Focused Ultrasound-Induced Cavitation Sensitizes Cancer Cells to Radiation Therapy and Hyperthermia
Abstract
1. Introduction
2. Materials and Methods
2.1. Tumor Cell Lines and Cell Culturing
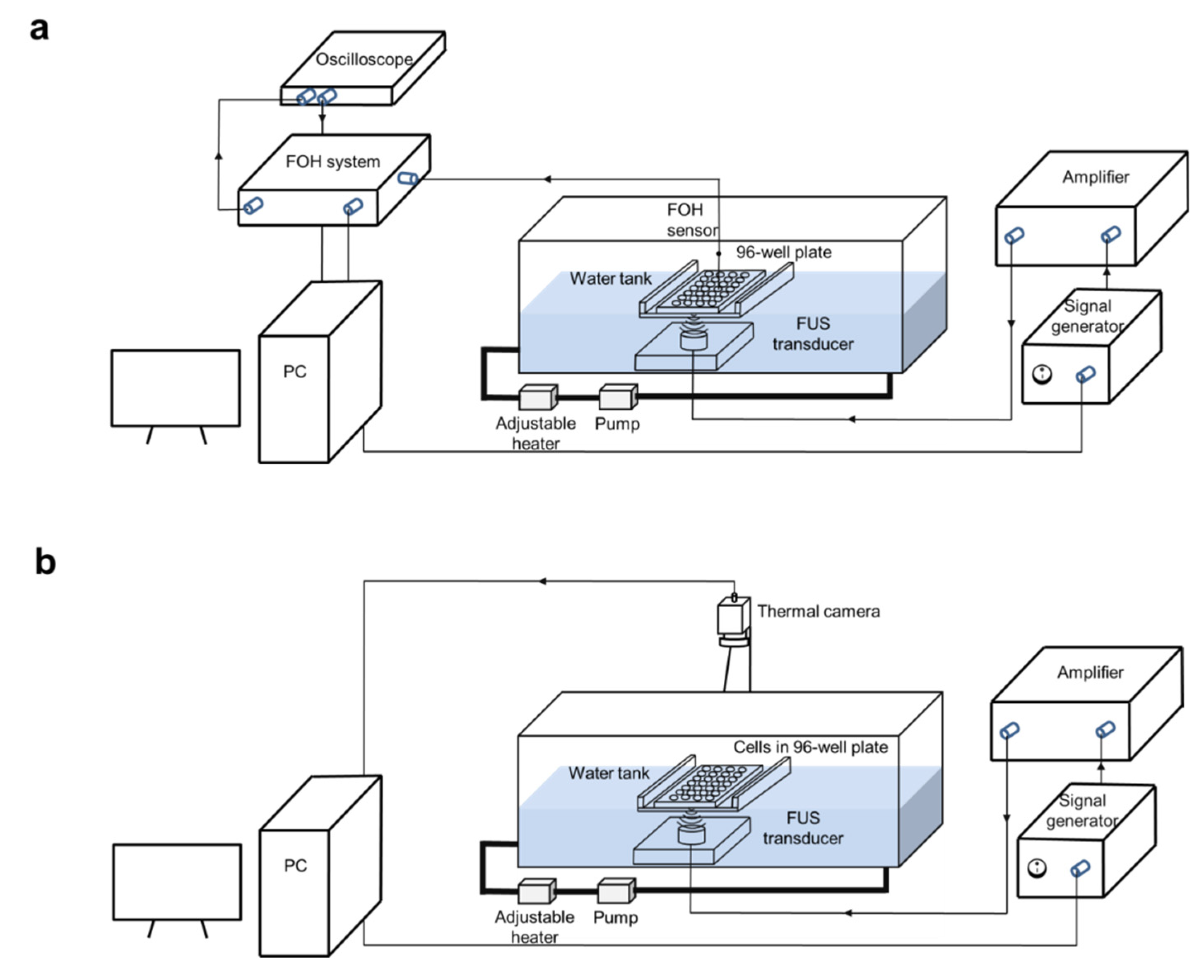
2.2. FUS In Vitro System
2.3. Cavitation Dose Measurement with a Fiber-Optic Hydrophone (FOH)
2.4. Cavitation Dose Measurement with Terephthalic Acid (TA)
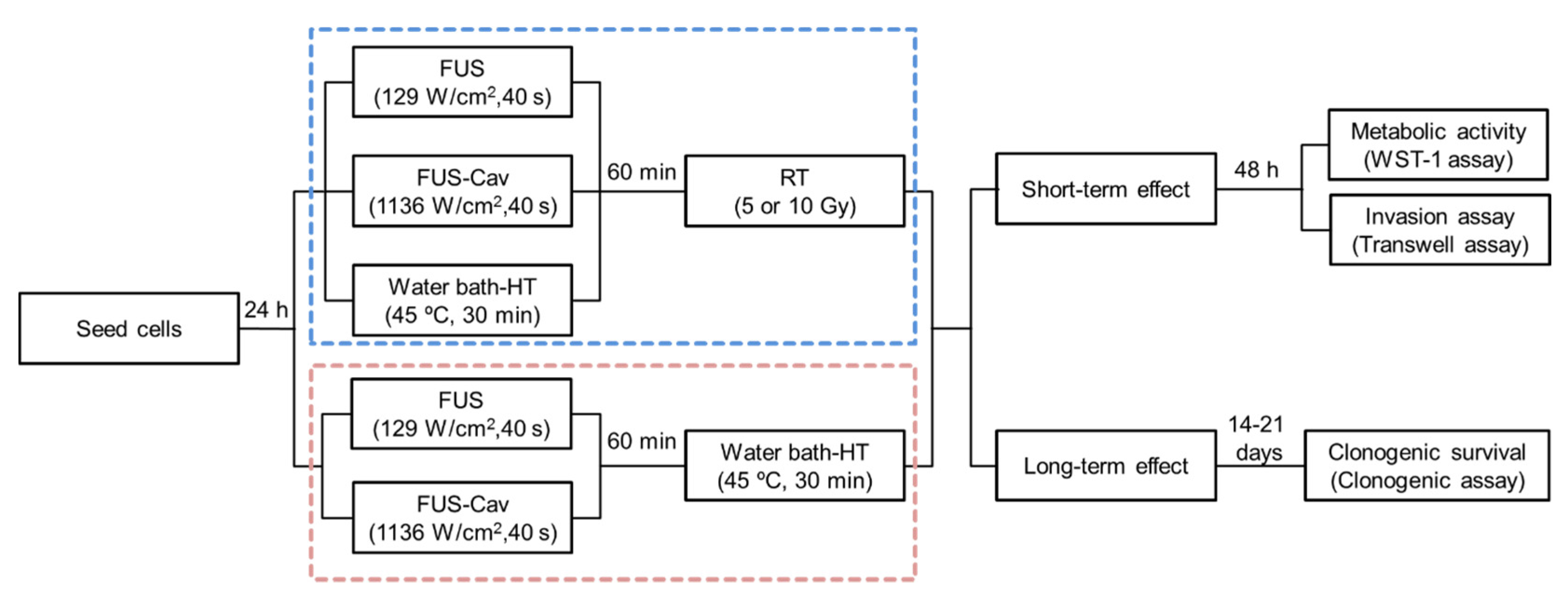
2.5. FUS Treatment of Cancer Cells
2.6. HT Treatment with Water Bath
2.7. RT with X-ray In Vitro
2.8. Combination Treatment Protocol of Cancer Cells
2.9. Clonogenic Assay
2.10. WST-1 Assay
2.11. Invasion Assay
2.12. Detection of Sonoporation by Cell Staining with Propidium Iodide (PI)
2.13. Statistical Analysis
3. Results
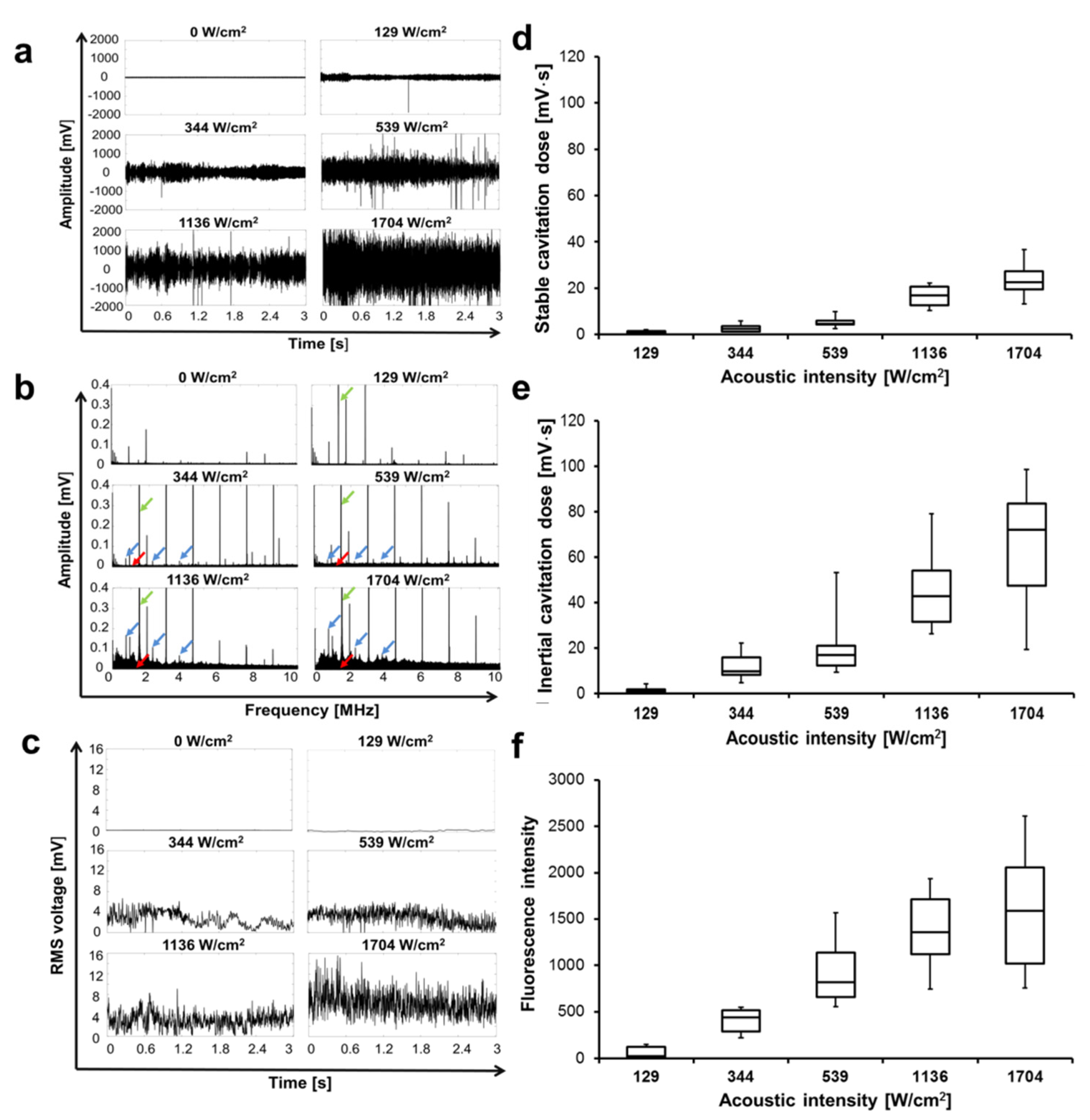
3.1. Cavitation Occurs at a Certain Level of Intensity
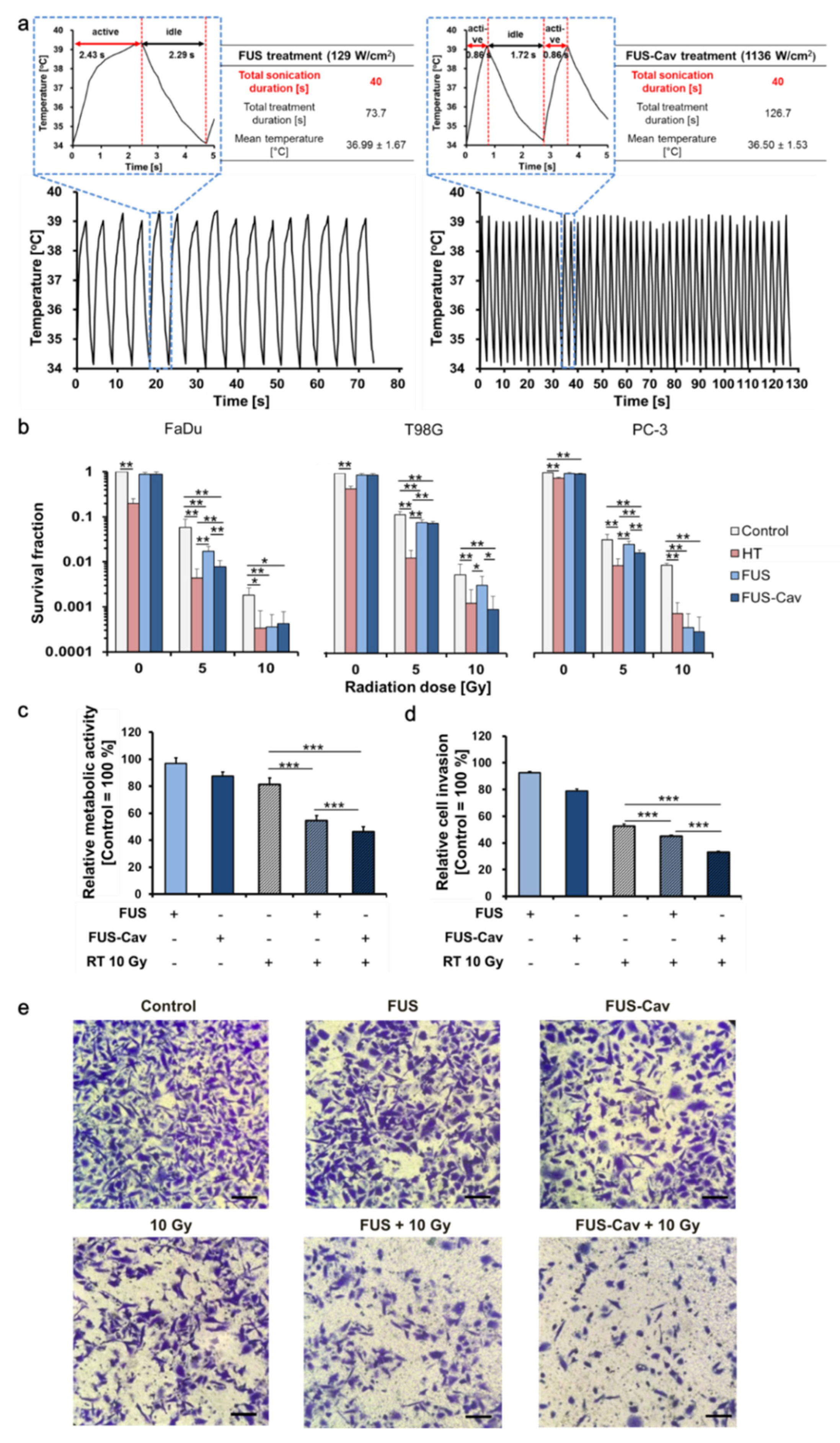
3.2. Short High-Intensity Cavitation-Inducing FUS Shots (FUS-Cav) Are Effective to Radiosensitize Tumor Cells
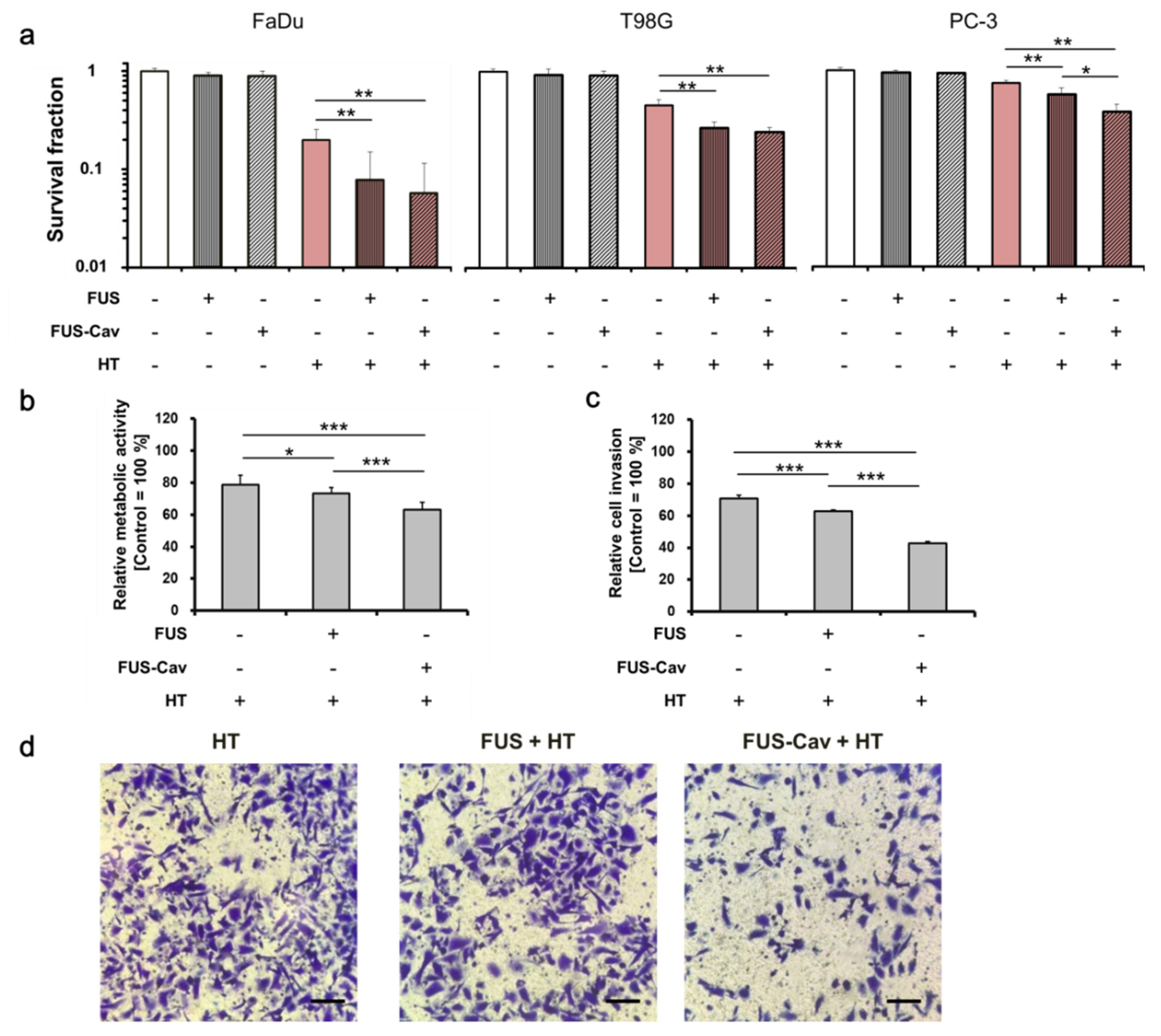
3.3. Short High-Intensity FUS-Induced Cavitation Shots (FUS-Cav) Increase the Effect of HT
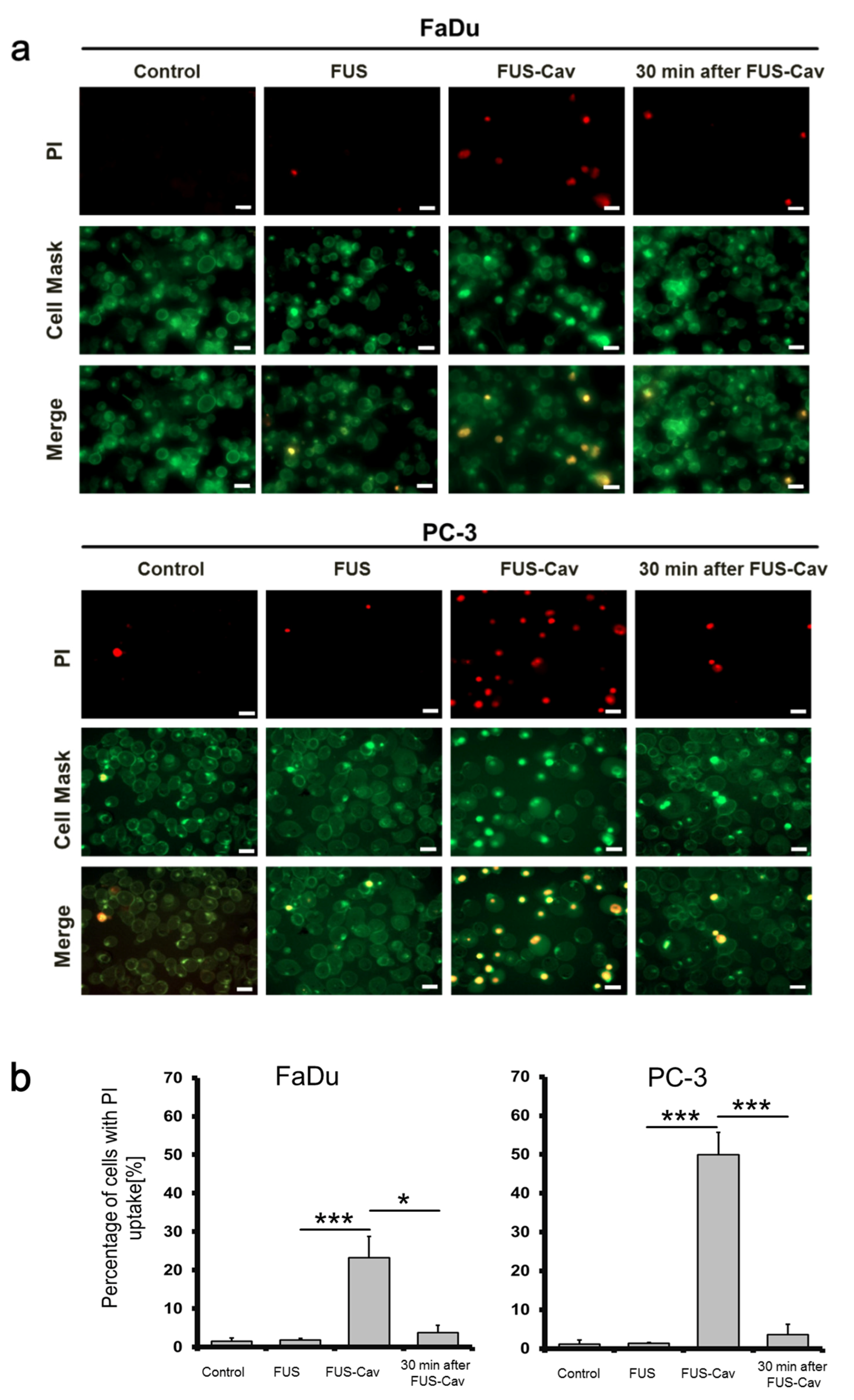
3.4. FUS-Cav Treatment Immediately Induced Sonoporation Effect
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| FUS | Focused ultrasound |
| RT | Radiation therapy |
| HT | Hyperthermia |
| FUS-Cav | FUS shot with cavitation |
| HIFU | High-intensity focused ultrasound |
| MR | Magnetic resonance |
| BBB | Blood–brain barrier |
| PCD | Passive cavitation detector |
| TA | Terephthalate acid |
| FOH | Fiber-optic hydrophone |
| DMEM | Dulbecco’s Modified Eagle’s Medium |
| HEPES | 4-(2- Hydroxyethyl)-piperazine- 1- ethanesulfonic acid |
| MEM | Minimum Essential Medium |
| FBS | Fetal bovine serum |
| PBS | Phosphate-buffered saline |
| EDTA | Ethylenediaminetetraacetic acid |
| FFT | Fast Fourier transformation |
| RMS | Root-mean-square |
| SF | Survival fraction |
| PI | Propidium iodide |
| SD | Standard deviation |
| SEM | Standard error of the mean |
References
- Siedek, F.; Yeo, S.Y.; Heijman, E.; Grinstein, O.; Bratke, G.; Heneweer, C.; Puesken, M.; Persigehl, T.; Maintz, D.; Grüll, H. Magnetic Resonance-Guided High-Intensity Focused Ultrasound (MR-HIFU): Technical Background and Overview of Current Clinical Applications (Part 1). RöFo—Fortschr. Geb. Röntgenstrahlen Bildgeb. Verfahr. 2019, 191, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Bour, P.; Ozenne, V.; Marquet, F.; De Senneville, B.D.; Dumont, E.; Quesson, B. Real-time 3D ultrasound based motion tracking for the treatment of mobile organs with MR-guided high-intensity focused ultrasound. Int. J. Hyperth. 2018, 34, 1225–1235. [Google Scholar] [CrossRef] [PubMed]
- Elming, P.B.; Sørensen, B.S.; Oei, A.L.; Franken, N.A.; Crezee, J.; Overgaard, J.; Horsman, M.R. Hyperthermia: The Optimal Treatment to Overcome Radiation Resistant Hypoxia. Cancers 2019, 11, 60. [Google Scholar] [CrossRef] [PubMed]
- Roti, J.L.R. Introduction: Radiosensitization by hyperthermia. Int. J. Hyperth. 2004, 20, 109–114. [Google Scholar] [CrossRef]
- Peeken, J.C.; Vaupel, P.; Combs, S.E. Integrating Hyperthermia into Modern Radiation Oncology: What Evidence Is Necessary? Front. Oncol. 2017, 7, 7. [Google Scholar] [CrossRef]
- Baronzio, G.; Parmar, G.; Ballerini, M.; Szasz, A.; Cassutti, V. A Brief Overview of Hyperthermia in Cancer Treatment. J. Integr. Oncol. 2014, 3. [Google Scholar] [CrossRef]
- Phenix, C.P.; Togtema, M.; Pichardo, S.; Zehbe, I.; Curiel, L. High intensity focused ultrasound technology, its scope and applications in therapy and drug delivery. J. Pharm. Pharm. Sci. 2014, 17, 136–153. [Google Scholar] [CrossRef]
- Bull, V.; Civale, J.; Rivens, I.; Ter Haar, G. A Comparison of Acoustic Cavitation Detection Thresholds Measured with Piezo-electric and Fiber-optic Hydrophone Sensors. Ultrasound Med. Biol. 2013, 39, 2406–2421. [Google Scholar] [CrossRef]
- Prentice, P.; Cuschieri, A.; Dholakia, K.; Prausnitz, M.; Campbell, P. Membrane disruption by optically controlled microbubble cavitation. Nat. Phys. 2005, 1, 107–110. [Google Scholar] [CrossRef]
- Collis, J.; Manasseh, R.; Liovic, P.; Tho, P.; Ooi, A.; Petkovic-Duran, K.; Zhu, Y. Cavitation microstreaming and stress fields created by microbubbles. Ultrasonics 2010, 50, 273–279. [Google Scholar] [CrossRef]
- Coussios, C.C.; Roy, R.A. Applications of Acoustics and Cavitation to Noninvasive Therapy and Drug Delivery. Annu. Rev. Fluid Mech. 2008, 40, 395–420. [Google Scholar] [CrossRef]
- Gourevich, D.; Volovick, A.; Dogadkin, O.; Wang, L.; Mulvana, H.; Medan, Y.; Melzer, A.; Cochran, S. In Vitro Investigation of the Individual Contributions of Ultrasound-Induced Stable and Inertial Cavitation in Targeted Drug Delivery. Ultrasound Med. Biol. 2015, 41, 1853–1864. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, A.; Liu, M.; Ojha, T.; Storm, G.; Kiessling, F.; Lammers, T.G.G.M. Ultrasound-mediated drug delivery to the brain: Principles, progress and prospects. Drug Discov. Today Technol. 2016, 20, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, A.; Sapozhnikov, O.; Bailey, M.; Crum, L.; Xu, Z.; Fowlkes, B.; Cain, C.; Khokhlova, V. Disintegration of Tissue Using High Intensity Focused Ultrasound: Two Approaches That Utilize Shock Waves. Acoust. Today 2012, 8, 24. [Google Scholar] [CrossRef]
- Chaplin, V.; Caskey, C.F. Multi-focal HIFU reduces cavitation in mild-hyperthermia. J. Ther. Ultrasound 2017, 5, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Bian, S.N.; Seth, A.; Daly, D.; Carlisle, R.; Stride, E. A multimodal instrument for real-time in situ study of ultrasound and cavitation mediated drug delivery. Rev. Sci. Instrum. 2017, 88, 034302. [Google Scholar] [CrossRef] [PubMed]
- Gerold, B.; Kotopoulis, S.; McDougall, C.; McGloin, D.; Postema, M.; Prentice, P. Laser-nucleated acoustic cavitation in focused ultrasound. Rev. Sci. Instrum. 2011, 82, 044902. [Google Scholar] [CrossRef]
- Canney, M.S.; Khokhlova, V.A.; Bessonova, O.V.; Bailey, M.R.; Crum, L.A. Shock-Induced Heating and Millisecond Boiling in Gels and Tissue Due to High Intensity Focused Ultrasound. Ultrasound Med. Biol. 2010, 36, 250–267. [Google Scholar] [CrossRef]
- Jensen, C.R.; Ritchie, R.; Gyongy, M.; Collin, J.R.T.; Leslie, T.A.; Coussios, C.C. Spatiotemporal Monitoring of High-Intensity Focused Ultrasound Therapy with Passive Acoustic Mapping. Radiology 2012, 262, 252–261. [Google Scholar] [CrossRef]
- Zhang, S.; Yin, L.; Fang, N. Focusing Ultrasound with an Acoustic Metamaterial Network. Phys. Rev. Lett. 2009, 102, 194301. [Google Scholar] [CrossRef]
- Villeneuve, L.; Alberti, L.; Steghens, J.; Lancelin, J.; Mestas, J.-L. Assay of hydroxyl radicals generated by focused ultrasound. Ultrason. Sonochem. 2009, 16, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Lai, P.; Tarapacki, C.; Tran, W.T.; El Kaffas, A.; Lee, J.; Hupple, C.; Iradji, S.; Giles, A.; Al-Mahrouki, A.; Czarnota, G.J. Breast tumor response to ultrasound mediated excitation of microbubbles and radiation therapy in vivo. Oncoscience 2016, 3, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Bobeica, M.; Unger, M.; Bednarz, A.; Gerold, B.; Patties, I.; Melzer, A.; Landgraf, L. Focused ultrasound radiosensitize human cancer cells by enhancement of DNA damage. 2020; Submitted. [Google Scholar]
- Barati, A.H.; Mokhtari-Dizaji, M.; Mozdarani, H.; Bathaie, Z.; Hassan, Z.M. Effect of exposure parameters on cavitation induced by low-level dual-frequency ultrasound. Ultrason. Sonochem. 2007, 14, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Bezjak, A.; Paulus, R.; Gaspar, L.E.; Timmerman, R.D.; Straube, W.L.; Ryan, W.F.; Garces, Y.I.; Pu, A.T.; Singh, A.K.; Videtic, G.M.; et al. Safety and Efficacy of a Five-Fraction Stereotactic Body Radiotherapy Schedule for Centrally Located Non–Small-Cell Lung Cancer: NRG Oncology/RTOG 0813 Trial. J. Clin. Oncol. 2019, 37, 1316–1325. [Google Scholar] [CrossRef] [PubMed]
- Le, Q.-T.; Loo, B.W.; Ho, A.; Cotrutz, C.; Koong, A.C.; Wakelee, H.; Kee, S.T.; Constantinescu, D.; Whyte, R.I.; Donington, J. Results of a Phase I Dose-Escalation Study Using Single-Fraction Stereotactic Radiotherapy for Lung Tumors. J. Thorac. Oncol. 2006, 1, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Franken, N.; Rodermond, H.M.; Stap, J.; Haveman, J.; Van Bree, C. Clonogenic assay of cells in vitro. Nat. Protoc. 2006, 1, 2315–2319. [Google Scholar] [CrossRef]
- Patties, I.; Kallendrusch, S.; Böhme, L.; Kendzia, E.; Oppermann, H.; Gaunitz, F.; Kortmann, R.-D.; Glasow, A. The Chk1 inhibitor SAR-020106 sensitizes human glioblastoma cells to irradiation, to temozolomide, and to decitabine treatment. J. Exp. Clin. Cancer Res. 2019, 38, 420. [Google Scholar] [CrossRef]
- Shaw, L.M. Tumor Cell Invasion Assays. Cell Migration 2004, 294, 97–106. [Google Scholar] [CrossRef]
- Wang, Y.; Bai, W.-K.; Shen, E.; Hu, B. Sonoporation by low-frequency and low-power ultrasound enhances chemotherapeutic efficacy in prostate cancer cells in vitro. Oncol. Lett. 2013, 6, 495–498. [Google Scholar] [CrossRef]
- Zhu, L.; Altman, M.B.; Laszlo, A.; Straube, W.; Zoberi, I.; Hallahan, D.E.; Chen, H. Ultrasound Hyperthermia Technology for Radiosensitization. Ultrasound Med. Biol. 2019, 45, 1025–1043. [Google Scholar] [CrossRef]
- Dalecki, D. Mechanical Bioeffects of Ultrasound. Annu. Rev. Biomed. Eng. 2004, 6, 229–248. [Google Scholar] [CrossRef] [PubMed]
- Ali, E.A.; Bordacahar, B.; Mestas, J.-L.; Batteux, F.; Lafon, C.; Camus, M.; Prat, F. Ultrasonic cavitation induces necrosis and impairs growth in three-dimensional models of pancreatic ductal adenocarcinoma. PLoS ONE 2018, 13, e0209094. [Google Scholar] [CrossRef]
- Bani, D.; Li, A.Q.; Freschi, G.; Russo, G.L. Histological and Ultrastructural Effects of Ultrasound-induced Cavitation on Human Skin Adipose Tissue. Plast. Reconstr. Surg. Glob. Open 2013, 1, e41. [Google Scholar] [CrossRef] [PubMed]
- Paliwal, S.; Mitragotri, S. Ultrasound-induced cavitation: Applications in drug and gene delivery. Expert Opin. Drug Deliv. 2006, 3, 713–726. [Google Scholar] [CrossRef] [PubMed]
- Kutty, S.; Liu, N.; Zhou, J.; Xiao, Y.; Wu, J.; Danford, D.A.; Lof, J.; Xie, F.; Porter, T.R. Ultrasound-Induced Microbubble Cavitation for the Treatment of Catheterization-Induced Vasospasm. JACC Basic Transl. Sci. 2017, 2, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Ter Haar, G. Heat and sound: Focused ultrasound in the clinic. Int. J. Hyperth. 2015, 31, 223–224. [Google Scholar] [CrossRef] [PubMed]
- Koulakis, J.P.; Rouch, J.; Huynh, N.; Dubrovsky, G.; Dunn, J.C.; Putterman, S. Interstitial Matrix Prevents Therapeutic Ultrasound From Causing Inertial Cavitation in Tumescent Subcutaneous Tissue. Ultrasound Med. Biol. 2018, 44, 177–186. [Google Scholar] [CrossRef]
- Coussios, C.C.; Farny, C.H.; Ter Haar, G.; Roy, R. Role of acoustic cavitation in the delivery and monitoring of cancer treatment by high-intensity focused ultrasound (HIFU). Int. J. Hyperth. 2007, 23, 105–120. [Google Scholar] [CrossRef]
- Yoshizawa, S.; Ikeda, T.; Ito, A.; Ota, R.; Takagi, S.; Matsumoto, Y. High intensity focused ultrasound lithotripsy with cavitating microbubbles. Med. Biol. Eng. Comput. 2009, 47, 851–860. [Google Scholar] [CrossRef]
- Snipstad, S.; Sulheim, E.; Davies, C.D.L.; Moonen, C.; Storm, G.; Kiessling, F.; Schmid, R.; Lammers, T. Sonopermeation to improve drug delivery to tumors: From fundamental understanding to clinical translation. Expert Opin. Drug Deliv. 2018, 15, 1249–1261. [Google Scholar] [CrossRef]
- Lipsman, N.; Meng, Y.; Bethune, A.J.; Huang, Y.; Lam, B.; Masellis, M.; Herrmann, N.; Heyn, C.; Aubert, I.; Boutet, A.; et al. Blood–brain barrier opening in Alzheimer’s disease using MR-guided focused ultrasound. Nat. Commun. 2018, 9, 1–8. [Google Scholar] [CrossRef]
- Hwang, J.H.; Tu, J.; Brayman, A.A.; Matula, T.J.; Crum, L.A. Correlation between inertial cavitation dose and endothelial cell damage in vivo. Ultrasound Med. Biol. 2006, 32, 1611–1619. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.W.; Everbach, E.C.; Cox, C.; Knapp, R.R.; A Brayman, A.; A Sherman, T. A comparison of the hemolytic potential of Optison and Albunex in whole human blood in vitro: Acoustic pressure, ultrasound frequency, donor and passive cavitation detection considerations. Ultrasound Med. Biol. 2001, 27, 709–721. [Google Scholar] [CrossRef]
- Wu, S.-Y.; Tung, Y.-S.; Marquet, F.; Downs, M.E.; Sanchez, C.S.; Chen, C.C.; Ferrera, V.; Konofagou, E. Transcranial cavitation detection in primates during blood-brain barrier opening-a performance assessment study. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 2014, 61, 966–978. [Google Scholar] [CrossRef] [PubMed]
- Brüningk, S.; Rivens, I.; Mouratidis, P.; Ter Haar, G. Focused Ultrasound-Mediated Hyperthermia in Vitro: An Experimental Arrangement for Treating Cells under Tissue-Mimicking Conditions. Ultrasound Med. Biol. 2019, 45, 3290–3297. [Google Scholar] [CrossRef]
- Robertson, J.; Becker, S. Influence of Acoustic Reflection on the Inertial Cavitation Dose in a Franz Diffusion Cell. Ultrasound Med. Biol. 2018, 44, 1100–1109. [Google Scholar] [CrossRef] [PubMed]
- Tempel, N.V.D.; Laffeber, C.; Odijk, H.; Van Cappellen, W.A.; Van Rhoon, G.C.; Franckena, M.; Kanaar, R. The effect of thermal dose on hyperthermia-mediated inhibition of DNA repair through homologous recombination. Oncotarget 2017, 8, 44593–44604. [Google Scholar] [CrossRef]
- Kwok, S.J.J.; El Kaffas, A.; Lai, P.; Al Mahrouki, A.; Lee, J.; Iradji, S.; Tran, W.T.; Giles, A.; Czarnota, G.J. Ultrasound-Mediated Microbubble Enhancement of Radiation Therapy Studied Using Three-Dimensional High-Frequency Power Doppler Ultrasound. Ultrasound Med. Biol. 2013, 39, 1983–1990. [Google Scholar] [CrossRef]
- Izadifar, Z.; Babyn, P.; Chapman, D. Mechanical and Biological Effects of Ultrasound: A Review of Present Knowledge. Ultrasound Med. Biol. 2017, 43, 1085–1104. [Google Scholar] [CrossRef]
- Daecher, A.; Stanczak, M.; Liu, J.-B.; Zhang, J.; Du, S.; Forsberg, F.; Leeper, D.B.; Eisenbrey, J.R. Localized microbubble cavitation-based antivascular therapy for improving HCC treatment response to radiotherapy. Cancer Lett. 2017, 411, 100–105. [Google Scholar] [CrossRef]
- Ganci, F.; Sacconi, A.; Manciocco, V.; Spriano, G.; Fontemaggi, G.; Carlini, P.; Blandino, G. Radioresistance in Head and Neck Squamous Cell Carcinoma — Possible Molecular Markers for Local Recurrence and New Putative Therapeutic Strategies. Contemp. Issues Head Neck Cancer Manag. 2015, 37, 763–770. [Google Scholar] [CrossRef]
- Toraya-Brown, S.; Fiering, S.N. Local tumour hyperthermia as immunotherapy for metastatic cancer. Int. J. Hyperth. 2014, 30, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.A.; Wu, S.-K.; Li, Z.; Goertz, D.E.; Hynynen, K. Microbubble-assisted MRI-guided focused ultrasound for hyperthermia at reduced power levels. Int. J. Hyperth. 2018, 35, 599–611. [Google Scholar] [CrossRef] [PubMed]
- Nofiele, J.I.T.; Karshafian, R.; Furukawa, M.; Al Mahrouki, A.; Giles, A.; Wong, C.S.; Czarnota, G.J. Ultrasound-Activated Microbubble Cancer Therapy: Ceramide Production Leading to Enhanced Radiation Effect in vitro. Technol. Cancer Res. Treat. 2013, 12, 53–60. [Google Scholar] [CrossRef]
- Ray, S.; Kassan, A.; Busija, A.R.; Rangamani, P.; Patel, H.H. The plasma membrane as a capacitor for energy and metabolism. Am. J. Physiol. Physiol. 2016, 310, C181–C192. [Google Scholar] [CrossRef]
- Van Wamel, A.; Kooiman, K.; Harteveld, M.; Emmer, M.; Cate, F.J.T.; Versluis, M.; De Jong, N. Vibrating microbubbles poking individual cells: Drug transfer into cells via sonoporation. J. Control. Release 2006, 112, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Kumon, R.E.; Cui, J.; Deng, C.X. The Size of Sonoporation Pores on the Cell Membrane. Ultrasound Med. Biol. 2009, 35, 1756–1760. [Google Scholar] [CrossRef]
- Miller, D.L.; Dou, C. Induction of Apoptosis in Sonoporation and Ultrasonic Gene Transfer. Ultrasound Med. Biol. 2009, 35, 144–154. [Google Scholar] [CrossRef]
- Zhong, W.; Sit, W.H.; Wan, J.M.; Yu, A.C. Sonoporation Induces Apoptosis and Cell Cycle Arrest in Human Promyelocytic Leukemia Cells. Ultrasound Med. Biol. 2011, 37, 2149–2159. [Google Scholar] [CrossRef]
- Yang, F.; Gu, N.; Chen, D.; Xi, X.; Zhang, D.; Li, Y.; Wu, J. Experimental study on cell self-sealing during sonoporation. J. Control. Release 2008, 131, 205–210. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, S.; Zhang, X.; Unger, M.; Patties, I.; Melzer, A.; Landgraf, L. Focused Ultrasound-Induced Cavitation Sensitizes Cancer Cells to Radiation Therapy and Hyperthermia. Cells 2020, 9, 2595. https://doi.org/10.3390/cells9122595
Hu S, Zhang X, Unger M, Patties I, Melzer A, Landgraf L. Focused Ultrasound-Induced Cavitation Sensitizes Cancer Cells to Radiation Therapy and Hyperthermia. Cells. 2020; 9(12):2595. https://doi.org/10.3390/cells9122595
Chicago/Turabian StyleHu, Shaonan, Xinrui Zhang, Michael Unger, Ina Patties, Andreas Melzer, and Lisa Landgraf. 2020. "Focused Ultrasound-Induced Cavitation Sensitizes Cancer Cells to Radiation Therapy and Hyperthermia" Cells 9, no. 12: 2595. https://doi.org/10.3390/cells9122595
APA StyleHu, S., Zhang, X., Unger, M., Patties, I., Melzer, A., & Landgraf, L. (2020). Focused Ultrasound-Induced Cavitation Sensitizes Cancer Cells to Radiation Therapy and Hyperthermia. Cells, 9(12), 2595. https://doi.org/10.3390/cells9122595




