Relationships between Exposure to Bioaerosols, Moldy Surface and Symptoms in French Mold-Damaged Homes
Abstract
1. Introduction
2. Experiments
2.1. House Selection and Bioaerosol Collection
2.2. Quantification of Biological Contaminants
2.3. Questionnaire
2.4. Statistical Analysis
3. Results
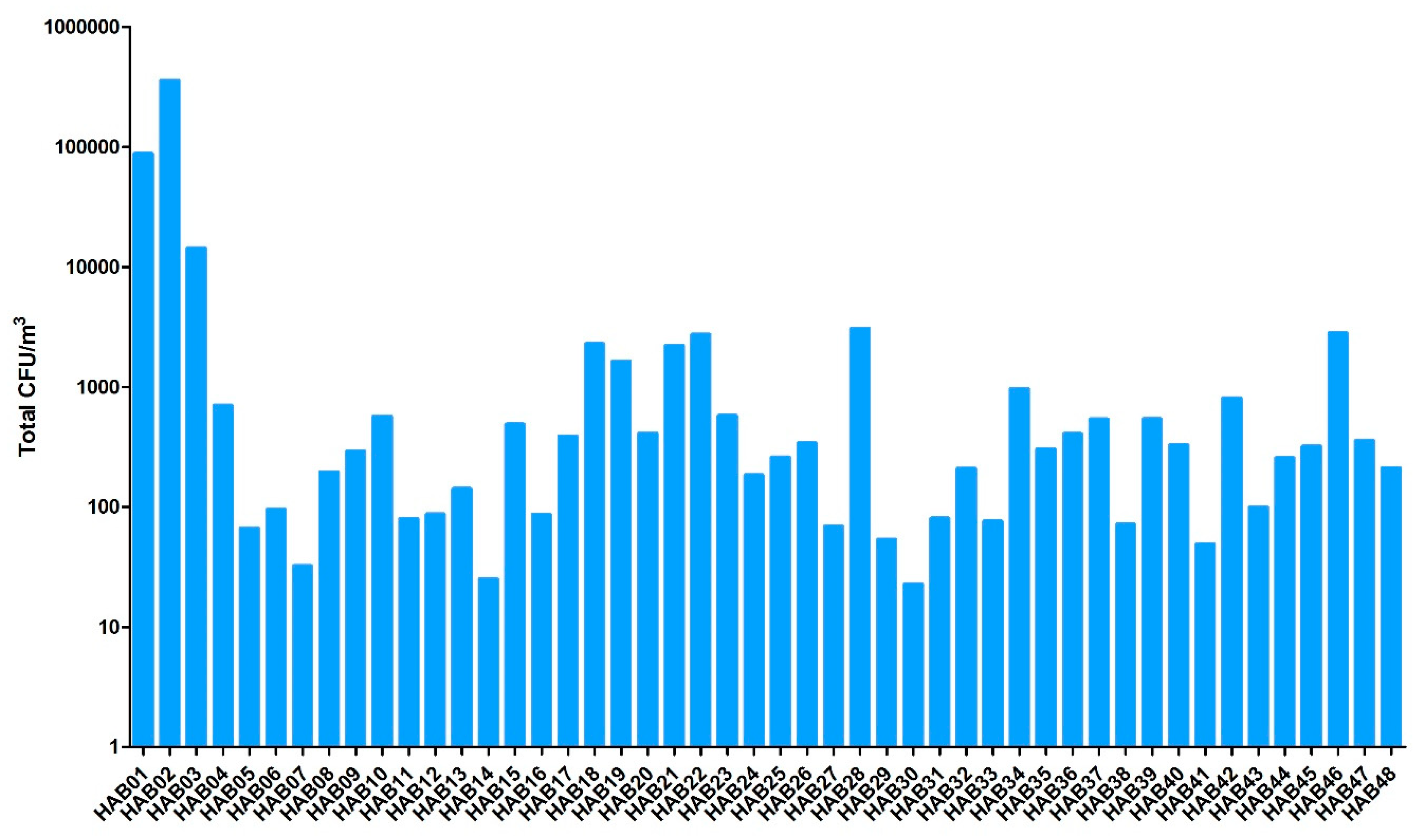
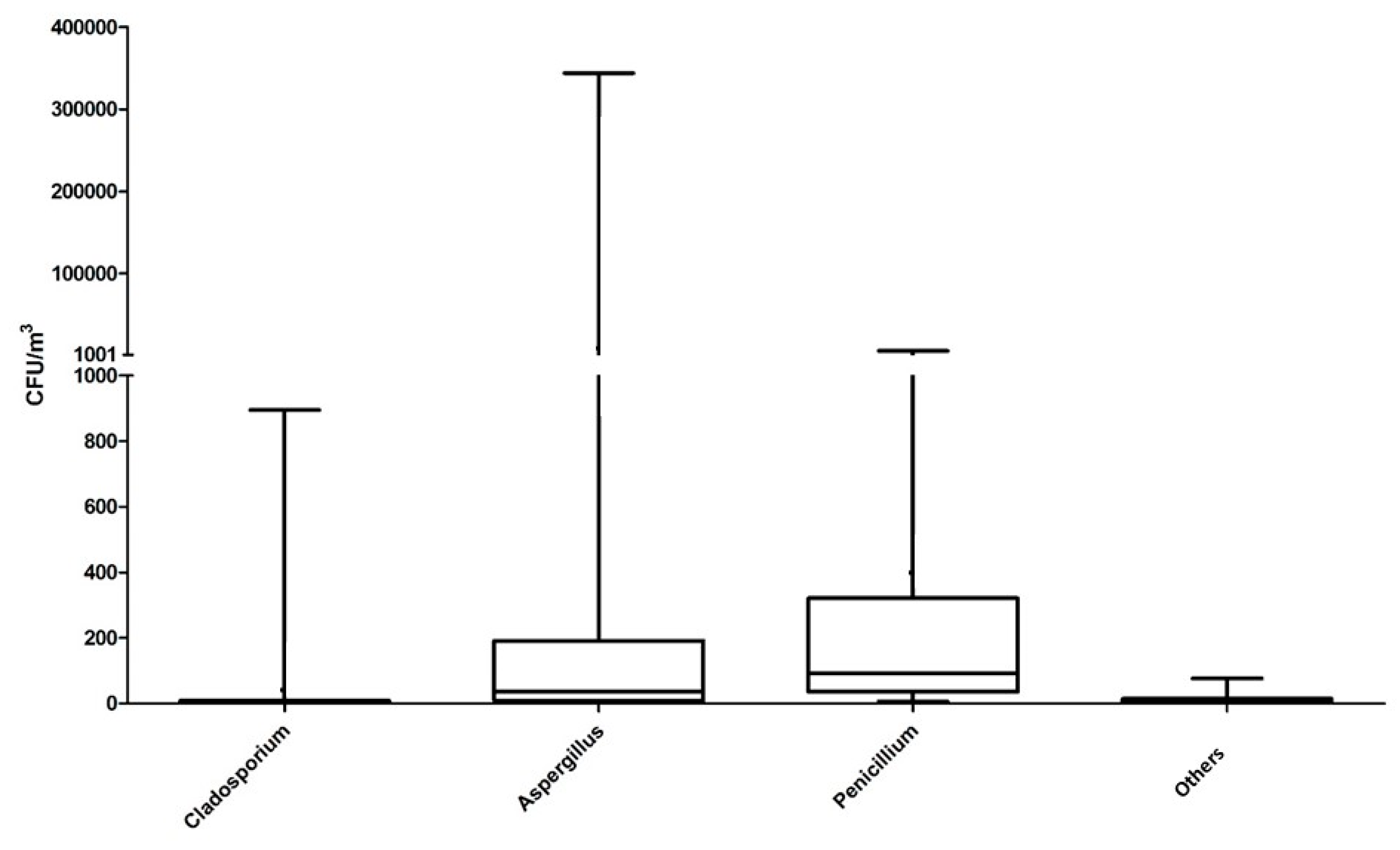
3.1. Characteristics of Bioaerosols
3.2. Health Status of Inhabitants
3.3. Statistical Analyses from Microbial and Health Data Collected in Mold-Damaged Homes
3.3.1. Correlations
3.3.2. Explanatory Variables
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- U.S. Environmental Protection Agency. Report to Congress on Indoor Air Quality; EPA/400/1-89/001C; National Service Center for Environmental Publications: Washington, DC, USA, 1989; Volume 2.
- Miller, D. Fungi as contaminants in indoor air. Atmos. Environ. 1992, 26, 2163–2172. [Google Scholar] [CrossRef]
- Lappalainen, H.; Salonen, H.; Lindroos, O.; Harju, R.; Reijula, K. Fungal species in mold-damaged and nondamaged office buildings in southern Finland. Scand. J. Work Environ. Health 2008, 4, 18–20. [Google Scholar]
- ANSES. Moisissures dans le bâti. Avis de l’ANSES, Rapport D’expertise Collective; ANSES: Maison-Alfort, France, 2016.
- Mudarri, D.H. Valuing the economic costs of allergic rhinitis, acute bronchitis, and asthma from exposure to indoor dampness and mold in the US. J. Environ. Public Health 2016, 2016, 2386596. [Google Scholar] [CrossRef]
- WHO Regional Office for Europe. WHO Guidelines for Indoor Air Quality: Dampness and Mould; WHO: Copenhagen, Denmark, 2009. [Google Scholar]
- Górny, R.L.; Reponen, T.; Willeke, K.; Schmechel, D.; Robine, E.; Boissier, M.; Grinshpun, S.A. Fungal fragments as indoor air biocontaminants. Environ. Microbiol. 2002, 68, 3522–3531. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.; Ji, Y.G.; Yoo, Y.; Kwon, M.H.; Choung, J.T. Submicron fungal fragments as another indoor biocontaminant in elementary schools. Environ. Sci. Processes Impacts 2015, 17, 1164–1172. [Google Scholar] [CrossRef] [PubMed]
- Rylander, R.; Lin, R.H. (1→3)-β-d-glucan—Relationship to indoor air-related symptoms, allergy and asthma. Toxicology 2000, 152, 47–52. [Google Scholar] [CrossRef]
- Veršilovskis, A.; De Saeger, S. Sterigmatocystin: Occurrence in foodstuffs and analytical methods—An overview. Mol. Nutr. Food Res. 2010, 54, 136–147. [Google Scholar] [CrossRef]
- Mendell, M.; Mirer, A.; Cheung, K.; Tong, M.; Douwes, J. Respiratory and Allergic Health Effects of Dampness, Mold, and Dampness-Related Agents: A Review of the Epidemiologic Evidence. Environ. Health Perspect. 2011, 119, 748–756. [Google Scholar] [CrossRef]
- Valkonen, M.; Täubel, M.; Pekkanen, J.; Tischer, C.; Rintala, H.; Zock, J.P.; Casas, L.; Probst-Hensch, N.; Forsberg, B.; Holm, M.; et al. Microbial characteristics in homes of asthmatic and non-asthmatic adults in the ECRHS cohort. Indoor Air 2018, 28, 16–27. [Google Scholar] [CrossRef]
- Zamfir, M.; Gerstner, D.G.; Walser, S.M.; Bünger, J.; Eikmann, T.; Heinze, S.; Kolk, A.; Nowak, D.; Raulf, M.; Sagunski, H.; et al. A systematic review of experimental animal studies on microbial bioaerosols: Dose-response data for the derivation of exposure limits. Int. J. Hyg. Environ. Health 2019, 222, 249–259. [Google Scholar] [CrossRef]
- Cabral, J. Can we use indoor fungi as bioindicators of indoor air quality? Historical perspectives and open questions. Sci. Total Environ. 2010, 408, 4285–4295. [Google Scholar] [CrossRef] [PubMed]
- Mendell, M.; Kumagai, K. Observation-based metrics for residential dampness and mold with dose–response relationships to health: A review. Indoor Air 2017, 27, 506–517. [Google Scholar] [CrossRef] [PubMed]
- Pottier, D.; André, V.; Rioult, J.; Bourreau, A.; Duhamel, C.; Bouchart, V.; Richard, E.; Guibert, M.; Verité, P.; Garon, D. Airborne molds and mycotoxins in Serpula lacrymans–damaged homes. Atmos. Pollut. Res. 2014, 5, 325–334. [Google Scholar] [CrossRef]
- Booth, C. The Genus Fusarium; Commonwealth Mycological Institute: Kew, UK, 1966; pp. 1–237. [Google Scholar]
- Domsch, K.H.; Gams, W.; Anderson, T.H. Compendium of Soil Fungi; Academic Press: London, UK, 1980; Volume 1, pp. 1–672. [Google Scholar]
- Klich, M.A. Identification of Common Aspergillus Species; Centraalbureau voor Schimmelcultures: Utrecht, The Netherlands, 2002; pp. 1–116. [Google Scholar]
- Pitt, J.I. The Genus Penicillium and Its Teleomorphic States Eupenicillium and Talaromyces; Academic Press: London, UK, 1979; pp. 1–634. [Google Scholar]
- Pitt, J.I. A Laboratory Guide to Common Penicillium Species; Food Science Australia: North Ryde, Australia, 2000; pp. 1–187. [Google Scholar]
- Samson, R.A.; Frisvad, J.C. Penicillium Subgenus Penicillium: New Taxonomic Schemes. Mycotoxins and Other Extrolites; Centraalbureau voor Schimmelcultures: Utrecht, The Netherlands, 2004; pp. 1–260. [Google Scholar]
- Samson, R.A.; Hoekstra, E.S.; Frisvad, J.C.; Filtenborg, O. Introduction to Food and Airborne Fungi; Centraalbureau voor Schimmelcultures: Utrecht, The Netherlands, 2002; pp. 1–389. [Google Scholar]
- Von Arx, J.A. The Genus of Fungi Sporulating in Pure Culture; Cramer: Vaduz, Liechtenstein, 1981; pp. 1–315. [Google Scholar]
- Visagie, C.; Houbraken, J.; Frisvad, J.; Hong, S.; Klaassen, C.; Perrone, G.; Seifert, K.; Varga, J.; Yaguchi, T.; Samson, R. Identification and nomenclature of the genus Penicillium. Stud. Mycol. 2014, 78, 343–371. [Google Scholar] [CrossRef]
- Beguin, H.; Nolard, N. Mould biodiversity in homes I. Air and surface analysis of 130 dwellings. Aerobiologia 1994, 10, 157–166. [Google Scholar] [CrossRef]
- Jovanovic, S.; Felder-Kennel, A.; Gabrio, T.; Kouros, B.; Link, B.; Maisner, V.; Piechotowski, I.; Schick, K.H.; Schrimpf, M.; Weidner, U.; et al. Indoor fungi levels in homes of children with and without allergy history. Int. J. Hyg. Environ. Health 2004, 207, 369–378. [Google Scholar] [CrossRef]
- Trout, T.; Bernstein, J.; Martinez, K.; Biagini, R.; Wallingford, K. Bioaerosol lung damage in a worker with repeated exposure to fungi in a water-damaged building. Environ. Health Perspct. 2001, 109, 641–644. [Google Scholar] [CrossRef]
- Chao, J.; Schwartz, J.; Milton, D.; Burge, H. Populations and determinants of airborne fungi in large office buildings. Environ. Health Perspect 2002, 110, 777–782. [Google Scholar] [CrossRef]
- Hargreaves, M.; Parappukkaran, S.; Morawska, L.; Hitchins, J.; He, C.; Gilbert, D. A pilot investigation into associations between indoor airborne fungal and non-biological particle concentrations in residential houses in Brisbane, Australia. Sci. Total Environ. 2003, 312, 89–101. [Google Scholar] [CrossRef]
- Frankel, M.; Bekö, G.; Timm, M.; Gustavsen, S.; Hansen, E.W.; Madsen, A.M. Seasonal Variations of Indoor Microbial Exposures and Their Relation to Temperature, Relative Humidity, and Air Exchange Rate. Appl. Environ. Microbiol. 2012, 78, 8289–8297. [Google Scholar] [CrossRef]
- Cho, S.J.; Cox-Ganser, J.; Park, J.H. Observational scores of dampness and mold associated with measurements of microbial agents and moisture in three public schools. Indoor Air 2016, 26, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Mensah-Attipoe, J.; Toyinbo, O. Fungal Growth and Aerosolization from Various Conditions and Materials. In Fungal Infection; Silva de Loreto, E., Ed.; IntechOpen: London, UK, 2019; pp. 1–10. [Google Scholar]
- Wolkoff, P. Indoor air humidity, air quality, and health—An overview. Int. J. Hyg. Environ. Health 2018, 221, 376–390. [Google Scholar] [CrossRef] [PubMed]
- Andersen, B.; Poulsen, R.; Hansen, G. Cellulolytic and xylanolytic activities of common indoor fungi. Int. Biodeterior. Biodegrad. 2016, 107, 111–116. [Google Scholar] [CrossRef]
- Flannigan, B.; Samson, R.A.; Miller, J.D. Microorganisms in Home and Indoor Work Environments: Diversity, Health Impacts, Investigation and Control, 1st ed.; CRC Press: London, UK, 2001; pp. 24, 62. [Google Scholar]
- Fischer, G.; Schwalbe, R.; Möller, M.; Ostrowski, R.; Dott, W. Species-specific production of microbial volatile organic compounds (MVOC) by airborne fungi from a compost facility. Chemosphere 1999, 39, 795–810. [Google Scholar] [CrossRef]
- Rundberget, T.; Skaar, I.; Flåøyen, A. The presence of Penicillium and Penicillium mycotoxins in food wastes. Int. J. Food Microbiol. 2004, 90, 181–188. [Google Scholar] [CrossRef]
- Kokkonen, M.; Jestoi, M.; Rizzo, A. The effect of substrate on mycotoxin production of selected Penicillium strains. Int. J. Food Microbiol. 2005, 99, 207–214. [Google Scholar] [CrossRef]
- Rand, T.; Giles, S.; Flemming, J.; Miller, D.; Puniani, E. Inflammatory and Cytotoxic Responses in Mouse Lungs Exposed to Purified Toxins from Building Isolated Penicillium brevicompactum Dierckx and P. chrysogenum Thom. Toxicol. Sci. 2005, 87, 213–222. [Google Scholar] [CrossRef]
- Jussila, J.; Komulainen, H.; Kosma, V.M.; Nevalainen, A.; Pelkonen, J.; Hirvonen, M.-R. Spores of Aspergillus versicolor isolated from indoor air of a moisture-damaged building provoke acute inflammation in mouse lungs. Inhal. Toxicol. 2002, 14, 1261–1277. [Google Scholar] [CrossRef]
- Jarvis, B.; Miller, D. Mycotoxins as harmful indoor air contaminants. Appl. Microbiol. Biotechnol. 2005, 66, 367–372. [Google Scholar] [CrossRef]
- Kurtzman, C.; Fell, J.; Boekhout, T. The Yeasts, 5th ed.; Elsevier Science: London, UK, 2010. [Google Scholar]
- Pollard, G.; Shaw, A.; Sowa, M.; Rand, T.; Thliveris, J.; Scott, J. Stachybotrys chartarum (atra) spore extract alters surfactant protein expression and surfactant function in isolated fetal rat lung epithelial cells, fibroblasts and human A549 cells. Open J. Pediatric 2013, 3, 243–256. [Google Scholar] [CrossRef]
- Beldman, G.; Searle van Leeuwen, M.; Rombouts, F.; Voragen, F. The cellulase of Trichoderma viride. Eur. J. Biochem. 1985, 146, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.W.; Ting, Y.T.; Horng, Y.J. Collection efficiency of liquid-based samplers for fungi in indoor air. Indoor Air 2019, 29, 380–389. [Google Scholar] [CrossRef]
- Holme, J.; Hägerhed-Engman, L.; Mattsson, J.; Sundell, J.; Bornehag, C.G. Culturable mold in indoor air and its association with moisture-related problems and asthma and allergy among Swedish children. Indoor Air 2010, 20, 329–340. [Google Scholar] [CrossRef]
- Jones, R.; Recer, G.; Hwang, S.; Lin, S. Association between indoor mold and asthma among children in Buffalo, New York. Indoor Air 2011, 21, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Reponen, T.; Hyvärinen, A.; Ruuskanen, J.; Raunemaa, T.; Nevalainen, A. Comparison of concentrations and size distributions of fungal spores in buildings with and without mould problems. J. Aerosol. Sci. 1994, 25, 1595–1603. [Google Scholar] [CrossRef]
- Libert, X.; Chasseur, C.; Bladt, S.; Packeu, A.; Bureau, F.; Roosens, N.; De Keersmaecker, S. Development and performance assessment of a qualitative SYBR® green real-time PCR assay for the detection of Aspergillus versicolor in indoor air. Appl. Microbiol. Biotechnol. 2015, 99, 7267–7282. [Google Scholar] [CrossRef][Green Version]
- Vesper, S.; Wymer, L.; Cox, D.; Dewalt, G. Populations of some molds in water-damaged homes may differ if the home was constructed with gypsum drywall compared to plaster. Sci. Total Environ. 2016, 562, 446–450. [Google Scholar] [CrossRef]
- Delanoë, A.; Guillamin, M.; Heutte, N.; Gente, S.; Séguin, V.; Garon, D. Interest of the qPCR method calibrated with flow cytometry to quantify Aspergillus versicolor in mold-damaged homes and comparison with the cultural approach. Atmospheric. Pollut. Res. 2018, 9, 871–876. [Google Scholar] [CrossRef]
- Lignell, U.; Meklin, T.; Rintala, H.; Hyvärinen, A.; Vepsäläinen, A.; Pekkanen, J.; Nevalainen, A. Evaluation of quantitative PCR and culture methods for detection of house dust fungi and streptomycetes in relation to moisture damage of the house. Lett. Appl. Microbiol. 2008, 47, 303–308. [Google Scholar] [CrossRef]
- Degois, J.; Clerc, F.; Simon, X.; Bontemps, C.; Leblond, P.; Duquenne, P. First Metagenomic Survey of the Microbial Diversity in Bioaerosols Emitted in Waste Sorting Plants. Ann. Work Expo. Health 2017, 61, 1076–1086. [Google Scholar] [CrossRef]
- Kettleson, E.; Adhikari, A.; Vesper, S.; Coombs, K.; Indugula, R.; Reponen, T. Key determinants of the fungal and bacterial microbiomes in homes. Environ. Res 2015, 138, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Hurraß, J.; Heinzow, B.; Aurbach, U.; Bergmann, K.C.; Bufe, A.; Buzina, W.; Cornely, O.A.; Engelhart, S.; Fischer, G.; Gabrio, T.; et al. Medical diagnostics for indoor mold exposure. Int. J. Hyg. Environ. Health 2017, 220, 305–328. [Google Scholar] [CrossRef] [PubMed]
- Seltzer, J.M.; Fedoruk, M.J. Health effects of mold in children. Pediatric Clin. N. Am. 2007, 54, 309–333. [Google Scholar] [CrossRef] [PubMed]
- Takigawa, T.; Wang, B.L.; Sakano, N.; Wang, D.H.; Ogino, K.; Kishi, R. A longitudinal study of environmental risk factors for subjective symptoms associated with sick building syndrome in new dwellings. Sci. Total Environ. 2009, 407, 5223–5228. [Google Scholar] [CrossRef] [PubMed]
- Fungand, F.; Hughson, W.G. Health Effects of Indoor Fungal Bioaerosol Exposure. Appl. Occup. Environ. Hyg. 2003, 18, 535–544. [Google Scholar]
- Hernberg, S.; Sripaiboonkij, P.; Quansah, R.; Jaakkola, J.; Jaakkola, M. Indoor molds and lung function in healthy adults. Respir. Med. 2014, 108, 677–684. [Google Scholar] [CrossRef]
- Richerson, H.B.; Bernstein, I.L.; Fink, J.N.; Hunninghake, G.W.; Novey, H.S.; Reed, C.E.; Salvaggio, J.E.; Schuyler, M.R.; Schwartz, H.J.; Stechschulte, D.J. Guidelines for the Clinical Evaluation of Hypersensitivity Pneumonitis. Report of the Subcommittee on Hypersensitivity Pneumonitis. J. Allergy Clin. Immunol. 1989, 84, 839–844. [Google Scholar] [CrossRef]
- Packer, C.N.; Stewart-Brown, S.; Fowle, S.E. Damp housing and adult health: Results from a lifestyle study in Worcester, England. J. Epidem. Comm. Health 1994, 48, 555–559. [Google Scholar] [CrossRef]
- Tiesler, C.M.; Thiering, E.; Tischer, C.; Lehmann, I.; Schaaf, B.; von Berg, A.; Heinrich, J. Exposure to visible mould or dampness at home and sleep problems in children: Results from the LISAplus study. Environ. Res. 2015, 137, 357–363. [Google Scholar] [CrossRef]
- Liao, L.Y.; Chen, K.M.; Chung, W.S.; Chien, J.Y. Efficacy of a respiratory rehabilitation exercise training package in hospitalized elderly patients with acute exacerbation of COPD: A randomized control trial. Int. J. Chronic Obstr. Pulm. Dis. 2015, 10, 1703–1709. [Google Scholar]
- Platt, S.D.; Martin, C.J.; Hunt, S.M.; Lewis, C.W. Damp housing, mould growth, and symptomatic health state. Br. Med. J. 1989, 298, 1673–1678. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.; Bearman, N.; Thornton, C.R.; Husk, K.; Osborne, N. Indoor fungal diversity and asthma: A meta-analysis and systematic review of risk factors. J. Allergy Clin. Immunol. 2015, 135, 110–122. [Google Scholar] [CrossRef] [PubMed]
- Douwes, J.; Pearce, N.; Heederik, D. Does environmental endotoxin exposure prevent asthma? Thorax 2002, 57, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Liebers, V.; Raulf-Heimsoth, M.; Brüning, T. Health effects due to endotoxin inhalation (review). Arch. Toxicol. 2008, 82, 203–210. [Google Scholar] [CrossRef]
- Huttunen, K.; Pelkonen, J.; Nielsen, K.F.; Nuutinen, U.; Jussila, J.; Hirvonen, M.R. Synergistic Interaction in Simultaneous Exposure to Streptomyces californicus and Stachybotrys chartarum. Environ. Health Perspect. 2004, 112, 659–665. [Google Scholar] [CrossRef]
| Data Documented | Type of Answers | |
|---|---|---|
| Habits of inhabitants | Daily time spent in the house; daily ventilation of room duration; ownership of a pet; presence of plants inside the house; Use of an absorber/dehumidifier | Yes/No |
| Building | Mold-contaminated surface | Categories Low (<0.2 m2)/Moderate (between 0.2 to 3 m2)/High (>3 m2) |
| Type of ventilation | Type of ventilation (Natural/Mechanical) | |
| Type of heating system | Type of heater (Electric/Gas/Heating oil) | |
| Moldy odor; history of water damage | Yes/No | |
| Symptoms | Allergy | Yes/No |
| Anxiety; asthma aggravation; clogged nose; cough; dizziness; dyspnea; expectorations; eye irritation; fever; flu-like symptoms; headache; insomnia; itching; muscular pain; respiratory pain; skin rash; sinusitis; sore throat | Yes/No and Intensity (Null/Weak/Moderate/Strong) | |
| Physical Characteristics | Mean | Median | Standard Deviation | Min | Max | Interquartile Range |
|---|---|---|---|---|---|---|
| Temperature of room (°C) | 21.99 | 22.25 | 2.51 | 12.64 | 26.10 | 3.28 |
| Relative Humidity of room (%) | 60.68 | 60.50 | 7.55 | 44.84 | 74.30 | 13.30 |
| Particles from 0.3 to 20 µm per m3 air | 1.16 × 108 | 3.57 × 107 | 3.07 × 108 | 7.80 × 106 | 2.01 × 109 | 5.74 × 107 |
| Fungal Species | Frequency (n = 48) | Mean Value (CFU m−3 of Air) |
|---|---|---|
| Penicillium chrysogenum | 36 | 243.04 |
| Aspergillus versicolor | 35 | 9321.47 |
| Penicillium crustosum | 32 | 37.68 |
| Penicillium brevicompactum | 30 | 38.36 |
| Aspergillus fumigatus | 20 | 2.18 |
| Penicillium glabrum | 19 | 17.79 |
| Penicillium expansum | 13 | 1.61 |
| Penicillium olsonii | 13 | 15.30 |
| Aspergillus flavus | 10 | 0.94 |
| Aspergillus niger | 10 | 0.26 |
| Botrytis cinerea | 10 | 1.68 |
| Cladosporium cladosporioides | 9 | 33.01 |
| Penicillium nalgiovense | 9 | 1.90 |
| Rhodotorula mucilaginosa | 9 | 0.68 |
| Aspergillus sydowii | 8 | 9.83 |
| Cladosporium herbarum | 8 | 6.60 |
| Chaetomium globosum | 7 | 0.40 |
| Paecilomyces variotii | 7 | 1.09 |
| Penicillium citrinum | 7 | 2.51 |
| Penicillium waksmanii | 7 | 1.93 |
| Aspergillus pseudoglaucus | 6 | 1.67 |
| Cladosporium sphaerospermum | 6 | 1.61 |
| Penicillium italicum | 5 | 1.00 |
| Penicillium piceum | 5 | 0.30 |
| Penicillium purpurogenum | 5 | 6.45 |
| Penicillium simplicissimum | 5 | 0.52 |
| Symptom | Occurrence | Weak Intensity | Moderate Intensity | Strong Intensity |
|---|---|---|---|---|
| Clogged nose | 75.00 | 11.54 | 23.08 | 40.38 |
| Dyspnea | 75.00 | 11.54 | 32.69 | 30.77 |
| Insomnia | 69.23 | 9.62 | 26.92 | 32.69 |
| Itching | 67.31 | 17.31 | 26.92 | 23.08 |
| Sore throat | 59.62 | 21.15 | 30.77 | 7.69 |
| Headaches | 59.62 | 26.92 | 25.00 | 7.69 |
| Eye irritation | 55.77 | 11.50 | 28.85 | 15.38 |
| Couch | 53.85 | 15.38 | 26.92 | 11.54 |
| Skin rash | 42.31 | 15.38 | 25.00 | 1.92 |
| Respiratory pain | 40.38 | 19.23 | 17.31 | 3.85 |
| Sinusitis | 34.62 | 9.62 | 15.38 | 9.62 |
| Expectorations | 32.69 | 1.92 | 23.08 | 7.69 |
| Muscular pain | 30.77 | 23.08 | 5.77 | 1.92 |
| Flu-like symptoms | 30.77 | 21.15 | 9.62 | 0.00 |
| Asthma aggravation | 25.00 | 1.92 | 9.62 | 13.46 |
| Anxiety | 23.08 | 7.69 | 13.46 | 1.92 |
| Dizziness | 19.23 | 13.46 | 3.85 | 1.92 |
| Fever | 17.31 | 9.62 | 3.85 | 3.85 |
| Fungal Concentration | Mold-Contaminated Surface 1 | N | Median | p-Value (Mann–Whitney Test) |
|---|---|---|---|---|
| Total CFU m−3 | Low | 8 | 257.50 | 0.8681 |
| Moderate | 29 | 212.00 | ||
| Moderate | 29 | 212.00 | 0.0167 * | |
| High | 11 | 408.00 | ||
| Low | 8 | 257.50 | 0.0632 | |
| High | 11 | 408.00 | ||
| Aspergillus versicolor CFU m−3 | Low | 8 | 0.00 | 0.0155 * |
| Moderate | 29 | 17.50 | ||
| Moderate | 29 | 17.50 | 0.0577 | |
| High | 11 | 122.00 | ||
| Low | 8 | 0.00 | 0.0035 * | |
| High | 11 | 122.00 | ||
| Penicillium chrysogenum CFU m−3 | Low | 8 | 11.40 | 0.6947 |
| Moderate | 29 | 7.78 | ||
| Moderate | 29 | 7.78 | 0.0190 * | |
| High | 11 | 32.90 | ||
| Low | 8 | 11.40 | 0.0465 * | |
| High | 11 | 32.90 | ||
| Penicillium crustosum CFU m−3 | Low | 8 | 3.86 | 0.3934 |
| Moderate | 29 | 0.96 | ||
| Moderate | 29 | 0.96 | 0.0549 | |
| High | 11 | 5.07 | ||
| Low | 8 | 3.86 | 0.4308 | |
| High | 11 | 5.07 |
| Explanatory Variable. | Symptom | N | Median | p-Value (Mann–Whitney or Kruskal–Wallis Test) | |
|---|---|---|---|---|---|
| A. versicolor (CFU m−3) | Dizziness | Yes | 10 | 2.1 × 102 | 0.0038 * |
| No | 39 | 9.46 | |||
| Fever | Yes | 9 | 2.1 × 102 | 0.0315 * | |
| No | 40 | 11.95 | |||
| Headache | Yes | 29 | 40.30 | 0.0154 * | |
| No | 20 | 6.16 | |||
| Itching | Null | 17 | 17.50 | 0.0438 * | |
| Weak | 7 | 5.65 | |||
| Moderate | 14 | 4.68 | |||
| Strong | 11 | 1.6 × 102 | |||
| Expectorations | Yes | 16 | 64.15 | 0.0489 * | |
| No | 33 | 11.10 | |||
| P. chrysogenum (CFU m−3) | Fever | Yes | 9 | 1.1 × 102 | 0.0197 * |
| No | 40 | 7.92 | |||
| Expectorations | Yes | 16 | 31.55 | 0.0053 * | |
| No | 33 | 3.78 | |||
| P. crustosum (CFU m−3) | Fever | Yes | 9 | 9.72 | 0.0344 * |
| No | 40 | 2.32 | |||
| Cough | Yes | 28 | 4.95 | 0.0418 * | |
| No | 21 | 0.00 | |||
| Headache | Yes | 29 | 5.07 | 0.0163 * | |
| No | 20 | 0.43 | |||
| Insomnia | Yes | 36 | 4.36 | 0.0359 * | |
| No | 13 | 0.00 | |||
| Endotoxins (ng m−3) | Dyspnea | Yes | 36 | 3.75 | 0.0052 * |
| No | 13 | 11.11 | |||
| Flu-like symptom | Yes | 13 | 2.16 | 0.0149 * | |
| No | 36 | 7.62 | |||
| Particles of 2–15 µm diameter (per m3 of air) | Dizziness | Yes | 10 | 6.1 × 105 | 0.0136 * |
| No | 39 | 3.1 × 105 | |||
| Headache | Yes | 29 | 4.4 × 105 | 0.0419 * | |
| No | 20 | 2.7 × 105 | |||
| Relative humidity (%) | Clogged nose | Yes | 37 | 60.80 | 0.0315 * |
| No | 12 | 55.28 | |||
| Expectorations | Yes | 16 | 68.50 | 0.0313 * | |
| No | 33 | 60.30 | |||
| Sore throat | Yes | 29 | 61.58 | 0.0451 * | |
| No | 20 | 55.68 | |||
| Explanatory Variable | Symptom | N | Low | Moderate | High | p-Value (chi² or Fisher Exact Test) | |
|---|---|---|---|---|---|---|---|
| Contaminated surface 1 | Dyspnea | Yes | 36 | 3 | 23 | 10 | 0.0354 * |
| No | 13 | 5 | 7 | 1 | |||
| Headache | Yes | 29 | 3 | 16 | 10 | 0.0385 * | |
| No | 20 | 5 | 14 | 1 | |||
| Expectorations | Yes | 16 | 10 | 2 | 4 | 0.0001 * | |
| No | 33 | 1 | 6 | 26 | |||
| Explanatory Variable | Symptom | N | Yes | No | p-Value (chi² or Fisher Exact Test) | |
|---|---|---|---|---|---|---|
| Moldy odor | Anxiety | Yes | 17 | 11 | 6 | 0.0131 * |
| No | 32 | 9 | 23 | |||
| Dyspnea | Yes | 36 | 18 | 18 | 0.0295 * | |
| No | 13 | 2 | 11 | |||
| Flu-like symptom | Yes | 13 | 9 | 4 | 0.0150 * | |
| No | 36 | 11 | 25 | |||
| Headache | Yes | 29 | 13 | 16 | 0.0138 * | |
| No | 20 | 16 | 4 | |||
| Muscular pain | Yes | 15 | 10 | 5 | 0.0145 * | |
| No | 34 | 10 | 24 | |||
| Expectorations | Yes | 16 | 10 | 6 | 0.0315 * | |
| No | 33 | 10 | 23 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delanoë, A.; Heutte, N.; Gente, S.; Séguin, V.; Garon, D. Relationships between Exposure to Bioaerosols, Moldy Surface and Symptoms in French Mold-Damaged Homes. Atmosphere 2020, 11, 223. https://doi.org/10.3390/atmos11030223
Delanoë A, Heutte N, Gente S, Séguin V, Garon D. Relationships between Exposure to Bioaerosols, Moldy Surface and Symptoms in French Mold-Damaged Homes. Atmosphere. 2020; 11(3):223. https://doi.org/10.3390/atmos11030223
Chicago/Turabian StyleDelanoë, Antoine, Natacha Heutte, Stéphanie Gente, Virginie Séguin, and David Garon. 2020. "Relationships between Exposure to Bioaerosols, Moldy Surface and Symptoms in French Mold-Damaged Homes" Atmosphere 11, no. 3: 223. https://doi.org/10.3390/atmos11030223
APA StyleDelanoë, A., Heutte, N., Gente, S., Séguin, V., & Garon, D. (2020). Relationships between Exposure to Bioaerosols, Moldy Surface and Symptoms in French Mold-Damaged Homes. Atmosphere, 11(3), 223. https://doi.org/10.3390/atmos11030223





