Arthroscopic Repair Versus Conservative Treatment in Degenerative Cuff Tears: Midterm Results
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Outcome Measures
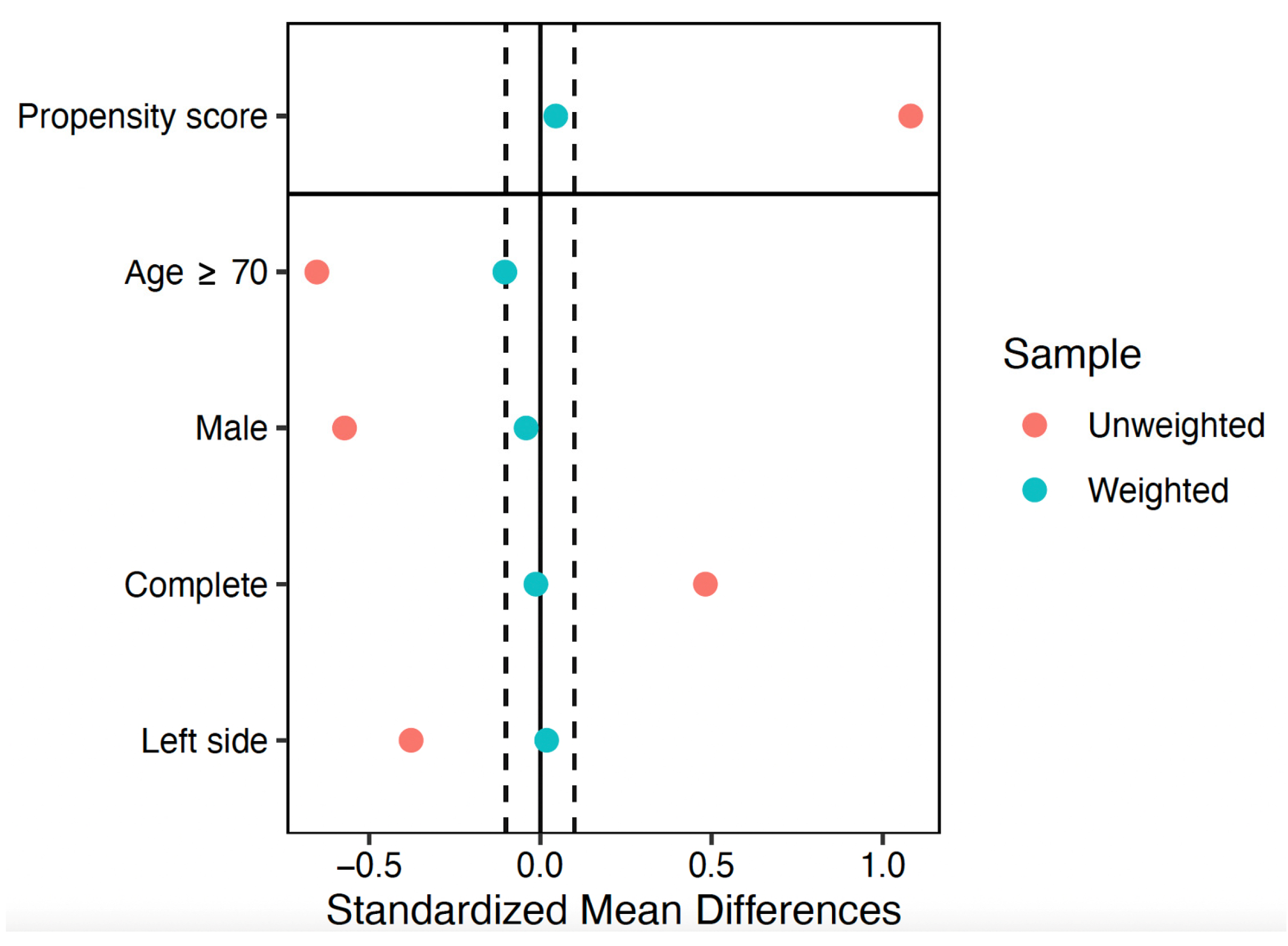
2.3. Clinical Assessment
2.4. Surgical Procedure and Postoperative Management
2.5. Conservative Treatment
2.6. Statistical Analysis
3. Results
3.1. Clinical Characteristics
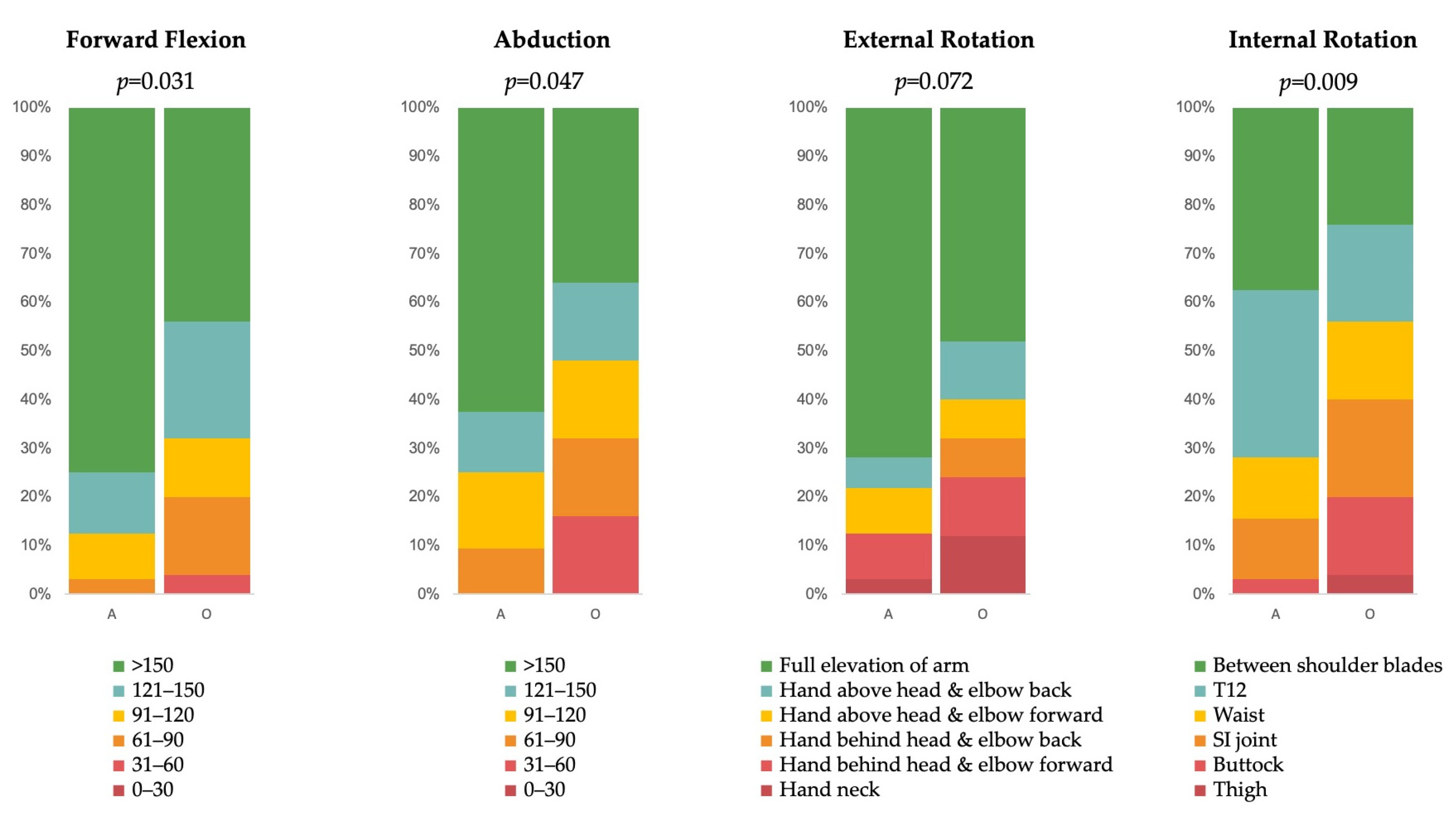
3.2. Functional Outcomes
3.3. Subgroup Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rahman, H.; Currier, E.; Johnson, M.; Goding, R.; Johnson, A.W.; Kersh, M.E. Primary and Secondary Consequences of Rotator Cuff Injury on Joint Stabilizing Tissues in the Shoulder. J. Biomech. Eng. 2017, 139, 110801. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Berton, A.; Papapietro, N.; Maffulli, N.; Denaro, V. Epidemiology, genetics and biological factors of rotator cuff tears. Med. Sport Sci. 2012, 57, 1–9. [Google Scholar]
- Devarasetty, V.V.N.M.; Kuhn, J.E.; Bowman, E.N. Public Perceptions of Rotator Cuff Tears. Clin. Pract. 2024, 14, 729–738. [Google Scholar] [CrossRef]
- Wolff, A.B.; Sethi, P.; Sutton, K.M.; Covey, A.S.; Magit, D.P.; Medvecky, M. Partial-thickness rotator cuff tears. J. Am. Acad. Orthop. Surg. 2006, 14, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Ellman, H. Diagnosis and treatment of incomplete rotator cuff tears. Clin. Orthop. Relat. Res. 1990, 254, 64–74. [Google Scholar] [CrossRef]
- Wang, T.; Ren, Z.; Zhang, Y.; Zhao, X.; Liu, X.; Yu, T.; Zhang, Y. Comparison of Arthroscopic Debridement and Repair in the Treatment of Ellman Grade II Bursal-side Partial-thickness Rotator Cuff Tears: A Prospective Randomized Controlled Trial. Orthop. Surg. 2021, 13, 2070–2080. [Google Scholar] [CrossRef]
- McCrum, E. MR Imaging of the Rotator Cuff. Magn. Reson. Imaging Clin. N. Am. 2020, 28, 165–179. [Google Scholar] [CrossRef]
- Patte, D. Classification of rotator cuff lesions. Clin. Orthop. Relat. Res. 1990, 254, 81–86. [Google Scholar] [CrossRef]
- Lewis, J. Rotator cuff related shoulder pain: Assessment, management and uncertainties. Man. Ther. 2016, 23, 57–68. [Google Scholar] [CrossRef]
- Zhao, J.; Luo, M.; Liang, G.; Pan, J.; Han, Y.; Zeng, L.; Yang, W.; Liu, J. What Factors Are Associated with Symptomatic Rotator Cuff Tears: A Meta-analysis. Clin. Orthop. Relat. Res. 2022, 480, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Neculau, D.C.; Avram, G.M.; Kwapisz, A.; Scarlat, M.M.; Obada, B.; Popescu, I.A. Long head of the biceps tendon versatility in reconstructive shoulder surgery: A narrative review of arthroscopic techniques and their biomechanical principles with video presentation. Int. Orthop. 2024, 48, 1249–1256. [Google Scholar] [CrossRef]
- Gadéa, F.; Dordain, F.; Merbah, J.; Charousset, C.; Berhouet, J.; Francophone Arthroscopy Society (SFA). Methods to analyse the long head of the biceps in the management of distal ruptures of the supraspinatus tendon. Part 1: The concept of the “biceps box”: Dynamic rotator interval approach. Incidence of lesions of the long head of the biceps tendon. Orthop. Traumatol. Surg. Res. 2023, 109, 103669. [Google Scholar] [CrossRef]
- Longo, U.G.; Ambrogioni, L.R.; Candela, V.; Berton, A.; Carnevale, A.; Schena, E.; Denaro, V. Correction to: Conservative versus surgical management for patients with rotator cuff tears: A systematic review and META-analysis. BMC Musculoskelet. Disord. 2021, 22, 752. [Google Scholar] [CrossRef]
- Narvani, A.A.; Imam, M.A.; Godenèche, A.; Calvo, E.; Corbett, S.; Wallace, A.; Itoi, E. Degenerative rotator cuff tear, repair or not repair? A review of current evidence. Ann. R. Coll. Surg. Engl. 2020, 102, 248–255. [Google Scholar] [CrossRef]
- Huang, D.G.; Wu, Y.L.; Chen, P.F.; Xia, C.L.; Lin, Z.J.; Song, J.Q. Surgical or nonsurgical treatment for nontraumatic rotator cuff tears: Study protocol clinical trial. Medicine 2020, 99, e20027. [Google Scholar] [CrossRef] [PubMed]
- Paraskevopoulos, E.; Christakou, A.; Smythe, A.; Kapreli, E.; Papandreou, M.; Papacharalambous, C.; Pavlou, K.; Pamboris, G.M. Addressing Rotator Cuff-Related Shoulder Pain: Findings from a Greek Regional Observational Study Utilizing a Clinical Case Scenario. Clin. Pract. 2025, 15, 30. [Google Scholar] [CrossRef]
- Vora, M.; Sing, D.C.; Curry, E.J.; Kamal, R.N.; Li, X. National Trends in the Surgical Treatment of Chronic Rotator Cuff Tear in Patients Without Arthritis. Orthopedics 2020, 43, e409–e414. [Google Scholar] [CrossRef] [PubMed]
- Avram, G.M.; Neculau, D.C.; Obada, B.; Bastidas, M.V.P.; Popescu, D.; Fiodorovas, M.; Popescu, I. Partial Articular Supraspinatus Tendon Avulsion Repair and Patch: A Technical Note for Augmenting the Supraspinatus Reinsertion with the Long Head of the Biceps Tendon. Orthop. Surg. 2023, 15, 2174–2180. [Google Scholar] [CrossRef] [PubMed]
- Lambers Heerspink, F.O.; van Raay, J.J.; Koorevaar, R.C.; van Eerden, P.J.; Westerbeek, R.E.; van ‘t Riet, E.; Akker-Scheek, I.v.D.; Diercks, R.L. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: A randomized controlled trial. J. Shoulder Elb. Surg. 2015, 24, 1274–1281. [Google Scholar] [CrossRef]
- Kukkonen, J.; Joukainen, A.; Lehtinen, J.; Mattila, K.T.; Tuominen, E.K.J.; Kauko, T.; Äärimaa, V. Treatment of Nontraumatic Rotator Cuff Tears: A Randomized Controlled Trial with Two Years of Clinical and Imaging Follow-up. J. Bone Jt. Surg. Am. 2015, 97, 1729–1737, Erratum in J. Bone Jt. Surg. Am. 2016, 98, e1. [Google Scholar] [CrossRef]
- Moosmayer, S.; Lund, G.; Seljom, U.S.; Haldorsen, B.; Svege, I.C.; Hennig, T.; Pripp, A.H.; Smith, H.-J. At a 10-Year Follow-up, Tendon Repair Is Superior to Physiotherapy in the Treatment of Small and Medium-Sized Rotator Cuff Tears. J. Bone Jt. Surg. Am. 2019, 101, 1050–1060. [Google Scholar] [CrossRef]
- Keçeci, T.; Polat, Y.; Şahin, A.A.; Alparslan, M.; Sipahioğlu, S.; Çıraklı, A. Comparison of All-Suture Anchors and Metal Anchors in Arthroscopic Rotator Cuff Repair: Short-Term Clinical Outcomes and Anchor Pullout Risk. J. Clin. Med. 2025, 14, 2619. [Google Scholar] [CrossRef]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Lippitt, S.B.; Harryman, D.T.; Matsen, F.A. A practical tool for evaluation of function: The Simple Shoulder Test. Am. Acad. Orthop. Surg. 1993, 545–559. [Google Scholar]
- Roach, K.E.; Budiman-Mak, E.; Songsiridej, N.; Lertratanakul, Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991, 4, 143–149. [Google Scholar] [CrossRef]
- Aldon-Villegas, R.; Ridao-Fernández, C.; Torres-Enamorado, D.; Chamorro-Moriana, G. How to Assess Shoulder Functionality: A Systematic Review of Existing Validated Outcome Measures. Diagnostics 2021, 11, 845. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C.; Stuart, E.A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat. Med. 2015, 34, 3661–3679. [Google Scholar] [CrossRef]
- Cinelli, C.; Hazlett, C. Making sense of sensitivity: Extending omitted variable bias. J. R. Stat. Soc. Ser. B Stat. Methodol. 2020, 82, 39–67. [Google Scholar] [CrossRef]
- Ranebo, M.C.; Björnsson Hallgren, H.C.; Holmgren, T.; Adolfsson, L.E. Surgery and physiotherapy were both successful in the treatment of small, acute, traumatic rotator cuff tears: A prospective randomized trial. J. Shoulder Elb. Surg. 2020, 29, 459–470. [Google Scholar] [CrossRef]
- Longo, U.G.; Franceschi, F.; Berton, A.; Maffulli, N.; Droena, V. Conservative treatment and rotator cuff tear progression. Med. Sport Sci. 2012, 57, 90–99. [Google Scholar] [PubMed]
- Chona, D.V.; Lakomkin, N.; Lott, A.; Workman, A.D.; Henry, A.C.; Kuntz, A.F.; Huffman, G.R.; Glaser, D.L. The timing of retears after arthroscopic rotator cuff repair. J. Shoulder Elb. Surg. 2017, 26, 2054–2059. [Google Scholar] [CrossRef] [PubMed]
- Chillemi, C.; Dei Giudici, L.; Mantovani, M.; Osimani, M.; Gumina, S. Rotator cuff failure after surgery: An all-arthroscopic transosseous approach. Musculoskelet. Surg. 2018, 102 (Suppl. 1), 3–12. [Google Scholar] [CrossRef]
- Moosmayer, S.; Lund, G.; Seljom, U.S.; Haldorsen, B.; Svege, I.C.; Hennig, T.; Pripp, A.H.; Smith, F.-J. Tendon repair compared with physiotherapy in the treatment of rotator cuff tears: A randomized controlled study in 103 cases with a five-year follow-up. J. Bone Jt. Surg. Am. 2014, 96, 1504–1514. [Google Scholar] [CrossRef]
- Kwong, C.A.; Ono, Y.; Carroll, M.J.; Fruson, L.W.; More, K.D.; Thornton, G.M.; Lo, I.K. Full-Thickness Rotator Cuff Tears: What Is the Rate of Tear Progression? A Systematic Review. Arthroscopy 2019, 35, 228–234. [Google Scholar] [CrossRef]
- Keener, J.D. Editorial Commentary: Progression of Degenerative Full-Thickness Rotator Cuff Tears: Are We Finally Using Natural History Data to Define At-Risk Tears? Arthroscopy 2019, 35, 235–236. [Google Scholar] [CrossRef]
- Ben, H.; Wang, C.; Jeon, I.H. Superior capsular reconstruction after failed rotator cuff repair using a fascia lata autograft is associated with inferior outcomes compared to primary superior capsular reconstruction for irreparable massive rotator cuff tears. Int. Orthop. 2025, 49, 1915–1922. [Google Scholar] [CrossRef]
- Moffatt, M.; Wade, J.; Foster, N.E.; Littlewood, C. Exploring the experiences and perceptions of patients awaiting rotator cuff repair surgery: An integrated qualitative study within the POWER pilot and feasibility trial. Musculoskelet. Sci. Pract. 2024, 69, 102893. [Google Scholar] [CrossRef] [PubMed]
- Gueniche, J.; Bierry, G. Rotator cuff muscles fatty infiltration increases with age: Retrospective review of 210 patients with intact cuff on computed tomography arthrography. J. Shoulder Elb. Surg. 2019, 28, 617–624. [Google Scholar] [CrossRef]
- Bowen, E.; Waque, A.; Su, F.; Davies, M.; Ode, G.; Lansdown, D.; Feeley, B.; Bedi, A. Muscle Health & Fatty Infiltration with Advanced Rotator Cuff Pathology. Curr. Rev. Musculoskelet. Med. 2025, 18, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Baytoon, D.; Schmidt, V.; Bazan, A.; Wadsten, M.; Sayed-Noor, A. Arthroscopic Repair of Rotator Cuff Tears in Older Adults: A Retrospective Case-Series Study. Geriatr. Orthop. Surg. Rehabil. 2024, 15, 21514593241294045. [Google Scholar] [CrossRef]
- Mera, B.J. Current Perspectives on Rotator Cuff Disease. Osteology 2022, 2, 62–69. [Google Scholar] [CrossRef]
- Torrens, C.; Miquel, J.; Santana, F. Do we really allow patient decision-making in rotator cuff surgery? A prospective randomized study. J. Orthop. Surg. Res. 2019, 14, 116. [Google Scholar] [CrossRef] [PubMed]



| Arthroscopy (n = 32) | Orthopedic (n = 25) | p | |
|---|---|---|---|
| Age at diagnosis, years | 58 (54–61) | 62 (55–66) | 0.018 |
| Age at evaluation, years | 65 (62–69) | 69 (63–73) | 0.023 |
| Sex | 0.040 | ||
| Female | 19 (59.4%) | 8 (32.0%) | |
| Male | 13 (40.6%) | 17 (68.0%) | |
| Type of tear | 0.205 | ||
| Partial | 4 (12.5%) | 8 (32.0%) | |
| <50% | 0 (0.0%) | 1 (4.0%) | |
| ≥50% | 4 (12.5%) | 7 (28.0%) | |
| Complete | 28 (87.5%) | 17 (68.0%) | |
| Grade I | 6 (18.8%) | 7 (28.0%) | |
| Grade II | 13 (40.6%) | 7 (28.0%) | |
| Grade III | 9 (28.1%) | 3 (12.0%) | |
| Laterality | 0.164 | ||
| Left | 12 (37.5%) | 14 (56.0%) | |
| Right | 20 (62.5%) | 11 (44.0%) |
| Arthroscopy (n = 32) | Orthopedic (n = 25) | Adjusted Mean Difference | Robust Standard Error | p | |
|---|---|---|---|---|---|
| CMS | 74.5 ± 16.6 | 58.4 ± 23.0 | 13.855 | 5.568 | 0.016 |
| SST | 7.3 ± 3.1 | 4.9 ± 4.2 | 2.379 | 0.958 | 0.016 |
| SPADI | 35.7 ± 26.6 | 56.1 ± 30.4 | −20.685 | 7.158 | 0.006 |
| SPADI—Pain | 41.0 ± 28.7 | 63.1 ± 27.3 | −19.549 | 7.294 | 0.009 |
| SPADI—Disability | 31.7 ± 26.6 | 51.6 ± 33.1 | −22.051 | 7.460 | 0.005 |
| VAS | 2.7 ± 2.6 | 4.8 ± 2.8 | −2.233 | 0.775 | 0.006 |
| Partial R2 | RV | RVα = 0.05 | |
|---|---|---|---|
| CMS | 0.120 | 0.307 | 0.091 |
| SST | 0.110 | 0.295 | 0.076 |
| SPADI | 0.136 | 0.325 | 0.116 |
| SPADI—Pain | 0.119 | 0.307 | 0.092 |
| SPADI—Disability | 0.142 | 0.332 | 0.125 |
| VAS | 0.151 | 0.343 | 0.139 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camacho-Sanchez, M.R.; Calzado-Alvarez, I.; Minarro, J.C.; Dussan-Arango, D.M.; López-Medina, C.; Izquierdo-Fernandez, A. Arthroscopic Repair Versus Conservative Treatment in Degenerative Cuff Tears: Midterm Results. Life 2025, 15, 1254. https://doi.org/10.3390/life15081254
Camacho-Sanchez MR, Calzado-Alvarez I, Minarro JC, Dussan-Arango DM, López-Medina C, Izquierdo-Fernandez A. Arthroscopic Repair Versus Conservative Treatment in Degenerative Cuff Tears: Midterm Results. Life. 2025; 15(8):1254. https://doi.org/10.3390/life15081254
Chicago/Turabian StyleCamacho-Sanchez, Maria Rosario, Irene Calzado-Alvarez, Jose Carlos Minarro, Diana Maria Dussan-Arango, Clementina López-Medina, and Alberto Izquierdo-Fernandez. 2025. "Arthroscopic Repair Versus Conservative Treatment in Degenerative Cuff Tears: Midterm Results" Life 15, no. 8: 1254. https://doi.org/10.3390/life15081254
APA StyleCamacho-Sanchez, M. R., Calzado-Alvarez, I., Minarro, J. C., Dussan-Arango, D. M., López-Medina, C., & Izquierdo-Fernandez, A. (2025). Arthroscopic Repair Versus Conservative Treatment in Degenerative Cuff Tears: Midterm Results. Life, 15(8), 1254. https://doi.org/10.3390/life15081254







