √ | X | X | √ | X | √ | √ | √ | 7 |
| Dejaco, B. et al. [24] | √ | √ | √ | √ | X | X | X | √ | √ | √ | √ | 7 |
| Vallés-Carracosa, E. et al. [22] | √ | √ | √ | √ | X | X | X | √ | √ | √ | √ | 7 |
| Bourdreau N. et al. [37] | √ | √ | √ | √ | X | X | √ | √ | √ | √ | √ | 8 |
| Assessment Tests | ||||||
|---|---|---|---|---|---|---|
| Studies | Hawkins-Kennedy Test | Neer Test | Isometric Test | Painful Arc | Empty Can Test | Others * |
| Maenhout, A. et al. [33] | √ | √ | √ | √ | √ | |
| Blume, C. et al. [34] | √ | √ | √ | |||
| Granvinken, F. et al. [35] | √ | √ | √ | √ | ||
| Chaconas, E. J. et al. [36] | √ | √ | √ | √ | √ | √ |
| Heron, S. et al. [23] | √ | √ | √ | |||
| Dejaco, B. et al. [24] | √ | √ | √ | |||
| Vallés-Carracosa, E. et al. [22] | √ | |||||
| Bourdreau N. et al. [37] | √ | √ | √ | √ | ||
| Total | 7 | 5 | 5 | 5 | 3 | 4 |
| Muscle Contraction Types | Number of Studies |
|---|---|
| Concentric + Eccentric (The load is applied during the concentric and eccentric phase) | 4 [22,23,35,37] |
| Concentric (The load is only applied during the concentric phase) | 1 [34] |
| Eccentric (The load is only applied during the eccentric phase) | 4 [24,33,34,36] |
| STUDIES | Monitoring and Evaluation of Variables | WEEKS | |||||||
| 0 | 3 | 4 | 5 | 6 | 8 | 12 | 26 | ||
| Maenhout, A. et al. [33] | √ | √ | √ | ||||||
| Blume, C. et al. [34] | √ | √ | √ | ||||||
| Granvinken, F. et al. [35] | √ | √ | √ | ||||||
| Chaconas, E. J. et al. [36] | √ | √ | √ | √ | |||||
| Heron, S. et al. [23] | √ | √ | |||||||
| Dejaco, B. et al. [24] | √ | √ | √ | √ | |||||
| Vallés-Carrascosa, E. et al. [22] | √ | √ | |||||||
| Bourdreau, N. et al. [37] | √ | √ | √ | ||||||
 End of intervention; √: Time of evaluation of the variables.
End of intervention; √: Time of evaluation of the variables.| Patient Reported Outcome Measures | ||||||||
|---|---|---|---|---|---|---|---|---|
| Studies | NPRS/VAS | SPADI | WORC | DASH | CM | FABQ | UQYBT | GROC |
| Maenhout, A. et al. [33] | √ | |||||||
| Blume, C. et al. [34] | √ | |||||||
| Granvinken, F. et al. [35] | √ | √ | √ | |||||
| Chaconas, E. J. et al. [36] | √ | √ | √ | √ | ||||
| Heron, S. et al. [23] | √ | |||||||
| Dejaco, B. et al. [24] | √ | √ | ||||||
| Vallés-Carracosa, E. et al. [22] | √ | √ | ||||||
| Bourdreau N. et al. [37] | √ | √ | √ | |||||
| Total | 5 | 3 | 2 | 2 | 2 | 1 | 1 | 1 |
| ROM | ISOMETRIC STRENGHT | SPADI | WORC | DASH | NPRS/VAS | CM | FABQ | UQYBT | GROC | |
|---|---|---|---|---|---|---|---|---|---|---|
| Maenhout, A. et al. [33] | √ | √ | ||||||||
| Blume, C. et al. [34] | √ | √ | √ | |||||||
| Granvinken, F. et al. [35] | √ | √ | √ | √ | ||||||
| Chaconas, E. J. et al. [36] | √ | √ | √ | √ | √ | √ | ||||
| Heron, S. et al. [23] | √ | |||||||||
| Dejaco, B. et al. [24] | √ | √ | √ | √ | ||||||
| Vallés-Carrascosa, E. et al. [22] | √ | √ | √ | |||||||
| Bourdreau, N. et al. [37] | √ | √ | √ |
 Significant and effective;
Significant and effective;  Not significant. √ Variable measured in study; Abbreviations: CM Constant Murlay; DASH, Disabilities of Arm, Shoulder and Hand; FABQ, Fear Avoidance Beliefs Questionnaire; GROC, Global Rating of Change; NPRS, Numeric Pain Rating Scale; OSI, Ocupational Stress Indicator; ROM, range of motion; SPADI, Shoulder Pain and Disabilities Index; UQYBT, Upper Quarter Y-Balance test; VAS, Visual Ananolgue Scale; WORC, Western Ontario Rotator Cuff Index.
Not significant. √ Variable measured in study; Abbreviations: CM Constant Murlay; DASH, Disabilities of Arm, Shoulder and Hand; FABQ, Fear Avoidance Beliefs Questionnaire; GROC, Global Rating of Change; NPRS, Numeric Pain Rating Scale; OSI, Ocupational Stress Indicator; ROM, range of motion; SPADI, Shoulder Pain and Disabilities Index; UQYBT, Upper Quarter Y-Balance test; VAS, Visual Ananolgue Scale; WORC, Western Ontario Rotator Cuff Index.Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dominguez-Romero, J.G.; Jiménez-Rejano, J.J.; Ridao-Fernández, C.; Chamorro-Moriana, G. Exercise-Based Muscle Development Programmes and Their Effectiveness in the Functional Recovery of Rotator Cuff Tendinopathy: A Systematic Review. Diagnostics 2021, 11, 529. https://doi.org/10.3390/diagnostics11030529
Dominguez-Romero JG, Jiménez-Rejano JJ, Ridao-Fernández C, Chamorro-Moriana G. Exercise-Based Muscle Development Programmes and Their Effectiveness in the Functional Recovery of Rotator Cuff Tendinopathy: A Systematic Review. Diagnostics. 2021; 11(3):529. https://doi.org/10.3390/diagnostics11030529
Chicago/Turabian StyleDominguez-Romero, Juan G., José J. Jiménez-Rejano, Carmen Ridao-Fernández, and Gema Chamorro-Moriana. 2021. "Exercise-Based Muscle Development Programmes and Their Effectiveness in the Functional Recovery of Rotator Cuff Tendinopathy: A Systematic Review" Diagnostics 11, no. 3: 529. https://doi.org/10.3390/diagnostics11030529
APA StyleDominguez-Romero, J. G., Jiménez-Rejano, J. J., Ridao-Fernández, C., & Chamorro-Moriana, G. (2021). Exercise-Based Muscle Development Programmes and Their Effectiveness in the Functional Recovery of Rotator Cuff Tendinopathy: A Systematic Review. Diagnostics, 11(3), 529. https://doi.org/10.3390/diagnostics11030529






