Predicting Pre- and Post-Diagnostic Depression in Women with Abnormal Pap Screening Tests: A Neural Network Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Study Design
2.3. Study Sample
2.4. Sample Size Calculation
2.5. Data Collection
2.6. Instruments
2.7. Statistical Analysis
2.8. Ethical Considerations
3. Results
4. Discussion
Strengths and Limitations of the Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Ervik, M.; Lam, F.; Laversanne, M.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. 2024. Available online: https://gco.iarc.who.int/today (accessed on 2 December 2024).
- Pettersson, B.F.; Hellman, K.; Vaziri, R.; Andersson, S.; Hellström, A.C. Cervical cancer in the screening era: Who fell victim in spite of successful screening programs? J. Gynecol. Oncol. 2011, 22, 76–82. [Google Scholar] [CrossRef]
- Simonella, L.; Canfell, K. The impact of a two- versus three-yearly cervical screening interval recommendation on cervical cancer incidence and mortality: An analysis of trends in Australia, New Zealand, and England. Cancer Causes Control 2013, 24, 1727–1736. [Google Scholar] [CrossRef]
- Vaccarella, S.; Franceschi, S.; Engholm, G.; Lönnberg, S.; Khan, S.; Bray, F. 50 years of screening in the Nordic countries: Quantifying the effects on cervical cancer incidence. Br. J. Cancer 2014, 111, 965–969. [Google Scholar] [CrossRef] [PubMed]
- Ilic, M.; Ilic, I. Cancer mortality in Serbia, 1991–2015: An age-period-cohort and joinpoint regression analysis. Cancer Commun. 2018, 38, 10. [Google Scholar] [CrossRef] [PubMed]
- Tota, J.E.; Bentley, J.; Blake, J.; Coutlée, F.; Duggan, M.A.; Ferenczy, A.; Franco, E.L.; Fung-Kee-Fung, M.; Gotlieb, W.; Mayrand, M.-H.; et al. Introduction of molecular HPV testing as the primary technology in cervical cancer screening: Acting on evidence to change the current paradigm. Prev. Med. 2017, 98, 5–14. [Google Scholar] [CrossRef]
- Saslow, D.; Solomon, D.; Lawson, H.W.; Killackey, M.; Kulasingam, S.L.; Cain, J.; Garcia, F.A.R.; Moriarty, A.T.; Waxman, A.G.; Wilbur, D.C.; et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J. Clin. 2012, 62, 147–172. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force; Curry, S.J.; Krist, A.H.; Owens, D.K.; Barry, M.J.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; et al. Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2018, 320, 674–686. [Google Scholar] [CrossRef]
- Walboomers, J.M.; Jacobs, M.V.; Manos, M.M.; Bosch, F.X.; Kummer, J.A.; Shah, K.V.; Snijders, P.J.; Peto, J.; Meijer, C.J.; Muñoz, N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 1999, 189, 12–19. [Google Scholar] [CrossRef]
- Armaroli, P.; Villain, P.; Suonio, E.; Almonte, M.; Anttila, A.; Atkin, W.S.; Dean, P.B.; de Koning, H.J.; Dillner, L.; Herrero, R.; et al. European Code against Cancer, 4th Edition: Cancer screening. Cancer Epidemiol. 2015, 39 (Suppl. S1), S139–S152. [Google Scholar] [CrossRef]
- Ramírez, A.T.; Valls, J.; Baena, A.; Rojas, F.D.; Ramírez, K.; Álvarez, R.; Cristaldo, C.; Henríquez, O.; Moreno, A.; Reynaga, D.C.; et al. Performance of cervical cytology and HPV testing for primary cervical cancer screening in Latin America: An analysis within the ESTAMPA study. Lancet Reg. Health Am. 2023, 26, 100593. [Google Scholar] [CrossRef]
- Nanda, K.; McCrory, D.C.; Myers, E.R.; Bastian, L.A.; Hasselblad, V.; Hickey, J.D.; Matchar, D.B. Accuracy of the Papanicolaou test in screening for and follow-up of cervical cytologic abnormalities: A systematic review. Ann. Intern. Med. 2000, 132, 810–819. [Google Scholar] [CrossRef]
- Arip, M.; Tan, L.F.; Jayaraj, R.; Abdullah, M.; Rajagopal, M.; Selvaraja, M. Exploration of biomarkers for the diagnosis, treatment and prognosis of cervical cancer: A review. Discov. Oncol. 2022, 13, 91. [Google Scholar] [CrossRef] [PubMed]
- Chrysostomou, A.C.; Stylianou, D.C.; Constantinidou, A.; Kostrikis, L.G. Cervical Cancer Screening Programs in Europe: The Transition Towards HPV Vaccination and Population-Based HPV Testing. Viruses 2018, 10, 729. [Google Scholar] [CrossRef] [PubMed]
- Villain, P.; Gonzalez, P.; Almonte, M.; Franceschi, S.; Dillner, J.; Anttila, A.; Park, J.Y.; De Vuyst, H.; Herrero, R. European Code against Cancer 4th Edition: Infections and Cancer. Cancer Epidemiol. 2015, 39 (Suppl. S1), S120–S138. [Google Scholar] [CrossRef] [PubMed]
- Staley, H.; Shiraz, A.; Shreeve, N.; Bryant, A.; Martin-Hirsch, P.P.; Gajjar, K. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database Syst. Rev. 2021, 9, CD002834. [Google Scholar] [CrossRef]
- Shepherd, J.; Weston, R.; Peersman, G.; Napuli, I.Z. Interventions for encouraging sexual lifestyles and behaviours intended to prevent cervical cancer. Cochrane Database Syst. Rev. 2000, 2, CD001035. [Google Scholar] [CrossRef]
- Breitkopf, C.R.; Dawson, L.; Grady, J.J.; Breitkopf, D.M.; Nelson-Becker, C.; Snyder, R.R. Intervention to improve follow-up for abnormal Papanicolaou tests: A randomized clinical trial. Health Psychol. 2014, 33, 307–316. [Google Scholar] [CrossRef]
- Miller, S.M.; Tagai, E.K.; Wen, K.-Y.; Lee, M.; Hui, S.-K.A.; Kurtz, D.; Scarpato, J.; Hernandez, E. Predictors of adherence to follow-up recommendations after an abnormal Pap smear among underserved inner-city women. Patient Educ. Couns. 2017, 100, 1353–1359. [Google Scholar] [CrossRef]
- Martinez-Gutierrez, J.; Chima, S.; Boyd, L.; Sherwani, A.; Drosdowsky, A.; Karnchanachari, N.; Luong, V.; Reece, J.C.; Emery, J. Failure to follow up abnormal test results associated with cervical cancer in primary and ambulatory care: A systematic review. BMC Cancer 2023, 23, 653. [Google Scholar] [CrossRef]
- Sharp, L.; Cotton, S.; Cruickshank, M.; Gray, N.; Smart, L.; Whynes, D.; Little, J.; TOMBOLA Group. Impact of post-colposcopy management on women’s long-term worries: Results from the UK population-based TOMBOLA trial. J. Fam. Plann. Reprod. Health Care 2016, 42, 43–51. [Google Scholar] [CrossRef]
- Sharp, L.; Cotton, S.; Little, J.; Gray, N.M.; Cruickshank, M.; Smart, L.; Thornton, A.; Waugh, N.; Walker, L.; on behalf of the TOMBOLA Group. Psychosocial impact of alternative management policies for low-grade cervical abnormalities: Results from the TOMBOLA randomised controlled trial. PLoS ONE 2013, 8, e80092. [Google Scholar] [CrossRef] [PubMed]
- Orbell, S.; Hagger, M.; Brown, V.; Tidy, J. Appraisal theory and emotional sequelae of first visit to colposcopy following an abnormal cervical screening result. Br. J. Health Psychol. 2004, 9, 533–555. [Google Scholar] [CrossRef]
- Gath, D.H.; Hallam, N.; Mynors-Wallis, L.; Day, A.; Bond, S.A. Emotional reactions in women attending a UK colposcopy clinic. J. Epidemiol. Community Health 1995, 49, 79–83. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, M.; Gallagher, P.; Waller, J.; Martin, C.M.; O’Leary, J.J.; Sharp, L.; Irish Cervical Screening Research Consortium (CERVIVA). Adverse psychological outcomes following colposcopy and related procedures: A systematic review. BJOG 2016, 123, 24–38. [Google Scholar] [CrossRef]
- Bell, S.; Porter, M.; Kitchener, H.; Fraser, C.; Fisher, P.; Mann, E. Psychological response to cervical screening. Prev. Med. 1995, 24, 610–616. [Google Scholar] [CrossRef]
- Hellsten, C.; Sjöström, K.; Lindqvist, P.G. A 2-year follow-up study of anxiety and depression in women referred for colposcopy after an abnormal cervical smear. BJOG 2008, 115, 212–218. [Google Scholar] [CrossRef]
- Sharp, L.; Cotton, S.; Gray, N.; Avis, M.; Russell, I.; Walker, L.; Waugh, N.; Whynes, D.; Woolley, C.; Thornton, A.; et al. Long-term psychosocial impact of alternative management policies in women with low-grade abnormal cervical cytology referred for colposcopy: A randomised controlled trial. Br. J. Cancer 2011, 104, 255–264. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Gray, N.M.; Sharp, L.; Cotton, S.C.; Avis, M.; Philips, Z.; Russell, I.; Walker, L.G.; Whynes, D.; Little, J.; TOMBOLA Group. Developing a questionnaire to measure the psychosocial impact of an abnormal cervical smear result and its subsequent management: The TOMBOLA (Trial of Management of Borderline and Other Low-grade Abnormal Smears) trial. Qual. Life Res. 2005, 14, 1553–1562. [Google Scholar] [CrossRef]
- Scheid, T.; Brown, T. Approaches to Mental Health and Illness: Conflicting Definitions and Emphases. In A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems; Scheid, T., Brown, T., Eds.; Cambridge University Press: Cambridge, UK, 2009; pp. 1–162. [Google Scholar]
- Ilic, I.; Babic, G.; Dimitrijevic, A.; Ilic, M.; SipeticGrujicic, S. Internal consistency and validity of the Hospital Anxiety and Depression Scale (HADS) in women with abnormal Pap smear in Serbia. Women Health 2021, 61, 363–371. [Google Scholar] [CrossRef]
- Ilic, I.; Babic, G.; Dimitrijevic, A.; Ilic, M.; SipeticGrujicic, S. Reliability and validity of the Center for Epidemiologic Studies Depression (CES-D) scale in Serbian women with abnormal Papanicolaou smear results. Int. J. Gynecol. Cancer 2019, 29, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- Ilic, I.; Babic, G.; SipeticGrujicic, S.; Zivanovic Macuzic, I.; Ravic-Nikolic, A.; Ilic, M.; Milicic, V. Validity of the Process and Outcome Specific Measure in women with abnormal Papanicolaou screening test. PLoS ONE 2025, 20, e0325131. [Google Scholar] [CrossRef]
- Zhao, F.F. Artificial neural network application for identifying risk of depression in high school students: A cross-sectional study. BMC Psychiatry 2021, 21, 517. [Google Scholar] [CrossRef]
- Sau, A.; Bhakta, I. Artificial neural network (ANN) model to predict depression among geriatric population at a slum in Kolkata, India. J. Clin. Diagn. Res. 2017, 11, VC01–VC04. [Google Scholar] [CrossRef]
- Tortajada, S.; García-Gómez, J.M.; Vicente, J.; Sanjuán, J.; de Frutos, R.; Martín-Santos, R.; García-Esteve, L.; Gornemann, I.; Gutiérrez-Zotes, A.; Canellas, F.; et al. Prediction of postpartum depression using multilayer perceptrons and pruning. Methods Inf. Med. 2009, 48, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Dabek, F.; Caban, J.J. A neural network based model for predicting psychological conditions. In Brain Informatics and Health; Guo, Y., Friston, K., Aldo, F., Hill, S., Peng, H., Eds.; BIH 2015, Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2015; Volume 9250. [Google Scholar] [CrossRef]
- Cotton, S.C.; Sharp, L.; Little, J.; Gray, N.M.; Walker, L.G.; Whynes, D.K.; Cruickshank, M.E.; TOMBOLA Group. A normal colposcopy examination fails to provide psychological reassurance for women who have had low-grade abnormal cervical cytology. Cytopathology 2015, 26, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Oscarsson, M.G.; Benzein, E.G.; Wijma, B.E. Reasons for non-attendance at cervical screening as reported by non-attendees in Sweden. J. Psychosom. Obstet. Gynaecol. 2008, 29, 23–31. [Google Scholar] [CrossRef]
- Rogstad, K. The psychological impact of abnormal cytology and colposcopy. Br. J. Obstet. Gynaecol. 2002, 109, 364–368. [Google Scholar] [CrossRef]
- O’Connor, M.; O’Brien, K.; Waller, J.; Gallagher, P.; D’Arcy, T.; Flannelly, G.; Martin, C.; McRae, J.; Prendiville, W.; Ruttle, C.; et al. Physical after-effects of colposcopy and related procedures, and their inter-relationship with psychological distress: A longitudinal survey. BJOG 2017, 124, 1402–1410. [Google Scholar] [CrossRef]
- Kelly, K.M.; Schoenberg, N.; Wilson, T.D.; Atkins, E.; Dickinson, S.; Paskett, E. Cervical cancer worry and screening among appalachian women. J. Prim. Prev. 2015, 36, 79–92. [Google Scholar] [CrossRef]
- Lofters, A.K.; Telner, D.; Kalia, S.; Slater, M. Association Between Adherence to Cancer Screening and Knowledge of Screening Guidelines: Feasibility Study Linking Self-Reported Survey Data with Medical Records. JMIR Cancer 2018, 4, e10529. [Google Scholar] [CrossRef] [PubMed]
- Hansen, B.T.; Hukkelberg, S.S.; Haldorsen, T.; Eriksen, T.; Skare, G.B.; Nygård, M. Factors associated with non-attendance, opportunistic attendance and reminded attendance to cervical screening in an organized screening program: A cross-sectional study of 12,058 Norwegian women. BMC Public Health 2011, 11, 264. [Google Scholar] [CrossRef]
- Zhang, X.; Mkuu, R.; Samman, E.; Cummings, S.; Sherman, L.; Wigfall, L.T.; Wilkinson, L.; Burdine, J.N. Anxiety and depressive symptoms and missing breast cancer and cervical screening: Results from Brazos valley community health survey. Psychol. Health Med. 2020, 25, 402–409. [Google Scholar] [CrossRef]
- Horsbøl, T.A.; Kjaer, S.K.; Andersen, E.W.; Ammitzbøll, G.; Thygesen, L.C.; Johansen, C.; Jensen, P.T.; Frøding, L.P.; Lajer, H.; Dalton, S.O. Use of hypnotics among women diagnosed with cervical cancer—A population-based cohort study. Gynecol. Oncol. 2022, 166, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Herweijer, E.; Wang, J.; Hu, K.; Valdimarsdóttir, U.A.; Adami, H.-O.; Sparén, P.; Sundström, K.; Fang, F. Overall and Cervical Cancer Survival in Patients with and Without Mental Disorders. JAMA Netw. Open 2023, 6, e2336213. [Google Scholar] [CrossRef] [PubMed]
- Suk, R.; Hong, Y.R.; Rajan, S.S.; Xie, Z.; Zhu, Y.; Spencer, J.C. Assessment of US Preventive Services Task Force Guideline-Concordant Cervical Cancer Screening Rates and Reasons for Underscreening by Age, Race and Ethnicity, Sexual Orientation, Rurality, and Insurance, 2005 to 2019. JAMA Netw. Open 2022, 5, e2143582. [Google Scholar] [CrossRef]
- Qian, Y.; Gao, J.; Zhou, Z.; Yan, J.; Xu, Y.; Yang, X.; Li, Y.; Callander, E. An equity analysis of health examination service utilization by women from underdeveloped areas in western China. PLoS ONE 2017, 12, e0186837. [Google Scholar] [CrossRef]
- Romocki, L.S.; Des Marais, A.; Cofie, L.; Anderson, C.; Curington, T.; Smith, J.S. Use of Short Messaging Service to Improve Follow-Up for Abnormal Pap Test Results in Minority and Medically Underserved Women in North Carolina: Questionnaire on Attitudes and Acceptability. JMIR Form. Res. 2019, 3, e12675. [Google Scholar] [CrossRef]
- Bengtsson, E.; Malm, P. Screening for cervical cancer using automated analysis of PAP-smears. Comput. Math. Methods Med. 2014, 2014, 842037. [Google Scholar] [CrossRef]
- Cenci, M.; Nagar, C.; Vecchione, A. PAPNET-assisted primary screening of conventional cervical smears. Anticancer Res. 2000, 20, 3887–3889. [Google Scholar] [PubMed]
- Koss, L.G.; Lin, E.; Schreiber, K.; Elgert, P.; Mango, L. Evaluation of the PAPNET cytologic screening system for quality control of cervical smears. Am. J. Clin. Pathol. 1994, 101, 220–229. [Google Scholar] [CrossRef]
- Ochi, T.; Murase, K.; Fujii, T.; Kawamura, M.; Ikezoe, J. Survival prediction using artificial neural networks in patients with uterine cervical cancer treated by radiation therapy alone. Int. J. Clin. Oncol. 2002, 7, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Pouliakis, A.; Karakitsou, E.; Margari, N.; Bountris, P.; Haritou, M.; Panayiotides, J.; Koutsouris, D.; Karakitsos, P. Artificial Neural Networks as Decision Support Tools in Cytopathology: Past, Present, and Future. Biomed. Eng. Comput. Biol. 2016, 7, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Liu, J.; Su, Q.; Chu, Y.; Xia, H.; Xu, R. Performance of artificial intelligence for diagnosing cervical intraepithelial neoplasia and cervical cancer: A systematic review and meta-analysis. eClinicalMedicine 2024, 80, 102992. [Google Scholar] [CrossRef]
- Cruz-Gonzalez, P.; He, A.W.-J.; Lam, E.P.; Ng, I.M.C.; Li, M.W.; Hou, R.; Chan, J.N.-M.; Sahni, Y.; Guasch, N.V.; Miller, T.; et al. Artificial intelligence in mental health care: A systematic review of diagnosis, monitoring, and intervention applications. Psychol. Med. 2025, 55, e18. [Google Scholar] [CrossRef]
- Manikis, G.C.; Simos, N.J.; Kourou, K.; Kondylakis, H.; Poikonen-Saksela, P.; Mazzocco, K.; Pat-Horenczyk, R.; Sousa, B.; Oliveira-Maia, A.J.; Mattson, J.; et al. Personalized Risk Analysis to Improve the Psychological Resilience of Women Undergoing Treatment for Breast Cancer: Development of a Machine Learning-Driven Clinical Decision Support Tool. J. Med. Internet Res. 2023, 25, e43838. [Google Scholar] [CrossRef]
- Kourou, K.; Manikis, G.; Mylona, E.; Poikonen-Saksela, P.; Mazzocco, K.; Pat-Horenczyk, R.; Sousa, B.; Oliveira-Maia, A.J.; Mattson, J.; Roziner, I.; et al. Personalized prediction of one-year mental health deterioration using adaptive learning algorithms: A multicenter breast cancer prospective study. Sci. Rep. 2023, 13, 7059. [Google Scholar] [CrossRef]
| Depression—Current | |||||
|---|---|---|---|---|---|
| Variables | Total | Prior to Diagnostics | Following Diagnostics | ||
| Number (%) | Number (%) | p * | Number (%) | p * | |
| Age (years) | |||||
| 12 (7.0) | 2 (3.1) | 5 (6.0) | ||
| 43 (25.0) | 9 (14.1) | 17 (20.5) | ||
| 42 (24.4) | 20 (31.2) | 24 (28.9) | ||
| 51 (29.7) | 21 (32.8) | 30 (36.1) | ||
| 24 (14.0) | 12 (18.8) | 0.006 | 7 (8.4) | 0.789 |
| Place of residence | |||||
| 45 (26.2) | 22 (34.4) | 38 (45.8) | ||
| 127 (73.8) | 42 (65.6) | 0.084 | 45 (54.2) | <0.001 |
| Education level | |||||
| 37 (21.5) | 17 (16.6) | 18 (21.7) | ||
| 135 (78.5) | 47 (73.4) | 0.216 | 65 (78.3) | 0.957 |
| Marital status | |||||
| 33 (19.2) | 13 (20.3) | 19 (21.3) | ||
| 139 (80.8) | 51 (79.7) | 0.773 | 70 (78.7) | 0.457 |
| Depression (HADS-D score ≥ 8) | |||||
| 108 (62.8) | 89 (51.7) | |||
| 64 (37.2) | 83 (48.3) | 0.038 | ||
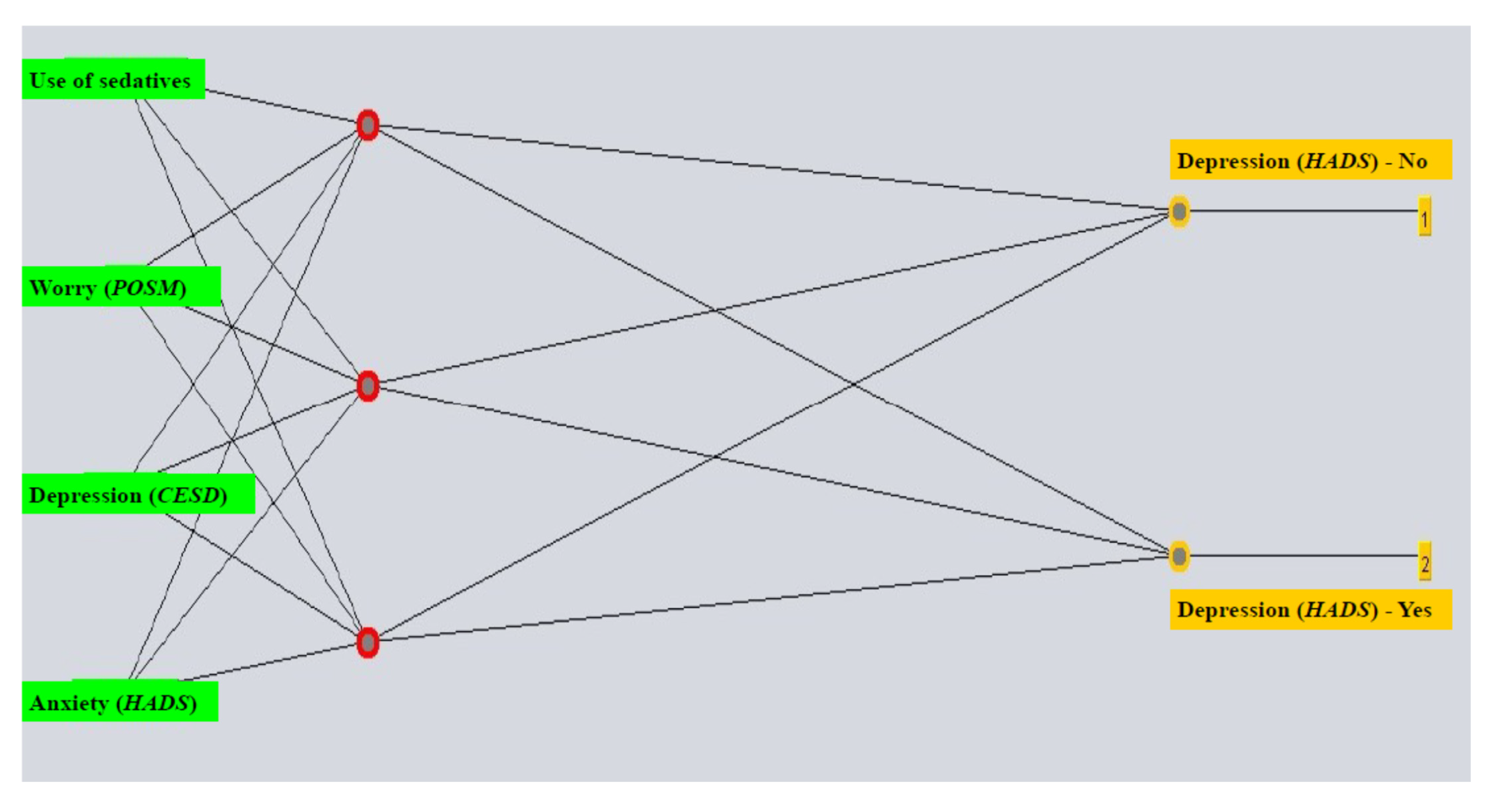
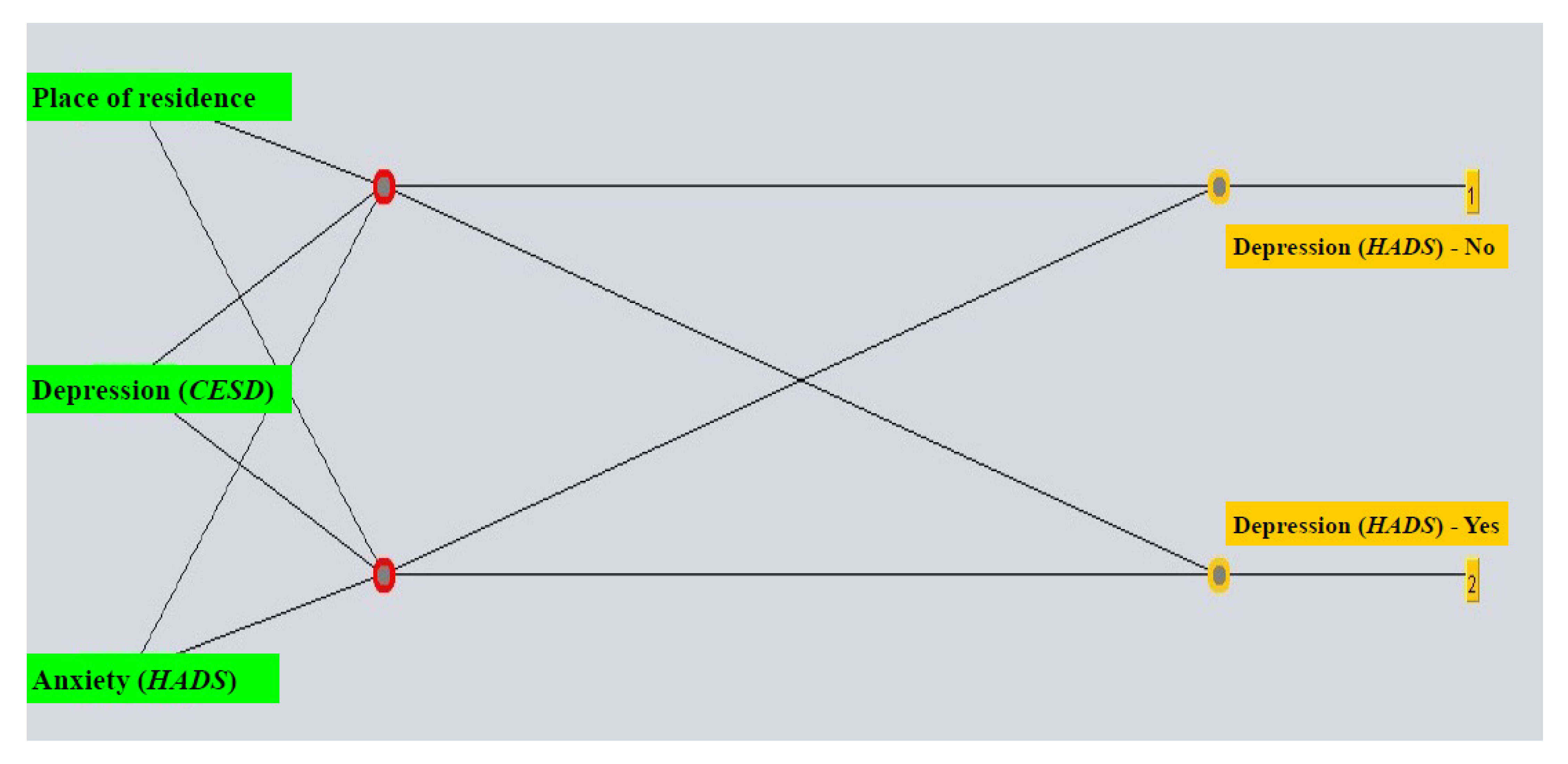
| Attributes | Depression—Prior | Depression—Following |
|---|---|---|
| Pearson Correlation Coefficient | ||
| HADS score for anxiety | 0.62003 | 0.73337 |
| CESD score for depression | 0.41789 | 0.32923 |
| POSM score for worry | 0.29043 | |
| Use of sedatives | 0.24591 | |
| Place of residence | 0.41539 | |
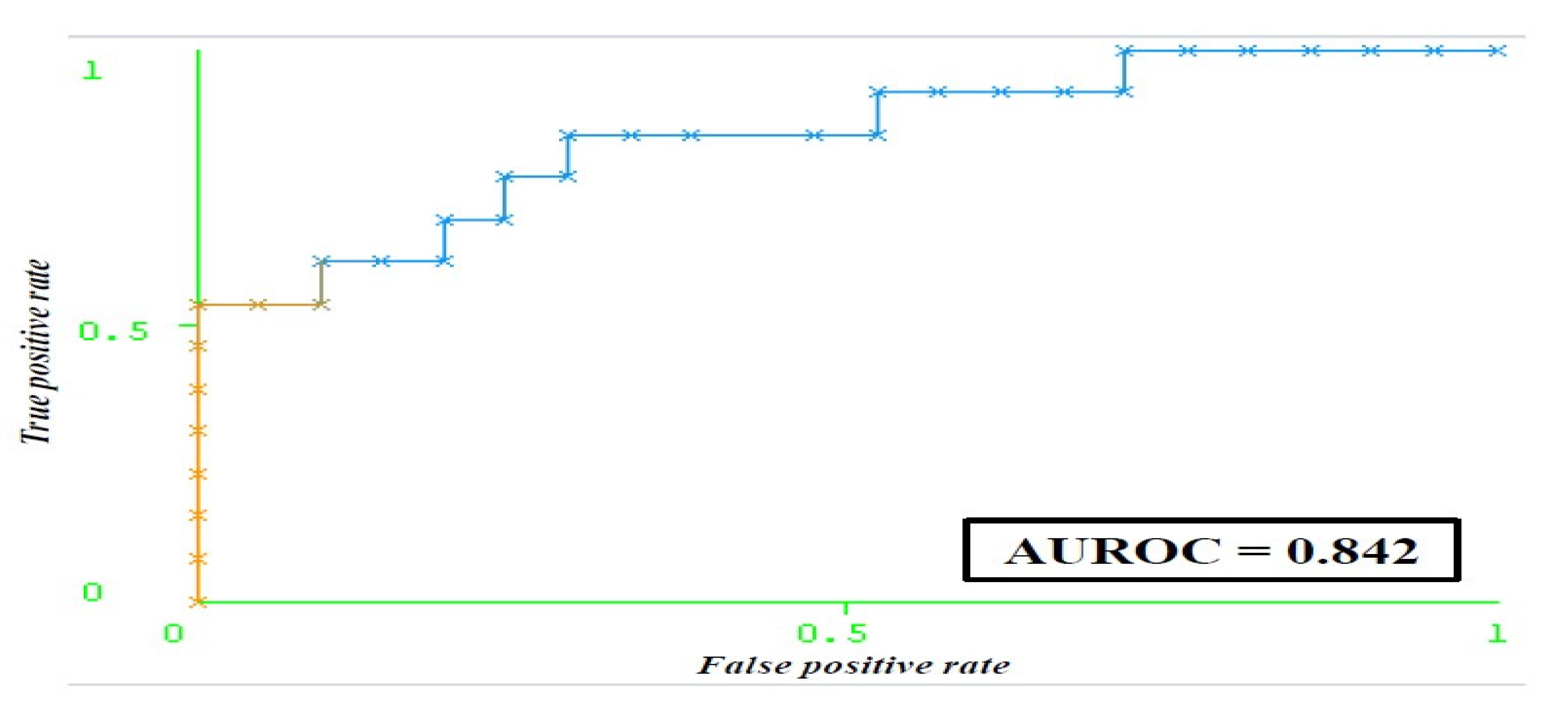
| Evaluation Metrics of the Model | Training Set + Validation ** Including All Attributes | Test Set Including All Attributes | Training Set + Validation ** Including Chosen Attributes | Test Set Including Chosen Attributes |
|---|---|---|---|---|
| Accuracy | 73.913% | 70.588% | 84.782% | 79.411% |
| Kappa | 0.430 | 0.358 | 0.684 | 0.529 |
| TP Rate * | 0.739 | 0.706 | 0.848 | 0.794 |
| FP Rate * | 0.315 | 0.358 | 0.138 | 0.303 |
| Precision * (PPV) | 0.736 | 0.700 | 0.859 | 0.810 |
| NPV | 0.659 | 0.636 | 0.750 | 0.875 |
| ROC Area * | 0.793 | 0.678 | 0.889 | 0.842 |
| MCC | 0.432 | 0.361 | 0.691 | 0.562 |
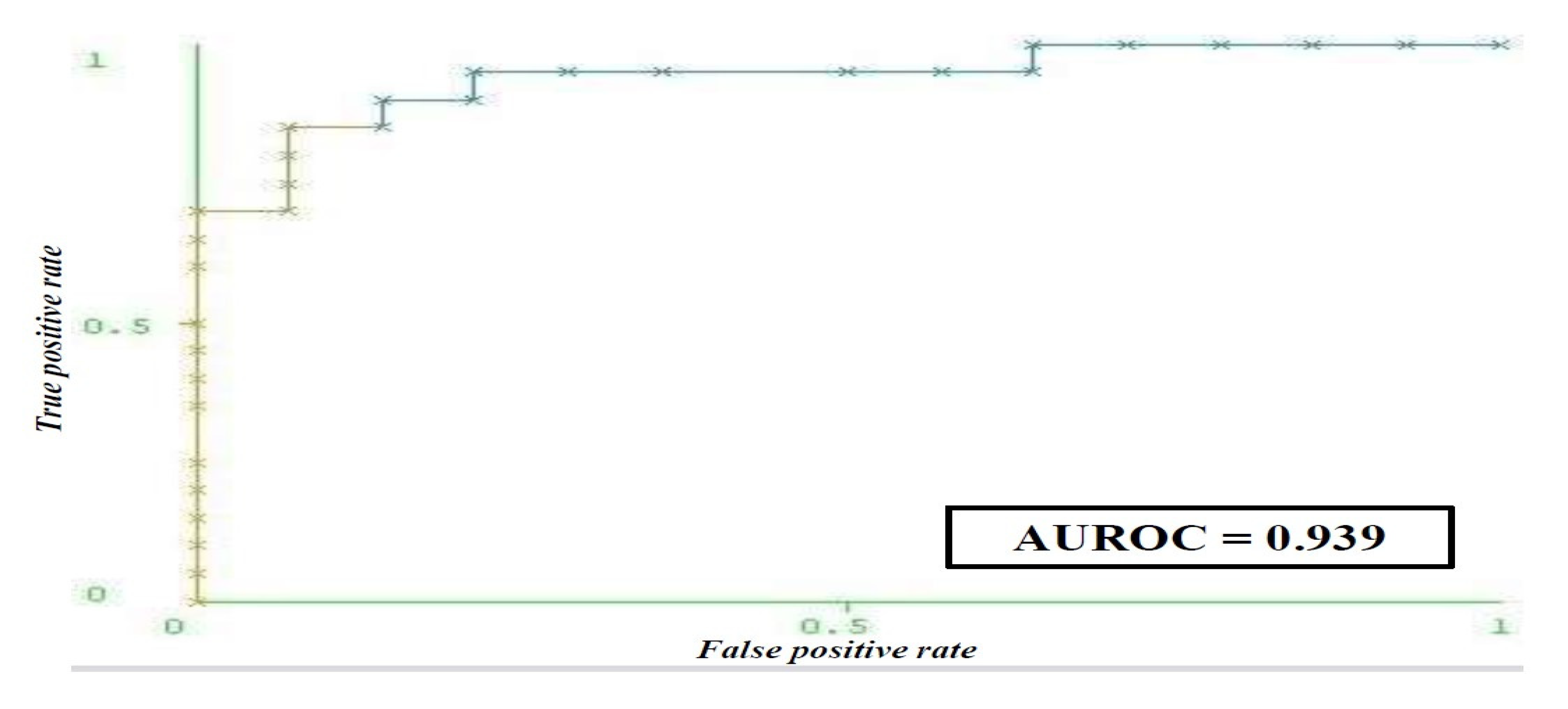
| Evaluation Metrics of the Model | Training Set + Validation ** Including All Attributes | Test Set Including All Attributes | Training Set + Validation ** Including Chosen Attributes | Test Set Including Chosen Attributes |
|---|---|---|---|---|
| Accuracy | 77.536% | 61.764% | 89.855% | 88.235% |
| Kappa | 0.550 | 0.250 | 0.797 | 0.762 |
| TP Rate * | 0.775 | 0.618 | 0.899 | 0.882 |
| FP Rate * | 0.222 | 0.353 | 0.095 | 0.104 |
| Precision * (PPV) | 0.778 | 0.648 | 0.902 | 0.890 |
| NPV | 0.735 | 0.733 | 0.855 | 0.944 |
| ROC Area * | 0.842 | 0.725 | 0.924 | 0.939 |
| MCC | 0.552 | 0.262 | 0.800 | 0.768 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilic, I.; Babic, G.; Sipetic Grujicic, S.; Zivanovic Macuzic, I.; Ilic, M.; Ravic-Nikolic, A.; Milicic, V. Predicting Pre- and Post-Diagnostic Depression in Women with Abnormal Pap Screening Tests: A Neural Network Approach. Life 2025, 15, 1041. https://doi.org/10.3390/life15071041
Ilic I, Babic G, Sipetic Grujicic S, Zivanovic Macuzic I, Ilic M, Ravic-Nikolic A, Milicic V. Predicting Pre- and Post-Diagnostic Depression in Women with Abnormal Pap Screening Tests: A Neural Network Approach. Life. 2025; 15(7):1041. https://doi.org/10.3390/life15071041
Chicago/Turabian StyleIlic, Irena, Goran Babic, Sandra Sipetic Grujicic, Ivana Zivanovic Macuzic, Milena Ilic, Ana Ravic-Nikolic, and Vesna Milicic. 2025. "Predicting Pre- and Post-Diagnostic Depression in Women with Abnormal Pap Screening Tests: A Neural Network Approach" Life 15, no. 7: 1041. https://doi.org/10.3390/life15071041
APA StyleIlic, I., Babic, G., Sipetic Grujicic, S., Zivanovic Macuzic, I., Ilic, M., Ravic-Nikolic, A., & Milicic, V. (2025). Predicting Pre- and Post-Diagnostic Depression in Women with Abnormal Pap Screening Tests: A Neural Network Approach. Life, 15(7), 1041. https://doi.org/10.3390/life15071041







