Abstract
Although 2-deoxy-2-[18F]-fluoro-D-glucose positron emission tomography/computed tomography (18F-FDG PET/CT) is a sensitive nuclear medicine modality, specificity for characterizing lung cancer is limited. Tumor proliferation and early response to molecularly targeted therapy could be visualized using 3′-deoxy-3′[(18)F]-fluorothymidine (18F-FLT) PET/CT. The superiority of 18F-FLT PET/CT over 18F-FDG PET/CT in early therapeutic monitoring has been well described in patients after chemotherapy, radiotherapy, and/or chemo/radiotherapy. In thispilot study, we explorethe use of 18F-FLT PET/CT as an early response evaluation modality in patients with lung cancerand provide specific case studies of patients with small cell lung cancer and non-small cell lung cancer who received novel targeted therapies. Early response for c-MET inhibitor was observed in four weeks and for MDM2 inhibitor in nine days.
1. Introduction
18F-fluorothymidine, [18F]3-deoxy-3-fluorothymidine (18F-FLT), is an imaging biomarker of cellular proliferation and has been utilized in various cancer types including blood (lymphoma and leukemia), breast, head and neck, esophageal, and lung cancers as well as in bone and soft tissue sarcomas [1,2,3,4,5]. 18F-FLT is derived from the cytostatic drug azidovudine developed for positron emission tomography (PET) imaging [6]. Its main role is in evaluating treatment response [1] by indirect monitoring of cell proliferation based on DNA synthesis. 18F-FLT is basically a radiolabeled structural analog of thymidine, which is a constituent nucleoside of DNA. Although 18F-FLT is not incorporated into DNA (or at least selectively), it reflects the level of DNA synthesis because of its entrapment inside the cell through phosphorylation by thymidine kinase-1 (TK1) expressed during the S-phase of DNA synthesis [7]. Precisely, 18F-FLT uptake in malignant cells correlate with activity of TK1 which is usually low in the cell resting stage but high in the deregulated cancer cell cycle.
In contrast with the most widely-used radiotracer for PET/CT imaging, the 2-deoxy-2-[18F]-fluoro-D-glucose (8F-FDG), 18F-FLT shows a lower accumulation in tumors than 18F-FDG as it only accumulates in cells that are in the S-phase of growth and demonstrates a low sensitivity for nodal staging in lung cancer. In addition, only 8–20% of the cells are in the S-phase, so in comparison to glucose metabolism and 18F-FDG accumulation, absolute accumulation of TK1-catalyzed radioactivity is relatively low. In spite of these limitations, 18F-FLT has shown to be superior in imaging proliferation [8,9,10]. In a meta-analysis of 27 articles involving 1213 lung cancer patients for correlating FDG uptake (22 studies) or FLT uptake (eight studies) with Ki-67 expression, the rho coefficient for 18F-FDG/Ki-67 and 18F-FLT/Ki-67 was 0.45 (95% CI, 0.41–0.50) and 0.65 (95% CI, 0.56–0.73), respectively, which indicated a moderate correlation for 18F-FDG and a significant one for 18F-FLT [8].
It has been shown that shortcomings of 18F-FLT and 18F-FDG can be theoretically solved with dual tracer imaging studies [11,12,13,14,15]. For instance, in 55 patients with pulmonary nodules who underwent 18F-FDG PET/CT and 18F-FLT PET/CT within seven days, the sensitivity and specificity for 18F-FDG PET/CT was 87.5% and 58.9% and for 18F-FLT PET/CT was 68.7% and 76.9%, respectively. The combination of 18F-FLT and 18F-FDG improved sensitivity up to 100% and specificity up to 89.7% [13]. This dual tracer imaging induced substantial change in clinical management of 31.5% of patients with pulmonary lesions and partial change in another 12.3% [14,15]. In a meta-analysis pooled from 17 studies [12] including 548 patients with malignant and benign lung lesions (bronchioloalveolar lung carcinoma, squamous cell carcinoma, non-small cell lung cancer, small cell lung cancer, adenocarcinoma, tuberculosis, fibromas, hamartomas, etc.), it showed that although 18F-FLT cannot replace 18F-FDG in detecting small cell lung cancer and early development of lung cancer, it may help to prevent patients with misdiagnosis of inflammatory lesions.
To date, there are no clinical studies of 18F-FLT PET/CT of novel targeted therapiesin assessing early response in lung cancer. c-MET inhibitors, have the potential to benefit subsets of lung cancer patients with specific genetic alterations [16]. Exon-14 skipping mutations appear so far to be the most promising molecular subset that is sensitive to c-MET inhibitors, whereas overexpression, amplification, and point mutations of MET seem more challenging subgroups to target [17]. Combination with other target agents, such as EGFR inhibitors, may represent a promising therapeutic strategy in specific areas (e.g., EGFR-TKI resistance), because HGF/c-MET pathway mediates VEGFR inhibitor resistance and vascular remodeling in NSCLC [18]. Mouse double minute 2 protein (MDM2) is a regulator of tumor suppressor P53. Inhibitors of MDM2 are in clinical development.
In this pilot study, we evaluated the early treatment response for. c-MET inhibitor and mdm-2 inhibitor in lung cancer. We show that early assessment of therapy response from these two new drugs was feasible with 18F-FLT PET/CT imaging and that the combination with 18F-FDG PET/CT would have more potential.
2. Materials and Methods
We reviewed the medical records of patients with advanced lung cancer (small cell and non-small cell lung cacer) who had FLT/PET imaging as part of their care at MD Anderson. This study was performed in accordance with the guidelines of the MD Anderson Institutional Review Board (IRB). Because this was a retrospective chart review IRB has waived the consent requirements. They were enrolled on c-MET inhibitor and MDM2 inhibitor based trials available in the institution. This study was compliant with the Health Insurance Portability and Accountability Act. Written informed consent was obtained from each participant for enrollment on the respective clinical trials.
2.1. PET/CT Study
PET/CT studies were performed using a Discovery ST8 PET/CT system (GE Healthcare) in combination with the CT, 8-MDCT scanner (LightSpeed, GE Healthcare). 18F-FLT (200–350 MBq) or 18F-FDG (10–15 MBq) was administered intravenously in a single dose injection. Whole-body PET imaging (WB PET) consisted of four or five 10 min bed positions, approximately 60 min from injection. PET images were reconstructed using standard vendor-provided algorithms. The CT consisted of a helical scan covering the head to the mid thighs (120 kVp, 300 mA, 0.5-s rotation; table speed, 13.5 mm/rotation) with no contrast enhancement. Axial CT slice thickness was 3.75 mm. The PET data was corrected for random coincidences, scatter, and attenuation. Transaxial images were reconstructed into 128 × 128 pixel matrices with a pixel size of at least 4.5 mm, using vendor-provided algorithms that incorporate ordered-subset expectation maximization and were corrected for attenuation using CT data; the emission data was corrected for scatter, random events, and dead-time losses as well, using the PET/CT scanner’s standard algorithms. Measures of uptake and retention in tumors were obtained from the WB PET data and compared to normal tissue.
2.2. 18F-FLT PET/CT Scan Interpretation
Blinded image interpretation was performed by two experienced nuclear medicine physicians (KK, EBS) with more than 20 years of experience in the field. 18F-FLT PET/CT uptake of target lesions was evaluated visually as present or absent, graded on a 3-point scale. After the final interpretation/score entered for each patient, the same reviewers determined the maximum standardized uptake value (SUV) for each residual mass/lesion by CT, regardless whether it was FLT-PET negative.
3. Results
Presented here are case studies of patients with biopsy-proven lung cancer in a clinical trial for 18F-FLT PET/CT monitoring of treatment response. Table 1 summarizes the results of these studies.

Table 1.
Summary of the study. Patient characteristics (age, gender, diagnosis), new therapy, previous therapies, and the scan changes in the current study (FLT-PET/CT, FDG-PET/CT and CT).
Patient 1: The first patient in the case study is a 49-year-old male with small cell lung cancer who received cisplatin and etoposide as standard therapy. After progression from standard therapy, the patient was placed on a c-MET inhibitor therapy. We compared conventional CT, FLT-PET/CT, and FDG-PET/CT scans pre- and post-four weeks of targeted therapy (Figure 1). In this patient, the pre-therapy tumor CT measurements were 1.5 cm × 0.7 cm, which remained unchanged post therapy after four weeks. While the 18F-FDG PET/CT showed a 2% increase in SUVmax from 1.64 to 1.67, 18F-FLT PET/CT showed a reduction in metabolic activity of 38% from 1.3 to 0.8 SUVmax (Figure 1).
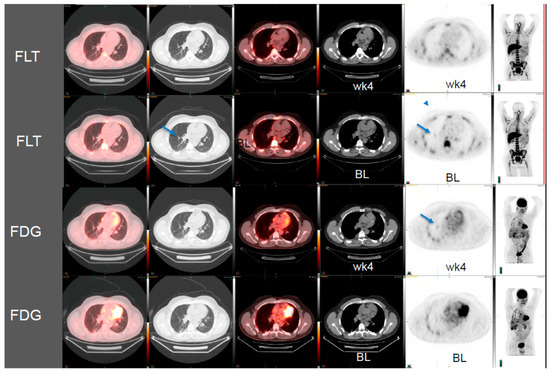
Figure 1.
3′-deoxy-3′[(18)F]-fluorothymidine (18F-FLT) positron emission tomography/computed tomography (PET/CT) scans shows early response to c-MET inhibitor targeted therapy whereas the conventional CT scan and 2-deoxy-2-[18F]-fluoro-D-glucose (18F-FDG) PET/CT images do not show any responses in this patient with small cell lung cancer (BL, baseline; wk4, at 4 weeks post therapy).Arrows show the location of tumors.
Patient 2: This is a 51-year-old female with a history of relapsed and refractory lung adenocarcinoma. This patient received several lines of therapy that included erlotinib, carboplatin, gemcitabine/docetaxel, pemetrexed, sorafenib, irinotecan, and then bevacizumab. After progression on standard therapy, the patient was enrolled in a c-MET inhibitor-targeted-therapy clinical trial. At that time, she presented with a right hilar mass (Figure 2). The two-dimensional CT tumor measurements were 5.2 cm × 4.6 cm and post therapy were 5.3 cm × 4.8 cm. The change corresponds to a 2% increase in tumor size. However, the 18F-FLT PET/CT imaging pre- and post-therapy after four weeks revealed a SUVmax of 5.1 and 3.9, respectively, which was a 24% reduction in 18F-FLT activity. Although not significant statistically, it was a clinically significant response to therapy.
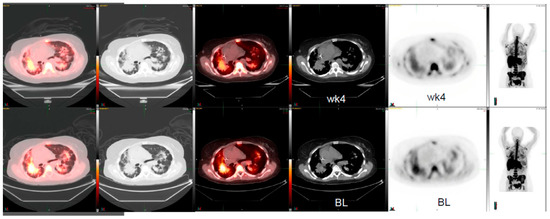
Figure 2.
18F-FLT PET/CT scans shows weak signals of early response to MET inhibitor targeted therapy whereas the conventional CT scan images do not show any responses in a patient with lung adenocarcinoma (BL, baseline; wk4, at 4 weeks post therapy).
Patient 3: The third case study is a 59-year-old female with a diagnosis of EGFR-negative lung adenocarcinoma. The patient received cisplatin, vinorelbine, pemetrexed, and cetuximab as part of standard therapy and was eventually enrolled on an MDM2 inhibitor. Herein, a nine-day pre- and post-targeted therapy image of the right middle lobe mass comparison was done using CT and 18F-FLT PET/CT. While CT demonstrated a change of 6% tumor size from 5.1 cm × 4.4 cm to 4.8 cm × 4.6 cm, 18F-FLT PET/CT showed a reduction of 31% from 3.6 to 2.5 SUVmax (Figure 3).
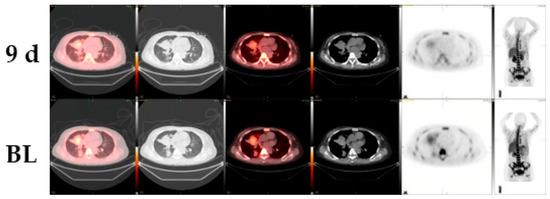
Figure 3.
18F-FLT PET/CT scans shows early response to MDM2-inhibitor targeted therapy whereas the conventional CT scan images do not show any responses in a patient with EGFR-negative lung adenocarcinoma (BL, baseline; 9d, at 9 days post therapy).
4. Discussion
18F-FLT PET/CT in monitoring treatment response in patients was evaluated in patients with lung cancer. We demonstrate early/signals of activity with c-MET in four-weeks post therapy and another case with MDM2 inhibitor in nine-days post therapy. The favorable change in 18F-FLT activity was not evident in 18F-FDG PET/CT and CT.
The advantages of 18F-FLT PET/CT over 18F-FDG PET/CT in monitoring treatment response have been well described in patients after chemotherapy, radiotherapy, and/or chemo/radiotherapy. Allen et al. showed significant decrease in tracer uptake in non-small cell lung cancer and mesothelioma patients at the end of treatment with cisplatin and pemetrexed suggesting that 18F-FLT is a more specific tracer for changes in proliferation than 18F-FDG [19]. This theory is supported by known pharmacology of arginine depletion in argininosuccinate synthetase 1 -deficient tumor [20]. In a head-to-head comparison of responders vs. non-responders, patients with advanced adenocarcinoma of the lung on gefitinib, an EGFR tyrosine kinase inhibitor, showed significant decrease in tracer uptake seven days after the start of therapy [19]. Maximum tumor standardized uptake value (SUV max) declined by a mean of 36% in responders, compared to a 10.1% increase in non-responders. 18F-FLT PET/CT responders had a median time to progression of 7.9 months in comparison to 1.2 months in non-responders.
18F-FLT can also be a suitable tracer for radiotherapy monitoring. Uptake of 18F-FLT can be significantly reduced after 5–11 treatment fractions [21]. More recently, different studies have shown that 18F-FLT is a more sensitive tracer of early chemo/radiotherapy treatment response over 18F-FDG [22,23,24]. Unfortunately, false positive findings of 18F-FLT PET/CT may also occur. The reason is 18F-FLT uptake by proliferating lymphoid cells in germinal centers of reactive lymph nodes [25,26]. However, further studies are needed to fully evaluate the role of FLT and FDG. For now, we would not advocate the use of FLT for tumor detection or staging. Early response evaluation by FLT/PET remain exploratory as described and will need CT confirmation.
5. Conclusions
18F-FLT PET/CT for early assessment of therapy response to evaluate for signals of preliminary activity of novel targeted therapy in patients with lung cancer is feasible. Future studies are warranted to compare FLT-PET with conventional modalities.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “conceptualization, K.K., E.S.B., H.A.M., and V.S.; methodology, K.K., E.B.S.; validation, K.K., E.B.S.; formal analysis, K.K., E.B.S., H.M., and V.S.; investigation, K.K., E.B.S., H.A.M., V.S.; data curation, K.K., E.B.S.; writing—original draft preparation, K.K., E.B., H.A.M. and V.S.; writing—review and editing, K.K., E.B.S., H.A.M. and V.S.; supervision, K.K., E.B.S., H.A.M. and V.S.; project administration, K.K., E.B.S., H.A.M. and V.S. All authors have read and agreed to the published version of the manuscript.
Funding
The MD Anderson Cancer Center Support Grant (P30 CA016672). The funders had no role in the design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; and the decision to submit the manuscript for publication.
Acknowledgments
The authors acknowledge the patients and their families for participating in this study.
Conflicts of Interest
Vivek Subbiah, Research funding/Grant support for clinical trials: FUJIFILM Pharmaceuticals U.S.A., Inc., Novartis, Bayer, GlaxoSmithKline, Nanocarrier, Vegenics, Celgene, Northwest Biotherapeutics, Berghealth, Incyte, Pharmamar, D3, Pfizer, Multivir, Amgen, Abbvie, Alfa-sigma, Agensys, Boston Biomedical, Idera Pharma, Inhibrx, Exelixis, Blueprint medicines, Loxo oncology, Medimmune, Altum, Dragonfly therapeutics, Takeda and Roche/Genentech, National Comprehensive Cancer Network, NCI-CTEP and UT MD Anderson Cancer Center. Travel: Novartis, Pharmamar, ASCO, ESMO, Helsinn, Incyte, US-FDA, Consultancy/Advisory board: Helsinn, LOXO Oncology/Eli Lilly, R-Pharma US, INCYTE, Medimmune, Novartis. All other authors declare no relevant conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Szyszko, T.A.; Yip, C.; Szlosarek, P.; Goh, V.; Cook, G.J. The role of new PET tracers for lung cancer. Lung Cancer 2016, 94, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Bollineni, V.R.; Kramer, G.M.; Jansma, E.P.; Liu, Y.; Oyen, W.J. A systematic review on [18F]FLT-PET uptake as a measure of treatment response in cancer patients. Eur. J. Cancer 2016, 55, 81–97. [Google Scholar] [CrossRef]
- Xie, X.; Chen, H.; Yang, H.; Lin, H.; Zhou, S.; Shen, R.; Lu, C.; Ling, L.; Lin, W.; Liao, Z. Predictive value of positron emission tomography for the prognosis of molecularly targeted therapy in solid tumors. Onco Targets Ther. 2018, 11, 8885–8899. [Google Scholar] [CrossRef] [PubMed]
- Hiniker, S.M.; Sodji, Q.; Quon, A.; Gutkin, P.M.; Arksey, N.; Graves, E.E.; Chin, F.T.; Maxim, P.G.; Diehn, M.; Loo, B.W., Jr. FLT-PET-CT for the Detection of Disease Recurrence After Stereotactic Ablative Radiotherapy or Hyperfractionation for Thoracic Malignancy: A Prospective Pilot Study. Front. Oncol. 2019, 9, 467. [Google Scholar] [CrossRef]
- Sanghera, B.; Wong, W.L.; Sonoda, L.I.; Beynon, G.; Makris, A.; Woolf, D.; Ardeshna, K. FLT PET-CT in evaluation of treatment response. Indian J. Nuclear Med. 2014, 29, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Drontle, D.P.; Wagner, C.R. Designing a pronucleotide stratagem: Lessons from amino acid phosphoramidates of anticancer and antiviral pyrimidines. Mini Rev. Med. Chem. 2004, 4, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Shields, A.F.; Grierson, J.R.; Dohmen, B.M.; Machulla, H.J.; Stayanoff, J.C.; Lawhorn-Crews, J.M.; Obradovich, J.E.; Muzik, O.; Mangner, T.J. Imaging proliferation in vivo with [18F]FLT and positron emission tomography. Nat. Med. 1998, 4, 1334–1336. [Google Scholar] [CrossRef] [PubMed]
- Shen, G.; Ma, H.; Pang, F.; Ren, P.; Kuang, A. Correlations of 18F-FDG and 18F-FLT uptake on PET with Ki-67 expression in patients with lung cancer: A meta-analysis. Acta Radiol. 2018, 59, 188–195. [Google Scholar] [CrossRef]
- McKinley, E.T.; Ayers, G.D.; Smith, R.A.; Saleh, S.A.; Zhao, P.; Washington, M.K.; Coffey, R.J.; Manning, H.C. Limits of [18F]-FLT PET as a biomarker of proliferation in oncology. PLoS ONE 2013, 8, e58938. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Nishiyama, Y.; Ishikawa, S.; Nakano, J.; Chang, S.S.; Bandoh, S.; Kanaji, N.; Haba, R.; Kushida, Y.; Ohkawa, M. Correlation of 18F-FLT and 18F-FDG uptake on PET with Ki-67 immunohistochemistry in non-small cell lung cancer. Eur. J. Nuclear Med. Mol. Imaging 2007, 34, 1610–1616. [Google Scholar] [CrossRef]
- Deppen, S.A.; Blume, J.D.; Kensinger, C.D.; Morgan, A.M.; Aldrich, M.C.; Massion, P.P.; Walker, R.C.; McPheeters, M.L.; Putnam, J.B., Jr.; Grogan, E.L. Accuracy of FDG-PET to diagnose lung cancer in areas with infectious lung disease: A meta-analysis. JAMA 2014, 312, 1227–1236. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, Y.; Sui, X.; Zhang, W.; Shi, R.; Zhang, Y.; Dang, Y.; Qiao, Z.; Zhang, B.; Song, W.; et al. Performance of FLT-PET for pulmonary lesion diagnosis compared with traditional FDG-PET: A meta-analysis. Eur. J. Radiol. 2015, 84, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Yang, X.; Yu, L.; Chen, P.; Xin, J.; Ma, L.; Feng, H.; Tan, Y.; Zhao, Z.; Wu, W. A multicenter clinical trial on the diagnostic value of dual-tracer PET/CT in pulmonary lesions using 3’-deoxy-3’-18F-fluorothymidine and 18F-FDG. J. Nuclear Med. 2008, 49, 186–194. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Xu, B.; Guan, Z.; Liu, C.; Wang, R.; Yin, D.; Zhang, J.; Chen, Y.; Yao, S.; Shao, M.; Wang, H.; et al. Can multimodality imaging using 18F-FDG/18F-FLT PET/CT benefit the diagnosis and management of patients with pulmonary lesions? Eur. J. Nuclear Med. Mol. Imaging 2011, 38, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Li, X.F.; Dai, D.; Song, X.Y.; Liu, J.J.; Zhu, Y.J.; Xu, W.G. Comparison of the diagnostic performance of 18F-fluorothymidine versus 18F-fluorodeoxyglucose positron emission tomography on pulmonary lesions: A meta-analysis. Mol. Clin. Oncol. 2015, 3, 101–108. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pasquini, G.; Giaccone, G. C-MET inhibitors for advanced non-small cell lung cancer. Expert Opin Investig Drugs. Expert Opin. Investig. Drugs 2018, 27, 363–375. [Google Scholar] [CrossRef]
- Awad, M.M.; Oxnard, G.R.; Jackman, D.M.; Heng, J.C.; Dahlberg, S.E.; Jänne, P.A.; Savukoski, D.O.; Hall, D.; Shivdasani, P.; Verma, S.; et al. MET Exon 14 Mutations in Non-Small-Cell Lung Cancer Are Associated With Advanced Age and Stage-Dependent MET Genomic Amplification and c-Met Overexpression. J. Clin. Oncol. 2016, 34, 721–730. [Google Scholar] [CrossRef]
- Cascone, T.; Xu, L.; Lin, H.Y.; Liu, W.; Tran, H.T.; Liu, Y.; Howells, K.; Haddad, V.; Hanrahan, E.; Nilsson, M.B.; et al. The HGF/c-MET Pathway Is a Driver and Biomarker of VEGFR-inhibitor Resistance and Vascular Remodeling in Non-Small Cell Lung Cancer. Clin. Cancer Res. 2017, 23, 5489–5501. [Google Scholar] [CrossRef]
- Allen, M.D.; Luong, P.; Hudson, C.; Leyton, J.; Delage, B.; Ghazaly, E.; Cutts, R.; Yuan, M.; Syed, N.; Lo Nigro, C.; et al. Prognostic and therapeutic impact of argininosuccinate synthetase 1 control in bladder cancer as monitored longitudinally by PET imaging. Cancer Res. 2014, 74, 896–907. [Google Scholar] [CrossRef]
- Sohn, H.J.; Yang, Y.J.; Ryu, J.S.; Oh, S.J.; Im, K.C.; Moon, D.H.; Lee, D.H.; Suh, C.; Lee, J.S.; Kim, S.W. [18F]Fluorothymidine positron emission tomography before and 7 days after gefitinib treatment predicts response in patients with advanced adenocarcinoma of the lung. Clin. Cancer Res. 2008, 14, 7423–7429. [Google Scholar] [CrossRef]
- Trigonis, I.; Koh, P.K.; Taylor, B.; Tamal, M.; Ryder, D.; Earl, M.; Anton-Rodriguez, J.; Haslett, K.; Young, H.; Faivre-Finn, C.; et al. Early reduction in tumour [18F]fluorothymidine (FLT) uptake in patients with non-small cell lung cancer (NSCLC) treated with radiotherapy alone. Eur. J. Nuclear Med. Mol. Imaging 2014, 41, 682–693. [Google Scholar] [CrossRef] [PubMed]
- Everitt, S.J.; Ball, D.L.; Hicks, R.J.; Callahan, J.; Plumridge, N.; Collins, M.; Herschtal, A.; Binns, D.; Kron, T.; Schneider, M.; et al. Differential (18)F-FDG and (18)F-FLT Uptake on Serial PET/CT Imaging Before and During Definitive Chemoradiation for Non-Small Cell Lung Cancer. J. Nuclear Med. 2014, 55, 1069–1074. [Google Scholar] [CrossRef] [PubMed]
- Frings, V.; Yaqub, M.; Hoyng, L.L.; Golla, S.S.; Windhorst, A.D.; Schuit, R.C.; Lammertsma, A.A.; Hoekstra, O.S.; Smit, E.F.; Boellaard, R.; et al. Assessment of simplified methods to measure 18F-FLT uptake changes in EGFR-mutated non-small cell lung cancer patients undergoing EGFR tyrosine kinase inhibitor treatment. J. Nuclear Med. 2014, 55, 1417–1423. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Leimgruber, A.; Möller, A.; Everitt, S.J.; Chabrot, M.; Ball, D.L.; Solomon, B.; MacManus, M.; Hicks, R.J. Effect of Platinum-Based Chemoradiotherapy on Cellular Proliferation in Bone Marrow and Spleen, Estimated by (18)F-FLT PET/CT in Patients with Locally Advanced Non-Small Cell Lung Cancer. J. Nuclear Med. 2014, 55, 1075–1080. [Google Scholar] [CrossRef] [PubMed]
- Yap, C.S.; Czernin, J.; Fishbein, M.C.; Cameron, R.B.; Schiepers, C.; Phelps, M.E.; Weber, W.A. Evaluation of thoracic tumors with 18F-fluorothymidine and 18F-fluorodeoxyglucosepositron emission tomography. Chest 2006, 129, 393–401. [Google Scholar] [CrossRef]
- Troost, E.G.; Bussink, J.; Oyen, W.J.; Kaanders, J.H. 18F-FDG and 18F-FLT do not discriminate between reactive and metastatic lymph nodes in oral cancer. J. Nuclear Med. 2009, 50, 490–491. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).