Dental Prosthesis in Esophagus: A Right Cervicotomic Approach
Abstract
1. Introduction
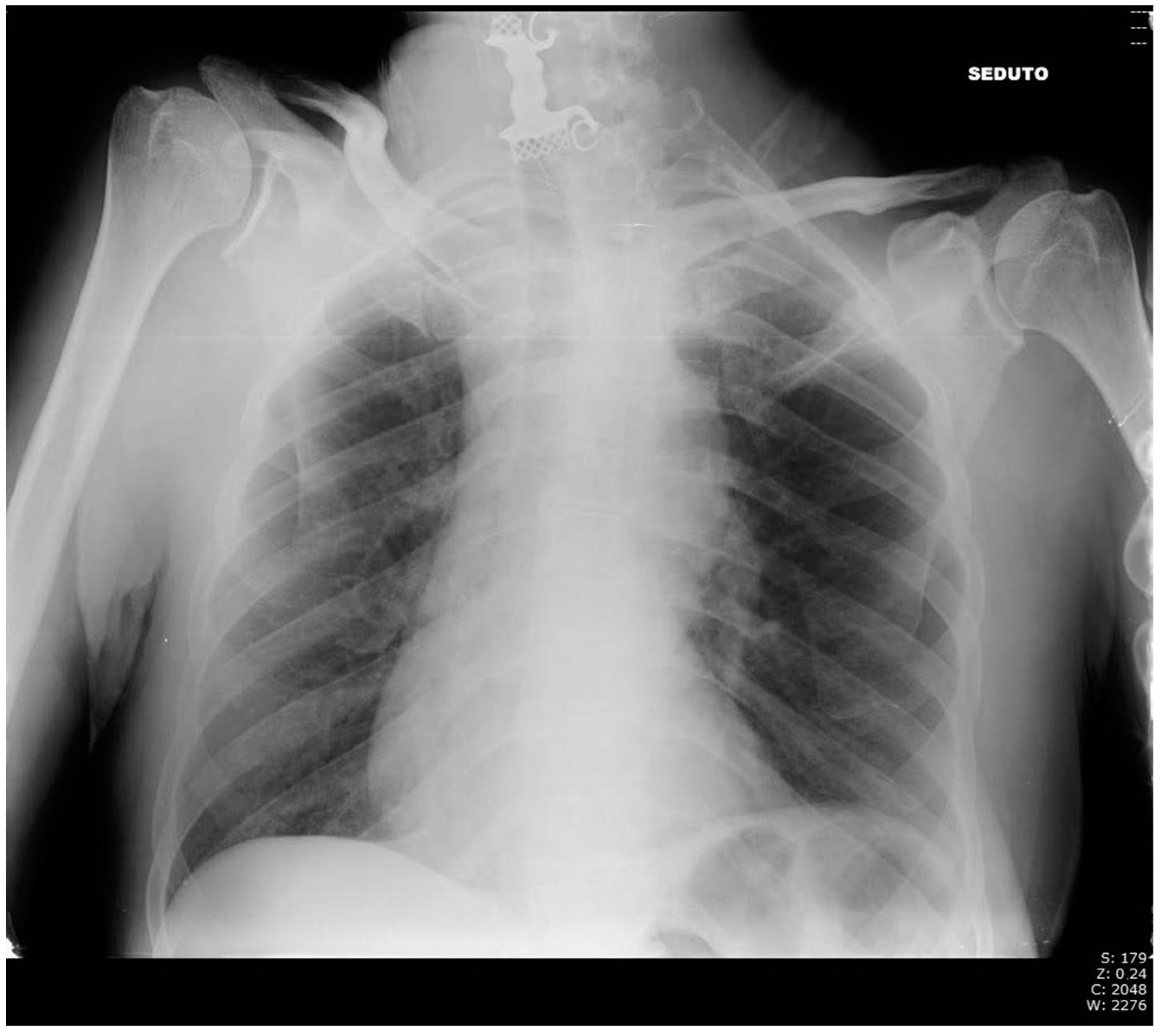
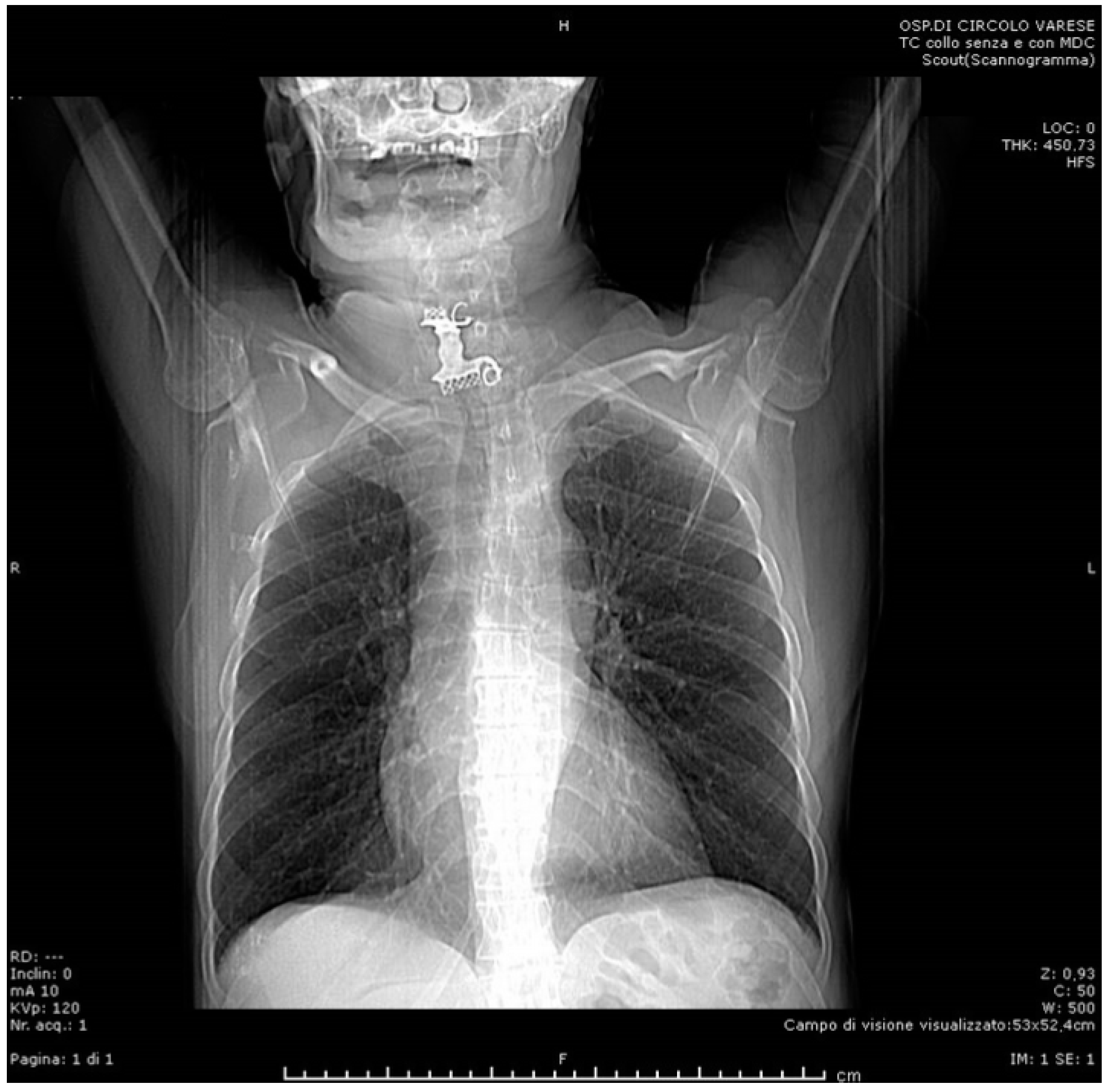
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, S.Y.; Park, B.; Kong, I.G.; Choi, H.G. Analysis of ingested foreign bodies according to age, type and location: A retrospective observational study. Clin. Otolaryngol. 2016, 41, 640–645. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, A.; Hsiehchen, D.; Layne, S.; Ginsberg, G.G.; Keo, T. Trends and clinical features of intentional and accidental adult foreign body ingestions in the United States, 2000 to 2017. Gastrointest. Endosc. 2019, 91, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Zong, Y.; Zhao, H.; Sun, C.; Ji, M.; Wu, Y.; Zhang, S.; Wang, Y. Differences between intentional and accidental ingestion of foreign body in China. BMC Gastroenterol. 2020, 20, 90. [Google Scholar] [CrossRef] [PubMed]
- Ambe, P.; Weber, S.A.; Schauer, M.; Knoefel, W.T. Swallowed Foreign Bodies in Adults. Dtsch. Arztebl. Int. 2012, 109, 869–875. [Google Scholar] [CrossRef]
- Webb, W.A. Management of foreign bodies of the upper gastrointestinal tract: Update. Gastrointest. Endosc. 1995, 41, 39–51. [Google Scholar] [CrossRef]
- Hong, K.H.; Kim, Y.J.; Kim, J.H.; Chun, S.W.; Kim, H.M.; Cho, J.H. Risk factors for complications associated with upper gastrointestinal foreign bodies. World J. Gastroenterol. 2015, 21, 8125–8131. [Google Scholar] [CrossRef]
- Smith, M.T.; Wong, R.K.H. Esophageal foreign bodies: Types and techniques for removal. Curr. Treat. Options Gastroenterol. 2006, 9, 75–84. [Google Scholar] [CrossRef]
- Wang, X.; Zhao, J.; Jiao, Y.; Wang, X.; Jiang, D. Upper gastrointestinal foreign bodies in adults: A systematic review. Am. J. Emerg. Med. 2021, 50, 136–141. [Google Scholar] [CrossRef]
- Birk, M.; Bauerfeind, P.; Deprez, P.H.; Häfner, M.; Hartmann, D.; Hassan, C.; Hucl, T.; Lesur, G.; Aabakken, L.; Meining, A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 489–496. [Google Scholar] [CrossRef]
- Cianci, P.; Tartaglia, N.; Altamura, A.; Di Lascia, A.; Fersini, A.; Neri, V.; Ambrosi, A. Cervical Esophagotomy for Foreign Body Extraction: A Case Report and Extensive Literature Review of the Last 20 Years. Am. J. Case Rep. 2018, 19, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Vallböhmer, D.; Hölscher, A.H.; Hölscher, M.; Bludau, M.; Gutschow, C.; Stippel, D.; Bollschweiler, E.; Schröder, W. Options in the management of esophageal perforation: Analysis over a 12-year period. Dis. Esophagus 2010, 23, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, T.; Hokama, N.; Kubo, N.; Ishiguro, T.; Sakimoto, T.; Ishibashi, K.; Kato, H.; Kuwano, H.; Oohata, A.; Kikuchi, S.; et al. Management of esophageal foreign bodies: Experience of 90 cases. Esophagus 2009, 6, 155–159. [Google Scholar] [CrossRef]
- Singh, B.; Har-El, G.; Kantu, M.; Lucente, F.E. Complications Associated with 327 Foreign Bodies of the Pharynx, Larynx, and Esophagus. Ann. Otol. Rhinol. Laryngol. 1997, 106, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Foley, M.J.; Ghahremani, G.G.; Rogers, L.F. Reappraisal of contrast media used to detect upper gastrointestinal perforations: Comparison of ionic water-soluble media with barium sulfate. Radiology 1982, 144, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Durand-Fontanier, S.; Valleix, D. Anatomia Chirurgica Dell’esofago; Tecniche Chirurgiche-Addominale; EMC (Elsevier Masson SAS): Paris, France, 2007; pp. 40–170. [Google Scholar]
- Hachimi-Idrissi, S.; Corne, L.; Vandenplas, Y. Management of ingested foreign bodies in childhood: Our experience and review of the literature. Eur. J. Emerg. Med. 1998, 5, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Tam, P. Foreign-body ingestion in children: Experience with 1,265 cases. J. Pediatr. Surg. 1999, 34, 1472–1476. [Google Scholar] [CrossRef]
- Abdullah, B.J.J.; Teong, L.K.; Mahadevan, J.; Jalaludin, A. Dental prosthesis ingested and impacted in the esophagus and orolaryn-gopharynx. J. Otolaryngol. 1998, 27, 190–194. [Google Scholar]
- Aiolfi, A.; Ferrari, D.; Riva, C.G.; Toti, F.; Bonitta, G.; Bonavina, L. Esophageal foreign bodies in adults: Systematic review of the literature. Scand. J. Gastroenterol. 2018, 53, 1171–1178. [Google Scholar] [CrossRef]
- Mosca, S.; Manes, G.; Martino, R.; Amitrano, L.; Bottino, V.; Bove, A.; Camera, A.; De Nucci, C.; Di Costanzo, G.; Guardascione, M.; et al. Endoscopic Management of Foreign Bodies in the Upper Gastrointestinal Tract: Report on a Series of 414 Adult Patients. Endoscopy 2001, 33, 692–696. [Google Scholar] [CrossRef]
- Brinster, C.J.; Singhal, S.; Lee, L.; Marshall, M.; Kaiser, L.R.; Kucharczuk, J.C. Evolving options in the management of esophageal perforation. Ann. Thorac. Surg. 2004, 77, 1475–1483. [Google Scholar] [CrossRef]
- Loh, K.S.; Tan, L.K.S.; Smith, J.D.; Yeoh, K.H.; Dong, F. Complications of Foreign Bodies in the Esophagus. Otolaryngol. Neck Surg. 2000, 123, 613–616. [Google Scholar] [CrossRef]
- Hung, C.-W.; Hung, S.-C.; Lee, C.J.; Lee, W.-H.; Wu, K.H. Risk Factors for Complications after a Foreign Body is Retained in the Esophagus. J. Emerg. Med. 2012, 43, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Karthikeyan, R.; Chandramohan, S.M.; Harikrishnan, S.; Vigneshwaran, V.B.; Singh, B. Lost Denture Found in Esophagus After a Decade: A Rare Case Report. Cureus 2020, 12, e8042. [Google Scholar] [CrossRef]
- Mughal, Z.; Charlton, A.R.; Dwivedi, R.; Natesh, B. Impacted denture in the oesophagus: Review of the literature and its management. BMJ Case Rep. 2019, 12, e229655. [Google Scholar] [CrossRef]
- Hashmi, S.; Walter, J.; Smith, W.; Latis, S. Swallowed partial dentures. J. R. Soc. Med. 2004, 97, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Tokar, B.; Cevik, A.A. Ilhan H: Ingested gastrointestinal foreign bodies: Predisposing factors for complications in children having surgical or endoscopic removal. Pediatr. Surg. Int. 2007, 23, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Liu, J.; Li, J.; Hu, J.; Yu, F.; Li, S.; Yang, X. Diagnosis and treatment of 32 cases with aortoesophageal fistula due to esophageal foreign body. Laryngoscope 2011, 121, 267–272. [Google Scholar] [CrossRef]
- Liu, Y.C.; Zhou, S.H.; Ling, L. Value of helical computed tomography in the early diagnosis of esophageal foreign bodies in adults. Am. J. Emerg. Med. 2013, 31, 1328–1332. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, H.; Passali, G.C.; Gregori, D.; Chinski, A.; Tiscornia, C.; Botto, H.; Nieto, M.; Zanetta, A.; Passali, D.; Cuestas, G. Management of foreign bodies in the airway and oesophagus. Int. J. Pediatr. Otorhinolaryngol. 2012, 76 (Suppl. 1), S84–S91. [Google Scholar] [CrossRef]
- Pinto, A.; Muzj, C.; Gagliardi, N.; Pinto, F.; Setola, F.R.; Scaglione, M.; Romano, L. Role of imaging in the assessment of impacted foreign bodies in the hypopharynx and cervical esophagus. Semin. Ultrasound CT MRI 2012, 33, 463–470. [Google Scholar] [CrossRef]
- Berreta, J.; Kociak, D.; Ferro, D.; Corti, R.; Balducci, A.; Marty, P.F. Mediastinis related to esophagogastric disease and injury. Warning clinical signs and inde-pendent predictors of intrahospitalary survival. Acta Gastroenterol. Latinoam. 2010, 40, 32–39. [Google Scholar]
- Chirica, M.; Kelly, M.D.; Siboni, S.; Aiolfi, A.; Riva, C.G.; Asti, E.; Ferrari, D.; Leppäniemi, A.; Broek, R.P.G.T.; Brichon, P.Y.; et al. Esophageal emergencies: WSES guidelines. World J. Emerg. Surg. 2019, 14, 26. [Google Scholar] [CrossRef] [PubMed]
- Saroul, N.; Dissard, A.; Gilain, L. Corpi estranei esofagei. EMC-Otorinolaringoiatria 2016, 15, 1–9. [Google Scholar] [CrossRef]
- Gmeiner, D.; Von Rahden, B.H.A.; Meco, C.; Hutter, J.; Oberascher, G.; Stein, H.J. Flexible versus rigid endoscopy for treatment of foreign body impaction in the esophagus. Surg. Endosc. 2007, 21, 2026–2029. [Google Scholar] [CrossRef] [PubMed]
- Popel, J.; El-Hakim, H.; El-Matary, W. Esophageal foreign body extraction in children: Flexible versus rigid endoscopy. Surg. Endosc. 2010, 25, 919–922. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-C.; Yan, X.-E.; Zhou, L.-Y.; Lin, S.-R.; Wang, Y. Therapeutic Effect of Esophageal Foreign Body Extraction Management: Flexible versus Rigid Endoscopy in 216 Adults of Beijing. Med. Sci. Monit. 2014, 20, 2054–2060. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wu, X.; Kubilay, N.Z.; Ren, J.; Allegranzi, B.; Bischoff, P.; Zayed, B.; Pittet, D.; Li, J. Antimicrobial-coated sutures to decrease surgical site infections: A systematic review and meta-analysis. Eur. J. Clin. Microbiol. 2017, 36, 19–32, Erratum in Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 2031–2034. [Google Scholar] [CrossRef] [PubMed]
- Athanassiadi, K.; Gerazounis, M.; Metaxas, E.; Kalantzi, N. Management of esophageal foreign bodies: A retrospective review of 400 cases1. Eur. J. Cardio-Thoracic Surg. 2002, 21, 653–656. [Google Scholar] [CrossRef]
- Ivatury, R.R.; Moore, F.A.; Biffl, W.; Leppeniemi, A.; Ansaloni, L.; Catena, F.; Peitzman, A.; Moore, E.E. Oesophageal injuries: Position paper, WSES, 2013. World J. Emerg. Surg. 2014, 9, 9. [Google Scholar] [CrossRef]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanchetta, M.; Monti, E.; Latham, L.; Costa, J.; Marzorati, A.; Odeh, M.; Colombo, E.M.; Ietto, G.; Inversini, D.; Iovino, D.; et al. Dental Prosthesis in Esophagus: A Right Cervicotomic Approach. Life 2022, 12, 1170. https://doi.org/10.3390/life12081170
Zanchetta M, Monti E, Latham L, Costa J, Marzorati A, Odeh M, Colombo EM, Ietto G, Inversini D, Iovino D, et al. Dental Prosthesis in Esophagus: A Right Cervicotomic Approach. Life. 2022; 12(8):1170. https://doi.org/10.3390/life12081170
Chicago/Turabian StyleZanchetta, Matteo, Elisa Monti, Lorenzo Latham, Jessica Costa, Alessandro Marzorati, Murad Odeh, Elisabetta Marta Colombo, Giuseppe Ietto, Davide Inversini, Domenico Iovino, and et al. 2022. "Dental Prosthesis in Esophagus: A Right Cervicotomic Approach" Life 12, no. 8: 1170. https://doi.org/10.3390/life12081170
APA StyleZanchetta, M., Monti, E., Latham, L., Costa, J., Marzorati, A., Odeh, M., Colombo, E. M., Ietto, G., Inversini, D., Iovino, D., Maffioli, M. P., Festi, L. F., & Carcano, G. (2022). Dental Prosthesis in Esophagus: A Right Cervicotomic Approach. Life, 12(8), 1170. https://doi.org/10.3390/life12081170





