Arthrodesis and Defect Bridging of the Upper Ankle Joint with Allograft Bone Chips and Allograft Cortical Bone Screws (Shark Screw®) after Removal of the Salto-Prosthesis in a Multimorbidity Patient: A Case Report
Abstract
:1. Introduction
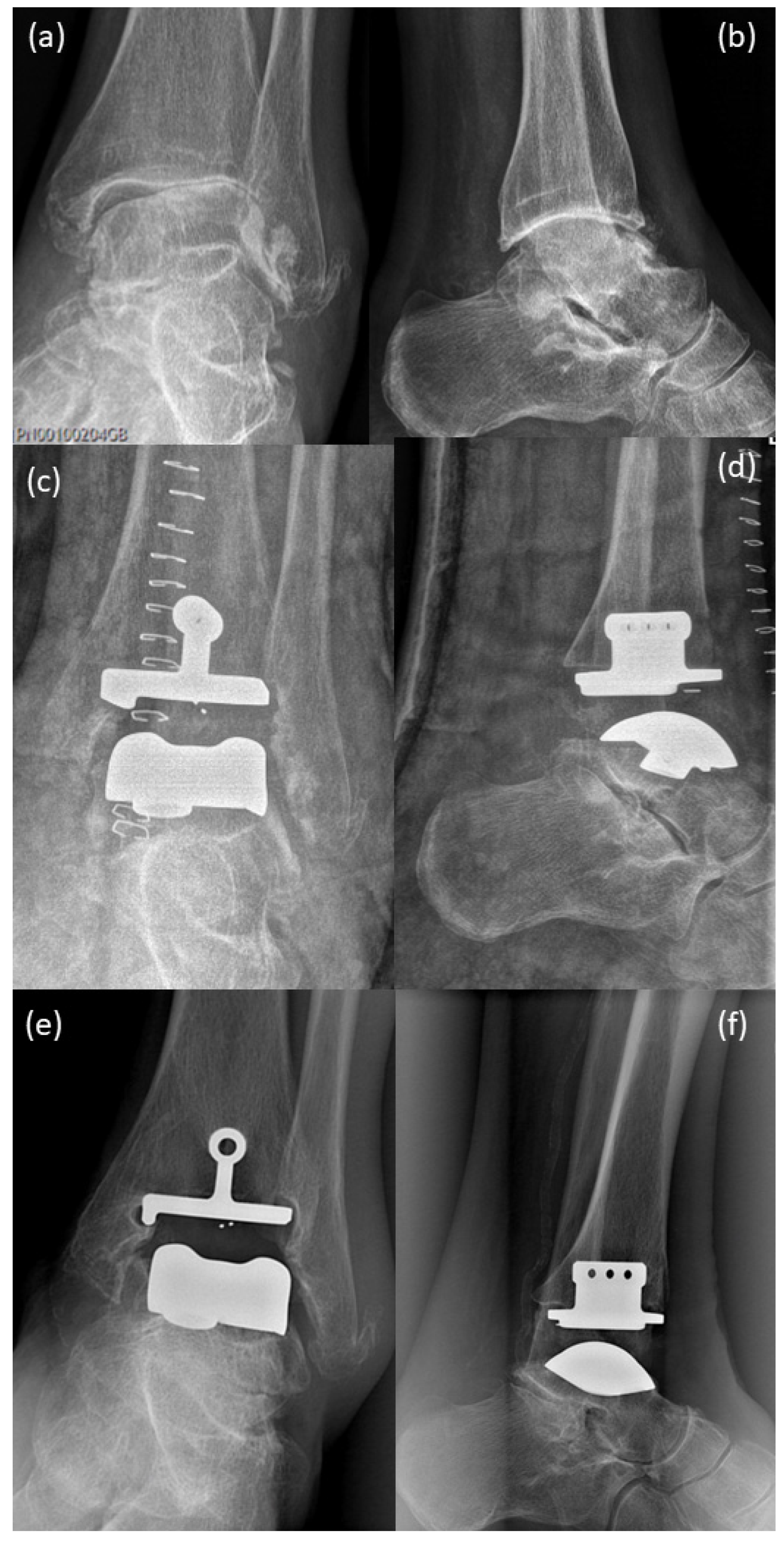
2. Case Presentation
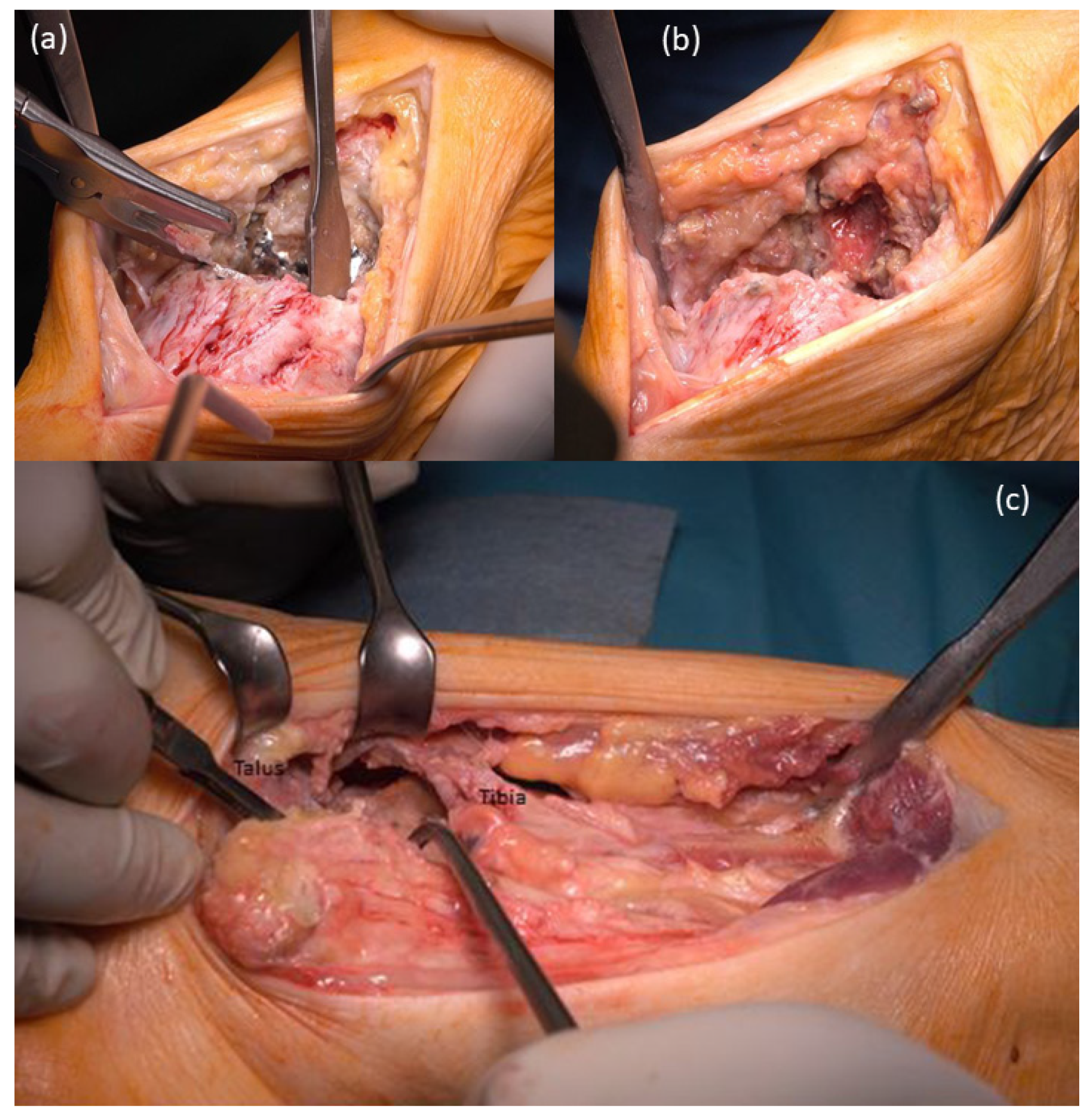
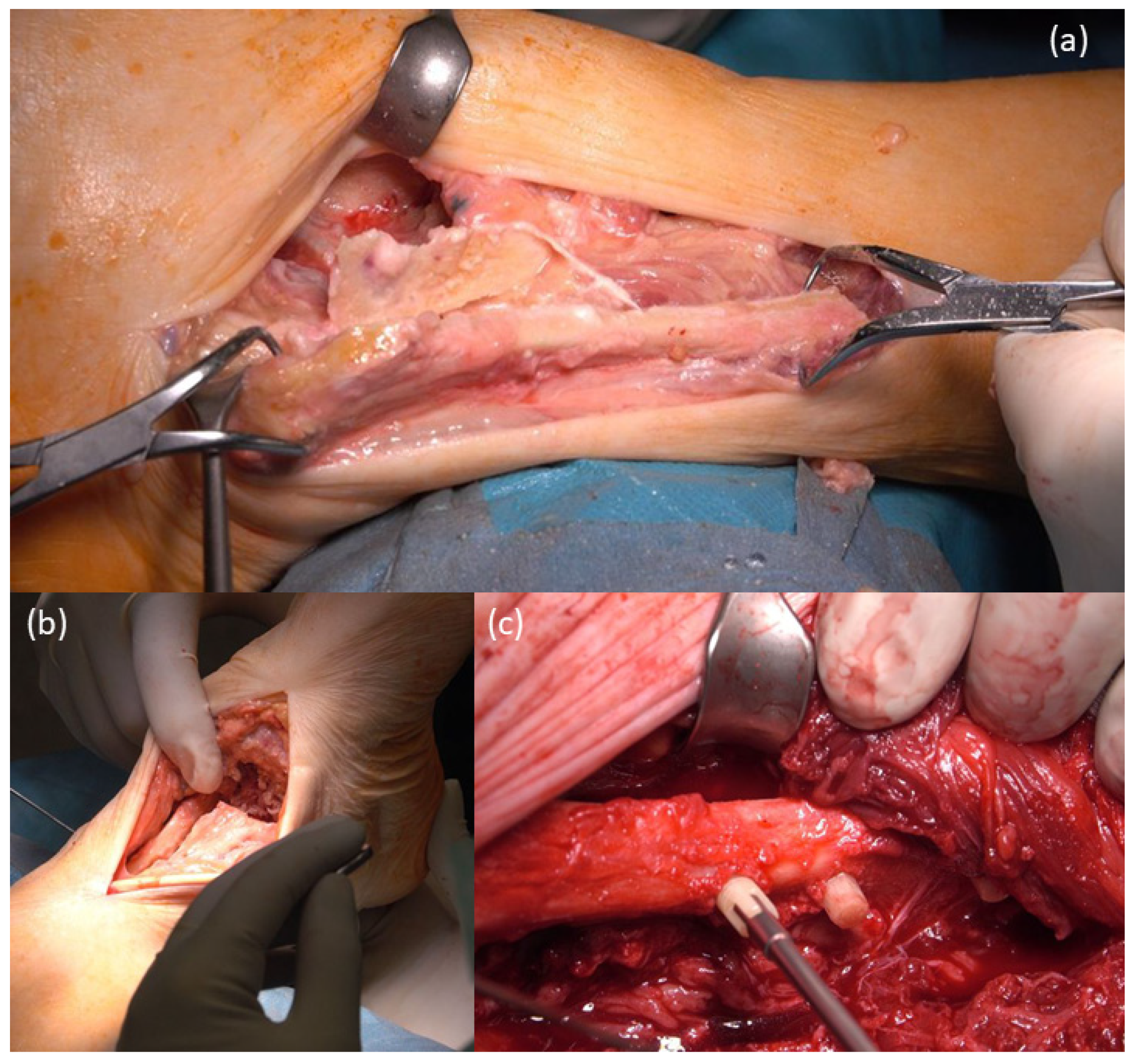
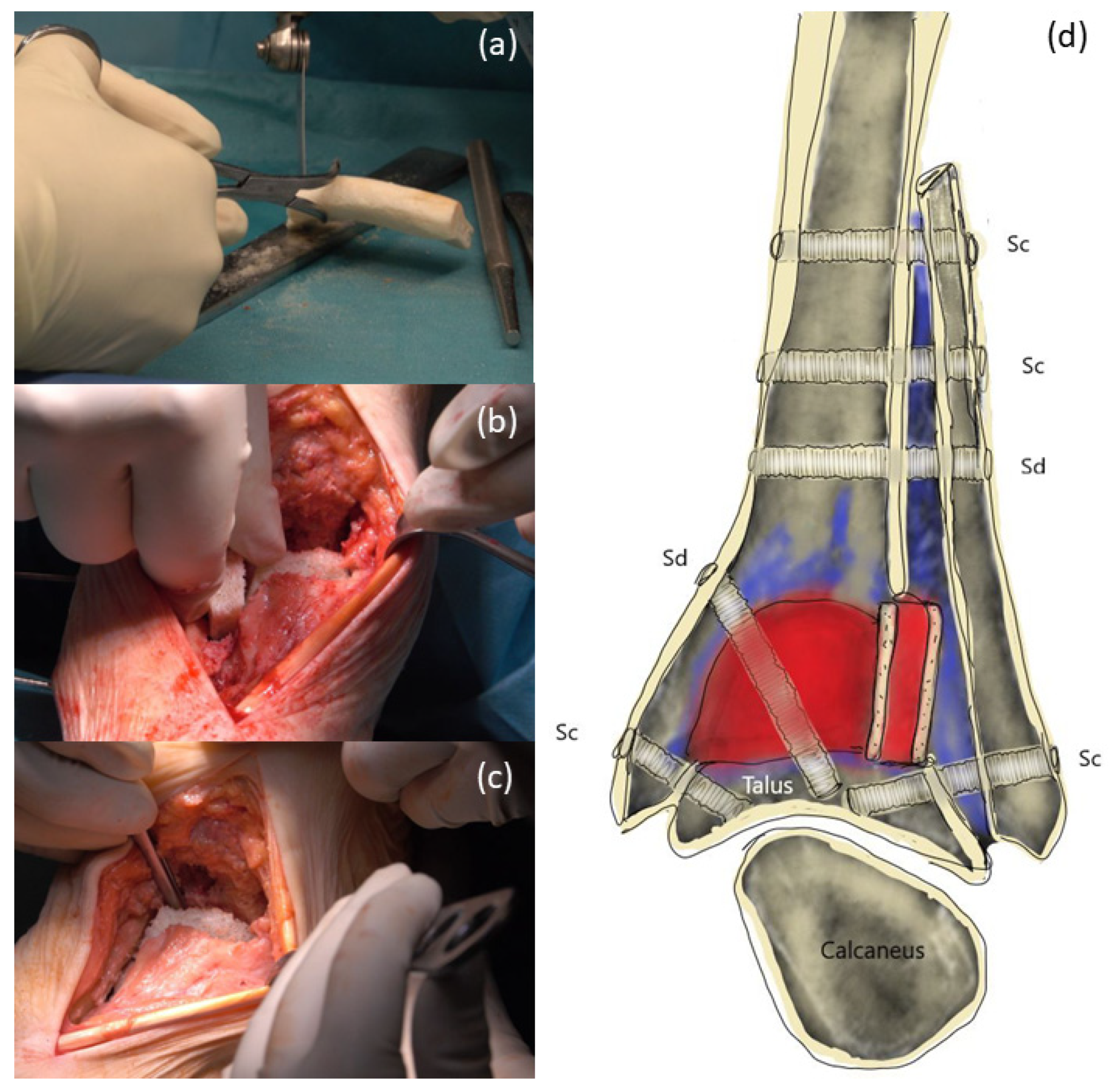
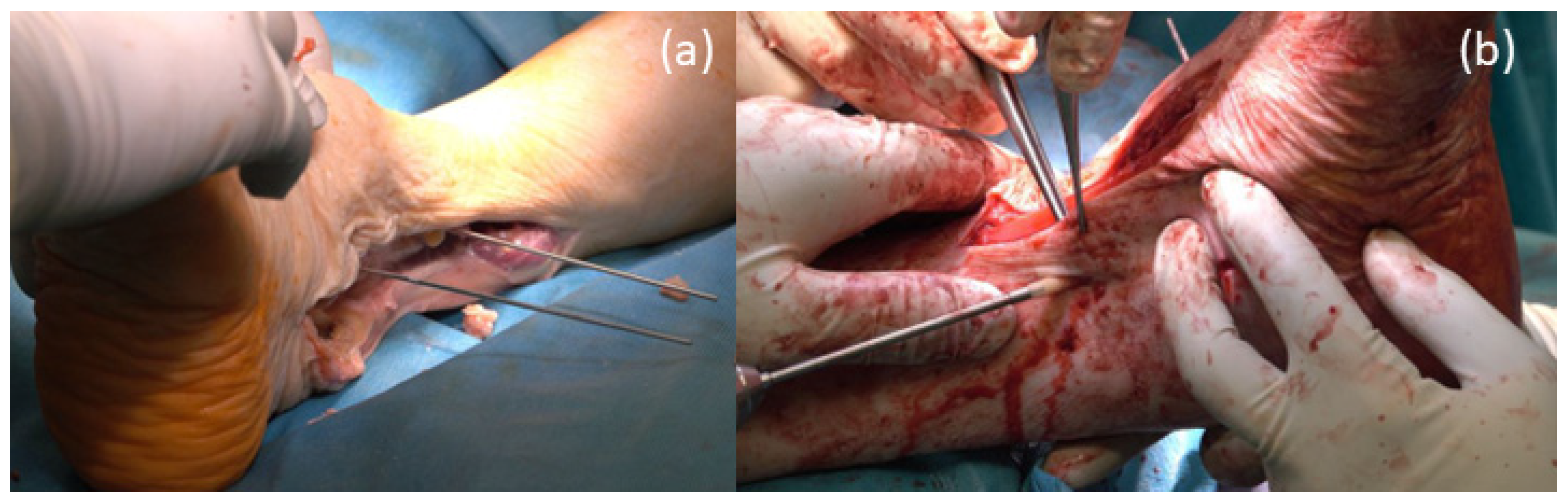
3. Surgical Procedure
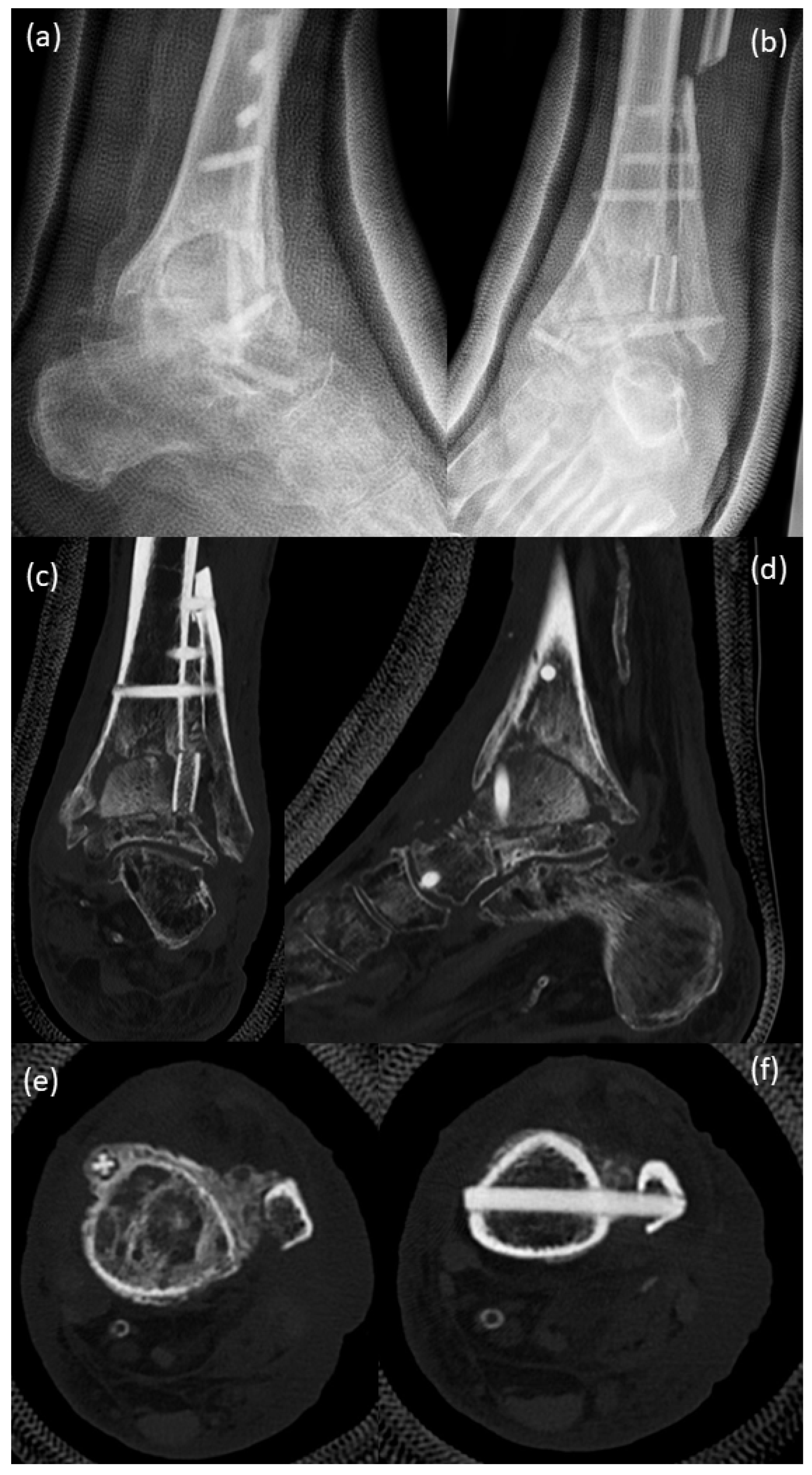
4. Postoperative Rehabilitation
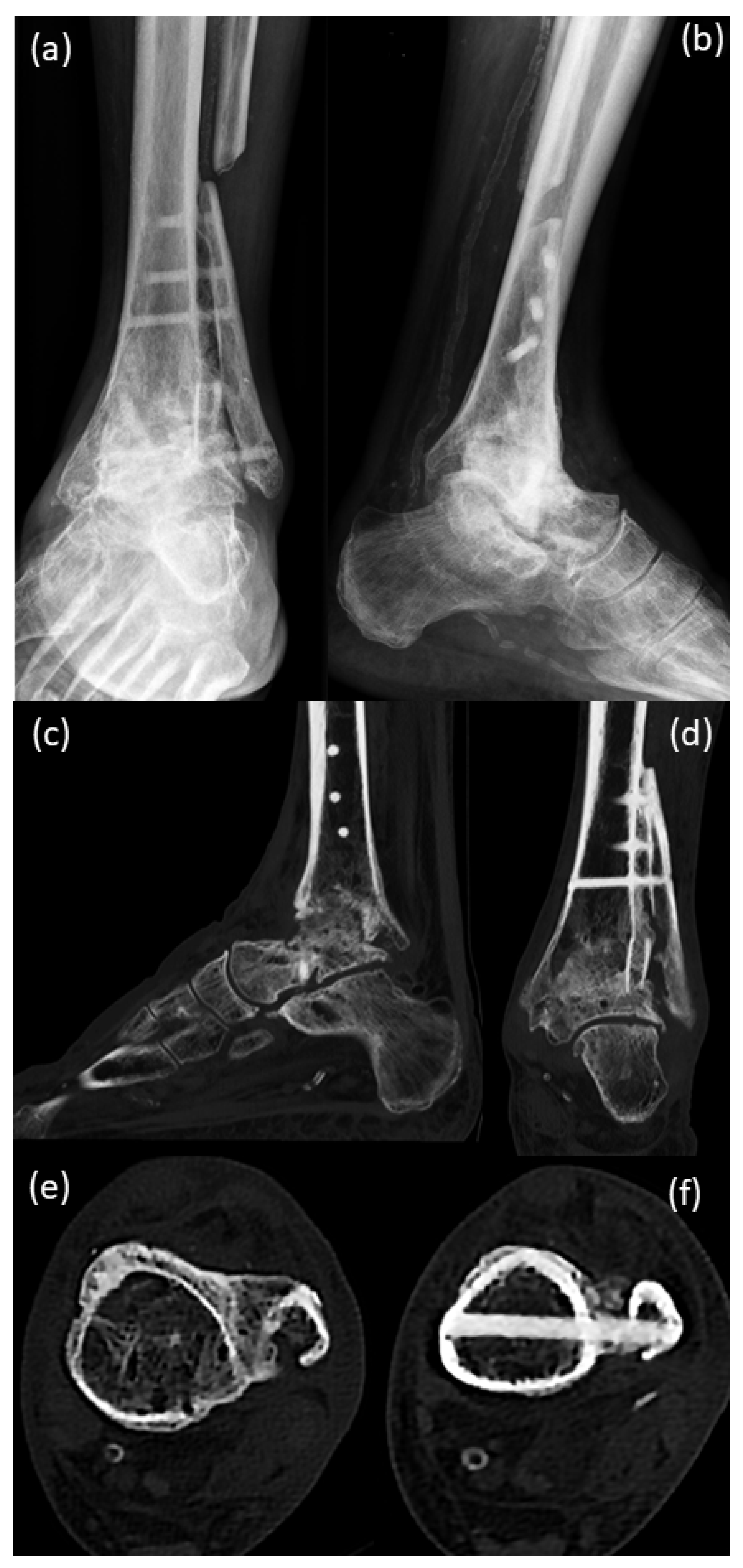
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gougoulias, N.; Maffulli, N. History of total ankle replacement. Clin. Podiatr. Med. Surg. 2013, 30, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Fanelli, D.; Mercurio, M.; Castioni, D.; Sanzo, V.; Gasparini, G.; Galasso, O. End-stage ankle osteoarthritis: Arthroplasty offers better quality of life than arthrodesis with similar complication and re-operation rates-an updated meta-analysis of comparative studies. Int. Orthop. 2021, 45, 2177–2191. [Google Scholar] [CrossRef] [PubMed]
- Stadler, C.; Stöbich, M.; Ruhs, B.; Kaufmann, C.; Pisecky, L.; Stevoska, S.; Gotterbarm, T.; Klotz, M.C. Intermediate to long-term clinical outcomes and survival analysis of the Salto Mobile Bearing total ankle prothesis. Arch. Orthop. Trauma Surg. 2021. [Google Scholar] [CrossRef] [PubMed]
- Vickerstaff, J.A.; Miles, A.W.; Cunningham, J.L. A brief history of total ankle replacement and a review of the current status. Med. Eng. Phys. 2007, 29, 1056–1064. [Google Scholar] [CrossRef] [PubMed]
- Piriou, P.; Culpan, P.; Mullins, M.; Cardon, J.N.; Pozzi, D.; Judet, T. Ankle replacement versus arthrodesis: A comparative gait analysis study. Foot Ankle Int. 2008, 29, 3–9. [Google Scholar] [CrossRef]
- Haddad, S.L.; Coetzee, J.C.; Estok, R.; Fahrbach, K.; Banel, D.; Nalysnyk, L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J. Bone Jt. Surg. Am. 2007, 89, 1899–1905. [Google Scholar] [CrossRef]
- Kerkhoff, Y.R.A.; Keijsers, N.L.W.; Louwerens, J.W.K. Sports Participation, Functional Outcome, and Complications after Ankle Arthrodesis: Midterm Follow-up. Foot Ankle Int. 2017, 38, 1085–1091. [Google Scholar] [CrossRef]
- Muir, D.C.; Amendola, A.; Saltzman, C.L. Long-term outcome of ankle arthrodesis. Foot Ankle Clin. 2002, 7, 703–708. [Google Scholar] [CrossRef]
- Mercurio, M.; Castioni, D.; Porco, E.; Familiari, F.; Gasparini, G.; Galasso, O. Periprosthetic ankle infection: Eradication rate, complications, and limb salvage. A systematic review. Foot Ankle Surg. 2021. [Google Scholar] [CrossRef]
- Brcic, I.; Pastl, K.; Plank, H.; Igrec, J.; Schanda, J.E.; Pastl, E.; Werner, M. Incorporation of an Allogenic Cortical Bone Graft Following Arthrodesis of the First Metatarsophalangeal Joint in a Patient with Hallux Rigidus. Life 2021, 11, 473. [Google Scholar] [CrossRef]
- Roth, H. Die Konservierung von Knochengewebe für Transplantationen, 1st ed.; Springer: Berlin/Heidelberg, Germany, 1952; p. 232. [Google Scholar]
- Virolainen, P.; Vuorio, E.; Aro, H.T. Gene expression at graft-host interfaces of cortical bone allografts and autografts. Clin. Orthop. Relat. Res. 1993, 297, 144–149. [Google Scholar] [CrossRef]
- Taira, H.; Moreno, J.; Ripalda, P.; Forriol, F. Radiological and histological analysis of cortical allografts: An experimental study in sheep femora. Arch. Orthop. Trauma Surg. 2004, 124, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Biedermann, R. Der aktuelle Stellenwert der Sprunggelenksendoprothetik. J. Für Miner. Muskuloskelet. Erkrank. 2008, 15, 43–47. [Google Scholar]
- Fischer, S.; Klug, A.; Faul, P.; Hoffmann, R.; Manegold, S.; Gramlich, Y. Superiority of upper ankle arthrodesis over total ankle replacement in the treatment of end-stage posttraumatic ankle arthrosis. Arch. Orthop. Trauma Surg. 2021, 142, 435–442. [Google Scholar] [CrossRef]
- Pastl, K.; Schimetta, W. The application of an allogeneic bone screw for osteosynthesis in hand and foot surgery: A case series. Arch. Orthop. Trauma Surg. 2021. [Google Scholar] [CrossRef]
- Amann, P.; Bock, P. Clinical and Radiological Results after Use of A Human Bone Graft (Shark Screw®) in TMT II/+II Arthrodesis. Foot Ankle Orthop. 2022, 7, 2473011421s2473000077. [Google Scholar] [CrossRef]
- Walther, M.; Pastl, K.; Hofstätter, S. Osteosynthese mit Schraubentransplantat Shark Screw® aus humanem Knochen. Jatros Unf. Sportstraumatol. 2018, 4, 54–56. [Google Scholar]
- Friedman, R.L.; Glisson, R.R.; Nunley, J.A., 2nd. A biomechanical comparative analysis of two techniques for tibiotalar arthrodesis. Foot Ankle Int. 1994, 15, 301–305. [Google Scholar] [CrossRef]
- Pilette, S.; Huk, O.L.; Yahia, L.; Fowles, J.V. Comparative biomechanical evaluation of the immediate stability of three fixators in arthrodesis of the ankle. Ann. Chir. 1993, 47, 905–911. [Google Scholar]
- Stauffer, R.N.; Chao, E.Y.; Brewster, R.C. Force and motion analysis of the normal, diseased, and prosthetic ankle joint. Clin. Orthop. Relat. Res. 1977, 127, 189–196. [Google Scholar] [CrossRef]
- Thomas, R.; Daniels, T.R.; Parker, K. Gait analysis and functional outcomes following ankle arthrodesis for isolated ankle arthritis. J. Bone Jt. Surg. Am. 2006, 88, 526–535. [Google Scholar] [CrossRef]
- Buchhorn, T.; Polzer, H.; Szymski, D. Open or arthroscopic arthrodesis of the ankle joint: Which is better? Unfallchirurg 2022, 125, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Ochman, S.; Milstrey, A.; Evers, J.; Raschke, M.J. Arthrodesis of the Upper Ankle and Subtalar Joint—Indication and Technique. Z. Orthop. Unfall. 2021, 159, 337–352. [Google Scholar] [CrossRef] [PubMed]




| Orthopedic Morbidities | Non-Orthopedic Morbidities | Medication |
|---|---|---|
| ligament rupture of left upper ankle joint, no operation, 1970 | Diabetes Mellites Type II, since 2011 | Tradolan 50 mg 1-0-0 |
| Chronic osteoarthritis, left upper ankle | Chronic obstructive pulmonary disease (Gold II-III) | Janumet 50/1000 mg 1-0-1 |
| Apoplex, 2006 | Jardiance 10 mg 1-0-0 | |
| left upper ankle joint prosthesis, 2006 | Arterial hypertension | Teveten Plus 1/2-0-0 |
| chronic osteoarthritis, right lower ankle joint, 2011 | Condition after multiembolic ischemia, September 2013, and insult, 2006 | Nomexor 5 mg 1-0-1/2 |
| Subtalar arthrodesis on the right foot, February 2012 | Condition after craniocerebral trauma with narrow right parafacial hematoma without RF signs | Lasix 40 mg, when needed |
| shoulder TEP, October 2018 | cavotricuspidal isthmus ablation, January 2017, tachycardic episodes, cardioversion after sedacorone bolus | Sortis 80 mg 0-0-1 |
| Paroxysmal atrial fibrillation | Lansobene 30 mg 1-0-0 | |
| Condition after appendectomy and tonsillectomy | Magnosolv 1-0-0 | |
| prolonged reversible ischemic neurological deficit with acute aphasia, October 2018 | Seebri breezhaler 44 µg, when needed | |
| Condition after Fracture Costae IIS4-8 right, October 2018 | Seretide discus forte 50 µg 1-0-1 | |
| Iron deficiency anemia | Diamicron 30 mg 1-0-0 | |
| Ultra-short Barret esophagus | Seloken | |
| Large axial hiatal hernia | Eliquis 5 mg 1-0-1 | |
| Steatosis hepatitis | ||
| Sigmoid diverticulosis | ||
| Accentuated gall bladder with polyps | ||
| Non-stenosing coronary stenosis, 2017 | ||
| Pulsarythmias with pulse around 180 beats per minute | ||
| Known spinal stenosis C3/C4 and C4/C5 | ||
| Hyperlipidemia | ||
| Anaphylactic reaction after eating pikeperch, celery, carrots, potatoes | ||
| allergies: penicillin, flavor enhancers, raw fruit and lettuce, fabric softener and starch in laundry |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pastl, K.; Pastl, E.; Flöry, D.; Borchert, G.H.; Chraim, M. Arthrodesis and Defect Bridging of the Upper Ankle Joint with Allograft Bone Chips and Allograft Cortical Bone Screws (Shark Screw®) after Removal of the Salto-Prosthesis in a Multimorbidity Patient: A Case Report. Life 2022, 12, 1028. https://doi.org/10.3390/life12071028
Pastl K, Pastl E, Flöry D, Borchert GH, Chraim M. Arthrodesis and Defect Bridging of the Upper Ankle Joint with Allograft Bone Chips and Allograft Cortical Bone Screws (Shark Screw®) after Removal of the Salto-Prosthesis in a Multimorbidity Patient: A Case Report. Life. 2022; 12(7):1028. https://doi.org/10.3390/life12071028
Chicago/Turabian StylePastl, Klaus, Eva Pastl, Daniel Flöry, Gudrun H. Borchert, and Michel Chraim. 2022. "Arthrodesis and Defect Bridging of the Upper Ankle Joint with Allograft Bone Chips and Allograft Cortical Bone Screws (Shark Screw®) after Removal of the Salto-Prosthesis in a Multimorbidity Patient: A Case Report" Life 12, no. 7: 1028. https://doi.org/10.3390/life12071028
APA StylePastl, K., Pastl, E., Flöry, D., Borchert, G. H., & Chraim, M. (2022). Arthrodesis and Defect Bridging of the Upper Ankle Joint with Allograft Bone Chips and Allograft Cortical Bone Screws (Shark Screw®) after Removal of the Salto-Prosthesis in a Multimorbidity Patient: A Case Report. Life, 12(7), 1028. https://doi.org/10.3390/life12071028






