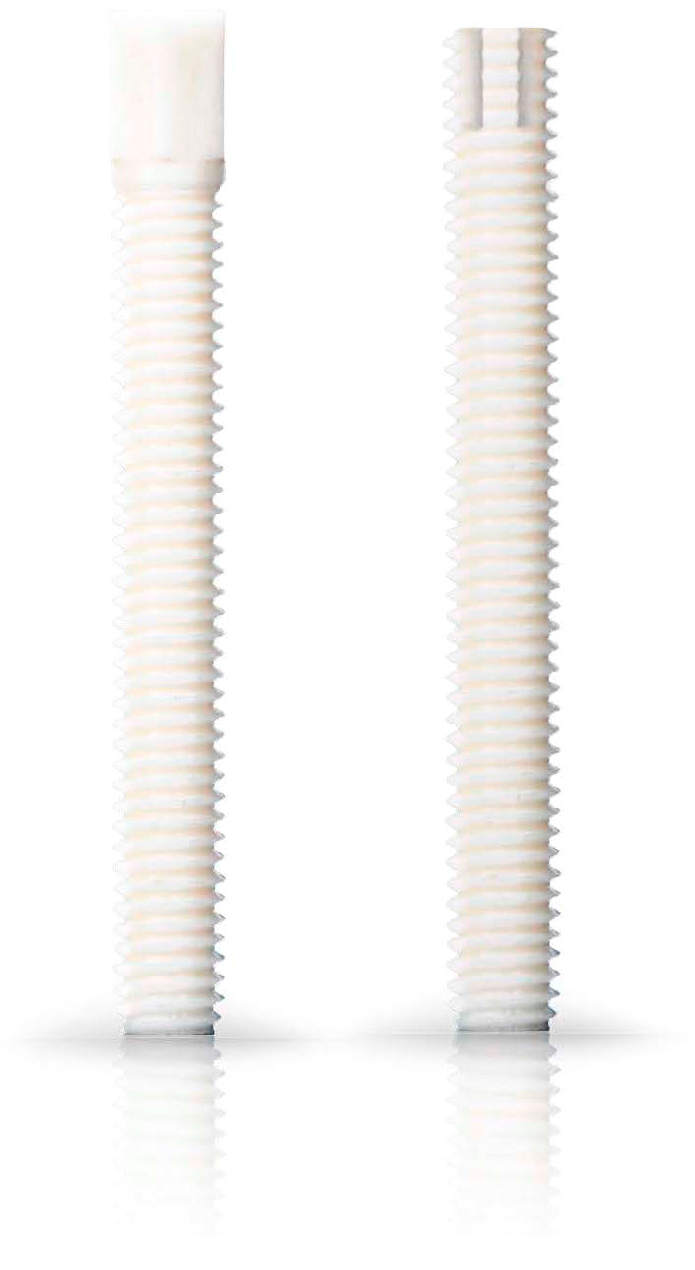
Non-Union Treatment in the Shoulder, Arm, Wrist, and Fingers: A Multicentre Retrospective Study Comparing Conventional Treatment with the Human Allogeneic Cortical Bone Screw (Shark Screw®)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Surgical Procedures
2.5. Complications
2.6. Statistics
3. Results
3.1. Patient Demographics and Clinical Characteristics
3.2. Clinical Outcomes
3.3. Complications
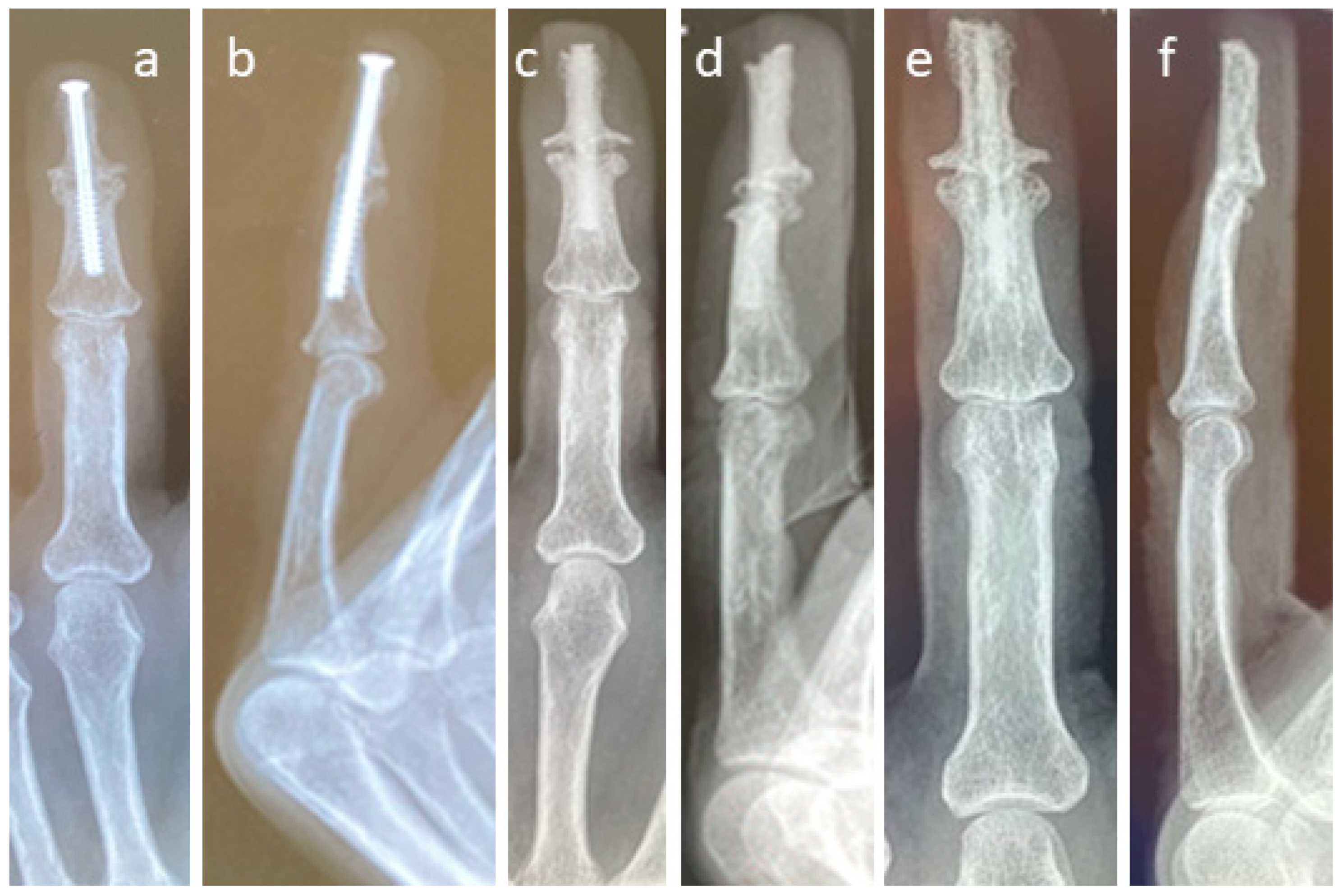
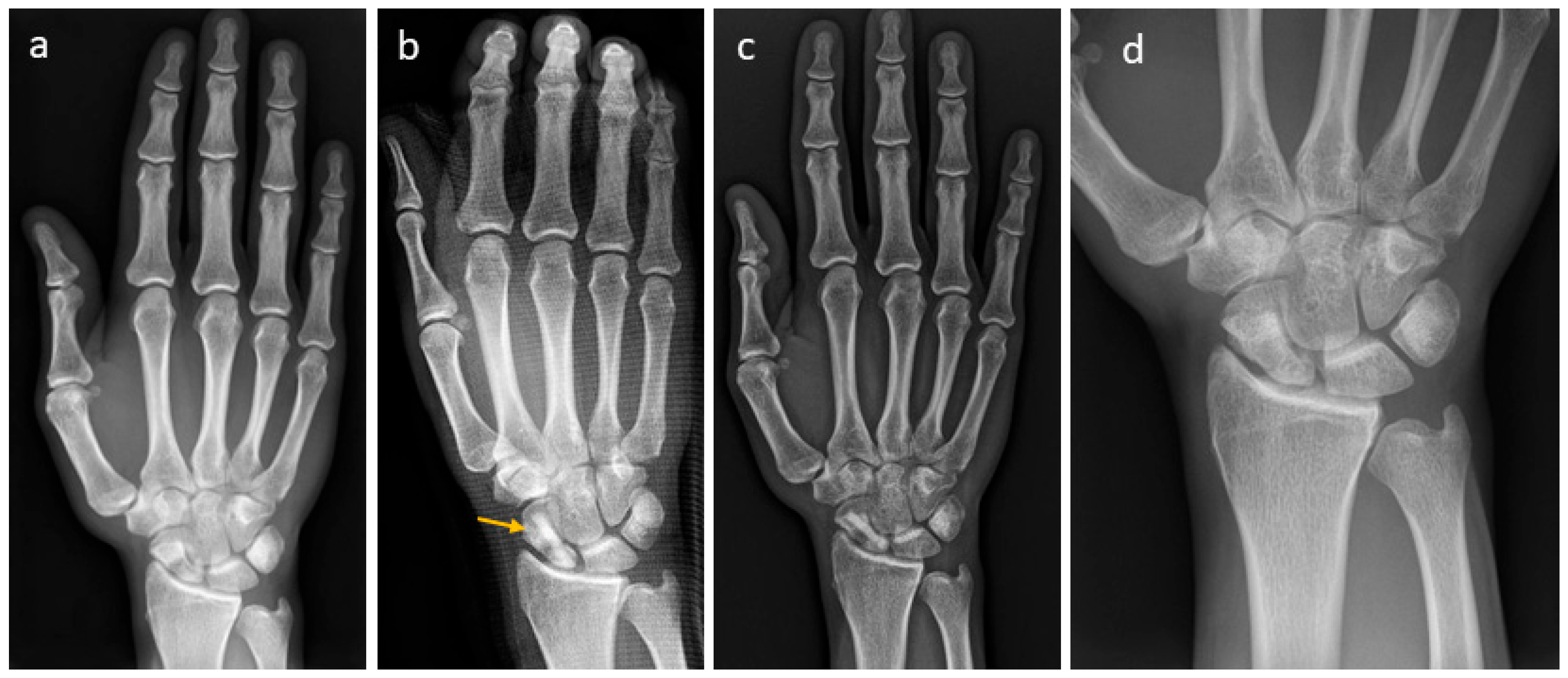
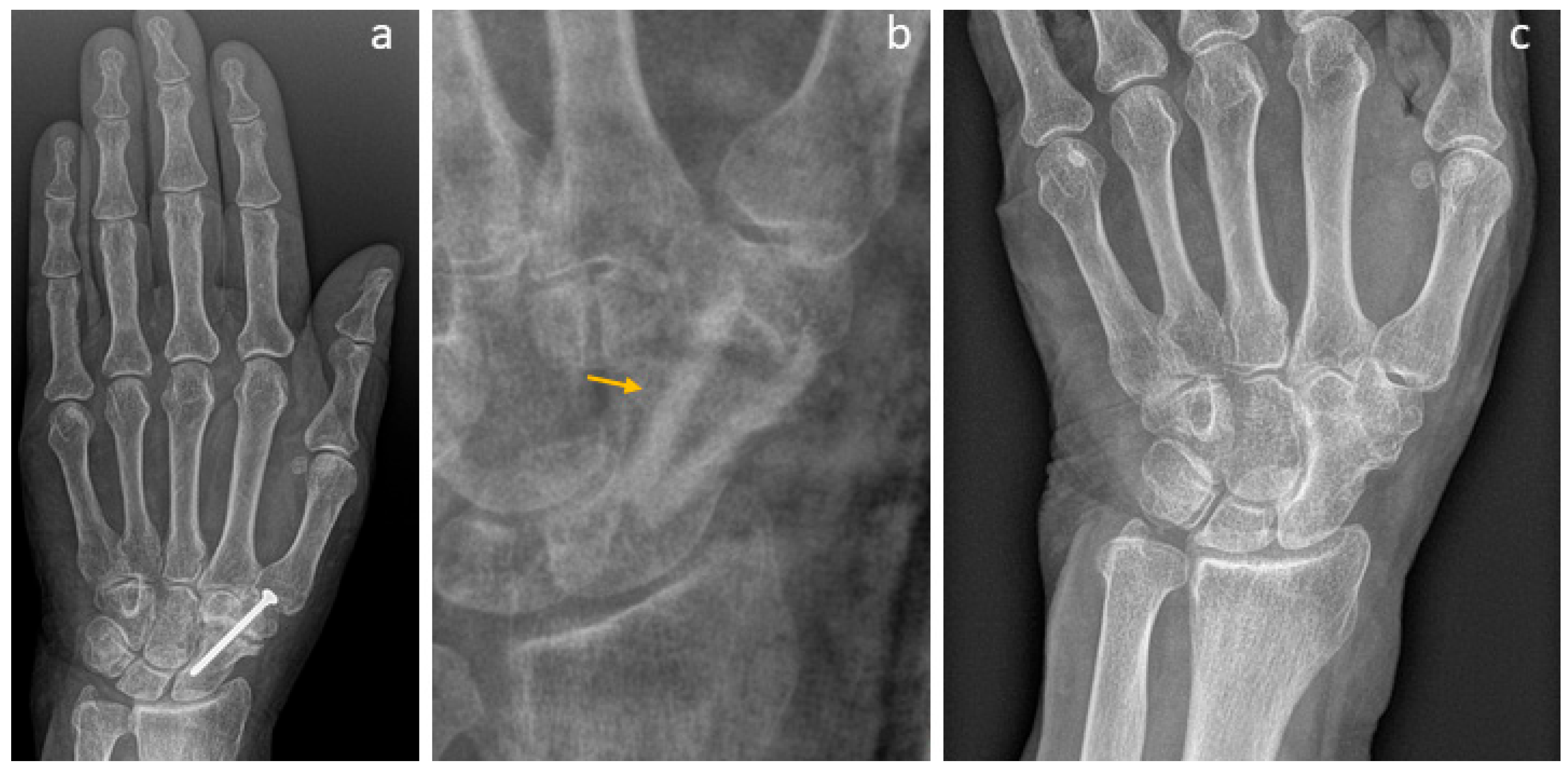
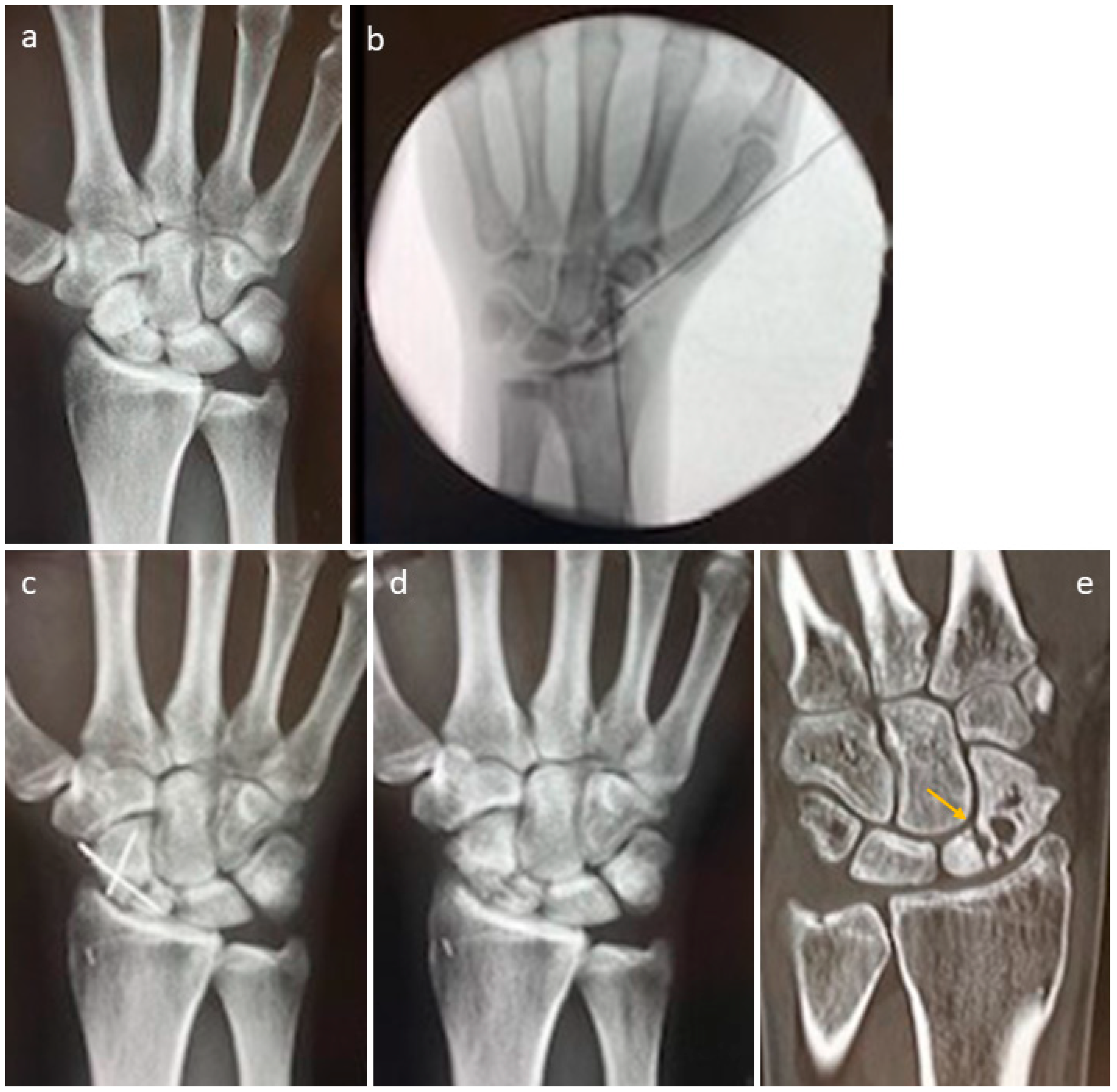
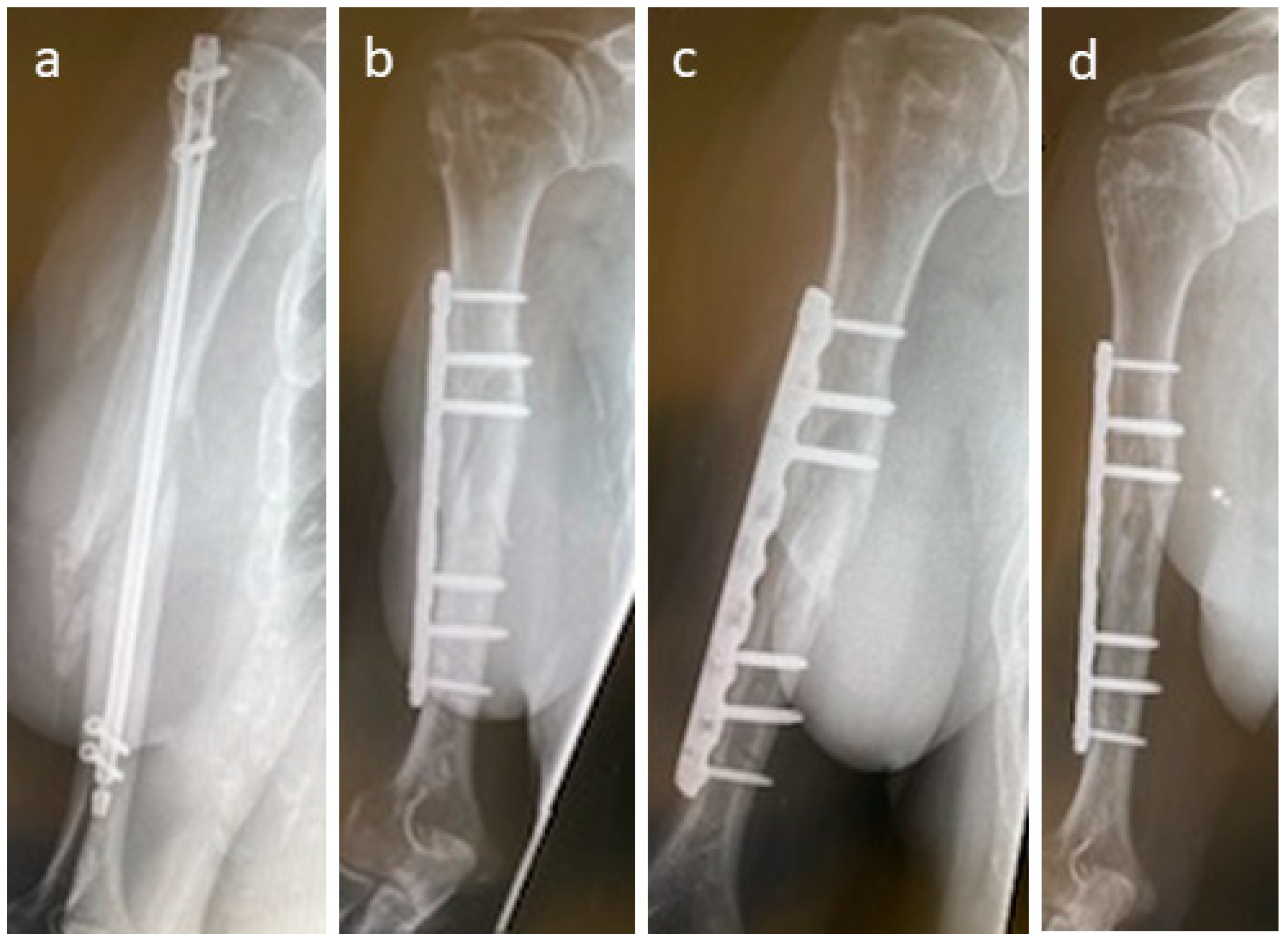
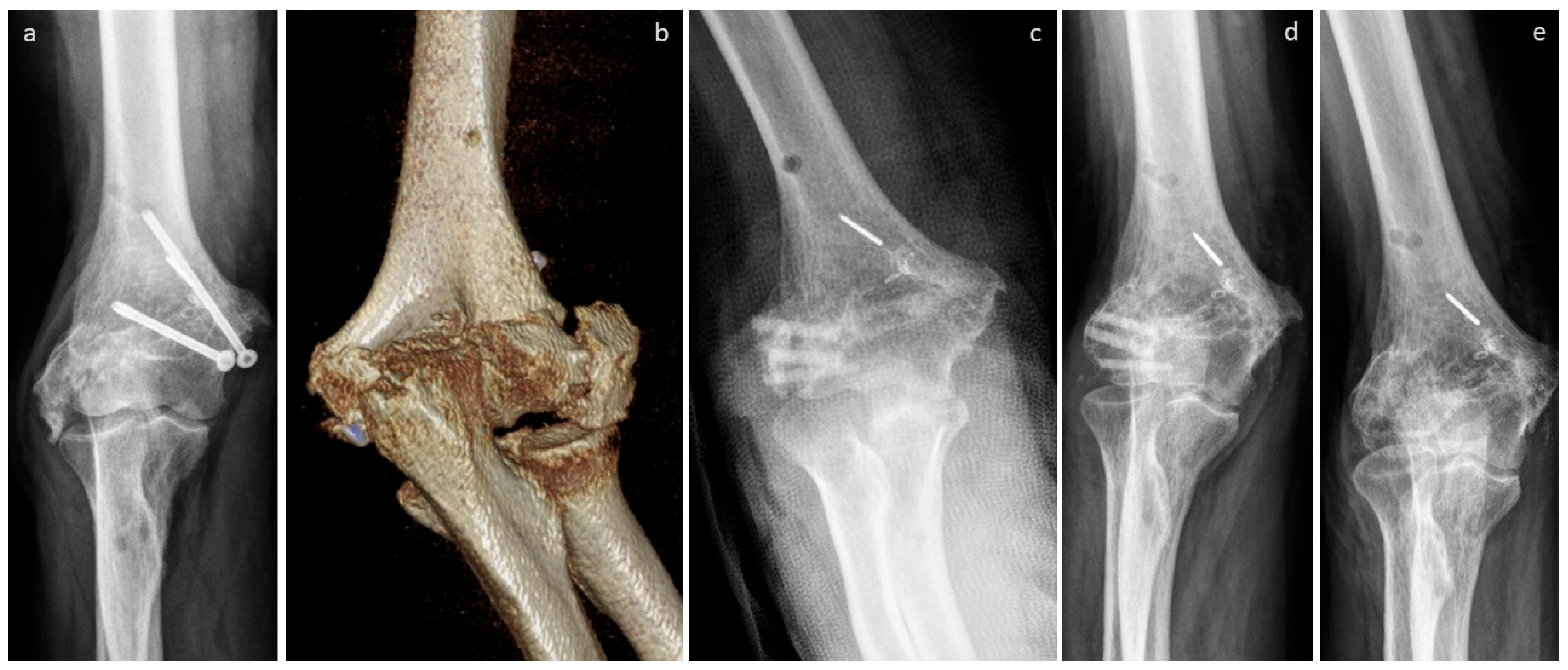
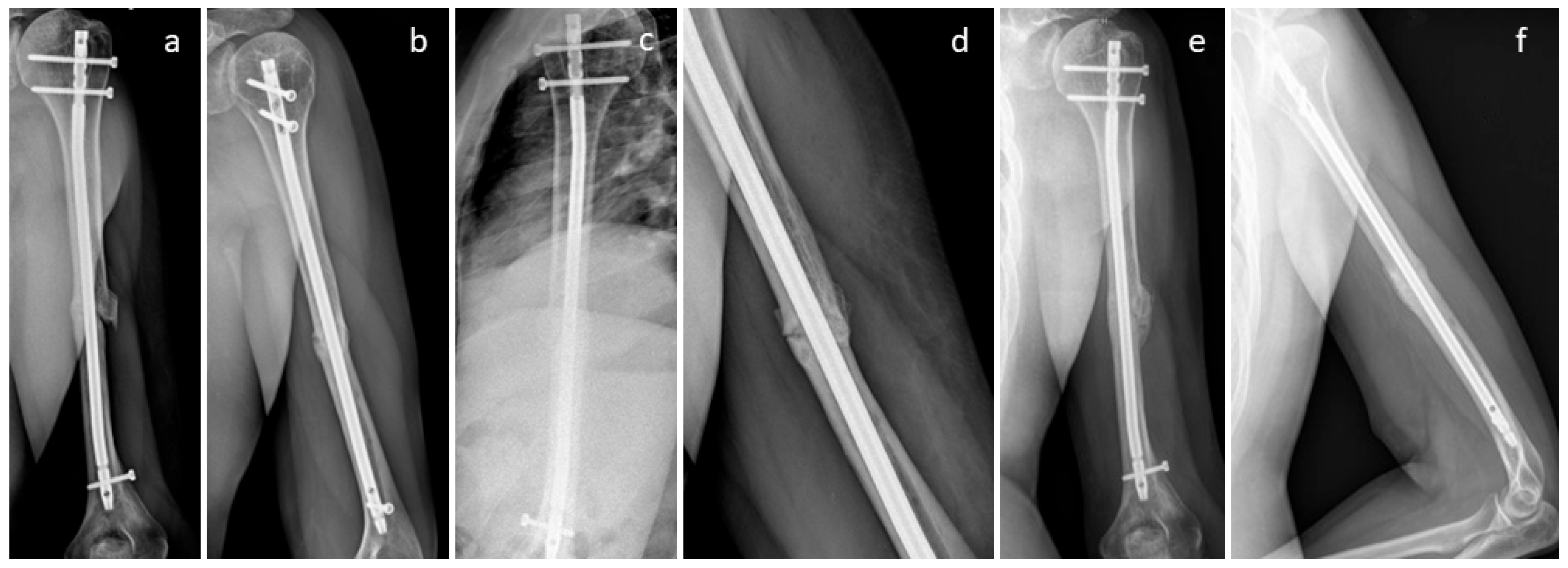
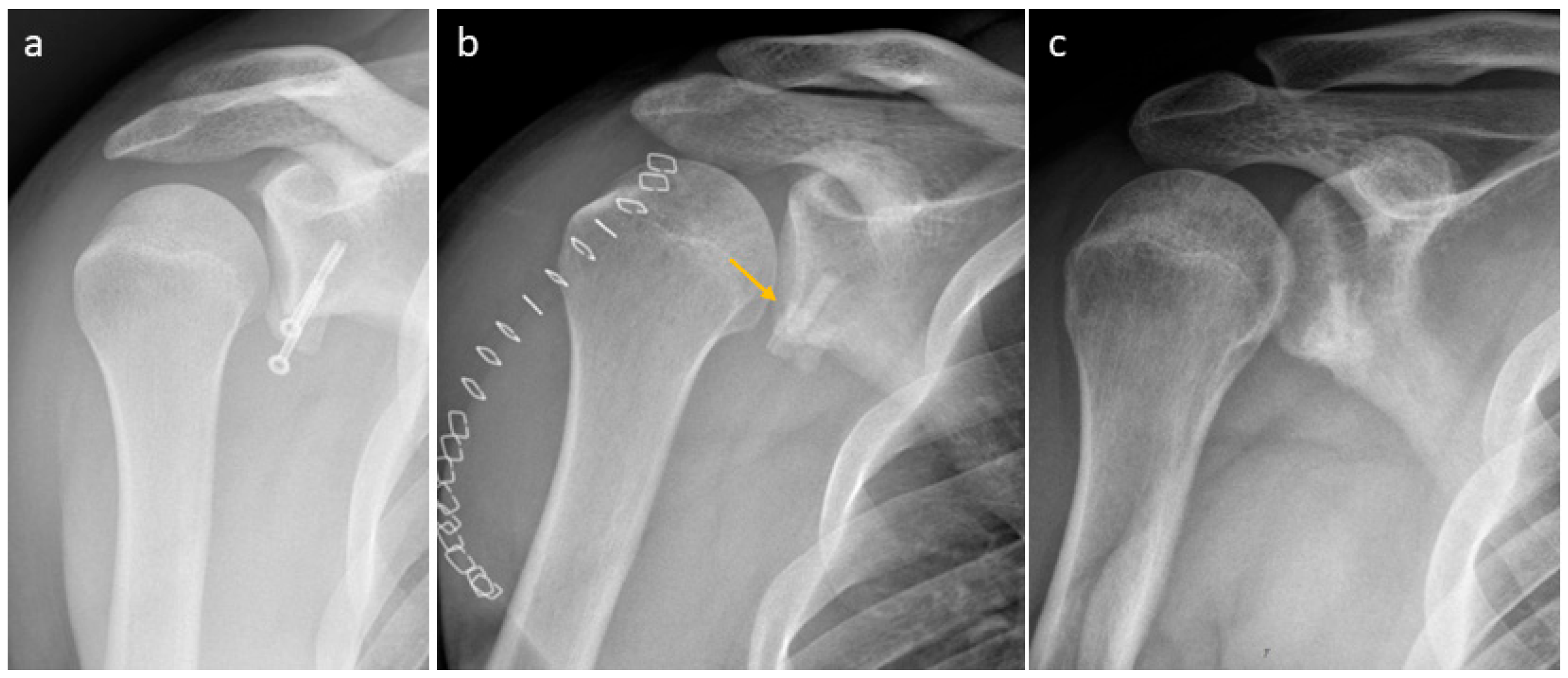
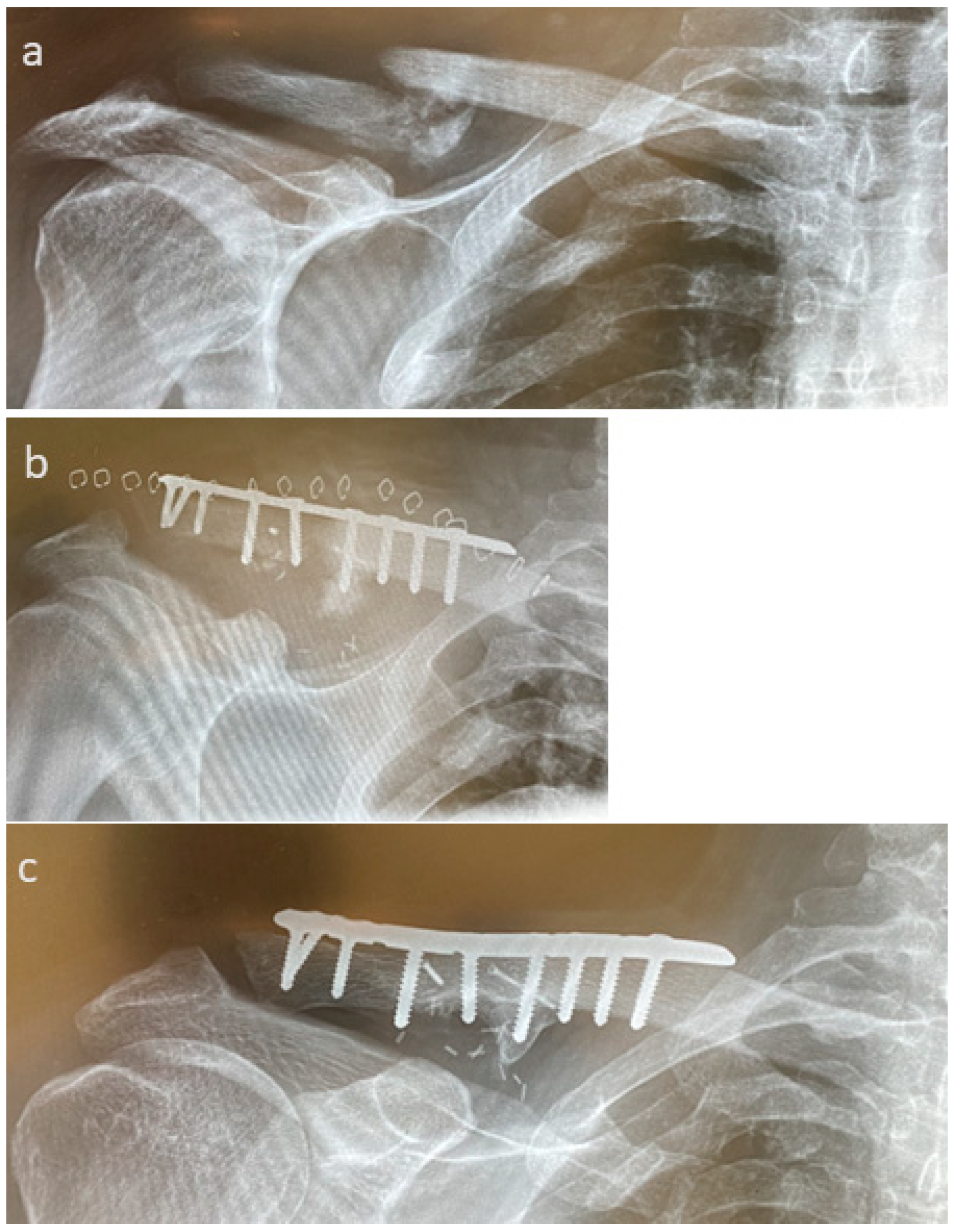
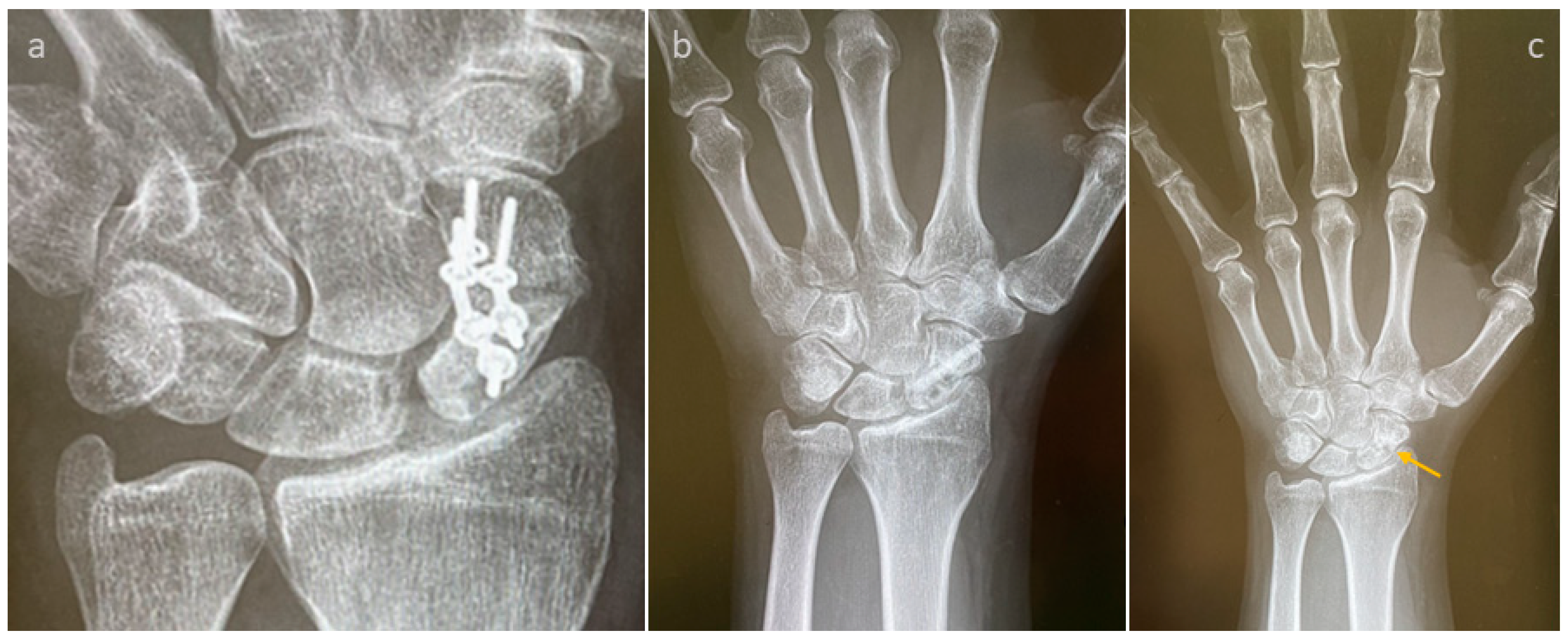
3.4. Selected Case Descriptions
4. Discussion
Limitation of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DIP1 | Distal interphalangeal joint finger 1 |
| DIP2,3,4 | Distal interphalangeal joint finger 2,3,4 |
| DIP2,3,5 | Distal interphalangeal joint finger 2,3,5 |
| IP Thumb | Interphalangeal joint, thumb |
| MCP | Metacarpophalangeal joints |
| PIP3 | Proximal interphalangeal joint finger 3 |
References
- Moghaddam-Alvandi, A.; Zimmermann, G.; Büchler, A.; Elleser, C.; Biglari, B.; Grützner, P.A.; Wölfl, C.G. Results of nonunion treatment with bone morphogenetic protein 7 (BMP-7). Unfallchirurg 2012, 115, 518–526. [Google Scholar] [CrossRef]
- Evers, S.C.; Daigeler, A.; Wahler, T. Möglichkeiten der vaskularisierten Knochentransplantationen bei Defektpseudarthrosen an ausgewählten Beispielen der oberen Extremität. OP-Journal 2019, 35, 231–240. [Google Scholar] [CrossRef]
- Patterson, E.D.; Elliott, C.; Dhaliwal, G.; Sayre, E.C.; White, N.J. Risk Factors for the Development of Persistent Scaphoid Non-Union After Surgery for an Established Non-Union. Hand 2025, 20, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Gagnon, D.; Mouallem, M.; Leduc, S.; Rouleau, D.M.; Chapleau, J. A systematic scoping review of the latest data on orthobiologics in the surgical treatment of non-union. Orthop. Traumatol. Surg. Res. OTSR 2024, 110, 103896. [Google Scholar] [CrossRef]
- Everding, J.; Roßlenbroich, S.; Raschke, M.J. Pseudarthroses of the long bones. Chirurg 2018, 89, 73–88. [Google Scholar] [CrossRef]
- Schmal, H.; Brix, M.; Bue, M.; Ekman, A.; Ferreira, N.; Gottlieb, H.; Kold, S.; Taylor, A.; Toft Tengberg, P.; Ban, I. Nonunion—Consensus from the 4th annual meeting of the Danish Orthopaedic Trauma Society. EFORT Open Rev. 2020, 5, 46–57. [Google Scholar] [CrossRef] [PubMed]
- Schädel-Höpfner, M.; Windolf, J.; Lögters, T.; Pillukat, T.; Jung, M.; Bickert, B. Scaphoid fractures: Current diagnostic and treatment concepts. Unfallchirurgie 2023, 126, 799–811. [Google Scholar] [CrossRef]
- Labmayr, V.; Huber, E.; Wenzel-Schwarz, F.; Holweg, P.; Ornig, M.; Jakob, G.; Palle, W.; Borchert, G.H.; Pastl, K. Non-Union Treatment in the Foot, Ankle, and Lower Leg: A Multicenter Retrospective Study Comparing Conventional Treatment with the Human Allogeneic Cortical Bone Screw (Shark Screw®). J. Pers. Med. 2024, 14, 352. [Google Scholar] [CrossRef]
- Reeh, F.M.; Sachse, S.; Wedekind, L.; Hofmann, G.O.; Lenz, M. Nonunions and Their Operative Treatment—A DRG-Based Epidemiological Analysis for the Years 2007–2019 in Germany. Dtsch. Arztebl. Int. 2022, 119, 869–875. [Google Scholar] [CrossRef]
- Hierholzer, C.; Sama, D.; Toro, J.B.; Peterson, M.; Helfet, D.L. Plate fixation of ununited humeral shaft fractures: Effect of type of bone graft on healing. J. Bone Jt. Surg. Am. 2006, 88, 1442–1447. [Google Scholar] [CrossRef]
- Ring, D.; Allende, C.; Jafarnia, K.; Allende, B.T.; Jupiter, J.B. Ununited diaphyseal forearm fractures with segmental defects: Plate fixation and autogenous cancellous bone-grafting. J. Bone Jt. Surg. Am. 2004, 86, 2440–2445. [Google Scholar] [CrossRef]
- Delamarre, M.; Leroy, M.; Barbarin, M.; Chantelot, C.; Saab, M. Long-term clinical and radiological results after scaphoid non-union treatment: A retrospective study about 60 cases. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 507–515. [Google Scholar] [CrossRef]
- Rollo, G.; Luceri, F.; Bisaccia, M.; Lanzetti, R.M.; Luceri, A.; Agnoletto, M.; Llaquet-Leiva, A.A.; Mangiavini, L.; Meccariello, L. Allograft versus autograft in forearm aseptic non-union treatment. J. Biol. Regul. Homeost. Agents 2020, 34, 207–212. [Google Scholar]
- Nwosu, C.; Rodriguez, K.; Zeng, S.; Klifto, K.M.; Klifto, C.S.; Ruch, D.S. Complications Following Volar Locking Plate Fixation of Distal Radius Fractures in Adults: A Systematic Review of Randomized Control Trials. J. Hand Surg. Am. 2023, 48, 861–874. [Google Scholar] [CrossRef] [PubMed]
- Shields, C.N.; Johnson, J.R.; Haglin, J.M.; Konda, S.R.; Egol, K.A. Some outcomes of patients treated operatively for distal humerus fractures are affected by hand dominance. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Lundqvist, E.; Fischer, P.; Wretenberg, P.; Pettersson, K.; Lopez Personat, A.; Sagerfors, M. Volar Locking Plate Compared with Combined Plating of AO Type C Distal Radius Fractures: A Randomized Controlled Study of 150 Cases. J. Hand Surg. Am. 2022, 47, 813–822. [Google Scholar] [CrossRef]
- Mehling, I.M.; Arsalan-Werner, A.; Wingenbach, V.; Seegmüller, J.; Schlageter, M.; Sauerbier, M. Practicability of a locking plate for difficult pathologies of the scaphoid. Arch. Orthop. Trauma Surg. 2019, 139, 1161–1169. [Google Scholar] [CrossRef] [PubMed]
- Hattori, Y.; Hayashi, K.; Chia, D.S.Y.; Sakamoto, S.; Doi, K. Arthrodesis for Primary Osteoarthritis of Trapeziometacarpal Joint Using Multiple Kirschner Wires and Tension Band Wire in Female Patients Older than 40. J. Hand Surg. Asian Pac. Vol. 2022, 27, 524–533. [Google Scholar] [CrossRef]
- Nowak, J.; Mallmin, H.; Larsson, S. The aetiology and epidemiology of clavicular fractures. A prospective study during a two-year period in Uppsala, Sweden. Injury 2000, 31, 353–358. [Google Scholar] [CrossRef]
- Vanderkarr, M.F.; Ruppenkamp, J.W.; Vanderkarr, M.; Holy, C.E.; Blauth, M. Risk factors and healthcare costs associated with long bone fracture non-union: A retrospective US claims database analysis. J. Orthop. Surg. Res. 2023, 18, 745. [Google Scholar] [CrossRef] [PubMed]
- Kalb, K.H.; Langer, M.; Windolf, J.; van Schoonhoven, J.; Pillukat, T. Scaphoid pseudarthrosis: Complex reconstruction using vascularized bone grafts. Unfallchirurg 2019, 122, 200–210. [Google Scholar] [CrossRef]
- Elgayar, L.; Elmajee, M.; Aljawadi, A.; Abdelaal, A.; Khan, S.; Pillai, A. A systematic review of mechanical stabilization by screw fixation without bone grafting in the management of stable scaphoid non-union. J. Clin. Orthop. Trauma 2021, 17, 112–117. [Google Scholar] [CrossRef]
- Van Nest, D.; Ilyas, A.M. Scaphoid Nonunion: A Review of Surgical Strategies. Orthopedics 2022, 45, e235–e242. [Google Scholar] [CrossRef] [PubMed]
- Kendall, C.B.; Brown, T.R.; Millon, S.J.; Rudisill, L.E., Jr.; Sanders, J.L.; Tanner, S.L. Results of four-corner arthrodesis using dorsal circular plate fixation. J. Hand Surg. Am. 2005, 30, 903–907. [Google Scholar] [CrossRef]
- Burnier, M.; Loisel, F.; Ardouin, L.; Beauthier, V.; Durand, A.; Erhard, L.; Gay, A.; Gras, M.; Mares, O.; Cognet, J.M. Treatment of scaphoid nonunion by arthroscopic cancellous bone grafting. Orthop. Traumatol. Surg. Res. OTSR 2023, 109, 103665. [Google Scholar] [CrossRef]
- Moog, P.; Cerny, M.K.; Schmauss, D.; Betzl, J.; Löw, S.; Erne, H. Osteophyte-induced impingement reduces range of motion in humpback deformity of incorrectly healed scaphoid reconstruction. Unfallchirurg 2021, 124, 132–137. [Google Scholar] [CrossRef]
- Yarar-Schlickewei, S.; Frosch, K.H.; Schlickewei, C. Scaphoid pseudarthrosis without circulatory disorder: Management and standard procedure for primary treatment. Unfallchirurg 2019, 122, 191–199. [Google Scholar] [CrossRef]
- Dodds, S.D.; Halim, A. Scaphoid Plate Fixation and Volar Carpal Artery Vascularized Bone Graft for Recalcitrant Scaphoid Nonunions. J. Hand Surg. Am. 2016, 41, e191–e198. [Google Scholar] [CrossRef] [PubMed]
- Millrose, M.; Gesslein, M.; Ittermann, T.; Kim, S.; Vonderlind, H.C.; Ruettermann, M. Arthrodesis of the proximal interphalangeal joint of the finger—A systematic review. EFORT Open Rev. 2022, 7, 49–58. [Google Scholar] [CrossRef]
- Mills, L.A.; Aitken, S.A.; Simpson, A. The risk of non-union per fracture: Current myths and revised figures from a population of over 4 million adults. Acta Orthop. 2017, 88, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Ekegren, C.L.; Edwards, E.R.; de Steiger, R.; Gabbe, B.J. Incidence, Costs and Predictors of Non-Union, Delayed Union and Mal-Union Following Long Bone Fracture. Int. J. Environ. Res. Public Health 2018, 15, 2845. [Google Scholar] [CrossRef]
- Basile, G.; Avato, F.M.; Passeri, A.; Accetta, R.; Amadei, F.; Giorgetti, A.; Castoldi, D.; Fozzato, S. Atrophic pseudarthrosis of humeral diaphyseal fractures: Medico-legal implications and methodological analysis of the evaluation. Acta Biomed. 2022, 93, e2022176. [Google Scholar] [CrossRef]
- Brcic, I.; Pastl, K.; Plank, H.; Igrec, J.; Schanda, J.E.; Pastl, E.; Werner, M. Incorporation of an Allogenic Cortical Bone Graft Following Arthrodesis of the First Metatarsophalangeal Joint in a Patient with Hallux Rigidus. Life 2021, 11, 473. [Google Scholar] [CrossRef]
- Pinder, R.M.; Brkljac, M.; Rix, L.; Muir, L.; Brewster, M. Treatment of Scaphoid Nonunion: A Systematic Review of the Existing Evidence. J. Hand Surg. Am. 2015, 40, 1797–1805.e1793. [Google Scholar] [CrossRef] [PubMed]
- Perren, S.M. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: Choosing a new balance between stability and biology. J. Bone Jt. Surg. Br. Vol. 2002, 84, 1093–1110. [Google Scholar] [CrossRef]
- Delloye, C.; Cornu, O.; Druez, V.; Barbier, O. Bone allografts: What they can offer and what they cannot. J. Bone Jt. Surg. Br. Vol. 2007, 89, 574–579. [Google Scholar] [CrossRef]
- Pastl, K.; Schimetta, W. The application of an allogeneic bone screw for osteosynthesis in hand and foot surgery: A case series. Arch. Orthop. Trauma Surg. 2021, 142, 2567–2575. [Google Scholar] [CrossRef]
- Walther, M.; Pastl, K.; Hofstätter, S. Osteosynthese mit Schraubentransplantat Shark Screw® aus humanem Knochen. Jatros Unfallchir Sport. 2018, 4, 54–56. [Google Scholar]
- Sailer, S.; Lechner, S.; Floßmann, A.; Wanzel, M.; Habeler, K.; Krasny, C.; Borchert, G.H. Treatment of scaphoid fractures and pseudarthroses with the human allogeneic cortical bone screw. A multicentric retrospective study. J. Orthop. Traumatol. 2023, 24, 6. [Google Scholar] [CrossRef] [PubMed]
- Krasny, C.; Radda, C.; Polke, R.; Schallmayer, D.; Borchert, G.H.; Albrecht, C. A human, allogeneic cortical bone screw for distal interphalangeal joint (DIP) arthrodesis: A retrospective cohort study with at least 10 months follow-up. Arch. Orthop. Trauma Surg. 2023, 143, 4557–4564. [Google Scholar] [CrossRef]
- Elliott, D.S.; Newman, K.J.; Forward, D.P.; Hahn, D.M.; Ollivere, B.; Kojima, K.; Handley, R.; Rossiter, N.D.; Wixted, J.J.; Smith, R.M.; et al. A unified theory of bone healing and nonunion: BHN theory. Bone Jt. J. 2016, 98-B, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Schmidmaier, G.; Moghaddam, A. Long Bone Nonunion. Z. Orthop. Unf. 2015, 153, 659–674. [Google Scholar] [CrossRef]
- Reigstad, O.; Thorkildsen, R.; Grimsgaard, C.; Melhuus, K.; Røkkum, M. Examination and treatment of scaphoid fractures and pseudarthrosis. Tidsskr. Nor. Legefore 2015, 135, 1138–1142. [Google Scholar] [CrossRef]
- Asmus, A.; Lautenbach, M.; Schacher, B.; Kim, S.; Eisenschenk, A. Scaphoid pseudarthrosis: Indications for avascular iliac crest or radius bone grafts. Orthopade 2016, 45, 951–965. [Google Scholar] [CrossRef]
- Atilgan, N.; Duman, N.; Colak, T.S.; Korucu, I.H.; Demiryurek, M.; Yilmaz, M. Comparison of the results of percutaneous and open screw fixation in the treatment of scaphoid nonunion fractures. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 9204–9211. [Google Scholar] [CrossRef]
- Braun, K.F.; Hanschen, M.; Biberthaler, P. Definition, Risikofaktoren und Klassifikationsmodelle von Pseudarthrosen. OP-Journal 2019, 35, 217–224. [Google Scholar] [CrossRef]
- Villani, F.; Uribe-Echevarria, B.; Vaienti, L. Distal interphalangeal joint arthrodesis for degenerative osteoarthritis with compression screw: Results in 102 digits. J. Hand Surg. Am. 2012, 37, 1330–1334. [Google Scholar] [CrossRef]
- Lari, A.; Nouri, A.; Alherz, M.; Prada, C. Operative treatment of distal radius fractures involving the volar rim-A systematic review of outcomes and complications. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 3419–3428. [Google Scholar] [CrossRef] [PubMed]
- Andre, C.; Coursier, R.; Saab, M.; Mezel, A.; Nectoux, É.; Fron, D.; Pougès, C.; Canavese, F. Functional and radiologic outcomes of non-displaced scaphoid waist fractures in adolescents approaching skeletal maturity: Comparison between conservative treatment and percutaneous screw fixation. Orthop. Traumatol. Surg. Res. OTSR 2023, 110, 103636. [Google Scholar] [CrossRef]
- Dunn, J.; Kusnezov, N.; Fares, A.; Mitchell, J.; Pirela-Cruz, M. The Scaphoid Staple: A Systematic Review. Hand 2017, 12, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Zenke, Y.; Oshige, T.; Menuki, K.; Hirasawa, H.; Yamanaka, Y.; Tajima, T.; Kosugi, K.; Sakai, A. Four-corner fusion method using a bioabsorbable plate for scapholunate advanced collapse and scaphoid nonunion advanced collapse wrists: A case series study. BMC Musculoskelet. Disord. 2020, 21, 683. [Google Scholar] [CrossRef] [PubMed]
- Waters, T.L.; Collins, L.K.; Cole, M.W.; Medvedev, G.; Lee, O.C.; Salas, Z.; Sherman, W.F. The Snuffbox: The Effect of Smokeless Tobacco Use on Scaphoid Fracture Healing. J. Am. Acad. Orthop. Surg. 2023, 31, e561–e569. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.; Hierl, K.; Brochhausen, C.; Alt, V.; Rupp, M. The epidemiology and direct healthcare costs of aseptic nonunions in Germany—A descriptive report. Bone Jt. Res. 2022, 11, 541–547. [Google Scholar] [CrossRef] [PubMed]





| Conventional Treatment (Metal Hardware ± Graft) | Shark Screw® Treatment (Shark Screw® ± Metal Plate) | |||
|---|---|---|---|---|
| Number of patients | Mean ± SD | Number of patients | Mean ± SD | |
| Number of patients | 11 | - | 30 | - |
| Age [years] | 11 | 40.8 ± 19.9 | 30 | 56.5 ± 13.8 * |
| BMI [kg/m2] | 11 | 25.1 ± 6.4 | 30 | 24.8 ± 5.2 |
| Gender [male/female] | 6/5 | - | 14/16 | - |
| Smoker [yes/no] | 5/6 | - | 7/23 | - |
| Comorbidities [yes/no] | 4/7 | - | 15/15 | - |
| Non-union revision following: | ||||
| Surgical fracture treatment | 3 | - | 12 | - |
| Elective surgery (arthrodesis, osteotomy) | 1 | - | 10 | - |
| Conservative fracture treatment | 7 | - | 8 | - |
| Aseptic/septic | 10/1 | - | 29/1 | - |
| Anatomic Localization of Non-Union | Conventional Treatment (Metal Hardware ± Graft) | Shark Screw® Treatment (Shark Screw® ± Metal Plate) | |
|---|---|---|---|
| Number of patients | 11 | 30 | |
| Shoulder | Clavicular | 3 | 1 |
| Shoulder (Latarjet) | 0 | 2 | |
| Arm | Humerus | 1 | 4 |
| Ulna | 1 | 2 | |
| Radius | 1 | 1 | |
| Elbow | 0 | 1 | |
| Hand | Scaphoid–Trapezoid–Trapezoidal (STT) | 0 | 1 |
| Wrist | 0 | 3 | |
| Repetitive Strain Injury (RSI) | 1 | 0 | |
| Scaphoid | 3 | 4 | |
| Finger | DIP1 | 0 | 2 |
| DIP2,3,4 | 0 | 1 | |
| DIP2,3,5 | 0 | 1 | |
| IP Thumb | 0 | 4 | |
| MCP 2 | 0 | 2 | |
| MCP Thumb | 0 | 1 | |
| PIP3 | 1 | 0 | |
| Conventional Treatment (Metal Hardware ± Graft) | Shark Screw® Treatment (Shark Screw® ± Metal Plate) | |
|---|---|---|
| Number of patients | Number of patients | |
| metal hardware use | 11 (per definition) | - |
| additional to Shark Screw® | - | 2 (1 × prothesis) |
| metal left in from previous surgery | - | 2 |
| Autograft use | ||
| Iliac crest | 2 | - |
| Medial femoral condylar span (MFC) | 2 | - |
| Lateral femoral condylar span (LFC) | 2 | - |
| Allograft use | ||
| DBM putty | 0 | 12 |
| cortical span | 0 | 1 |
| spongiosa chips | 0 | 1 |
| Conventional Treatment (Metal Hardware ± Graft) | Shark Screw® Treatment (Shark Screw® ± Metal Plate) | |||
|---|---|---|---|---|
| Number of patients | Mean ± SD/% | Number of patients | Mean ± SD/% | |
| Number of patients | 11 | - | 30 | - |
| Follow-up [weeks] | 11 | 71.0 ± 41.0 | 30 | 42.6 ± 37.5 † |
| Complications [yes/no] [%] | 4/7 | 36.4 | 1/29 * | 3.4 |
| Metal hardware removal [%] | 7 | 63.6 | 1 ‡** | 3.3 |
| Bony union rate [%] | 8 | 72.7 | 29 | 96.7 |
| Partial union [%] | 1 | 9.1 | 1 | 3.4 |
| Non-union [%] | 2 | 18.2 | 0 | 0.0 |
| Time to union [weeks] | 8 | 38.8 ± 26.3 | 29 | 10.8 ± 4.9 *** |
| Return to work [weeks] | 10 | 25.3 ± 16.3 | 30 | 12.0 ± 5.5 **** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huber, E.; Jakob, G.; Palle, W.; Borchert, G.H.; Pastl, K. Non-Union Treatment in the Shoulder, Arm, Wrist, and Fingers: A Multicentre Retrospective Study Comparing Conventional Treatment with the Human Allogeneic Cortical Bone Screw (Shark Screw®). Life 2025, 15, 1421. https://doi.org/10.3390/life15091421
Huber E, Jakob G, Palle W, Borchert GH, Pastl K. Non-Union Treatment in the Shoulder, Arm, Wrist, and Fingers: A Multicentre Retrospective Study Comparing Conventional Treatment with the Human Allogeneic Cortical Bone Screw (Shark Screw®). Life. 2025; 15(9):1421. https://doi.org/10.3390/life15091421
Chicago/Turabian StyleHuber, Elisabeth, Gerd Jakob, Wolfgang Palle, Gudrun H. Borchert, and Klaus Pastl. 2025. "Non-Union Treatment in the Shoulder, Arm, Wrist, and Fingers: A Multicentre Retrospective Study Comparing Conventional Treatment with the Human Allogeneic Cortical Bone Screw (Shark Screw®)" Life 15, no. 9: 1421. https://doi.org/10.3390/life15091421
APA StyleHuber, E., Jakob, G., Palle, W., Borchert, G. H., & Pastl, K. (2025). Non-Union Treatment in the Shoulder, Arm, Wrist, and Fingers: A Multicentre Retrospective Study Comparing Conventional Treatment with the Human Allogeneic Cortical Bone Screw (Shark Screw®). Life, 15(9), 1421. https://doi.org/10.3390/life15091421






