Do Pharmacological Treatments Act in Collaboration with Rehabilitation in Spinal Cord Injury Treatment? A Review of Preclinical Studies
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Neuromodulation
3.1.1. Quipazine and 8-OH-DPAT
3.1.2. Commercially Available Serotonin Agonists
| Basic Information/Model | Rehabilitation | Combinatorial Treatment/Groups | Effect |
|---|---|---|---|
| 2006 de Leon [28] SD rats (female, N = 28) T8/9 transection | Subacute started at 3 weeks -Robot-assisted training, 20 min/day, 5 days/week for 10 weeks | Subacute; started at 3 weeks -Quipazine: daily (i.t.), 2–3 min before training Groups: Combined, Trained, Quipazine | Only behavioral assessments. (1) More stepping movements in trained group than untrained; (2) No significant effect of combinatorial treatment on stepping recovery. |
| 2016 Foffani G [27] SD rats (N = 70) T8/9 transection | Subacute start at 1 week -Quadrupedal TMT, 3 min/day, 5 days/week for 8 weeks -Bike training, two sessions of 30 min/day, 3 days/week for 8 weeks | Subacute; treated at 2 weeks -Quipazine: daily (i.p.) Groups: Bike, TMT, Quipazine, Bike + Quipazine, TMT + Quipazine, Bike + TMT + Quipazine | Responding cell number in the primary somatosensory cortex decreased in quipazine-treated animals in combination with bike exercise but increased with TMT. TMT and quipazine were collaborative, while bike and quipazine were competing. |
| 2013 Ganzer PD [33] SD rats (female, N = 24) T8/9 transection | Subacute start at 1 week -BWS passive bicycling, two sessions of 30 min/day, 3 days/week for 8 weeks | Subacute; treated at 2 weeks -Quipazine, 8-OH-DPAT, 5 days/week for 8 weeks Groups: Saline + Rehab, Low dose + Rehab, High dose + Rehab | Combinatorial effect of training was not evaluated. (1) Dose-dependent reorganization of sensorimotor cortex, extended to cortex corresponding to unaffected forelimb. |
| 2018 Ganzer PD [34] SD rats (female, N = 26; second experiment) T8/9 transection | Subacute start at 1 week -BWS passive bicycling, two sessions of 30 min/day, 3 days/week for 8 weeks | Subacute; treated at 2 weeks -Quipazine, 8-OH-DPAT, 5 days/week for 8 weeks Groups: Bike, Quipazine/8-OH-DPAT, Combined | (1) While TMT alone increased 5-HT receptor immunoreactivity, quipazine reversed it. Addition of TMT to quipazine did not exert any effect; (2) Addition of TMT restored MAP2-positive dendritic processes and improved weight-supported stepping. |
| 2009 Courtine G [29] SD rats (female, N = 7–10, per group) T7 transection | Subacute start at 8 days -Partial BWS-TMT, 20 min/day, every other day for 8 weeks | Subacute; together with training -EES to L2 + S1 at 40–50 Hz, 1–4 V -Quipazine (i.p.)/8-OH-DPAT (s.c.) 10–15 min before training Groups: TMT + EES (L2 + S1), TMT + Quipazine + 8-OH-DPAT, Combined | Addition of BWSTT restored MEPs, reduced c-Fos expression, and improved kinematics and electromyography patterns. |
| 2012 van den Brand R [30] SD rats (female, N = 27) T6 transection | Subacute start at 8 days -TMT alone or TMT + bipedal overground training with a robotic device, 30 min/day for 8 weeks | Subacute; together with training -EES to L2 + S1 at 40 Hz -Systemic injection of a cocktail of quipazine/8-OH-DPAT/ D1 agonist Groups: Drug, Drug + TMT, Drug + Overground/TMT | (1) CST fiber density was restored accompanying MEP amplitude restoration in overground gait-trained animals; (2) Upregulation in c-Fos expression secondary to overground gait training; (3) Automated treadmill-restricted training failed to promote trans-lesional plasticity and recovery. |
| 2018 Asboth L [14] Lewis rats (female, N = 15) T8/9 severe contusion | Subacute start at 7 days -Bipedal TMT + overground training with a robotic device, 40 min/day, 6 days/week for 9 weeks | Subacute; together with training -EES to L2 + S1 at 40 Hz, 100–300 μA -Quipazine/8-OH-DPAT/D1 agonist 5 min before training Groups: Training, Training + EES, Training + EES + Drug | This study included a further investigation using mice without rehabilitation. (1) Combinatorial treatment improved parameters related to natural locomotion, stair climbing, and swimming; (2) Combination of training increased projections from cortex and ventral gigantocellular reticular neurons to lumbar enlargement. |
| 2021 Yao Q [35] SD rats (female, N = 60) T8 transection | Subacute start at 1 week -High-intensity BWS bipedal gait, 30 min/day for 11 weeks | Subacute; together with training -EES (20/40/60 Hz) at T12–L2 during training -Quipazine (i.p.) and 8-OH-DPAT (s.c.) 10 min before training Groups: Training, Training + EES, Training + Quipazine/8-OH-DPAT, Combined | Combinatorial effect of training was not evaluated except for behavior. (1) EES restored gait rhythm; (2) 5-HT agonists increased task metabolism, which is essential to facilitate locomotor activity, in a frequency-dependent manner; (3) The sensitive stimulation frequency differed between segments: 40 Hz for L1–L2 and 60 Hz for T12–T13. |
| 2010 Liu H [40] SD rats (female, N = 56) T8/9 transection | Subacutely started at 7 DPI -Passive motorized bicycle exercise, two 30 min/day sessions, 5 days/week for 30 days | Subacute, together with training Carbidopa (a decarboxylase inhibitor) + L-DOPA (a noradrenergic/dopaminergic precursor (p.o.) 30 min before training Groups: Training, Dopaminergic treatment, Combined | Electrophysiological measurement of spasticity improved in all treatment groups, thus no additive effect of training was observed. |
| 2012 Ung RV [39] CD1 mice (male, N = 43) T9/10 transection | Subacute start at 1 week -Quadrupedal BWS-TMT, 15 min/day, 3 days/week for 8 weeks | Subacute; together with training (1) BCD: buspirone + carbidopa + L-DOPA (i.p.) coupled with training (3 days/week) (2) Clenbuterol (a β2-adrenergic agonist similar to anabolic steroids) (s.c.) daily Groups: TMT, TMT + BCD, Combined | Combinatorial effect of training was not evaluated; all groups had accompanying rehabilitative training. BCD + training induced locomotor recovery accompanied by larger muscle volume; clenbuterol increased muscle volume. |
| 2013 Cristante AF [37] Wistar rats (male, N = 96) T9/10 moderate contusion | Acute start after SCI -TMT 15 min/day, 5 days/week for 6 weeks | Acute; together with training -Fluoxetine (a selective serotonin reuptake inhibitor) (i.p.) until 42 DPI Groups: TMT, Fluoxetine, Combined | Though each single treatment induced greater functional improvement accompanied by better MEP parameters, no combinatorial effect was observed. No effect on the residual fiber count. |
| 2018 Ryu Y [38] SD rats (N = 64) T8 severe contusion | Late-subacute start at 4 weeks -BWS passive bipedal gait followed by quadrupedal gait, 30 min/day for 2 weeks | Late-subacute; together with training -Fluoxetine (i.p.) or cyproheptadine (a 5-HT2 receptor antagonist) Groups: TMT, Fluoxetine, Cyproheptadine, TMT + Fluoxetine, TMT + Cyproheptadine | (1) While spasticity was suppressed by cyproheptadine treatment and increased by fluoxetine, TMT did not modify those effects; (2) Addition of TMT effectively induced downregulation of 5-HT2A receptor in combination groups as well as control. |
3.2. Neurotrophic Factors
3.2.1. BDNF
3.2.2. NT3
3.2.3. Other Neurotrophic Factors
| Basic Information/Model | Rehabilitation | Combinatorial Treatment | Effect |
|---|---|---|---|
| 2020 Marchionne F [43] Domestic shorthair cats (adult, female, N = 14) T11/12 transection | Acute -Bipedal TMT, 20 min/day: forelimbs were kept stationary on the platform | Immediate -BDNF (i.t.) with an osmotic pump throughout the experimental period Groups: TMT, BDNF + TMT | Combinatorial effect of training was not evaluated; all groups had accompanying rehabilitative training. (1) BDNF-treated cats recovered weight-bearing plantar stepping, while control animals dragged H/L at a higher velocity qualitatively. |
| 2015 Han S [44] Beagle dogs (adult, female, N = 28) T12 transection | Subacute start at 3 weeks -Daily massage and stretch, pinched foot, and suspended body for involuntary H/L movement -Ambulation with body support by holding the tail after wound healing | Immediate -LOCS fibers with/without collagen-binding BDNF implant Groups: LOCS + Training, LOCS-BDNF + Training | Combinatorial effect of training was not evaluated; all groups had accompanying rehabilitative training. LOCS-BDNF promoted locomotion and sensory recovery, accompanied by reductions of lesion volume and collagen deposition and increases of axonal regeneration and myelination. |
| 2019 Lin J [47] SD rats (female, N = 26) T9/10 transection with a 2 mm gap | Subacute start at 1 week -Quadrupedal BWS-TMT with a device to enable normal gait, 30 min/day, 3 days/week for 11 weeks | Immediate implantation -Biofunctional scaffold: poly(ε-caprolactone-co-ethyl ethylene phosphate) loaded with NT3 Groups: Scaffold, Scaffold + TMT | Rehabilitated animals showed better motor function together with more regenerated axons, a higher percentage of anti-inflammatory M2-like macrophages, and greater perineuronal net formation than non-rehabilitated animals. |
| 2018 Tom B [48] Rats (N = 56) T9/10 moderate contusion | Acute -BWS-TMT, 1000 steps/day, 5 day/week for 8 weeks | Immediate implantation -Bioengineered scaffold made of poly N-isopropylacrylamide-g-poly ethylene glycol loaded with BDNF/NT3 Groups: TMT, Scaffold-BDNF/NT3, Combined | (1) Motor function did not significantly differ among the groups; (2) Spasticity was improved, as assessed by the rate depression property of the H-reflex, in the trained groups; (3) KCC2 expression was restored in the trained groups. |
| 2014 Alluin O [54] * Wistar rats (female, N = 48), Mid thoracic clip compression | Acute start on day 1 -Quadrupedal TMT, some of 15 min sessions/day, 5 days/week for 7 weeks | Acute; started at 4 DPI -cABC and growth factors (GFs: EGF, FGF2, and PDGF-AA), osmotic pump infusion, for 7 days Groups: TMT, cABC + GFs, Combined | (1) Absence of synergistic effects on kinematic parameters; (2) cABC effect to suppress astrogliosis was increased; (3) Synergistic effects on neuroanatomical plasticity in collateral sprouting of CST and serotonergic fibers. |
| 2020 Park CH [52] SD rats (N = 24) T9 clip moderate contusion | Subacute start at 1 week -Quadrupedal gait exercise, 30 min/day, 5 days/week for 4 weeks | Acute intervention -G-CSF (i.p.) for 5 days Groups: Exercise, G-CSF, Combined | The G-CSF/exercise group showed the most effective functional recovery, the smallest cavity size, higher BDNF, and lower GFAP immunoreactivity. There was lower VEGF in the combination group than the single treatment groups, but it was still higher than in the control group. |
3.3. Agents Targeting Inhibitory Factors in Scar Tissue
3.3.1. cABC
3.3.2. Other Agents to Degrade CSPG
3.3.3. Anti-Nogo-A Treatments
3.3.4. Inhibitors for Axonal Regrowth Inhibitor
| Basic Information/Model | Rehabilitation | Combinatorial Treatment | Effect |
|---|---|---|---|
| 2011 Jakeman LB [74] C57BL/6 mice (female, N = 16) Midthoracic spinal contusion | Subacute start at 1 week (day following initiation of medication) Voluntary wheel running exercise, for 5 weeks | Subacute; treated at 1 week -cABC (L4/5 intra-parenchymal injection, once) Groups: Wheel-run, cABC, Combined | No effect on motor and sensory function of each single treatment or combinatorial treatment. |
| 2008 Tester NJ [56] Purpose bred SPF cats (adult, female, N = 9) T10 hemisection | Acute start within 2–3 days, trained before SCI (1) Bipedal TMT at 5 days/week and basic overground runway at least 3 days/week (2) A horizontal ladder, narrow beam crossing, and a pegboard 2 days/week were reintegrated when ability allowed | Immediate -cABC in gel form placed for 30 min after injury and then injected via a subdural port every other day for 1 month Groups: Training, cABC + Training | (1) While recovery of skilled locomotion (ladder, peg, and beam) was accelerated, that of basic locomotion (bipedal treadmill and overground) was unaffected; (2) Combinatorial treatment with cABC enhanced serotonergic plasticity. |
| 2009 Garcia-Alias G [57] LH rats (male, N = 60), C4 dorsal funiculi cut | Subacutely started at 7 DPI, 1 h/day, 5 days/week. (1) Specific: placed in a cage where rats are facilitated to retrieve seeds with their forepaws (2) Non-specific: enriched environment cage where rats were encouraged to explore food pellets | Acute treatment -cABC or penicillinase injection above and below the lesion after SCI, followed by five intrathecal infusions on alternate days. 6 Groups: cABC or penicillinase infusion for no rehabilitation, specific or non-specific rehabilitation | (1) cABC enhanced CST axonal crossing and sprouting independently of rehabilitation regime, but specific rehabilitation showed the greatest recovery; (2) cABC + specific rehabilitation improved manual dexterity; (3) Non-specific rehabilitation improved ladder walking but showed worse skilled reaching abilities. |
| 2011 Wang D [58] LH rats (male, N = 44), C4 dorsal spinal cord injury | Late-subacute start at 1 month Task-specific paw-reaching rehabilitation, 30 min twice/day for 10 weeks | Late-subacute; started at 1 month -cABC: injection rostral and caudal to the lesion + five injections (i.t.), every other day after initial treatment Groups: cABC, Rehabilitation, Combined | (1) Combinatorial treatment induced greater recovery of skilled paw reaching and ladder/beam walking; (2) Rehabilitation increased modest recovery of skilled paw reaching; (3) Combinatorial treatment increased sprouting of the CST accompanied by increased levels of VGLUT1-positive presynaptic boutons and perineuronal net component. |
| 2016 Shinozaki M [60] SD rats (female, N = 61) Very severe thoracic spinal contusion | Chronic start at 6 weeks -Quadrupedal TMT, 30 min/day, 5 days/week for 8 weeks | Chronic; started at 6 weeks -cABC (i.t.) with an osmotic pump for 1 week Groups: TMT, cABC + Training | (1) Combinatorial treatment induced slight motor functional recovery; (2) Recovery at 6–9 weeks with TMT and at 12–14 weeks with cABC; (3) cABC restored the transverse residual tissue area and induced neuronal/serotonergic fiber regeneration. |
| 2014 Alluin O [54] * Wistar rats (female, N = 48) Mid thoracic clip compression | Acute start on day 1 -Quadrupedal TMT, some of 15 min sessions/day, 5 days/week for 7 weeks | Acute; started on 4 DPI -cABC and growth factors (GFs: EGF, FGF2, and PDGF-AA) (i.t.) with an osmotic pump for 7 days: no single administration Groups: TMT, cABC + GFs, Combined | (1) Absence of synergistic effects on kinematic parameters after cABC + GFs treatment; (2) cABC + GFs induced synergistic effects on neuroanatomical plasticity in collateral sprouting of CST and serotonergic fibers. |
| 2015 Ichikawa Y [64] SD rats (female, N = 58) C3/4 dorsal hemisection | Subacute start at 1 week -Single-pellet reaching task with Whishaw apparatus, 20 min/day, 5 days/week for 5 weeks | Subacute; started at 1 week -K-II or cABC (i.t.) with an osmotic pump for 14 days Groups: Training, K-II, cABC, K-II + Training, cABC + Training | (1) K-II combinatorial treatment induced better functional recovery than each single treatment; (2) Each combinatorial treatment synergistically increased neurite growth; (3) The effects of K-II and cABC were comparable. |
| 2009 Maier JC [66] SD rats (female, N = 40 + 28), T-shaped lesion (T8), a bilateral dorsal hemisection, and a complete midline transection | Subacute start at 1 week -Bipedal TMT 20 min + quadrupedal TMT 20 min for 8 weeks | Acute intervention -Anti-Nogo-A antibody (i.t.) with an osmotic pump for 14 days Groups: TMT, anti-Nogo-A, Combined | (1) While both single treatments improved behavior, kinematics were different; (2) An anti-Nogo-A antibody increased regeneration and neuronal reorganization; (3) Combinatorial treatment did not show synergistic effects, possibly due to an increase in pain perception or interference with the recovery process. |
| 2017 Chen K [67] SD rats (female, N = 28) T-shaped lesion (T9) | Subacute start at 3 weeks -Bipedal TMT 20 min + quadrupedal TMT 20 min, 5 days/week for 8 weeks | Acute intervention -Anti-Nogo-A antibody (i.t.) with an osmotic pump for 14 days -Anticyclosporin-A antibody (ACsA) as the control Groups: ACsA, TMT + ACsA, anti-Nogo-A, TMT + anti-Nogo-A | (1) Combinatorial therapy improved motor function together with CST sprouting caudal to the lesion, increased serotonergic synapses onto lumbar motoneurons, and yielded the greatest reduction of lumbar interneural activity (c-Fos expression); (2) There were no treatment effects on thermal nociception, mechanical allodynia, or lesion volume. |
| 2013 Zhao RR [69] LH rats (N = 42) C4 bilateral dorsal column injuries | Late-subacute start multitask after cessation of anti-Nogo-A antibody treatment for 12 weeks (1) Montoya-type staircase reaching, 1 h/day, 5 days/week (2) Ladder walking, three rounds/session, four sessions/week | (1) Acute anti-Nogo-A (i.t.) injection for 2 weeks (2) Subacute cABC (i.t.) started at 3 weeks, five injections/10 days, with scar tissue dissection Groups: Training, Training + cABC, Training + anti-Nogo-A, Combined | (1) Each single agent in combination with rehabilitation showed similar effects, with increased sprouting and axonal regeneration; (2) Combinatorial treatment with an anti-Nogo-A antibody or cABC and rehabilitation was more effective; (3) An anti-Nogo-A antibody stimulated growth of larger axons (diameter > 3 μm), while cABC affected finer axons with varicosities more. |
| 2014 Zhang L [71] SD rats (female, N = 53) T10 transection | Subacute start at 1 week -Bipedal BWS-TMT, 20 min/day, 5 days/week for 8 weeks | Immediate implantation -Silicon sheet containing semaphorin 3A inhibitor (sema3Ai) for release over 2 months Groups: sema3Ai, Combined | (1) Combinatorial treatment induced better gait kinematics than a single treatment; (2) Highest level of synaptogenesis and reduction of lumbar interneural activity in the extensor pool at L4. |
| 2023 Griffin JM [73] SD rats (N = 194) T10 Moderate contusion. | Subacute start at 3 weeks post SCI -Bipedal and quadrupedal training. 20 + 20 min/days for each training, 5 days/week for 7 weeks | Acute -Epo D, Epo B, or Ixabepilone at 1 and 15 DPI (s.c. or i.p.) Groups: Each medication, Training, Epo D, Epo D + Training, Epo B, Epo B + Training | (1) Ixabepilone did not effectively cross the blood–brain barrier; (2) Epo B exerted the highest effect to decrease fibrotic scarring and increase serotonergic fiber regeneration and VGLUT1 expression; (3) Epo B and rehabilitation acted complementarily on gait parameter. |
3.4. Other Biochemical Treatments
3.4.1. Neuroprotective Agents
3.4.2. Neuroregenerative Agents
3.4.3. Others
| Basic Information/Model | Rehabilitation | Combinatorial Treatment | Effect |
|---|---|---|---|
| 2012 Wong JK [89] SD rats T9 hemisection (female) C5 hemisection (male) | Acute (main) or subacute start at 1 or 14 DPI -Two trials of a beam walking task for 5 days over 10 days (every other day) | Paired with training -AMPH (i.p.) Groups: Training, Combined | (1) AMPH treatment in combination with testing/retraining resulted in a larger lesion and impaired locomotor recovery; (2) Results were unique in the cervical and thoracic SCI models regardless of the treatment phase. |
| 2012 Krisa L [88] SD rats (male, N = 101) C3–C4 right side contusion | Subacute start at 13 DPI -Task-specific forelimb motor training, 15 min twice/day, 7 days/week for 12 weeks | Together with training -AMPH (i.p.) every third day until week 12 of training, excluding testing weeks Groups: Training, AMPH, Combined, Combined + EE | (1) Combinatorial treatment improved qualitative reaching but not kinematics, and there was no evidence of neuroprotection; (2) Rats in EE combined group showed less improvement. |
| 2020 Goldschmit Y [79] C57BL/6 mice (male, N = 82) T12 left hemisection | Subacute start at 1 week -Quadrupedal TMT with textured tread, 10 min twice/day, 5 days/week for 3 months | Acute; 60 min after SCI -BGS, rGOT1, and OxAc (i.v.) for 5 consecutive days Groups: TMT, BGS, Combined | (1) BGS treatment decreased the level of glutamate in CSF and increased axonal survival and GAP-43 expression in neuronal cells; (2) Combinatorial treatment reduced inflammation, scarring, and lesion size; enhanced axonal regeneration through the lesion; increased the level of synapses around motor neurons; and improved motor function at 3 months post SCI. |
| 2022 Hubscher CH [76] Wistar rats (male, N = 60) T9 moderate contusion | Subacute start at 2 weeks -Activity-based forelimb training + TMT stepping, 70 daily sessions | Chronic medication after all training sessions -Desmopressin (DDAVP, synthetic analog of arginine vasopressin) (i.p.) 3 days Groups: Training, DDAVP, Combined | Either intervention or treatment alone effectively decreased urination despite there being no additive effect. |
| 2017 Liu ZH [80] SD rats (female) C4/5 lateral hemisection | Acute start at 2 DPI -Pellet grasping training, 30 min twice/day for 3 weeks | Immediate; 30 min after SCI -DHA (i.v.) Groups: Training, DHA, Combined | (1) Combinatorial therapy induced greater functional recovery; (2) Combinatorial therapy induced more sprouting of uninjured CST and serotonergic fibers and synaptogenesis. |
| 2018 Torres-Espin A [78] Lewis rats (female, N = 132) C4 dorsolateral quadrant section | Chronic start at 8 week -Forelimb single-pellet reaching and grasping, 10 min/session, 4–5 days/week | Chronic inflammation induction at 8 weeks -Low dose of LPS (i.p.) Groups: Training, LPS, Combined | (1) Rehabilitation enhanced recovery dependent on intensity; (2) Combinatorial treatment restored original function rather than enhancing new motor strategies; (3) Cortical drive to affected forelimb muscles was recovered, and corticospinal innervation was restructured. |
| 2021 Schmidt E [77] Lewis rats (female, N = 60) C4 dorsolateral quadrant section | Subacute start at 14 DPI -Forelimb single-pellet reaching and grasping at high intensity, 10 min/session, 4–5 days/week | Subacute inflammation induction at 10 DPI -LPS (i.p.) Groups: Training, Combined | (1) Motor function was recovered secondarily without compensatory strategies; (2) Combinatorial treatment with LPS resolved chronic neuroinflammation around the lesion; (3) Combinatorial treatment with LPS increased long-term anxiety-like behavior. |
| 2021 Liu JT [84] SD rats (male, N = 50) T10 moderate contusion | Subacute start at 2 weeks -Quadrupedal TMT, 10 min twice/day, 6 days/week for 8 weeks | Acute; 30 min after SCI -MP (i.v.) Groups: MP, Combined | Combinatorial treatment induced (1) Better H/L function with preserved histology; (2) Reduced expression of Nogo receptor and CSPGs. |
| 2010 Park K [81] SD rats (male, N = 24) -T10 moderate contusion | Acutely started at 3 DPI -TMT for 15 min, twice a day, 6 days/week for 4 weeks | Acutely started at 1 DPI -MT administration twice per day for 28 days Groups: TMT, Combined | Combinatorial treatment with MT increased hindlimb movement and number of motor neuron at ventral horn and reduced level of iNOS. |
| 2014 Lee Y [82] SD rats (male, N = 21) T10 moderate contusion | Acute start at 3 DPI -TMT for 15 min, 6 days/week for 18 days | Immediate -MT administration twice per day for 21 days Groups: MT, Combined | (1) MT increased dendritic spine density; (2) Combinatorial treatment facilitated H/L functional recovery, reduced lesion size, increased the density of dendritic spines and axons, and increased the number of BrdU- and nestin-positive endogenous NS/PCs. |
| 2016 Wei D [86] Lewis rats (female, N = 23 + 20) C4 unilateral dorsolateral quadrant lesion | Subacute start at 1 week -Single-pellet skilled reaching task, 15 min/day, 5 days/week for 6 weeks | Immediate -Inhibition of cortical phosphokinase A using Rp-cAMP (i.t.) with an osmotic pump for 6 (experiment 1) or 4 (experiment 2) weeks Groups: Training, Rp-cAMP, Combined | Combinatorial treatment with Rp-cAMPS promoted functional recovery and collateral sprouting of CST axons, and Rp-cAMPS did not affect CREB phosphorylation. |
| 2016 Osuna-Carrasco LP [83] SD rats (female, N = 24) Penetrating ventral injury T13–L1 | Acute start at 3 DPI -TMT, 5 days/week, increasing duration (10–20 min for 4 weeks) | Immediate: 0, 24, and 48 h after SCI -TMX (a selective estrogen receptor modulator) (i.p.) Groups: TMT, TMX, Combined | (1) Combinatorial treatment induced the best kinematics; (2) TMX preserved spinal cord gray and white matter; (3) Training improved morphology. |
| 2018 Yin W [87] Beagle canines (18 months old, female, N = 12) T8 transection | Acute start -Passive ROM exercise Subacute -Ambulation training with slings and wheelchairs to support hip joints | Immediate implantation -Neuroprotective Taxol-modified LOCS Groups: Training, LOCS + Taxol | LOCS + Taxol promoted locomotor recovery with MEP improvement, neurogenesis, and axon regeneration to reconnect the spinal cord stumps and reduced glial scar formation. |
| 2020 Yarrow JF [75] SD rats (N = 73) T9 severe contusion | Subacute start at 7 DPI -Quadrupedal manually assisted BWS-TMT, 40 min/day, 5 days/week | Acute -Adjuvant TE weekly (i.m.) Groups: TE, Combined | (1) TE suppressed bone resorption, attenuated cancellous bone loss, and constrained muscle fiber-type transition and atrophy, and stepping was recovered in 20% of rats; (2) Addition of training stimulated bone formation and maintained muscle force production, and stepping was recovered in 75% of rats. |
4. Discussion
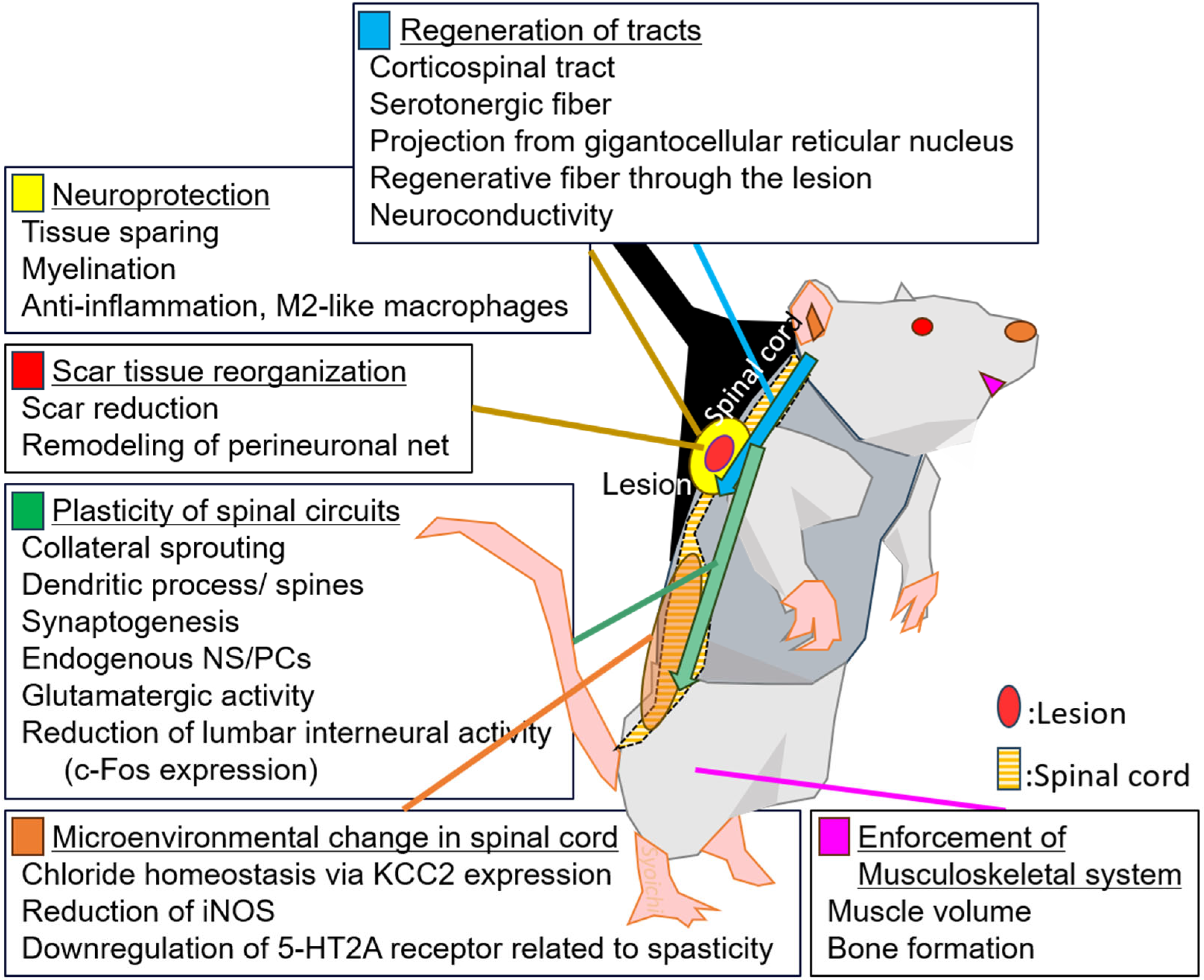
4.1. Mechanisms Underlying the Beneficial Effects of Combinatorial Treatment
4.2. Rehabilitative Training and Pharmacological Treatment Sometimes Act as Competing
4.3. Prospects of Rehabilitation Training and Medication for SCI Treatment
4.4. Limitation
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Teng, Y.D.; Zafonte, R.D. Prelude to the special issue on novel neurocircuit, cellular and molecular targets for developing functional rehabilitation therapies of neurotrauma. Exp. Neurol. 2021, 341, 113689. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, S.; Nakamura, M.; Okano, H. The prospects of regenerative medicine combined with rehabilitative approaches for chronic spinal cord injury animal models. Neural Regen. Res. 2017, 12, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Wessels, M.; Lucas, C.; Eriks, I.; de Groot, S. Body weight-supported gait training for restoration of walking in people with an incomplete spinal cord injury: A systematic review. J. Rehabil. Med. 2010, 42, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Okawara, H.; Tashiro, S.; Sawada, T.; Sugai, K.; Matsubayashi, K.; Kawakami, M.; Nori, S.; Tsuji, O.; Nagoshi, N.; Matsumoto, M.; et al. Neurorehabilitation using a voluntary driven exoskeletal robot improves trunk function in patients with chronic spinal cord injury: A single-arm study. Neural Regen. Res. 2022, 17, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Nam, K.Y.; Kim, H.J.; Kwon, B.S.; Park, J.W.; Lee, H.J.; Yoo, A. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injury: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 24. [Google Scholar] [CrossRef]
- Patil, S.; Raza, W.A.; Jamil, F.; Caley, R.; O’Connor, R.J. Functional electrical stimulation for the upper limb in tetraplegic spinal cord injury: A systematic review. J. Med. Eng. Technol. 2014, 39, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Santos, L.V.; Pereira, E.T.; Reguera-Garcia, M.M.; Oliveira, C.E.P.; Moreira, O.C. Resistance Training and Muscle Strength in people with Spinal cord injury: A systematic review and meta-analysis. J. Bodyw. Mov. Ther. 2022, 29, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, S.; Tsuji, O.; Shinozaki, M.; Shibata, T.; Yoshida, T.; Tomioka, Y.; Unai, K.; Kondo, T.; Itakura, G.; Kobayashi, Y.; et al. Current progress of rehabilitative strategies in stem cell therapy for spinal cord injury: A review. NPJ Regen. Med. 2021, 6, 81. [Google Scholar] [CrossRef] [PubMed]
- Houle, J.D.; Cote, M.P. Axon regeneration and exercise-dependent plasticity after spinal cord injury. Ann. N. Y. Acad. Sci. 2013, 1279, 154–163. [Google Scholar] [CrossRef]
- Girgis, J.; Merrett, D.; Kirkland, S.; Metz, G.A.; Verge, V.; Fouad, K. Reaching training in rats with spinal cord injury promotes plasticity and task specific recovery. Brain 2007, 130, 2993–3003. [Google Scholar] [CrossRef]
- Ichiyama, R.M.; Courtine, G.; Gerasimenko, Y.P.; Yang, G.J.; van den Brand, R.; Lavrov, I.A.; Zhong, H.; Roy, R.R.; Edgerton, V.R. Step training reinforces specific spinal locomotor circuitry in adult spinal rats. J. Neurosci. 2008, 28, 7370–7375. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tahayori, B.; Koceja, D.M. Activity-dependent plasticity of spinal circuits in the developing and mature spinal cord. Neural Plast. 2012, 2012, 964843. [Google Scholar] [CrossRef] [PubMed]
- Takeoka, A.; Vollenweider, I.; Courtine, G.; Arber, S. Muscle spindle feedback directs locomotor recovery and circuit reorganization after spinal cord injury. Cell 2014, 159, 1626–1639. [Google Scholar] [CrossRef] [PubMed]
- Asboth, L.; Friedli, L.; Beauparlant, J.; Martinez-Gonzalez, C.; Anil, S.; Rey, E.; Baud, L.; Pidpruzhnykova, G.; Anderson, M.A.; Shkorbatova, P.; et al. Cortico-reticulo-spinal circuit reorganization enables functional recovery after severe spinal cord contusion. Nat. Neurosci. 2018, 21, 576–588. [Google Scholar] [CrossRef]
- Petruska, J.C.; Ichiyama, R.M.; Jindrich, D.L.; Crown, E.D.; Tansey, K.E.; Roy, R.R.; Edgerton, V.R.; Mendell, L.M. Changes in motoneuron properties and synaptic inputs related to step training after spinal cord transection in rats. J. Neurosci. 2007, 27, 4460–4471. [Google Scholar] [CrossRef] [PubMed]
- Winchester, P.; McColl, R.; Querry, R.; Foreman, N.; Mosby, J.; Tansey, K.; Williamson, J. Changes in supraspinal activation patterns following robotic locomotor therapy in motor-incomplete spinal cord injury. Neurorehabilit. Neural Repair 2005, 19, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Cote, M.P.; Azzam, G.A.; Lemay, M.A.; Zhukareva, V.; Houle, J.D. Activity-dependent increase in neurotrophic factors is associated with an enhanced modulation of spinal reflexes after spinal cord injury. J. Neurotrauma 2011, 28, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Ward, P.J.; Herrity, A.N.; Smith, R.R.; Willhite, A.; Harrison, B.J.; Petruska, J.C.; Harkema, S.J.; Hubscher, C.H. Novel multi-system functional gains via task specific training in spinal cord injured male rats. J. Neurotrauma 2014, 31, 819–833. [Google Scholar] [CrossRef]
- Hwang, D.H.; Shin, H.Y.; Kwon, M.J.; Choi, J.Y.; Ryu, B.Y.; Kim, B.G. Survival of neural stem cell grafts in the lesioned spinal cord is enhanced by a combination of treadmill locomotor training via insulin-like growth factor-1 signaling. J. Neurosci. 2014, 34, 12788–12800. [Google Scholar] [CrossRef]
- Tashiro, S.; Nakamura, M.; Okano, H. Regenerative Rehabilitation and Stem Cell Therapy Targeting Chronic Spinal Cord Injury: A Review of Preclinical Studies. Cells 2022, 11, 685. [Google Scholar] [CrossRef]
- Teng, Y.D.; Liao, W.L.; Choi, H.; Konya, D.; Sabharwal, S.; Langer, R.; Sidman, R.L.; Snyder, E.Y.; Frontera, W.R. Physical activity-mediated functional recovery after spinal cord injury: Potential roles of neural stem cells. Regen. Med. 2006, 1, 763–776. [Google Scholar] [CrossRef]
- Foret, A.; Quertainmont, R.; Botman, O.; Bouhy, D.; Amabili, P.; Brook, G.; Schoenen, J.; Franzen, R. Stem cells in the adult rat spinal cord: Plasticity after injury and treadmill training exercise. J. Neurochem. 2010, 112, 762–772. [Google Scholar] [CrossRef]
- Bodine, S.C. Disuse-induced muscle wasting. Int. J. Biochem. Cell Biol. 2013, 45, 2200–2208. [Google Scholar] [CrossRef]
- Stevens, J.E.; Liu, M.; Bose, P.; O’Steen, W.A.; Thompson, F.J.; Anderson, D.K.; Vandenborne, K. Changes in soleus muscle function and fiber morphology with one week of locomotor training in spinal cord contusion injured rats. J. Neurotrauma 2006, 23, 1671–1681. [Google Scholar] [CrossRef]
- Tashiro, S.; Nishimura, S.; Iwai, H.; Sugai, K.; Zhang, L.; Shinozaki, M.; Iwanami, A.; Toyama, Y.; Liu, M.; Okano, H.; et al. Functional Recovery from Neural Stem/Progenitor Cell Transplantation Combined with Treadmill Training in Mice with Chronic Spinal Cord Injury. Sci. Rep. 2016, 6, 30898. [Google Scholar] [CrossRef] [PubMed]
- Antri, M.; Orsal, D.; Barthe, J.Y. Locomotor recovery in the chronic spinal rat: Effects of long-term treatment with a 5-HT2 agonist. Eur. J. Neurosci. 2002, 16, 467–476. [Google Scholar] [CrossRef] [PubMed]
- Foffani, G.; Shumsky, J.; Knudsen, E.B.; Ganzer, P.D.; Moxon, K.A. Interactive Effects between Exercise and Serotonergic Pharmacotherapy on Cortical Reorganization after Spinal Cord Injury. Neurorehabilit. Neural Repair 2016, 30, 479–489. [Google Scholar] [CrossRef]
- de Leon, R.D.; Acosta, C.N. Effect of robotic-assisted treadmill training and chronic quipazine treatment on hindlimb stepping in spinally transected rats. J. Neurotrauma 2006, 23, 1147–1163. [Google Scholar] [CrossRef] [PubMed]
- Courtine, G.; Gerasimenko, Y.; van den Brand, R.; Yew, A.; Musienko, P.; Zhong, H.; Song, B.; Ao, Y.; Ichiyama, R.M.; Lavrov, I.; et al. Transformation of nonfunctional spinal circuits into functional states after the loss of brain input. Nat. Neurosci. 2009, 12, 1333–1342. [Google Scholar] [CrossRef] [PubMed]
- van den Brand, R.; Heutschi, J.; Barraud, Q.; DiGiovanna, J.; Bartholdi, K.; Huerlimann, M.; Friedli, L.; Vollenweider, I.; Moraud, E.M.; Duis, S.; et al. Restoring voluntary control of locomotion after paralyzing spinal cord injury. Science 2012, 336, 1182–1185. [Google Scholar] [CrossRef] [PubMed]
- Bonizzato, M.; James, N.D.; Pidpruzhnykova, G.; Pavlova, N.; Shkorbatova, P.; Baud, L.; Martinez-Gonzalez, C.; Squair, J.W.; DiGiovanna, J.; Barraud, Q.; et al. Multi-pronged neuromodulation intervention engages the residual motor circuitry to facilitate walking in a rat model of spinal cord injury. Nat. Commun. 2021, 12, 1925. [Google Scholar] [CrossRef]
- Pizzolato, C.; Gunduz, M.A.; Palipana, D.; Wu, J.; Grant, G.; Hall, S.; Dennison, R.; Zafonte, R.D.; Lloyd, D.G.; Teng, Y.D. Non-invasive approaches to functional recovery after spinal cord injury: Therapeutic targets and multimodal device interventions. Exp. Neurol. 2021, 339, 113612. [Google Scholar] [CrossRef]
- Ganzer, P.D.; Moxon, K.A.; Knudsen, E.B.; Shumsky, J.S. Serotonergic pharmacotherapy promotes cortical reorganization after spinal cord injury. Exp. Neurol. 2013, 241, 84–94. [Google Scholar] [CrossRef]
- Ganzer, P.D.; Beringer, C.R.; Shumsky, J.S.; Nwaobasi, C.; Moxon, K.A. Serotonin receptor and dendritic plasticity in the spinal cord mediated by chronic serotonergic pharmacotherapy combined with exercise following complete SCI in the adult rat. Exp. Neurol. 2018, 304, 132–142. [Google Scholar] [CrossRef]
- Yao, Q.; Guan, J.; Ma, L.; Cheng, L.; Duan, F.; Xu, F.; Zhao, W.; Duan, W.; Wu, H.; Chen, Z.; et al. Wireless Epidural Electrical Stimulation in Combination With Serotonin Agonists Improves Intraspinal Metabolism in Spinal Cord Injury Rats. Neuromodul. Technol. Neural Interface 2021, 24, 416–426. [Google Scholar] [CrossRef]
- Graziano, A.; Foffani, G.; Knudsen, E.B.; Shumsky, J.; Moxon, K.A. Passive exercise of the hind limbs after complete thoracic transection of the spinal cord promotes cortical reorganization. PLoS ONE 2013, 8, e54350. [Google Scholar] [CrossRef]
- Cristante, A.F.; Filho, T.E.; Oliveira, R.P.; Marcon, R.M.; Ferreira, R.; Santos, G.B. Effects of antidepressant and treadmill gait training on recovery from spinal cord injury in rats. Spinal Cord 2013, 51, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Ryu, Y.; Ogata, T.; Nagao, M.; Sawada, Y.; Nishimura, R.; Fujita, N. Effects of Treadmill Training Combined with Serotonergic Interventions on Spasticity after Contusive Spinal Cord Injury. J. Neurotrauma 2018, 35, 1358–1366. [Google Scholar] [CrossRef] [PubMed]
- Ung, R.V.; Rouleau, P.; Guertin, P.A. Functional and physiological effects of treadmill training induced by buspirone, carbidopa, and L-DOPA in clenbuterol-treated paraplegic mice. Neurorehabilit. Neural Repair 2012, 26, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Skinner, R.D.; Arfaj, A.; Yates, C.; Reese, N.B.; Williams, K.; Garcia-Rill, E. L-Dopa effect on frequency-dependent depression of the H-reflex in adult rats with complete spinal cord transection. Brain Res. Bull. 2010, 83, 262–265. [Google Scholar] [CrossRef]
- Harvey, A.R.; Lovett, S.J.; Majda, B.T.; Yoon, J.H.; Wheeler, L.P.; Hodgetts, S.I. Neurotrophic factors for spinal cord repair: Which, where, how and when to apply, and for what period of time? Brain Res. 2015, 1619, 36–71. [Google Scholar] [CrossRef]
- Tohda, C.; Kuboyama, T. Current and future therapeutic strategies for functional repair of spinal cord injury. Pharmacol. Ther. 2011, 132, 57–71. [Google Scholar] [CrossRef]
- Marchionne, F.; Krupka, A.J.; Smith, G.M.; Lemay, M.A. Intrathecal Delivery of BDNF into the Lumbar Cistern Re-Engages Locomotor Stepping after Spinal Cord Injury. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 2459–2467. [Google Scholar] [CrossRef]
- Han, S.; Wang, B.; Jin, W.; Xiao, Z.; Li, X.; Ding, W.; Kapur, M.; Chen, B.; Yuan, B.; Zhu, T.; et al. The linear-ordered collagen scaffold-BDNF complex significantly promotes functional recovery after completely transected spinal cord injury in canine. Biomaterials 2015, 41, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Poduslo, J.F.; Curran, G.L. Permeability at the blood-brain and blood-nerve barriers of the neurotrophic factors: NGF, CNTF, NT-3, BDNF. Mol. Brain Res. 1996, 36, 280–286. [Google Scholar] [CrossRef]
- Boyce, V.S.; Park, J.; Gage, F.H.; Mendell, L.M. Differential effects of brain-derived neurotrophic factor and neurotrophin-3 on hindlimb function in paraplegic rats. Eur. J. Neurosci. 2012, 35, 221–232. [Google Scholar] [CrossRef]
- Lin, J.; Anopas, D.; Milbreta, U.; Lin, P.H.; Chin, J.S.; Zhang, N.; Wee, S.K.; Tow, A.; Ang, W.T.; Chew, S.Y. Regenerative rehabilitation: Exploring the synergistic effects of rehabilitation and implantation of a bio-functional scaffold in enhancing nerve regeneration. Biomater. Sci. 2019, 7, 5150–5160. [Google Scholar] [CrossRef] [PubMed]
- Tom, B.; Witko, J.; Lemay, M.; Singh, A. Effects of bioengineered scaffold loaded with neurotrophins and locomotor training in restoring H-reflex responses after spinal cord injury. Exp. Brain Res. 2018, 236, 3077–3084. [Google Scholar] [CrossRef]
- Tashiro, S.; Shinozaki, M.; Mukaino, M.; Renault-Mihara, F.; Toyama, Y.; Liu, M.; Nakamura, M.; Okano, H. BDNF Induced by Treadmill Training Contributes to the Suppression of Spasticity and Allodynia after Spinal Cord Injury via Upregulation of KCC2. Neurorehabilit. Neural Repair 2015, 29, 677–689. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Li, Y.; Yu, B.; Zhang, Z.; Brommer, B.; Williams, P.R.; Liu, Y.; Hegarty, S.V.; Zhou, S.; Zhu, J.; et al. Reactivation of Dormant Relay Pathways in Injured Spinal Cord by KCC2 Manipulations. Cell 2018, 174, 1599. [Google Scholar] [CrossRef] [PubMed]
- Petrosyan, H.A.; Alessi, V.; Hunanyan, A.S.; Sisto, S.A.; Arvanian, V.L. Spinal electro-magnetic stimulation combined with transgene delivery of neurotrophin NT-3 and exercise: Novel combination therapy for spinal contusion injury. J. Neurophysiol. 2015, 114, 2923–2940. [Google Scholar] [CrossRef]
- Park, C.H.; Joa, K.L.; Lee, M.O.; Yoon, S.H.; Kim, M.O. The combined effect of granulocyte-colony stimulating factor (G-CSF) treatment and exercise in rats with spinal cord injury. J. Spinal Cord Med. 2020, 43, 339–346. [Google Scholar] [CrossRef]
- Han, Q.; Xiang, J.; Zhang, Y.; Qiao, H.; Shen, Y.; Zhang, C. Enhanced neuroprotection and improved motor function in traumatized rat spinal cords by rAAV2-mediated glial-derived neurotrophic factor combined with early rehabilitation training. Chin. Med. J. 2014, 127, 4220–4225. [Google Scholar] [CrossRef]
- Alluin, O.; Delivet-Mongrain, H.; Gauthier, M.K.; Fehlings, M.G.; Rossignol, S.; Karimi-Abdolrezaee, S. Examination of the combined effects of chondroitinase ABC, growth factors and locomotor training following compressive spinal cord injury on neuroanatomical plasticity and kinematics. PLoS ONE 2014, 9, e111072. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, E.J.; Moon, L.D.; Popat, R.J.; King, V.R.; Bennett, G.S.; Patel, P.N.; Fawcett, J.W.; McMahon, S.B. Chondroitinase ABC promotes functional recovery after spinal cord injury. Nature 2002, 416, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Tester, N.J.; Howland, D.R. Chondroitinase ABC improves basic and skilled locomotion in spinal cord injured cats. Exp. Neurol. 2008, 209, 483–496. [Google Scholar] [CrossRef]
- Garcia-Alias, G.; Barkhuysen, S.; Buckle, M.; Fawcett, J.W. Chondroitinase ABC treatment opens a window of opportunity for task-specific rehabilitation. Nat. Neurosci. 2009, 12, 1145–1151. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Ichiyama, R.M.; Zhao, R.; Andrews, M.R.; Fawcett, J.W. Chondroitinase combined with rehabilitation promotes recovery of forelimb function in rats with chronic spinal cord injury. J. Neurosci. 2011, 31, 9332–9344. [Google Scholar] [CrossRef]
- Prager, J.; Ito, D.; Carwardine, D.R.; Jiju, P.; Chari, D.M.; Granger, N.; Wong, L.F. Delivery of chondroitinase by canine mucosal olfactory ensheathing cells alongside rehabilitation enhances recovery after spinal cord injury. Exp. Neurol. 2021, 340, 113660. [Google Scholar] [CrossRef]
- Shinozaki, M.; Iwanami, A.; Fujiyoshi, K.; Tashiro, S.; Kitamura, K.; Shibata, S.; Fujita, H.; Nakamura, M.; Okano, H. Combined treatment with chondroitinase ABC and treadmill rehabilitation for chronic severe spinal cord injury in adult rats. Neurosci. Res. 2016, 113, 37–47. [Google Scholar] [CrossRef]
- Sinopoulou, E.; Spejo, A.B.; Roopnarine, N.; Burnside, E.R.; Bartus, K.; De Winter, F.; McMahon, S.B.; Bradbury, E.J. Chronic muscle recordings reveal recovery of forelimb function in spinal injured female rats after cortical epidural stimulation combined with rehabilitation and chondroitinase ABC. J. Neurosci. Res. 2022, 100, 2055–2076. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.S.; Hellenbrand, D.; Reichl, K.; Umhoefer, J.; Filipp, M.; Choe, J.; Hanna, A.; Murphy, W.L. A Localized Materials-Based Strategy to Non-Virally Deliver Chondroitinase ABC mRNA Improves Hindlimb Function in a Rat Spinal Cord Injury Model. Adv. Healthc. Mater. 2022, 11, e2200206. [Google Scholar] [CrossRef] [PubMed]
- Griffin, J.M.; Fackelmeier, B.; Clemett, C.A.; Fong, D.M.; Mouravlev, A.; Young, D.; O’Carroll, S.J. Astrocyte-selective AAV-ADAMTS4 gene therapy combined with hindlimb rehabilitation promotes functional recovery after spinal cord injury. Exp. Neurol. 2020, 327, 113232. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Imagama, S.; Ohgomori, T.; Ishiguro, N.; Kadomatsu, K. A combination of keratan sulfate digestion and rehabilitation promotes anatomical plasticity after rat spinal cord injury. Neurosci. Lett. 2015, 593, 13–18. [Google Scholar] [CrossRef]
- He, Z.; Koprivica, V. The Nogo signaling pathway for regeneration block. Annu. Rev. Neurosci. 2004, 27, 341–368. [Google Scholar] [CrossRef]
- Maier, I.C.; Ichiyama, R.M.; Courtine, G.; Schnell, L.; Lavrov, I.; Edgerton, V.R.; Schwab, M.E. Differential effects of anti-Nogo-A antibody treatment and treadmill training in rats with incomplete spinal cord injury. Brain 2009, 132, 1426–1440. [Google Scholar] [CrossRef]
- Chen, K.; Marsh, B.C.; Cowan, M.; Al’Joboori, Y.D.; Gigout, S.; Smith, C.C.; Messenger, N.; Gamper, N.; Schwab, M.E.; Ichiyama, R.M. Sequential therapy of anti-Nogo-A antibody treatment and treadmill training leads to cumulative improvements after spinal cord injury in rats. Exp. Neurol. 2017, 292, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Harel, N.Y.; Song, K.H.; Tang, X.; Strittmatter, S.M. Nogo receptor deletion and multimodal exercise improve distinct aspects of recovery in cervical spinal cord injury. J. Neurotrauma 2010, 27, 2055–2066. [Google Scholar] [CrossRef]
- Zhao, R.R.; Andrews, M.R.; Wang, D.; Warren, P.; Gullo, M.; Schnell, L.; Schwab, M.E.; Fawcett, J.W. Combination treatment with anti-Nogo-A and chondroitinase ABC is more effective than single treatments at enhancing functional recovery after spinal cord injury. Eur. J. Neurosci. 2013, 38, 2946–2961. [Google Scholar] [CrossRef]
- Kaneko, S.; Wang, J.; Kaneko, M.; Yiu, G.; Hurrell, J.M.; Chitnis, T.; Khoury, S.J.; He, Z. Protecting axonal degeneration by increasing nicotinamide adenine dinucleotide levels in experimental autoimmune encephalomyelitis models. J. Neurosci. 2006, 26, 9794–9804. [Google Scholar] [CrossRef]
- Zhang, L.; Kaneko, S.; Kikuchi, K.; Sano, A.; Maeda, M.; Kishino, A.; Shibata, S.; Mukaino, M.; Toyama, Y.; Liu, M.; et al. Rewiring of regenerated axons by combining treadmill training with semaphorin3A inhibition. Mol. Brain 2014, 7, 14. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Tashiro, S.; Nagoshi, N.; Shinozaki, M.; Shibata, T.; Inoue, M.; Shibata, S.; Tsuji, T.; Okano, H.; Nakamura, M. Chronic Spinal Cord Injury regeneration with Neural Stem/Progenitor Cell transplantation, Rehabilitation and Semaphorin 3A inhibitor combined therapy. eNeuro 2024, 11, 0378-2. [Google Scholar] [CrossRef] [PubMed]
- Griffin, J.M.; Hingorani Jai Prakash, S.; Bockemuhl, T.; Benner, J.M.; Schaffran, B.; Moreno-Manzano, V.; Buschges, A.; Bradke, F. Rehabilitation enhances epothilone-induced locomotor recovery after spinal cord injury. Brain Commun. 2023, 5, fcad005. [Google Scholar] [CrossRef] [PubMed]
- Jakeman, L.B.; Hoschouer, E.L.; Basso, D.M. Injured mice at the gym: Review, results and considerations for combining chondroitinase and locomotor exercise to enhance recovery after spinal cord injury. Brain Res. Bull. 2011, 84, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Yarrow, J.F.; Kok, H.J.; Phillips, E.G.; Conover, C.F.; Lee, J.; Bassett, T.E.; Buckley, K.H.; Reynolds, M.C.; Wnek, R.D.; Otzel, D.M.; et al. Locomotor training with adjuvant testosterone preserves cancellous bone and promotes muscle plasticity in male rats after severe spinal cord injury. J. Neurosci. Res. 2020, 98, 843–868. [Google Scholar] [CrossRef]
- Hubscher, C.H.; Gumbel, J.H.; Armstrong, J.E.; Montgomery, L.R. Impact of activity-based recovery training and desmopressin on spinal cord injury-induced polyuria in Wistar rats. J. Spinal Cord Med. 2022, 46, 910–916. [Google Scholar] [CrossRef]
- Schmidt, E.; Raposo, P.; Vavrek, R.; Fouad, K. Inducing inflammation following subacute spinal cord injury in female rats: A double-edged sword to promote motor recovery. Brain Behav. Immun. 2021, 93, 55–65. [Google Scholar] [CrossRef]
- Torres-Espin, A.; Forero, J.; Fenrich, K.K.; Lucas-Osma, A.M.; Krajacic, A.; Schmidt, E.; Vavrek, R.; Raposo, P.; Bennett, D.J.; Popovich, P.G.; et al. Eliciting inflammation enables successful rehabilitative training in chronic spinal cord injury. Brain 2018, 141, 1946–1962. [Google Scholar] [CrossRef]
- Goldshmit, Y.; Banyas, E.; Bens, N.; Yakovchuk, A.; Ruban, A. Blood glutamate scavengers and exercises as an effective neuroprotective treatment in mice with spinal cord injury. J. Neurosurg. Spine 2020, 33, 692–704. [Google Scholar] [CrossRef]
- Liu, Z.H.; Yip, P.K.; Priestley, J.V.; Michael-Titus, A.T. A Single Dose of Docosahexaenoic Acid Increases the Functional Recovery Promoted by Rehabilitation after Cervical Spinal Cord Injury in the Rat. J. Neurotrauma 2017, 34, 1766–1777. [Google Scholar] [CrossRef]
- Park, K.; Lee, Y.; Park, S.; Lee, S.; Hong, Y.; Kil Lee, S.; Hong, Y. Synergistic effect of melatonin on exercise-induced neuronal reconstruction and functional recovery in a spinal cord injury animal model. J. Pineal Res. 2010, 48, 270–281. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lee, S.; Lee, S.R.; Park, K.; Hong, Y.; Lee, M.; Park, S.; Jin, Y.; Chang, K.T.; Hong, Y. Beneficial effects of melatonin combined with exercise on endogenous neural stem/progenitor cells proliferation after spinal cord injury. Int. J. Mol. Sci. 2014, 15, 2207–2222. [Google Scholar] [CrossRef] [PubMed]
- Osuna-Carrasco, L.P.; Lopez-Ruiz, J.R.; Mendizabal-Ruiz, E.G.; De la Torre-Valdovinos, B.; Banuelos-Pineda, J.; Jimenez-Estrada, I.; Duenas-Jimenez, S.H. Quantitative analysis of hindlimbs locomotion kinematics in spinalized rats treated with Tamoxifen plus treadmill exercise. Neuroscience 2016, 333, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.T.; Wang, S.Y.; Xiao, H.P.; Gu, B.; Li, H.N. Effects of methylprednisolone and treadmill training on spinal cord injury in experimental rats. Exp. Ther. Med. 2021, 22, 1413. [Google Scholar] [CrossRef] [PubMed]
- Caron, G.; Bilchak, J.; Cote, M.P. Bumetanide increases postsynaptic inhibition after chronic SCI and decreases presynaptic inhibition with step-training. J. Physiol. 2023, 601, 1425–1447. [Google Scholar] [CrossRef] [PubMed]
- Wei, D.; Hurd, C.; Galleguillos, D.; Singh, J.; Fenrich, K.K.; Webber, C.A.; Sipione, S.; Fouad, K. Inhibiting cortical protein kinase A in spinal cord injured rats enhances efficacy of rehabilitative training. Exp. Neurol. 2016, 283, 365–374. [Google Scholar] [CrossRef]
- Yin, W.; Li, X.; Zhao, Y.; Tan, J.; Wu, S.; Cao, Y.; Li, J.; Zhu, H.; Liu, W.; Tang, G.; et al. Taxol-modified collagen scaffold implantation promotes functional recovery after long-distance spinal cord complete transection in canines. Biomater. Sci. 2018, 6, 1099–1108. [Google Scholar] [CrossRef]
- Krisa, L.; Frederick, K.L.; Canver, J.C.; Stackhouse, S.K.; Shumsky, J.S.; Murray, M. Amphetamine-enhanced motor training after cervical contusion injury. J. Neurotrauma 2012, 29, 971–989. [Google Scholar] [CrossRef]
- Wong, J.K.; Steward, O. One day of motor training with amphetamine impairs motor recovery following spinal cord injury. Exp. Neurol. 2012, 233, 693–707. [Google Scholar] [CrossRef]
- Alvarez-Mejia, L.; Morales, J.; Cruz, G.J.; Olayo, M.G.; Olayo, R.; Diaz-Ruiz, A.; Rios, C.; Mondragon-Lozano, R.; Sanchez-Torres, S.; Morales-Guadarrama, A.; et al. Functional recovery in spinal cord injured rats using polypyrrole/iodine implants and treadmill training. J. Mater. Sci. Mater. Med. 2015, 26, 209. [Google Scholar] [CrossRef]
- Coyoy-Salgado, A.; Orozco-Barrios, C.; Sanchez-Torres, S.; Olayo, M.G.; Cruz, G.J.; Morales-Corona, J.; Olayo, R.; Diaz-Ruiz, A.; Rios, C.; Alvarez-Mejia, L.; et al. Gene expression and locomotor recovery in adult rats with spinal cord injury and plasma-synthesized polypyrrole/iodine application combined with a mixed rehabilitation scheme. Front. Neurol. 2023, 14, 1124245. [Google Scholar] [CrossRef]
- Sanchez-Torres, S.; Diaz-Ruiz, A.; Rios, C.; Olayo, M.G.; Cruz, G.J.; Olayo, R.; Morales, J.; Mondragon-Lozano, R.; Fabela-Sanchez, O.; Orozco-Barrios, C.; et al. Recovery of motor function after traumatic spinal cord injury by using plasma-synthesized polypyrrole/iodine application in combination with a mixed rehabilitation scheme. J. Mater. Sci. Mater. Med. 2020, 31, 58. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.X.; Zhao, Y.; Pan, S.; Qi, Z.P.; Kong, W.J.; Pan, Y.R.; Li, H.R.; Yang, X.Y. Intramuscular Injection of Adenoassociated Virus Encoding Human Neurotrophic Factor 3 and Exercise Intervention Contribute to Reduce Spasms after Spinal Cord Injury. Neural Plast. 2019, 2019, 3017678. [Google Scholar] [CrossRef]
- Shibata, T.; Tashiro, S.; Shinozaki, M.; Hashimoto, S.; Matsumoto, M.; Nakamura, M.; Okano, H.; Nagoshi, N. Treadmill training based on the overload principle promotes locomotor recovery in a mouse model of chronic spinal cord injury. Exp. Neurol. 2021, 345, 113834. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, X.; Li, W.; Zhang, Q.; Li, Y.; Zhang, Z.; Zhu, J.; Chen, B.; Williams, P.R.; Zhang, Y.; et al. A Sensitized IGF1 Treatment Restores Corticospinal Axon-Dependent Functions. Neuron 2017, 95, 817–833.e814. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.H.; Park, H.H.; Shin, H.Y.; Cui, Y.; Kim, B.G. Insulin-like Growth Factor-1 Receptor Dictates Beneficial Effects of Treadmill Training by Regulating Survival and Migration of Neural Stem Cell Grafts in the Injured Spinal Cord. Exp. Neurobiol. 2018, 27, 489–507. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.N.; Fisher, L.C.; Deibert, R.J.; Jakeman, L.B.; Zhang, H.; Noble-Haeusslein, L.; White, S.; Basso, D.M. Elevated MMP-9 in the lumbar cord early after thoracic spinal cord injury impedes motor relearning in mice. J. Neurosci. 2013, 33, 13101–13111. [Google Scholar] [CrossRef]
- Huie, J.R.; Baumbauer, K.M.; Lee, K.H.; Bresnahan, J.C.; Beattie, M.S.; Ferguson, A.R.; Grau, J.W. Glial tumor necrosis factor alpha (TNFalpha) generates metaplastic inhibition of spinal learning. PLoS ONE 2012, 7, e39751. [Google Scholar] [CrossRef]
- Endo, T.; Ajiki, T.; Inoue, H.; Kikuchi, M.; Yashiro, T.; Nakama, S.; Hoshino, Y.; Murakami, T.; Kobayashi, E. Early exercise in spinal cord injured rats induces allodynia through TrkB signaling. Biochem. Biophys. Res. Commun. 2009, 381, 339–344. [Google Scholar] [CrossRef]
- Weishaupt, N.; Li, S.; Di Pardo, A.; Sipione, S.; Fouad, K. Synergistic effects of BDNF and rehabilitative training on recovery after cervical spinal cord injury. Behav. Brain Res. 2013, 239, 31–42. [Google Scholar] [CrossRef]
- Brommer, B.; He, M.; Zhang, Z.; Yang, Z.; Page, J.C.; Su, J.; Zhang, Y.; Zhu, J.; Gouy, E.; Tang, J.; et al. Improving hindlimb locomotor function by Non-invasive AAV-mediated manipulations of propriospinal neurons in mice with complete spinal cord injury. Nat. Commun. 2021, 12, 781. [Google Scholar] [CrossRef]
- Kramer, A.A.; Olson, G.M.; Chakraborty, A.; Blackmore, M.G. Promotion of corticospinal tract growth by KLF6 requires an injury stimulus and occurs within four weeks of treatment. Exp. Neurol. 2021, 339, 113644. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Tan, B.; Tang, W.; Luo, M.; Liu, Y.; Yu, L.; Yin, Y. Combining task-based rehabilitative training with PTEN inhibition promotes axon regeneration and upper extremity skilled motor function recovery after cervical spinal cord injury in adult mice. Behav. Brain Res. 2021, 405, 113197. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Yi, L.; Liu, Y.; Liu, L.; Zhu, Y.; Zhong, J.; Wang, Y.; Yin, Y.; Yu, L.; Tan, B.; et al. Effects of task-based rehabilitative training combined with PTEN/SOCS3 coinhibition promotes axon regeneration and upper extremity skilled motor function recovery after cervical spinal cord injury in adult mice. Neurosci. Lett. 2023, 800, 137121. [Google Scholar] [CrossRef]
- Huang, Z.; Yarong, G.; Shimoda, Y.; Watanabe, K.; Liu, Y. Induced NB-3 Limits Regenerative Potential of Serotonergic Axons after Complete Spinal Transection. J. Neurotrauma 2019, 36, 436–447. [Google Scholar] [CrossRef]
- Shackleton, C.; Hodgkiss, D.; Samejima, S.; Miller, T.; Perez, M.A.; Nightingale, T.E.; Sachdeva, R.; Krassioukov, A.V. When the whole is greater than the sum of its parts: A scoping review of activity-based therapy paired with spinal cord stimulation following spinal cord injury. J. Neurophysiol. 2022, 128, 1292–1306. [Google Scholar] [CrossRef] [PubMed]
- Teng, Y.D. Functional Multipotency of Stem Cells and Recovery Neurobiology of Injured Spinal Cords. Cell Transplant. 2019, 28, 451–459. [Google Scholar] [CrossRef]
- Leydeker, M.; Delva, S.; Tserlyuk, I.; Yau, J.; Wagdy, M.; Hawash, A.; Bendaoud, S.; Mohamed, S.; Wieraszko, A.; Ahmed, Z. The effects of 15 Hz trans-spinal magnetic stimulation on locomotor control in mice with chronic contusive spinal cord injury. Electromagn. Biol. Med. 2013, 32, 155–164. [Google Scholar] [CrossRef]
- Theisen, C.C.; Sachdeva, R.; Austin, S.; Kulich, D.; Kranz, V.; Houle, J.D. Exercise and Peripheral Nerve Grafts as a Strategy to Promote Regeneration after Acute or Chronic Spinal Cord Injury. J. Neurotrauma 2017, 34, 1909–1914. [Google Scholar] [CrossRef]
- Shibata, T.; Tashiro, S.; Shibata, S.; Shinozaki, M.; Shindo, T.; Hashimoto, S.; Kawai, M.; Kitagawa, T.; Ago, K.; Matsumoto, M.; et al. Rehabilitative Training Enhances Therapeutic Effect of Human-iPSC-Derived Neural Stem/Progenitor Cells Transplantation in Chronic Spinal Cord Injury. Stem Cells Transl. Med. 2023, 12, 83–96. [Google Scholar] [CrossRef]
- Tashiro, S.; Nishimura, S.; Shinozaki, M.; Takano, M.; Konomi, T.; Tsuji, O.; Nagoshi, N.; Toyama, Y.; Liu, M.; Okano, H.; et al. The Amelioration of Pain-Related Behavior in Mice with Chronic Spinal Cord Injury Treated with Neural Stem/Progenitor Cell Transplantation Combined with Treadmill Training. J. Neurotrauma 2018, 35, 2561–2571. [Google Scholar] [CrossRef] [PubMed]
- Terashima, T. Anatomy, development and lesion-induced plasticity of rodent corticospinal tract. Neurosci. Res. 1995, 22, 139–161. [Google Scholar] [CrossRef] [PubMed]
- Fenrich, K.K.; Hallworth, B.W.; Vavrek, R.; Raposo, P.J.F.; Misiaszek, J.E.; Bennett, D.J.; Fouad, K.; Torres-Espin, A. Self-directed rehabilitation training intensity thresholds for efficient recovery of skilled forelimb function in rats with cervical spinal cord injury. Exp. Neurol. 2021, 339, 113543. [Google Scholar] [CrossRef] [PubMed]
| Agent | Training | Treatment Effect | Condition, Study |
|---|---|---|---|
| Quipazine | TMT | Increase in responding cells’ number in somatosensory cortex | Subacute, SD rats, T8/9 transection [27] |
| Bike training | Decrease in responding cells’ number in somatosensory cortex | ||
| cABC | Specific training with seeds retrieving | Better skill reaching accompanying histology | Subacute, LH rats, C4 dorsal funiculi cut [57] |
| Enriched environment | Worse skill reaching | ||
| Amphetamine | Single-pellet test training Staircase test training | Better skill reaching | Subacute, SD rats, C3–4 hemicontusion [88] |
| To further add enriched environment | Worse skill reaching | ||
| Beam walking | Impaired locomotion | Acute, SD rats, 2 models [89] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tashiro, S.; Shibata, S.; Nagoshi, N.; Zhang, L.; Yamada, S.; Tsuji, T.; Nakamura, M.; Okano, H. Do Pharmacological Treatments Act in Collaboration with Rehabilitation in Spinal Cord Injury Treatment? A Review of Preclinical Studies. Cells 2024, 13, 412. https://doi.org/10.3390/cells13050412
Tashiro S, Shibata S, Nagoshi N, Zhang L, Yamada S, Tsuji T, Nakamura M, Okano H. Do Pharmacological Treatments Act in Collaboration with Rehabilitation in Spinal Cord Injury Treatment? A Review of Preclinical Studies. Cells. 2024; 13(5):412. https://doi.org/10.3390/cells13050412
Chicago/Turabian StyleTashiro, Syoichi, Shinsuke Shibata, Narihito Nagoshi, Liang Zhang, Shin Yamada, Tetsuya Tsuji, Masaya Nakamura, and Hideyuki Okano. 2024. "Do Pharmacological Treatments Act in Collaboration with Rehabilitation in Spinal Cord Injury Treatment? A Review of Preclinical Studies" Cells 13, no. 5: 412. https://doi.org/10.3390/cells13050412
APA StyleTashiro, S., Shibata, S., Nagoshi, N., Zhang, L., Yamada, S., Tsuji, T., Nakamura, M., & Okano, H. (2024). Do Pharmacological Treatments Act in Collaboration with Rehabilitation in Spinal Cord Injury Treatment? A Review of Preclinical Studies. Cells, 13(5), 412. https://doi.org/10.3390/cells13050412








