Abstract
Information regarding the longitudinal effects of natural/environmental disasters on obstetrics outcomes is limited. This study aimed to analyze the longitudinal changes in obstetrics outcomes over 8 years after the Great East Japan Earthquake and the Fukushima power plant accident. We used data from the first 8 years of the Pregnancy and Birth Survey by the Fukushima prefectural government, launched in 2011. We compared data on obstetrics outcomes by year and divided Fukushima Prefecture into six districts based on administrative districts. Longitudinal changes in the occurrence of preterm birth before 37 gestational weeks, low birth weight, and anomalies in newborns were accessed using the Mantel–Haenszel test for trends in all six districts. Overall, 57,537 participants were included. In 8 years, maternal age, conception rate after sterility treatment, and cesarean section delivery incidence increased. Although significant differences were observed in preterm birth and low birth weight occurrence among districts, there was no significant trend in the occurrence of preterm birth, low birth weight, and anomalies in newborns in all six districts of Fukushima Prefecture. The Great East Japan Earthquake and Fukushima power plant accident were associated with increased cesarean section delivery incidence but had no significant adverse effects on obstetrics outcomes.
1. Introduction
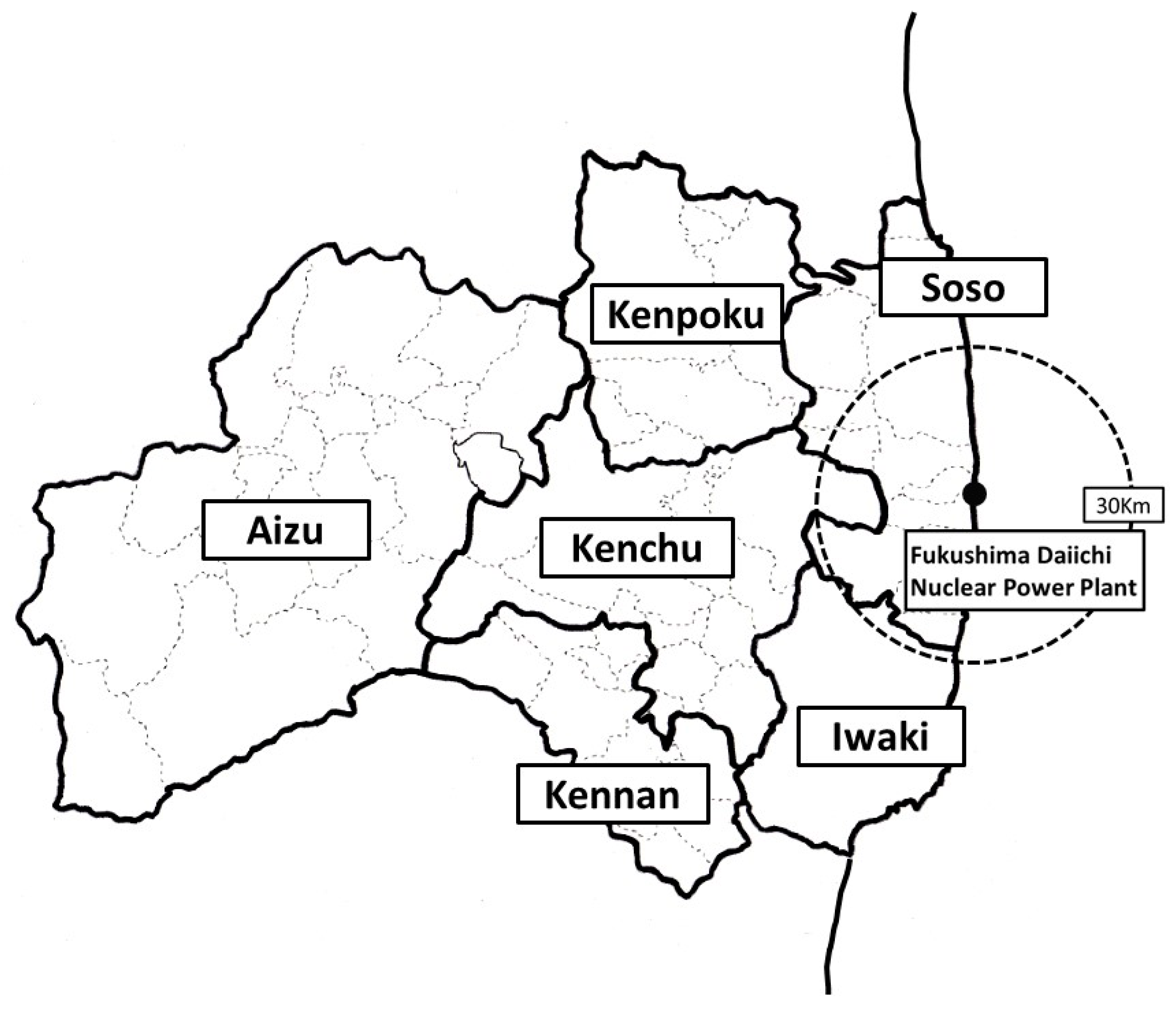
The Great East Japan Earthquake, which occurred on 11 March 2011, along with the subsequent tsunami and nuclear accident at the Fukushima Daiichi Nuclear Power Plant, was the most devastating event in recent Japanese history. In the Fukushima Prefecture, thousands of deaths were reported due to the tsunami, with the devastation affecting many people living in the coastal areas of the Soso and Iwaki districts. After the power plant accident, residents living in coastal areas were forced to evacuate suddenly. The Aizu district, located in a mountainous region in Fukushima Prefecture and far from the power plant, experienced less damage than the coastal regions (Figure 1).
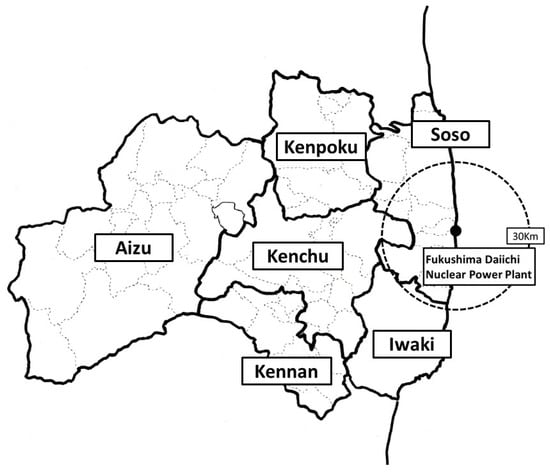
Figure 1.
Geographic information of Fukushima Prefecture. Geographic districts were first classified into seven areas, Kenpoku, Kenchu, Kennan, Soso, Iwaki, Aizu, and Minami-Aizu, and, then, the Aizu and Minami-Aizu areas were combined and called the Aizu area. The black dot within the Soso district represents the location of the Fukushima Daiichi Nuclear Power Plant. The circular dotted line indicates a distance of 30 km from the Fukushima Daiichi Nuclear Power Plant.
After the disaster, the Fukushima Health Management Survey (FHMS), a population-based study that included geographical and birth information used to evaluate pregnancy outcomes, was launched by Fukushima Prefecture to provide valuable data on the investigation of the health effect of low radiation dose and disaster-related stress in 2011 [1]. It is well established that disasters can significantly impact perinatal outcomes. Numerous studies have reported associations between such disasters and various aspects of perinatal health [2]. Even without direct exposure to the disaster, the surrounding circumstances can increase the risk of adverse pregnancy outcomes, including more unplanned pregnancies and sexually transmitted infections [2]. Specifically, regarding the Great East Japan Earthquake, some studies have reported its impact on perinatal outcomes in 2011 [3,4,5,6,7]. It has been shown that this disaster impacted both immediate outcomes and longer-term postnatal factors, such as the incidence of postnatal depression and the state of breastfeeding nutrition. Only a few studies have examined chronological trends in the occurrence of perinatal outcomes after the disaster. The chronological trends in pregnancy outcomes after the Great East Japan Earthquake is of worldwide interest; currently, the FHMS maintains the data from the investigation of the effect of this disaster on pregnancy and infant care.
This study aimed to examine the 8-year chronological trends in perinatal outcomes after the Great East Japan Earthquake in Fukushima Prefecture by district, using data from the FHMS.
2. Materials and Methods
2.1. Study Design
We used the maternal survey questionnaire results from the FHMS. The methods used for the FHMS and maternal survey have been previously reported [1]. The maternal survey is a population-based study conducted as part of the FHMS launched by the Fukushima Prefecture government in 2011 to assess the health condition of pregnant women and their neonates after the Great East Japan Earthquake. In this study, Fukushima Prefecture was divided into six districts [3], and women who received the maternal and child health handbook since 1 August 2010, were included. The maternal and child health handbook is a unique perinatal healthcare initiative in Japan. The handbooks help maintain a record of women’s antenatal and postnatal checkups by physicians. The self-report questionnaire was mailed to the participants on 18 January 2012. The mothers were asked to refer to their maternal and child health handbooks while completing the questionnaire. The issuance of the maternal and child health handbooks is carried out through administrative services. The linkage between the issuance of these handbooks and the mailing addresses was carried out through the administration. The response to the questionnaire was made through postage-paid return mail. This study was approved by the local ethics review committee of the authors’ institution (Approval No. 1317), and written informed consent was obtained from all participants.
The participants were pregnant women and their newborns delivered between 11 March 2011 and 31 December 2018. Cases of delivery before 11 March 2011, women who received a maternal and child health handbook outside Fukushima Prefecture, those with insufficient data, women pregnant at the time of the survey, women who had had an abortion, and mothers of triplets were excluded from this analysis.
2.2. Maternal Information and Obstetrics Outcome
The self-report questionnaire included maternal information such as the geographic district where women received the maternal and child health handbook when pregnant, year of delivery, maternal age at delivery, single or multiple gestational pregnancies, gestational weeks at delivery, mode of pregnancy, and mode of delivery, and neonatal information such as neonatal birth weight, sex of newborn, and presence of anomalies in newborns. Geographic districts were classified into six areas, namely, Kenpoku, Kenchu, Kennan, Soso, Iwaki, and Aizu (Figure 1). Delivery before 37 gestational weeks was defined as preterm birth (PTB), and a birth weight of <2500 g was defined as low birth weight (LBW). The mode of pregnancy was categorized as a natural pregnancy or the use of sterility treatment, such as ovulation induction, artificial insemination, or in vitro fertilization. The mode of delivery was categorized into vaginal delivery or cesarean section. Major anomalies reported in newborns were as follows: cataract, cardiac malformation, kidney or urinary tract malformation, spina bifida, microcephaly, hydrocephalus, cleft lip or palate, intestinal atresia (esophagus, duodenum, and ileum), imperforate anus, and poly- or syndactylism. Every anomaly reported in the questionnaire was defined as a major anomaly.
2.3. Statistical Analysis
The maternal characteristics of neonates were categorized into six groups according to birth year. The Chi-square test was used to compare the categorical variables, such as response rate and perinatal outcomes among areas per year. The extended Mantel–Haenszel Chi-square test for linear trends was used to analyze the trends in proportion between 2011 and 2018. The Jonckheere–Terpstra trend test was used to analyze trends in continuous variables between 2011 and 2018. SPSS ver. 26 (IBM Japan, Tokyo) was used for data analysis. A p-value of <0.05 was considered statistically significant.
3. Results
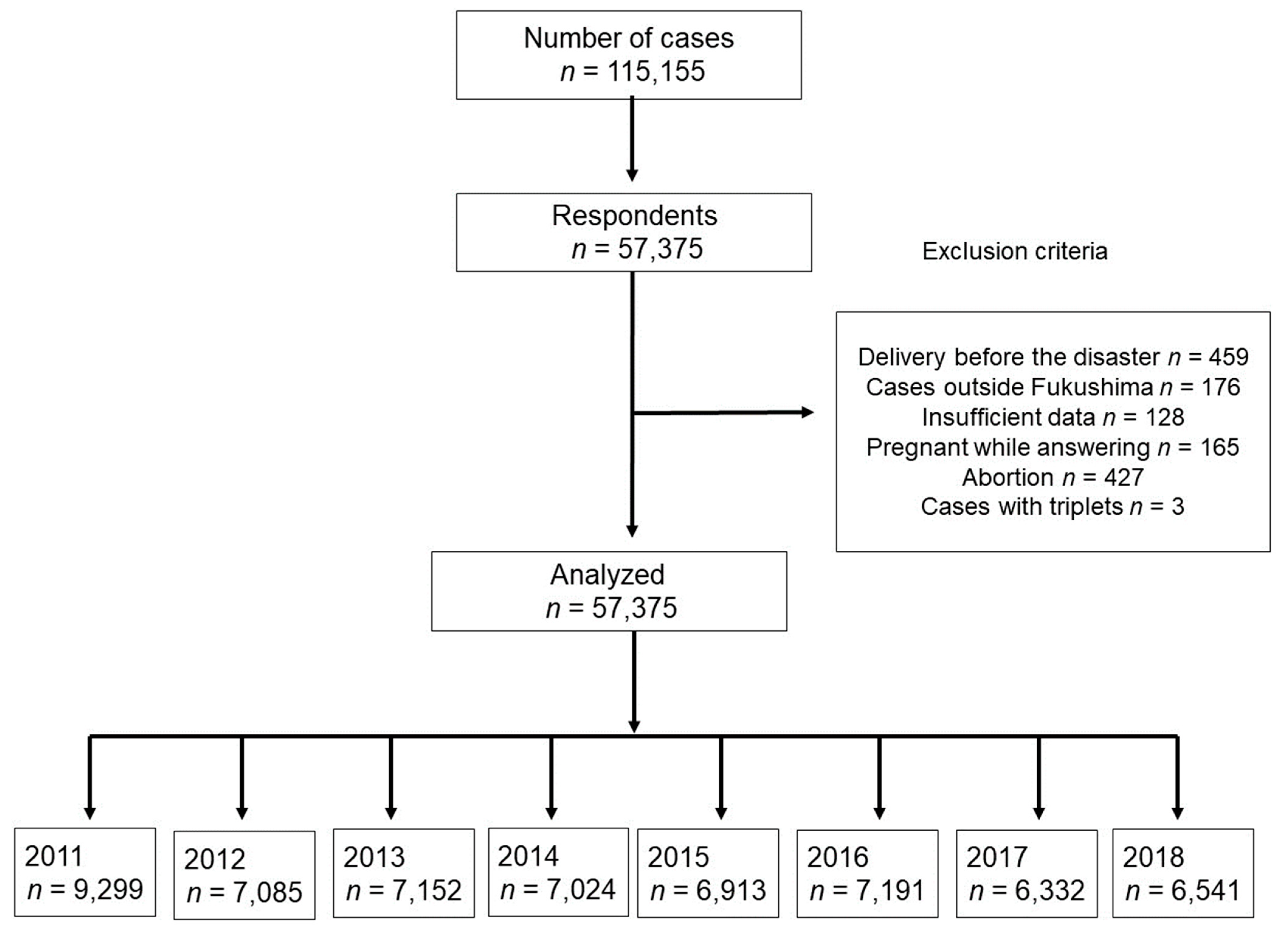
The survey questionnaire was mailed to 115,155 women who had experienced pregnancy during the study period. In total, 57,537 women (response rate 50.0%) responded to the questionnaire. Women who had given birth before 11 March 2011 (n = 459), who received maternal and child health handbooks outside Fukushima Prefecture (n = 176), for whom sufficient data were unavailable (n = 128), who were pregnant at the time of the survey (n = 165), who had had an abortion (n = 427), and those with triplets (n = 3) were excluded from the study. After applying these exclusion criteria, 57,375 women were finally included in the analyses. The number of cases in each of the eight years from 2011 to 2018 inclusive was 9299, 7085, 7152, 7024, 6913, 7191, 6332, and 6541, respectively (Figure 2).
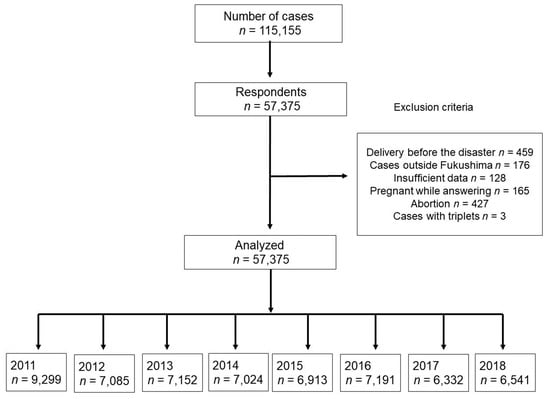
Figure 2.
Study flow.
Table 1 shows the chronological changes in response rates by district. The Mantel–Haenzel test showed a significantly decreasing trend in the response rate from 58.2% in 2011 to 51.4% in 2018 (p < 0.001). This was observed in all districts except Kennan (p = 0.652). The Chi-square test showed differences in response rates among districts. During the study period, Kenpoku had the highest response rate, except in 2011, when the area with the highest response rate was Soso (65.6%), the location of the coastal area and the Fukushima Daiichi power plant.

Table 1.
Chronological change in response rate by each district.
Table 2 summarizes the characteristics of the respondents based on the year of delivery. Although maternal age, gestational age at delivery, and ratio of male newborns showed significant differences during the study period (p < 0.001, p < 0.001, and p = 0.046, respectively), there was no significant difference in mean neonatal weight (p = 0.912). Additionally, there were no significant differences in the rate of single pregnancy (p = 0.368). The conception rate after sterility treatment and cesarean delivery tended to increase (p < 0.001 and p = 0.005, respectively).

Table 2.
Characteristics of respondents based on year of delivery.
Table 3 shows the chronological change in the occurrence of preterm birth by district. The Chi-square test showed no significant difference in the occurrence of preterm birth among the districts, except in 2012 (p = 0.020). The overall rate of preterm birth was 4.6% in 2011 and increased to 5.2% by 2018. However, there was no significant trend in the occurrence of preterm birth between 2011 and 2018 in all areas (p = 0.197).

Table 3.
Chronological change in the occurrence of preterm birth by each district.
Table 4 shows the chronological change in the occurrence of LBW by district. There was no significant difference in the occurrence of LBW during the study period. In 2011, a significant difference in the occurrence of LBW was observed between Kempoku (7.6%) and Iwaki districts (10.3%). In 2012, there was also a significant difference with respect to the occurrence of LBW between Kenpoku (7.6%) and Aizu districts (11.3%). The overall rate of LBW was 8.6% in 2011 and rose to 9.1% by 2018; however, no significant increasing trend was observed over time (p = 0.500).

Table 4.
Chronological change in the occurrence of low-birth-weight infants by each district.
Table 5 shows the chronological change in the occurrence of anomalies in newborns. The rate of anomalies across all regions was 2.85% in 2011; however, it was 2.23% in 2018. There was no significant trend in the occurrence of newborn anomalies between 2011 and 2018 in all areas (p = 0.069), and the Kenchu district showed a decrease in the rate of anomalies in newborns (p = 0.011).

Table 5.
Chronological change in the occurrence of anomalies in newborns by district.
Table 6 delineates the incidence rate of anomalies each year, classified into 11 different types. Excluding the category of “Others,” the most frequently observed anomaly each year was “Cardiac malformation,” which was found at a rate of 1.01% in 2013. There was no significant trend in the occurrence of each neonatal anomaly.

Table 6.
Chronological change in the occurrence of major anomalies in newborns.
4. Discussion
To our knowledge, this is the first population-based study that examined chronological trends for pregnancy outcomes following the disaster. Although the response rate in 2011 was the highest, especially in the Soso district, where the most disaster-related damage had occurred, the response rate decreased over the years, with more than 50% reported in 2018. We also found an increasing trend for mean maternal age, rate of conception after sterility treatment, and rate of cesarean delivery over the years. Regarding PTB, LBW, and fetal anomalies, there were no distinct changes in the trend of occurrence.
The response rate in this study was approximately 50%, which varied significantly over the years and between districts. While Kenpoku constantly had a higher response rate than the remaining districts, Soso had a higher rate only in 2011. This difference may be related to the concern of pregnant women in the Kenpoku and Soso districts that they were exposed to relatively higher radiation doses. Disasters potentially influence a range of reproductive outcomes [8]. Previous studies examined the effects of exposure to disasters on pregnancy outcomes, and these exposures were usually from so-called “attacks” such as the World Trade Center Disaster, the bombing attack in Serbia, and the Madrid train bombing; environmental and chemical disasters such as the Bhopal gas release in India, the Three Mile Island accident, and the Chernobyl accident; and natural disasters such as earthquakes, hurricanes, floods, and avalanches [2]. The Great East Japan Earthquake and Fukushima Daiichi nuclear accident form a complex disaster because they included natural disasters such as the Great Earthquake and tsunami and environmental/industrial disasters such as the nuclear power plant accident.
4.1. Disaster in Fukushima and Preterm Birth or LBW
Findings on the association between environmental/chemical disasters and gestational age or birth weight are conflicting. For instance, Goldman et al. reported that the Love Canal disaster in the USA showed no significant association with gestational age among 227 residents [9]. Meanwhile, Levi et al. reported that the Chernobyl accident affected gestational age and maternal anxiety among 88 Swedish women who were early in their pregnancies during the disaster [10]. Inconsistent with our study, the Wenchuan earthquake disaster in China increased the risk of PTB. Tan et al. compared the incidence of PTB between 6638 pregnant women before the Wenchuan earthquake disaster and 6365 pregnant women after the disaster [11]. The incidence of PTB was 5.6% and 7.4%, respectively, significantly higher after the disaster (p < 0.01). In Japan, high-risk pregnancies have increased due to advanced maternal age and complicated pregnancies [12,13,14]. The incidences of PTB at <37 gestational weeks (5.7%) and LBW of <2500 g (9.4%) in the 6 areas in the study have almost been stable after the disaster. The evidence on the effect of the Fukushima disaster is also conflicting. Hyashi et al. used the same FMHS data and found that the Great East Japan Earthquake had no significant association with the incidence of PTB at <37 gestational weeks during the first year of the disaster among total Fukushima residents [15]. Several pregnant women were forced to evacuate during the disaster, resulting in maternal depressive symptoms [4,16]. Suzuki et al. reported that pregnant women who changed their perinatal checkup institution due to medical indication were significantly associated with shorter gestational duration (β = −10.6, p < 0.001) and preterm birth (adjusted odds ratio, 8.5; 95% confidence interval, 5.8–12.5) compared with women who visited only one institution [17].
The association between the environment or a natural disaster and fetal growth is also controversial [15,18,19,20,21]. Regarding the Great East Japan Earthquake and Fukushima Daiichi nuclear accident, we have previously reported no evidence that the disaster increased the incidence of small gestational age in the Fukushima Prefecture during the first year of the disaster [5]. Using an institution-based investigation of the coastal area where the most catastrophic damage occurred, Leppold et al. reported no increased proportions in preterm births or LBW in any year after the disaster (merged post-disaster risk ratio of preterm birth: 0.68, 95% confidence interval: 0.38–1.21 and LBW birth: 0.98, 95% confidence interval: 0.64–1.51) [22]. In Japan, pregnant women may have better access to relief programs or receive adequate support from their families, society, and government during disasters [4].
4.2. Congenital Anomalies
The association between disasters and congenital anomalies is a major public concern. Several major environmental or industrial disasters have been related to congenital anomalies. These include the nuclear reactor accidents at Chernobyl, Ukraine, in 1986 and Three Mile Island, Pennsylvania, in 1979. The accident at Chernobyl involved a much larger radiation dose exposure and affected more people than the Three Mile Island or Fukushima incidents. Reviews on the effect of the Chernobyl disaster indicated increased microcephaly and neural tube defects [23,24,25]. However, the incidence of most congenital anomalies did not increase in most European countries [26,27,28]. Previous studies have reported that 2–3% of all newborns have a major congenital abnormality, which is detectable at birth [29,30] In Japan, from 2011 to 2016, the incidence of congenital anomalies was 2.43–2.59%, according to a report of the International Clearinghouse for Birth Defects Surveillance and Research Japan Center [31]. Using a Japanese birth cohort study, which included 12,804 pregnant women in Fukushima Prefecture, Kyozuka et al. reported that the prevalence of major congenital anomalies at delivery between 2011 and 2014 in Fukushima Prefecture was 1.6–3.2%, depending on maternal age [6]. Using the same data set as this study, Fujimori et al. reported that the occurrence of congenital anomalies in Fukushima Prefecture during the first year after the disaster was 2.72% (238/8672) [3].
Environmental endocrine disrupters, a group of compounds with potentially adverse health effects, are thought to be associated with cryptorchidism [32]. Kojima et al. suggested that it is difficult to clarify the prevalence of cryptorchidism due to the complexities of the design settings of epidemiological surveys of this disease. They rejected the hypothesis that cryptorchidism increased anywhere in Japan due to the Fukushima Daiichi Nuclear Power Plant accident [33]. Hirata et al., using the All Japanese Cardiovascular Surgery Database, reported no increase in the number of patients with congenital heart disease during the period 2010–2013 [34].
Our study has several strengths. In Japan, few epidemiological studies include pregnant women. Large-scale studies and data supported by the government are considered valuable. In addition, we obtained relatively precise data on gestational ages and birth weights from participants’ maternal and child health handbooks. Nevertheless, this study has some limitations. First, because the response rate was only 50–60% throughout the study period, the incidence of negative outcomes may have been overestimated due to the possible over-representation of women affected the most by the disasters, especially those pregnant between 2011 and 2012. Second, as this study used a self-administered questionnaire, it is assumed that the mothers answered correctly, especially regarding fetal anomalies. Lastly, this survey analyzed each district but did not investigate the relationship with individual radiation exposure doses.
5. Conclusions
In conclusion, the findings of our study and previous study suggest that the Great East Japan Earthquake and associated disasters had little effect on exposed pregnant women in the first 8 years following the earthquake. A better understanding of the adverse reproductive effects of disasters is required to allow as much preparedness as is needed during an emergency response to prevent mortality and morbidity [4]. Further studies to determine whether the disaster causes early pregnancy loss, such as miscarriage or abortion, or psychological-associated complications, are warranted.
Author Contributions
Conceptualization, K.K. and H.O.; methodology, S.Y. (Seiji Yasumura) and S.Y. (Shun Yasuda); formal analysis, K.I.; investigation, T.M. and T.O.; data curation, K.I.; writing—original draft preparation, H.K.; writing—review and editing, T.O.; supervision, K.F.; project administration, K.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and The local ethics review committee of the authors’ institution approved this study (Approval No. 1317).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, H.K., upon reasonable request.
Acknowledgments
This survey was partially supported by the National Health Fund for Children and Adults Affected by the Nuclear Incident. The findings and conclusions of this article are solely the responsibility of the authors and do not represent the official views of the government of Fukushima Prefecture.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Yasumura, S.; Hosoya, M.; Yamashita, S.; Kamiya, K.; Abe, M.; Akashi, M.; Kodama, K.; Ozasa, K.; Fukushima Health Management Survey Group. Study protocol for the Fukushima Health Management Survey. J. Epidemiol. 2012, 22, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Harville, E.; Xiong, X.; Buekens, P. Disasters and perinatal health: A systematic review. Obstet. Gynecol. Surv. 2010, 65, 713–728. [Google Scholar] [CrossRef] [PubMed]
- Fujimori, K.; Kyozuka, H.; Yasuda, S.; Goto, A.; Yasumura, S.; Ota, M.; Ohtsuru, A.; Nomura, Y.; Hata, K.; Suzuki, K.; et al. Pregnancy and birth survey after the Great East Japan Earthquake and Fukushima Daiichi Nuclear Power Plant accident in Fukushima Prefecture. Fukushima J. Med. Sci. 2014, 60, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Kyozuka, H.; Yasuda, S.; Kawamura, M.; Nomura, Y.; Fujimori, K.; Goto, A.; Yasumura, S.; Abe, M. Impact of the Great East Japan Earthquake on feeding methods and newborn growth at 1 month postpartum: Results from the Fukushima Health Management Survey. Radiat. Environ. Biophys. 2016, 55, 139–146. [Google Scholar] [CrossRef]
- Yasuda, S.; Kyozuka, H.; Nomura, Y.; Fujimori, K.; Goto, A.; Yasumura, S.; Hata, K.; Ohira, T.; Abe, M. Influence of the Great East Japan Earthquake and the Fukushima Daiichi nuclear disaster on the birth weight of newborns in Fukushima Prefecture: Fukushima Health Management Survey. J. Matern. Fetal Neonatal Med. 2017, 30, 2900–2904. [Google Scholar] [CrossRef] [PubMed]
- Kyozuka, H.; Fujimori, K.; Hosoya, M.; Yasumura, S.; Yokoyama, T.; Sato, A.; Hashimoto, K. The Japan environment and children’s study (JECS) in Fukushima Prefecture: Pregnancy outcome after the great east Japan earthquake. Tohoku J. Exp. Med. 2018, 246, 27–33. [Google Scholar] [CrossRef]
- Kyozuka, H.; Murata, T.; Yasuda, S.; Fujimori, K.; Goto, A.; Yasumura, S.; Abe, M.; Pregnancy and Birth Survey Group of the Fukushima Health Management Survey. The effect of the Great East Japan Earthquake on hypertensive disorders during pregnancy: A study from the Fukushima Health Management Survey. J. Matern. Fetal Neonatal Med. 2020, 33, 4043–4048. [Google Scholar] [CrossRef]
- Cordero, J.F. The epidemiology of disasters and adverse reproductive outcomes: Lessons learned. Environ. Health Perspect. 1993, 101 (Suppl. S2), 131–136. [Google Scholar] [CrossRef]
- Goldman, L.R.; Paigen, B.; Magnant, M.M.; Highland, J.H. Low birth weight, prematurity and birth defects in children living near the hazardous waste site, love Canal. Hazard Waste Hazard Mater. 1985, 2, 209–223. [Google Scholar] [CrossRef]
- Levi, R.; Lundberg, U.; Hanson, U.; Frankenhacuser, M. Anxiety during pregnancy after the Chernobyl accident as related to obstetric outcome. J. Psychosom. Obstet. Gynecol. 1989, 10, 221–230. [Google Scholar] [CrossRef]
- Tan, C.E.; Li, H.J.; Zhang, X.G.; Zhang, H.; Han, P.Y.; An, Q.; Ding, W.J.; Wang, M.Q. The impact of the Wenchuan earthquake on birth outcomes. PLoS ONE 2009, 4, e8200. [Google Scholar] [CrossRef] [PubMed]
- Kyozuka, H.; Fujimori, K.; Hosoya, M.; Yasumura, S.; Yokoyama, T.; Sato, A.; Hashimoto, K. The effect of maternal age at the first childbirth on gestational age and birth weight: The Japan environment and children’s study (JECS). J. Epidemiol. 2019, 29, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Kyozuka, H.; Yamaguchi, A.; Suzuki, D.; Fujimori, K.; Hosoya, M.; Yasumura, S.; Yokoyama, T.; Sato, A.; Hashimoto, K.; Japan Environment and Children’s Study (JECS) Group. Risk factors for placenta accreta spectrum: Findings from the Japan environment and children’s study. BMC Preg. Childbirth 2019, 27, 447. [Google Scholar] [CrossRef]
- Yamaguchi, A.; Kyozuka, H.; Fujimori, K.; Hosoya, M.; Yasumura, S.; Yokoyama, T.; Sato, A.; Hashimoto, K.; Japan Environment and Children’s Study Group. Risk of preterm birth, low birthweight and small-for-gestational-age infants in pregnancies with adenomyosis: A cohort study of the Japan Environment and children’s Study. Acta Obstet. Gynecol. Scand. 2019, 98, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Fujimori, K.; Yasumura, S.; Goto, A.; Nakai, A. Obstetric outcomes in women in Fukushima Prefecture during and after the Great East Japan Earthquake and Fukushima Nuclear Power Plant Accident: The Fukushima Health Management Survey. Open J. Obstet. Gynecol. 2016, 6, 705–713. [Google Scholar] [CrossRef]
- Goto, A.; Bromet, E.J.; Fujimori, K.; Pregnancy and Birth Survey Group of Fukushima Health Management Survey. Immediate effects of the Fukushima nuclear power plant disaster on depressive symptoms among mothers with infants: A prefectural-wide cross-sectional study from the Fukushima Health Management Survey. BMC Psychiatry 2015, 15, 59. [Google Scholar] [CrossRef]
- Suzuki, K.; Goto, A.; Fujimori, K. Effect of medical institution change on gestational duration after the Great East Japan Earthquake: The Fukushima Health Management Survey. J. Obstet. Gynaecol. Res. 2016, 42, 1704–1711. [Google Scholar] [CrossRef]
- Chang, H.L.; Chang, T.C.; Lin, T.Y.; Kuo, S.S. Psychiatric morbidity and pregnancy outcome in a disaster area of Taiwan 921 earthquake. Psychiatry Clin. Neurosci. 2002, 56, 139–144. [Google Scholar] [CrossRef]
- Xiong, X.; Harville, E.W.; Mattison, D.R.; Elkind-Hirsch, K.; Pridjian, G.; Buekens, P. Exposure to Hurricane Katrina, post-traumatic stress disorder and birth outcomes. Am. J. Med. Sci. 2008, 336, 111–115. [Google Scholar] [CrossRef]
- Tong, V.T.; Zotti, M.E.; Hsia, J. Impact of the Red River catastrophic flood on women giving birth in North Dakota, 1994–2000. Matern. Child Health J. 2011, 15, 281–288. [Google Scholar] [CrossRef]
- Hamilton, B.E.; Sutton, P.D.; Mathews, T.J.; Martin, J.A.; Ventura, S.J. The effect of Hurricane Katrina: Births in the U.S. Gulf Coast region, before and after the storm. Natl. Vital Stat. Rep. 2009, 58, 1–32. [Google Scholar]
- Leppold, C.; Nomura, S.; Sawano, T.; Ozaki, A.; Tsubokura, M.; Hill, S.; Kanazawa, Y.; Anbe, H. Birth outcomes after the Fukushima Daiichi nuclear power plant disaster: A long-term retrospective study. Int. J. Environ. Res. Public Health 2017, 14, 542. [Google Scholar] [CrossRef]
- Wertelecki, W. Malformations in a Chornobyl-impacted region. Pediatrics 2010, 125, e836–e843. [Google Scholar] [CrossRef] [PubMed]
- Wertelecki, W.; Chambers, C.D.; Yevtushok, L.; Zymak-Zakutnya, N.; Sosyniuk, Z.; Lapchenko, S.; Ievtushok, B.; Akhmedzhanova, D.; Komov, O. Chornobyl 30 years later: Radiation, pregnancies, and developmental anomalies in Rivne, Ukraine. Eur. J. Med. Genet. 2017, 60, 2–11. [Google Scholar] [CrossRef]
- Wertelecki, W.; Yevtushok, L.; Kuznietsov, I.; Komov, O.; Lapchenko, S.; Akhmedzanova, D.; Ostapchuk, L. Chornobyl, radiation, neural tube defects, and microcephaly. Eur. J. Med. Genet. 2018, 61, 556–563. [Google Scholar] [CrossRef]
- Dolk, H.; Nichols, R. Evaluation of the impact of Chernobyl on the prevalence of congenital anomalies in 16 regions of Europe. EUROCAT Working Group. Int. J. Epidemiol. 1999, 28, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, W. Fallout from the Chernobyl nuclear disaster and congenital malformations in Europe. Arch. Environ. Health 2001, 56, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Little, J. The Chernobyl accident, congenital anomalies and other reproductive outcomes. Paediatr. Perinat. Epidemiol. 1993, 7, 121–151. [Google Scholar] [CrossRef] [PubMed]
- Cragan, J.D.; Gilboa, S.M. Including prenatal diagnoses in birth defects monitoring: Experience of the Metropolitan Atlanta Congenital Defects Program. Birth Defects Res. A Clin. Mol. Teratol. 2009, 85, 20–29. [Google Scholar] [CrossRef]
- Dolk, H.; Loane, M.; Garne, E. The prevalence of congenital anomalies in Europe. Adv. Exp. Med. Biol. 2010, 686, 349–364. [Google Scholar] [CrossRef]
- ICBDSR (International Clearinghouse for Birth Defects Surveillance and Research) Japan Center. Available online: https://icbdsr-j.jp/data.html (accessed on 13 July 2020). (In Japanese).
- Gurney, J.K.; McGlynn, K.A.; Stanley, J.; Merriman, T.; Signal, V.; Shaw, C.; Edwards, R.; Richiardi, L.; Hutson, J.; Sarfati, D. Risk factors for cryptorchidism. Nat. Rev. Urol. 2017, 14, 534–548. [Google Scholar] [CrossRef] [PubMed]
- Kojima, Y.; Yokoya, S.; Kurita, N.; Idaka, T.; Ishikawa, T.; Tanaka, H.; Ezawa, Y.; Ohto, H. Cryptorchidism after the Fukushima Daiichi Nuclear Power Plant accident:causation or coincidence? Fukushima J. Med. Sci. 2019, 65, 76–98. [Google Scholar] [CrossRef] [PubMed]
- Hirata, Y.; Shimizu, H.; Kumamaru, H.; Takamoto, S.; Motomura, N.; Miyata, H.; Okita, Y. Congenital heart disease After the Fukushima nuclear accident: The Japan cardiovascular surgery database study. J. Am. Heart Assoc. 2020, 9, e014787. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).