Analysis of the Correlation Between the Accessibility of Built Environment Elements and Residents’ Self-Rated Health in New Rural Communities
Abstract
1. Introduction
2. Materials and Methods
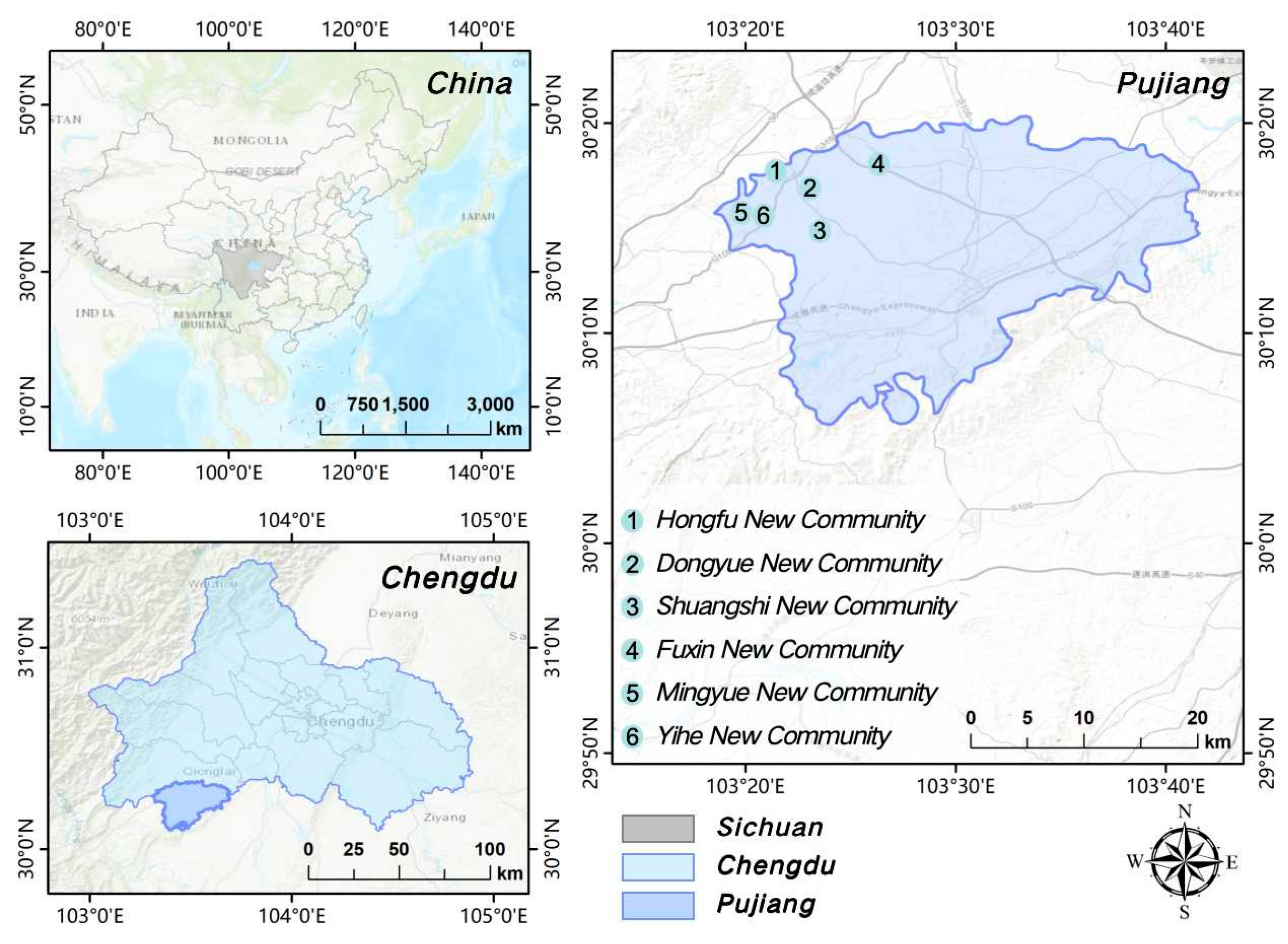
2.1. Study Area
2.2. Measurement
2.2.1. Accessibility
2.2.2. Self-Rated Health
2.3. Methods
2.3.1. Research Framework
2.3.2. GBDT
2.3.3. SHAP
3. Results
3.1. Model Comparison
3.2. Overall Model Performance Evaluation
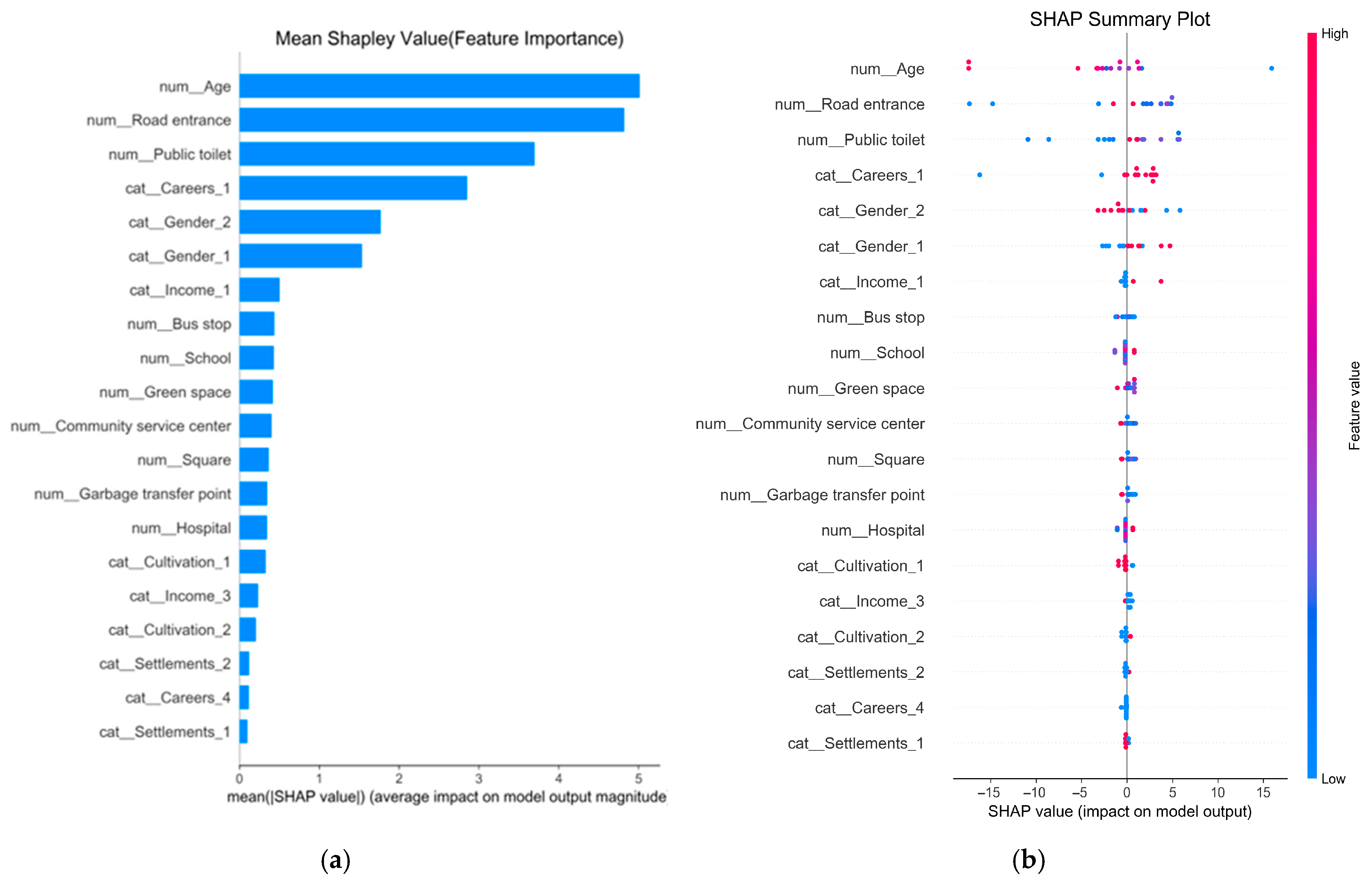
3.3. Self-Rated Health
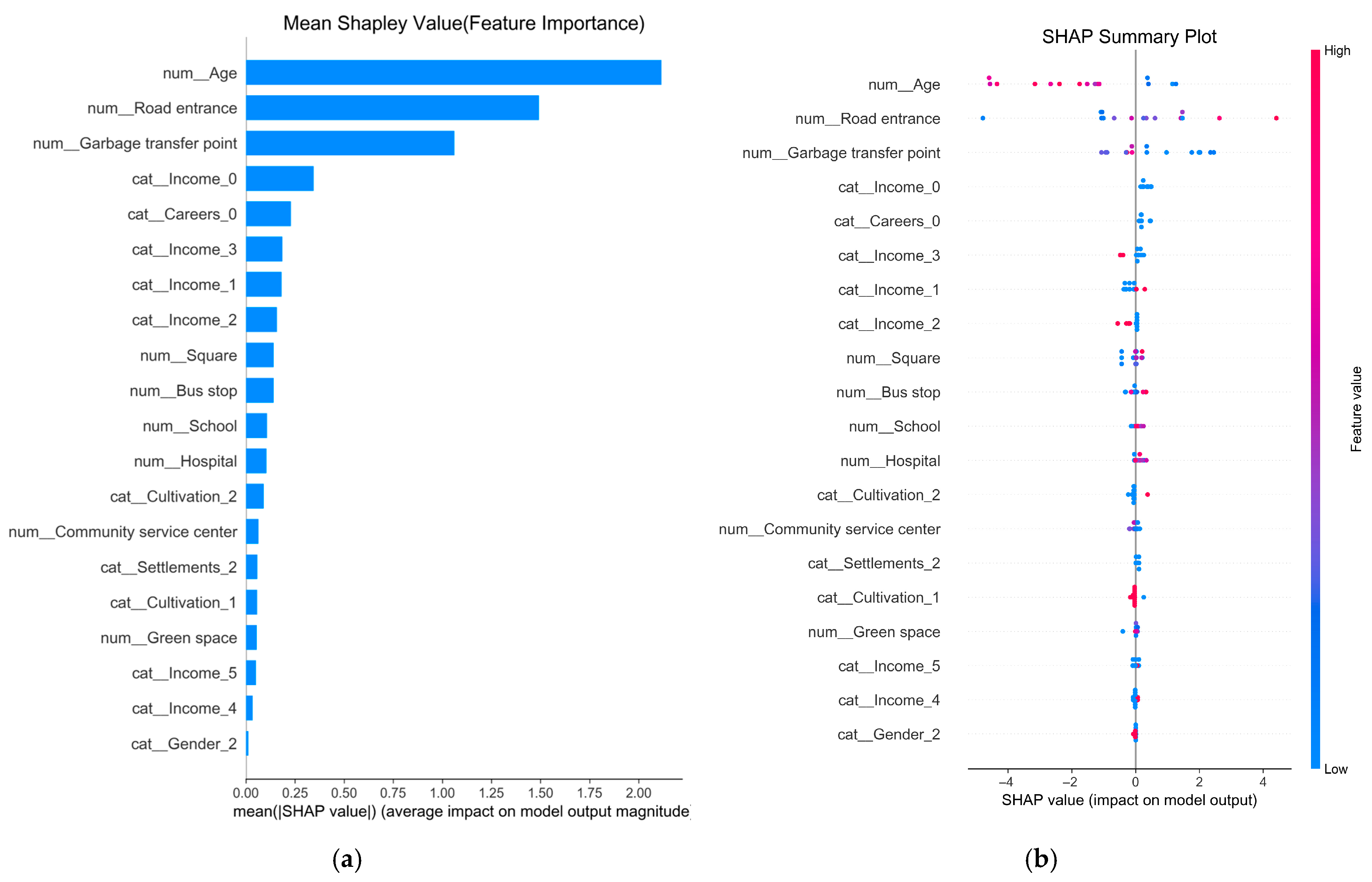
3.4. Self-Rated Physical Health
3.5. Self-Rated Mental Health
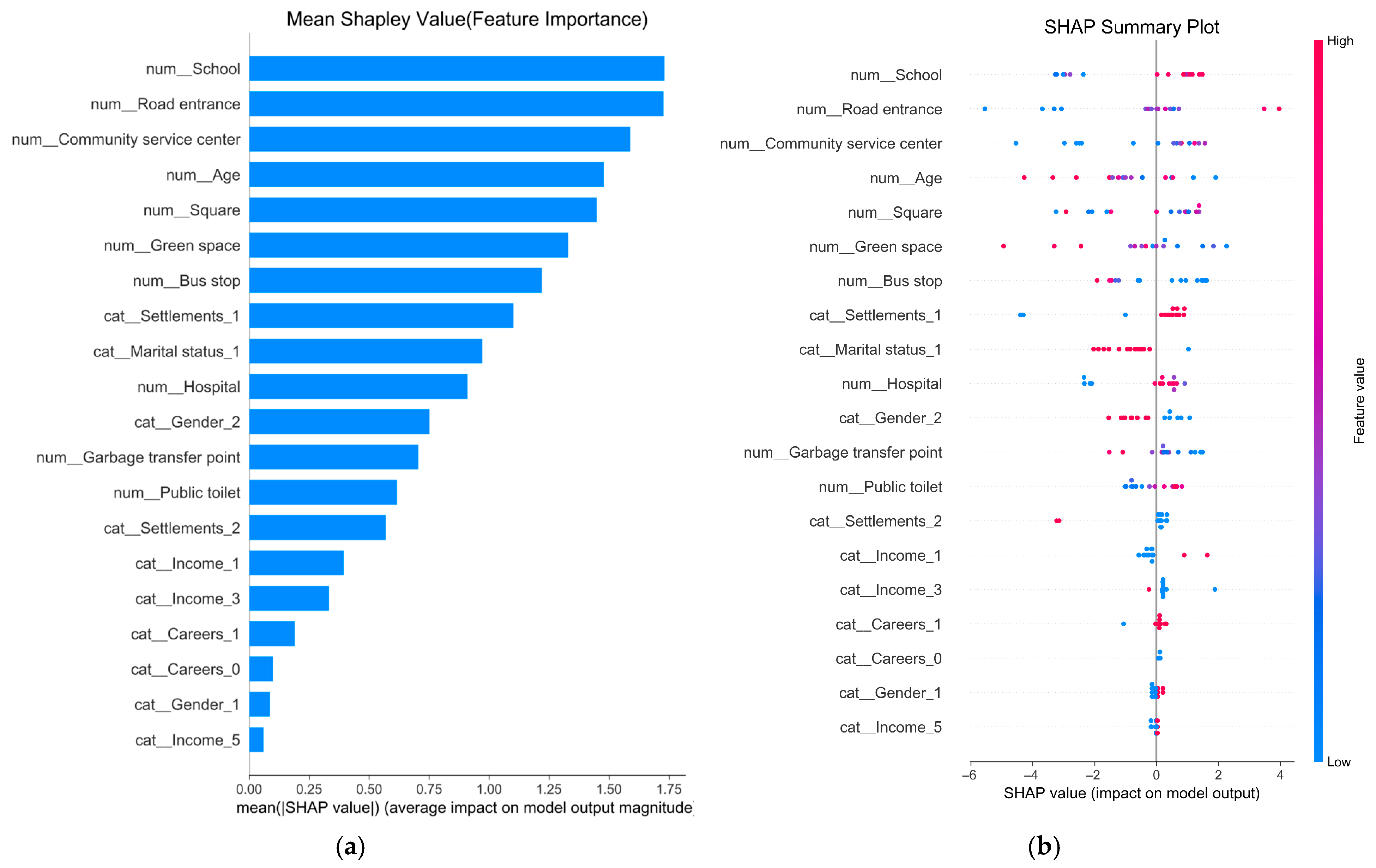
3.6. Self-Rated Social Health
4. Discussion
4.1. Key Findings and Interpretation
4.1.1. Relationship Between Road Entrance and Health
4.1.2. Relationship Between Environmental Sanitation Facility and Health
4.1.3. Relationship Between Public Service Facility and Health
4.1.4. Social Health Cannot Be Adequately Explained by Physical Accessibility
4.2. Policy Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Questionnaire on Healthy Development in New Rural Community
References
- Zang, Y.; Liu, Y.; Yang, Y.; Woods, M.; Fois, F. Rural decline or restructuring? Implications for sustainability transitions in rural China. Land Use Policy 2020, 94, 104531. [Google Scholar] [CrossRef]
- Yuan, J.; Lu, Y.; Ferrier, R.C.; Liu, Z.; Su, H.; Meng, J.; Song, S.; Jenkins, A. Urbanization, rural development and environmental health in China. Environ. Dev. 2018, 28, 101–110. [Google Scholar] [CrossRef]
- Chen, M.; Zhou, Y.; Huang, X.; Ye, C. The integration of new-type urbanization and rural revitalization strategies in China: Origin, reality and future trends. Land 2021, 10, 207. [Google Scholar] [CrossRef]
- Zhang, X.; Brandt, M.; Tong, X.; Ciais, P.; Yue, Y.; Xiao, X.; Zhang, W.; Wang, K.; Fensholt, R. A large but transient carbon sink from urbanization and rural depopulation in China. Nat. Sustain. 2022, 5, 321–328. [Google Scholar] [CrossRef]
- Lang, W.; Chen, T.; Li, X. A new style of urbanization in China: Transformation of urban rural communities. Habitat Int. 2016, 55, 1–9. [Google Scholar] [CrossRef]
- Zhang, C.; Gong, P. Healthy China: From words to actions. Lancet Public Health 2019, 4, e438–e439. [Google Scholar] [CrossRef]
- Zhang, R.; Yuan, Y.; Li, H.; Hu, X. Improving the framework for analyzing community resilience to understand rural revitalization pathways in China. J. Rural Stud. 2022, 94, 287–294. [Google Scholar] [CrossRef]
- Rao, M.; Prasad, S.; Adshead, F.; Tissera, H. The built environment and health. Lancet 2007, 370, 1111–1113. [Google Scholar] [CrossRef] [PubMed]
- Jackson, L.E. The relationship of urban design to human health and condition. Landsc. Urban Plan. 2003, 64, 191–200. [Google Scholar] [CrossRef]
- Jiang, Y.; Long, H.; Ives, C.D.; Deng, W.; Chen, K.; Zhang, Y. Modes and practices of rural vitalisation promoted by land consolidation in a rapidly urbanising China: A perspective of multifunctionality. Habitat Int. 2022, 121, 102514. [Google Scholar] [CrossRef]
- Ewing, R.; Cervero, R. Travel and the built environment: A synthesis. Transp. Res. Rec. 2001, 1780, 87–114. [Google Scholar] [CrossRef]
- Dannenberg, A.L.; Jackson, R.J.; Frumkin, H.; Schieber, R.A.; Pratt, M.; Kochtitzky, C.; Tilson, H.H. The impact of community design and land-use choices on public health: A scientific research agenda. Am. J. Public Health 2003, 93, 1500–1508. [Google Scholar] [CrossRef]
- Hasson, R.; Sallis, J.F.; Coleman, N.; Kaushal, N.; Nocera, V.G.; Keith, N. COVID-19: Implications for physical activity, health disparities, and health equity. Am. J. Lifestyle Med. 2022, 16, 420–433. [Google Scholar] [CrossRef]
- Zou, Y.; Wang, D. Differences in the influence of the built environment on physical activities for people with normal weight, overweight, and obesity. Health Place 2024, 90, 103385. [Google Scholar] [CrossRef]
- Chen, S.; Bao, Z.; Lou, V. Assessing the impact of the built environment on healthy aging: A gender-oriented Hong Kong study. Environ. Impact Assess. Rev. 2022, 95, 106812. [Google Scholar] [CrossRef]
- Dixon, B.N.; Ugwoaba, U.A.; Brockmann, A.N.; Ross, K. Associations between the built environment and dietary intake, physical activity, and obesity: A scoping review of reviews. Obes. Rev. 2021, 22, e13171. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Chi, A.; Sun, Y. Physical activity among older Chinese adults living in urban and rural areas: A review. J. Sport Health Sci. 2016, 5, 281–286. [Google Scholar] [CrossRef]
- Moreno-Llamas, A.; García-Mayor, J.; De la Cruz-Sánchez, E. Urban–rural differences in perceived environmental opportunities for physical activity: A 2002–2017 time-trend analysis in Europe. Health Promot. Int. 2023, 38, daad087. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Ahn, C.R.; Nam, Y. The influence of built environment features on crowdsourced physiological responses of pedestrians in neighborhoods. Comput. Environ. Urban Syst. 2019, 75, 161–169. [Google Scholar] [CrossRef]
- Lin, L.; Moudon, A.V. Objective versus subjective measures of the built environment, which are most effective in capturing associations with walking? Health Place 2010, 16, 339–348. [Google Scholar] [CrossRef]
- Hansen, A.Y.; Umstattd Meyer, M.R.; Lenardson, J.D.; Hartley, D. Built environments and active living in rural and remote areas: A review of the literature. Curr. Obes. Rep. 2015, 4, 484–493. [Google Scholar] [CrossRef]
- Paquet, C.; Orschulok, T.P.; Coffee, N.T.; Howard, N.J.; Hugo, G.; Taylor, A.W.; Adams, R.J.; Daniel, M. Are accessibility and characteristics of public open spaces associated with a better cardiometabolic health? Landsc. Urban Plan. 2013, 118, 70–78. [Google Scholar] [CrossRef]
- Zhang, R.; Zhang, C.Q.; Rhodes, R.E. The pathways linking objectively-measured greenspace exposure and mental health: A systematic review of observational studies. Environ. Res. 2021, 198, 111233. [Google Scholar] [CrossRef]
- Geary, R.S.; Thompson, D.; Mizen, A.; Akbari, A.; Garrett, J.K.; Rowney, F.M.; Watkins, A.; Lyons, R.A.; Stratton, G.; Lovell, R.; et al. Ambient greenness, access to local green spaces, and subsequent mental health: A 10-year longitudinal dynamic panel study of 2 3 million adults in Wales. Lancet Planet. Health 2023, 7, e809–e818. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Ta, N.; Yu, B.; Wu, J. Are the accessibility and facility environment of parks associated with mental health? A comparative analysis based on residential areas and workplaces. Landsc. Urban Plan. 2023, 237, 104807. [Google Scholar] [CrossRef]
- Høyer-Kruse, J.; Schmidt, E.B.; Hansen, A.F.; Pedersen, M.R.L. The interplay between social environment and opportunities for physical activity within the built environment: A scoping review. BMC Public Health 2024, 24, 2361. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Han, H.; Yang, C.; Liu, Q. The Influence Mechanism of the Community Subjectively Built Environment on the Physical and Mental Health of Older Adults. Sustainability 2023, 15, 13211. [Google Scholar] [CrossRef]
- Giles-Corti, B.; Kelty, S.F.; Zubrick, S.R.; Villanueva, K.P. Encouraging walking for transport and physical activity in children and adolescents: How important is the built environment? Sports Med. 2009, 39, 995–1009. [Google Scholar] [CrossRef]
- Cervero, R.; Kockelman, K. Travel demand and the 3Ds: Density, diversity, and design. Transp. Res. Part D Transp. Environ. 1997, 2, 199–219. [Google Scholar] [CrossRef]
- Parga, J.P.F.A.; Tiznado-Aitken, I.; Jamal, S.; Farber, S.; Yu, A.; Higgins, C. Perceived accessibility and self-rated health: Examining subjective well-being in the suburbs of Scarborough, Canada. Transp. Res. Part A Policy Pract. 2024, 190, 104261. [Google Scholar] [CrossRef]
- Wolff, M. Taking one step further–Advancing the measurement of green and blue area accessibility using spatial network analysis. Ecol. Indic. 2021, 126, 107665. [Google Scholar] [CrossRef]
- Yiqiu, Z.; Xinlei, D.; Yajuan, W.; Wenguo, W.; Mingjing, W. GIS-based accessibility analysis of urban park green space landscape. Sci. Rep. 2025, 15, 28498. [Google Scholar] [CrossRef]
- Wood, S.M.; Alston, L.; Beks, H.; Namara, K.M.; Coffee, N.T.; Clark, R.A.; Shee, A.W.; Versace, V.L. The application of spatial measures to analyse health service accessibility in Australia: A systematic review and recommendations for future practice. BMC Health Serv. Res. 2023, 23, 330. [Google Scholar] [CrossRef]
- Mazzulla, G.; Pirrone, C.G. Accessibility Measures: From a Literature Review to a Classification Framework. ISPRS Int. J. Geo-Inf. 2024, 13, 450. [Google Scholar] [CrossRef]
- Maddox, G.L. Self-assessment of health status a longitudinal study of selected elderly subjects. J. Chronic Dis. 1964, 17, 449–460. [Google Scholar] [CrossRef]
- Fayers, P.M.; Sprangers, M.A.G. Understanding self-rated health. Lancet 2002, 359, 187–188. [Google Scholar] [CrossRef]
- Layes, A.; Asada, Y.; Kephart, G. Whiners and deniers–What does self-rated health measure? Soc. Sci. Med. 2012, 75, 1–9. [Google Scholar] [CrossRef]
- Eriksson, I.; Undén, A.L.; Elofsson, S. Self-rated health. Comparisons between three different measures. Results from a population study. Int. J. Epidemiol. 2001, 30, 326–333. [Google Scholar] [CrossRef]
- Ye, Y.; Shu, X. Unequal but Widespread Despairs: Social Inequalities and Self-Rated Health Trends in the United States in 1972–2018. Soc. Sci. Med. 2025, 367, 117732. [Google Scholar] [CrossRef] [PubMed]
- Levinson, H.S.; Wynn, F.H. Effects of density on urban transportation requirements. Highw. Res. Rec. 1963, 38–64. [Google Scholar]
- McCormack, G.R.; Shiell, A. In search of causality: A systematic review of the relationship between the built environment and physical activity among adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 125. [Google Scholar] [CrossRef]
- McCormack, G.R.; Shiell, A.; Doyle-Baker, P.K.; Friedenreich, C.M.; Sandalack, B.A. Subpopulation differences in the association between neighborhood urban form and neighborhood-based physical activity. Health Place 2014, 28, 109–115. [Google Scholar] [CrossRef]
- Wang, M.; Qiu, M.; Chen, M.; Zhang, Y.; Zhang, S.; Wang, L. How does urban green space feature influence physical activity diversity in high-density built environment? An on-site observational study. Urban For. Urban Green. 2021, 62, 127129. [Google Scholar] [CrossRef]
- Ramirez, L.K.B.; Hoehner, C.M.; Brownson, R.C.; Cook, R.; Orleans, C.T.; Hollander, M.; Barker, D.C.; Bors, P.; Ewing, R.; Killingsworth, R.; et al. Indicators of activity-friendly communities: An evidence-based consensus process. Am. J. Prev. Med. 2006, 31, 515–524. [Google Scholar]
- Pikora, T.; Giles-Corti, B.; Bull, F.; Jamrozik, K.; Donovan, R. Developing a framework for assessment of the environmental determinants of walking and cycling. Soc. Sci. Med. 2003, 56, 1693–1703. [Google Scholar] [CrossRef]
- Handy, S.; Cao, X.; Mokhtarian, P. Correlation or causality between the built environment and travel behavior? Evidence from Northern California. Transp. Res. Part D Transp. Environ. 2005, 10, 427–444. [Google Scholar] [CrossRef]
- Iacono, M.; Krizek, K.J.; El-Geneidy, A. Measuring non-motorized accessibility: Issues, alternatives, and execution. J. Transp. Geogr. 2010, 18, 133–140. [Google Scholar] [CrossRef]
- Han, Y.; Qin, C.; Xiao, L.; Ye, Y. The nonlinear relationships between built environment features and urban street vitality: A data-driven exploration. Environ. Plan. B Urban Anal. City Sci. 2024, 51, 195–215. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, X.; Grekousis, G.; Huang, Y.; Hua, F.; Pan, Z.; Liu, Y. Examining the importance of built and natural environment factors in predicting self-rated health in older adults: An extreme gradient boosting (XGBoost) approach. J. Clean. Prod. 2023, 413, 137432. [Google Scholar] [CrossRef]
- Ewing, R.; Greenwald, M.J.; Zhang, M.; Walters, J.; Feldman, M.; Cervero, R.; Thomas, J. Measuring the Impact of Urban Form and Transit Access on Mixed Use Site Trip Generation Rates—Portland Pilot Study; US Environmental Protection Agency: Washington, DC, USA, 2009. [Google Scholar]
- Ewing, R.; Cervero, R. Travel and the built environment: A meta-analysis. J. Am. Plan. Assoc. 2010, 76, 265–294. [Google Scholar] [CrossRef]
- Brownson, R.C.; Hoehner, C.M.; Day, K.; Forsyth, A.; Sallis, J.F. Measuring the built environment for physical activity: State of the science. Am. J. Prev. Med. 2009, 36, S99–S123.e12. [Google Scholar] [CrossRef]
- Zhang, C.J.P.; Barnett, A.; Ming, W.K.; Lai, P.C.; Lee, R.S.; Cerin, E. How urban environments affect quality of life in older socio-demographic groups: The role of physical activity behaviour. In Handbook of Quality of Life Research; Edward Elgar Publishing: Cheltenham, UK, 2024; pp. 355–371. [Google Scholar]
- Xu, J.; Xie, Y.; Li, B.; Hu, M. The study of validity on self-rated health measurement scale-the revised version 1.0. Chin. J. Clin. Rehab. 2002, 6, 2082–2085. [Google Scholar]
- Xu, J.; Zhang, J.; Feng, L.; Qiu, J. Self-rated health of population in southern China: Association with socio-demographic characteristics measured with multiple-item self-rated health measurement scale. BMC Public Health 2010, 10, 393. [Google Scholar] [CrossRef]
- Friedman, J.H. Greedy function approximation: A gradient boosting machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Lee, S.I. A unified approach to interpreting model predictions. Adv. Neural Inf. Process. Syst. 2017, 30, 4768–4777. [Google Scholar]
- Pun, V.C.; Manjourides, J.; Suh, H.H. Close proximity to roadway and urbanicity associated with mental ill-health in older adults. Sci. Total Environ. 2019, 658, 854–860. [Google Scholar] [CrossRef]
- Dzhambov, A.; Tilov, B.; Markevych, I.; Dimitrova, D. Residential road traffic noise and general mental health in youth: The role of noise annoyance, neighborhood restorative quality, physical activity, and social cohesion as potential mediators. Environ. Int. 2017, 109, 1–9. [Google Scholar] [CrossRef]
- Conceição, M.A.; Monteiro, M.M.; Kasraian, D.; Berg, P.; Haustein, S.; Alves, I.; Azevedo, C.L.; Miranda, L. The effect of transport infrastructure, congestion and reliability on mental wellbeing: A systematic review of empirical studies. Transp. Rev. 2023, 43, 264–302. [Google Scholar] [CrossRef]
- Silva, C.; Xue, S. Situating spatial determinism in urban design and planning for sustainable walkability: A simulation of street morphology and pedestrian behaviour. Discov. Sustain. 2024, 5, 212. [Google Scholar] [CrossRef]
- Goel, R.; Tiwari, G.; Varghese, M.; Bhalla, K.; Agrawal, G.; Saini, G.; Jha, A.; John, D.; Saran, A.; White, D.; et al. Effectiveness of road safety interventions: An evidence and gap map. Campbell Syst. Rev. 2024, 20, e1367. [Google Scholar] [CrossRef]
- Wang, Y.; Shen, C.; Bartsch, K.; Zuo, J. Exploring the trade-off between benefit and risk perception of NIMBY facility: A social cognitive theory model. Environ. Impact Assess. Rev. 2021, 87, 106555. [Google Scholar] [CrossRef]
- Sun, W.; Wu, Y.; Wang, L.; Li, X.; Guo, Q.; Hu, Z. Associations between environmental perception and self-rated health in the city hierarchy of China: Findings from a national cross-sectional survey. Soc. Sci. Med. 2024, 348, 116785. [Google Scholar] [CrossRef]
- Braubach, M. Residential conditions and their impact on residential environment satisfaction and health: Results of the WHO large analysis and review of European housing and health status (LARES) study. Int. J. Environ. Pollut. 2007, 30, 384–403. [Google Scholar] [CrossRef]
- Lin, Y.; Fu, H.; Zhong, Q.; Zuo, Z.; Chen, S.; He, Z.; Zhang, H. The influencing mechanism of the communities’ built environment on residents’ subjective well-being: A case study of Beijing. Land 2024, 13, 793. [Google Scholar] [CrossRef]
- Honold, J.; Beyer, R.; Lakes, T.; Meer, E. Multiple environmental burdens and neighborhood-related health of city residents. J. Environ. Psychol. 2012, 32, 305–317. [Google Scholar] [CrossRef]
- Thornton, L.E.; Pearce, J.R.; Kavanagh, A.M. Using Geographic Information Systems (GIS) to assess the role of the built environment in influencing obesity: A glossary. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 71. [Google Scholar] [CrossRef]
- Dinwiddie, G.Y.; Gaskin, D.J.; Chan, K.S.; Norrington, J.; McCleary, R. Residential segregation, geographic proximity and type of services used: Evidence for racial/ethnic disparities in mental health. Soc. Sci. Med. 2013, 80, 67–75. [Google Scholar] [CrossRef]
- Van Cauwenberg, J.; Van Holle, V.; Simons, D.; Deridder, R.; Clarys, P.; Goubert, P.; Nasar, J.; Salmon, J.; Bourdeaudhuij, I.D.; Deforche, B. Environmental factors influencing older adults’ walking for transportation: A study using walk-along interviews. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 85. [Google Scholar] [CrossRef]
- Wakefield, S.E.L.; Poland, B. Family, friend or foe? Critical reflections on the relevance and role of social capital in health promotion and community development. Soc. Sci. Med. 2005, 60, 2819–2832. [Google Scholar] [CrossRef]
- Carrasco, M.A.; Bilal, U. A sign of the times: To have or to be? Social capital or social cohesion? Soc. Sci. Med. 2016, 159, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Yen, I.H.; Michael, Y.L.; Perdue, L. Neighborhood environment in studies of health of older adults: A systematic review. Am. J. Prev. Med. 2009, 37, 455–463. [Google Scholar] [CrossRef]
- Chatterji, S.; Byles, J.; Cutler, D.; Seeman, T.; Verdes, E. Health, functioning, and disability in older adults—Present status and future implications. Lancet 2015, 385, 563–575. [Google Scholar] [CrossRef]
- Keating, N. A research framework for the United Nations Decade of Healthy Ageing (2021–2030). Eur. J. Ageing 2022, 19, 775–787. [Google Scholar] [CrossRef]

| Variables | Code | Definition |
|---|---|---|
| Gender | 1 | Male |
| 2 | Female | |
| Age | - | - |
| Career | 1 | peasants |
| 2 | government official | |
| 3 | individual businesses | |
| 4 | workers | |
| Marital status | 1 | married |
| 2 | unmarried | |
| 3 | divorcee | |
| 4 | bereaved of one’s spouse | |
| Settlement | 1 | Living in a rural community |
| 2 | Living in a rural community or county | |
| Income | 1 | <50,000 CNY |
| 2 | 50,000 CNY–100,000 CNY | |
| 3 | 100,000 CNY–200,000 CNY | |
| 4 | >200,000 CNY | |
| Cultivation | 1 | Still engaged in farming activities |
| 2 | Not engaged in farming activities |
| AUC | Accuracy | Precision | Recall | F1-Score | |
|---|---|---|---|---|---|
| Self-rated Health | 0.5139 | 0.7333 | 0.7857 | 0.9167 | 0.8462 |
| Self-rated Physical Health | 0.3056 | 0.6000 | 0.7500 | 0.7500 | 0.7500 |
| Self-rated Mental Health | 0.4318 | 0.6667 | 0.7143 | 0.9091 | 0.8000 |
| Self-rated Social Health | 0.8846 | 0.9333 | 0.9286 | 1.0000 | 0.9630 |
| AUC | Accuracy | Precision | Recall | F1-Score | |
|---|---|---|---|---|---|
| Self-rated Health | 0.5179 | 0.4667 | 0.4444 | 0.5714 | 0.5000 |
| Self-rated Physical Health | 0.3750 | 0.4000 | 0.2500 | 0.1429 | 0.1818 |
| Self-rated Mental Health | 0.6161 | 0.6667 | 0.6250 | 0.7143 | 0.6667 |
| Self-rated Social Health | 0.5893 | 0.6000 | 0.5714 | 0.5714 | 0.5714 |
| AUC | Accuracy | Precision | Recall | F1-Score | |
|---|---|---|---|---|---|
| Self-rated Health | 0.7407 | 0.6667 | 0.7500 | 0.6667 | 0.7059 |
| Self-rated Physical Health | 0.7037 | 0.6667 | 0.7000 | 0.7778 | 0.7368 |
| Self-rated Mental Health | 0.6852 | 0.5333 | 0.7500 | 0.3333 | 0.4615 |
| Self-rated Social Health | 0.5000 | 0.6000 | 0.6154 | 0.8889 | 0.7273 |
| Feature Name | Mean|SHAP|Value | Mean SHAP Value | Importance Rank |
|---|---|---|---|
| num__Age | 5.01 | −2.32 | 1 |
| num__Road entrance | 4.82 | −0.07 | 2 |
| num__Public toilet | 3.70 | −0.11 | 3 |
| cat__Careers_1 | 2.86 | 0.29 | 4 |
| cat__Gender_2 | 1.77 | 0.40 | 5 |
| cat__Gender_1 | 1.53 | 0.29 | 6 |
| cat__Income_1 | 0.50 | 0.09 | 7 |
| num__Bus stop | 0.44 | 0.03 | 8 |
| num__School | 0.43 | −0.22 | 9 |
| num__Green space | 0.42 | 0.25 | 10 |
| Feature Name | Mean|SHAP|Value | Mean SHAP Value | Importance Rank |
|---|---|---|---|
| num__Age | 2.12 | −1.69 | 1 |
| num__Road entrance | 1.49 | 0.19 | 2 |
| num__Garbage transfer point | 1.06 | 0.57 | 3 |
| cat__Income_0 | 0.34 | 0.34 | 4 |
| cat__Careers_0 | 0.23 | 0.23 | 5 |
| cat__Income_3 | 0.19 | 0.01 | 6 |
| cat__Income_1 | 0.18 | −0.14 | 7 |
| cat__Income_2 | 0.16 | −0.11 | 8 |
| num__Square | 0.14 | −0.04 | 9 |
| num__Bus stop | 0.14 | −0.01 | 10 |
| Feature Name | Mean|SHAP|Value | Mean SHAP Value | Importance Rank |
|---|---|---|---|
| num__School | 1.73 | −0.62 | 1 |
| num__Road entrance | 1.73 | −0.46 | 2 |
| num__Community service center | 1.59 | −0.51 | 3 |
| num__Age | 1.48 | −0.89 | 4 |
| num__Square | 1.45 | −0.35 | 5 |
| num__Green space | 1.33 | −0.43 | 6 |
| num__Bus stop | 1.22 | 0.08 | 7 |
| cat__Settlements_1 | 1.10 | −0.19 | 8 |
| cat__Marital status_1 | 0.97 | −0.83 | 9 |
| num__Hospital | 0.91 | −0.28 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, X.; Liu, C.; Liu, W.; Hu, X.; Li, K. Analysis of the Correlation Between the Accessibility of Built Environment Elements and Residents’ Self-Rated Health in New Rural Communities. Land 2025, 14, 1867. https://doi.org/10.3390/land14091867
Yang X, Liu C, Liu W, Hu X, Li K. Analysis of the Correlation Between the Accessibility of Built Environment Elements and Residents’ Self-Rated Health in New Rural Communities. Land. 2025; 14(9):1867. https://doi.org/10.3390/land14091867
Chicago/Turabian StyleYang, Xiu, Chao Liu, Wei Liu, Ximin Hu, and Kehao Li. 2025. "Analysis of the Correlation Between the Accessibility of Built Environment Elements and Residents’ Self-Rated Health in New Rural Communities" Land 14, no. 9: 1867. https://doi.org/10.3390/land14091867
APA StyleYang, X., Liu, C., Liu, W., Hu, X., & Li, K. (2025). Analysis of the Correlation Between the Accessibility of Built Environment Elements and Residents’ Self-Rated Health in New Rural Communities. Land, 14(9), 1867. https://doi.org/10.3390/land14091867







