Subtypes of Depression: Latent Class Analysis in Spanish Old People with Depressive Symptoms
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Procedure, and Participants
2.2. Measurement Instruments
2.3. Statistical Analyses
3. Results
3.1. Latent Class Analyses
3.2. Relations with the Latent Classes
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Ruiz-Rodriguez, P.; Cano-Vindel, A.; Muñoz-Navarro, R.; Medrano, L.; Moriana, J.A.; Aguado, C.B.; Cabré, G.J.; González-Blanch´. Impacto económico y carga de los trastornos mentales comunes en España: Una revisión sistemática y crítica. Ansiedad y Estrés 2017, 23, 118–123. [Google Scholar] [CrossRef]
- Álvarez, M.; Atienza, G.; Avila, M.; González, A.; Guitian, D.; Louro, A.; y Triñares, Y. Guía de Práctica Clínica sobre el Manejo de la Depresión en el Adulto; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2014. [Google Scholar]
- Ezquiaga, E.; López, A.G.; Ramírez, R.H.; Rada Álvaro, P. Tasas de prevalencia de depresión en atención primaria en relación con las características metodológicas de los estudios. Medicina Clínica 2011, 137, 612–615. [Google Scholar] [CrossRef] [PubMed]
- Stek, M.; Gussekloo, J.; Beekman, A.; Van Tilburg, W.; Westendorp, R. Prevalence, correlates and recognition of depression in the oldest old: The Leiden 85-plus study. J. Affect. Disord. 2004, 78, 193–200. [Google Scholar] [CrossRef]
- Hybels, C.F.; Landerman, L.R.; Blazer, D.G. Latent subtypes of depression in a community sample of older adults: Can depression clusters predict future depression trajectories? J. Psychiatr. Res. 2013, 47, 1288–1297. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Parés-Badell, O.; Barbaglia, M.G.; Jerinic, P.; Gustavsson, A.; Salvador-Carulla, L.; Alonso, J. Cost of Disorders of the Brain in Spain. PLoS ONE 2014, 9, e105471. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, G.S. Depression in the elderly. Lancet 2005, 365, 1961–1970. [Google Scholar] [CrossRef]
- Ulbricht, C.M.; Chrysanthopoulou, S.A.; Levin, L.; Lapane, K.L. The use of latent class analysis for identifying subtypes of depression: A systematic review. Psychiatry Res. Neuroimaging 2018, 266, 228–246. [Google Scholar] [CrossRef]
- Sneed, J.R.; Rindskopf, D.; Steffens, D.C.; Krishnan, K.R.R.; Roose, S.P. The Vascular Depression Subtype: Evidence of Internal Validity. Boil. Psychiatry 2008, 64, 491–497. [Google Scholar] [CrossRef]
- Lee, C.-T.; Leoutsakos, J.-M.; Lyketsos, C.G.; Steffens, D.C.; Breitner, J.C.S.; Norton, M. Latent class-derived subgroups of depressive symptoms in a community sample of older adults: The Cache County Study. Int. J. Geriatr. Psychiatry 2011, 27, 1061–1069. [Google Scholar] [CrossRef]
- Grove, W.M.; Andreasen, N.C.; Young, M.; Endicott, J.; Keller, M.B.; Hirschfeld, R.M.A.; Reich, T. Isolation and characterization of a nuclear depressive syndrome. Psychol. Med. 1987, 17, 471–484. [Google Scholar] [CrossRef]
- Parker, G.; Hadzi-Pavlovic, D.; Boyce, P.; Wilhelm, K.; Brodaty, H.; Mitchell, P.; Hickie, I.; Eyers, K. Classifying Depression by Mental State Signs. Br. J. Psychiatry 1990, 157, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Parker, G.; Hadzi-Pavlovic, D. Old data, new interpretation: A re-analysis of Sir Aubrey Lewis’ M.D. thesis. Psychol. Med. 1993, 23, 859–870. [Google Scholar] [CrossRef] [PubMed]
- Parker, G.; Hadzi-Pavlovic, D.; Hickie, I.; Boyce, P.; Mitchell, P.B.; Wilhelm, K.; Brodaty, H. Distinguishing psychotic and non-psychotic melancholia. J. Affect. Disord. 1991, 22, 135–148. [Google Scholar] [CrossRef]
- Parker, G.; Hadzi-Pavlovic, D.; Brodaty, H.; Austin, M.-P.; Mitchell, P.B.; Wilhelm, K.; Hickie, I. Sub-typing depression, II. Clinical distinction of psychotic depression and non-psychotic melancholia. Psychol. Med. 1995, 25, 825–832. [Google Scholar] [CrossRef]
- Parker, G.; Wilhelm, K.; Mitchell, P.B.; Roy, K.; Hadzi-Pavlovic, D. Subtyping Depression. J. Nerv. Ment. Dis. 1999, 187, 610–617. [Google Scholar] [CrossRef]
- Prisciandaro, J.J.; Roberts, J.E. A comparison of the predictive abilities of dimensional and categorical models of unipolar depression in the National Comorbidity Survey. Psychol. Med. 2008, 39, 1087. [Google Scholar] [CrossRef]
- Lamers, F.; De Jonge, P.; Nolen, W.A.; Smit, J.H.; Zitman, F.G.; Beekman, A.T.F.; Penninx, B.W.J.H. Identifying Depressive Subtypes in a Large Cohort Study. J. Clin. Psychiatry 2010, 71, 1582–1589. [Google Scholar] [CrossRef]
- Sunderland, M.; Carragher, N.; Wong, N.; Andrews, G. Factor mixture analysis of DSM-IV symptoms of major depression in a treatment seeking clinical population. Compr. Psychiatry 2013, 54, 474–483. [Google Scholar] [CrossRef]
- Rodgers, S.; Holtforth, M.G.; Mueller, M.; Hengartner, M.P.; Rössler, W.; Ajdacic-Gross, V. Symptom-based subtypes of depression and their psychosocial correlates: A person-centered approach focusing on the influence of sex. J. Affect. Disord. 2014, 156, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Carragher, N.; Adamson, G.; Bunting, B.P.; McCann, S.; O’Neill, S. Subtypes of depression in a nationally representative sample. J. Affect. Disord. 2009, 113, 88–99. [Google Scholar] [CrossRef]
- Lee, S.Y.; Xue, Q.-L.; Spira, A.P.; Lee, H.B. Racial and ethnic differences in depressive subtypes and access to mental health care in the United States. J. Affect. Disord. 2014, 155, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Aliño, J.J.L.-I.; Association, A.P.; Miyar, M.V. DSM-IV-TR: Manual Diagnóstico y Estadístico de los Trastornos Mentales; American Psychiatric Pub.: Barcelona, Spain, 2008; ISBN 978-84-458-1087-3. [Google Scholar]
- Ulbricht, C.M.; Rothschild, A.J.; Lapane, K.L. The association between latent depression subtypes and remission after treatment with citalopram: A latent class analysis with distal outcome. J. Affect. Disord. 2015, 188, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Have, M.T.; Lamers, F.; Wardenaar, K.; Beekman, A.; De Jonge, P.; Van Dorsselaer, S.; Tuithof, M.; Kleinjan, M.; De Graaf, R. The identification of symptom-based subtypes of depression: A nationally representative cohort study. J. Affect. Disord. 2016, 190, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, P.F.; Kessler, R.C.; Kendler, K.S. Latent Class Analysis of Lifetime Depressive Symptoms in the National Comorbidity Survey. Am. J. Psychiatry 1998, 155, 1398–1406. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, P.F.; Prescott, C.A.; Kendler, K.S. The subtypes of major depression in a twin registry. J. Affect. Disord. 2002, 68, 273–284. [Google Scholar] [CrossRef]
- Lamers, F.; Burstein, M.; He, J.-P.; Avenevoli, S.; Angst, J.; Merikangas, K.R. Structure of major depressive disorder in adolescents and adults in the US general population. Br. J. Psychiatry 2012, 201, 143–150. [Google Scholar] [CrossRef]
- Marquand, A.F.; Wolfers, T.; Mennes, M.; Buitelaar, J.; Beckmann, C.F. Beyond Lumping and Splitting: A Review of Computational Approaches for Stratifying Psychiatric Disorders. Boil. Psychiatry Cogn. Neurosci. Neuroimaging 2016, 1, 433–447. [Google Scholar] [CrossRef]
- Rodgers, S.; Ajdacic-Gross, V.; Müller, M.; Hengartner, M.P.; Holtforth, M.G.; Angst, J.; Rössler, W. The role of sex on stability and change of depression symptom subtypes over 20 years: A latent transition analysis. Eur. Arch. Psychiatry Clin. Neurosci. 2013, 264, 577–588. [Google Scholar] [CrossRef][Green Version]
- Portellano-Ortiz, C.; Garre-Olmo, J.; Calvó-Perxas, L.; Conde-Sala, J.L. Depresión y variables asociadas en personas mayores de 50 años en España. Revista de Psiquiatría y Salud Mental 2018, 11, 216–226. [Google Scholar] [CrossRef]
- Quiroz, C.O.A.; Quintana, J.T.; Flores, R.G.; Castro, S.B.E.; García, J.J.V.; Rubio, L.R. Soledad, depresión y calidad de vida en adultos mayores mexicanos. Psicol. Salud 2017, 27, 179–188. [Google Scholar]
- Iden, K.R.; Engedal, K.; Hjørleifsson, S.; Ruths, S. Prevalence of Depression among Recently Admitted Long-Term Care Patients in Norwegian Nursing Homes: Associations with Diagnostic Workup and Use of Antidepressants. Dement. Geriatr. Cogn. Disord. 2014, 37, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Rubiano, E.K.; Frias, D.R.; Abarca, I.O.; Villanueva, M.V.; Martínez, E.B.; Villalba, M.C.; Ortega, J.A.; Fransí, J.C.; García, Y.R.; Carmona, S.M.; et al. Riesgo de depresión en personas de 75 años o más, valoración geriátrica integral y factores de vulnerabilidad asociados en Atención Primaria. Atención Primaria 2015, 47, 616–625. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peña-Solano, D.M.; Herzo-Dilson, M.I.; Calvo-Gómez, J.M. Depresión en ancianos. Rev. Fac. Med. 2009, 57, 347–355. [Google Scholar]
- Bridle, C.; Spanjers, K.; Patel, S.; Atherton, N.M.; Lamb, S.E. Effect of exercise on depression severity in older people: Systematic review and meta-analysis of randomised controlled trials. Br. J. Psychiatry 2012, 201, 180–185. [Google Scholar] [CrossRef]
- Sivertsen, H.; Bjørkløf, G.H.; Engedal, K.; Selbæk, G.; Helvik, A.-S. Depression and Quality of Life in Older Persons: A Review. Dement. Geriatr. Cogn. Disord. 2015, 40, 311–339. [Google Scholar] [CrossRef] [PubMed]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Schaan, B.; Stuck, S.; Zuber, S.; Team, S.C.C. Data Resource Profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). Int. J. Epidemiol. 2013, 42, 992–1001. [Google Scholar] [CrossRef]
- The Survey of Health, Ageing and Retirement in Europe (SHARE): Data Access. Available online: http://www.share-project.org/data-documentation/waves-overview/wave-6.html (accessed on 8 April 2020).
- Malter, F.; Börsch-Supan, A. SHARE Wave 6: Panel Innovations and Collecting Dried Blood Spots; MEA, Max Planck Institute for Social Law and Social Policy: Munich, Germany, 2007. [Google Scholar]
- The RESPECT Code of Practice. Available online: http://www.respectproject.org/code/?id=es (accessed on 11 May 2020).
- The World Medical Association-WMA Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 11 May 2020).
- Prince, M.J.; Reischies, F.; Beekman, A.T.F.; Fuhrer, R.; Jonker, C.; Kivela, S.-L.; Lawlor, B.A.; Lobo, A.; Magnusson, H.; Fichter, M.; et al. Development of the EURO–D scale—A European Union initiative to compare symptoms of depression in 14 European centres. Br. J. Psychiatry 1999, 174, 330–338. [Google Scholar] [CrossRef]
- Ware, J.E.; Gandek, B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J. Clin. Epidemiol. 1998, 51, 903–912. [Google Scholar] [CrossRef]
- Hyde, M.; Wiggins, R.D.; Higgs, P.; Blane, D.B. A measure of quality of life in early old age: The theory, development and properties of a needs satisfaction model (CASP-19). Aging Ment. Health 2003, 7, 186–194. [Google Scholar] [CrossRef]
- Knesebeck, O.; Hyde, M.; Higgs, P.; Kupfer, A.; Siegrist, J. Quality of life and well-being. In Health, Ageing and Retirement in Europe; First results from the survey of health, ageing and retirement in Europe; Börsch-Supan, A., Brugiavini, A., Jürges, H., Mackenbach, J., Siegrist, J., Weber, G., Eds.; Mannheim Research Institute for the Economics of Ageing: Mannheim, Germany, 2005; pp. 199–203. [Google Scholar]
- Nylund, K.L.; Asparouhov, T.; Muthén, B. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. A Multidiscip. J. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Andersen, R.; Hagenaars, J.A.; McCutcheon, A.L. Applied Latent Class Analysis. Can. J. Sociol. 2003, 28, 584. [Google Scholar] [CrossRef]
- Nylund, K.L. Latent Transition Analysis: Modeling Extensions and an Application to Peer Victimization Doctoral Dissertation. Ph.D. Thesis, University of California, Los Angeles, CA, USA, 2007. [Google Scholar]
- Lukočienė, O.; Varriale, R.; Vermunt, J.K. The Simultaneous Decision(s) about the Number of Lower- and Higher-Level Classes in Multilevel Latent Class Analysis. Sociol. Methodol. 2010, 40, 247–283. [Google Scholar] [CrossRef]
- Cruz Menor, E.; Hernández Rodríguez, Y.; Morera Rojas, B.P.; Fernández Montequín, Z.; Rodríguez Benítez, J.C. Trastornos del sueño en el adulto mayor en la comunidad. Rev. Cienc. Médicas Pinar Río 2008, 12, 121–130. [Google Scholar]
- DSM-5: Manual Diagnóstico y Estadístico de los Trastornos Mentales. Available online: http://www.eafit.edu.co/ninos/reddelaspreguntas/Documents/dsm-v-guia-consulta-manual-diagnostico-estadistico-trastornos-mentales.pdf (accessed on 16 May 2020).
- Van Loo, H.M.; Wanders, R.B.K.; Wardenaar, K.J.; Fried, E.I. Problems with latent class analysis to detect data-driven subtypes of depression. Mol. Psychiatry 2016, 23, 495–496. [Google Scholar] [CrossRef]
- Sotelo-Alfonso, I.; Rojas-Soto, J.E.; Sánchez-Arenas, C.; Irigoyen-Coria, A. La depresión en el adulto mayor: Epidemiológica desde el primer nivel de atención. Arch. Med. Fam. 2012, 14, 5–13. [Google Scholar]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Alexandrino-Silva, C.; Wang, Y.P.; Viana, M.C.; Bulhões, R.S.; Martins, S.S.; Andrade, L.H. Gender differences in symptomatic profiles of depression: Results from the São Paulo Megacity Mental Health Survey. J. Affect. Disord. 2013, 147, 355–364. [Google Scholar] [CrossRef]
- Li, Y.; Aggen, S.; Shi, S.; Gao, J.; Tao, M.; Zhang, K.; Wang, X.; Gao, C.; Yang, L.; Liu, Y.; et al. Subtypes of major depression: Latent class analysis in depressed Han Chinese women. Psychol. Med. 2014, 44, 3275–3288. [Google Scholar] [CrossRef]
| #classes | AIC | BIC | ABIC | Entropy | LMR Test | p | BLR Test | p |
|---|---|---|---|---|---|---|---|---|
| 1 | 8258.827 | 8311.828 | 8273.731 | NA | NA | NA | NA | NA |
| 2 | 8163.057 | 8273.475 | 8194.106 | 0.561 | 120.328 | = 0.057 | 121.77 | < 0.001 |
| 3 | 8122.544 | 8290.380 | 8169.738 | 0.707 | 65.725 | = 0.030 | 66.513 | < 0.001 |
| 4 | 8093.859 | 8319.112 | 8157.198 | 0.738 | 54.037 | = 0.056 | 54.685 | < 0.001 |
| 5 | 8083.220 | 8365.891 | 8162.704 | 0.803 | 36.204 | = 0.015 | 36.638 | < 0.020 |
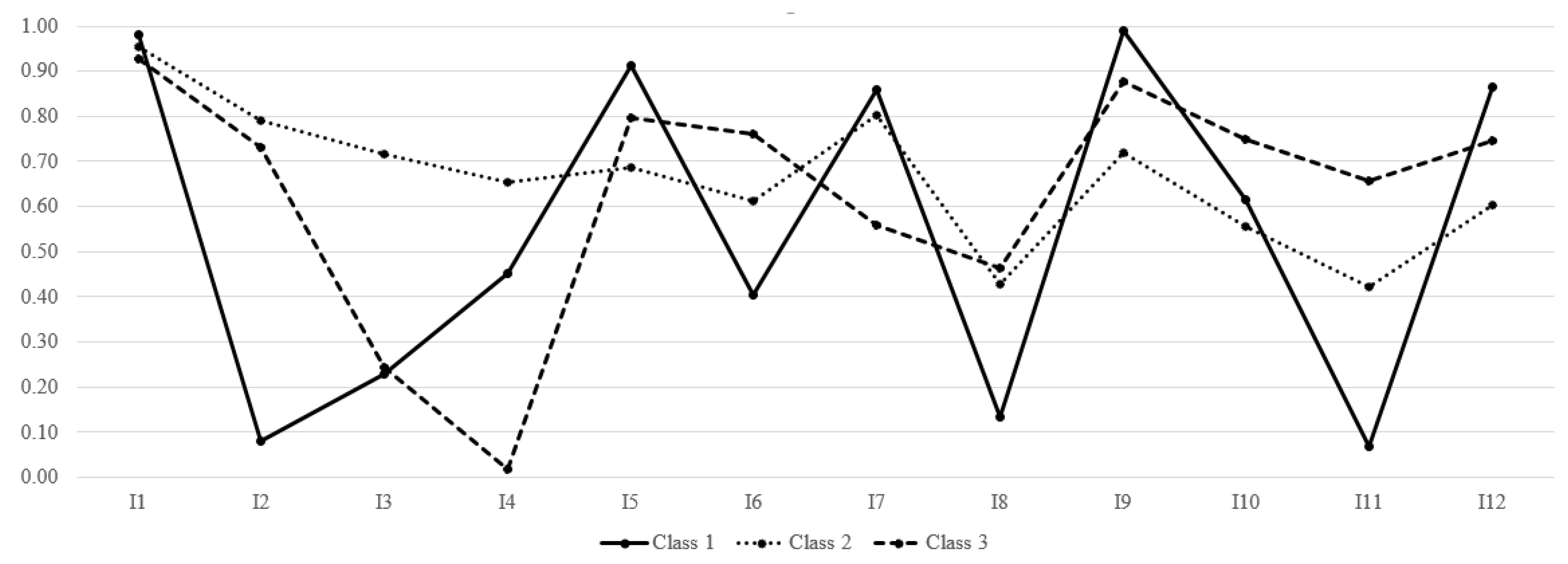
| Items | Class 1 (Psychosomatic) | Class 2 (Melancholic) | Class 3 (Anhedonic) | χ2 | p |
|---|---|---|---|---|---|
| 1. Depressed mood | 0.980 | 0.953 | 0.927 | 3.14 | 0.207 |
| 2. Pessimism/hopelessness | 0.080 | 0.790 | 0.731 | 147.5 | <0.001 |
| 3. Suicidal thoughts | 0.229 | 0.717 | 0.245 | 80.63 | <0.001 |
| 4. Feelings of guilt | 0.452 | 0.655 | 0.018 | 420.5 | <0.001 |
| 5. Sleep disorders | 0.912 | 0.686 | 0.797 | 19.01 | <0.001 |
| 6. Loss of interest | 0.403 | 0.611 | 0.761 | 44.78 | <0.001 |
| 7. Irritability | 0.858 | 0.801 | 0.560 | 44.01 | <0.001 |
| 8. Changes in appetite | 0.135 | 0.427 | 0.464 | 35.14 | <0.001 |
| 9. Fatigue | 0.990 | 0.720 | 0.876 | 33.43 | <0.001 |
| 10. Concentration problems | 0.615 | 0.557 | 0.748 | 19.31 | <0.001 |
| 11. Lack of pleasure | 0.070 | 0.421 | 0.658 | 102.3 | <0.001 |
| 12. Tears | 0.866 | 0.604 | 0.745 | 17.45 | <0.001 |
| ANOVAs | Psychosomatic Class | Melancholic class | Anhedonic class | |||||||||||||
| F | df | p | η2 | M | SD | M | SD | M | SD | |||||||
| Age | 14.803 | 2.609 | <0.001 | 0.046 | 71.222 | 8.082 | 74.712 | 8.829 | 77.126 | 8.829 | ||||||
| Perceived health | 2.594 | 2.609 | 0.076 | 0.008 | 1.89 | 0.73 | 1.90 | 0.87 | 1.73 | 0.77 | ||||||
| No. of chronic diseases | 12.458 | 2.608 | 0.032 | 0.011 | 1.51 | 1.185 | 1.99 | 1.435 | 1.96 | 1.346 | ||||||
| Quality of life | 9.242 | 2.570 | <0.001 | 0.031 | 30.40 | 6.237 | 27.32 | 5.519 | 27.53 | 5.221 | ||||||
| Chi-square | Women | Men | Women | Men | Women | Men | ||||||||||
| χ2 | df | p | V | |||||||||||||
| Gender | 5.227 | 2 | 0.073 | 0.092 | 80.9% | 19.1% | 64.4% | 35.6% | 72.4% | 27.6% | ||||||
| No | Yes | No | Yes | No | Yes | |||||||||||
| Widowhood | 12.633 | 2 | 0.002 | 0.145 | 82.8% | 17.2% | 76,7% | 23.3% | 64.1% | 35.9% | ||||||
| Living with partner | 14.622 | 2 | 0.001 | 0.155 | 76.5% | 23.5% | 69.0% | 31.0% | 55.4% | 44.6% | ||||||
| Mobility problems | 24.331 | 2 | 0.001 | 0.200 | 41.2% | 58.8% | 45.3% | 54.7% | 23.0% | 77.0% | ||||||
| Received help | 13.187 | 2 | 0.001 | 0.147 | 88.2% | 11.8% | 79.3% | 20.7% | 69.1% | 30.9% | ||||||
| 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | |||||
| Sports practice | 19.414 | 6 | 0.126 | 0.004 | 19.1% | 5.9% | 10.3% | 64.7% | 11.5% | 4.6% | 2.3% | 81.6% | 6.8% | 3.5% | 5.3% | 84.5% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Belmonte, S.; Galiana, L.; Sancho, P.; Oliver, A.; Tomás, J.M. Subtypes of Depression: Latent Class Analysis in Spanish Old People with Depressive Symptoms. Life 2020, 10, 70. https://doi.org/10.3390/life10050070
Pérez-Belmonte S, Galiana L, Sancho P, Oliver A, Tomás JM. Subtypes of Depression: Latent Class Analysis in Spanish Old People with Depressive Symptoms. Life. 2020; 10(5):70. https://doi.org/10.3390/life10050070
Chicago/Turabian StylePérez-Belmonte, Sergio, Laura Galiana, Patricia Sancho, Amparo Oliver, and José M. Tomás. 2020. "Subtypes of Depression: Latent Class Analysis in Spanish Old People with Depressive Symptoms" Life 10, no. 5: 70. https://doi.org/10.3390/life10050070
APA StylePérez-Belmonte, S., Galiana, L., Sancho, P., Oliver, A., & Tomás, J. M. (2020). Subtypes of Depression: Latent Class Analysis in Spanish Old People with Depressive Symptoms. Life, 10(5), 70. https://doi.org/10.3390/life10050070






