Is Computed Tomography Necessary for Diagnostic Workup in Displaced Pediatric Medial Epicondyle Fractures?
Abstract
1. Introduction
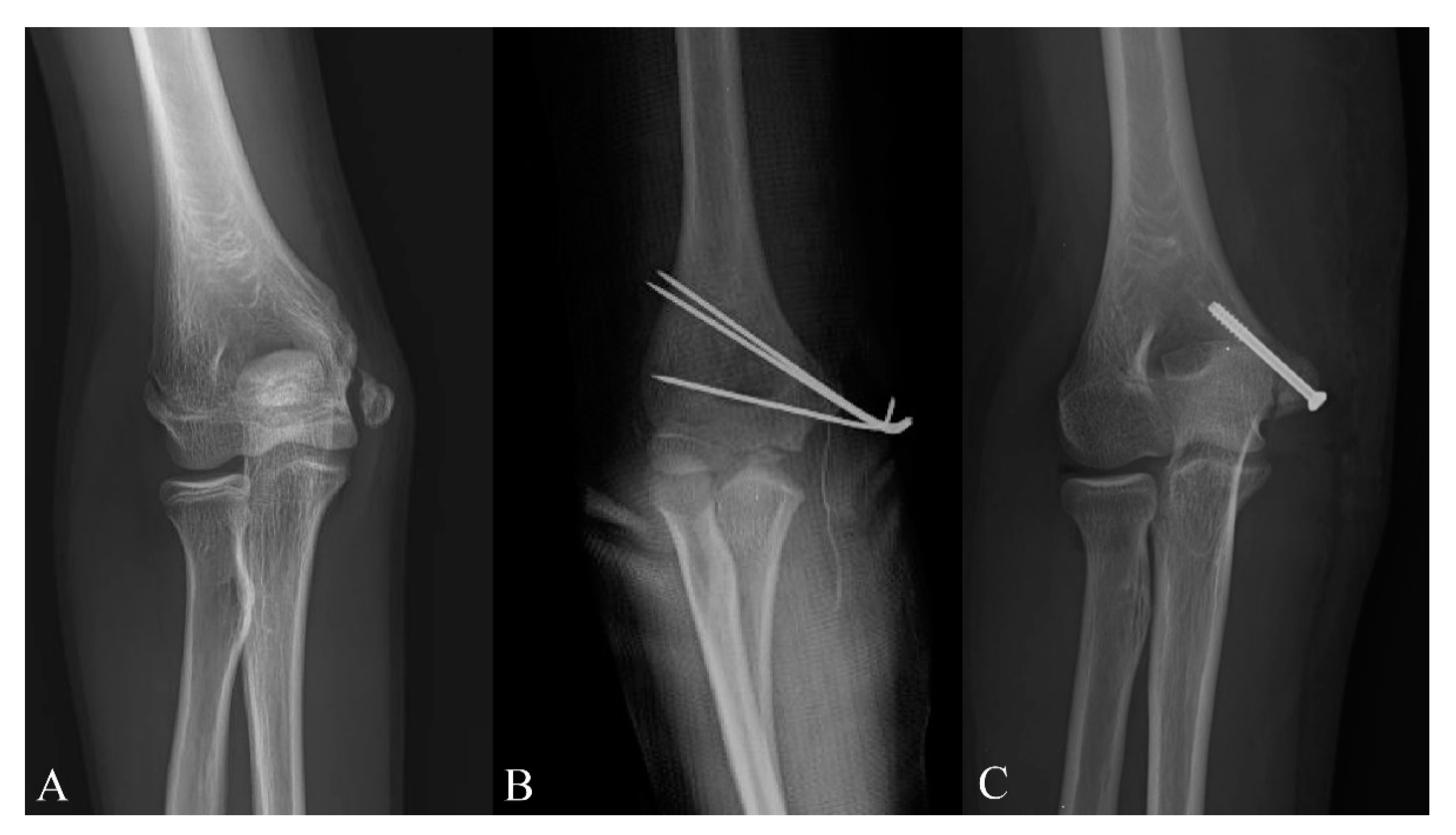
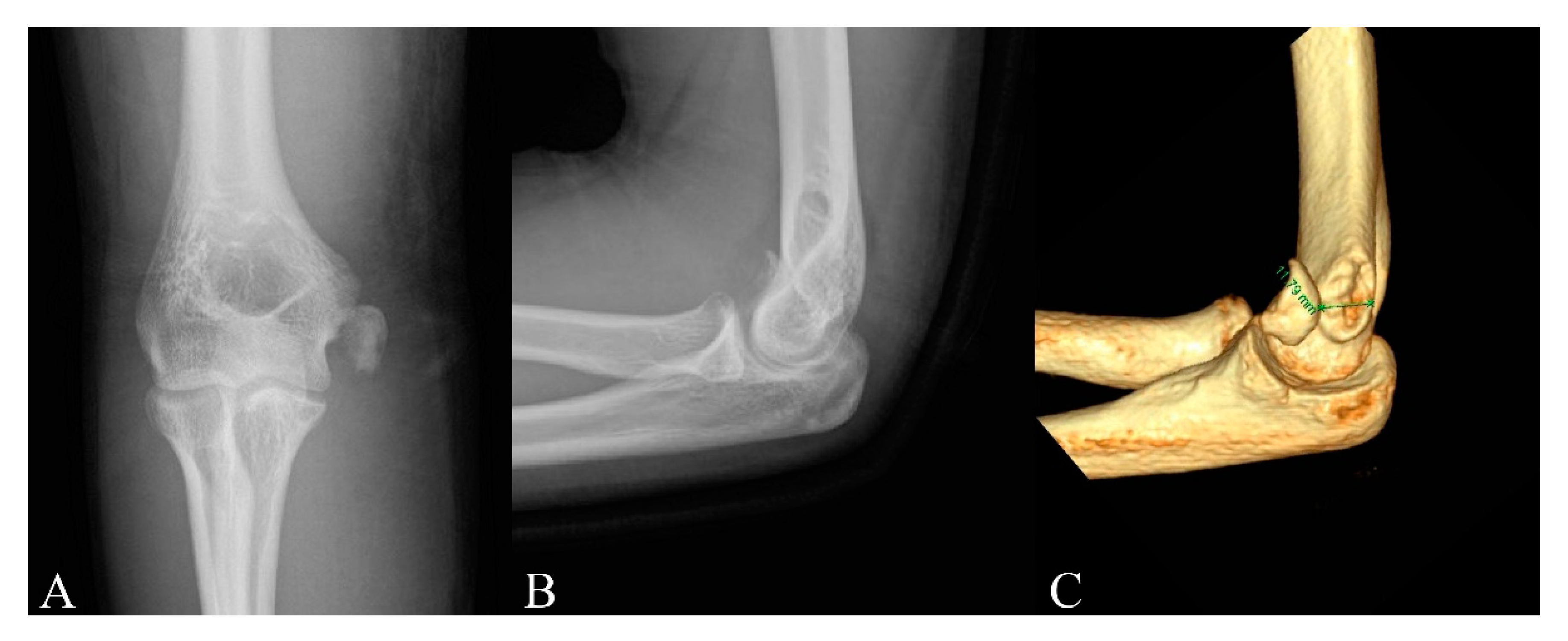
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gottschalk, H.P.; Eisner, E.; Hosalkar, H.S. Medial epicondyle fractures in the pediatric population. J. Am. Acad. Orthop. Surg. 2012, 20, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Ip, D.; Tsang, W.L. Medial humeral epicondylar fracture in children and adolescents. J. Orthop. Surg. 2007, 15, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.H.; Shen, H.C.; Chang, J.H.; Lee, C.H.; Wu, S.S. Operative treatment of displaced medial epicondyle fractures in children and adolescents. J. Shoulder Elb. Surg. 2005, 14, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Pathy, R.; Dodwell, E.R. Medial epicondyle fractures in children. Curr. Opin. Pediatrics 2015, 27, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Farsetti, P.; Potenza, V.; Caterini, R.; Ippolito, E. Long-term results of treatment of fractures of the medial humeral epicondyle in children. J. Bone Jt. Surg. Am. Vol. 2001, 83, 1299–1305. [Google Scholar] [CrossRef] [PubMed]
- Axibal, D.P.; Ketterman, B.; Skelton, A.; Carry, P.; Georgopoulos, G.; Miller, N.; Mayer, S.W. No difference in outcomes in a matched cohort of operative versus nonoperatively treated displaced medial epicondyle fractures. J. Pediatric Orthop. Part. B 2019, 28, 520–525. [Google Scholar] [CrossRef]
- Axibal, D.P.; Carry, P.; Skelton, A.; Mayer, S.W. No difference in return to sport and other outcomes between operative and nonoperative treatment of medial epicondyle fractures in pediatric upper-extremity athletes. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2018. [Google Scholar] [CrossRef]
- Lawrence, J.T.; Patel, N.M.; Macknin, J.; Flynn, J.M.; Cameron, D.; Wolfgruber, H.C.; Ganley, T.J. Return to competitive sports after medial epicondyle fractures in adolescent athletes: Results of operative and nonoperative treatment. Am. J. Sports Med. 2013, 41, 1152–1157. [Google Scholar] [CrossRef]
- Stepanovich, M.; Bastrom, T.P.; Munch, J., 3rd; Roocroft, J.H.; Edmonds, E.W.; Pennock, A.T. Does operative fixation affect outcomes of displaced medial epicondyle fractures? J. Child. Orthop. 2016, 10, 413–419. [Google Scholar] [CrossRef]
- Hughes, M.; Dua, K.; O’Hara, N.N.; Brighton, B.K.; Ganley, T.J.; Hennrikus, W.L.; Herman, M.J.; Hyman, J.E.; Lawrence, J.T.; Mehlman, C.T. Variation among pediatric orthopaedic surgeons when treating medial epicondyle fractures. J. Pediatric Orthop. 2019, 39, e592–e596. [Google Scholar] [CrossRef]
- Beck, J.J.; Bowen, R.E.; Silva, M. What’s new in pediatric medial epicondyle fractures? J. Pediatric Orthop. 2018, 38, e202–e206. [Google Scholar] [CrossRef] [PubMed]
- Edmonds, E.W. How displaced are “nondisplaced” fractures of the medial humeral epicondyle in children? Results of a three-dimensional computed tomography analysis. J. Bone Jt. Surg. Am. Vol. 2010, 92, 2785–2791. [Google Scholar] [CrossRef]
- Pappas, N.; Lawrence, J.T.; Donegan, D.; Ganley, T.; Flynn, J.M. Intraobserver and interobserver agreement in the measurement of displaced humeral medial epicondyle fractures in children. J. Bone Jt. Surg. Am. Vol. 2010, 92, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Onay, T.; Aydemir, A.N.; Okay, E.; Topkar, O.M.; Gulabi, D.; Erol, B. Does computerized tomography change the treatment decision in pediatric medial epicondyle fractures? Acta Orthop. Belg. 2019, 85, 79–85. [Google Scholar] [PubMed]
- Beals, R.K. The normal carrying angle of the elbow. A radiographic study of 422 patients. Clin. Orthop. Relat. Res. 1976, 119, 194–196. [Google Scholar] [CrossRef]
- Beaton, D.E.; Wright, J.G.; Katz, J.N. Development of the quickdash: Comparison of three item-reduction approaches. J. Bone Jt. Surg. Am. Vol. 2005, 87, 1038–1046. [Google Scholar]
- Biggers, M.D.; Bert, T.M.; Moisan, A.; Spence, D.D.; Warner, W.C., Jr.; Beaty, J.H.; Sawyer, J.R.; Kelly, D.M. Fracture of the medial humeral epicondyle in children: A comparison of operative and nonoperative management. J. Surg. Orthop. Adv. 2015, 24, 188–192. [Google Scholar]
- Kamath, A.F.; Baldwin, K.; Horneff, J.; Hosalkar, H.S. Operative versus non-operative management of pediatric medial epicondyle fractures: A systematic review. J. Child. Orthop. 2009, 3, 345–357. [Google Scholar] [CrossRef]
- Pezzutti, D.; Lin, J.S.; Singh, S.; Rowan, M.; Balch Samora, J. Pediatric medial epicondyle fracture management: A systematic review. J. Pediatric Orthop. 2020, 40, e697–e702. [Google Scholar] [CrossRef]
- Papavasiliou, V.A. Fracture-separation of the medial epicondylar epiphysis of the elbow joint. Clin. Orthop. Relat. Res. 1982, 171, 172–174. [Google Scholar] [CrossRef]
- García-Mata, S.; Arbeloa-Gutierrez, L.; Brun, M.; Sánchez-Guardamino, D. Prospective study of pediatric medial humeral epicondyle fractures nonoperatively treated. Clinical, radiologic, and functional evaluation at long term. J. Pediatric Orthop. Part. B 2020. [Google Scholar] [CrossRef]
- Dias, J.J.; Johnson, G.V.; Hoskinson, J.; Sulaiman, K. Management of severely displaced medial epicondyle fractures. J. Orthop. Trauma 1987, 1, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, V.S.; Arora, N.; Gehlot, H.; Saxena, S.; Kulkarni, S.G.; Bajwa, S. Symptomatic medial humeral epicondylar fracture non-union- rare presentation of a relatively common injury. Injury 2017, 48 (Suppl. 2), S50–S53. [Google Scholar] [CrossRef]
- Chorney, M.; Sylvestre, D.; Seeley, M. Medial epicondyle nonunions in children: Case report with overview and management. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2019, 3, e046. [Google Scholar] [CrossRef] [PubMed]
- Rickert, K.D.; Sarrel, K.L.; Sanders, J.S.; Jeffords, M.E.; Hughes, J.L.; Upasani, V.V.; Farnsworth, C.L.; Edmonds, E.W.; Pennock, A.T. Medial epicondyle fractures: Biomechanical evaluation and clinical comparison of 3 fixation methods used in pediatric patients. J. Pediatric Orthop. 2020, 40, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.F.; Vuillermin, C.; Naqvi, M.; Miller, P.E.; Bae, D.S.; Shore, B.J. Early outcomes of pediatric elbow dislocation-risk factors associated with morbidity. J. Pediatric Orthop. 2017, 37, 440–446. [Google Scholar] [CrossRef]

| Variables | Nonoperative (n = 21) | Operative (n = 56) | p-Value |
|---|---|---|---|
| Age at injury, year | 10.8 (7 to 15) | 11.6 (7 to 15) | 0.218 |
| Sex, n (%) | 0.380 | ||
| Male | 12 (57.1) | 38 (67.9) | |
| Female | 9 (42.9) | 18 (32.1) | |
| Dominant arm, n (%) | 13 (61.9) | 32 (57.1) | 0.706 |
| Fracture displacement, mm (range) | 8.7 (6 to 15) | 9.6 (5 to 20) | 0.262 |
| Immobilization period, week (range) | 4.1 (3 to 5) | 4.5 (2 to 6) | 0.118 |
| Radiological follow-up period, month | 7.6 (3 to 23) | 7.4 (3 to 20) | 0.884 |
| Union, n (%) | 5 (23.8) | 54 (96.4) | <0.001 |
| Quick DASH score | 1.3 (0 to 9.08) | 0.6 (0 to 9.08) | 0.169 |
| Score = 0, n (%) | 17 (81) | 47 (84) | |
| Score > 0, n (%) | 4 (19) | 9 (16) | |
| Functional follow-up period for phone survey, month | 36.6 (6 to 70) | 40.1 (6 to 70) | 0.456 |
| Patients with restoration of full ROM, n (%) | 16 (76.2) | 46 (82.1) | 0.557 |
| Time to restore full ROM, week | 9.6 (6 to 12) | 12.6 (7 to 20) | <0.001 |
| Within 3 months, n (%) | 16 (100) | 30 (65.2) | |
| Cubitus valgus, n (%) | 4 (19) | 3 (5.4) | 0.063 |
| Variables | K-Wire (n = 31) | Screw (n = 25) | p-Value |
|---|---|---|---|
| Age at injury, year | 11.1 (7 to 14) | 12.3 (8 to 15) | 0.083 |
| Sex, n (%) | 0.081 | ||
| Male | 18 (57.1) | 20 (80) | |
| Female | 13 (42.9) | 5 (20) | |
| Dominant arm, n (%) | 17 (54.8) | 15 (60) | 0.698 |
| Fracture displacement, mm (range) | 9.4 (5 to 14) | 10.1 (5 to 20) | 0.496 |
| Immobilization period, week (range) | 5.6 (4 to 6) | 3.3 (2 to 4) | <0.001 |
| Radiological follow-up period, month | 6.8 (3 to 20) | 8.1 (3 to 18) | 0.232 |
| Quick DASH score | 0.4 (0 to 4.50) | 0.7 (0 to 9.08) | 0.502 |
| Score = 0, n (%) | 27 (87) | 20 (80) | |
| Score > 0, n (%) | 4 (13) | 5 (20) | |
| Functional follow-up period for phone survey, month | 45.2 (6 to 70) | 36.9 (6 to 70) | 0.196 |
| Patients with restoration of full ROM, n (%) | 26 (83.9) | 20 (80) | 0.707 |
| Time to restore full ROM, week | 13.5 (8 to 20) | 11.3 (7 to 16) | 0.008 |
| Within 3 months, n (%) | 14 (53.8) | 16 (80) | |
| Cubitus valgus, n (%) | 1 (3.2) | 2 (8) | 0.430 |
| Variables | Nonoperative (n = 21) | K-Wire (n = 31) | Screw (n = 25) |
|---|---|---|---|
| Nonunion, n (%) | 16 (76.2) | 0 (0) | 2 (8) |
| Limitation of full ROM, n | 5 | 5 | 5 |
| <15 degrees | 2 | 5 | 5 |
| >15 degrees | 3 | 0 | 0 |
| Symptomatic nonunion with valgus instability, n | 3 | 0 | 0 |
| Cubitus valgus, n | 4 | 1 | 2 |
| Superficial wound infection, n | N/A | 2 | 0 |
| Fragment breakage, n | N/A | 0 | 1 |
| Subsequent surgery, n | |||
| Osteosynthesis | 2 | 0 | 0 |
| Excision of bony fragment | 1 | 0 | 0 |
| Removal of hardware | 0 | 0 | 18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Kim, H.W.; Park, K.-B.; Hong, K.-B.; Park, H. Is Computed Tomography Necessary for Diagnostic Workup in Displaced Pediatric Medial Epicondyle Fractures? Diagnostics 2020, 10, 957. https://doi.org/10.3390/diagnostics10110957
Kim S, Kim HW, Park K-B, Hong K-B, Park H. Is Computed Tomography Necessary for Diagnostic Workup in Displaced Pediatric Medial Epicondyle Fractures? Diagnostics. 2020; 10(11):957. https://doi.org/10.3390/diagnostics10110957
Chicago/Turabian StyleKim, Sungmin, Hyun Woo Kim, Kun-Bo Park, Kee-Bum Hong, and Hoon Park. 2020. "Is Computed Tomography Necessary for Diagnostic Workup in Displaced Pediatric Medial Epicondyle Fractures?" Diagnostics 10, no. 11: 957. https://doi.org/10.3390/diagnostics10110957
APA StyleKim, S., Kim, H. W., Park, K.-B., Hong, K.-B., & Park, H. (2020). Is Computed Tomography Necessary for Diagnostic Workup in Displaced Pediatric Medial Epicondyle Fractures? Diagnostics, 10(11), 957. https://doi.org/10.3390/diagnostics10110957






