Impact of Transanal Drainage Tube Placement on Anastomosis Leakage Incidence After Rectal Cancer Surgery
Abstract
1. Introduction
2. Material and Methods
2.1. Study Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
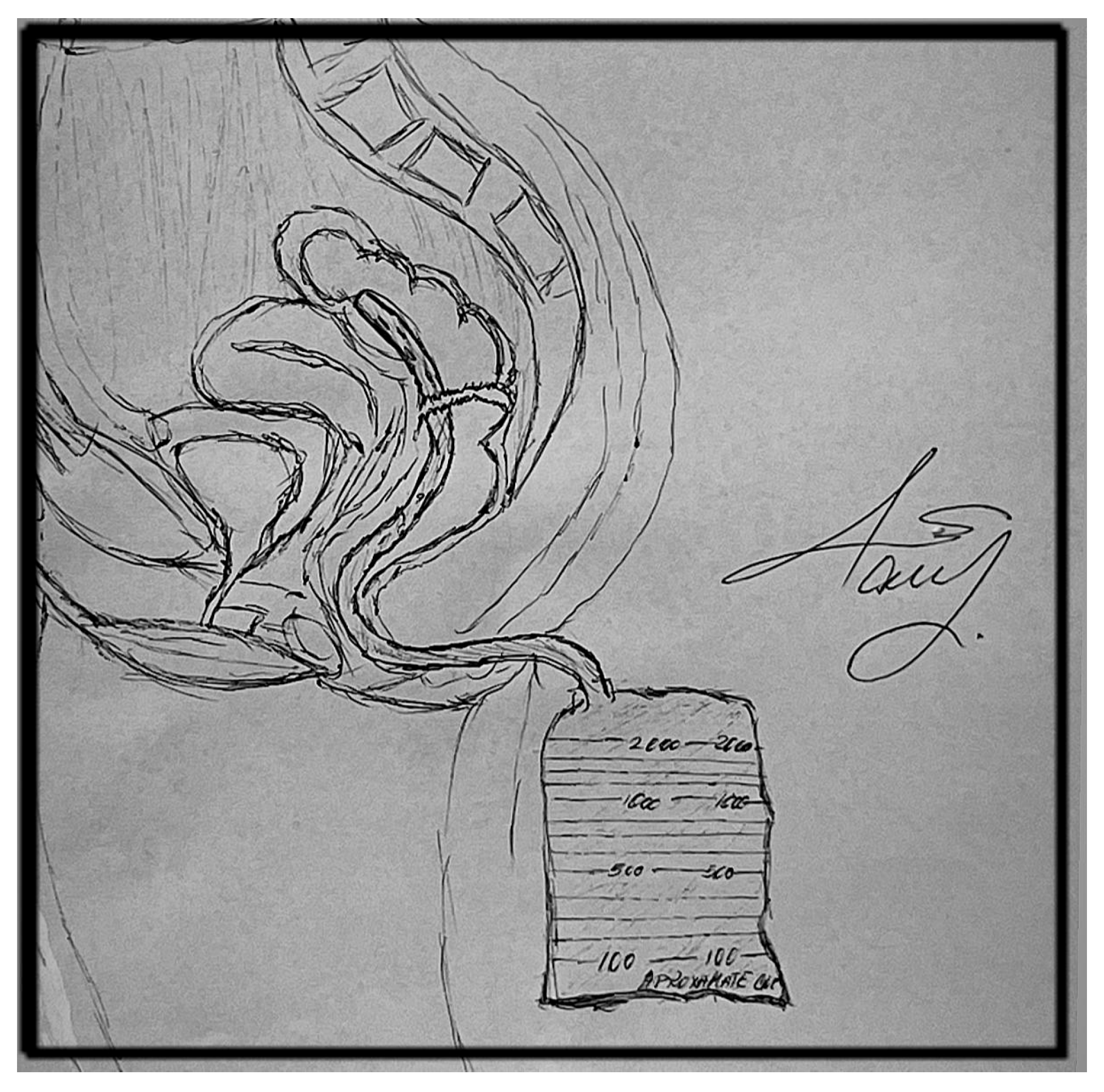
2.4. Treatment
2.5. Outcomes
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Comparation of TAD vs. Non-TAD
3.3. Comparation of TAD vs. Ileostomy
3.4. Comparation of TAD vs. Colostomy
4. Summary
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GLOBOCAN. Available online: https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21834 (accessed on 14 December 2025).
- American Cancer Society. Colorectal Cancer Statistics|How Common Is Colorectal Cancer? 13 January 2023. Available online: https://www.cancer.org/cancer/types/colon-rectal-cancer/about/key-statistics.html (accessed on 14 December 2025).
- Siegel, R.L.; Wagle, N.S.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics. CA Cancer J. Clin. 2023, 73, 233–254. [Google Scholar] [CrossRef]
- Plasencia, A.; Bahna, H. Diverting Ostomy: For Whom, When, What, Where, and Why. Clin. Colon Rectal Surg. 2019, 32, 171–175. [Google Scholar] [CrossRef]
- Rahbari, N.N.; Weitz, J.; Hohenberger, W.; Heald, R.J.; Moran, B.; Ulrich, A.; Holm, T.; Wong, W.D.; Tiret, E.; Moriya, Y.; et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: A proposal by the International Study Group of Rectal Cancer. Surgery 2010, 147, 339–351. [Google Scholar] [CrossRef]
- Klein, P.; Immler, F.; Sterk, P.; Schubert, F. Secure anastomoses of the large intestine (especially with transanal drainage. Zentralblatt Fur Chir. 1997, 122, 528–532; discussion 533–534. [Google Scholar]
- Chen, H.; Cai, H.-K.; Tang, Y.-H. An updated meta-analysis of transanal drainage tube for prevention of anastomotic leak in anterior resection for rectal cancer. Surg. Oncol. 2018, 27, 333–340. [Google Scholar] [CrossRef]
- Goto, S.; Hida, K.; Kawada, K.; Okamura, R.; Hasegawa, S.; Kyogoku, T.; Ota, S.; Adachi, Y.; Sakai, Y. Multicenter analysis of transanal tube placement for prevention of anastomotic leak after low anterior resection. J. Surg. Oncol. 2017, 116, 989–995. [Google Scholar] [CrossRef]
- Myrseth, E.; Nymo, L.S.; Gjessing, P.F.; Norderval, S. Diverting stomas reduce reoperation rates for anastomotic leak but not overall reoperation rates within 30 days after anterior rectal resection: A national cohort study. Int. J. Color. Dis. 2022, 37, 1681–1688. [Google Scholar] [CrossRef]
- Xiao, L.; Zhang, W.B.; Jiang, P.C.; Bu, X.F.; Yan, Q.; Li, H.; Zhang, Y.J.; Yu, F. Can Transanal Tube Placement after Anterior Resection for Rectal Carcinoma Reduce Anastomotic Leakage Rate? A Single-institution Prospective Randomized Study. World J. Surg. 2011, 35, 1367–1377. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Li, N.; He, D.; Feng, J. Transanal Tube for the Prevention of Anastomotic Leakage After Rectal Cancer Surgery: A Systematic Review and Meta-analysis. World J. Surg. 2016, 41, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Rennie, O.; Sharma, M.; Helwa, N. Colorectal anastomotic leakage: A narrative review of definitions, grading systems, and consequences of leaks. Front. Surg. 2024, 11, 1371567. [Google Scholar] [CrossRef] [PubMed]
- Hermanek, H.C.P.; Hermanek, P. Role of the surgeon as a variable in the treatment of rectal cancer. Semin. Surg. Oncol. 2000, 19, 329–335. [Google Scholar] [CrossRef]
- Ellis, C.T.; Maykel, J.A. Defining Anastomotic Leak and the Clinical Relevance of Leaks. Clin. Colon Rectal Surg. 2021, 34, 1371567. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Hu, X.; Huang, Y.; Yin, X.; Zhang, P.; Hao, Y.; Li, H.; Wang, G. Does transanal drainage tubes placement have an impact on the incidence of anastomotic leakage after rectal cancer surgery? A systematic review and meta-analysis. BMC Cancer 2024, 24, 263. [Google Scholar] [CrossRef]
- Jha, M.K.; Shah, K.B.; Thapa, A.; Basukala, S.; Sah, S.K. Postoperative Complications among Major Abdominal Surgeries using Clavien-Dindo Classification in Tertiary Hospital: An Observational Study. J. Nepal Med. Assoc. 2024, 63, 12–17. [Google Scholar] [CrossRef]
- Nash, G.F. Anastomotic leakage after curative anterior resection results in a higher prevalence of local recurrence colectomy (Br. J. Surg. 2003, 90, 1261–1266). Br. J. Surg. 2003, 91, 125–126. [Google Scholar] [CrossRef]
- Merkel, S.; Wang, W.Y.; Schmidt, O.; Dworak, O.; Wittekind, C.H.; Hohenberger, W.; Hermanek, P. Locoregional recurrence in patients with anastomotic leakage after anterior resection for rectal carcinoma. Color. Dis. 2001, 3, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, M.-H. Risk factors for anastomotic fistula development after radical colon cancer surgery and their impact on prognosis. World J. Gastrointest. Surg. 2023, 15, 2470–2481. [Google Scholar] [CrossRef] [PubMed]
- Škrabec, C.G.; Carne, A.V.; Perez, M.C.; Corral, J.; Pujol, A.F.; Cuadrado, M.; Troya, J.; Ibanez, J.F.J.; Pares, D. Early and late anastomotic leak after colorectal surgery: A systematic review of the literature. Cirugía Española 2023, 101, 3–11. [Google Scholar] [CrossRef]
- Sparreboom, C.L.; van Groningen, J.T.; Lingsma, H.F.; Wouters, M.W.; Menon, A.G.; Kleinrensink, G.J.; Jeekel, J.; Lange, J.F. Different Risk Factors for Early and Late Colorectal Anastomotic Leakage in a Nationwide Audit. Dis. Colon Rectum 2018, 61, 1258–1266. [Google Scholar] [CrossRef]
- Phan, K.; Oh, L.; Ctercteko, G.; Pathma-Nathan, N.; El Khoury, T.; Azam, H.; Wright, D.; Toh, J.W.T. Does a stoma reduce the risk of anastomotic leak and need for re-operation following low anterior resection for rectal cancer: Systematic review and meta-analysis of randomized controlled trials. J. Gastrointest. Oncol. 2019, 10, 179–187. [Google Scholar] [CrossRef]
- McGiffin, T.; Clark, D.A.; Edmundson, A.; Steffens, D.; Stevenson, A.; Solomon, M. Surgical management and long-term functional outcomes after anastomotic leak in patients undergoing minimally invasive restorative rectal resection and without a diverting ileostomy. ANZ J. Surg. 2022, 92, 806–812. [Google Scholar] [CrossRef]
- Matsumoto, Y.; Aisu, N.; Kajitani, R.; Nagano, H.; Yoshimatsu, G.; Hasegawa, S. Complications associated with loop ileostomy: Analysis of risk factors. Tech. Coloproctology 2024, 28, 60. [Google Scholar] [CrossRef]
- Fujino, S.; Yasui, M.; Ohue, M.; Miyoshi, N. Efficacy of transanal drainage tube in preventing anastomotic leakage after surgery for rectal cancer: A meta-analysis. World J. Gastrointest. Surg. 2023, 15, 1202–1210. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Hu, F.; Li, Y.; Li, H.; Luo, W.; Sun, F. Use of a Transanal Drainage Tube for Prevention of Anastomotic Leakage and Bleeding after Anterior Resection for Rectal Cancer. World J. Surg. 2012, 37, 227–232. [Google Scholar] [CrossRef]
- Cong, Z.; Fu, C.; Wang, H.; Liu, L.; Zhang, W.; Wang, H. Influencing Factors of Symptomatic Anastomotic Leakage After Anterior Resection of the Rectum for Cancer. World J. Surg. 2009, 33, 1292–1297. [Google Scholar] [CrossRef] [PubMed]
- Nishigori, H.; Ito, M.; Nishizawa, Y.; Nishizawa, Y.; Kobayashi, A.; Sugito, M.; Saito, N. Effectiveness of a transanal tube for the prevention of anastomotic leakage after rectal cancer surgery. World J. Surg. 2014, 38, 1843–1851. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Zhu, C.-K.; Wu, D.-Q.; Zhou, L.-B.; Wang, C.-S. Effect comparison of three different types of transanal drainage tubes after anterior resection for rectal cancer. BMC Surg. 2020, 20, 166. [Google Scholar] [CrossRef]
| Variable | Group A TAD (n = 47, 27.5%) | Group B ileostomy (n = 45, 23.6%) | Group C colostomy n = 25, 14.6% | Group D No protection n= 54, 32.2% | TOTAL 171 |
| Gender, Male Female | 26 (55.31%) 21 (47.72%) | 35 (77.8%) 10 (22.2) | 15 (60%) 10 (40%) | 36 (66.7%) 18 (33.3%) | 112 (65.59%) 59 (34.50%) |
| Radio-chemotherapy | 38/35 (80.85%/74.46%) | 43/38 (95.5%/84.44%) | 21/20 (84%/80%) | 30/31 (55.55%/57.40%) | 135/124 (78.94%/72.51%) |
| Distance from anal verge (cm) | |||||
| I < 5 cm M5- < 10 cm S > 10 cm J | 1 (2.1%) | 10 (22.22%) | 2 (8%) | 8 (14.81%) | 21 (12.28%) |
| 17(36.2%) | 26 (57.8%) | 19 (76%) | 21 (12.3%) | 83 (48.53%) | |
| 23 (48.9%) | 7 (15.6%) | 3(12%) | 16 (29.62%) | 49 (28.65%) | |
| 6 (12.76%) | 2 (4.4%) | 1 (4%) | 10 (18.51%) | 19 (11.11%) | |
| Grade | |||||
| I | 3 (6.4%) | 6 (13.3%) | 11 (44%) | 6 (11.11%) | 26 (15.20%) |
| II | 18 (38.3%) | 10 (22.2%) | 23 (92%) | 12 (22.22%) | 54 (31.57%) |
| III | 23 (48.9%) | 24 (53.33%) | 22 (88%) | 27 (50%) | 96 (56.14%) |
| IV | 3 (6.38%) | 2 (4.4%) | 7 (28%) | 9 (16.16%) | 21 (12.28%) |
| TT/tt | 18/10 | 27/1 | 15/0 | 14/2 | (43.37%/7.60%) |
| LL/ll | 1/0 | 7/0 | 3 | 2/1 | (7.01%/2.30%) |
| LT/lt | 3/11 | 10/0 | 7 | 6/1 | (15.20%/11.11%) |
| Deads. | 0 | 1 (2.20%) | 1 (4.50%) | 1 (1.85%) | 3 (1.75%) |
| Anastomotic leakage (AL) | 1 (2.12%) | 2 (4.40%) | 2 (8%) | 3 (5.50%) | 8 (4.67%) |
| Group | TAD (n = 47) | NON-TAD (n = 54) | p-Value |
|---|---|---|---|
| Early General Surgical Complication | 3 (6.40%) | 11 (20.40%) | 0.004 |
| Early Septic Surgical Complications | 0 (0%) | 4 (7.40%) | 0.121 |
| Tardive General Surgical Complications | 2 (4.30%) | 8 (14.80%) | 0.1003 |
| Tardive Septic Surgical Complications | 1 (2.10%) | 1 (1.85%) | 1 |
| Total Septic Complications | 1 (2.10%) | 5 (9.25%) | 0.0001 |
| Total Complications | 5 (10.60%) | 18 (33.3%) | 0.0085 |
| Group | TAD (n = 47) | Ileostomy (n = 45) | p-Value |
|---|---|---|---|
| Early General Surgical Complication | 3 (6.40%) | 4 (8.9%) | 0.711 |
| Early Septic Surgical Complications | 0 (0%) | 2 (4.4%) | 0.236 |
| Tardive General Surgical Complications | 2 (4.30%) | 14 (31.10%) | 0.00078 |
| Tardive Septic Surgical Complications | 1 (2.10%) | 3 (6.7%) | 0.356 |
| Total Septic Complications | 1 (2.10%) | 5 (11.11%) | 0.107 |
| Total Complications | 5 (10.60%) | 17 (37.80%) | 0.0031 |
| Group | TAD (n = 47) | Colostomy (n = 25) | p-Value |
|---|---|---|---|
| Early General Surgical Complication | 3 (6.40%) | 4 (16%) | 0.207 |
| Early Septic Surgical Complications | 0 (0%) | 1 (4%) | 0.347 |
| Tardive General Surgical Complications | 2 (4.30%) | 4 (16%) | 0.173 |
| Tardive Septical Surgical Complications | 1 (2.10%) | 1 (4%) | 0.645 |
| Total Septic Complications | 1 (2.10%) | 2 (4.44%) | 0.275 |
| Study [Ref] | Year | TAD Group | Controls Non-TAD | Type of Study | Anastomotic Leak % | p Value | |
|---|---|---|---|---|---|---|---|
| TAD | Non TAD | ||||||
| Fujino et al. [25] | 2023 | 489 | 486 | Meta-analyze | 4.5% | 8.8% | 0.012 |
| Zhao et al. [26] | 2013 | 81 | 77 | Non-randomized | 3.7% | 10.3% | ns |
| Wang et al. [27] | 2025 | 287 | 287 | Retrospective | 3.8% | 8% | 0.034 |
| Xiao et al. [10] | 2011 | 200 | 198 | Randomized | 2% | 5% | 0.026 |
| Liu et al. [15] | 2024 | 890 | 884 | Meta-analyze | 9.3% | 10.3% | 0.580 |
| Nishigori et al. [28] | 2014 | 36 | 140 | Retrospective | 9% | 11.4% | 0.040 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Răvaș, M.-M.; Marincaș, M.; Brătucu, E.; Prunoiu, V.; Simion, L.; Manea, L.-M.; Brătucu, M.-N. Impact of Transanal Drainage Tube Placement on Anastomosis Leakage Incidence After Rectal Cancer Surgery. Life 2026, 16, 5. https://doi.org/10.3390/life16010005
Răvaș M-M, Marincaș M, Brătucu E, Prunoiu V, Simion L, Manea L-M, Brătucu M-N. Impact of Transanal Drainage Tube Placement on Anastomosis Leakage Incidence After Rectal Cancer Surgery. Life. 2026; 16(1):5. https://doi.org/10.3390/life16010005
Chicago/Turabian StyleRăvaș, Maria-Manuela, Marian Marincaș, Eugen Brătucu, Vrgiliu Prunoiu, Laurentiu Simion, Laura-Maria Manea, and Mircea-Nicolae Brătucu. 2026. "Impact of Transanal Drainage Tube Placement on Anastomosis Leakage Incidence After Rectal Cancer Surgery" Life 16, no. 1: 5. https://doi.org/10.3390/life16010005
APA StyleRăvaș, M.-M., Marincaș, M., Brătucu, E., Prunoiu, V., Simion, L., Manea, L.-M., & Brătucu, M.-N. (2026). Impact of Transanal Drainage Tube Placement on Anastomosis Leakage Incidence After Rectal Cancer Surgery. Life, 16(1), 5. https://doi.org/10.3390/life16010005








