Arthroscopic Anterior Cuciate Ligament Reconstruction Using Neither a Tourniquet nor Drainage: A Perioperative Case Series Report
Abstract
1. Introduction
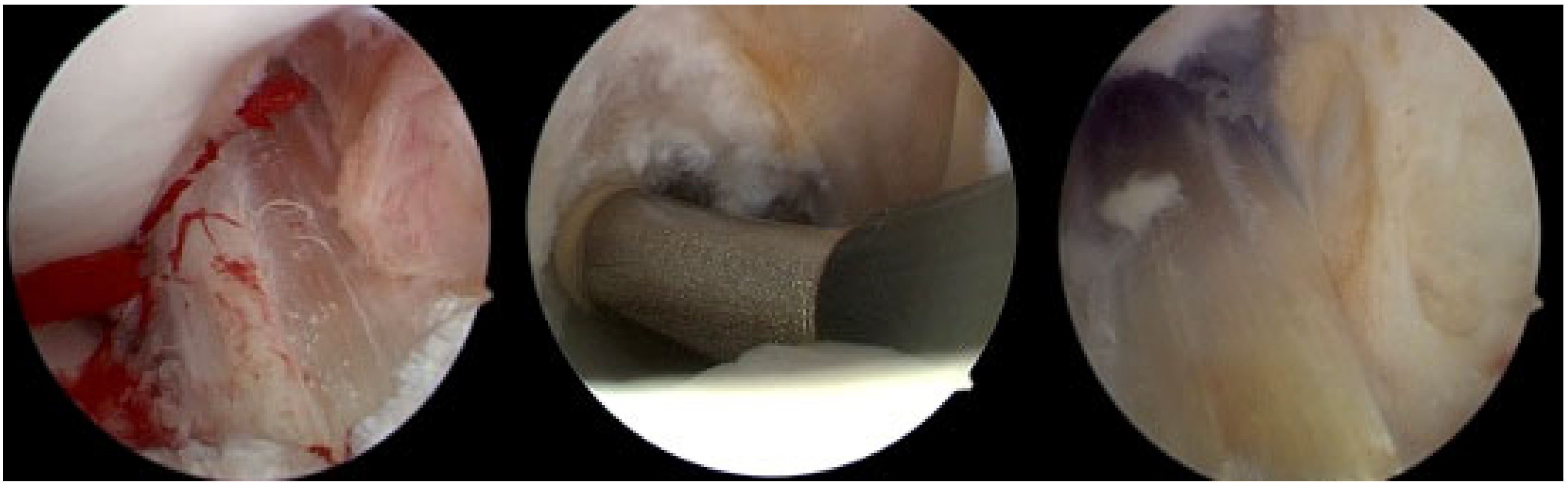
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, J.; Xu, W.; Lv, J. Is It Better to Routinely Use Tourniquet for Knee Arthroscopic Surgery: A Systematic Review and Meta-analysis. J. Knee Surg. 2020, 33, 866–874. [Google Scholar] [CrossRef] [PubMed]
- Shu, H.T.; Bodendorfer, B.M.; Michaelson, E.M.; Argintar, E.H. Posteromedial versus Anteromedial Hamstring Tendon Harvest for Anterior Cruciate Ligament Reconstruction: A Retrospective Comparison of Accidental Gracilis Harvests, Outcomes, and Operative Times. J. Knee Surg. 2019, 32, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Williams, A. Tourniquet Use Did Not Adversely Affect Recovery After Arthroscopic Meniscectomy. J. Bone Jt. Surg. 2013, 95, 1514. [Google Scholar] [CrossRef]
- Reda, W.; El Guindy, A.M.F.; Zahry, G.; Faggal, M.S.; Karim, M.A. Anterior cruciate ligament reconstruction; is a tourniquet necessary? A randomized controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2948–2952. [Google Scholar] [CrossRef]
- Tsarouhas, A.; Hantes, M.E.; Tsougias, G.; Dailiana, Z.; Malizos, K.N. Tourniquet Use Does Not Affect Rehabilitation, Return to Activities, and Muscle Damage After Arthroscopic Meniscectomy: A Prospective Randomized Clinical Study. Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 1812–1818. [Google Scholar] [CrossRef]
- Wu, H.; Chen, L.-X.; Li, Y.-L.; Wu, Q.; Wu, Q.-L.; Ning, G.-Z.; Feng, S.-Q. Tourniquet used in anterior cruciate ligament reconstruction: A system review. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 999–1003. [Google Scholar] [CrossRef]
- Arciero, R.A.; Scoville, C.R.; Hayda, R.A.; Snyder, R.J. The Effect of Tourniquet Use in Anterior Cruciate Ligament Reconstruction: A Prospective, Randomized Study. Am. J. Sports Med. 1996, 24, 758–764. [Google Scholar] [CrossRef]
- Hooper, J.; Rosaeg, O.P.; Krepski, B.; Johnson, D.H. Tourniquet inflation during arthroscopic knee ligament surgery does not increase postoperative pain. Can. J. Anesth. 1999, 46, 925–929. [Google Scholar] [CrossRef]
- Vermesan, D.; Vermesan, D.; Trocan, I.; Prejbeanu, R.; Poenaru, D.V.; Haragus, H.; Gratian, D.; Marrelli, M.; Inchingolo, F.; Caprio, M.; et al. Reduced Operating Time but Not Blood Loss with Cruciate Retaining Total Knee Arthroplasty. J. Clin. Med. Res. 2015, 7, 171–175. [Google Scholar] [CrossRef]
- Fitzgibbons, P.G.; DiGiovanni, C.; Hares, S.; Akelman, E. Safe Tourniquet Use: A Review of the Evidence. J. Am. Acad. Orthop. Surg. 2012, 20, 310–319. [Google Scholar] [CrossRef]
- Papalia, R.; Zampogna, B.; Franceschi, F.; Torre, G.; Maffulli, N.; Denaro, V. Tourniquet in knee surgery. Br. Med. Bull. 2014, 111, 63–76. [Google Scholar] [CrossRef]
- Kornbluth, I.D.; Freedman, M.K.; Sher, L.; Frederick, R.W. Femoral, saphenous nerve palsy after tourniquet use: A case report11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the author(s) or upon any organization with which the author(s) is/are associated. Arch. Phys. Med. Rehabil. 2003, 84, 909–911. [Google Scholar] [CrossRef] [PubMed]
- Mingo-Robinet, J.; Castañeda-Cabrero, C.; Alvarez, V.; Alonso-Cortés, J.M.L.; Monge-Casares, E. Tourniquet-Related Iatrogenic Femoral Nerve Palsy after Knee Surgery: Case Report and Review of the Literature. Case Rep. Orthop. 2013, 2013, 368290. [Google Scholar] [CrossRef] [PubMed]
- Kuo, L.-T.; Yu, P.-A.; Chen, C.-L.; Hsu, W.-H.; Chi, C.-C. Tourniquet use in arthroscopic anterior cruciate ligament reconstruction: A systematic review and meta-analysis of randomised controlled trials. BMC Musculoskelet. Disord. 2017, 18, 358. [Google Scholar] [CrossRef]
- Geddes, R.D.T. Skin protection beneath the tourniquet a prospective randomized trial. ANZ J. Surg. 2004, 74, 721–722. [Google Scholar] [CrossRef]
- Kauvar, D.S.; Miller, D.; Walters, T.J. Tourniquet use is not associated with limb loss following military lower extremity arterial trauma. J. Trauma Acute Care Surg. 2018, 85, 495–499. [Google Scholar] [CrossRef]
- Saw, K.M.; Hee, H.I. Tourniquet-induced common peroneal nerve injury in a pediatric patient after knee arthroscopy—Raising the red flag. Clin. Case Rep. 2017, 5, 1438–1440. [Google Scholar] [CrossRef]
- Daniel, D.M.; Lumkong, G.; Stone, M.L.; Pedowitz, R.A. Effects of tourniquet use in anterior cruciate ligament reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 1995, 11, 307–311. [Google Scholar] [CrossRef]
- Yoshiya, H.N.S. The effect of tourniquet use on operative performance and early postoperative results of anatomic double-bundle anterior cruciate ligament reconstruction. J. Orthop. Sci. 2013, 18, 586–591. [Google Scholar] [CrossRef]
- Murphy, C.G.; Winter, D.C.; Bouchier-Hayes, D.J. Tourniquet injuries: Pathogenesis and modalities for attenuation. Acta Orthop. Belg. 2005, 71, 635–645. [Google Scholar]
- Gardner, V.O.; Caiozzo, V.J.; Long, S.T.; Stoffel, J.; McMaster, W.C.; Prietto, C.A. Contractile properties of slow and fast muscle following tourniquet ischemia. Am. J. Sports Med. 1984, 12, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Clark, B.M.; Pagani-Estevez, G.L.; Johnson, R.L. Lidocaine Patch to Treat Postoperative Tourniquet Pain After Total Knee Replacement: A Case Report. A&A Pract. 2018, 11, 173–174. [Google Scholar] [CrossRef]
- Choudhary, A.; Kanodia, N.; Agrawal, S.; Bhasin, V.B.; Singh, A. Tourniquet Use in Arthroscopic ACL Reconstruction: A Blinded Randomized Trial. Indian J. Orthop. 2021, 55, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Shimozaki, K.; Nakase, J.; Yoshimizu, R.; Kanayama, T.; Yanatori, Y.; Sengoku, T.; Tsuchiya, H. Non-use of intra-articular drain after anterior cruciate ligament reconstruction does not affect postoperative knee pain and muscle strength on early period. Asia-Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2023, 32, 7–11. [Google Scholar] [CrossRef]
- Shamim, S.; Kushwaha, S.S.; Shantanu, K.; Maurya, G.; Arshad, I. Assessment of an Intra-Articular Drain in Arthroscopy-Assisted Anterior Cruciate Ligament Reconstruction. Cureus 2021, 13, e16928. [Google Scholar] [CrossRef]
- Dhawan, A.; Doukas, W.C.; Papazis, J.A.; Scoville, C.R. Effect of Drain Use in the Early Postoperative Period after Arthroscopically Assisted Anterior Cruciate Ligament Reconstruction with Bone-Patellar Tendon-Bone Graft. Am. J. Sports Med. 2003, 31, 419–424. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, L.; Wang, J.; Li, Z.; Shi, Z. Do patients benefit from tourniquet in arthroscopic surgeries of the knee? Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1125–1130. [Google Scholar] [CrossRef]
- Samei, M.; Daliri, M.; Sadeghi, M.; Ganji, R.; Parsa, A.; Ebrahimzadeh, M.H. Arthroscopic anterior cruciate ligament reconstruction with and without tourniquet use: An updated systematic review and meta-analysis on clinical outcomes. BMC Musculoskelet. Disord. 2024, 25, 994. [Google Scholar] [CrossRef]
- Abdel-Salam, A.; Eyres, K.S. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J. Bone Joint Surg. Br. 1995, 77, 250–253. [Google Scholar] [CrossRef]
- Hoogeslag, R.A.G.; Brouwer, R.W.; Van Raay, J.J.A.M. The Value of Tourniquet Use for Visibility During Arthroscopy of the Knee: A Double-Blind, Randomized Controlled Trial. Arthrosc. J. Arthrosc. Relat. Surg. 2010, 26, S67–S72. [Google Scholar] [CrossRef]
- Zaid, H.H.G.; Hua, X.; Chen, B.; Yang, Q.; Yang, G.; Cheng, W. Tourniquet Use Improves Intraoperative Parameters, Leading to Similar Postoperative Outcomes Compared with No Tourniquet Use in Anterior Cruciate Ligament Reconstruction: A Prospective, Double-Blind, Randomized Clinical Trial. Arthrosc. J. Arthrosc. Relat. Surg. 2023, 39, 626–637.e3. [Google Scholar] [CrossRef]
- Nicholas, S.J.; Tyler, T.F.; McHugh, M.P.; Gleim, G.W. The effect on leg strength of tourniquet use during anterior cruciate ligament reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 2001, 17, 603–607. [Google Scholar] [CrossRef]
- Su, L.; Yan, L.; Guo, H.; Lan, Q. Is Tourniquet Use Necessary for Arthroscopic Meniscal Repair. 2023, preprint. [CrossRef]
- Akan, K. Suction drainage influence on knee effusion following partial meniscectomy with partial fat pad or synovium resection. Acta Orthop. Traumatol. Turc. 2011, 45, 221–224. [Google Scholar] [CrossRef]
- McCormack, R.G.; Greenhow, R.J.; Fogagnolo, F.; Shrier, I. Intra-articular Drain Versus No Drain After Arthroscopic Anterior Cruciate Ligament Reconstruction: A Randomized, Prospective Clinical Trial. Arthrosc. J. Arthrosc. Relat. Surg. 2006, 22, 889–893. [Google Scholar] [CrossRef]
- Khalifa, T.; Mahozi, A.; Dhaif, B. Intra-articular drain versus no drain after arthroscopic anterior cruciate ligament reconstruction: A randomized prospective clinical trial. Bahrain Med. Bull. 2008, 30, 9–11. [Google Scholar]
| N | Mean Age (Range) | Hamstrings | BPTB | QT | Knee Hematoma | Infection | |
|---|---|---|---|---|---|---|---|
| Male | 334 | 34.7 (18–53) | 282 | 40 | 12 | 2 | 2 |
| Female | 122 | 32.3 (18–47) | 107 | 10 | 5 | 1 | |
| Total | 456 | 389 | 50 | 17 | 3 | 2 |
| Type of Complication | N | Mean Age (Ages) | Male | Female | Hamstrings |
|---|---|---|---|---|---|
| Knee Hematoma | 3 | 28 (24, 29, 31) | 2 | 1 | 3 |
| Infection | 2 | 48 (46, 50) | 2 | - | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flevas, D.A.; Sarantis, M.; Tsakotos, G.; Sasalos, G.G.; Tokis, A.V. Arthroscopic Anterior Cuciate Ligament Reconstruction Using Neither a Tourniquet nor Drainage: A Perioperative Case Series Report. Life 2025, 15, 619. https://doi.org/10.3390/life15040619
Flevas DA, Sarantis M, Tsakotos G, Sasalos GG, Tokis AV. Arthroscopic Anterior Cuciate Ligament Reconstruction Using Neither a Tourniquet nor Drainage: A Perioperative Case Series Report. Life. 2025; 15(4):619. https://doi.org/10.3390/life15040619
Chicago/Turabian StyleFlevas, Dimitrios A., Michail Sarantis, Georgios Tsakotos, Grigorios G. Sasalos, and Anastasios V. Tokis. 2025. "Arthroscopic Anterior Cuciate Ligament Reconstruction Using Neither a Tourniquet nor Drainage: A Perioperative Case Series Report" Life 15, no. 4: 619. https://doi.org/10.3390/life15040619
APA StyleFlevas, D. A., Sarantis, M., Tsakotos, G., Sasalos, G. G., & Tokis, A. V. (2025). Arthroscopic Anterior Cuciate Ligament Reconstruction Using Neither a Tourniquet nor Drainage: A Perioperative Case Series Report. Life, 15(4), 619. https://doi.org/10.3390/life15040619






