Dynamics of Parkinson’s Disease Multimodal Complex Treatment in Germany from 2010–2016: Patient Characteristics, Access to Treatment, and Formation of Regional Centers
Abstract
:1. Introduction
2. Materials and Methods
- Single cases of PD treatments and possible false entries (<3): no regular experience can be presumed.
- Occasional PD treatments (3–12 per year): with less than one treatment per month only occasional experience can be presumed.
- Regular PD treatments (13–52 per year): with up to 1 treatment per week, a regular experience can be presumed.
- Frequent PD treatments (53–520 per year): with 1 to 10 treatments per week, a good experience with a good regular standard can be presumed.
- High volume PD treatments (>520 per year): with more than 10 treatments per week, a very good experience and a high-performance standard can be presumed.
- Frequent PD-MCT (52–104 per year): with 1 to 2 treatments per week, a good standard with an experienced multiprofessional team can be presumed.
- High volume PD-MCT (>104 per year): with more than 2 treatments per week, a highly experienced multiprofessional team can be presumed.
3. Results
3.1. Inpatient Treatment and PD-MCT on Federal Level
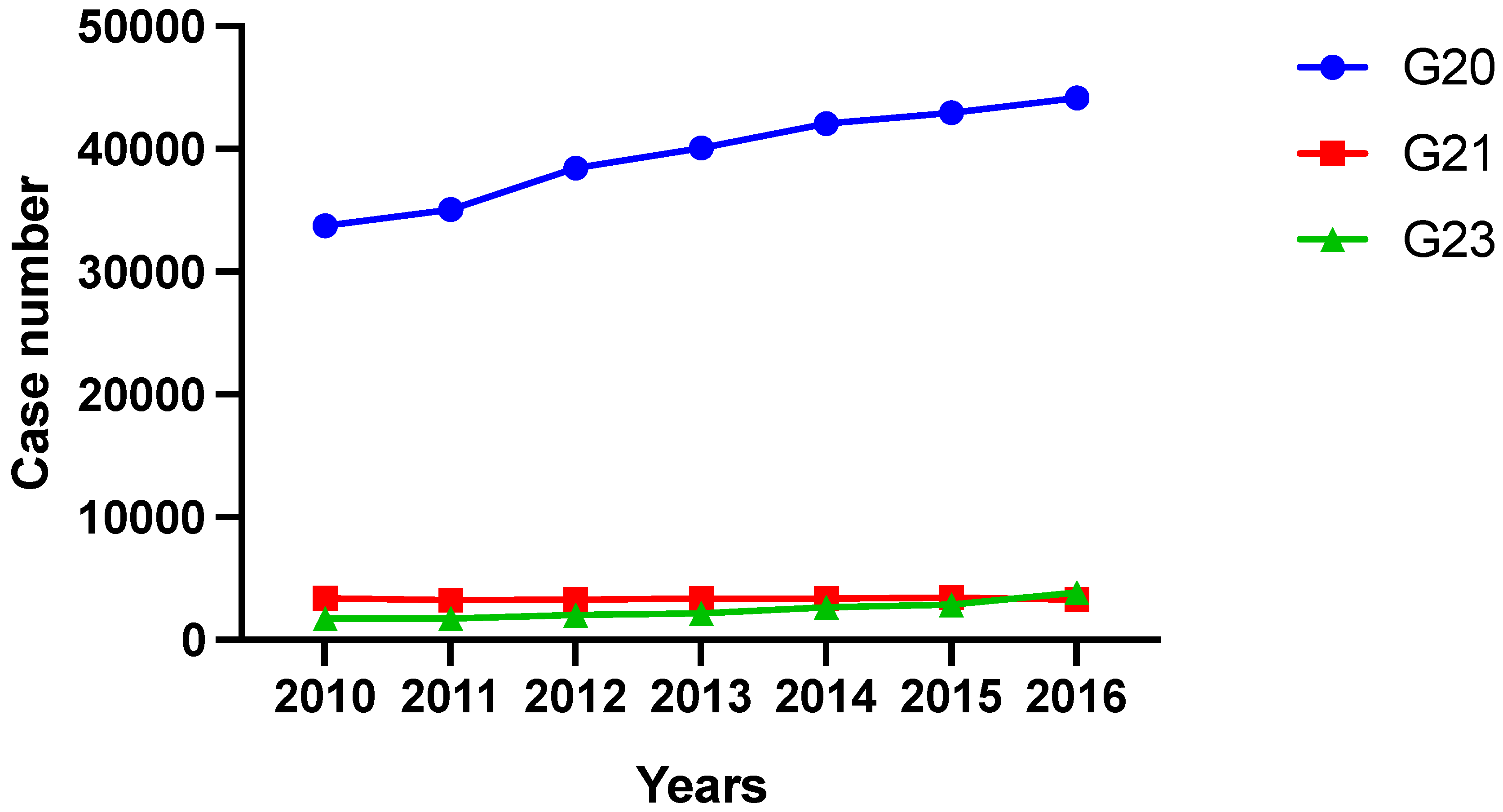
3.1.1. Case Numbers of Inpatient Treatment for PD and Other Basal Ganglia Disorders and Proportion of PD-MCT
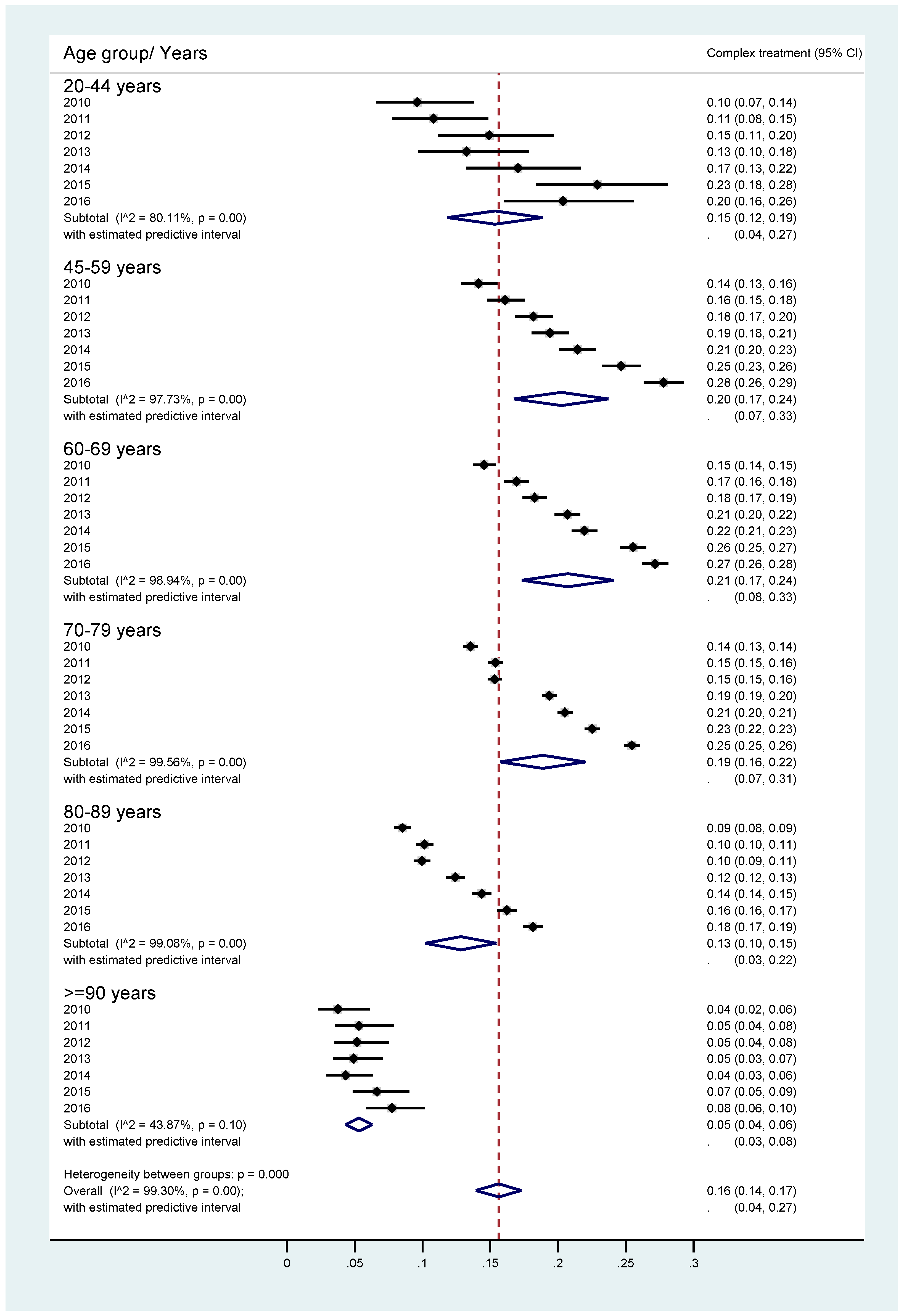
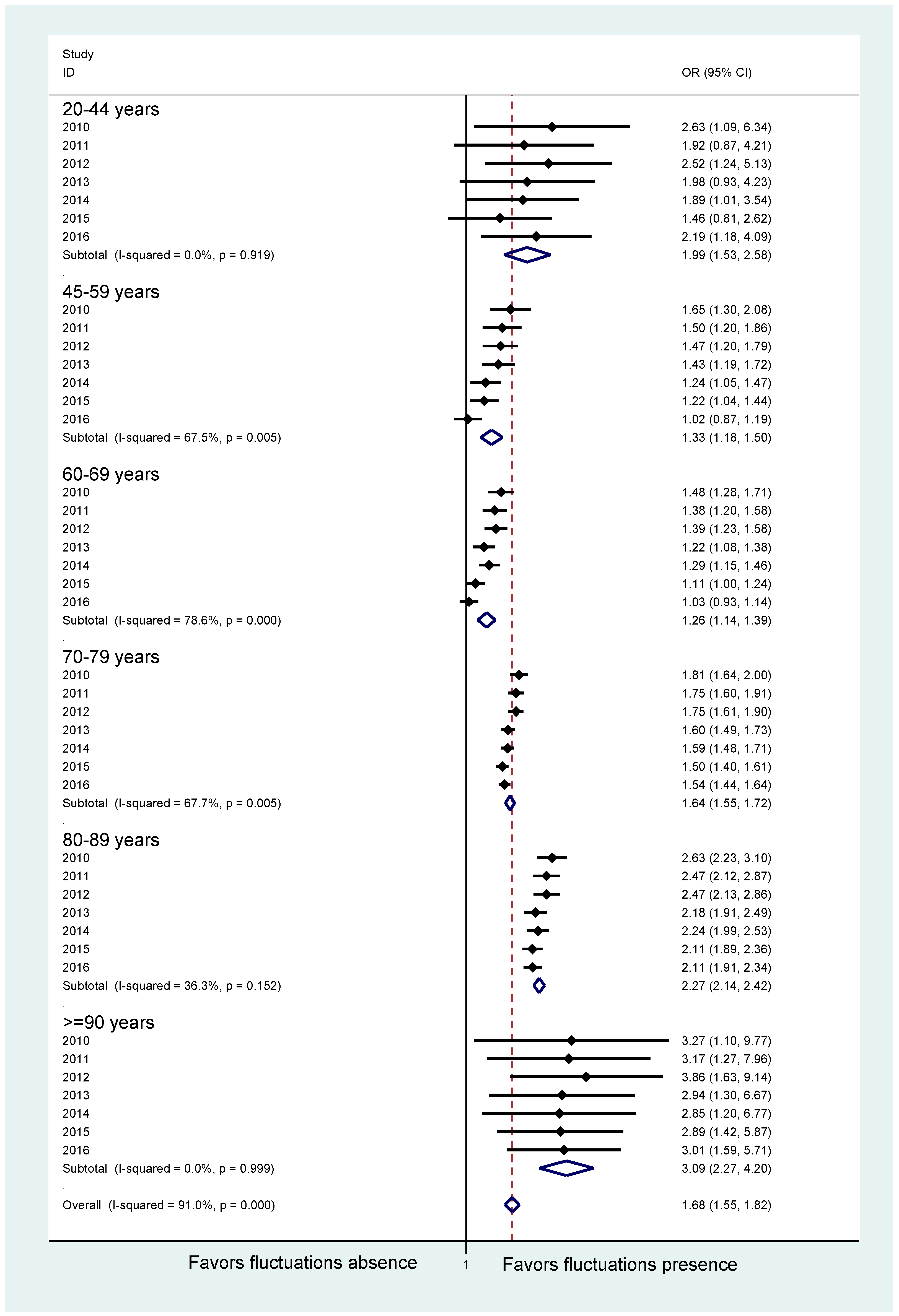
3.1.2. Age and Gender Characteristics and Treatment Rates of PD-MCT
3.2. Inpatient Treatment and PD-MCT on Hospital Level
3.2.1. General PD Inpatient Treatment
3.2.2. Inpatient PD-MCT
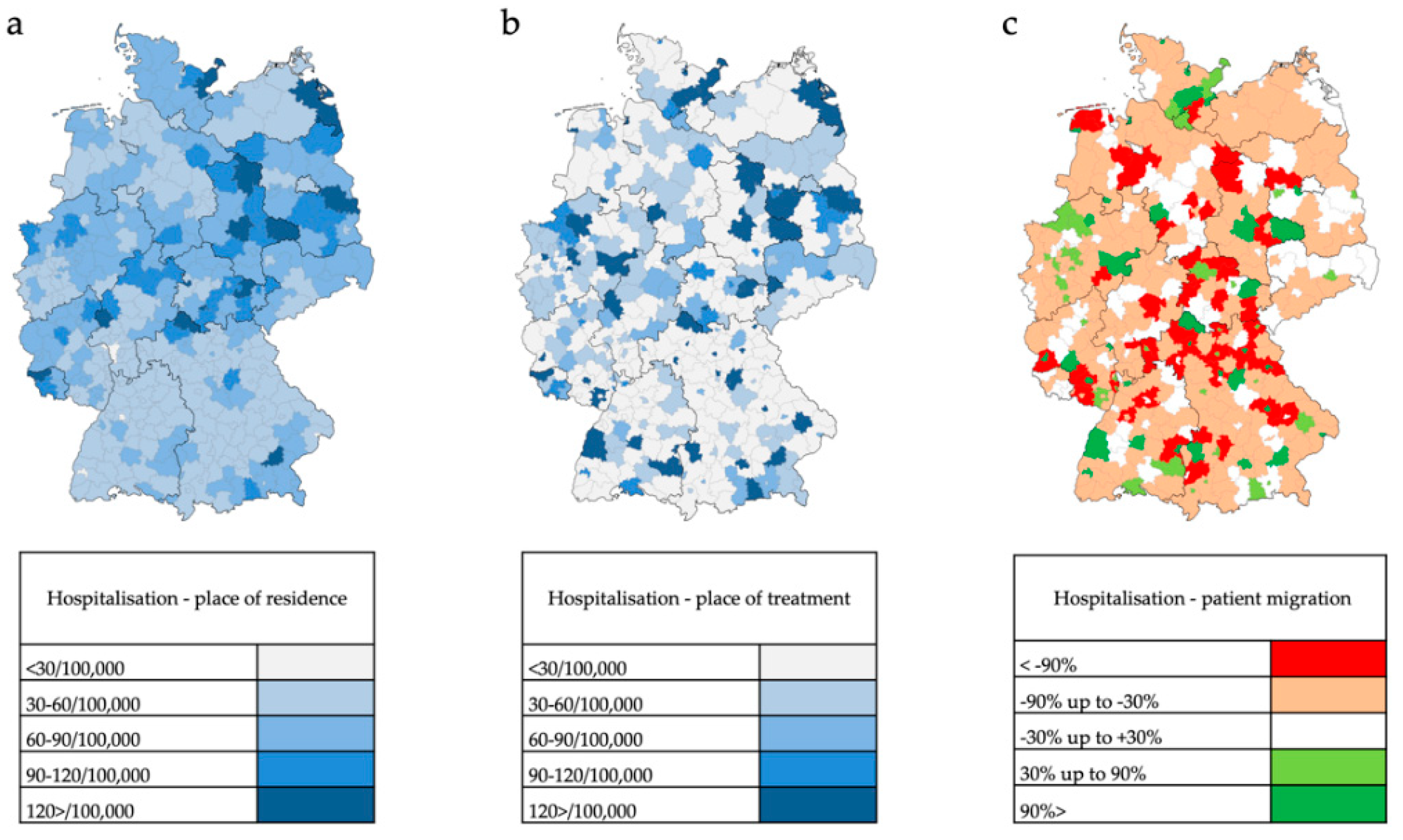
3.3. Regional Distribution of General PD Inpatient Treatment and PD-MCT in Germany
3.3.1. General PD Inpatient Treatment
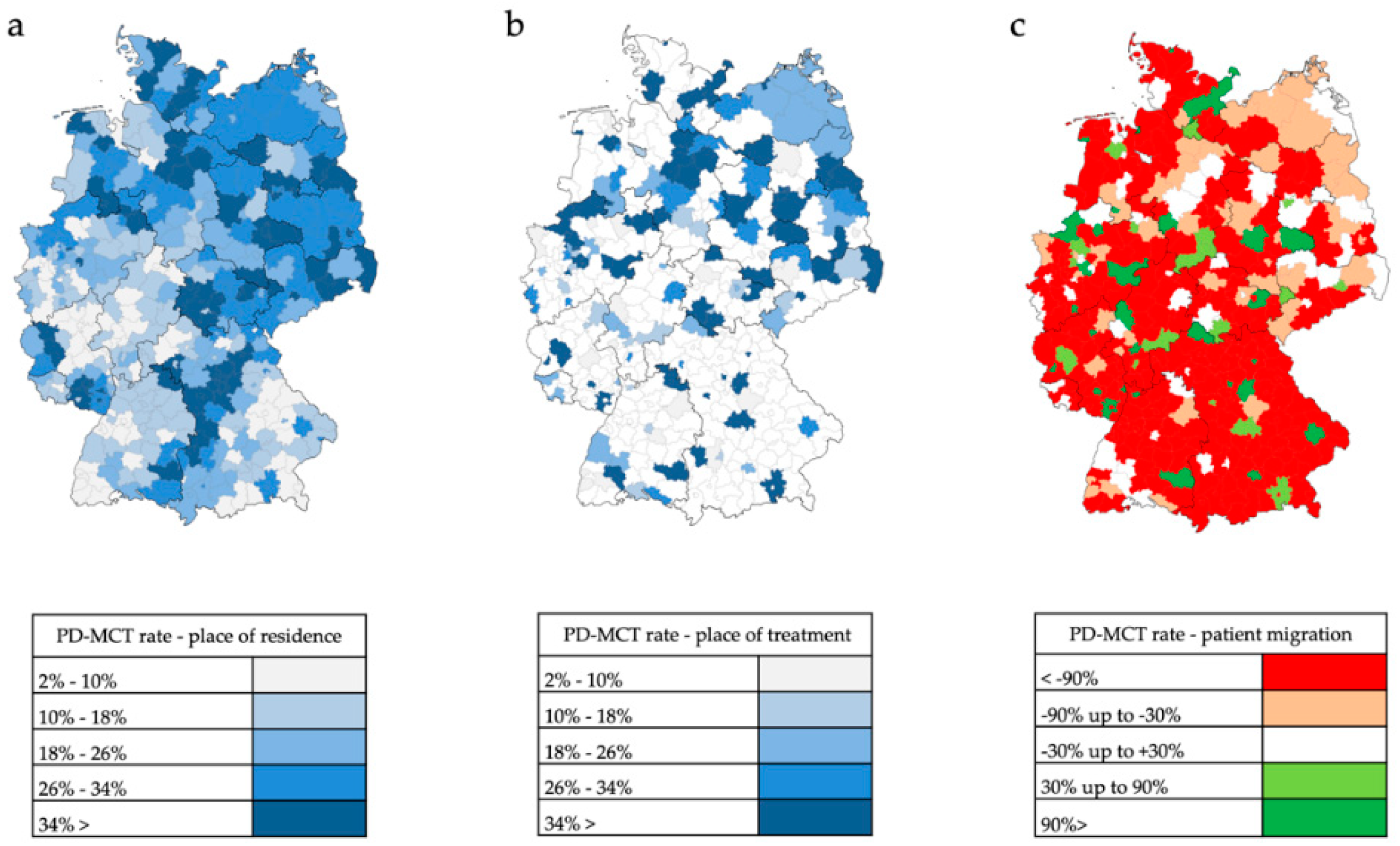
3.3.2. Inpatient PD-MCT
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- GBD 2015 Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017, 16, 877–897. [Google Scholar] [CrossRef]
- Tönges, L.; Bartig, D.; Muhlack, S.; Jost, W.; Gold, R.; Krogias, C. Characteristics and dynamics of inpatient treatment of patients with Parkinson’s disease in Germany: Analysis of 1.5 million patient cases from 2010 to 2015. Nervenarzt 2018. [Google Scholar] [CrossRef]
- Schapira, A.H.V.; Chaudhuri, K.R.; Jenner, P. Non-motor features of Parkinson disease. Nat. Rev. Neurosci. 2017, 18, 435–450. [Google Scholar] [CrossRef] [PubMed]
- Enders, D.; Balzer-Geldsetzer, M.; Riedel, O.; Dodel, R.; Wittchen, H.U.; Sensken, S.C.; Wolff, B.; Reese, J.P. Prevalence, duration and severity of Parkinson’s disease in Germany: A combined meta-analysis from literature data and outpatient samples. Eur. Neurol. 2017, 78, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Gustavsson, A.; Svensson, M.; Jacobi, F.; Allgulanderd, C.; Alonsoe, J.; Beghif, E.; Dodelg, R.; Ekmana, M.; Faravellih, C.; Fratiglionii, L.; et al. Cost of disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 718–779. [Google Scholar] [CrossRef] [PubMed]
- Trenkwalder, C.; Schwarz, J.; Gebhard, J.; Ruland, D.; Trenkwalder, P.; Hense, H.W.; Oertel, W.H. Starnberg trial on epidemiology of Parkinsonism and hypertension in the elderly. Prevalence of Parkinson’s disease and related disorders assessed by a door-to-door survey of inhabitants older than 65 years. Arch. Neurol. 1995, 52, 1017–1022. [Google Scholar] [CrossRef] [PubMed]
- Dorsey, E.R.; Bloem, B.R. The Parkinson pandemic—A call to action. JAMA Neurol. 2018, 75, 9–10. [Google Scholar] [CrossRef] [PubMed]
- Binder, S.; Groppa, S.; Woitalla, D.; Müller, T.; Wellach, I.; Klucken, J.; Eggers, C.; Liersch, S.; Amelung, V.E. Patients’ Perspective on Provided Health Services in Parkinson’s Disease in Germany—A Cross-Sectional Survey. Akt Neurol. 2018, 45, 703–713. [Google Scholar] [CrossRef]
- Tönges, L.; Ehret, R.; Lorrain, M.; Riederer, P.; Müngersdorf, M. Epidemiology of Parkinson’s Disease and Current Concepts of Outpatient Care in Germany. Fortschr. Neurol. Psychiatr. 2017, 85, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Müller, T.; Voss, B.; Hellwig, K.; Josef, S.F.; Schulte, T.; Przuntek, H. Treatment benefit and daily drug costs associated with treating Parkinson’s disease in a Parkinson’s disease clinic. CNS Drugs 2004, 18, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Müller, T.; Öhm, G.; Eilert, K.; Möhr, K.; Rotter, S.; Haas, T.; Küchler, M.; Lütge, S.; Marg, M.; Rothe, H. Benefit on motor and non-motor behavior in a specialized unit for Parkinson’s disease. J. Neural. Transm. (Vienna) 2017, 124, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Ypinga, J.H.L.; de Vries, N.M.; Boonen, L.H.H.M.; Koolman, X.; Munneke, M.; Zwinderman, A.H.; Bloem, B.R. Effectiveness and costs of specialised physiotherapy given via ParkinsonNet: A retrospective analysis of medical claims data. Lancet Neurol. 2018, 17, 153–161. [Google Scholar] [CrossRef]
- Ferrazzoli, D.; Ortelli, P.; Zivi, I.; Cian, V.; Urso, E.; Ghilardi, M.F.; Maestri, R.; Frazzitta, G. Efficacy of intensive multidisciplinary rehabilitation in Parkinson’s disease: A randomised controlled study. J. Neurol. Neurosurg. Psychiatry 2017, 89, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Krüger, R.; Klucken, J.; Weiss, D.; Tönges, L.; Kolber, P.; Unterecker, S.; Lorrain, M.; Baas, H.; Müller, T.; Riederer, P. Classification of advanced stages of Parkinson’s disease: Translation into stratified treatments. J. Neural Transm. 2017, 124, 1015–1027. [Google Scholar] [CrossRef] [PubMed]
- Heinzel, S.; Berg, D.; Binder, S.; Ebersbach, G. Do We Need to Rethink the Epidemiology and Healthcare Utilization of Parkinson’s Disease in Germany? Front. Neurol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Poewe, W.; Seppi, K.; Tanner, C.M.; Halliday, G.M.; Brundin, P.; Volkmann, J.; Schrag, A.-E.; Lang, A.E. Parkinson disease. Nat. Rev. Dis. Primers 2017, 3, 17013. [Google Scholar] [CrossRef] [PubMed]
- Boxer, A.L.; Yu, J.T.; Golbe, L.I.; Litvan, I.; Lang, A.E.; Höglinger, G.U. Advances in progressive supranuclear palsy: New diagnostic criteria, biomarkers, and therapeutic approaches. Lancet Neurol. 2017, 16, 552–563. [Google Scholar] [CrossRef]

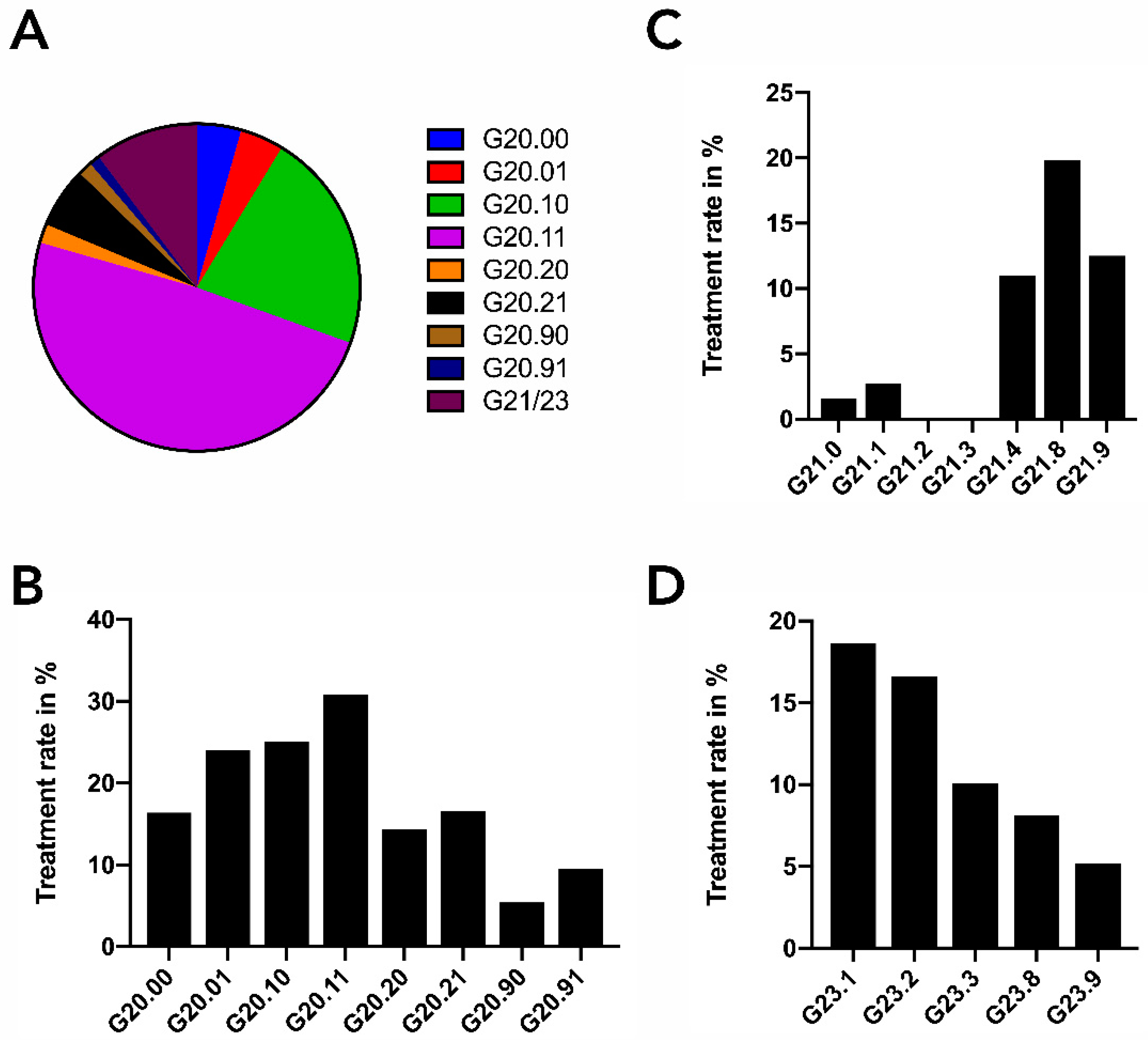

| ICD-10 | Diagnoses |
|---|---|
| G20.– | Primary Parkinson’s syndrome |
| G20.00 | Primary Parkinson’s syndrome without or with less impairment and no fluctuation of action |
| G20.01 | Primary Parkinson’s syndrome without or with less impairment and fluctuation of action |
| G20.10 | Primary Parkinson’s syndrome moderate to severe impairment and no fluctuation of action |
| G20.11 | Primary Parkinson’s syndrome moderate to severe impairment and fluctuation of action |
| G20.20 | Primary Parkinson’s syndrome with the most serious impairment and no fluctuation of action |
| G20.21 | Primary Parkinson’s syndrome with the most serious impairment and fluctuation of action |
| G20.90 | Primary Parkinson’s syndrome not further defined and no fluctuation of action |
| G20.91 | Primary Parkinson’s syndrome not further defined and fluctuation of action |
| G21.– | Secondary Parkinson’s syndrome |
| G21.0 | Neuroleptic malignant syndrome |
| G21.1 | Medication induced Parkinson’s syndrome |
| G21.2 | Parkinson’s syndrome caused by other exogenic agents |
| G21.3 | Post encephalitic Parkinson’s syndrome |
| G21.4 | Vascular Parkinson’s syndrome |
| G21.8 | Other secondary Parkinson’s syndrome |
| G21.9 | Secondary Parkinson’s syndrome not further defined |
| G23.– | Other degenerative disease of the basal ganglia |
| G23.0 | Neurodegeneration with Brain Iron Accumulation |
| G23.1 | Steele–Richardson–Olzewksi syndrome |
| G23.2 | Multi system atrophy |
| G23.8 | Other specified degenerative disease of the basal ganglia |
| G23.9 | Other degenerative disease of the basal ganglia not further defined |
| OPS-Code | Signification |
|---|---|
| 8-97d | PD-MCT treatment of any duration |
| 8-97d.0 | PD-MCT treatment of 7–13 days |
| 8-97d.1 | PD-MCT treatment of 14–20 days |
| 8-97d.2 | PD-MCT treatment of at least 21 days |
| OPS | 2010 | 2016 |
|---|---|---|
| 8-97d.0 | 73.4 | 73.8 |
| 8-97d.1 | 72.1 | 72.6 |
| 8-97d.2 | 72.5 | 73.1 |
| 8-97d | 72.4 | 72.8 |
| Inpatient Treatment [Male/Female] | PD-MCT [Male/Female] | PD-MCT Treatment Rate [Male/Female] | |||||
|---|---|---|---|---|---|---|---|
| Year | G20 Cases | G21 Cases | G23 Cases | G20+G21+G23 Cases | 8–97d Cases | 8–97d Ratio | G20+G21+G23 Ratio |
| 2010 | 19,111/14,649 | 1834/1554 | 901/848 | 21,846/17,051 | 2642/1993 | 57%/43% | 12%/12% |
| 2011 | 19,900/15,181 | 1779/1459 | 944/802 | 22,623/17,442 | 3075/2410 | 56%/44% | 14%/14% |
| 2012 | 22,257/16,208 | 1826/1460 | 1128/894 | 25,211/18,562 | 3596/2564 | 58%/42% | 14%/14% |
| 2013 | 23,509/16,588 | 1840/1499 | 1178/990 | 26,527/19,077 | 4642/3212 | 59%/41% | 17%/17% |
| 2014 | 24,936/17,137 | 1912/1458 | 1368/1290 | 28,216/19,885 | 5195/3754 | 58%/42% | 18%/19% |
| 2015 | 25,478/17,512 | 1957/1485 | 1571/1304 | 28,996/20,301 | 6037/4266 | 59%/41% | 21%/21% |
| 2016 | 26,399/17,793 | 1909/1362 | 2122/1736 | 30,430/20,891 | 6887/4868 | 59%/41% | 23%/23% |
| Cases | Proportion of Cases in 2016 | Hospitals | Proportion of All Hospitals Which Treated PD Patients | |
|---|---|---|---|---|
| Single Cases | 490 | 1.0% | 245 | 18.9% |
| <1 Case Monthly | 3052 | 6.0% | 495 | 38.2% |
| <1 Case Weekly | 9076 | 17.9% | 326 | 25.2% |
| 1–10 Cases Weekly | 28,590 | 56.4% | 223 | 17.2% |
| >10 Cases Weekly | 9503 | 18.7% | 7 | 0.5% |
| ICD | Department of Neurology | Department of Internal Medicine | Department of Geriatrics | Other Departments |
|---|---|---|---|---|
| G20 | 76.9% | 11.8% | 7.3% | 4.0% |
| G21 | 69.7% | 17.9% | 9.4% | 3.0% |
| G23 | 84.3% | 9.8% | 4.0% | 1.9% |
| Total | 77.0% | 12.0% | 7.2% | 3.8% |
| Cases | Proportion of Cases in 2016 | Hospitals | Proportion of all Hospitals Which Treated PD Patients | |
|---|---|---|---|---|
| Single Cases | 31 | 0.3% | 24 | 11.6% |
| <1 Case Monthly | 304 | 2.6% | 36 | 17.4% |
| <1 Case Weekly | 2750 | 23.5% | 97 | 46.9% |
| 1–2 Cases Weekly | 1759 | 15.0% | 24 | 11.6% |
| >2 Cases Weekly | 6878 | 58.7% | 26 | 12.6% |
| OPS | Department of Neurology | Department of Internal Medicine | Department of Geriatric Medicine | Other Departments |
|---|---|---|---|---|
| 8-97d.0 | 93.9% | 5.1% | 0.4% | 0.6% |
| 8-97d.1 | 94.3% | 4.8% | 0.8% | 0.0% |
| 8-97d.2 | 92.9% | 6.7% | 0.4% | 0.0% |
| 8-97d | 94.1% | 5.0% | 0.7% | 0.1% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Richter, D.; Bartig, D.; Muhlack, S.; Hartelt, E.; Scherbaum, R.; Katsanos, A.H.; Müller, T.; Jost, W.; Ebersbach, G.; Gold, R.; et al. Dynamics of Parkinson’s Disease Multimodal Complex Treatment in Germany from 2010–2016: Patient Characteristics, Access to Treatment, and Formation of Regional Centers. Cells 2019, 8, 151. https://doi.org/10.3390/cells8020151
Richter D, Bartig D, Muhlack S, Hartelt E, Scherbaum R, Katsanos AH, Müller T, Jost W, Ebersbach G, Gold R, et al. Dynamics of Parkinson’s Disease Multimodal Complex Treatment in Germany from 2010–2016: Patient Characteristics, Access to Treatment, and Formation of Regional Centers. Cells. 2019; 8(2):151. https://doi.org/10.3390/cells8020151
Chicago/Turabian StyleRichter, Daniel, Dirk Bartig, Siegfried Muhlack, Elke Hartelt, Raphael Scherbaum, Aristeides H. Katsanos, Thomas Müller, Wolfgang Jost, Georg Ebersbach, Ralf Gold, and et al. 2019. "Dynamics of Parkinson’s Disease Multimodal Complex Treatment in Germany from 2010–2016: Patient Characteristics, Access to Treatment, and Formation of Regional Centers" Cells 8, no. 2: 151. https://doi.org/10.3390/cells8020151
APA StyleRichter, D., Bartig, D., Muhlack, S., Hartelt, E., Scherbaum, R., Katsanos, A. H., Müller, T., Jost, W., Ebersbach, G., Gold, R., Krogias, C., & Tönges, L. (2019). Dynamics of Parkinson’s Disease Multimodal Complex Treatment in Germany from 2010–2016: Patient Characteristics, Access to Treatment, and Formation of Regional Centers. Cells, 8(2), 151. https://doi.org/10.3390/cells8020151








