Covid-19 Airborne Transmission and Its Prevention: Waiting for Evidence or Applying the Precautionary Principle?
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. In Vitro Studies on Coronavirus
3.1.1. Evaluation of Sampling Methods
3.1.2. Survival Experiments
3.2. Environmental Monitoring (Air Samples)
3.2.1. Animal Coronaviruses
3.2.2. Common Human Coronavirus (HCoV)
3.2.3. SARS-CoV
3.2.4. MERS-CoV
3.2.5. SARS-CoV-2
3.3. Epidemiological and Airflow Model Studies
3.3.1. SARS and MERS
3.3.2. COVID-19
4. Discussion
5. Conclusions
- Viral load of infected clinical materials (upper and lower air ways, saliva, feces, urines, etc.) in symptomatic and asymptomatic persons and determination of the infectivity in those samples;
- Probability of aerosolization, droplet sizes and speed for different acts (sneezing, coughing, talking, breathing, singing, etc.), procedures (intubation, resuscitation, etc.) and plants (toilets, wastewater treatments, etc.);
- Virus survival in air according to different temperature and humidity conditions;
- Viral aerosol dynamics in the air according to the airflows and the viral survival;
- Minimal Infectious Dose and dose-response relations;
- Ways and amount of exposure for susceptible people in different settings (community, healthcare and non-healthcare working environments), including the fecal–oral route;
- Estimated reduction in exposure of different preventive measures (use of different types of masks, ventilation systems, etc.).
Supplementary Materials
Funding
Conflicts of Interest
References
- World Health Organization. 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 7 June 2020).
- World Health Organization. 2020. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 7 June 2020).
- Han, H.; Luo, Q.; Mo, F.; Long, L.; Zheng, W. SARS-CoV-2 RNA more readily detected in induced sputum than in throat swabs of convalescent COVID-19 patients. Lancet Infect. Dis. 2020, 20, 655–656. [Google Scholar] [CrossRef]
- Zou, L.; Ruan, F.; Huang, M.; Liang, L.; Huang, H.; Hong, Z.; Yu, J.; Kang, M.; Song, Y.; Xia, J.; et al. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. N. Engl. J. Med. 2020, 382, 1177–1179. [Google Scholar] [CrossRef] [PubMed]
- Holshue, M.L.; DeBolt, C.; Lindquist, S.; Lofy, K.H.; Wiesman, J.; Bruce, H.; Spitters, C.; Ericson, K.; Wilkerson, S.; Tural, A.; et al. Washington state 2019-nCoV case investigation team. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020, 382, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Lou, J.; Bai, Y.; Wang, M. COVID-19 Disease with positive fecal and negative pharyngeal and sputum viral tests. Am. J. Gastroenterol. 2020, 115, 790. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Feng, H.; Zhang, S.; Ni, Z.; Ni, L.; Chen, Y.; Zhuo, L.; Zhong, Z.; Qu, T. SARS-CoV-2 RNA detection of hospital isolation wards hygiene monitoring during the Coronavirus Disease 2019 outbreak in a Chinese hospital. Int. J. Infect. Dis. 2020, 94, 103–106. [Google Scholar] [CrossRef]
- Xiao, F.; Tang, M.; Zheng, X.; Liu, Y.; Li, X.; Shan, H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology. 2020, 158, 1831–1833. [Google Scholar] [CrossRef]
- Ma, X.; Su, L.; Zhang, Y.; Zhang, X.; Gai, Z.; Zhang, Z. Do children need a longer time to shed SARS-CoV-2 in stool than adults? J. Microbiol. Immunol. Infect. 2020, 53, 373–376. [Google Scholar] [CrossRef]
- Tang, A.; Tong, Z.D.; Wang, H.L.; Dai, Y.X.; Li, K.F.; Liu, J.N.; Wu, W.J.; Chen, Y.; Yu, M.L.; Li, P.; et al. Detection of Novel Coronavirus by RT-PCR in Stool Specimen from Asymptomatic Child, China. Emerg. Infect. Dis. 2020, 26, 1337–1339. [Google Scholar] [CrossRef]
- Frieden, T.R.; Lee, C.T. Identifying and Interrupting Superspreading Events—Implications for Control of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg. Infect. Dis. 2020, 26, 1059–1066. [Google Scholar] [CrossRef]
- European Commission Directive 2020/739 of 3 June 2020 Amending Annex III to Directive 2000/54/EC of the European Parliament and of the Council as Regards the Inclusion of SARS-CoV-2 in the List of Biological Agents Known to Infect Humans and Amending Commission Directive (EU) 2019/1833. Available online: https://op.europa.eu/en/publication-detail/-/publication/26c2097f-a626-11ea-bb7a-01aa75ed71a1/language-en (accessed on 7 June 2020).
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Pan, Y.; Zhang, D.; Yang, P.; Poon, L.L.M.; Wang, Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect. Dis. 2020, 20, 411–412. [Google Scholar] [CrossRef]
- To, K.K.W.; Tsang, O.T.Y.; Yip, C.C.Y.; Chan, K.H.; Wu, T.C.; Chan, J.M.C.; Leung, W.S.; Chik, T.S.H.; Choi, C.Y.C.; Kandamby, D.H.; et al. Consistent detection of 2019 novel coronavirus in saliva. Clin. Infect. Dis. 2020, ciaa149. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, C.; Zhu, S.; Shu, C.; Wang, D.; Song, J.; Song, Y.; Zhen, W.; Feng, Z.; Wu, G.; et al. Isolation of 2019-nCoV from a stool specimen of a laboratory-confirmed case of the coronavirus disease 2019 (COVID-19). China CDC Weekly 2020, 2, 123–124. [Google Scholar] [CrossRef]
- Sun, J.; Zhu, A.; Li, H.; Zheng, K.; Zhuang, Z.; Chen, Z.; Shi, Y.; Zhang, Z.; Chen, S.B.; Liu, X.; et al. Isolation of infectious SARS-CoV-2 from urine of a COVID-19 patient. Emerg. Microbes Infect. 2020, 9, 991–993. [Google Scholar] [CrossRef]
- World Health Organization. Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care; World Health Organization: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/112656/9789241507134_eng.pdf?sequence=1 (accessed on 7 June 2020).
- World Health Organization. 2020. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Scientific brief 29 March 2020. Available online: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations (accessed on 7 June 2020).
- Haas, C.N. Coronavirus and Environmental Engineering. Sci. Environ. Eng. Sci. 2020, 37. [Google Scholar] [CrossRef]
- Favre, J. No Evidence the New Coronavirus Spreads through the Air–but it’s Still Possible. The Conversation, UK, 13 February 2020. Available online: https://theconversation.com/theres-no-evidence-the-new-coronavirus-spreads-through-the-air-but-its-still-possible-131653 (accessed on 7 June 2020).
- Duguid, J.P. The size and duration of air-carriage of respiratory droplets and droplet-nuclei. J. Hyg. 1946, 4, 471–480. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.L.; Mead, K.R.; Lynch, R.A.; Hirst, D.V. Lifting the lid on toilet plume aerosol: A literature review with suggestions for future research. Am. J. Infect. Control 2013, 41, 254–258. [Google Scholar] [CrossRef]
- Deacon, J. The Microbial World—Airborne Microorganisms. Institute of Cell and Molecular Biology, and Biology Teaching Organisation, University of Edinburgh. 2001. Available online: http://archive.bio.ed.ac.uk/jdeacon/microbes/airborne.htm#Top (accessed on 7 June 2020).
- Anfinrud, P.; Stadnytskyi, V.; Bax, C.E.; Bax, A. Visualizing Speech-GeneratedOral Fluid Droplets with Laser Light Scattering. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Somsen, G.A.; van Rijn, C.; Kooij, S.; Bem, R.A.; Bonn, D. Small droplet aerosols in poorly ventilated spaces and SARS-CoV-2 transmission. Lancet Respir. Med. 2020, S2213–S2600, 30245–30249. [Google Scholar] [CrossRef]
- The American Society of Heating Refrigerating and Air-Conditioning Engineers. ASHRAE 2009. Available online: http://www.ashrae.org (accessed on 7 June 2020).
- Wells, W.F. On air-borne infection. Study II. Droplets and droplet nuclei. Am. J. Hyg. 1934, 20, 611–618. [Google Scholar]
- Chao, C.Y.; Wan, M.P. A study of the dispersion of expiratory aerosols in unidirectional downward and ceiling-return type airflows using a multiphase approach. Indoor Air 2006, 16, 296–312. [Google Scholar] [CrossRef]
- Wan, M.P.; Chao, C.Y.H. Transport characteristics of expiratory droplets and droplet nuclei in indoor environments with different ventilation air flow patterns. J. Biomech. Eng. T-ASME 2007, 129, 341–353. [Google Scholar] [CrossRef]
- Wan, M.P.; Chao, C.Y.H.; Ng, Y.D.; Sze To, G.N.; Yu, W.C. Dispersion of expiratory droplets in a general hospital ward with ceiling mixing type mechanical ventilation system. Aerosol. Sci. Technol. 2007, 41, 244–258. [Google Scholar] [CrossRef]
- Qian, H.; Li, Y.; Nielsen, P.V.; Hyldgaard, C.E.; Wong, T.W.; Chwang, A.T.Y. Dispersion of exhaled droplet nuclei in a two-bed hospital ward with three different ventilation systems. Indoor Air 2006, 16, 111–128. [Google Scholar] [CrossRef]
- Qian, H.; Li, Y.; Nielsen, P.V.; Hyldgaard, C.E. Dispersion of exhalation pollutants in a two-bed hospital ward with a downward ventilation system. Build. Environ. 2008, 43, 334–354. [Google Scholar] [CrossRef]
- Wang, B.; Zhang, A.; Sun, J.; Liu, H.; Hu, J.; Xu, L. Study of SARS transmission via liquid droplets in air. Trans. ASME 2005, 127, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Li, Y.; Chwang, A.T.Y.; Ho, P.L.; Seto, W.H. How far droplets can move in indoor environments – revisiting the Wells evaporation–falling curve. Indoor Air 2007, 17, 211–225. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Zhang, Z.; Li, X.T. Numerical study of the transport of droplets or particles generated by respiratory system indoors. Build. Environ. 2005, 40, 1032–1039. [Google Scholar] [CrossRef]
- Chen, C.; Zhao, B. Some questions on dispersion of human exhaled droplets in ventilation room: Answers from numerical investigation. Indoor Air. 2010, 20, 95–111. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic (1 April 2020); The National Academies Press: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Kutter, J.S.; Spronken, M.I.; Fraaij, P.L.; Fouchier, R.A.; Herfst, S. Transmission routes of respiratory viruses among humans. Curr. Opin. Virol. 2018, 28, 142–151. [Google Scholar] [CrossRef]
- Tellier, R.; Li, Y.; Cowling, B.J.; Tang, J.W. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019, 19, 101. [Google Scholar] [CrossRef]
- Jones, R.M.; Brosseau, L.M. Aerosol transmission of infectious disease. J. Occup. Environ. Med. 2015, 57, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS ONE Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Carducci, A.; Federigi, I.; Liu, D.; Thompson, J.R.; Verani, M. Making Waves: Coronavirus detection, presence and persistence in the water environment: State of the art and knowledge needs for public health. Water Res. 2020, 179, 115907. [Google Scholar] [CrossRef] [PubMed]
- Ijaz, M.K.; Karim, Y.G.; Sattar, S.A.; Johnson-Lussenburg, C.M. Development of methods to study the survival of airborne viruses. J. Virol. Methods 1987, 18, 87–106. [Google Scholar] [CrossRef]
- Agranovski, I.E.; Safatov, A.S.; Pyankov, O.V.; Sergeev, A.N.; Agafonov, A.P.; Ignatiev, G.M.; Ryabchikova, E.I.; Borodulin, A.I.; Sergeev, A.A.; Doerr, H.W.; et al. Monitoring of viable airborne SARS virus in ambient air. Atmos. Environ. 2004, 38, 3879–3884. [Google Scholar] [CrossRef]
- Tseng, C.C.; Li, C.S. Collection efficiencies of aerosol samplers for virus-containing aerosols. J. Aerosol Sci. 2005, 36, 593–607. [Google Scholar] [CrossRef]
- Kim, S.W.; Ramakrishnan, M.A.; Raynor, P.C.; Goyal, S.M. Effects of humidity and other factors on the generation and sampling of a coronavirus aerosol. Aerobiologia 2007, 23, 239–248. [Google Scholar] [CrossRef]
- Farnsworth, J.E.; Goyal, S.M.; Kim, S.W.; Kuehn, T.H.; Raynor, P.C.; Ramakrishnan, M.A.; Anantharaman, S.; Tang, W. Development of a method for bacteria and virus recovery from heating, ventilation, and air conditioning (HVAC) filters. J. Environ. Monit. 2006, 8, 1006–1013. [Google Scholar] [CrossRef]
- Ijaz, M.K.; Brunner, A.H.; Sattar, S.A.; Nair, R.C.; Johnson-Lussenburg, C.M. Survival characteristics of airborne human coronavirus 229E. J. Gen. Virol. 1985, 66, 2743–2748. [Google Scholar] [CrossRef]
- Prussin, A.J.; Schwake, D.O.; Lin, K.; Gallagher, D.L.; Buttling, L.; Marr, L.C. Survival of the Enveloped Virus Phi6 in Droplets as a Function of Relative Humidity, Absolute Humidity, and Temperature. Appl Environ. Microbiol. 2018, 84, e00551-e18. [Google Scholar] [CrossRef]
- Pyankov, O.V.; Bodnev, S.A.; Pyankova, O.G.; Agranovski, I.E. Survival of aerosolized coronavirus in the ambient air. J. Aerosol Sci. 2018, 115, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Van Doremalen, N.; Bushmaker, T.; Munster, V.J. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Eurosurveillance 2013, 18, 20590. [Google Scholar] [CrossRef] [PubMed]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Smither, S.J.; Eastaugh, L.S.; Findlay, J.S.; Lever, M.S. Experimental Aerosol Survival of SARS-CoV-2 in Artificial Saliva and Tissue Culture Media at Medium and High Humidity. Emerg. Microbes Infect. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.M.; Ko, G. Effect of ultraviolet germicidal irradiation on viral aerosols. Environ. Sci. Technol. 2007, 41, 5460–5465. [Google Scholar] [CrossRef] [PubMed]
- Verreault, D.; Moineau, S.; Duchaine, C. Methods for sampling of airborne viruses. Microbiol. Mol. Biol. Rev. 2008, 72, 413–444. [Google Scholar] [CrossRef]
- Bosch, A.; Sánchez, G.; Abbaszadegan, M.; Carducci, A.; Guix, S.; Le Guyader, F.S.; Netshikweta, R.; Pintó, R.M.; van der Poel, W.H.M.; Rutjes, S.; et al. Analytical Methods for Virus Detection in Water and Food. Food Anal. Methods 2011, 4, 4–12. [Google Scholar] [CrossRef]
- Gendron, L.; Verreault, D.; Veillette, M.; Moineau, S.; Duchaine, C. Evaluation of filters for the sampling and quantification of RNA phage aerosols. Aerosol Sci. Technol. 2010, 44, 893–901. [Google Scholar] [CrossRef]
- Turgeon, N.; Toulouse, M.-J.; Martel, B.; Moineau, S.; Duchaine, C. Comparison of five bacteriophages as models for viral aerosol studies. Appl. Environ. Microbiol. 2014, 80, 4242–4250. [Google Scholar] [CrossRef]
- Hermann, J.R.; Brockmeier, S.L.; Yoon, K.J.; Zimmerman, J.J. Detection of respiratory pathogens in air samples from acutely infected pigs. Can. J. Vet. Res. 2008, 72, 367–370. [Google Scholar] [PubMed]
- Alonso, C.; Goede, D.P.; Morrison, R.B.; Davies, P.R.; Rovira, A.; Marthaler, D.G.; Torremorell, M. Evidence of infectivity of airborne porcine epidemic diarrhea virus and detection of airborne viral RNA at long distances from infected herds. Vet. Res. 2014, 45, 73. [Google Scholar] [CrossRef] [PubMed]
- Alonso, C.; Raynor, P.C.; Davies, P.R.; Torremorell, M. Concentration, Size Distribution, and Infectivity of Airborne Particles Carrying Swine Viruses. PLoS ONE 2015, 10, e0135675. [Google Scholar] [CrossRef] [PubMed]
- Alonso, C.; Raynor, P.C.; Goyal, S.; Olson, B.A.; Alba, A.; Davies, P.R.; Torremorell, M. Assessment of air sampling methods and size distribution of virus-laden aerosols in outbreaks in swine and poultry farms. J. Vet. Diagn. Invest. 2017, 29, 298–304. [Google Scholar] [CrossRef]
- Borkenhagen, L.K.; Mallinson, K.A.; Tsao, R.W.; Ha, S.J.; Lim, W.H.; Toh, T.H.; Anderson, B.D.; Fieldhouse, J.K.; Philo, S.E.; Chong, K.S.; et al. Surveillance for respiratory and diarrheal pathogens at the human-pig interface in Sarawak, Malaysia. PLoS ONE 2018, 13, e0201295. [Google Scholar] [CrossRef]
- Coleman, K.K.; Nguyen, T.T.; Yadana, S.; Hansen-Estruch, C.; Lindsley, W.G.; Gray, G.C. Bioaerosol Sampling for Respiratory Viruses in Singapore’s Mass Rapid Transit Network. Sci. Rep. 2018, 8, 17476. [Google Scholar] [CrossRef]
- Memish, Z.A.; Almasri, M.; Assirri, A.; Al-Shangiti, A.M.; Gray, G.C.; Lednicky, J.A.; Yezli, S. Environmental sampling for respiratory pathogens in Jeddah airport during the 2013 Hajj season. Am. J. Infect. Control. 2014, 42, 1266–1269. [Google Scholar] [CrossRef]
- Xie, C.; Lau, E.H.; Yoshida, T.; Yu, H.; Wang, X.; Wu, H.; Wei, J.; Cowling, B.; Peiris, M.; Li, Y.; et al. Detection of Influenza and Other Respiratory Viruses in Air Sampled From a University Campus: A Longitudinal Study. Clin. Infect. Dis. 2020, 70, 850–858. [Google Scholar] [CrossRef]
- Nguyen, T.T.; Poh, M.K.; Low, J.; Kalimuddin, S.; Thoon, K.C.; Ng, W.C.; Anderson, B.D.; Gray, G.C. Bioaerosol Sampling in Clinical Settings: A Promising, Noninvasive Approach for Detecting Respiratory Viruses. Open Forum Infect. Dis. 2016, 4, ofw259. [Google Scholar] [CrossRef]
- Yadana, S.; Coleman, K.K.; Nguyen, T.T.; Hansen-Estruch, C.; Kalimuddin, S.; Thoon, K.C.; Low, J.G.H.; Gray, G.C. Monitoring for airborne respiratory viruses in a general pediatric ward in Singapore. J. Public Health Res. 2019, 8, 1407. [Google Scholar] [CrossRef]
- Booth, T.F.; Kournikakis, B.; Bastien, N.; Ho, J.; Kobasa, D.; Stadnyk, L.; Li, Y.; Spence, M.; Paton, S.; Henry, B.; et al. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J. Infect. Dis. 2005, 191, 1472–1477. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.H.; Wan, G.H.; Wu, Y.K.; Tsao, K.C. Airborne severe acute respiratory syndrome coronavirus concentrations in a negative-pressure isolation room. Infect. Control Hosp. Epidemiol. 2006, 27, 523–525. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wan, G.H.; Tsai, Y.H.; Wu, Y.K.; Tsao, K.C. A large-volume nebulizer would not be an infectious source for severe acute respiratory syndrome. Infect. Control Hosp. Epidemiol. 2004, 25, 1113–1115. [Google Scholar] [CrossRef] [PubMed]
- Azhar, E.I.; Hashem, A.M.; El-Kafrawy, S.A.; Sohrab, S.S.; Aburizaiza, A.S.; Farraj, S.A.; Hassan, A.M.; Al-Saeed, M.S.; Jamjoom, G.A.; Madani, T.A. Detection of the Middle East respiratory syndrome coronavirus genome in an air sample originating from a camel barn owned by an infected patient. mBio 2014, 5, e01450-e14. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Chang, S.Y.; Sung, M.; Park, J.H.; Kim, H.B.; Lee, H.; Choi, J.P.; Choi, W.S.; Min, J.Y. Extensive Viable Middle East Respiratory Syndrome (MERS) Coronavirus Contamination in Air and Surrounding Environment in MERS Isolation Wards. Clin. Infect. Dis. 2016, 63, 363–369. [Google Scholar] [CrossRef]
- Guo, Z.D.; Wang, Z.Y.; Zhang, S.F.; Li, X.; Li, L.; Li, C.; Cui, Y.; Fu, R.B.; Dong, Y.Z.; Chi, X.Y.; et al. Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020. Emerg. Infect. Dis. 2020, 26, 10–3201. [Google Scholar] [CrossRef]
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020, 582, 557–560. [Google Scholar] [CrossRef]
- Cheng, V.C.C.; Wong, S.C.; Chen, J.H.K.; Yip, C.C.Y.; Chuang, V.W.M.; Tsang, O.T.Y.; Sridhar, S.; Chan, J.F.W.; Ho, P.L.; Yuen, K.Y. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect. Control Hosp. Epidemiol. 2020, 41, 493–498. [Google Scholar] [CrossRef]
- Faridi, S.; Niazi, S.; Sadeghi, K.; Naddafi, K.; Yavarian, J.; Shamsipour, M.; Jandaghi, N.Z.S.; Sadeghniiat, K.; Nabizadeh, R.; Yunesian, M.; et al. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci. Total Environ. 2020, 725, 138401. [Google Scholar] [CrossRef]
- Ong, S.W.X.; Tan, Y.K.; Chia, P.Y.; Lee, T.H.; Ng, O.T.; Wong, M.S.Y.; Marimuthu, K. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA 2020, 323, 1610–1612. [Google Scholar] [CrossRef]
- Chia, P.Y.; Coleman, K.K.; Tan, Y.K.; Ong, S.W.X.; Gum, M.; Lau, S.K.; Lim, X.F.; Lim, A.S.; Sutjipto, S.; Lee, P.H.; et al. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat. Commun. 2020, 11, 2800. [Google Scholar] [CrossRef] [PubMed]
- Setti, L.; Passarini, F.; De Gennaro, G.; Barbieri, P.; Pallavicini, A.; Ruscio, M.; Piscitelli, P.; Colao, A.; Miani, A. Searching for SARS-COV-2 on Particulate Matter: A Possible Early Indicator of COVID-19 Epidemic Recurrence. Int. J. Environ. Res. Public Health 2020, 17, 2986. [Google Scholar] [CrossRef] [PubMed]
- Qian, H.; Miao, T.; Liu, L.; Zheng, X.; Luo, D.; Li, Y. Indoor transmission of SARS-CoV-2. medRxiv 2020. [Google Scholar] [CrossRef]
- McKinney, K.R.; Gong, Y.Y.; Lewis, T.G. Environmental transmission of SARS at Amoy Gardens. J. Environ. Health 2006, 68, 26–52. [Google Scholar] [PubMed]
- Yu, I.T.; Li, Y.; Wong, T.W.; Tam, W.; Chan, A.T.; Lee, J.H.W.; Leung, D.Y.C.; Ho, T. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N. Engl. J. Med. 2004, 350, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Duan, S.; Yu, I.T.; Wong, T.W. Multi-zone modeling of probable SARS virus transmission by airflow between flats in Block E, Amoy Gardens. Indoor Air 2005, 15, 96–111. [Google Scholar] [CrossRef]
- Chu, C.M.; Cheng, V.C.; Hung, I.F.; Chan, K.S.; Tang, B.S.F.; Tsang, T.H.F.; Chan, K.H.; Yuen, K.Y. Viral load distribution in SARS outbreak. Emerg. Infect. Dis. 2005, 11, 1882–1886. [Google Scholar] [CrossRef]
- Yip, C.; Chang, W.L.; Yeung, K.H.; Yu, I.T. Possible meteorological influence on the severe acute respiratory syndrome (SARS) community outbreak at Amoy Gardens, Hong Kong. J. Environ. Health 2007, 70, 39–46. [Google Scholar]
- Niu, J.; Tung, T.C. On-site quantification of re-entry ratio of ventilation exhausts in multi-family residential buildings and implications. Indoor Air 2008, 18, 12–26. [Google Scholar] [CrossRef]
- Gao, N.P.; Niu, J.L.; Perino, M.; Heiselberg, P. The airborne transmission of infection between flats in high-rise residential buildings: Tracer gas simulation. Build. Environ. 2008, 43, 1805–1817. [Google Scholar] [CrossRef]
- Gao, N.P.; Niu, J.L.; Perino, M.; Heiselberg, P. The airborne transmission of infection between flats in high-rise residential buildings: Particle simulation. Build. Environ. 2009, 44, 402–410. [Google Scholar] [CrossRef]
- Yu, I.T.; Qiu, H.; Tse, L.A.; Wong, T.W. Severe acute respiratory syndrome beyond Amoy Gardens: Completing the incomplete legacy. Clin. Infect. Dis. 2014, 58, 683–686. [Google Scholar] [CrossRef]
- Olsen, S.J.; Chang, H.L.; Cheung, T.Y.; Tang, A.F.Y.; Fisk, T.L.; Ooi, S.P.L.; Kuo, H.W.; Jiang, D.D.S.; Chen, K.T.; Lando, J.; et al. Transmission of the severe acute respiratory syndrome on aircraft. N. Engl. J. Med. 2003, 349, 2416–2422. [Google Scholar] [CrossRef]
- Han, Z.; To, G.N.; Fu, S.C.; Chao, C.Y.; Weng, W.; Huang, Q. Effect of human movement on airborne disease transmission in an airplane cabin: Study using numerical modeling and quantitative risk analysis. BMC Infect. Dis. 2014, 14, 434. [Google Scholar] [CrossRef]
- Lei, H.; Li, Y.; Xiao, S.; Lin, C.H.; Norris, S.L.; Wei, D.; Hu, Z.; Ji, S. Routes of transmission of influenza A H1N1, SARS CoV, and norovirus in air cabin: Comparative analyses. Indoor Air 2018, 28, 394–403. [Google Scholar] [CrossRef]
- You, R.; Lin, C.H.; Wei, D.; Chen, Q. Evaluating the commercial airliner cabin environment with different air distribution systems. Indoor Air 2019, 29, 840–853. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Update: Outbreak of severe acute respiratory syndrome--worldwide, 2003 [published correction appears in MMWR Morb Mortal Wkly Rep. 2003 Apr 4;52(13):284]. MMWR Morb. Mortal. Wkly Rep. 2003, 52, 241–248. [Google Scholar]
- World Health Organization. SARS-How a Global Epidemic Was Stopped; WHO Press: Geneva, Switzerland, 2006. [Google Scholar]
- Varia, M.; Wilson, S.; Sarwal, S.; McGeer, A.; Gournis, E.; Galanis, E.; Henry, B. Hospital Outbreak Investigation Team Investigation of a nosocomial outbreak of severe acute respiratory syndrome (SARS) in Toronto, Canada. CMAJ 2003, 169, 285–292. [Google Scholar]
- Christian, M.D.; Loutfy, M.; McDonald, L.C.; Martinez, K.F.; Ofner, M.; Wong, T.; Wallington, T.; Gold, W.L.; Mederski, B.; Green, K.; et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect. Dis. 2004, 10, 287–293. [Google Scholar] [CrossRef]
- Li, Y.; Huang, X.; Yu, I.T.; Wong, T.W.; Qian, H. Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air 2005, 15, 83–95. [Google Scholar] [CrossRef]
- Wong, T.W.; Lee, C.K.; Tam, W.; Lau, J.T.F.; Yu, T.S.; Lui, S.F.; Chan, P.K.S.; Li, Y.; Bresee, J.S.; Sung, J.J.Y.; et al. Cluster of SARS among medical students exposed to single patient, Hong Kong. Emerg. Infect. Dis. 2004, 10, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Yu, I.T.; Wong, T.W.; Chiu, Y.L.; Lee, N.; Li, Y. Temporal-spatial analysis of severe acute respiratory syndrome among hospital inpatients. Clin. Infect. Dis. 2005, 40, 1237–1243. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhao, B.; Yang, X.; Li, Y. Role of two-way airflow owing to temperature difference in severe acute respiratory syndrome transmission: Revisiting the largest nosocomial severe acute respiratory syndrome outbreak in Hong Kong. J. R. Soc. Interface 2011, 8, 699–710. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.; Li, Y.; Wong, T.W.; Hui, D.S.C. Role of fomites in SARS transmission during the largest hospital outbreak in Hong Kong. PLoS ONE 2017, 12, e0181558. [Google Scholar] [CrossRef]
- Xiao, S.; Li, Y.; Sung, M.; Wei, J.; Yang, Z. A study of the probable transmission routes of MERS-CoV during the first hospital outbreak in the Republic of Korea. Indoor Air 2018, 28, 51–63. [Google Scholar] [CrossRef]
- Jo, S.; Hong, J.; Lee, S.E.; Ki, M.; Choi, B.Y.; Sung, M. Airflow analysis of Pyeongtaek St Mary’s Hospital during hospitalization of the first Middle East respiratory syndrome patient in Korea. R. Soc. Open Sci. 2019, 6, 181164. [Google Scholar] [CrossRef]
- Wang, J.; Du, G. COVID-19 may transmit through aerosol. Ir. J. Med. Sci. 2020, 1–2. [Google Scholar] [CrossRef]
- Park, S.Y.; Kim, Y.M.; Yi, S.; Lee, S.; Na, B.J.; Kim, C.B.; Kim, J.I.; Kim, H.S.; Kim, Y.B.; Park, Y.; et al. Coronavirus Disease Outbreak in Call Center, South Korea. Emerg. Infect. Dis. 2020, 26, 8. [Google Scholar] [CrossRef]
- Cai, J.; Sun, W.; Huang, J.; Gamber, M.; Wu, J.; He, G. Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020. Emerg. Infect. Dis. 2020, 26, 1343–1345. [Google Scholar] [CrossRef]
- Hamner, L.; Dubbel, P.; Capron, I.; Ross, A.; Jordan, A.; Lee, J.; Lynn, J.; Ball, A.; Narwal, S.; Russell, S.; et al. High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice-Skagit County, Washington, March 2020. MMWR Morb. Mortal. Wkly Rep. 2020, 69, 606–610. [Google Scholar] [CrossRef]
- Hijnen, D.; Marzano, A.V.; Eyerich, K.; GeurtsvanKessel, C.; Giménez-Arnau, A.M.; Joly, P.; Vestergaard, C.; Sticherling, M.; Schmidt, E. SARS-CoV-2 Transmission from Presymptomatic Meeting Attendee, Germany. Emerg. Infect. Dis. 2020, 26, 8. [Google Scholar] [CrossRef]
- Lu, J.; Gu, J.; Li, K.; Xu, C.; Su, W.; Lai, Z.; Zhou, D.; Yu, C.; Xu, B.; Yan, Z. COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020. Emerg. Infect. Dis. 2020, 26, 1628–1631. [Google Scholar] [CrossRef]
- Heinzerling, A.; Stuckey, M.J.; Scheuer, T.; Xu, K.; Perkins, K.M.; Resseger, H.; Magill, S.; Verani, J.R.; Jain, S.; Acosta, M.; et al. Transmission of COVID-19 to Health Care Personnel During Exposures to a Hospitalized Patient-Solano County, California, February 2020. MMWR Morb. Mortal. Wkly Rep. 2020, 69, 472–476. [Google Scholar] [CrossRef]
- Wong, S.C.; Kwong, R.T.; Wu, T.C.; Chan, J.W.; Chu, M.Y.; Lee, S.Y.; Wong, H.Y.; Lung, D.C. Risk of nosocomial transmission of coronavirus disease 2019: An experience in a general ward setting in Hong Kong. J. Hosp. Infect. 2020, 105, 119–127. [Google Scholar] [CrossRef]
- Shen, Y.; Li, C.; Dong, H.; Wang, Z.; Martinez, L.; Sun, Z.; Handel, A.; Chen, Z.; Chen, E.; Ebell, M.; et al. Airborne Transmission of COVID-19: Epidemiologic Evidence from Two Outbreak Investigations (11 May 2020). Available online: https://ssrn.com/abstract (accessed on 7 June 2020).
- Guyatt, G.; Cairns, J.; Churchill, D.; Cook, D.; Haynes, B.; Hirsh, J.; Irvine, J.; Levine, M.; Levine, M.; Nishikawa, J.; et al. Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA 1992, 268, 2420–2425. [Google Scholar] [CrossRef]
- Rajagopaian, S.; Huang, S.; Brook, R.D. Flattening the curve in COVID-19 using personalised protective equipment: Lessons from air pollution. Heart 2020, 1–3. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Schmid, M.B.; Czypionka, T.; Bassler, D.; Gruer, L. Face masks for the public during the covid-19 crisis. BMJ 2020, 369, m1435. [Google Scholar] [CrossRef]
- Adhikari, U.; Chabrelie, A.; Weir, M.; Boehnke, K.; McKenzie, E.; Ikner, L.; Wang, M.; Wang, Q.; Young, K.; Haas, C.N.; et al. A Case Study Evaluating the Risk of Infection from Middle Eastern Respiratory Syndrome Coronavirus (MERS-CoV) in a Hospital Setting Through Bioaerosols. Risk Anal. 2019, 39, 2608–2624. [Google Scholar] [CrossRef]
- Buonanno, G.; Stabile, L.; Morawska, L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020, 141, 105794. [Google Scholar] [CrossRef]

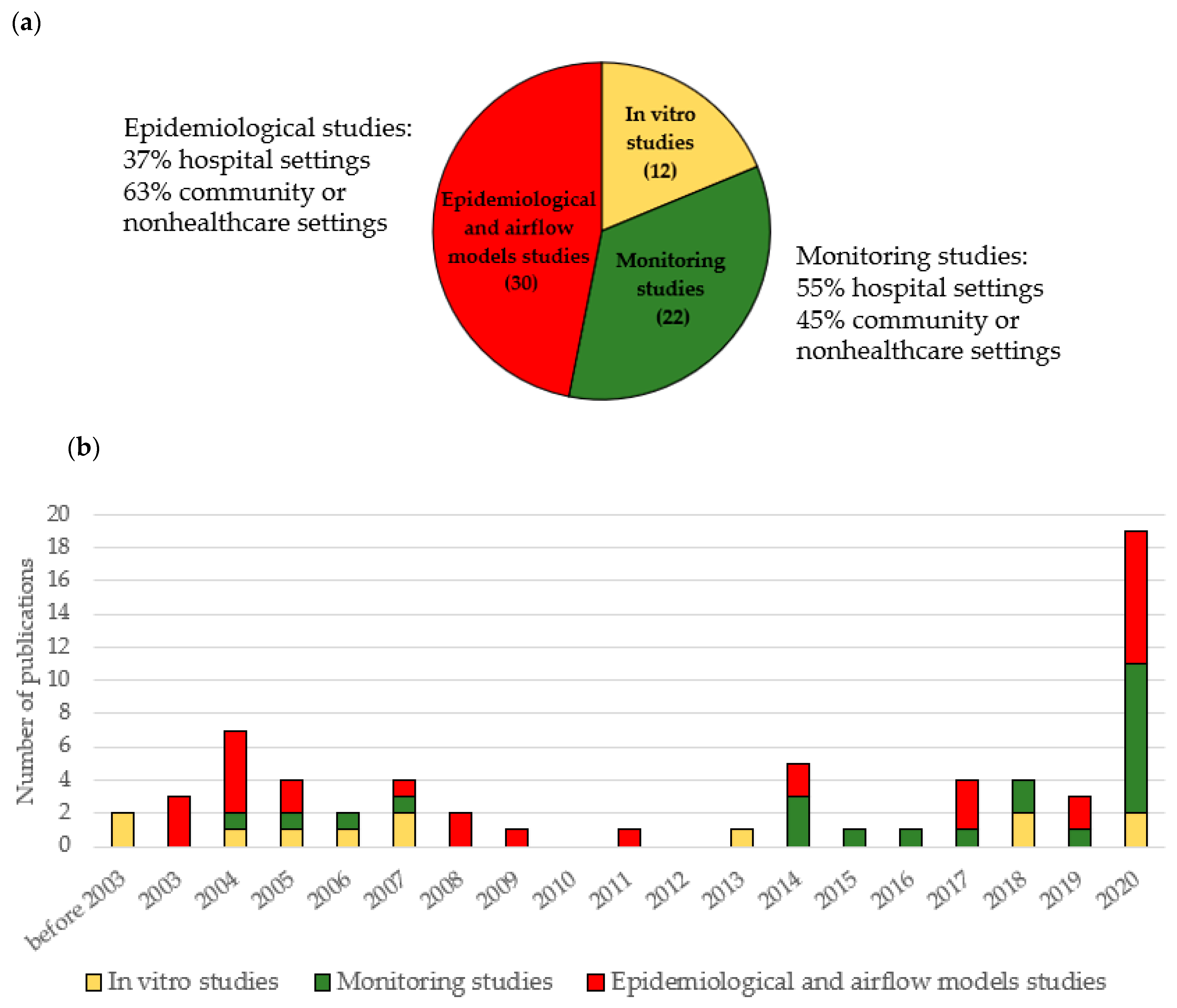
| Type of Study | Phage phi6 | Animal Coronaviruses | Common Human Coronaviruses * | SARS-CoV | MERS-CoV | SARS-CoV-2 | Total Number of the Studies | |
|---|---|---|---|---|---|---|---|---|
| In vitro studies | 2 | 3 | 2 | 2 | 2 | 2 | 12 ** | |
| Monitoring studies | Nonhealthcare settings or community | NA | 4 | 4 | 0 | 1 | 1 | 10 |
| Healthcare settings | NA | 0 | 2 | 3 | 1 | 6 | 12 | |
| Epidemiological and airflow models studies | Nonhealthcare settings or community | NA | 0 | 0 | 13 | 0 | 6 | 19 |
| Healthcare settings | NA | 0 | 0 | 7 | 2 | 2 | 11 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carducci, A.; Federigi, I.; Verani, M. Covid-19 Airborne Transmission and Its Prevention: Waiting for Evidence or Applying the Precautionary Principle? Atmosphere 2020, 11, 710. https://doi.org/10.3390/atmos11070710
Carducci A, Federigi I, Verani M. Covid-19 Airborne Transmission and Its Prevention: Waiting for Evidence or Applying the Precautionary Principle? Atmosphere. 2020; 11(7):710. https://doi.org/10.3390/atmos11070710
Chicago/Turabian StyleCarducci, Annalaura, Ileana Federigi, and Marco Verani. 2020. "Covid-19 Airborne Transmission and Its Prevention: Waiting for Evidence or Applying the Precautionary Principle?" Atmosphere 11, no. 7: 710. https://doi.org/10.3390/atmos11070710
APA StyleCarducci, A., Federigi, I., & Verani, M. (2020). Covid-19 Airborne Transmission and Its Prevention: Waiting for Evidence or Applying the Precautionary Principle? Atmosphere, 11(7), 710. https://doi.org/10.3390/atmos11070710







