Midshaft Clavicle Fractures Treated Nonoperatively Using Figure-of-Eight Bandage: Are Fracture Type, Shortening, and Displacement Radiographic Predictors of Failure?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
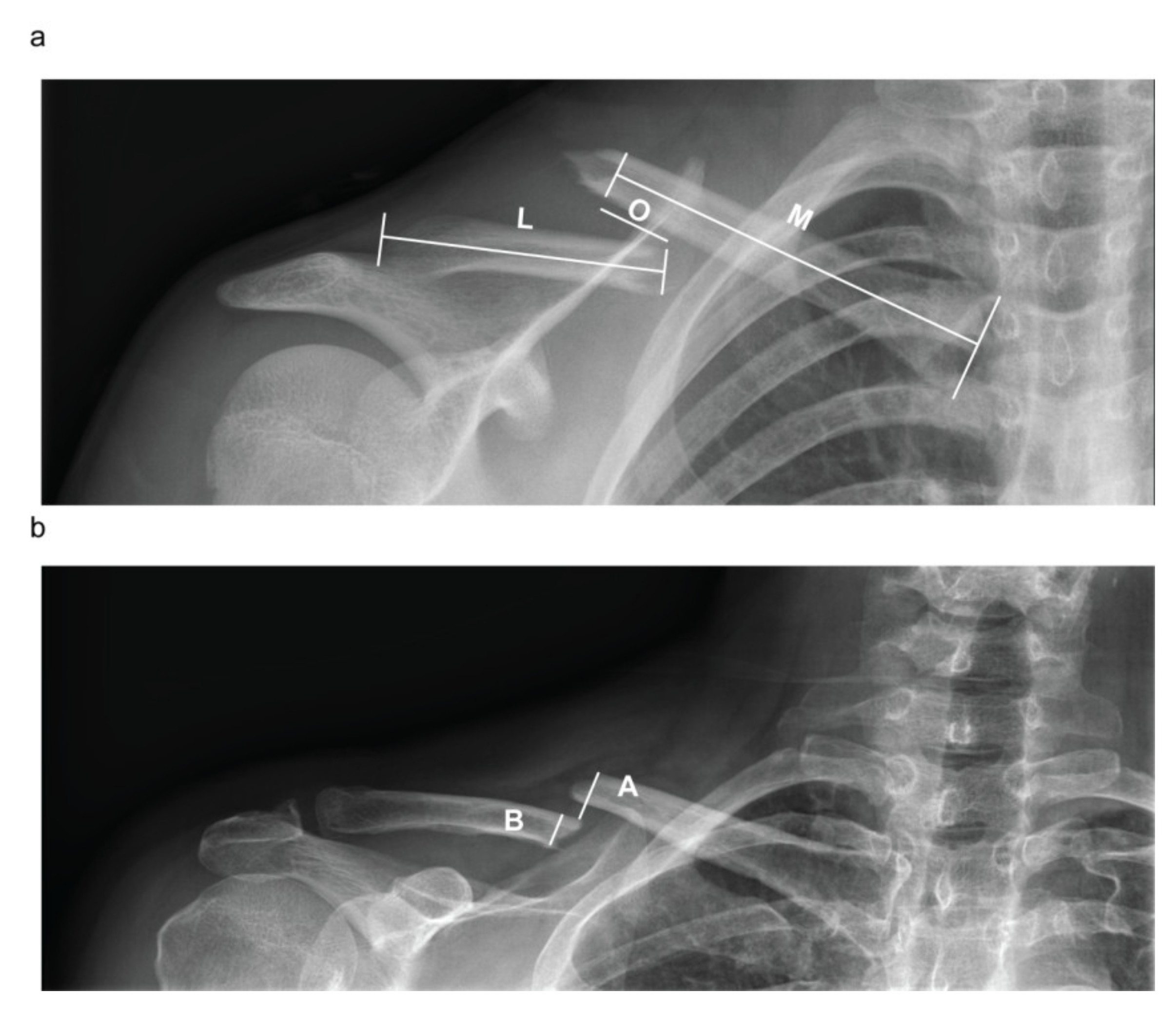
2.2. Patient Assessment and Evaluation of the Radiographic Outcomes
2.3. Nonoperative Treatment and Follow-Up Program
2.4. Statistical Analysis
3. Results
Patient Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Coppa, V.; Dei Giudici, L.; Cecconi, S.; Marinelli, M.; Gigante, A. Midshaft clavicle fractures treatment: Threaded Kirschner wire versus conservative approach. Strateg. Trauma Limb Reconstr. (Online) 2017, 12, 141–150. [Google Scholar]
- Nordqvist, A.; Petersson, C. The incidence of fractures of the clavicle. Clin. Orthop. Relat. Res. 1994, 127–132. [Google Scholar] [CrossRef]
- Postacchini, F.; Gumina, S.; De Santis, P.; Albo, F. Epidemiology of clavicle fractures. J. Shoulder Elb. Surg. 2002, 11, 452–456. [Google Scholar] [CrossRef]
- Herteleer, M.; Winckelmans, T.; Hoekstra, H.; Nijs, S. Epidemiology of clavicle fractures in a level 1 trauma center in Belgium. Eur. J. Trauma Emerg. Surg. 2017, 44, 717–726. [Google Scholar] [CrossRef]
- Robinson, C.M. Fractures of the clavicle in the adult. Epidemiology and classification. J. Bone Jt. Surg. Br. Vol. 1998, 80, 476–484. [Google Scholar] [CrossRef]
- Ledger, M.; Leeks, N.; Ackland, T.; Wang, A. Short malunions of the clavicle: An anatomic and functional study. J. Shoulder Elb. Surg. 2005, 14, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Naveen, B.M.; Joshi, G.R.; Harikrishnan, B. Management of mid-shaft clavicular fractures: Comparison between non-operative treatment and plate fixation in 60 patients. Strateg. Trauma Limb Reconstr. (Online) 2017, 12, 11–18. [Google Scholar] [CrossRef]
- Oki, S.; Matsumura, N.; Kiriyama, Y.; Iwamoto, T.; Sato, K.; Nagura, T. Three-Dimensional Deformities of Nonoperative Midshaft Clavicle Fractures: A Surface Matching Analysis. J. Orthop. Trauma 2017, 31, e385–e389. [Google Scholar] [CrossRef]
- Van Tongel, A.; De Wilde, L. Sternoclavicular joint injuries: A literature review. Muscles Ligaments Tendons J. 2011, 1, 100–105. [Google Scholar]
- Lenza, M.; Belloti, J.C.; Andriolo, R.B.; Faloppa, F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst. Rev. 2014, Cd007121. [Google Scholar] [CrossRef]
- McKee, R.C.; Whelan, D.B.; Schemitsch, E.H.; McKee, M.D. Operative versus nonoperative care of displaced midshaft clavicular fractures: A meta-analysis of randomized clinical trials. J. Bone Jt. Surg. Am. Vol. 2012, 94, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Rehn, C.H.; Kirkegaard, M.; Viberg, B.; Larsen, M.S. Operative versus nonoperative treatment of displaced midshaft clavicle fractures in adults: A systematic review. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2014, 24, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.H.; Guo, W.J.; Li, A.B.; Cheng, G.J.; Lei, T.; Zhao, Y.M. Operative versus nonoperative treatment for displaced midshaft clavicle fractures: A meta-analysis based on current evidence. Clinics 2015, 70, 584–592. [Google Scholar] [CrossRef]
- Hoogervorst, P.; van Schie, P.; van den Bekerom, M.P. Midshaft clavicle fractures: Current concepts. EFORT Open Rev. 2018, 3, 374–380. [Google Scholar] [CrossRef]
- Frima, H.; van Heijl, M.; Michelitsch, C.; van der Meijden, O.; Beeres, F.J.P.; Houwert, R.M.; Sommer, C. Clavicle fractures in adults; current concepts. Eur. J. Trauma Emerg. Surg. 2020, 46, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Neer, C.S., 2nd. Nonunion of the clavicle. J. Am. Med. Assoc. 1960, 172, 1006–1011. [Google Scholar] [CrossRef] [PubMed]
- Rowe, C.R. An atlas of anatomy and treatment of midclavicular fractures. Clin. Orthop. Relat. Res. 1968, 58, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Tagliapietra, J.; Angelini, A.; Belluzzi, E.; Pozzuoli, A.; Berizzi, A.; Ruggieri, P. The challenging management of a delayed union midshaft clavicle fracture complicated by an acute pseudoaneurysm of the subclavian artery in a superelderly diabetic patient. Aging Clin. Exp. Res. 2019, 31, 567–569. [Google Scholar] [CrossRef]
- Robinson, C.M.; Goudie, E.B.; Murray, I.R.; Jenkins, P.J.; Ahktar, M.A.; Read, E.O.; Foster, C.J.; Clark, K.; Brooksbank, A.J.; Arthur, A.; et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: A multicenter, randomized, controlled trial. J. Bone Jt. Surg. Am. Vol. 2013, 95, 1576–1584. [Google Scholar] [CrossRef]
- Tamaoki, M.J.S.; Matsunaga, F.T.; Costa, A.; Netto, N.A.; Matsumoto, M.H.; Belloti, J.C. Treatment of Displaced Midshaft Clavicle Fractures: Figure-of-Eight Harness Versus Anterior Plate Osteosynthesis: A Randomized Controlled Trial. J. Bone Jt. Surg. Am. Vol. 2017, 99, 1159–1165. [Google Scholar] [CrossRef]
- Zlowodzki, M.; Zelle, B.A.; Cole, P.A.; Jeray, K.; McKee, M.D. Treatment of acute midshaft clavicle fractures: Systematic review of 2144 fractures: On behalf of the Evidence-Based Orthopaedic Trauma Working Group. J. Orthop. Trauma 2005, 19, 504–507. [Google Scholar] [CrossRef] [PubMed]
- Nowak, J.; Holgersson, M.; Larsson, S. Can we predict long-term sequelae after fractures of the clavicle based on initial findings? A prospective study with nine to ten years of follow-up. J. Shoulder Elb. Surg. 2004, 13, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, A.; Troelsen, A.; Ban, I. Predictors associated with nonunion and symptomatic malunion following non-operative treatment of displaced midshaft clavicle fractures—A systematic review of the literature. Int. Orthop. 2014, 38, 2543–2549. [Google Scholar] [CrossRef] [PubMed]
- Housner, J.A.; Kuhn, J.E. Clavicle fractures: Individualizing treatment for fracture type. Physician Sportsmed. 2003, 31, 30–36. [Google Scholar] [CrossRef]
- Lenza, M.; Faloppa, F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst. Rev. 2016, 12, Cd007121. [Google Scholar] [CrossRef]
- Onizuka, N.; Anderson, J.P.; Gilbertson, J.A.; MacCormick, L.M.; Cole, P.A. Displacement of diaphyseal clavicle fractures related to patient position and progressive displacement in the peri-injury period. J. Shoulder Elb. Surg. 2018, 27, 667–673. [Google Scholar] [CrossRef]
- Stegeman, S.A.; Fernandes, N.C.; Krijnen, P.; Schipper, I.B. Online radiographic survey of midshaft clavicular fractures: No consensus on treatment for displaced fractures. Acta Orthop. Belg. 2014, 80, 161–165. [Google Scholar]
- van der Meijden, O.A.; Gaskill, T.R.; Millett, P.J. Treatment of clavicle fractures: Current concepts review. J. Shoulder Elb. Surg. 2012, 21, 423–429. [Google Scholar] [CrossRef]
- Marsh, J.L.; Slongo, T.F.; Agel, J.; Broderick, J.S.; Creevey, W.; DeCoster, T.A.; Prokuski, L.; Sirkin, M.S.; Ziran, B.; Henley, B.; et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J. Orthop. Trauma 2007, 21 (Suppl. S10), S1–S133. [Google Scholar] [CrossRef]
- Woltz, S.; Stegeman, S.A.; Krijnen, P.; van Dijkman, B.A.; van Thiel, T.P.; Schep, N.W.; de Rijcke, P.A.; Frolke, J.P.; Schipper, I.B. Plate Fixation Compared with Nonoperative Treatment for Displaced Midshaft Clavicular Fractures: A Multicenter Randomized Controlled Trial. J. Bone Jt. Surg. Am. Vol. 2017, 99, 106–112. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014. [Google Scholar]
- Louviere, J.J.; Hensher, D.A.; Swait, J.D. Stated Choice Methods: Analysis and Applications; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Hill, J.M.; McGuire, M.H.; Crosby, L.A. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J. Bone Jt. Surg. Br. Vol. 1997, 79, 537–539. [Google Scholar] [CrossRef]
- Kirmani, S.J.; Pillai, S.K.; Madegowda, B.R.; Shahane, S.A. Vertical fragment in adult midshaft clavicle fractures: An indicator for surgical intervention. Orthopedics 2009, 32, 726–730. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, K.J.; Remes, V.; Pajarinen, J.; Savolainen, V.; Bjorkenheim, J.M.; Paavola, M. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: A randomized clinical trial. J. Bone Jt. Surg. Am. Vol. 2012, 94, 1546–1553. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, G.S.d.L.; Tamaoki, M.J.S.; Dragone, B.; Utino, A.Y.; Netto, N.A.; Matsumoto, M.H.; Matsunaga, F.T. Correlation of the degree of clavicle shortening after non-surgical treatment of midshaft fractures with upper limb function. BMC Musculoskel. Disord. 2015, 16, 151. [Google Scholar] [CrossRef] [PubMed]
- Fuglesang, H.F.S.; Flugsrud, G.B.; Randsborg, P.-H.; Stavem, K.; Utvåg, S.E. Radiological and functional outcomes 2.7 years following conservatively treated completely displaced midshaft clavicle fractures. Arch. Orthop. Trauma Surg. 2016, 136, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Murray, I.R.; Foster, C.J.; Eros, A.; Robinson, C.M. Risk factors for nonunion after nonoperative treatment of displaced midshaft fractures of the clavicle. J. Bone Jt. Surg. Am. Vol. 2013, 95, 1153–1158. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, B.P.; McLaren, A.; Richardson, M.; McLemore, R. Clavicular length: The assumption of symmetry. Orthopedics 2013, 36, e343–e347. [Google Scholar] [CrossRef][Green Version]
- De Giorgi, S.; Notarnicola, A.; Tafuri, S.; Solarino, G.; Moretti, L.; Moretti, B. Conservative treatment of fractures of the clavicle. BMC Res. Notes 2011, 4, 333. [Google Scholar] [CrossRef]
- Andermahr, J.; Jubel, A.; Elsner, A.; Prokop, A.; Tsikaras, P.; Jupiter, J.; Koebke, J. Malunion of the clavicle causes significant glenoid malposition: A quantitative anatomic investigation. Surg. Radiol. Anat. SRA 2006, 28, 447–456. [Google Scholar] [CrossRef]
- Hillen, R.J.; Burger, B.J.; Poll, R.G.; van Dijk, C.N.; Veeger, D.H. The effect of experimental shortening of the clavicle on shoulder kinematics. Clin. Biomech. (BristolAvon) 2012, 27, 777–781. [Google Scholar] [CrossRef]
- Su, W.R.; Chen, W.L.; Chen, R.H.; Hong, C.K.; Jou, I.M.; Lin, C.L. Evaluation of three-dimensional scapular kinematics and shoulder function in patients with short malunion of clavicle fractures. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2016, 21, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Lazarides, S.; Zafiropoulos, G. Conservative treatment of fractures at the middle third of the clavicle: The relevance of shortening and clinical outcome. J. Shoulder Elb. Surg. 2006, 15, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Heuer, H.J.; Boykin, R.E.; Petit, C.J.; Hardt, J.; Millett, P.J. Decision-making in the treatment of diaphyseal clavicle fractures: Is there agreement among surgeons? Results of a survey on surgeons’ treatment preferences. J. Shoulder Elb. Surg. 2014, 23, e23–e33. [Google Scholar] [CrossRef] [PubMed]
- Lenza, M.; Taniguchi, L.F.P.; Ferretti, M. Figure-of-eight bandage versus arm sling for treating middle-third clavicle fractures in adults: Study protocol for a randomised controlled trial. Trials 2016, 17, 229. [Google Scholar] [CrossRef] [PubMed]
- Ersen, A.; Atalar, A.C.; Birisik, F.; Saglam, Y.; Demirhan, M. Comparison of simple arm sling and figure of eight clavicular bandage for midshaft clavicular fractures: A randomised controlled study. Bone Jt. J. 2015, 97-b, 1562–1565. [Google Scholar] [CrossRef]

| Patients Enrolled (122) | |
|---|---|
| Age, mean (SD) Median (range) | 37 (12.7) 38 (62–18) |
| Sex, Female (%) Male (%) | 19 (15.6) 103 (84.4) |
| Type of fractures (FT), number (%) A1 A2 A3 B1 B2 B3 | 9 (7.4) 31 (25.4) 12 (9.8) 10 (8.2) 23 (18.9) 37 (30.3) |
| Type of fractures (FT), number (%) A B | 52 (42.6) 70 (57.4) |
| Fracture healed within 12 weeks, number (%) Delayed union Nonunion | 81 (66.4) 24 (19.7) 17 (13.9) |
| Initial shortening % (IS), median (range) | 0 (12–0) |
| Residual shortening % (RS), median (range) | 0 (12–0) |
| Initial displacement % (ID), median (range) | 114.5 (230–16) |
| Residual displacement % (RD), median (range) | 100 (185–10) |
| Variable | Healed Fracture (81/122) | Delayed Union (24/122) | Nonunion (17/122) | p-Value (Kruskal–Wallis) |
|---|---|---|---|---|
| Age, mean (SD) Median (range) | 37.4 (11.7) 38 (61–18) | 36.2 (14.5) 36.5 (62–18) | 39.5 (14.5) 38 (60–18) | 0.720 |
| Type of fracture, % (number/total n =122) A1 A2 A3 B1 B2 B3 | 66.7 (6/9) 67.7 (21/31) 25 (3/12) 60 (6/10) 86.7 (20/23) 67.6 (25/37) | 11.1 (1/9) 19.4 (6/31) 33.3 (4/12) 30 (3/10) 8.7 (2/23) 21.6 (8/37) | 22.2 (2/9) 12.9 (4/31) 41.7 (5/12) 10 (1/10) 4.3 (1/23) 10.8 (4/37) | 0.494 |
| Type of fracture (FT), % (number/total n =122) A B | 57.7 (30/52) 72.8 (51/70) | 21.15 (11/52) 18.6 (13/70) | 21.15 (11/52) 8.6 (6/70) | χ2 0.10 |
| Initial shortening % (IS), median (range) | 0 (12–0) | 3.85 (11–0) | 2 (10–0) | 0.15 |
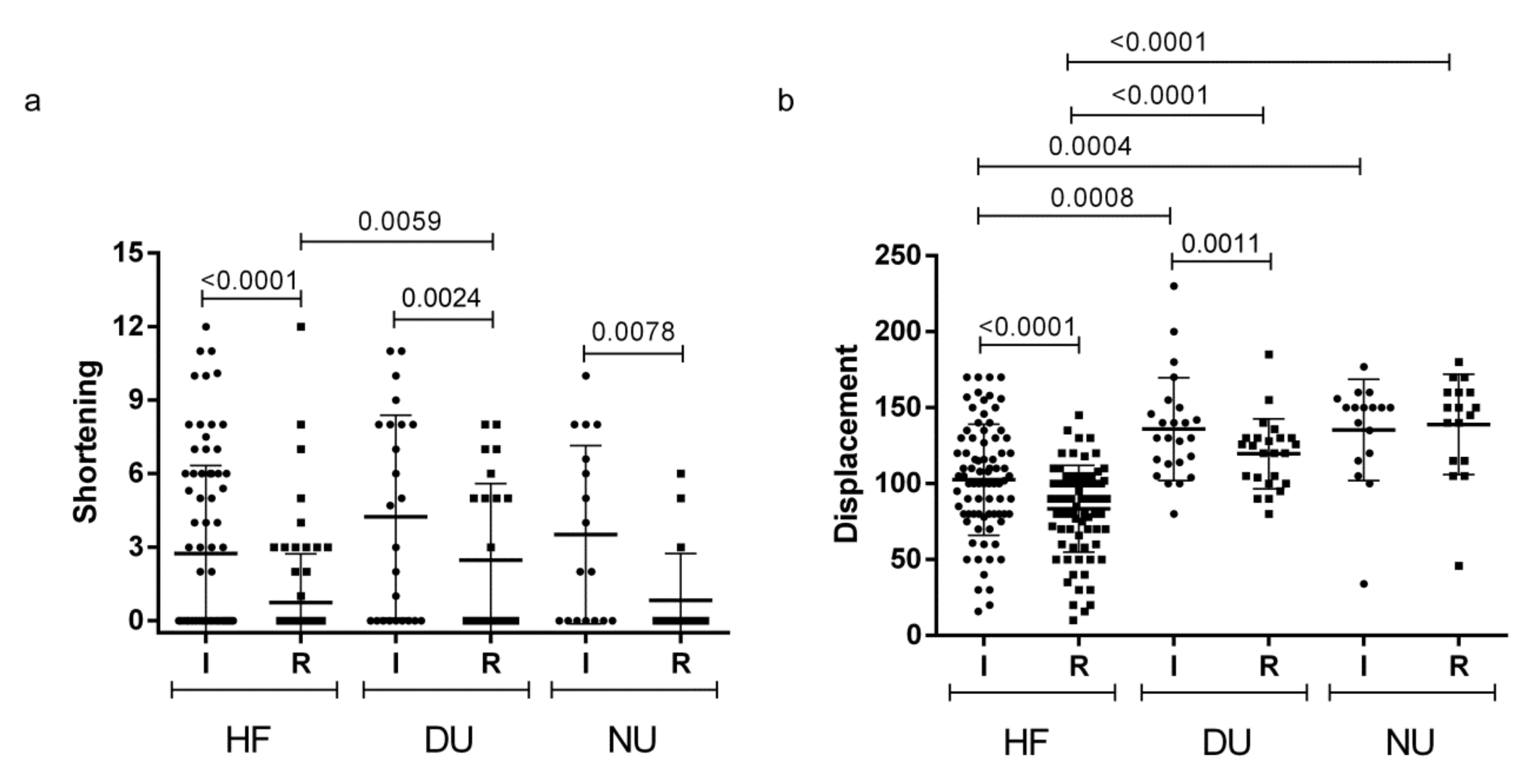
| Residual shortening % (RS), median (range) | 0 (12–0) | 0 (8–0) | 0 (6–0) | 0.014 * 0.0059 § 1 # 0.06571 |
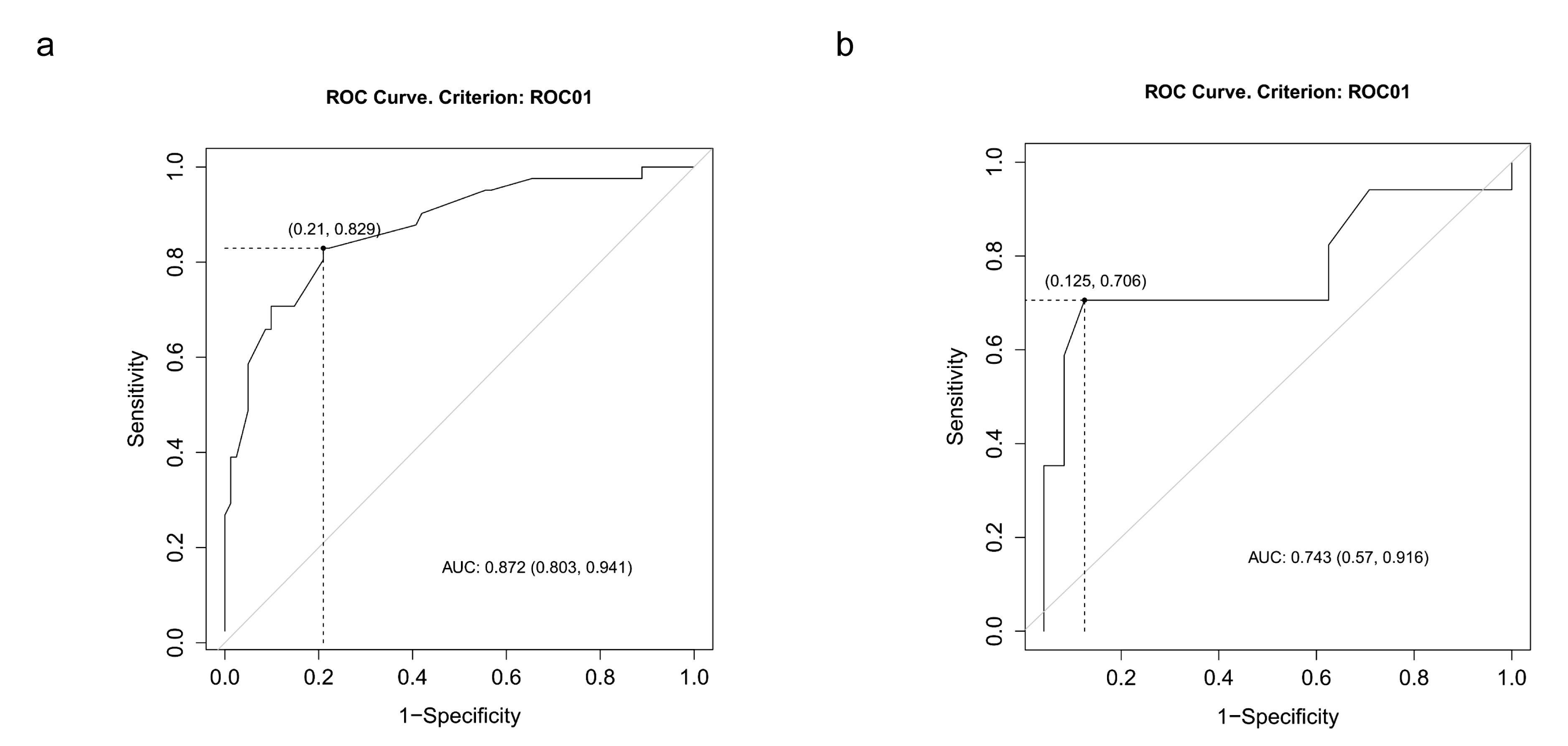
| Initial displacement % (ID), median (range) | 102 (170–16) | 130 (230–80) | 150 (177–34) | <0.0001 * 0.0008 § 0.0004 # 0.890 |
| Residual displacement % (RD), median (range) | 90 (145–10) | 122.5 (185–80) | 150 (180–46) | <0.0001 * <0.0000 § <0.0000 # 0.2425 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tagliapietra, J.; Belluzzi, E.; Biz, C.; Angelini, A.; Fantoni, I.; Scioni, M.; Bolzan, M.; Berizzi, A.; Ruggieri, P. Midshaft Clavicle Fractures Treated Nonoperatively Using Figure-of-Eight Bandage: Are Fracture Type, Shortening, and Displacement Radiographic Predictors of Failure? Diagnostics 2020, 10, 788. https://doi.org/10.3390/diagnostics10100788
Tagliapietra J, Belluzzi E, Biz C, Angelini A, Fantoni I, Scioni M, Bolzan M, Berizzi A, Ruggieri P. Midshaft Clavicle Fractures Treated Nonoperatively Using Figure-of-Eight Bandage: Are Fracture Type, Shortening, and Displacement Radiographic Predictors of Failure? Diagnostics. 2020; 10(10):788. https://doi.org/10.3390/diagnostics10100788
Chicago/Turabian StyleTagliapietra, Jacopo, Elisa Belluzzi, Carlo Biz, Andrea Angelini, Ilaria Fantoni, Manuela Scioni, Mario Bolzan, Antonio Berizzi, and Pietro Ruggieri. 2020. "Midshaft Clavicle Fractures Treated Nonoperatively Using Figure-of-Eight Bandage: Are Fracture Type, Shortening, and Displacement Radiographic Predictors of Failure?" Diagnostics 10, no. 10: 788. https://doi.org/10.3390/diagnostics10100788
APA StyleTagliapietra, J., Belluzzi, E., Biz, C., Angelini, A., Fantoni, I., Scioni, M., Bolzan, M., Berizzi, A., & Ruggieri, P. (2020). Midshaft Clavicle Fractures Treated Nonoperatively Using Figure-of-Eight Bandage: Are Fracture Type, Shortening, and Displacement Radiographic Predictors of Failure? Diagnostics, 10(10), 788. https://doi.org/10.3390/diagnostics10100788









