Effects of Self-Assisted Manual Therapy Combined with a High-Intensity Walking Program on Musculoskeletal Pain, Functionality, and Posture in Older Adults: A Multicentre Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Randomization and Blinding
2.4. Outcomes
2.4.1. Primary Outcomes
- -
- Pressure pain threshold (PPT): Measured by establishing the minimal pressure (kg/cm2) at which pain is induced using pressure algometry (Wagner Instruments FDK 20, Greenwich, USA). The patient was seated, and the trapezius muscles were assessed bilaterally, applying pressure 3 cm distal to the midpoint of the upper trapezius muscle, performing three measurements on each muscle, with a thirty-second rest between them. The physiotherapist instructed the patient to say “stop” when their sensation changed from pressure to pain. The average of the three scores was obtained for analysis. ICC = 0.91 (95% CI: 0.82, 0.97) [34].
- -
- Pain Intensity: Participants were asked to rate their overall perception of musculoskeletal back pain measured by the Visual analogue scale (VAS), a unidimensional measure of non-specific perceived pain intensity, which has been widely used in diverse adult populations. The pain VAS is a continuous scale comprised of a horizontal or vertical line, typically 10 cm in length (a range of 0 to 100 is established). In order to score pain intensity, the person marked on the scale “no pain” (score of 0) and “worst imaginable pain”. The participants were asked to report “current” pain intensity or pain intensity “in the last 24 h”. A higher score indicates greater pain intensity [35]. The VAS has a high internal consistency (0.92) [36].
2.4.2. Secondary Outcomes
- -
- Functional capacity, using the five Times Sit-to-Stand Test (5XSST) [37,38]. This test assesses risk of recurrent falls, with the cut off score of >15 s, indicating poor functional capacity and risk of falls [39]. For the 5XSST, participants were asked to stand up from and sit down on a slightly padded 43 cm high armless chair as quickly as possible 5 times. Participants folded their arms across their chest and were instructed to stand up completely and make firm contact when sitting. Timing began on the command “go” and stopped when the patient sat down again after the 5th repetition. Participants were allowed a practice trial of 2 repetitions before the timing of 2 test trials of 5 repetitions. The fastest of the 2 test trials was used in subsequent analysis.
- -
- Change in thorax position, based on the distance between the acromion and base, measuring the linear distance from the posterior edge of the acromion to the flat surface. Participants were requested to lie supine on a standard stretcher and adopt their natural relaxed posture. As described by Sahrmann (2001), the participants rested with their arms alongside their body and with the elbows flexed in contact with the lateral wall of the abdomen [40]. The hands rested gently on the abdomen, placing the glenohumeral joint in slight internal rotation. The investigator measured the linear distance in mm using a standard plastic transparent ruler. Without exerting any downward pressure, the base of the protractor was placed on the stretcher, and the vertical side was placed adjacent to the lateral aspect of the acromion. Each measurement for each side was measured 3 times in succession, and on each occasion, the right angle was replaced as previously described. Furthermore, in the same study, they demonstrated the reliability of the test with an ICC of between 0.92 and 0.93 for people with symptoms and between 0.90 and 0.93 for people without symptoms [41].
2.5. Intervention
- Self-administered manual therapy (MTWG). A self-administered manual therapy protocol was carried out in 30-min sessions, including seven techniques adapted from Yilmaz Yelvar et al., 2016 [42]. In addition, two myofascial techniques were added, making a total of 9 techniques. At the beginning and end of each session, breathing exercises were performed to make the participants aware of their breathing [42]. Subsequently, a battery of 9 specific techniques were self-administered: (1) Neurolymphatic technique [43,44]; (2) Suboccipital decompression technique [42]; (3) Gliding technique on the cervical vertebral joints (anterior/posterior) [42]; (4) Inhibition and stretching of the sternocleidomastoid and trapezius muscles [45]; (5) Gliding technique on the sternoclavicular joint using an anterior/posterior direction [42]; (6) Mobilization of the scapulothoracic joint and gliding of the thoracic vertebral joints [42]; (7) Myofascial release technique of intercostal muscles and paravertebral muscles [42] (Yilmaz Yelvar et al., (2016); (8) Diaphragmatic release technique [42]; (9) Rib elevation technique [42]. As noted, breathing exercises were performed at the beginning and the end of each session [42] (Supplementary S1). In each of the centres the implementation of all techniques was guided by a physiotherapist with more than 20 years of experience in manual therapy.
- Walking activity. Walking was performed immediately after the manual therapy intervention in the case of the MTWG, as this has been shown to enhance the synergistic effect of combining the two interventions [46]. It was implemented by the same physiotherapist who guided the self-administered manual therapy. A vigorous or high-intensity walking protocol was followed, having a weekly walking goal of 75 min per week of vigorous aerobic activity, consistent with recommendations of the World Health Organization 2010 [47]. This protocol consisted of supervised walking on a 400 m circular terrain. The Borg perceived exertion scale was used to determine exercise intensity during the walking protocol [48]. In this way, walking goals were customized based on each participant’s level of physical fitness. Before starting the walking time in each session, this scale was described to the participants, and the intensity at which they should walk in each session was indicated. The structure of the walking sessions began with a warm-up where participants walked at <12 grades of the Borg scale, with a duration of 10 min. After the warm-up, participants walked at a target intensity of minimum of 16 on the Borg scale for 40 min, reaching an intensity at which they could not hold a conversation [49]. Afterwards, a cool-down was performed for 10 min.
2.6. Sample Size Calculation
2.7. Statistical Analysis
3. Results
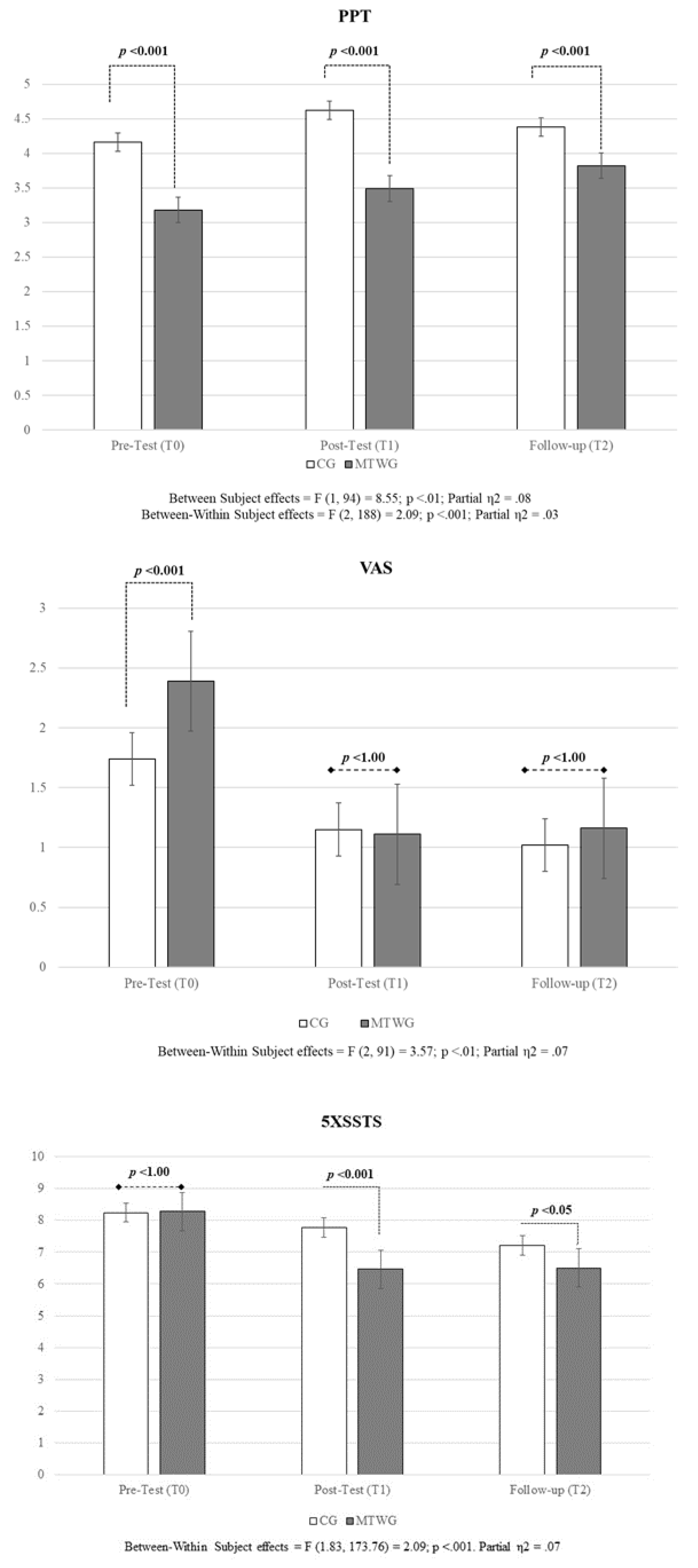
3.1. Primary Outcomes
3.2. Secondary Outcomes
4. Discussion
Strength and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MTWG | manual therapy plus walking at high-intensity Group |
| CG | Comparator-controlled group |
| PPT | pressure pain threshold |
| VAS | visual analogue scale |
| BMI | body mass index |
| 5XSST | five Times Sit-to-Stand Test |
| ACROM | distance between the acromion and base |
References
- Envejecimiento y Salud. Available online: https://www.who.int/es/news-room/fact-sheets/detail/ageing-and-health (accessed on 31 July 2024).
- Hussain, A.; Umair, M.; Khan, S.; Alonazi, W.B.; Almutairi, S.S.; Malik, A. Exploring Sustainable Healthcare: Innovations in Health Economics, Social Policy, and Management. Heliyon 2024, 10, e33186. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.J. The Longevity Economy. Lancet Healthy Longev. 2021, 2, e828–e835. [Google Scholar] [CrossRef] [PubMed]
- De Jaeger, C. Fisiología del envejecimiento. EMC Kinesiterapia Med. Física 2018, 39, 1–12. [Google Scholar] [CrossRef]
- Ünlüer, N.Ö.; Ateş, Y. An Investigation of Neck Pain in Older Adults, and Its Relation with Shoulder Position Sense and Upper Extremity Function. Somatosens. Mot. Res. 2021, 38, 333–338. [Google Scholar] [CrossRef]
- Domínguez-Gasca, L.; Chico-Carpizo, F.; Magaña-Reyes, J.; Domínguez-Carrillo, L. Lesiones de Hombro En La Tercera Edad y Su Repercusión Funcional En Escala de DASH. Acta Ortopédica Mex. 2018, 32, 13–16. [Google Scholar]
- Hogg-Johnson, S.; Van Der Velde, G.; Carroll, L.J.; Holm, L.W.; Cassidy, J.D.; Guzman, J.; Côté, P.; Haldeman, S.; Ammendolia, C.; Carragee, E.; et al. The Burden and Determinants of Neck Pain in the General Population: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33, S39–S51. [Google Scholar] [CrossRef]
- Mika, A.; Unnithan, V.B.; Mika, P. Differences in Thoracic Kyphosis and in Back Muscle Strength in Women with Bone Loss due to Osteoporosis. Spine 2005, 30, 241–246. [Google Scholar] [CrossRef]
- Tavares, D.; Schlemer, G.B.V.; Turchiello, M.P.; dos Santos, J.C.; Pivetta, H.M.F.; Braz, M.M. Perfil Da Postural Corporal Estática Em Idosos: Revisão Integrativa. Salão Inter Ensino Pesq Ext 2018, 10, 1–4. [Google Scholar]
- Szeto, G.P.Y.; Straker, L.; Raine, S. A Field Comparison of Neck and Shoulder Postures in Symptomatic and Asymptomatic Office Workers. Appl. Ergon. 2002, 33, 75–84. [Google Scholar] [CrossRef]
- Kado, D.M.; Huang, M.-H.; Nguyen, C.B.; Barrett-Connor, E.; Greendale, G.A. Hyperkyphotic Posture and Risk of Injurious Falls in Older Persons: The Rancho Bernardo Study. J. Gerontol. A. Biol. Sci. Med. Sci. 2007, 62, 652–657. [Google Scholar] [CrossRef]
- Huang, M.-H.; Barrett-Connor, E.; Greendale, G.A.; Kado, D.M. Hyperkyphotic Posture and Risk of Future Osteoporotic Fractures: The Rancho Bernardo Study. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2006, 21, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, M.; De Souto Barreto, P.; Arai, H.; Bischoff-Ferrari, H.A.; Cadore, E.L.; Cesari, M.; Chen, L.-K.; Coen, P.M.; Courneya, K.S.; Duque, G.; et al. Global Consensus on Optimal Exercise Recommendations for Enhancing Healthy Longevity in Older Adults (ICFSR). J. Nutr. Health Aging 2025, 29, 100401. [Google Scholar] [CrossRef]
- Booth, J.; Moseley, G.L.; Schiltenwolf, M.; Cashin, A.; Davies, M.; Hübscher, M. Exercise for Chronic Musculoskeletal Pain: A Biopsychosocial Approach. Musculoskelet. Care 2017, 15, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Gmiąt, A.; Jaworska, J.; Micielska, K.; Kortas, J.; Prusik, K.; Prusik, K.; Lipowski, M.; Radulska, A.; Szupryczyńska, N.; Antosiewicz, J.; et al. Improvement of Cognitive Functions in Response to a Regular Nordic Walking Training in Elderly Women—A Change Dependent on the Training Experience. Exp. Gerontol. 2018, 104, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Gomeñuka, N.A.; Oliveira, H.B.; Silva, E.S.; Costa, R.R.; Kanitz, A.C.; Liedtke, G.V.; Schuch, F.B.; Peyré-Tartaruga, L.A. Effects of Nordic Walking Training on Quality of Life, Balance and Functional Mobility in Elderly: A Randomized Clinical Trial. PLoS ONE 2019, 14, e0211472. [Google Scholar] [CrossRef]
- Huang, Y.-H.; Fang, I.-Y.; Kuo, Y.-L. The Influence of Nordic Walking on Spinal Posture, Physical Function, and Back Pain in Community-Dwelling Older Adults: A Pilot Study. Healthcare 2021, 9, 1303. [Google Scholar] [CrossRef]
- Podsiadło, S.; Skiba, A.; Kałuża, A.; Ptaszek, B.; Stożek, J.; Skiba, A.; Marchewka, A. Influence of Nordic Walking Training on Vitamin D Level in the Blood and Quality of Life among Women Aged 65–74. Healthcare 2021, 9, 1146. [Google Scholar] [CrossRef]
- Saeterbakken, A.H.; Nordengen, S.; Andersen, V.; Fimland, M.S. Nordic Walking and Specific Strength Training for Neck- and Shoulder Pain in Office Workers: A Pilot-Study. Eur. J. Phys. Rehabil. Med. 2017, 53, 928–935. [Google Scholar] [CrossRef]
- Suh, J.H.; Kim, H.; Jung, G.P.; Ko, J.Y.; Ryu, J.S. The Effect of Lumbar Stabilization and Walking Exercises on Chronic Low Back Pain: A Randomized Controlled Trial. Medicine 2019, 98, e16173. [Google Scholar] [CrossRef]
- Fathollahnejad, K.; Letafatkar, A.; Hadadnezhad, M. The Effect of Manual Therapy and Stabilizing Exercises on Forward Head and Rounded Shoulder Postures: A Six-Week Intervention with a One-Month Follow-up Study. BMC Musculoskelet. Disord. 2019, 20, 86. [Google Scholar] [CrossRef]
- Henley, C.E.; Ivins, D.; Mills, M.; Wen, F.K.; Benjamin, B.A. Osteopathic Manipulative Treatment and Its Relationship to Autonomic Nervous System Activity as Demonstrated by Heart Rate Variability: A Repeated Measures Study. Osteopath. Med. Prim. Care 2008, 2, 7. [Google Scholar] [CrossRef] [PubMed]
- Bron, C.; de Gast, A.; Dommerholt, J.; Stegenga, B.; Wensing, M.; Oostendorp, R.A.B. Treatment of Myofascial Trigger Points in Patients with Chronic Shoulder Pain: A Randomized, Controlled Trial. BMC Med. 2011, 9, 8. [Google Scholar] [CrossRef] [PubMed]
- Hains, G.; Descarreaux, M.; Hains, F. Chronic Shoulder Pain of Myofascial Origin: A Randomized Clinical Trial Using Ischemic Compression Therapy. J. Manip. Physiol. Ther. 2010, 33, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sánchez, A.M.; Matarán-Peñarrocha, G.A.; Arroyo-Morales, M.; Saavedra-Hernández, M.; Fernández-Sola, C.; Moreno-Lorenzo, C. Effects of Myofascial Release Techniques on Pain, Physical Function, and Postural Stability in Patients with Fibromyalgia: A Randomized Controlled Trial. Clin. Rehabil. 2011, 25, 800–813. [Google Scholar] [CrossRef]
- Rocha, H.M.; Muniz de Souza, H.C.; Viana, R.; Neves, V.R.; Dornelas de Andrade, A. Immediate Effects of Rib Mobilization and Diaphragm Release Techniques on Cardiac Autonomic Control in Patients with Chronic Obstructive Pulmonary Disease: A Pilot Study. J. Chiropr. Med. 2020, 19, 167–174. [Google Scholar] [CrossRef]
- Cunha, A.C.V.; Burke, T.N.; França, F.J.R.; Marques, A.P. Effect of Global Posture Reeducation and of Static Stretching on Pain, Range of Motion, and Quality of Life in Women with Chronic Neck Pain: A Randomized Clinical Trial. Clinics 2008, 63, 763–770. [Google Scholar] [CrossRef]
- Liang, X.; You, M.; Wen, C.; Hou, F.; Kang, J.; Lv, Z.; Tian, J. Self-Administration of Complex Decongestive Therapy Facilitated by the Mobile Application WeChat Improves Lymphedema and Quality of Life in Breast Cancer Survivors: An Observational Study. Ann. Transl. Med. 2022, 10, 146. [Google Scholar] [CrossRef]
- Trapé, A.A.; Lizzi, E.A.D.S.; Gonçalves, T.C.P.; Rodrigues, J.A.L.; Tavares, S.S.; Lacchini, R.; Pinheiro, L.C.; Ferreira, G.C.; Tanus-Santos, J.E.; Ovídio, P.P.; et al. Effect of Multicomponent Training on Blood Pressure, Nitric Oxide, Redox Status, and Physical Fitness in Older Adult Women: Influence of Endothelial Nitric Oxide Synthase (NOS3) Haplotypes. Oxid. Med. Cell. Longev. 2017, 2017, 2578950. [Google Scholar] [CrossRef]
- VanDerVeer, S.; Markert, R.; Bickford, B.; Yuhas, J.; Pikman, P.; Wall, T.; Burtson, K. Increasing Exercise Adherence among Elderly Patients with Chronic Disease in Primary Care: A Prospective Cohort Study. BMC Geriatr. 2021, 21, 616. [Google Scholar] [CrossRef]
- World Medical Association. Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191. [Google Scholar] [CrossRef]
- Lobo, A.; Saz, P.; Marcos, G.; Día, J.L.; de la Cámara, C.; Ventura, T.; Morales Asín, F.; Fernando Pascual, L.; Montañés, J.A.; Aznar, S. Revalidation and standardization of the cognition mini-exam (first Spanish version of the Mini-Mental Status Examination) in the general geriatric population. Med. Clin. 1999, 112, 767–774. [Google Scholar]
- Charlson, M.E.; Charlson, R.E.; Peterson, J.C.; Marinopoulos, S.S.; Briggs, W.M.; Hollenberg, J.P. The Charlson Comorbidity Index Is Adapted to Predict Costs of Chronic Disease in Primary Care Patients. J. Clin. Epidemiol. 2008, 61, 1234–1240. [Google Scholar] [CrossRef]
- Chesterton, L.S.; Sim, J.; Wright, C.C.; Foster, N.E. Interrater Reliability of Algometry in Measuring Pressure Pain Thresholds in Healthy Humans, Using Multiple Raters. Clin. J. Pain 2007, 23, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of Adult Pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar] [CrossRef]
- Scott, J.; Huskisson, E.C. Vertical or Horizontal Visual Analogue Scales. Ann. Rheum. Dis. 1979, 38, 560. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Bubela, D.J.; Magasi, S.R.; Wang, Y.-C.; Gershon, R.C. Sit-to-Stand Test: Performance and Determinants across the Age-Span. Isokinet. Exerc. Sci. 2010, 18, 235–240. [Google Scholar] [CrossRef]
- Coltman, C.E.; Steele, J.R.; McGhee, D.E. Effect of Breast Size on Upper Torso Musculoskeletal Structure and Function: A Cross-Sectional Study. Plast. Reconstr. Surg. 2019, 143, 686–695. [Google Scholar] [CrossRef]
- Buatois, S.; Perret-Guillaume, C.; Gueguen, R.; Miget, P.; Vançon, G.; Perrin, P.; Benetos, A. A Simple Clinical Scale to Stratify Risk of Recurrent Falls in Community-Dwelling Adults Aged 65 Years and Older. Phys. Ther. 2010, 90, 550–560. [Google Scholar] [CrossRef]
- Sahrmann, S. Diagnosis and Treatment of Movement Impairment Syndromes—E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2001; ISBN 978-0-323-26635-2. [Google Scholar]
- Lewis, J.S.; Valentine, R.E. The Pectoralis Minor Length Test: A Study of the Intra-Rater Reliability and Diagnostic Accuracy in Subjects with and without Shoulder Symptoms. BMC Musculoskelet. Disord. 2007, 8, 64. [Google Scholar] [CrossRef]
- Yilmaz Yelvar, G.D.; Cirak, Y.; Parlak Demir, Y.; Dalkilinc, M.; Bozkurt, B. Immediate Effect of Manual Therapy on Respiratory Functions and Inspiratory Muscle Strength in Patients with COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2016, 11, 1353–1357. [Google Scholar] [CrossRef]
- Espí-López, G.V.; Ruescas-Nicolau, M.-A.; Sanchez-Sanchez, M.L.; Arnal-Gómez, A.; Balasch-Bernat, M.; Marques-Sule, E. Immediate Changes After Manual Therapy in Patients wth Persistent, Nonspecific Back Pain: A Randomized Controlled Trial. Altern. Ther. Health Med. 2018, 24, 14–23. [Google Scholar] [PubMed]
- Pánková, K.; Hlavácek, V. Rheumatoid in childhood and Movirene (author’s transl). Acta Chir. Orthop. Traumatol. Cech. 1977, 44, 335–336. [Google Scholar] [PubMed]
- Simons, D.G.; Travell, J.G.; Simons, L.S. Travell & Simons’ Myofascial Pain and Dysfunction: Upper Half of Body; Lippincott Williams & Wilkins: Waltham, MA, USA, 1999; Volume 1, ISBN 0-683-08363-5. [Google Scholar]
- Engel, R.M.; Vemulpad, S. The Effect of Combining Manual Therapy with Exercise on the Respiratory Function of Normal Individuals: A Randomized Control Trial. J. Manip. Physiol. Ther. 2007, 30, 509–513. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Recommendations on Physical Activity for Health; WHO: Geneva Switzerland, 2010; p. 60. [Google Scholar]
- Fielding, R.A.; Rejeski, W.J.; Blair, S.; Church, T.; Espeland, M.A.; Gill, T.M.; Guralnik, J.M.; Hsu, F.-C.; Katula, J.; King, A.C.; et al. The Lifestyle Interventions and Independence for Elders Study: Design and Methods. J. Gerontol. A. Biol. Sci. Med. Sci. 2011, 66, 1226–1237. [Google Scholar] [CrossRef]
- Bok, D.; Rakovac, M.; Foster, C. An Examination and Critique of Subjective Methods to Determine Exercise Intensity: The Talk Test, Feeling Scale, and Rating of Perceived Exertion. Sports Med. 2022, 52, 2085–2109. [Google Scholar] [CrossRef]
- Da Costa, B.R.; Saadat, P.; Basciani, R.M.; Agarwal, A.; Johnston, B.C.; Jüni, P. Visual Analogue Scale Has Higher Assay Sensitivity than WOMAC Pain in Detecting Between-Group Differences in Treatment Effects: A Meta-Epidemiological Study. Osteoarthr. Cartil. 2021, 29, 304–312. [Google Scholar] [CrossRef]
- Espí-López, G.V.; Zurriaga-Llorens, R.; Monzani, L.; Falla, D. The Effect of Manipulation plus Massage Therapy versus Massage Therapy Alone in People with Tension-Type Headache. A Randomized Controlled Clinical Trial. Eur. J. Phys. Rehabil. Med. 2016, 52, 606–617. [Google Scholar]
- Binderup, A.T.; Arendt-Nielsen, L.; Madeleine, P. Pressure pain threshold mapping of the trapezius muscle reveals heterogeneity in the distribution of muscular hyperalgesia after eccentric exercise. Eur. J. Pain. 2010, 14, 705–712. [Google Scholar] [CrossRef]
- Moraska, A.F.; Stenerson, L.; Butryn, N.; Krutsch, J.P.; Schmiege, S.J.; Mann, J.D. Myofascial Trigger Point-Focused Head and Neck Massage for Recurrent Tension-Type Headache: A Randomized, Placebo-Controlled Clinical Trial. Clin. J. Pain 2015, 31, 159–168. [Google Scholar] [CrossRef]
- Dahlhamer, J. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1001–1006. [Google Scholar] [CrossRef]
- Nasir, M.F.; Jawed, R.; Baig, N.N.; Younus, M.; Arshad, A.; Tahir, A. A Study to Observe the Effects of Physiotherapy with and without Manual Therapy in the Management Postural Neck Pain: A Randomized Control Trial. J. Pak. Med. Assoc. 2021, 71, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Arjona Retamal, J.J.; Fernández Seijo, A.; Torres Cintas, J.D.; de-la-Llave-Rincón, A.I.; Caballero Bragado, A. Effects of Instrumental, Manipulative and Soft Tissue Approaches for the Suboccipital Region in Subjects with Chronic Mechanical Neck Pain. A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 8636. [Google Scholar] [CrossRef] [PubMed]
- Nakamaru, K.; Aizawa, J.; Kawarada, K.; Uemura, Y.; Koyama, T.; Nitta, O. Immediate Effects of Thoracic Spine Self-Mobilization in Patients with Mechanical Neck Pain: A Randomized Controlled Trial. J. Bodyw. Mov. Ther. 2019, 23, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Omura, J.D.; Ussery, E.N.; Loustalot, F.; Fulton, J.E.; Carlson, S.A. Walking as an Opportunity for Cardiovascular Disease Prevention. Prev. Chronic Dis. 2019, 16, 180690. [Google Scholar] [CrossRef]
- Voukelatos, A.; Merom, D.; Rissel, C.; Sherrington, C.; Watson, W.; Waller, K. The Effect of Walking on Falls in Older People: The “Easy Steps to Health” Randomized Controlled Trial Study Protocol. BMC Public Health 2011, 11, 888. [Google Scholar] [CrossRef]
- Chodzko-Zajko, W.J. ACSM’s Exercise for Older Adults; Lippincott Williams & Wilkins: Waltham, MA, USA, 2014; ISBN 978-1-60913-647-5. [Google Scholar]
- Kocur, P.; Pospieszna, B.; Choszczewski, D.; Michalowski, L.; Wiernicka, M.; Lewandowski, J. The Effects of Nordic Walking Training on Selected Upper-Body Muscle Groups in Female-Office Workers: A Randomized Trial. Work 2017, 56, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Heo, M.-Y.; Kim, K.; Hur, B.-Y.; Nam, C.-W. The Effect of Lumbar Stabilization Exercises and Thoracic Mobilization and Exercises on Chronic Low Back Pain Patients. J. Phys. Ther. Sci. 2015, 27, 3843–3846. [Google Scholar] [CrossRef]
- Yuen, T.S.; Lam, P.Y.; Lau, M.Y.; Siu, W.L.; Yu, K.M.; Lo, C.N.; Ng, J. Changes in Lower Limb Strength and Function Following Lumbar Spinal Mobilization. J. Manip. Physiol. Ther. 2017, 40, 587–596. [Google Scholar] [CrossRef]
- Jeong, H.-J.; Kim, B.-J. The Effect of Thoracic Joint Mobilization on the Changes of the Thoracic Kyphosis Angle and Static and Dynamic Balance. Biomed. Sci. Lett. 2019, 25, 149–158. [Google Scholar] [CrossRef]
- Drzał-Grabiec, J.; Snela, S.; Rykała, J.; Podgórska, J.; Banaś, A. Changes in the Body Posture of Women Occurring with Age. BMC Geriatr. 2013, 13, 108. [Google Scholar] [CrossRef]
- Thoomes, E.J. Effectiveness of Manual Therapy for Cervical Radiculopathy, a Review. Chiropr. Man. Ther. 2016, 24, 45. [Google Scholar] [CrossRef] [PubMed]
- Espí-López, G.V.; Inglés, M.; Soliva-Cazabán, I.; Serra-Añó, P. Effect of the Soft-Tissue Techniques in the Quality of Life in Patients with Crohn’s Disease: A Randomized Controlled Trial. Medicine 2018, 97, e13811. [Google Scholar] [CrossRef] [PubMed]
- Jaeger, B. Myofascial Trigger Point Pain. Alpha Omegan 2013, 106, 14–22. [Google Scholar]
- Nitayarak, H.; Charntaraviroj, P. Effects of Scapular Stabilization Exercises on Posture and Muscle Imbalances in Women with Upper Crossed Syndrome: A Randomized Controlled Trial. J. Back Musculoskelet. Rehabil. 2021, 34, 1031–1040. [Google Scholar] [CrossRef]
- Mercado Rus, M. Manual de Fisioterapia Respiratoria; Ergon: Baden-Baden, Germany, 2003; ISBN 84-8473-144-8. [Google Scholar]
- Babatunde, O.O.; Jordan, J.L.; Van Der Windt, D.A.; Hill, J.C.; Foster, N.E.; Protheroe, J. Effective Treatment Options for Musculoskeletal Pain in Primary Care: A Systematic Overview of Current Evidence. PLoS ONE 2017, 12, e0178621. [Google Scholar] [CrossRef] [PubMed]
- Yanuck, S.B.; Fox, S.K.; Harting, B.R.; Motyka, T.M. Effect of Manual Manipulation on Mechanical Gait Parameters. J. Osteopath. Med. 2024, 124, 437–446. [Google Scholar] [CrossRef]
- Krekoukias, G.; Sakellari, V.; Anastasiadi, E.; Gioftsos, G.; Dimitriadis, Z.; Soultanis, K.; Gelalis, I.D. Gait Kinetic and Kinematic Changes in Chronic Low Back Pain Patients and the Effect of Manual Therapy: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 3593. [Google Scholar] [CrossRef]
- Sun, M.; Min, L.; Xu, N.; Huang, L.; Li, X. The Effect of Exercise Intervention on Reducing the Fall Risk in Older Adults: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2021, 18, 12562. [Google Scholar] [CrossRef]
- Anton, S.D.; Cruz-Almeida, Y.; Singh, A.; Alpert, J.; Bensadon, B.; Cabrera, M.; Clark, D.J.; Ebner, N.C.; Esser, K.A.; Fillingim, R.B.; et al. Innovations in Geroscience to Enhance Mobility in Older Adults. Exp. Gerontol. 2020, 142, 111123. [Google Scholar] [CrossRef]
- Du, S.; Hu, L.; Dong, J.; Xu, G.; Chen, X.; Jin, S.; Zhang, H.; Yin, H. Self-Management Program for Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Patient Educ. Couns. 2017, 100, 37–49. [Google Scholar] [CrossRef]
- Silveira, P.; Reve, E.V.H.; Daniel, F.; Casati, F.; De Bruin, E.D. Motivating and Assisting Physical Exercise in Independently Living Older Adults: A Pilot Study. Int. J. Med. Inf. 2013, 82, 325–334. [Google Scholar] [CrossRef] [PubMed]


| Categories/Units | Total Sample N = 114 | MTWG N = 50 | CG N = 64 | p | |
|---|---|---|---|---|---|
| Sex n (%) | Women | 85(74.60%) | 36 (72%) | 49 (76.60%) | 0.58 B |
| Men | 29 (25.40%) | 14 (28%) | 15 (23.40%) | ||
| Age (mean/SD) | Years | 69.40 (4.20) | 69.70 (4.30) | 69.30 (5.50) | 0.65 B |
| Marital status n (%) | Single | 11 (9.60%) | 7 (14%) | 4 (6.30%) | 0.00 A* |
| Married | 64 (56.10%) | 24 (48%) | 40 (62.50%) | ||
| Widowed | 20 (17.50%) | 9 (18%) | 11 (17.20%) | ||
| Divorced | 15 (13.20%) | 9 (18%) | 6 (9.40%) | ||
| Separated | 2 (1.80%) | 2 (3.10%) | |||
| Other | 2 (1.80%) | 1 (2%) | 1 (1.60%) | ||
| Level of education n (%) | Primary | 1 (0.90%) | 1 (1.60%) | 0.00 A* | |
| Secondary | 38 (33.40%) | 16 (32%) | 22 (34.40%) | ||
| University | 75 (65.80%) | 34 (68%) | 41 (64.10%) | ||
| Employment status n (%) | Employed | 10 (8.80%) | 1(2%) | 9 (14.10%) | 0.00 A* |
| Retired | 104 (91.20%) | 49 (98%) | 55 (85.90%) | ||
| Weight mean (SD) | kg | 70.01 (12.45) | 69.72 (11.45) | 70.23 (13.26) | 0.81 A |
| Height mean (SD) | m | 1.63 (.08) | 1.63 (0.09) | 1.63 (0.79) | 0.99 A |
| Body mass index mean (SD) | kg/m2 | 26.18 (4.24) | 26.09 (4.11) | 26.25 (4.37) | 0.85 B |
| Charlson Comorbidity index (IRQ) | Total score | 0.00 (3.00) | 0.00 (2.00) | 0.00 (3.00) | 0.66 C |
| Mini-mental Cognitive Test (IRQ) | Scores | 34(6.00) | 34(3.00) | 34(2.00) | 0.19 C |
| − | M | SD | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Group | 1.45 | 0.50 | - | ||||||||||||||
| 2. PPT–T0 | 3.64 | 1.53 | −0.29 ** | - | |||||||||||||
| 3. PPT–T1 | 4.17 | 1.78 | −0.31 ** | 0.72 ** | - | ||||||||||||
| 4. PPT–T2 | 4.12 | 1.75 | −0.17 | 0.75 ** | 0.76 ** | - | |||||||||||
| 5. VAS–T0 | 2.09 | 1.63 | 0.24 * | −0.04 | −0.08 | −0.04 | - | ||||||||||
| 6. VAS–T1 | 1.10 | 1.17 | −0.01 | −0.03 | −0.21 * | −0.08 | 0.49 ** | - | |||||||||
| 7. VAS–T2 | 1.10 | 1.39 | 0.06 | −0.06 | −0.10 | −0.04 | 0.72 ** | 0.56 ** | - | ||||||||
| 8. ACROM R– T0 | 8.36 | 1.90 | −0.32 ** | 0.32 ** | 0.31 ** | 0.23 * | −0.15 | 0.10 | −0.07 | - | |||||||
| 9. ACROM R–T1 | 8.13 | 1.60 | −0.20 * | 0.20 * | 0.23 * | 0.19 | −0.22 * | 0.09 | −0.07 | 0.69 ** | - | ||||||
| 10. ACROM R–T2 | 7.94 | 1.76 | −0.36 ** | 0.37 ** | 0.38 ** | 0.22 * | −0.17 | 0.08 | −0.01 | 0.62 ** | 0.75 ** | - | |||||
| 11. ACROM L–T0 | 8.18 | 1.84 | −0.30 ** | 0.35 ** | 0.35 ** | 0.30 ** | −0.15 | 0.09 | −0.06 | 0.87 ** | 0.64 ** | 0.61 ** | - | ||||
| 12. ACROM L–T1 | 7.99 | 1.63 | −0.18 | 0.29 ** | 0.27 ** | 0.24 * | −0.21 * | 0.10 | −0.06 | 0.67 ** | 0.86 ** | 0.71 ** | 0.77 ** | - | |||
| 13. ACROM L–T2 | 7.82 | 1.83 | −0.36 ** | 0.40 ** | 0.45 ** | 0.20 * | −0.21 * | 0.02 | −0.01 | 0.57 ** | 0.67 ** | 0.92 ** | 0.64 ** | −0.01 | - | ||
| 14. 5XSST–T0 | 8.39 | 2.43 | 0.03 | −0.002 | 0.04 | 0.16 | 0.35 ** | 0.13 | 0.32 ** | −0.16 | −0.11 | −0.05 | −0.07 | 0.25 * | 0.66 ** | - | |
| 15. 5XSST–T1 | 7.26 | 2.42 | −0.29 ** | 0.06 | 0.15 | 0.21 * | 0.02 | 0.21 * | 0.27 ** | 0.10 | 0.14 | 0.20 * | 0.17 | 0.13 | 0.60 ** | 0.79 ** | - |
| 16. 5XSST–T2 | 6.94 | 2.34 | −0.13 | 0.08 | 0.04 | 0.03 | 0.15 | 0.23 * | 0.42 ** | −0.04 | −0.05 | 0.09 | 0.02 | 0.00 | 0.13 | 0.60 ** | 0.79 ** |
| EMM (SE); [95 CI%] | F-Test | ||||
|---|---|---|---|---|---|
| T0 | T1 | T2 | |||
| PPT | CG | 4.16 (0.20); [3.76, 4.57] | 4.62 (0.23); [4.17, 5.07] | 4.38 (0.24); [3.91, 4.85] | W-S: F (2, 188) = 7.51; p < 0.001; Partial η2 = 0.07 |
| MTWG | 3.18 (0.23); [2.72, 3.69] | 3.49 (0.25); [2.91, 3.99] | 3.82 (0.27); [3.29, 4.36] | ||
| F-Test | B-S: F (1, 94) = 8.55; p < 0.01; Partial η2 = 0.08 | B-W: F (2, 188) = 2.09; p < 0.001; Partial η2 = 0.03 | |||
| VAS | CG | 1.74 (0.21); [1.34, 2.16] | 1.15 (0.16); [0.83, 1.48] | 1.02 (0.19); [0.65, 1.40] | W-S: Wilks Λ = 0.54, F (2, 91) = 38.91; p < 0.0001; Partial η2 = 0.46 |
| MTWG | 2.39 (0.24); [1.91, 2.88] | 1.11 (0.19); [0.74, 1.49] | 1.16 (0.22); [0.72, 1.60] | ||
| F-Test | B-S: F (1, 92) = 1.02, ns; Partial η2 = 0.01 | W-B: Wilks Λ = 0.93, F (2, 91) = 3.57; p < 0.01; Partial η2 = 0.07 | |||
| 5XSST | CG | 8.24 (0.32); [7.61, 8.87] | 7.77 (0.31); [7.16, 8.39] | 7.21 (0.31); [6.59, 7.84] | W-S: F (1.83, 173.76) = 7.51; p < 0.001; Partial η2 = 0.25 |
| MTWG | 8.28 (0.36); [7.56, 9.00] | 6.46 (0.36); [5.75, 7.16] | 6.50 (0.36); [5.79, 7.22] | ||
| F-Test | B-S: F (1, 95) = 2.43, ns; Partial η2 = 0.03 | B-W: F (1.83, 173.76) = 2.09; p < 0.001; Partial η2 = 0.07 | |||
| ACROM R | CG | 8.89 (0.25); [8.39, 9.39] | 8.42 (0.22); [7.99, 8.85] | 8.50 (0.23); [8.06, 8.95] | W-S: F (1.83, 171.78) = 5.93, p < 0.01; Partial η2 = 0.06 |
| MTWG | 7.88 (0.28); [7.31, 8.43] | 7.84 (0.25); [7.35, 8.33] | 7.27 (0.28); [6.76, 7.77] | ||
| ACROM L | CG | 8.65 (0.23); [8.18, 9.11] | 8.20 (0.23); [7.75, 8.65] | 8.42 (0.23); [7.95, 8.88] | W-S: F (1.80, 169.19) = 5.20, p < 0.01; Partial η2 = 0.05 |
| MTWG | 7.78 (0.27); [7.24, 8.30] | 7.71 (0.26); [7.20, 8.22] | 7.13 (0.26); [6.60, 7.65] | ||
| F-Test | B-S: Wilks Λ = 0.91, F (4, 91) = 4.69; p < 0.01; Partial η2 = 0.09 | W-B: Wilks Λ = 0.89, F (4, 91) = 2.71, p < 0.05; Partial η2 = 0.11 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Espí-López, G.V.; Fuentes-Aparicio, L.; Cogollos-de-la-Peña, R.; Monzani, L.; Marques-Sule, E.; Pavlu, D.; Arnal-Gómez, A. Effects of Self-Assisted Manual Therapy Combined with a High-Intensity Walking Program on Musculoskeletal Pain, Functionality, and Posture in Older Adults: A Multicentre Randomized Controlled Trial. Life 2025, 15, 844. https://doi.org/10.3390/life15060844
Espí-López GV, Fuentes-Aparicio L, Cogollos-de-la-Peña R, Monzani L, Marques-Sule E, Pavlu D, Arnal-Gómez A. Effects of Self-Assisted Manual Therapy Combined with a High-Intensity Walking Program on Musculoskeletal Pain, Functionality, and Posture in Older Adults: A Multicentre Randomized Controlled Trial. Life. 2025; 15(6):844. https://doi.org/10.3390/life15060844
Chicago/Turabian StyleEspí-López, Gemma Victoria, Laura Fuentes-Aparicio, Rocío Cogollos-de-la-Peña, Lucas Monzani, Elena Marques-Sule, Dagmar Pavlu, and Anna Arnal-Gómez. 2025. "Effects of Self-Assisted Manual Therapy Combined with a High-Intensity Walking Program on Musculoskeletal Pain, Functionality, and Posture in Older Adults: A Multicentre Randomized Controlled Trial" Life 15, no. 6: 844. https://doi.org/10.3390/life15060844
APA StyleEspí-López, G. V., Fuentes-Aparicio, L., Cogollos-de-la-Peña, R., Monzani, L., Marques-Sule, E., Pavlu, D., & Arnal-Gómez, A. (2025). Effects of Self-Assisted Manual Therapy Combined with a High-Intensity Walking Program on Musculoskeletal Pain, Functionality, and Posture in Older Adults: A Multicentre Randomized Controlled Trial. Life, 15(6), 844. https://doi.org/10.3390/life15060844








