Paediatric Hospitalised Immune Thrombocytopenia in Real-Life Recent Viral Infection Outbreaks: A Retrospective Study
Abstract
1. Introduction
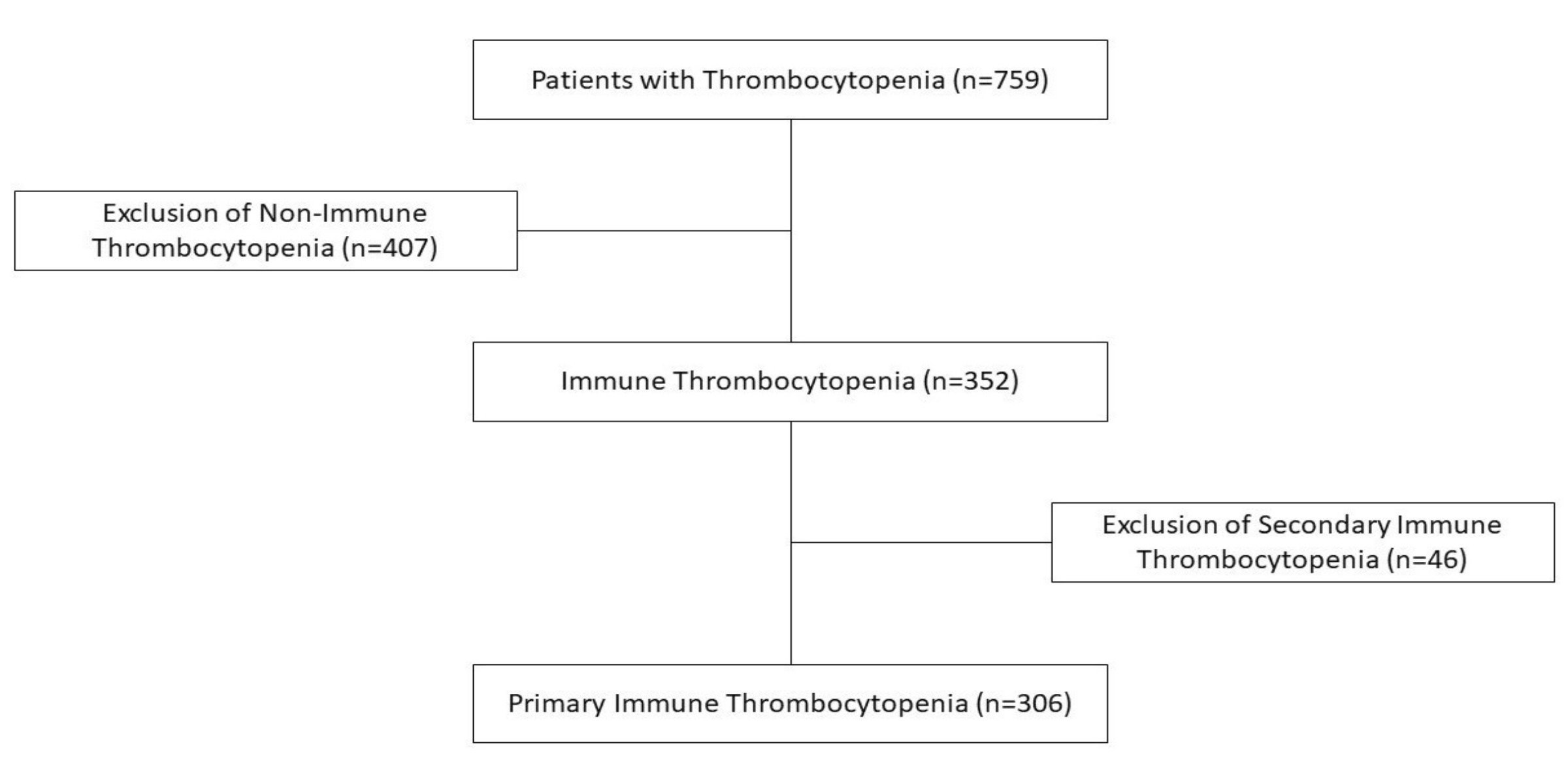
2. Patients and Methods
- Study population and setting
- b.
- Study periods and cohort definition
- -
- Cohort I of patients (306) admitted during 5 years between 2020 and 2024 (the period from 2020 to 2022 marked by officially declared SARS-CoV-2 pandemics, followed by 2023–2024 when influenza A/B endemics were declared in the country, alongside outbreaks of measles, varicella, and EBV infections).
- -
- Cohort II of patients (213) is a control group focused on the 5 years pre-COVID-19 pandemic period from 2015 to 2019, free of declared viral outbreaks.
- c.
- Inclusion and exclusion criteria
- -
- Patients ≤18 years of age, not vaccinated against SARS-CoV-2;
- -
- Newly diagnosed thrombocytopenia ≤100,000/mm3 measured on two occasions within 48 h; and,
- -
- Without clinical and biological signs suggesting a possible non-ITP type of thrombocytopenia.
- d.
- Diagnostic and laboratory investigations
- e.
- Outcome measures
- f.
- Statistical analysis
- g.
- Ethical approval
3. Results
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grace, R.F.; Lambert, M.P. An update on pediatric ITP: Differentiating primary ITP, IPD, and PID. Blood 2022, 140, 542–555. [Google Scholar] [CrossRef]
- Gafter-Gvili, A. Current approaches for the diagnosis and management of immune thrombocytopenia. Eur. J. Intern. Med. 2023, 108, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Mititelu, A.; Onisâi, M.C.; Roșca, A.; Vlădăreanu, A.M. Current Understanding of Immune Thrombocytopenia: A Review of Pathogenesis and Treatment Options. Int. J. Mol. Sciences. 2024, 25, 2163. [Google Scholar] [CrossRef]
- Pietras, N.M.; Gupta, N.; Justiz Vaillant, A.A.; Pearson-Shaver, A.L. Immune Thrombocytopenia. 5 May 2024. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Rubens, J.H.; Akindele, N.P.; Tschudy, M.M.; Sick-Samuels, A.C. Acute Covid-19 and Multisystem Inflammatory Syndrome in Children. BMJ 2021, 372, n385. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yang, Q.; Wang, Y.; Wu, Y.; Xu, J.; Yu, Y.; Shang, Y. Thrombocytopenia and its association with mortality in patients with COVID-19. J. Thromb. Haemost. 2020, 18, 1469–1472. [Google Scholar] [CrossRef]
- Cines, D.B.; Bussel, J.B.; Liebman, H.A.; Luning Prak, E.T. The ITP syndrome: Pathogenic and clinical diversity. Blood 2009, 113, 6511–6521. [Google Scholar] [CrossRef]
- Raadsen, M.; Du Toit, J.; Langerak, T.; van Bussel, B.; van Gorp, E.; Goeijenbier, M. Thrombocytopenia in Virus Infections. J. Clin. Med. 2021, 10, 877. [Google Scholar] [CrossRef]
- Schrottmaier, W.C.; Schmuckenschlager, A.; Pirabe, A.; Assinger, A. Platelets in Viral Infections—Brave Soldiers or Trojan Horses. Front. Immunol. 2022, 13, 856713. [Google Scholar] [CrossRef] [PubMed]
- Assinger, A. Platelets and Infection: An Emerging Role of Platelets in Viral Infection. Front. Immunol. 2014, 5, 649. [Google Scholar] [CrossRef]
- Swinkels, M.; Rijkers, M.; Voorberg, J.; Vidarsson, G.; Leebeek, F.W.G.; Jansen, A.J.G. Emerging Concepts in Immune Thrombocytopenia. Front. Immunol. 2018, 9, 880. [Google Scholar] [CrossRef]
- Marinescu, A.R.; Lazureanu, V.E.; Musta, V.F.; Nicolescu, N.D.; Mocanu, A.; Cut, T.G.; Muresan, C.O.; Tudoran, C.; Licker, M.; Laza, R. Severe Thrombocytopenic Purpura Associated with COVID-19 in a Pediatric Patient. Infect. Drug Resist. 2022, 15, 3405–3415. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://diagnostics.roche.com/global/en/products/instruments/cobas-e-411-ins-502.html (accessed on 6 August 2025).
- Choi, Y.B.; Jung, H.J.; Kim, H.-R.; Jeong, S.I. Changes in the Incidence of Immune Thrombocytopenia in the Coronavirus Disease 2019 Era: A Nationwide Observational Study in Korea. Risk Manag. Healthc. Policy 2023, 16, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Lemos, J.; Poças, J.F.; Castro, I.; Ferreira Mota, L.; Correia de Oliveira, A. Immune Thrombocytopenia Purpura Associated with COVID-19 Infection: A Challenging Diagnosis and Management. Cureus 2023, 15, e47433. [Google Scholar] [CrossRef]
- Zong, X.; Gu, Y.; Yu, H.; Li, Z.; Wang, Y. Thrombocytopenia Is Associated with COVID-19 Severity and Outcome: An Updated Meta-Analysis of 5637 Patients with Multiple Outcomes. Lab. Med. 2021, 52, 10–15. [Google Scholar] [CrossRef]
- Nagori, E.K.; Ghantarchyan, H.; Qadir, A.; Arabian, S. COVID-19-Induced Thrombocytopenia: A Brief Literature Review and Case Report. Cureus 2022, 14, e30993. [Google Scholar] [CrossRef]
- Nguyen, H.; Nguyen, M.; Olenik, A.; Nguyen, H.; Nguyen, M.; Olenik, A. Immune Thrombocytopenic Purpura Following COVID-19 Infection: A Case Report and Literature Review. Cureus 2023, 15, e39342. [Google Scholar] [CrossRef]
- Ceglie, G.; De Ioris, M.A.; Mercadante, S.; Olivini, N.; Del Bufalo, F.; Marchesani, S.; Cocca, F.; Monteferrario, E.; Boccieri, E.; Pianese, J.; et al. Immune Thrombocytopenia in a Child with COVID-19: Is It the Calm after the (Cytokine) Storm? Pediatr. Blood Cancer 2021, 69, e29326. [Google Scholar] [CrossRef] [PubMed]
- Hashemieh, M.; Tabatabaee, S.; Radfar, M.; Fahim, P. COVID-19 Associated Thrombocytopenia in Children: An Emerging Issue. Int. J. Pediatr. 2021, 9, 13635–13642. [Google Scholar] [CrossRef]
- Mettananda, C.; Williams, S. Persistent, Poorly Responsive Immune Thrombocytopenia Secondary to Asymptomatic COVID-19 Infection in a Child. Case Rep. Infect. Dis. 2023, 2023, 3298520. [Google Scholar] [CrossRef] [PubMed]
- Shinno, K.; Banno, Y.; Kamimaki, I. Severe Immune Thrombocytopenia That Developed Immediately after COVID-19 in a School-Aged Patient: A Case Report. Front. Pediatr. 2023, 11, 1120093. [Google Scholar] [CrossRef] [PubMed]
- Zairi, M.; Maritsi, D.; Tsolia, M.; Kossiva, L. Immune Thrombocytopenia in a Toddler Testing Positive for SARS-CoV-2 Antibodies. Authorea Preprints 2024. [Google Scholar] [CrossRef]
- Alam, M.M. Idiopathic Thrombocytopenic Purpura in Children: A 10 Years Experience at Tertiary Care Hospital. J. Pak. Med. Assoc. 2014, 64, 1358–1362. [Google Scholar]
- Shim, Y.J.; Kim, U.H.; Suh, J.K.; Lee, K.S. Natural Course of Childhood Chronic Immune Thrombocytopenia Using the Revised Terminology and Definitions of the International Working Group: A Single Center Experience. Blood Res. 2014, 49, 187–191. [Google Scholar] [CrossRef]
- Heitink-Pollé, K.M.J.; Nijsten, J.; Boonacker, C.W.B.; de Haas, M.; Bruin, M.C.A. Clinical and Laboratory Predictors of Chronic Immune Thrombocytopenia in Children: A Systematic Review and Meta-Analysis. Blood 2014, 124, 3295–3307. [Google Scholar] [CrossRef]
- Chen, W.; Li, Z.; Yang, B.; Wang, P.; Zhou, Q.; Zhang, Z.; Zhu, J.; Chen, X.; Yang, P.; Zhou, H. Delayed-phase thrombocytopenia in patients with coronavirus disease 2019 (COVID-19). Br. J. Haematol. 2020, 190, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Williams, Z. The ‘quad-demic’ is here—And with it I have become a disease detective. The Guardian, 17 December 2024. [Google Scholar]
- Bhattacharjee, S.; Banerjee, M. Immune Thrombocytopenia Secondary to COVID-19: A Systematic Review. SN Compr. Clin. Med. 2020, 2, 2048–2058. [Google Scholar] [CrossRef] [PubMed]
- Małecki, P.; Grosicki, S. Diagnosis and Treatment of Immune Thrombocytopenia in Poland. Hematologia 2022, 13, 49–54. [Google Scholar] [CrossRef]
- Rasizadeh, R.; Ebrahimi, F.; Zamani Kermanshahi, A.; Sorkhabi, A.D.; Sarkesh, A.; Nahand, J.S.; Baghi, H.B. Viruses and Thrombocytopenia. Heliyon 2024, 10, e27844. [Google Scholar] [CrossRef]
- Hassan, H.; Ahmed, Y.; Nasser, Y.; Aboghabsha, M. Prevalence of Thrombocytopenia in COVID-19 Isolated Patients. Int. J. Med Arts 2023, 4, 2885–2890. [Google Scholar] [CrossRef]
- Kuhne, T.; Berchtold, W.; Michaels, L.A.; Wu, R.; Donato, H.; Espina, B.; Tamary, H.; Rodeghiero, F.; Chitlur, M.; Rischewski, J.; et al. Newly Diagnosed Immune Thrombocytopenia in Children and Adults: A Comparative Prospective Observational Registry of the Intercontinental Cooperative Immune Thrombocytopenia Study Group. Haematologica 2011, 96, 1831–1837. [Google Scholar] [CrossRef]
- Schifferli, A.; Holbro, A.; Chitlur, M.; Coslovsky, M.; Imbach, P.; Donato, H.; Elalfy, M.S.; Graciela, E.; Grainger, J.D.; Holzhauer, S.; et al. A Comparative Prospective Observational Study of Children and Adults with Immune Thrombocytopenia: 2-Year Follow-Up. Am. J. Hematol. 2018, 93, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Jaime-Pérez, J.C.; Ramos-Dávila, E.M.; Meléndez-Flores, J.D.; Gómez-De León, A.; Gómez-Almaguer, D. Insights on Chronic Immune Thrombocytopenia Pathogenesis: A Bench to Bedside Update. Blood Rev. 2021, 49, 100827. [Google Scholar] [CrossRef] [PubMed]
- Alpdoğan, S.; Gülen, H. Assessment of Clinical and Laboratory Predictors for Chronic Childhood Immune Thrombocytopenia. J. Pediatr. Res. 2023, 10, 278–284. [Google Scholar] [CrossRef]
- Jung, J.Y.; O, A.R.; Kim, J.K.; Park, M. Clinical Course and Prognostic Factors of Childhood Immune Thrombocytopenia: Single Center Experience of 10 Years. Korean J. Pediatr. 2016, 59, 335–340. [Google Scholar] [CrossRef]
- Roșu, V.E.; Roșu, S.T.; Ivanov, A.V.; Starcea, I.M.; Streanga, V.; Miron, I.C.; Mocanu, A.; Lupu, A.; Lupu, V.V.; Gavrilovici, C. Predictor Factors for Chronicity in Immune Thrombocytopenic Purpura in Children. Children 2023, 10, 911. [Google Scholar] [CrossRef]
- Ekstrand, C.; Linder, M.; Cherif, H.; Kieler, H.; Bahmanyar, S. Increased Susceptibility to Infections before the Diagnosis of Immune Thrombocytopenia. J. Thromb. Haemost. 2016, 14, 807–814. [Google Scholar] [CrossRef]
- Evangelidis, P.; Tragiannidis, K.; Gavriilaki, E.; Tragiannidis, A. Impact of Thrombopoietin Receptor Agonists on Pathophysiology of Pediatric Immune Thrombocytopenia. Curr. Issues Mol. Biol. 2025, 47, 65. [Google Scholar] [CrossRef] [PubMed]

| Year | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|
| Number of hospitalisations | 17,403 | 17,489 | 17,243 | 17,987 | 19,122 | 89,244 |
| UMRN | 12,373 | 12,240 | 12,064 | 12,482 | 12,924 | 62,083 |
| Plt. no. ˂ 100,000/mm3 | 42 | 55 | 43 | 37 | 36 | 213 |
| Incidence of ITP person’s years/‰ | 3.39 | 4.49 | 3.56 | 2.96 | 2.78 | 3.43 |
| Plt. no. = 50–100,000/mm3 | 23 | 24 | 19 | 16 | 27 | 109 |
| Plt. no. = 20–50,000/mm3 | 7 | 15 | 12 | 15 | 5 | 54 |
| Plt. no. ˂ 20,000/mm3 | 12 | 16 | 12 | 6 | 4 | 50 |
| Year | 2020 | 2021 | 2022 | 2023 | 2024 | Total |
|---|---|---|---|---|---|---|
| Number of hospitalisations | 8607 | 9443 | 13,650 | 17,108 | 19,297 | 68,105 |
| UMRN | 5864 | 6386 | 9253 | 12,338 | 12,596 | 46,437 |
| Plt. no. ˂ 100,000/mm3 | 32 | 46 | 77 | 79 | 72 | 306 |
| Incidence of ITP persons years/‰ | 5.45 | 7.2 | 8.32 | 6.4 | 5.71 | 6.58 |
| Plt. no. = 50–100,000/mm3 | 19 | 33 | 52 | 40 | 50 | 194 |
| Plt. no. = 20–50,000/mm3 | 8 | 5 | 13 | 12 | 5 | 43 |
| Plt. no. ˂ 20,000/mm3 | 5 | 8 | 12 | 27 | 17 | 69 |
| Cohort I | Cohort II | p Value | |
|---|---|---|---|
| Number of hospitalizations | 68,105 | 89,244 | 0.08 |
| UMRN | 46,437 | 62,083 | 0.06 |
| Plt. no. ˂ 100,000/mm3 | 306 | 213 | 0.05 |
| Incidence of ITP person- years (‰) | 6.58 | 3.43 | 0.001 |
| Plt. no. = 50–100,000/mm3 | 194 (63.4%) | 109 (51.17%) | 0.028 |
| Plt. no. = 20–50,000/mm3 | 43 (14.05%) | 54 (25.35%) | 0.43 |
| Plt. no. ˂ 20,000/mm3 | 69 (22.55%) | 50 (23.48%) | 0.41 |
| Age (years) -mean ± SD | 5.33 ± 5.28 | 5.87 ± 5.70 | 0.267 |
| Gender -male (no, %) -female (no, %) | 177 (57.84%) 129 (42.16%) | 109 (51.17%) 104 (48.83%) | |
| Residency -Urban -Rural | 156 (50.98%) 150 (49.02%) | 129 (60.56%) 84 (39.44%) |
| Year | 2020 | 2021 | 2022 | 2023 | 2024 | Total | p Value |
|---|---|---|---|---|---|---|---|
| Plt. no. ˂ 100,000/mm3 | 32 | 46 | 77 | 79 | 72 | 306 | |
| Acute (no./%) | 27 (84.37%) | 39 (84.78%) | 70 (90.90%) | 68 (86.07%) | 66 (91.66%) | 270 (88.23%) | 0.001 |
| Chronic (no./%) | 5 (15.62%) | 5 (10.87%) | 6 (7.8%) | 9 (11.39%) | 4 (5.55%) | 29 (9.48%) | 0.423 |
| Persistent (no./%) | 0 | 2 (4.35%) | 1 (1.29%) | 2 (2.53%) | 2 (2.78%) | 7 (2.28%) | 0.319 |
| Persistent + chronic (no./%) | 5 (15.62%) | 7 (15.22%) | 7 (9.09%) | 11 (13.92%) | 6 (8.33%) | 36 (11.76%) | 0.265 |
| Total | Acute ITP | Chronic ITP | Persistent ITP |
|---|---|---|---|
| no. | 270 | 29 | 7 |
| Age -mean ± SD | 4.91 ± 5.14 | 8.27 ± 5.19 | 9.57 ± 5.94 |
| p-value - age acute vs. chronic ITP - age acute vs. persistent ITP - age chronic vs. persistent ITP | 0.001 0.019 0.568 | ||
| Gender -male -female | 160 110 | 15 14 | 2 5 |
| Residency -urban -rural | 131 139 | 22 7 | 3 4 |
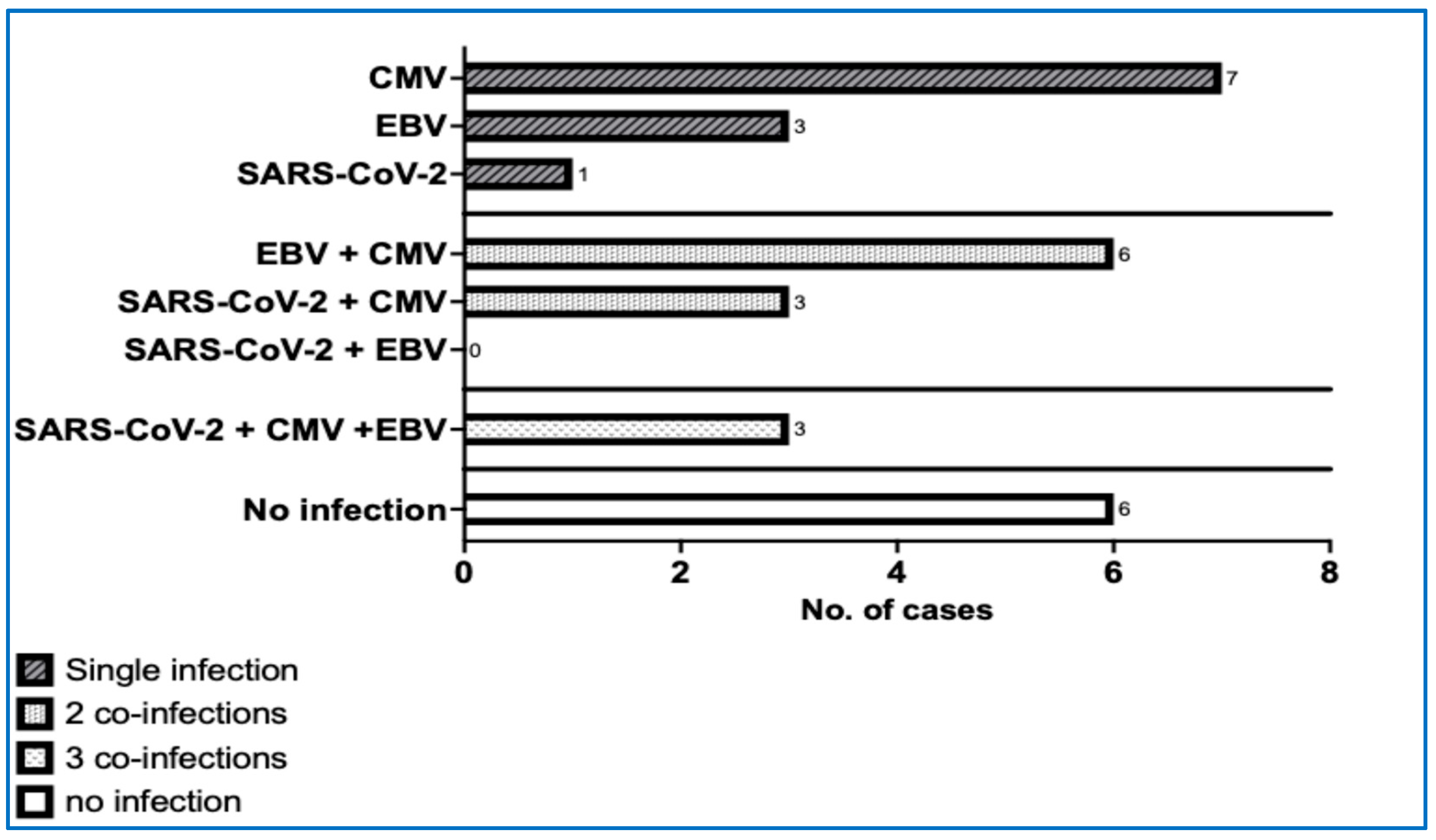
| Type of Virus Infection | Type of Infection | 2020 | 2021 | 2022 | 2023 | 2024 | Total |
|---|---|---|---|---|---|---|---|
| SARS-CoV-2 | Acute | 0 | 3 | 14 | 5 | 6 | 28 |
| Past infection | 0 | 4 | 5 | 23 | 14 | 46 | |
| EBV | Acute | 3 | 7 | 5 | 4 | 4 | 23 |
| Persistent/Chronic | 0 | 0 | 3 | 19 | 3 | 25 | |
| CMV | Acute | 0 | 2 | 1 | 1 | 4 | 8 |
| Past-infection | 14 | 8 | 15 | 30 | 6 | 73 | |
| Influenza | Acute | 0 | 1 | 5 | 6 | 8 | 20 |
| Measles | Acute | 0 | 0 | 0 | 0 | 15 | 15 |
| Varicella | Acute | 1 | 0 | 1 | 2 | 1 | 5 |
| Roseola Infantum | Acute | 1 | 0 | 0 | 1 | 0 | 2 |
| SRV | Acute | 0 | 0 | 0 | 0 | 1 | 1 |
| Rotavirus | Acute | 0 | 2 | 4 | 0 | 2 | 8 |
| Adenovirus | Acute | 0 | 0 | 3 | 0 | 1 | 4 |
| Norovirus | Acute | 0 | 0 | 1 | 2 | 2 | 5 |
| Herpes simplex | Acute | 1 | 0 | 0 | 0 | 1 | 2 |
| HIV | Chronic | 3 | 3 | 3 | 0 | 1 | 10 |
| Hepatitis B Surface Antigen | Chronic | 1 | 0 | 1 | 1 | 0 | 3 |
| Total | 24 | 30 | 61 | 94 | 69 | 278 |
| Total | r | p-Value | ρ | p-Value | |
|---|---|---|---|---|---|
| Platelet no. ˂ 100,000/mm3 | 306 | ||||
| SARS-CoV-2 | 74 | 0.967 | 0.007 | - | - |
| EBV | 48 | - | - | 0.974 | 0.004 |
| CMV | 81 | 0.483 | 0.41 | - | - |
| Influenza | 20 | 0.901 | 0.037 | - | - |
| Varicella | 5 | 0.555 | 0.331 | - | - |
| Measles | 15 | 0.287 | 0.639 | - | - |
| Roseola infantum | 2 | −0.248 | 0.688 | - | - |
| SRV | 1 | 0.287 | 0.639 | - | - |
| Enteroviruses (adeno-, noro- and rotavirus) | 17 | 0.705 | 0.183 | - | - |
| Herpes simplex | 2 | - | - | −0.577 | 0.308 |
| HIV | 10 | - | - | −0.671 | 0.215 |
| HBs antigen | 3 | - | - | 0.288 | 0.637 |
| Total infections | 278 | 0.916 | 0.029 | - | - |
| Year | Number of Acute Infections/Total Number of Patients with Thrombocytopenia | Number of Chronic Infections/Total Number of Patients with Thrombocytopenia | Total Number of Infections/Total Number of Patients with Thrombocytopenia |
|---|---|---|---|
| 2020 | 6/32 | 18/32 | 24/32 |
| 2021 | 15/46 | 15/46 | 30/46 |
| 2022 | 34/77 | 27/77 | 61/77 |
| 2023 | 21/79 | 73/79 | 94/79 |
| 2024 | 45/72 | 24/72 | 69/72 |
| Total | 121/306 | 157/306 | 278/306 |
| r | 0.744 | - | 0.916 |
| p value | 0.150 | - | 0.029 |
| ρ | - | 0.900 | - |
| p value | - | 0.037 | - |
| Type of Treatment | ITP Form | 2020 | 2021 | 2022 | 2023 | 2024 | Total |
|---|---|---|---|---|---|---|---|
| Platelet concentrate | Acute | 0 | 0 | 1 | 1 | 1 | 3 |
| Chronic | 0 | 0 | 0 | 0 | 0 | 0 | |
| Steroids | Acute | 5 | 1 | 6 | 13 | 7 | 32 |
| Persistent | 0 | 0 | 1 | 1 | 0 | 2 | |
| Chronic | 0 | 0 | 1 | 2 | 1 | 4 | |
| Intravenous human immunoglobulin | Acute | 0 | 2 | 2 | 5 | 2 | 11 |
| Chronic | 0 | 0 | 0 | 0 | 0 | 0 | |
| Intravenous human immunoglobulin + steroids | Acute | 1 | 0 | 1 | 3 | 0 | 5 |
| Chronic | 0 | 0 | 0 | 0 | 0 | 0 | |
| TPO-RAs | Acute | 0 | 0 | 0 | 0 | 0 | 0 |
| Persistent | 0 | 0 | 0 | 0 | 1 | 1 | |
| Chronic | 3 | 2 | 3 | 4 | 3 | 15 | |
| Total | 9 | 5 | 15 | 29 | 15 | 73 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ursu, C.E.; Șerban, M.; Jinca, C.M.; Boeriu, E.; Ionita, I.; Coriu, D.; Brînză, M.; Tomuleasa, C.; Arghirescu, T.S. Paediatric Hospitalised Immune Thrombocytopenia in Real-Life Recent Viral Infection Outbreaks: A Retrospective Study. Life 2025, 15, 1736. https://doi.org/10.3390/life15111736
Ursu CE, Șerban M, Jinca CM, Boeriu E, Ionita I, Coriu D, Brînză M, Tomuleasa C, Arghirescu TS. Paediatric Hospitalised Immune Thrombocytopenia in Real-Life Recent Viral Infection Outbreaks: A Retrospective Study. Life. 2025; 15(11):1736. https://doi.org/10.3390/life15111736
Chicago/Turabian StyleUrsu, Cristina Emilia, Margit Șerban, Cristian Marius Jinca, Estera Boeriu, Ioana Ionita, Daniel Coriu, Melen Brînză, Ciprian Tomuleasa, and Teodora Smaranda Arghirescu. 2025. "Paediatric Hospitalised Immune Thrombocytopenia in Real-Life Recent Viral Infection Outbreaks: A Retrospective Study" Life 15, no. 11: 1736. https://doi.org/10.3390/life15111736
APA StyleUrsu, C. E., Șerban, M., Jinca, C. M., Boeriu, E., Ionita, I., Coriu, D., Brînză, M., Tomuleasa, C., & Arghirescu, T. S. (2025). Paediatric Hospitalised Immune Thrombocytopenia in Real-Life Recent Viral Infection Outbreaks: A Retrospective Study. Life, 15(11), 1736. https://doi.org/10.3390/life15111736






