Updates in the Field of Submucosal Endoscopy
Abstract
1. Introduction
2. Peroral Endoscopic Myotomy
2.1. Efficacy of POEM
| Study | Patients (N) | Median Follow-Up (year) | Previous Treatment (%) | Efficacy (%) | Adverse Events (%) | Reflux (%) |
|---|---|---|---|---|---|---|
| Shiwaku et al., 2020 [15] | 1346 | 1 | 31 | 95.1 (3 m) 94.7 (1 y) | 3.7 | 14.8 |
| Shiwaku et al., 2019 [18] | 233 | 1 | 21.9 | 97.1 (3 m) 97.4 (1 y) | 10.3 | 54.2 |
| Li et al., 2018 [32] | 564 | 4.1 | 34.2 | 94.2 (1 y) 92.2 (2y) 91.1 (3 y) 88.6 (4 y) 87.1 (5 y) | 6.4 | 37.3 |
| Nabi et al., 2018 [33] | 502 | 1.8 | 48.2 | 90.9 (1 y) 86.0 (2 y) 81.2 (3 y) | 1.6 | 21.5 |
| Zhang et al., 2018 [34] | 318 | 2.3 | 40.1 | 95.7 | 2.5 | 35.8 |
| Kumbhari et al., 2017 [11] | 282 | 1 | 28.6 | 94.3 | − | 23.2 |
| Nabi et al., 2017 [16] | 423 | 1.7 | 46 | 94 (1 y) 91 (2 y) 90 (3 y) | 4.5 | 28.3 |
| Ramchandani et al., 2016 [35] | 220 | 1 | 41.3 | 94 (6 m) 92 (1 y) | 6.4 | 21.6 |
| Inoue et al., 2015 [8] | 500 | 3 | 39 | 91 (1 y) 88.5 (3 y) | 3.2 | 16.8 |
2.2. Adverse Events of POEM
3. Peroral Endoscopic Tumor Resection/Submucosal Tunnel Endoscopic Resection
4. Gastric Peroral Endoscopic Myotomy/Peroral Endoscopic Pyloromyotomy
5. Diverticular Peroral Endoscopic Myotomy/Zenker’s Peroral Endoscopic Myotomy
6. Submucosal Tunneling Biopsy
7. Endoscopic Submucosal “Tunnel” Dissection/Pocket-Creation Method
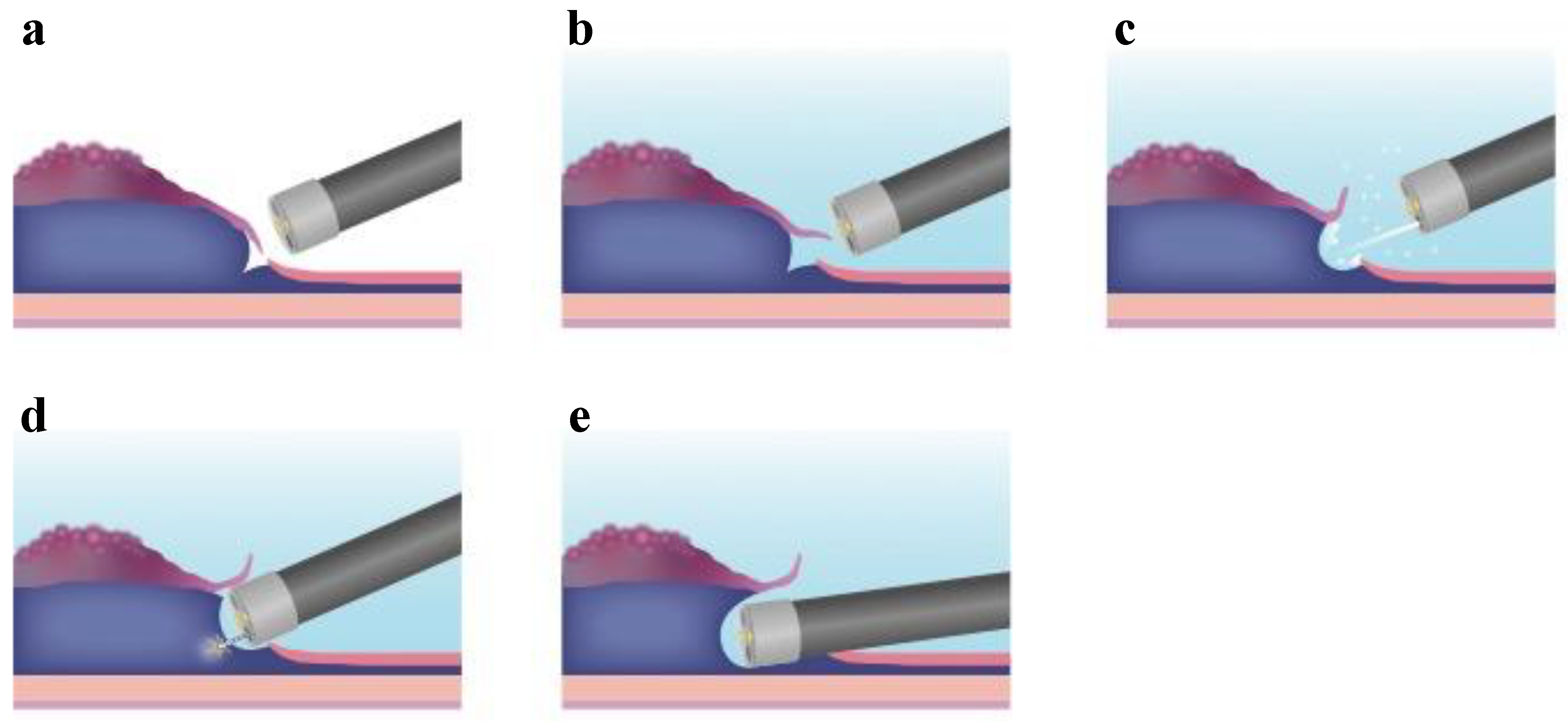
8. Solutions for Submucosal Injection
9. Conclusions
10. Expert Opinion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kalloo, A.N.; Singh, V.K.; Jagannath, S.B.; Niiyama, H.; Hill, S.L.; Vaughn, C.A.; Magee, C.A.; Kantsevoy, S.V. Flexible transgastric peritoneoscopy: A novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest. Endosc. 2004, 60, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Rao, G.V.; Reddy, D.N.; Banerjee, R. NOTES: Human experience. Gastrointest. Endosc. Clin. N. Am. 2008, 18, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Sumiyama, K.; Gostout, C.J.; Rajan, E.; Bakken, T.A.; Knipschield, M.A.; Marler, R.J. Submucosal endoscopy with mucosal flap safety valve. Gastrointest. Endosc. 2007, 65, 688–694. [Google Scholar] [CrossRef]
- Khashab, M.A.; Pasricha, P.J. Conquering the third space: Challenges and opportunities for diagnostic and therapeutic endoscopy. Gastrointest. Endosc. 2013, 77, 146–148. [Google Scholar] [CrossRef] [PubMed]
- Inoue, H.; Minami, H.; Kobayashi, Y.; Sato, Y.; Kaga, M.; Suzuki, M.; Satodate, H.; Odaka, N.; Itoh, H.; Kudo, S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010, 42, 265–271. [Google Scholar] [CrossRef]
- Schlottmann, F.; Luckett, D.J.; Fine, J.; Shaheen, N.J.; Patti, M.G. Laparoscopic heller myotomy versus peroral endoscopic myotomy (POEM) for achalasia: A systematic review and meta-analysis. Ann. Surg. 2018, 267, 451–460. [Google Scholar] [CrossRef]
- Shea, G.E.; Johnson, M.K.; Venkatesh, M.; Jolles, S.A.; Prout, T.M.; Shada, A.L.; Greenberg, J.A.; Lidor, A.O.; Funk, L.M. Long-term dysphagia resolution following POEM versus Heller myotomy for achalasia patients. Surg. Endosc. 2019, 34, 1704–1711. [Google Scholar] [CrossRef]
- Inoue, H.; Sato, H.; Ikeda, H.; Onimaru, M.; Sato, C.; Minami, H.; Yokomichi, H.; Kobayashi, Y.; Grimes, K.L.; Kudo, S.E. Per-oral endoscopic myotomy: A series of 500 patients. J. Am. Coll. Surg. 2015, 221, 256–264. [Google Scholar] [CrossRef]
- Teitelbaum, E.N.; Soper, N.J.; Santos, B.F.; Arafat, F.O.; Pandolfino, J.E.; Kahrilas, P.J.; Hirano, I.; Hungness, E.S. Symptomatic and physiologic outcomes one year after peroral esophageal myotomy (POEM) for treatment of achalasia. Surg. Endosc. 2014, 28, 3359–3365. [Google Scholar] [CrossRef]
- Shiwaku, H.; Inoue, H.; Yamashita, K.; Ohmiya, T.; Beppu, R.; Nakashima, R.; Takeno, S.; Sasaki, T.; Nimura, S.; Yamashita, Y. Peroral endoscopic myotomy for esophageal achalasia: Outcomes of the first 100 patients with short-term follow-up. Ann. Surg. 2016, 263, 82–87. [Google Scholar] [CrossRef]
- Kumbhari, V.; Familiari, P.; Bjerregaard, N.C.; Pioche, M.; Jones, E.; Ko, W.J.; Hayee, B.; Cali, A. Gastroesophageal reflux after peroral endoscopic myotomy: A multicenter case-control study. Endoscopy 2017, 49, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Inoue, H.; Shiwaku, H.; Iwakiri, K.; Onimaru, M.; Kobayashi, Y.; Minami, H.; Sato, H.; Kitano, S.; Iwakiri, R.; Omura, N.; et al. Clinical practice guidelines for peroral endoscopic myotomy. Dig. Endosc. 2018, 30, 563–579. [Google Scholar] [CrossRef] [PubMed]
- Inoue, H.; Tianle, K.M.; Ikeda, H.; Hosoya, T.; Onimaru, M.; Yoshida, A.; Minami, H.; Kudo, S.E. Peroral endoscopic myotomy for esophageal achalasia: Technique, indication, and outcomes. Thorac. Surg. Clin. 2011, 21, 519–525. [Google Scholar] [CrossRef]
- Khashab, M.A.; Messallam, A.A.; Onimaru, M.; Teitelbaum, E.N.; Ujiki, M.B.; Gitelis, M.E.; Modayil, R.J.; Hungness, E.S.; Stavropoulos, S.N.; El Zein, M.H.; et al. International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest. Endosc. 2015, 81, 1170–1177. [Google Scholar] [CrossRef] [PubMed]
- Shiwaku, H.; Inoue, H.; Onimaru, M.; Minami, H.; Sato, H.; Sato, C.; Tanaka, S.; Ogawa, R.; Okushima, N. Multicenter collaborative retrospective evaluation of peroral endoscopic myotomy for esophageal achalasia: Analysis of data from more than 1300 patients at eight facilities in Japan. Surg. Endosc. 2020, 34, 464–468. [Google Scholar] [CrossRef]
- Nabi, Z.; Ramchandani, M.; Chavan, R.; Kalapala, R.; Darisetty, S.; Rao, G.V.; Reddy, N. Peroral endoscopic myotomy for achalasia cardia: Outcomes in over 400 consecutive patients. Endosc. Int. Open 2017, 5, E331–E339. [Google Scholar]
- Ngamruengphong, S.; Inoue, H.; Chiu, P.W.Y.; Yip, H.C.; Bapaye, A.; Ujiki, M.; Patel, L.; Desai, P.N.; Hayee, B.; Haji, A.; et al. RETRACTED: Long-term outcomes of per-oral endoscopic myotomy in achalasia patients with a minimum follow-up of 2 years: An international multicenter study. Gastrointest. Endosc. 2017, 85, 927.e2–933.e2. [Google Scholar] [CrossRef]
- Shiwaku, H.; Inoue, H.; Sato, H.; Onimaru, M.; Minami, H.; Tanaka, S.; Sato, C.; Ogawa, R.; Okushima, N.; Yokomichi, H. Peroral endoscopic myotomy for achalasia: A prospective multicenter study in Japan. Gastrointest. Endosc. 2019, 91, 1037–1044. [Google Scholar] [CrossRef]
- Teitelbaum, E.N.; Dunst, C.M.; Reavis, K.M.; Sharata, A.M.; Ward, M.A.; DeMeester, S.R.; Swanström, L.L. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg. Endosc. 2018, 32, 421–427. [Google Scholar] [CrossRef]
- Kumbhari, V.; Tieu, A.H.; Onimaru, M.; El Zein, M.H.; Teitelbaum, E.N.; Ujiki, M.B.; Gitelis, M.E.; Modayil, R.J.; Hungness, E.S.; Stavropoulos, S.N.; et al. Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of type III achalasia in 75 patients: A multicenter comparative study. Endosc. Int. Open 2015, 3, E195–E201. [Google Scholar] [CrossRef]
- Hungness, E.S.; Teitelbaum, E.N.; Santos, B.F.; Arafat, F.O.; Pandolfino, J.E.; Kahrilas, P.J.; Soper, N.J. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J. Gastrointest. Surg. 2013, 17, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Bhayani, N.H.; Kurian, A.A.; Dunst, C.M.; Sharata, A.M.; Rieder, E.; Swanstrom, L.L. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann. Surg. 2014, 259, 1098–1103. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.M.; Wu, J.C.Y.; Teoh, A.Y.B.; Yip, H.C.; Ng, E.K.W.; Lau, J.Y.W.; Chiu, P.W.Y. Comparison of early outcomes and quality of life after laparoscopic Heller’s cardiomyotomy to peroral endoscopic myotomy for treatment of achalasia. Dig. Endosc. 2016, 28, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Ujiki, M.B.; Yetasook, A.K.; Zapf, M.; Linn, J.G.; Carbray, J.M.; Denham, W. Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery 2013, 154, 897–900. [Google Scholar] [CrossRef]
- Kumagai, K.; Tsai, J.A.; Thorell, A.; Lundell, L.; Håkanson, B. Per-oral endoscopic myotomy for achalasia. Are results comparable to laparoscopic Heller myotomy? Scand. J. Gastroenterol. 2015, 50, 505–512. [Google Scholar] [CrossRef]
- Ponds, F.A.; Fockens, P.; Lei, A.; Neuhaus, H.; Beyna, T.; Kandler, J.; Frieling, T.; Chiu, P.W.; Wu, J.C.; Wong, V.W.; et al. Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment-naive patients with achalasia: A randomized clinical trial. JAMA 2019, 322, 134–144. [Google Scholar] [CrossRef]
- Kuipers, T.; Ponds, F.A.; Fockens, P.; Bastiaansen, B.A.J.; Lei, A.; Oude Nijhuis, R.A.B.; Neuhaus, H.; Beyna, T.; Kandler, J.; Frieling, T.; et al. Peroral endoscopic myotomy versus pneumatic dilation in treatment-naive patients with achalasia: 5-year follow-up of a randomised controlled trial. Lancet Gastroenterol. Hepatol. 2022, 12, 1103–1111. [Google Scholar] [CrossRef]
- Aiolfi, A.; Bona, D.; Riva, C.G.; Micheletto, G.; Rausa, E.; Campanelli, G.; Olmo, G.; Bonitta, G.; Bonavina, L. Systematic review and Bayesian network meta-analysis comparing laparoscopic Heller myotomy, pneumatic dilatation, and peroral endoscopic myotomy for esophageal achalasia. J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 147–155. [Google Scholar] [CrossRef]
- Familiari, P.; Marchese, M.; Gigante, G.; Boskoski, I.; Tringali, A.; Perri, V.; Costamagna, G. Peroral endoscopic myotomy for the treatment of achalasia in children. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 794–797. [Google Scholar] [CrossRef]
- Caldaro, T.; Familiari, P.; Romeo, E.F.; Gigante, G.; Marchese, M.; Contini, A.C.I.; Di Abriola, G.F.; Cucchiara, S.; De Angelis, P.; Torroni, F.; et al. Treatment of esophageal achalasia in children: Today and tomorrow. J. Pediatr. Surg. 2015, 50, 726–730. [Google Scholar] [CrossRef]
- Lee, Y.; Brar, K.; Doumouras, A.G.; Hong, D. Peroral endoscopic myotomy (POEM) for the treatment of pediatric achalasia: A systematic review and meta-analysis. Surg. Endosc. 2019, 33, 1710–1720. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.L.; Wu, Q.N.; Zhang, X.C.; Xu, M.D.; Zhang, W.; Chen, S.Y.; Zhong, Y.S.; Zhang, Y.Q.; Chen, W.F.; Qin, W.Z.; et al. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest. Endosc. 2018, 87, 1405.e3–1412.e3. [Google Scholar] [CrossRef] [PubMed]
- Nabi, Z.; Ramchandani, M.; Chavan, R.; Tandan, M.; Kalapala, R.; Darisetty, S.; Lakhtakia, S.; Rao, G.V.; Reddy, D.N. Peroral endoscopic myotomy in treatment-naïve achalasia patients versus prior treatment failure cases. Endoscopy 2018, 50, 358–370. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Modayil, R.J.; Friedel, D.; Gurram, K.C.; Brathwaite, C.E.; Taylor, S.I.; Kollarus, M.M.; Modayil, S.; Halwan, B.; Grendell, J.H.; et al. Per-oral endoscopic myotomy in patients with or without prior Heller’s myotomy: Comparing long-term outcomes in a large U.S. single-center cohort (with videos). Gastrointest. Endosc. 2018, 87, 972–985. [Google Scholar] [CrossRef]
- Ramchandani, M.; Reddy, D.N.; Darisetty, S.; Kotla, R.; Chavan, R.; Kalpala, R.; Galasso, D.; Lakhtakia, S.; Rao, G.V. Peroral endoscopic myotomy for achalasia cardia: Treatment analysis and follow up of over 200 consecutive patients at a single center. Dig. Endosc. 2016, 28, 19–26. [Google Scholar] [CrossRef]
- Inoue, H.; Shiwaku, H.; Kobayashi, Y.; Chiu, P.W.; Hawes, R.H.; Neuhaus, H.; Costamagna, G.; Stavropoulos, S.N.; Fukami, N.; Seewald, S.; et al. Statement for gastroesophageal reflux disease after peroral endoscopic myotomy from an international multicenter experience. Esophagus 2020, 17, 3–10. [Google Scholar] [CrossRef]
- Baldaque-Silva, F.; Marques, M.; Vilas-Boas, F.; Maia, J.D.; Sá, F.; Macedo, G. New transillumination auxiliary technique for peroral endoscopic myotomy. Gastrointest. Endosc. 2014, 79, 544–545. [Google Scholar] [CrossRef]
- Grimes, K.L.; Inoue, H.; Onimaru, M.; Ikeda, H.; Tansawet, A.; Bechara, R.; Tanaka, S. Double-scope per oral endoscopic myotomy (POEM): A prospective randomized controlled trial. Surg. Endosc. 2016, 30, 1344–1351. [Google Scholar] [CrossRef]
- Miftahussurur, M.; Tandan, M.; Makmun, D.; Nabi, Z. Peroral endoscopic myotomy in a patient with achalasia cardia with prior heller’s myotomy. Case Rep. Gastroenterol. 2020, 14, 48–55. [Google Scholar] [CrossRef]
- Inoue, H.; Ikeda, H.; Hosoya, T.; Onimaru, M.; Yoshida, A.; Eleftheriadis, N.; Maselli, R.; Kudo, S. Submucosal endoscopic tumor resection for subepithelial tumors in the esophagus and cardia. Endoscopy 2012, 44, 225–230. [Google Scholar] [CrossRef]
- Xu, M.D.; Cai, M.Y.; Zhou, P.H.; Qin, X.Y.; Zhong, Y.S.; Chen, W.F.; Hu, J.W.; Zhang, Y.Q.; Ma, L.L.; Qin, W.Z.; et al. Submucosal tunneling endoscopic resection: A new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest. Endosc. 2012, 75, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.P.; Zhang, Y.; Mao, X.L.; Zhu, L.H.; Zhou, X.; Chen, J.Y. Submucosal tunneling endoscopic resection for small upper gastrointestinal subepithelial tumors originating from the muscularis propria layer. Surg. Endosc. 2014, 28, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tan, Y.; Zhou, Y.; Wang, Y.; Li, C.; Zhou, J.; Duan, T.; Zhang, J.; Liu, D. Submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors originating from the muscularis propria layer. Eur. J. Gastroenterol. Hepatol. 2015, 27, 776–780. [Google Scholar] [CrossRef]
- Chen, T.; Zhang, C.; Yao, L.Q.; Zhou, P.H.; Zhong, Y.S.; Zhang, Y.Q.; Chen, W.F.; Li, Q.L.; Cai, M.Y.; Chu, Y.; et al. Management of the complications of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors. Endoscopy 2016, 48, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Chiu, P.W.; Inoue, H.; Rösch, T. From POEM to POET: Applications and perspectives for submucosal tunnel endoscopy. Endoscopy 2016, 48, 1134–1142. [Google Scholar] [CrossRef]
- Mao, X.L.; Ye, L.P.; Zheng, H.H.; Zhou, X.B.; Zhu, L.H.; Zhang, Y. Submucosal tunneling endoscopic resection using methylene-blue guidance for cardial subepithelial tumors originating from the muscularis propria layer. Dis. Esophagus 2017, 30, 1–7. [Google Scholar] [CrossRef]
- Li, Q.Y.; Meng, Y.; Xu, Y.Y.; Zhang, Q.; Cai, J.Q.; Zheng, H.X.; Qing, H.T.; Huang, S.L.; Han, Z.L.; Li, A.M.; et al. Comparison of endoscopic submucosal tunneling dissection and thoracoscopic enucleation for the treatment of esophageal submucosal tumors. Gastrointest. Endosc. 2017, 86, 485–491. [Google Scholar] [CrossRef]
- Du, C.; Chai, N.L.; Ling-Hu, E.Q.; Li, Z.J.; Li, L.S.; Zou, J.L.; Jiang, L.; Lu, Z.S.; Meng, J.Y.; Tang, P. Submucosal tunneling endoscopic resection: An effective and safe therapy for upper gastrointestinal submucosal tumors originating from the muscularis propria layer. World J. Gastroenterol. 2019, 25, 245–257. [Google Scholar] [CrossRef]
- Chiu, P.W.Y.; Yip, H.C.; Teoh, A.Y.B.; Wong, V.W.Y.; Chan, S.M.; Wong, S.K.H.; Ng, E.K.W. Per oral endoscopic tumor (POET) resection for treatment of upper gastrointestinal subepithelial tumors. Surg. Endosc. 2019, 33, 1326–1333. [Google Scholar] [CrossRef]
- Onimaru, M.; Inoue, H.; Bechara, R.; Tanabe, M.; Abad, M.R.A.; Ueno, A.; Shimamura, Y.; Sumi, K.; Ikeda, H.; Ito, H. Clinical outcomes of per-oral endoscopic tumor resection for submucosal tumors in the esophagus and gastric cardia. Dig. Endosc. 2020, 32, 328–336. [Google Scholar] [CrossRef]
- He, Z.; Sun, C.; Zheng, Z.; Yu, Q.; Wang, T.; Chen, X.; Cao, H.; Liu, W.; Wang, B. Endoscopic submucosal dissection of large gastrointestinal stromal tumors in the esophagus and stomach. J. Gastroenterol. Hepatol. 2013, 28, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.S.; Zhang, Z.H.; Hong, Y.Y.; Li, D.J.; Lin, J.Q.; Chen, X.; Ji, F. Comparison of endoscopic submucosal dissection and surgery for the treatment of gastric submucosal tumors originating from the muscularis propria layer: A single-center study (with video). Surg. Endosc. 2016, 30, 5099–5107. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, S.N.; Modayil, R.; Friedel, D.; Brathwaite, C.E. Endoscopic full-thickness resection for GI stromal tumors. Gastrointest. Endosc. 2014, 80, 334–335. [Google Scholar] [CrossRef]
- Goto, O.; Uraoka, T.; Horii, J.; Yahagi, N. Expanding indications for ESD: Submucosal disease (SMT/carcinoid tumors). Gastrointest. Endosc. Clin. N. Am. 2014, 24, 169–181. [Google Scholar] [CrossRef]
- Lv, X.H.; Wang, C.H.; Xie, Y. Efficacy and safety of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors: A systematic review and meta-analysis. Surg. Endosc. 2017, 31, 49–63. [Google Scholar] [CrossRef]
- Zhang, M.; Wu, S.; Xu, H. Comparison between submucosal tunneling endoscopic resection (STER) and other resection modules for esophageal muscularis propria tumors: A retrospective study. Med. Sci. Monit. 2019, 25, 4560–4568. [Google Scholar] [CrossRef]
- Chen, T.; Lin, Z.W.; Zhang, Y.Q.; Chen, W.F.; Zhong, Y.S.; Wang, Q.; Yao, L.Q.; Zhou, P.H.; Xu, M.D. Submucosal tunneling endoscopic resection vs thoracoscopic enucleation for large submucosal tumors in the esophagus and the esophagogastric junction. J. Am. Coll. Surg. 2017, 225, 806–816. [Google Scholar] [CrossRef]
- Tan, Y.; Tang, X.; Guo, T.; Peng, D.; Tang, Y.; Duan, T.; Wang, X.; Lv, L.; Huo, J.; Liu, D. Comparison between submucosal tunneling endoscopic resection and endoscopic full-thickness resection for gastric stromal tumors originating from the muscularis propria layer. Surg. Endosc. 2017, 31, 3376–3382. [Google Scholar] [CrossRef]
- Li, Z.; Gao, Y.; Chai, N.; Xiong, Y.; Ma, L.; Zhang, W.; Du, C.; Linghu, E. Effect of submucosal tunneling endoscopic resection for submucosal tumors at esophagogastric junction and risk factors for failure of en bloc resection. Surg. Endosc. 2018, 32, 1326–1335. [Google Scholar] [CrossRef]
- Camilleri, M.; Parkman, H.P.; Shafi, M.A.; Abell, T.L.; Gerson, L. Clinical guideline: Management of gastroparesis. Am. J. Gastroenterol. 2013, 108, 18–37. [Google Scholar] [CrossRef]
- Soykan, I.; Sivri, B.; Sarosiek, I.; Kiernan, B.; Mccallum, R.W. Demography, clinical characteristics, psychological and abuse profiles, treatment, and long-term follow-up of patients with gastroparesis. Dig. Dis. Sci. 1998, 43, 2398–2404. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.A.; Nikitina, Y.; Kedar, A.; Lahr, C.J.; Helling, T.S.; Abell, T.L. Long-term effects of gastric stimulation on gastric electrical physiology. J. Gastrointest. Surg. 2013, 17, 50–55. [Google Scholar] [CrossRef]
- Arts, J.; Holvoet, L.; Caenepeel, P.; Bisschops, R.; Sifrim, D.; Verbeke, K.; Janssens, J.; Tack, J. Clinical trial: A randomized controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment. Pharmacol. Ther. 2007, 26, 1251–1258. [Google Scholar] [CrossRef] [PubMed]
- Friedenberg, F.K.; Palit, A.; Parkman, H.P.; Hanlon, A.; Nelson, D.B. Botulinum toxin A for the treatment of delayed gastric emptying. Am. J. Gastroenterol. 2008, 103, 416–423. [Google Scholar] [CrossRef]
- Kawai, M.; Peretta, S.; Burckhardt, O.; Dallemagne, B.; Marescaux, J.; Tanigawa, N. Endoscopic pyloromyotomy: A new concept of minimally invasive surgery for pyloric stenosis. Endoscopy 2012, 44, 169–173. [Google Scholar] [CrossRef]
- Khashab, M.A.; Stein, E.; Clarke, J.O.; Saxena, P.; Kumbhari, V.; Roland, B.C.; Kalloo, A.N.; Stavropoulos, S.; Pasricha, P.; Inoue, H. Gastric peroral endoscopic myotomy for refractory gastroparesis: First human endoscopic pyloromyotomy (with video). Gastrointest. Endosc. 2013, 78, 764–768. [Google Scholar] [CrossRef] [PubMed]
- Mekaroonkamol, P.; Dacha, S.; Patel, V.; Li, B.; Luo, H.; Shen, S.; Chen, H.; Cai, Q. Outcomes of per oral endoscopic pyloromyotomy in the United States. Gastrointest. Endosc. Clin. N. Am. 2019, 29, 151–160. [Google Scholar] [CrossRef]
- Spadaccini, M.; Maselli, R.; Chandrasekar, V.T.; Anderloni, A.; Carrara, S.; Galtieri, P.A.; Di Leo, M.; Fugazza, A.; Pellegatta, G.; Colombo, M.; et al. Gastric peroral endoscopic pyloromyotomy for refractory gastroparesis: A systematic review of early outcomes with pooled analysis. Gastrointest. Endosc. 2020, 91, 746–752. [Google Scholar] [CrossRef]
- Malik, Z.; Kataria, R.; Modayil, R.; Ehrlich, A.C.; Schey, R.; Parkman, H.P.; Stavropoulos, S.N. Gastric per oral endoscopic myotomy (G-POEM) for the treatment of refractory gastroparesis: Early experience. Dig. Dis. Sci. 2018, 63, 2405–2412. [Google Scholar] [CrossRef]
- Rodriguez, J.H.; Haskins, I.N.; Strong, A.T.; Plescia, R.L.; Allemang, M.T.; Butler, R.S.; Cline, M.S.; El-Hayek, K.; Ponsky, J.L.; Kroh, M.D. Per oral endoscopic pyloromyotomy for refractory gastroparesis: Initial results from a single institution. Surg. Endosc. 2017, 31, 5381–5388. [Google Scholar] [CrossRef]
- Kahaleh, M.; Gonzalez, J.M.; Xu, M.M.; Andalib, I.; Gaidhane, M.; Tyberg, A.; Saumoy, M.; Marchena, A.J.B.; Barthet, M. Gastric peroral endoscopic myotomy for the treatment of refractory gastroparesis: A multicenter international experience. Endoscopy 2018, 50, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Martinek, J.; Hustak, R.; Mares, J.; Vackova, Z.; Spicak, J.; Kieslichova, E.; Buncova, M.; Pohl, D.; Amin, S.; Tack, J. Endoscopic pyloromyotomy for the treatment of severe and refractory gastroparesis: A pilot, randomised, sham-controlled trial. Gut 2022, 71, 2170–2178. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.L.; Anthony, A.A.; Fosh, B.G.; Finch, J.G.; Maddern, G.J. Esophageal diverticula. Br. J. Surg. 2001, 88, 629–642. [Google Scholar] [CrossRef] [PubMed]
- Aiolfi, A.; Scolari, F.; Saino, G.; Bonavina, L. Current status of minimally invasive endoscopic management for Zenker diverticulum. World J. Gastrointest. Endosc. 2015, 7, 87–93. [Google Scholar] [CrossRef]
- Albers, D.V.; Kondo, A.; Bernardo, W.M.; Sakai, P.; Moura, R.N.; Silva, G.L.R.; Ide, E.; Tomishige, T.; de Moura, E.G. Endoscopic versus surgical approach in the treatment of Zenker’s diverticulum: Systematic review and meta-analysis. Endosc. Int. Open 2016, 4, E678–E686. [Google Scholar] [CrossRef]
- Li, Q.L.; Chen, W.F.; Zhang, X.C.; Cai, M.Y.; Zhang, Y.Q.; Hu, J.W.; He, M.J.; Yao, L.Q.; Zhou, P.H.; Xu, M.D. Submucosal tunneling endoscopic septum division: A novel technique for treating Zenker’s diverticulum. Gastroenterology 2016, 151, 1071–1074. [Google Scholar] [CrossRef]
- Hernández Mondragón, O.V.; Solórzano Pineda, M.O.; Blancas Valencia, J.M. Zenkerʼs diverticulum: Submucosal tunneling endoscopic septum division (Z-POEM). Dig. Endosc. 2018, 30, 124. [Google Scholar] [CrossRef]
- Costamagna, G.; Iacopini, F.; Bizzotto, A.; Familiari, P.; Tringali, A.; Perri, V.; Bella, A. Prognostic variables for the clinical success of flexible endoscopic septotomy of Zenker’s diverticulum. Gastrointest. Endosc. 2016, 83, 765–773. [Google Scholar] [CrossRef]
- Yang, J.; Novak, S.; Ujiki, M.; Hernández, Ó.; Desai, P.; Benias, P.; Lee, D.; Chang, K.; Brieau, B.; Barret, M.; et al. An international study on the use of peroral endoscopic myotomy in the management of Zenker’s diverticulum. Gastrointest. Endosc. 2020, 91, 163–168. [Google Scholar] [CrossRef]
- Spadaccini, M.; Maselli, R.; Chandrasekar, V.T.; Patel, H.K.; Fugazza, A.; Galtieri, P.A.; Pellegatta, G.; Attardo, S.; Carrara, S.; Anderloni, A.; et al. Submucosal tunnelling techniques for Zenker’s diverticulum: A systematic review of early outcomes with pooled analysis. Eur. J. Gastroenterol. Hepatol. 2021, 33, e78–e83. [Google Scholar] [CrossRef]
- Yang, J.; Zeng, X.; Yuan, X.; Chang, K.; Sanaei, O.; Fayad, L.; Kumbhari, V.; Singh, V.; Kalloo, A.N.; Hu, B.; et al. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: The first multicenter D-POEM experience. Endoscopy 2019, 51, 346–349. [Google Scholar] [CrossRef] [PubMed]
- Mandavdhare, H.S.; Samanta, J.; Jafra, A.; Singh, H.; Gupta, P. Recurrence after Zenker’s peroral endoscopic myotomy despite complete septotomy: How far to go with myotomy on the esophageal side. VideoGIE 2022, 7, 350–352. [Google Scholar] [CrossRef] [PubMed]
- Huberty, V.; El Bacha, S.; Blero, D.; Le Moine, O.; Hassid, S.; Devière, J. Endoscopic treatment for Zenker’s diverticulum: Long-term results (with video). Gastrointest. Endosc. 2013, 77, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Kobara, H.; Mori, H.; Rafiq, K.; Fujihara, S.; Nishiyama, N.; Ayaki, M.; Yachida, T.; Matsunaga, T.; Tani, J.; Miyoshi, H.; et al. Submucosal tunneling techniques: Current perspectives. Clin. Exp. Gastroenterol. 2014, 7, 67–74. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kobara, H.; Mori, H.; Nishimoto, N.; Fujihara, S.; Nishiyama, N.; Ayaki, M.; Yachida, T.; Matsunaga, T.; Chiyo, T.; Kobayashi, N.; et al. Comparison of submucosal tunneling biopsy versus EUS-guided FNA for gastric subepithelial lesions: A prospective study with crossover design. Endosc. Int. Open 2017, 5, E695–E705. [Google Scholar] [CrossRef] [PubMed]
- Smirnov, A.A.; Kiriltseva, M.M.; Burakov, A.N.; Maksimov, M.V.; Botina, A.V.; Saadulaeva, M.M.; Konkina, N.V. Submucosal tunneling muscle biopsy for esophageal motility disorders: A case report. Clin. Endosc. 2019, 53, 370–373. [Google Scholar] [CrossRef] [PubMed]
- Rajan, E.; Gostout, C.J.; Lurken, M.S.; Talley, N.J.; Locke, G.R.; Szarka, L.A.; Sumiyama, K.; Bakken, T.A.; Stoltz, G.J.; Knipschield, M.A. Endoscopic “no hole” full-thickness biopsy of the stomach to detect myenteric ganglia. Gastrointest. Endosc. 2008, 68, 301–307. [Google Scholar] [CrossRef]
- Rajan, E.; Gostout, C.J.; Song, L.M.W.K.; Szarka, L.A.; Kashyap, P.C.; Smyrk, T.C.; Bingener, J.; Deters, J.L.; Knipschield, M.A.; Bernard, C.E.; et al. Innovative gastric endoscopic muscle biopsy to identify all cell types, including myenteric neurons and interstitial cells of Cajal in patients with idiopathic gastroparesis: A feasibility study (with video). Gastrointest. Endosc. 2016, 84, 512–517. [Google Scholar] [CrossRef]
- Blackstein, M.E.; Blay, J.Y.; Corless, C.; Driman, D.K.; Riddell, R.; Soulières, D.; Swallow, C.J.; Verma, S. Gastrointestinal stromal tumours: Consensus statement on diagnosis and treatment. Can. J. Gastroenterol. 2006, 20, 157–163. [Google Scholar] [CrossRef]
- Nishida, T.; Hirota, S.; Yanagisawa, A.; Sugino, Y.; Minami, M.; Yamamura, Y.; Otani, Y.; Shimada, Y.; Takahashi, F.; Kubota, T. Clinical practice guidelines for gastrointestinal stromal tumor (GIST) in Japan: English version. Int. J. Clin. Oncol. 2008, 13, 416–430. [Google Scholar] [CrossRef]
- Zhang, X.C.; Li, Q.L.; Yu, Y.F.; Yao, L.Q.; Xu, M.D.; Zhang, Y.Q.; Zhong, Y.S.; Chen, W.F.; Zhou, P.H. Diagnostic efficacy of endoscopic ultrasound-guided needle sampling for upper gastrointestinal subepithelial lesions: A meta-analysis. Surg. Endosc. 2016, 30, 2431–2441. [Google Scholar] [CrossRef] [PubMed]
- Linghu, E. Therapeutics of Digestive Endoscopic Tunnel Technique; Springer: Berlin, Germany, 2014. [Google Scholar]
- Linghu, E.; Li, H.; Huang, Q.; Wang, X.; Du, H.; Meng, J.; Kong, J. Using tunnel technology dissecting long circumferential lesions of esophagus. China Contin. Med. Educ. 2011, 3, 69–71. [Google Scholar]
- Hayashi, Y.; Sunada, K.; Takahashi, H.; Shinhata, H.; Lefor, A.T.; Tanaka, A.; Yamamoto, H. Pocket-creation method of endoscopic submucosal dissection to achieve en bloc resection of giant colorectal subpedunculated neoplastic lesions. Endoscopy 2014, 46, E421–E422. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Ma, B.; Gong, S.; Zhang, X.; Li, W. Endoscopic submucosal tunnel dissection for superficial esophageal neoplastic lesions: A meta-analysis. Surg. Endosc. 2020, 34, 1214–1223. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Cai, H.; Zhao, X.; Lu, X.; Liu, M.; Lv, W.; Liu, Z.; Wu, K.; Han, Y. Efficacy and safety of endoscopic submucosal tunnel dissection for superficial esophageal squamous cell carcinoma: A propensity score matching analysis. Gastrointest. Endosc. 2017, 86, 831–838. [Google Scholar] [CrossRef]
- Takezawa, T.; Hayashi, Y.; Shinozaki, S.; Sagara, Y.; Okada, M.; Kobayashi, Y.; Sakamoto, H.; Miura, Y.; Sunada, K.; Lefor, A.K.; et al. The pocket-creation method facilitates colonic endoscopic submucosal dissection (with video). Gastrointest. Endosc. 2019, 89, 1045–1053. [Google Scholar] [CrossRef]
- Yoshida, N.; Naito, Y.; Yasuda, R.; Murakami, T.; Hirose, R.; Ogiso, K.; Inada, Y.; Konishi, H.; Rani, R.A.; Kishimoto, M.; et al. The efficacy of the pocket-creation method for cases with severe fibrosis in colorectal endoscopic submucosal dissection. Endosc. Int. Open 2018, 6, E975–E983. [Google Scholar]
- Harada, H.; Nakahara, R.; Murakami, D.; Suehiro, S.; Ujihara, T.; Sagami, R.; Katsuyama, Y.; Hayasaka, K.; Amano, Y. Saline-pocket endoscopic submucosal dissection for superficial colorectal neoplasms: A randomized controlled trial (with video). Gastrointest. Endosc. 2019, 90, 278–287. [Google Scholar] [CrossRef]
- Yahagi, N.; Nishizawa, T.; Sasaki, M.; Ochiai, Y.; Uraoka, T. Water pressure method for duodenal endoscopic submucosal dissection. Endoscopy 2017, 49, E227–E228. [Google Scholar] [CrossRef]
- Zhang, X.; Shi, D.; Yu, Z.; Li, R.; Chen, W.; Bai, F.; Wu, X.; Cheng, C.; Shi, R.; Liu, P. A multicenter retrospective study of endoscopic submucosal tunnel dissection for large lesser gastric curvature superficial neoplasms. Surg. Endosc. 2019, 33, 1910–1919. [Google Scholar] [CrossRef]
- Zhang, W.; Zhai, Y.; Chai, N.; Linghu, E.; Lu, Z.; Li, H.; Feng, X. Endoscopic submucosal tunnel dissection and endoscopic submucosal dissection for large superficial esophageal squamous cell neoplasm: Efficacy and safety study to guide future practice. Surg. Endosc. 2018, 32, 2814–2821. [Google Scholar] [CrossRef] [PubMed]
- Harada, H.; Murakami, D.; Suehiro, S.; Nakahara, R.; Ujihara, T.; Sagami, R.; Katsuyama, Y.; Hayasaka, K.; Amano, Y. Water-pocket endoscopic submucosal dissection for superficial gastric neoplasms (with video). Gastrointest. Endosc. 2018, 88, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, H.; Hayashi, Y.; Miura, Y.; Shinozaki, S.; Takahashi, H.; Fukuda, H.; Okada, M.; Ino, Y.; Takezawa, T.; Sunada, K.; et al. Pocket-creation method facilitates endoscopic submucosal dissection of colorectal laterally spreading tumors, non-granular type. Endosc. Int. Open 2017, 5, E123–E129. [Google Scholar] [CrossRef]
- Kanamori, A.; Nakano, M.; Kondo, M.; Tanaka, T.; Abe, K.; Suzuki, T.; Kino, H.; Kaneko, Y.; Tsuchida, C.; Tsuchida, K.; et al. Clinical effectiveness of the pocket-creation method for colorectal endoscopic submucosal dissection. Endosc. Int. Open 2017, 12, E1299–E1305. [Google Scholar] [CrossRef] [PubMed]

| Study | Patients (N) | Location | Size (Range) (mm) | En Bloc Resection Rate (%) | Adverse Events (%) | Recurrence (%) | Pathological Diagnosis |
|---|---|---|---|---|---|---|---|
| Du et al., 2019 [48] | 165 | Esophagus: 106 Cardia: 59 | 20.0 (5.0–80.0) | 77.6 | 21.2 | 0 | Leiomyoma: 157 GIST: 3 Other: 5 |
| Li et al., 2017 [47] | 74 | Esophagus: 74 | 18.9 | 98.6 | 9.5 | 2.7 | Leiomyoma: 67 GIST: 7 |
| Mao et al., 2017 [46] | 56 | Esophagus: 18 Stomach: 38 | 18 (10–32) | 100 | 15.3 | 0 | Leiomyoma: 45 GIST: 10 Other: 1 |
| Chen et al., 2016 [44] | 290 | Esophagus: 199 Esophagogastric junction: 68 Stomach: 23 | 21 (10–70) | 89.3 | 23.4 | − | Leiomyoma: 226 GIST: 53 Other: 11 |
| Wang et al., 2015 [43] | 80 (tumors: 83) | Esophagus: 67 Cardia: 16 | 23.2 (10–55) | 97.6 | 8.75 | 0 | Leiomyoma: 68 GIST: 15 |
| Ye et al., 2014 [42] | 85 | Esophagus: 60 Cardia: 16 Stomach: 9 | 19.2 (10–30) | 100 | 9.4 | 0 | Leiomyoma: 65 GIST: 19 Other: 1 |
| Onimaru et al., 2020 [50] | 47 | Esophagus: 31 Cardia: 16 | 25.7 | 91.9 | 4.7 | 0 | Leiomyoma: 34 GIST: 6 Other: 7 |
| Chiu et al., 2019 [49] | 51 | Esophagus: 11 Stomach: 39 Duodenum: 1 | 20.71 | 94.1 | 4 | 1.96 | Leiomyoma: 20 GIST: 15 Other: 16 |
| Study | Method | Patients Study/ESD (N) | Location | Specimen Size Study/ESD (mm) | Specimen Area Study/ESD (mm2) | Procedure Time (Study/ESD) (min) | Dissection Speed Study/ESD (mm2/min) | En Bloc Resection Rate Study/ESD (%) | Adverse Events Study/ESD (%) |
|---|---|---|---|---|---|---|---|---|---|
| Zhang et al., 2019 [101] | ESTD | 32/55 | Stomach | − | 1573.0/930.1 (p < 0.01) | 87.3/136.7 (p < 0.01) | 18.0/7.8 (p < 0.01) | 100/87.3 (p = 0.035) | 59.4/100 (p < 0.01) |
| Zhang et al., 2018 [102] | ESTD | 52/98 | Esophagus | 15.37/12.95 | − | 93.21/92.39 | 21.54/16.10 (p = 0.002) | 96.15/88.78 | 9.62/8.16 |
| Huang et al., 2017 [96] | ESTD | 38/38 | Esophagus | 39.0/36.0 | − | 38.0/48.0 (p = 0.006) | 23/17 (p < 0.001) | 100/100 | 0/7.9 |
| Harada et al., 2019 [99] | PCM | 46/45 | Colorectum | 32.5/34.0 | − | 29.5/41.0 (p < 0.001) | 20.1/16.3 (p < 0.001) | 100/100 | 8.7/8.9 |
| Takezawa et al., 2019 [97] | PCM | 280/263 | Colorectum | 35.3/35.7 | − | 69.5/78.7 | 23.5/20.9 (p < 0.001) | 100/96 (p < 0.001) | 3.9/4.9 |
| Harada et al., 2018 [103] | PCM | 48/48 | Stomach | − | 34.0/32.5 | 27.5/41.0 (p < 0.001) | 22.5/17.3 (p < 0.001) | 100/100 | 8.3/6.3 |
| Sakamoto et al., 2017 [104] | PCM | 73/53 | Colorectum | 27/25 | − | − | 19/14 (p = 0.03) | 100/92 (p = 0.03) | 1.4/4.1 |
| Kanamori et al., 2017 [105] | PCM | 47/49 | Colorectum | 26/30 | − | 77/85 | 14.3/11.8 | 100/88 (p = 0.015) | 10.6/24.5 (p = 0.018) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maehata, T.; Sato, Y.; Nakamoto, Y.; Kato, M.; Kawashima, A.; Kiyokawa, H.; Yasuda, H.; Yamamoto, H.; Tateishi, K. Updates in the Field of Submucosal Endoscopy. Life 2023, 13, 104. https://doi.org/10.3390/life13010104
Maehata T, Sato Y, Nakamoto Y, Kato M, Kawashima A, Kiyokawa H, Yasuda H, Yamamoto H, Tateishi K. Updates in the Field of Submucosal Endoscopy. Life. 2023; 13(1):104. https://doi.org/10.3390/life13010104
Chicago/Turabian StyleMaehata, Tadateru, Yoshinori Sato, Yusuke Nakamoto, Masaki Kato, Akiyo Kawashima, Hirofumi Kiyokawa, Hiroshi Yasuda, Hiroyuki Yamamoto, and Keisuke Tateishi. 2023. "Updates in the Field of Submucosal Endoscopy" Life 13, no. 1: 104. https://doi.org/10.3390/life13010104
APA StyleMaehata, T., Sato, Y., Nakamoto, Y., Kato, M., Kawashima, A., Kiyokawa, H., Yasuda, H., Yamamoto, H., & Tateishi, K. (2023). Updates in the Field of Submucosal Endoscopy. Life, 13(1), 104. https://doi.org/10.3390/life13010104








