Cement-Augmented Screw Fixation for Unreconstructible Acetabular Posterior Wall Fractures: A Technical Note
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Information
2.2. Preoperative Assessment
2.3. Surgical Technique: Step-by-Step Description
- Positioning and Approach: The patient was placed in the lateral decubitus position. A standard Kocher–Langenbeck posterolateral approach was utilized, with careful identification and protection of the sciatic nerve throughout the procedure.
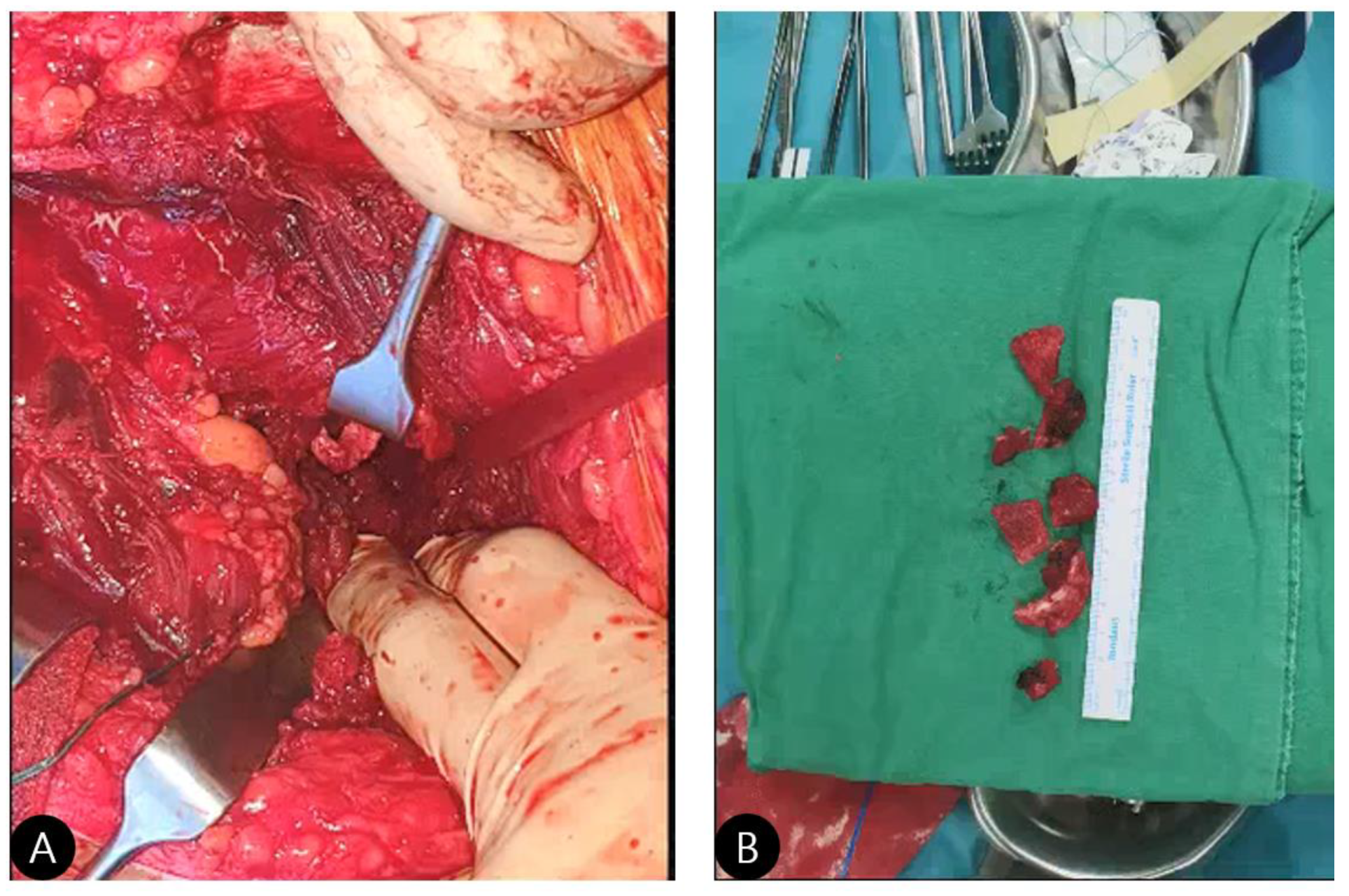
- Exposure and Assessment: The hip joint was exposed. The femoral head was found to be dislocated posteriorly. The posterior wall was severely comminuted into six small, non-viable osteochondral fragments (Figure 3), confirming the impossibility of anatomical reduction and stable fragment fixation.
- Debridement: All irreparable, devitalized fracture fragments were meticulously debrided to create a clean, bleeding bone bed for cement interdigitation.
- Framework Construction (The “Raft”): Three 3.5 mm cortical screws were inserted from the stable posterior column (ilium) into the remaining stable bone bed of the posterior wall. The key technical point here is that these screws are not placed for interfragmentary compression but to create a stable metallic framework or “raft” [8]. This scaffold provides a mechanical anchor and prevents the cement mantle from displacing under load.
- Cement Augmentation (The Critical Step):
- Material: Standard surgical-grade PMMA bone cement was used.
- Timing: The cement was applied in its late doughy phase to minimize the risk of intravasation and allow for manual contouring.
- Application: The cement was carefully applied over and around the screw heads, meticulously sculpted to recreate the native acetabular curvature and provide a congruent socket for the reduced femoral head.
- Precision: Meticulous care was taken to ensure no cement extended beyond the reconstructed margin into the joint space.
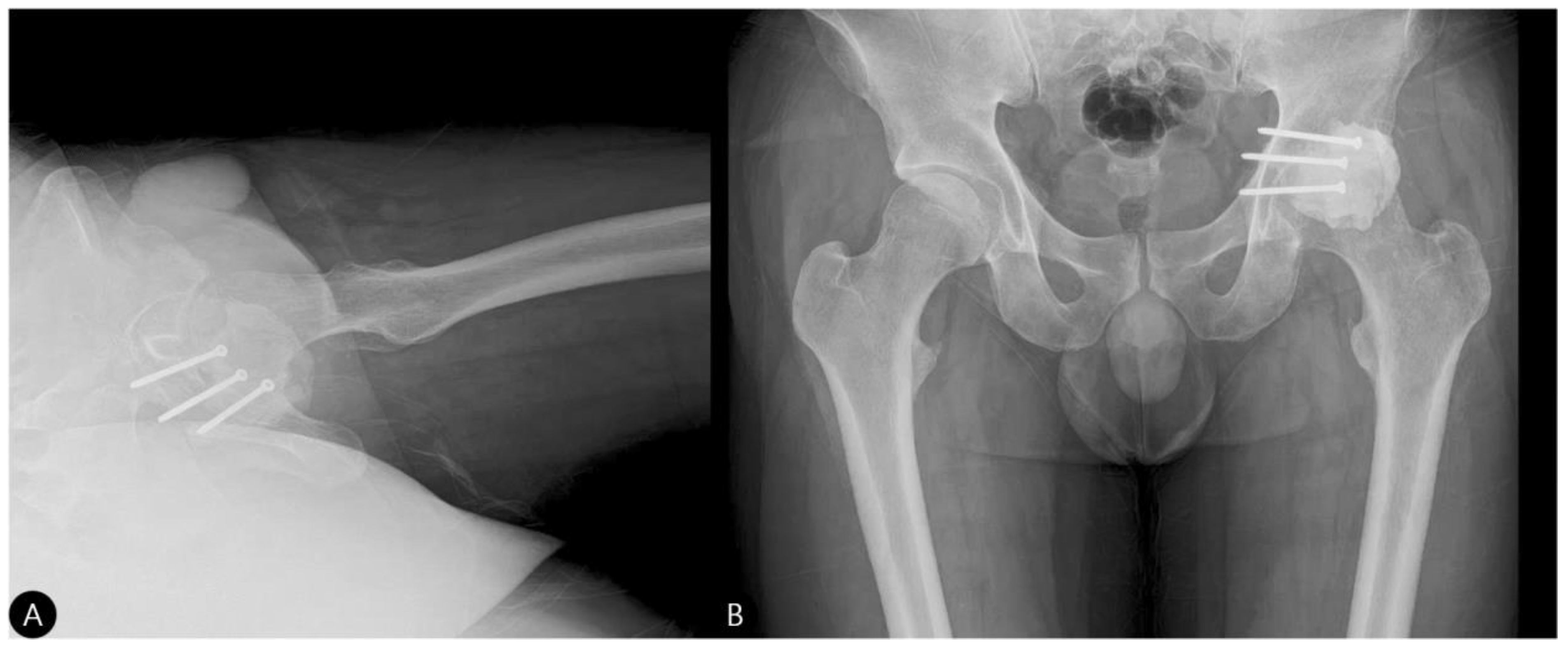
- Reduction and Final Assessment: The hip was reduced under direct vision. Intraoperative fluoroscopy confirmed a concentric reduction, correct implant placement, and the absence of cement fragments in the joint. The stability of the construct was tested through a range of motion. Postoperative imaging confirmed the anatomical reduction and the accurate contouring of the cement construct (Figure 4 and Figure 5).
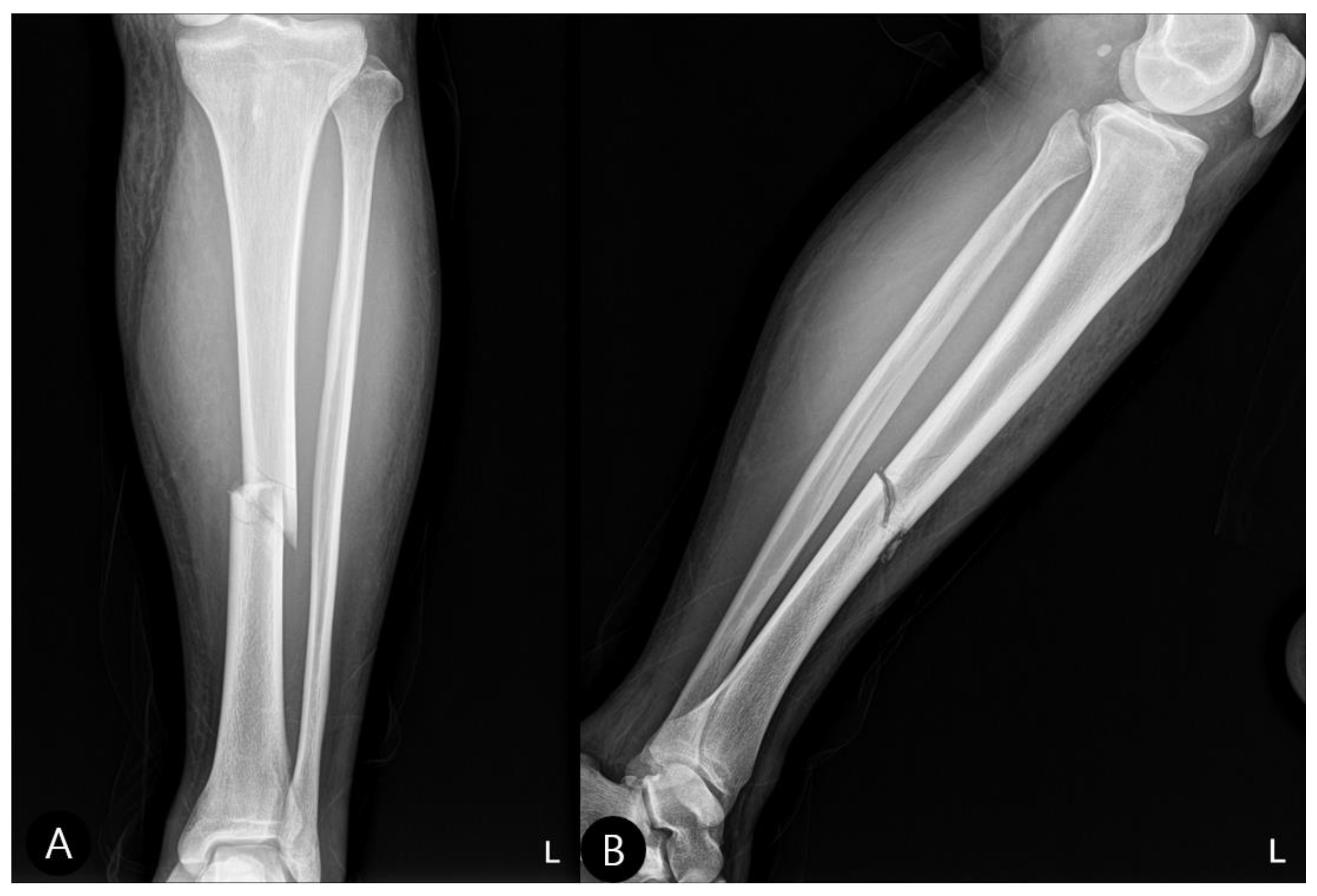
- Concomitant Injury Management:The tibial shaft fracture was subsequently stabilized with an antegrade intramedullary nail (Figure 6).
- Closure: The wound was closed in layers over a drain.
2.4. Fragment Boundary, Cement Volume, and Screw Angle Determination
2.5. Complication Prevention Strategies
3. Results
3.1. Intraoperative Results
3.2. Postoperative Course and Rehabilitation
3.3. Follow-Up Outcomes
- 3 Months: Radiographs showed a stable hip construct with no signs of subluxation or screw migration (Figure 7). The patient had returned to activities of daily living without major discomfort. The mHHS was 78/100.
- 15 Months: A CT scan showed a stable joint, concentric reduction, and no signs of screw loosening or osteolysis (Figure 8). The patient reported no functional limitations. The mHHS was 82/100.
- 21 Months: AP pelvic radiographs showed excellent maintenance of joint space and a stable construct without loosening (Figure 9). The patient’s functional outcome was excellent, reporting no pain during daily activities, with only mild discomfort during deep squatting. The mHHS was 85/100.
- No radiographic evidence of cement loosening, screw migration, or secondary osteoarthritic change was observed at any follow-up interval.
- The mHHS excludes cross-legged sitting ability, making it more appropriate for functional assessment in cases where this specific activity may be limited. All other activities of daily living were performed without difficulty throughout the follow-up period.
4. Discussion
4.1. Novel Aspects of Our Technique
- Strict Indications is Crucial: This is strictly a salvage procedure for unreconstructible fractures confined to the non-weight-bearing portion of the posterior wall. It is contraindicated for weight-bearing dome fractures or when viable fragments can be fixed.
- Stable Framework: The primary role of the screws is not interfragmentary compression but to create a stable mechanical anchor for the cement mantle [8].
- Early Mobilization: The immediate stability afforded by the cement permits early weight-bearing [11], which is crucial for functional recovery and preventing stiffness.
4.2. Long-Term Cement Management Strategy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Melton, L. Epidemiology of hip fractures: Implications of the exponential increase with age. Bone 1996, 18, S121–S125. [Google Scholar] [CrossRef] [PubMed]
- Anglen, J.O.; Burd, T.A.; Hendricks, K.J.; Harrison, P. The “Gull Sign”: A harbinger of failure for internal fixation of geriatric acetabular fractures. J. Orthop. Trauma 2003, 17, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Letournel, E.; Judet, R. Fractures of the Acetabulum; Springer: Berlin, Germany, 1993. [Google Scholar]
- Matta, J.M. Fractures of the acetabulum: Accuracy of reduction and clinical results in patients managed operatively within three weeks after injury. J. Bone Jt. Surg. Am. 1996, 78, 1632–1645. [Google Scholar] [CrossRef]
- Sermon, A.; Broos, P.; Vanderschot, P. Total hip replacement for acetabular fractures. Results in 121 patients operated between 1983 and 2003. Injury 2008, 39, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Mears, D.C.; Velyvis, J.H. Primary total hip arthroplasty after acetabular fracture. J. Bone Jt. Surg. Am. Vol. 2000, 82, 1328–1353. [Google Scholar] [CrossRef]
- Moed, B.R.; Carr, S.E.; Watson, J.T. Results of operative treatment of fractures of the posterior wall of the acetabulum. J. Bone Jt. Surg. Am. 2002, 84, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Giordano, V.; Pires, R.E.; Kojima, K.E.; Fischer, S.T.; Giannoudis, P.V. Subchondral Rafting Plate for the Treatment of Fragmented Articular Central Depression Tibial Plateau Fracture Patterns: Case Series and Technical Illustra-tion. Cureus 2021, 13, e12740. [Google Scholar] [CrossRef] [PubMed]
- Szoradi, G.T.; Feier, A.M.; Zuh, S.G.; Russu, O.M.; Pop, T.S. Polymethyl Methacrylate Bone Cement Polymerization Induced Thermal Necrosis at the Cement–Bone Interface: A Narrative Review. Appl. Sci. 2024, 14, 11651. [Google Scholar] [CrossRef]
- Kazemi, S.M.; Mirahmadi, A.; Hosseini-Monfared, P.; Moghimi, H.R.; Mahboubi, A.; Gandomkarzaneh, M.; Salmannezhad, A.; Farrokhi, M. Impact of saline irrigation on the early mechanical characteristics and microstructure of bone cement. Sci. Rep. 2024, 14, 31299. [Google Scholar] [CrossRef] [PubMed]
- Giannoudis, P.V.; Kontakis, G.; Christoforakis, Z.; Akula, M.; Tosounidis, T.; Koutras, C. Management, complica-tions and clinical results of femoral head fractures. Injury 2009, 40, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Ramadanov, N.; Voss, M.; Hable, R.; Prill, R.; Salzmann, M.; Becker, R. Comparative evaluation and ranking of anterior surgical approaches for acetabular fractures: A systematic review and network meta-analysis. Injury 2025, 56, 112241. [Google Scholar] [CrossRef] [PubMed]
- Calori, G.M.; Mazza, E.; Colombo, M.; Ripamonti, C. The use of bone-graft substitutes in large bone defects: Any specific needs? Injury 2011, 42, S56–S63. [Google Scholar] [CrossRef] [PubMed]
- Bellabarba, C.; Berger, R.A.; Bentley, C.D.; Quigley, L.R.; Jacobs, J.J.; Rosenberg, A.G.; Sheinkop, M.B.; Galante, J.O. Cementless acetabular reconstruction after acetabular fracture. J. Bone Jt. Surgery. Am. Vol. 2001, 83, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Tannast, M.; Najibi, S.; Matta, J.M. Two- to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J. Bone Jt. Surg. Am. 2012, 94, 1559–1567. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S. Cement Augmentation in Fracture Treatment. Scand. J. Surg. 2006, 95, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Radev, B.R.; Kase, J.A.; Askew, M.J.; Weiner, S.D. Potential for thermal damage to articular cartilage by PMMA reconstruction of a bone cavity following tumor excision: A finite element study. J. Biomech. 2009, 42, 1120–1126. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, J.; Lee, H.w.; Yoon, Y.; Lam, K.H.S. Cement-Augmented Screw Fixation for Unreconstructible Acetabular Posterior Wall Fractures: A Technical Note. Life 2025, 15, 1573. https://doi.org/10.3390/life15101573
Hwang J, Lee Hw, Yoon Y, Lam KHS. Cement-Augmented Screw Fixation for Unreconstructible Acetabular Posterior Wall Fractures: A Technical Note. Life. 2025; 15(10):1573. https://doi.org/10.3390/life15101573
Chicago/Turabian StyleHwang, Jihyo, Ho won Lee, Yonghyun Yoon, and King Hei Stanley Lam. 2025. "Cement-Augmented Screw Fixation for Unreconstructible Acetabular Posterior Wall Fractures: A Technical Note" Life 15, no. 10: 1573. https://doi.org/10.3390/life15101573
APA StyleHwang, J., Lee, H. w., Yoon, Y., & Lam, K. H. S. (2025). Cement-Augmented Screw Fixation for Unreconstructible Acetabular Posterior Wall Fractures: A Technical Note. Life, 15(10), 1573. https://doi.org/10.3390/life15101573







