Abstract
Polyamines, spermidine and spermine, are synthesized in every living cell and are therefore contained in foods, especially in those that are thought to contribute to health and longevity. They have many physiological activities similar to those of antioxidant and anti-inflammatory substances such as polyphenols. These include antioxidant and anti-inflammatory properties, cell and gene protection, and autophagy activation. We have first reported that increased polyamine intake (spermidine much more so than spermine) over a long period increased blood spermine levels and inhibited aging-associated pathologies and pro-inflammatory status in humans and mice and extended life span of mice. However, it is unlikely that the life-extending effect of polyamines is exerted by the same bioactivity as polyphenols because most studies using polyphenols and antioxidants have failed to demonstrate their life-extending effects. Recent investigations revealed that aging-associated pathologies and lifespan are closely associated with DNA methylation, a regulatory mechanism of gene expression. There is a close relationship between polyamine metabolism and DNA methylation. We have shown that the changes in polyamine metabolism affect the concentrations of substances and enzyme activities involved in DNA methylation. I consider that the increased capability of regulation of DNA methylation by spermine is a key of healthy long life of humans.
1. Introduction
Biological aging or senescence is associated with declines in physiological function and altered structural changes. The elderly become increasingly susceptibile to aging-associated pathologies such as sarcopenia, frailty, decreases in higher brain function such as decreased cognitive impairment, cardiovascular disease, metabolic diseases, neoplastic diseases, and neurodegenerative diseases. Epidemiological analyses and interventional trials have shown that, among many life-style factors, the differences in food preferences and dietary patterns contribute to the inhibition of aging-associated diseases and senescence. Among them, what has been carefully examined is that the relationship between increased consumption of soybeans and decreases in the incidence of cardiovascular diseases (CVDs) [1,2] and malignancies such as breast [3,4,5] and colon cancer [6,7,8,9], or a Mediterranean diet and increased vegetable intake are associated with a decreased incidence of lifestyle-related diseases, such as CVDs [10,11,12] and breast and colon cancer [13,14,15,16]. These findings indicate that ingredients contained in these foods play an important role in the inhibition of aging-associated pathologies.
Among these substances, antioxidant polyphenols were considered important candidates for extending healthy lifespans. Examples include isoflavones, found at high levels in soybeans, and resveratrol, which is prevalent in the Mediterranean diet. The molecules have many biological activities that counteract the pathogenesis of aging-associated pathologies. For example, they have antioxidant and anti-inflammatory properties [17,18,19,20,21,22], protect cells and genes from harmful stimuli [18,23], increase sirtuin expression, and induce autophagy [17,18,24,25,26,27,28,29,30,31]. Early animal experiments and research performed under specific conditions or in a particular animal demonstrated that the increased intake of polyphenols extended lifespans [32,33]. However, evidence from human intervention studies and recent animal experiments is inconsistent and inconclusive because many studies have failed to show any effects on the prevention of aging-associated pathologies and the extension of lifespan [27,34,35,36,37,38,39,40]. Similarly, vitamin E and β-carotene with potent antioxidant and autophagy-induction properties increased, rather than decreased, the incidence of CVDs and related mortality [41,42,43,44,45,46,47,48].
Based on these scientific facts, we considered that substances other than antioxidants contained in these foods are exerting their health and longevity effects. At that time, we found that natural polyamine synthesized in all cells from the lower primitive organisms to humans and contained abundantly in soybeans and the Mediterranean diet have strong anti-inflammatory properties [49]. Polyamines, spermine and spermidine, in food are absorbed from the intestinal tract, and these polyamines are considered one of the most important sources of polyamines in the body. We also examined the relationship between polyamine content and dietary patterns using the food supply database of 49 Western countries from the Food and Agriculture Organization of the United Nations, and we found that the Mediterranean diet is composed of many polyamine-rich food [50,51]. Simultaneously, we first showed that mouse lifespans were increased by the life-time consumption of chow containing synthetic polyamines with an overall polyamine concentration of about three times that in soybeans [52]. Moreover, when mice with no baseline-elevated risk of carcinogenesis or prior treatment with carcinogenic stimuli were reared on three types of chow with different polyamine concentrations and then multiple, moderate doses of a carcinogen were administered, mice that were fed high-polyamine chow had a significantly lower incidence of colon tumors (most of them were cancer) [53]. In addition, we further examined the biological background of life span extension by increased polyamine intake [53,54,55]. Simultaneously, an intervention trial in humans confirmed the same changes in biological markers observed in mouse models and in vitro studies [56]. The current review will introduce the polyamines in general that has been clarified by many previous papers and discuss the biological background of polyamine-induced life span extension of mammals including humans.
2. Polyamine
The natural polyamines (spermine and spermidine) and their precursor, putrescine, are ubiquitous low-molecular-weight aliphatic amines, which contain multiple amino groups (-NH2). Spermine and spermidine have four and three amino groups, respectively, and molecular weights of approximately 140 and 200 g/mol, respectively. Putrescine, a precursor of polyamine, has two amines and is therefore referred to as a diamine. Polyamines are synthesized within all living cells. In eukaryotes, polyamine synthesis begins with ornithine, which is synthesized through the urea cycle from arginine. The decarboxylation of ornithine catalyzed by ornithine decarboxylase (ODC) is the rate-limiting step in polyamine synthesis. Spermidine and spermine are then synthesized by the sequential addition of aminopropyl groups donated from decarboxylated S-adenosylmethionine (dcSAM), which is converted from S-adenosylmethionine (SAM) by the enzymatic activities of adenosylmethionine decarboxylase (AdoMetDC) (Figure 1).
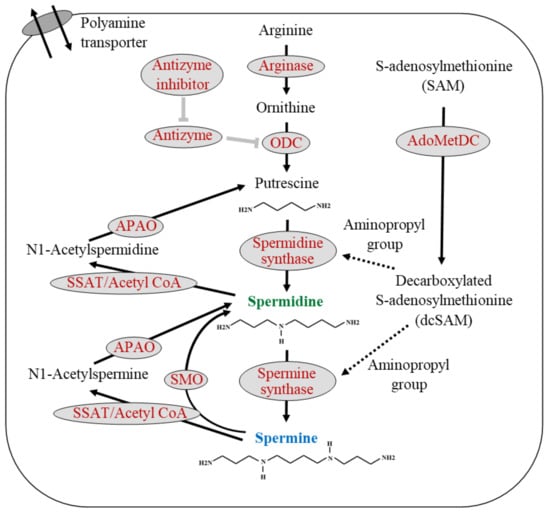
Figure 1.
Polyamine biosynthesis, degradation, and transmembrane transport. The polyamines are synthesized from arginine. Arginase converts arginine to ornithine, and ornithine decarboxylase (ODC), a rate-limiting enzyme with a short half-life, catalyzes the decarboxylation of ornithine to form putrescine, a polyamine precursor containing two amine groups. ODC is inhibited by antizyme, and antizyme is inhibited by an antizyme inhibitor. S-adenosylmethionine decarboxylase (AdoMetDC) is the second rate-limiting enzyme in polyamine synthesis and is involved in the decarboxylation of s-adenosylmethionine (SAM). Spermidine synthetase and spermine synthase are constitutively expressed aminopropyl transferases that catalyze the transfer of the aminopropyl group from decarboxylated s-adenosylmethionine (dcSAM) to putrescine and spermidine to form spermidine and spermine, respectively. Polyamine catabolism is mediated by the back conversion pathway in which spermine or spermidine are first acetylated by spermine/spermidine N1-acetyltransferase (SSAT) and then oxidized by N1-acetylpolyamine oxidase (APAO) to yield spermidine or putrescine, respectively. Spermine can be directly converted to spermidine via the spermine oxidase (SMO) reaction. Polyamines are transported across the membrane by the polyamine transporter. Black text indicates the substance name, while spermidine and spermine are shown in green and blue, respectively. Red letters indicate enzyme names. The solid black arrows indicate the metabolic pathway, and the dashed black arrows indicate the transfer of some material from the upstream material. Thick gray T-bars indicate inhibitory activity on the target. ODC: Ornithine decarboxylase; SSAT: Spermidine/spermine N1-acetyltransferase; APAO: N1-acetylpolyamine oxidase; SMO: Spermine oxidase; SAM: S-adenosylmethionine; AdoMetDC: Adenosylmethionine decarboxylase; dcSAM: Decarboxylated S-adenosylmethionine.
Spermidine/spermine N-(1)-acetyltransferase (SSAT) and N1-acetylpolyamine oxidase (APAO) degrade intracellular spermine and spermidine. SSAT, a highly inducible enzyme, catalyzes the transfer of acetyl groups from acetyl-coenzyme A to the terminal amines of spermine and spermidine. APAO preferentially catalyzes the oxidation of the N1-acetylspermine and N1-acetylspermidine produced by SSAT activity and yields spermidine and putrescine with the release of an aldehyde and hydrogen peroxide. Alternatively, spermine oxidase (SMO) directly convert spermine to spermidine and release an aldehyde and hydrogen peroxide. Additionally, the polyamine transporter located in the cell membrane can transport polyamines across the cell membrane. The cellular levels of polyamines are tightly regulated through their import, export, synthesis, and catabolism (Figure 1).
Polyamines are universally prerequisite for cell growth and differentiation. However, each of them is of different importance to different organisms. In lower organisms such as bacteria and fungi, putrescine is essential for growth, whereas spermine is not present in the cell [57,58,59,60,61]. In yeasts and nematodes, the concentration of spermine is low and is nonessential for growth [62,63]. These indicate that the role of spermine in cell growth, differentiation, and cell function is insignificant in these lower primitive organisms. Spermine is considered more important in highly developed animals. In fact, a decrease in spermine levels due to a deficiency in spermine synthase have dreadful consequences in humans [64].
In addition to intracellular de novo synthesis, cells can take up polyamine from the extracellular space through a polyamine transporter in the cell membrane. The effects of extracellular polyamine on intracellular polyamine concentration are noticeable in cancer patients. Polyamine biosynthesis is upregulated in cancer cells, and therefore, polyamine concentrations are higher in cancer tissues than in normal surrounding tissues [65,66,67]. Circulating blood cells also take up polyamines synthesized in cancer cells; as a result, the blood cell concentrations and urinary excretion of polyamines, especially those of spermidine, are increased in cancer patients [65,67,68]. These levels decrease after tumor eradication and increase after relapse, indicating that polyamines synthesized in any part of the body, e.g., in cancer tissues, are transferred to blood cells [69].
3. Aging and Polyamine
The activity of ODC, the rate-limiting enzyme in polyamine synthesis, declines with age [70,71,72]. ODC has been well characterized and has had a short half-life and to be stimulated by various factors [71,73]. The properties of spermidine synthase and spermine synthase have not been fully clarified, however, they seem to lack a regulatory or rate-limiting role in polyamine synthesis. The administration of arginine or ornithine stimulates putrescine levels; however, the subsequent synthesis of polyamines is not necessarily stimulated in elderly people or aged animals [72,74,75,76]. These findings indicate that the activities of spermine and spermidine synthases decrease gradually with aging.
From these findings, it appears that the polyamine concentrations decrease with aging, and it has been reported that there is an age-associated decrease in polyamine concentrations. Madeo et al., citing mainly their own papers, stated that spermidine concentrations decline in an age-dependent manner [77]. However, their group did not show any data on aging-associated changes in polyamine concentrations in humans. The age-associated decline in polyamine concentrations described in the title and abstract in the papers indicate a decline during early life (fetal period or developmental period) [78]. This decrease slows down markedly in adulthood, and there is no significant decrease in healthy adult animals or humans. Nishimura et al. found that polyamine concentrations in various tissues and organs were significantly lower in 10- and 26-week-old mice than in 3-week-old mice, but no differences in spermine and spermidine concentrations were observed between 10- and 26-week-old mice, except the skin [79]. Morrison et al. measured polyamine levels in autopsied human brain, and they reported that no statistically significant influence of aging (from 1 day to 103 years old) on either putrescine or spermine levels, and spermidine levels increased markedly from birth, reaching maximal levels up to 40 years of age and maintained up to old age [80]. Similarly, an age-associated increase, but not decrease, in spermidine concentrations was also reported in a few organs and the semen of animals and humans in good health [81,82].
Polyamine concentrations in blood cells reflect polyamine levels in organs and tissues throughout the body. Elworthy and Hitchcock measured red blood cell polyamine concentrations in 117 patients (ranging from 0 to 80 years old) who were largely in good health but had various neurological problems known not to affect polyamine levels and reported no statistically significant age-dependent changes in spermine or spermidine concentrations [83]. Chaisiri et al. also showed no age-associated decline in plasma polyamine concentrations [84]. Our analyses of aging-associated changes in blood polyamine concentrations in human male volunteers showed no age-associated decline in polyamine concentrations [49,56].
Similarly, urinary polyamine excretion, which reflects blood polyamine concentrations, does not change with age during adulthood. van den Berg et al. measured urinary polyamine excretion in 51 healthy volunteers whose ages ranged from 4 days to 77 years and found an age-dependent decrease in urinary excretion of spermidine in terms of creatinine excretion. However, they clearly indicated that the overall age-dependent decline was merely due to the rapid decrease during the first year of life, and it did not occur during adulthood [85]. Yodfat et al. also examined urinary polyamine concentrations in 171 male and 166 female healthy volunteers whose ages ranged from 14 days to 84 years and demonstrated an age-dependent decrease in diamine levels in males but no age-dependent decrease of polyamines (either spermidine or spermine) in either gender [86]. Several reports have shown that the ratio of spermine/spermidine tends to decrease due to the absence of an age-related decrease in spermidine concentration and an age-related decreasing trend in spermine concentration [56,83,87].
While there is no age-associated decline in polyamine concentrations in tissues, organs, blood, and urine of animals and humans, it is pointed out that there are large inter-individual differences in blood polyamine concentrations [49,83]. The exact biological mechanisms underlying the large inter-individual differences in blood polyamine concentrations are not fully understood. However, these large individual differences in polyamine concentration are one aspect that makes the clinical application of polyamines difficult. In cancer patients, polyamine levels are elevated due to the active synthesis of polyamines in cancer cells, and attempts have been made to diagnose the presence of cancer using polyamine levels as an indicator. Due to this large individual difference, it has been difficult to apply polyamine blood levels and urinary polyamine excretion to the diagnosis of neoplastic diseases. These indicate that reports examining polyamine concentrations in few cases are unreliable. Note that due to the large difference in polyamine concentration, the analysis results vary greatly depending on the choice of cases. For example, Pekar et al. showed that impaired cognitive function is associated with low serum spermidine level [88]. In contrast, Sternberg et al. showed that impaired cognitive function is associated with high serum spermidine levels [89].
4. The Effect of Dietary Polyamines on the Body Polyamine
In healthy adult animals and humans, the major source of polyamines is thought to be in the digestive tract, i.e., polyamines in food and polyamines synthesized by the intestinal microbiota. Therefore, a factor to create wide inter-individual differences in polyamine concentrations is thought to be the difference in the polyamine amount supplied from the digestive tract. In fact, a decrease in polyamine intake due to a polyamine-deficient diet and a decrease in polyamine synthesis by intestinal bacteria due to the elimination of intestinal microbiota by antimicrobial agents will lead to a gradual decrease in blood polyamine levels [90,91,92]. Conversely, a long-term increase in the polyamine supply from food gradually increases blood polyamine concentrations, especially spermine concentrations, in humans and mice [52,56,93].
Polyamines exist in all living organisms, and thus, foods that comprise various types of organisms and their related substances contain polyamines, though at a wide variety of concentrations. Germ and bran, legumes such as soybeans, vegetables, and shellfish are foods with high polyamine concentrations per calorie, and spermidine is contained much more than spermine in food [79,94,95,96]. The polyamine concentration in a particular food differs depending on the part of the food examined [96,97]. For example, although fish and shellfish are lower in polyamines than beans and vegetables, higher concentrations of polyamines are found in the internal organs and roe of the fish and shellfish. Therefore, personal food preferences and regional dietary patterns affect polyamine intake from food and influence polyamine levels in the body.
Because polyamine homeostasis maintains individual polyamine concentrations, short-term increases in polyamine supply do not change them [52,56,93,98,99]. Schwarz et al. showed that 28 days of augmentation of spermidine supplementation in mice resulted in no change in blood polyamines in mice [99]. Brodal et al. also reported similar results. For 20 days of feeding with experimental chow with different polyamine concentrations, the levels of putrescine, spermine, and spermidine in rat blood remained remarkably constant irrespective of chow [98]. In our animal experiments using mice, chow containing synthetic polyamine of which concentrations are about 3 times higher than those of soybean failed to increase blood spermine and spermidine concentrations for at least 16 weeks [52,93]. Eisenberg et al. postulated that increased spermidine intake supply spermidine to tissues and organs and spermidine provokes biological activities. They showed using few mice that spermidine ingestion increases blood spermidine levels with large individual differences for 16 weeks, but they did not show a study of a large enough number of mice to be able to rule out the effect of large individual differences in blood spermidine levels [100]. We confirmed that spermine (but not spermidine) concentrations in whole blood of mice fed high-polyamine chow for 26 weeks increased significantly, after repeated attempts with more mice. Spermidine concentrations increased in some animals, however, there were no significant changes [53].
Similar findings were observed in human interventional studies. Schwarz et al. showed that a human trial of 3-months of increased oral spermidine supplementation did not change blood spermidine levels at all [99]. A few intervention studies reported the favorable effects of increased spermidine intake on human memory function, however, they did not present individual data concerning the effect of increased spermidine intake on blood polyamine concentrations or a relationship between spermidine intake and changes in blood spermidine levels [101]. As they seemed to finish a large scale of intervention study [102], I am looking forward to the results of how spermidine consumption affected polyamine levels in humans. In our latest study, in which volunteers were asked to eat fermented soybeans containing high levels of polyamines, blood spermine levels gradually rose very slowly. During the first 8 months of the study, spermine levels slightly elevated in the high-polyamine diet group, however, there was no difference between the control group and the high-polyamine diet group. After 12 months of intervention, the blood spermine level in the high-polyamine group increased with a significant difference [56]. The lack of changes in blood polyamine concentration upon an increase in polyamine intake for a short period indicates that the intracellular polyamine concentration is strictly maintained by polyamine homeostasis. In addition, the findings that the concentration of spermine in blood cells increases only when polyamine intake is increased over a long period indicate that the presence of a long-lasting polyamine supply from the digestive tract can affect polyamine homeostasis and alter intracellular spermine concentrations. However, up to the present, it is unlikely that spermidine supplementation affects spermidine levels in the organs, tissues, or blood in animals and humans because of the lack of data from studies with sufficient populations for analysis.
In both our animal experiments and human interventional studies, increased polyamine intake increased blood spermine levels, while spermidine levels did not change, despite both animals and humans taking more spermidine than spermine [53,56]. Several studies indicate the importance of the composition of the intestinal microbiota for synthesis of intestinal polyamines [103]. Matsumoto et al. reported that probiotics administration increased spermine, but not spermidine, concentrations in feces in humans and animals, although probiotics and intestinal microbiota by themselves cannot synthesize spermine [104,105]. Considering these scientific facts, we can consider that the long-term and continuous increase in polyamine (spermidine > spermine) intake increases the supply of spermine, but not of spermidine, from the digestive tract. The role of intestinal environment and microbiota, especially in the composition of the intestinal microbiota, in polyamine synthesis in the intestinal lumen should be further examined.
In our intervention study using a high-polyamine diet, we found that the relationship between increases in polyamine intake and those in blood spermine levels seems not to be simply additive. The continuous intake of the high-polyamine diet increased blood spermine concentration of the subjects, but the increase in polyamine intake was not necessarily reflected in the increase in blood concentration [52,53,56]. The difference in the increase in blood polyamines in response to increased polyamine intake and wide inter-individual differences in blood polyamine concentration reflect differences in the intestinal environment.
5. Polyamine Localization in the Body
Polyamines have a binding capacity to DNA, RNA, and various protein molecules, and are implicated in diverse cellular functions such as transcription, RNA modification, protein synthesis, and modulation of enzyme activities. It has been estimated that a high percentage of total polyamines is bound by ionic interactions to nucleic acids, proteins, and other negatively charged molecules in the cell, while the free intracellular concentration of each polyamine is much lower (7–15% of total for spermidine and 2–5% for spermine in tissues and organs) [106,107]. Therefore, most polyamines in circulating blood are present in blood cells. Copper et al. showed that spermidine and spermine concentrations in plasma account for only 1.0% (spermine) to 1.2% (spermidine) of whole blood [108]. When we measure serum or plasma polyamine concentration by HPLC, it is sometimes hard to detect the peak of spermine due to the low levels [109]. When the concentration of spermine is low, HPLC can only depict the peak of spermine as a shaking of the baseline. We consider that it is difficult to determine accurate polyamine concentrations using such unclear peak. It is also important to note that even if a small amount of hemolysis occurs in the blood sample, the polyamines present in the cells leak out and have a significant effect on the polyamine concentration. The reason for measuring whole blood polyamine levels is to accurately measure all the polyamines present or attached to blood cells.
Blood cells circulate in organs and tissues throughout the body. Polyamine concentrations are increased in cancer tissues due to active polyamine synthesis, and blood polyamine concentrations are increased in cancer patients. These indicate that blood polyamine levels reflect polyamine concentrations in some organs and tissues in the body. Conversely, polyamines in blood cells can be passed to cells in tissues and organs, affecting their concentration. The brain is a typical example of an organ where polyamines in the blood cannot be transferred. Polyamines are highly water-soluble and polar compounds and thus their passage across the intact blood–brain barrier (BBB) is poor [110,111]. Polyamines have been noxious to the BBB by several investigators in different pathological states of the brain, including cerebral ischemia [112,113,114,115]. In animal models, there have been reports of the collapse of the BBB, allowing polyamines to enter brain tissue. However, such disruption occurs only in critical situations such as following traumatic brain injury [116] and ischemic injury [117]. Similarly, BBB dysfunction is reported in 14 patients following traumatic brain injury [118]. Several studies have reported that polyamine aggravate structural defects and even lead to membrane and vascular dysfunction after several different pathological conditions [113,119]. Considering these reports, the BBB protects the brain from being damaged by polyamines entering the brain tissue in otherwise normal conditions, and disruption of the BBB indicates that vascular function and the brain tissue is affected by some serious pathology.
6. Biological Activities of Polyamines
The biological activities of putrescine differ from those of polyamines, spermine and spermidine. For example, whereas spermine and spermidine have strong anti-inflammatory activities and are absorbed quickly from the intestinal lumen [120,121], putrescine has little to no anti-inflammatory effect and is degraded in the intestinal lumen [121,122]. Both spermidine and spermine have superficially similar biological activities, however, experiments have shown that spermine has greater potency. In cells with normal homeostasis, the influx of polyamines from the extracellular space suppresses ODC activity. Yuan Q et al. showed that putrescine, spermidine, and spermine inhibited ODC activity stimulated by serum to 85, 46, and 0% of control, indicating spermine is the most, and putrescine the least, effective polyamine in regulating ODC activity [123]. The difference in the strength of the suppression of one of the polyamine synthetic enzymes, e.g., ODC, between spermine and spermidine is reflected in the difference in their ability to regulate DNA methylation and the resultant change in the amount of lymphocyte function-associated antigen 1 (LFA-1), a protein involved in immune function that we have noted. In in vitro studies, we and others found that increasing the spermine concentration to about 1.2 times the level that occurs in vivo resulted in significant biological activity [49,123]. However, intracellular concentrations of spermidine had to increase two- to three-fold in human mononuclear blood cells to elicit obvious biological activities, i.e., the suppression of LFA-1 expression, the production of proinflammatory cytokines, and autophagy induction [49,87,121]. A two- to three-fold change in spermidine concentration is rare, except for a few cases in cancer patients. The difference in activity between spermidine and spermine is also observed in the relationship between blood concentration and LFA-1 levels, one of the bioactive targets of polyamine. When the relationship between polyamine concentration and LFA-1 level was examined in healthy volunteers, blood spermine concentration was inversely correlated with LFA-1 expression, while blood spermidine concentration was not [49,56]. Similarly, Saiki et al. reported that spermine is three to four times more capable of inducing autophagy than spermidine, and that the activity of spermine can be confirmed at concentrations in the physiological range [87].
Polyamines have many biological activities that may counteract the pathogenesis of aging-associated pathologies. For instance, they exert anti-inflammatory [49,121,124,125,126,127,128] and antioxidant properties [129,130,131,132,133,134,135,136,137,138]; protect cells and genes from harmful stimuli such as radiation [139,140,141,142,143,144,145,146,147], ultraviolet rays [148,149,150], toxic chemicals [128,151,152,153,154], and other stresses [148,155,156,157]; and they promote autophagy [128,158,159]. Very interestingly, polyphenols and antioxidant vitamins, which are abundant in legumes such as soybeans and in the Mediterranean diet, also have the same bioactivity as polyamines. For example, they have anti-inflammatory and antioxidant properties [17,19,20,21,22], and they protect cells and genes from harmful stimuli [18,23] and activate autophagy [17,25,26,28,29,30,31]. These biological activities were considered to inhibit the development of age-related pathologies. However, despite the large number of research conducted with antioxidants, the majority failed to show any effects on the prevention of aging-associated pathologies and the extension of lifespan of mammals [27,34,35,36,37,39,40] (Figure 2).
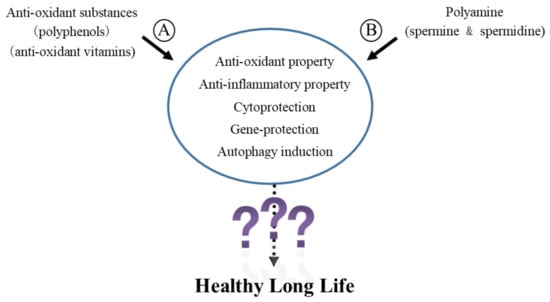
Figure 2.
Biological activities of polyamine and polyphenols. Both polyamines (spermidine and spermine) and antioxidants such as polyphenols and antioxidant vitamins have anti-inflammatory properties, antioxidant properties, and protect cells and genes from harmful stimuli and activate autophagy. Despite the vast amount of research on antioxidants, most of the studies have failed to show any benefit in preventing age-related conditions or extending lifespan. Therefore, the biological activities described in the figure are not enough to achieve life span extension and inhibition of the progression of senescence, especially of mammals, even if the mechanism and/or the pathway by which polyamines and polyphenols elicit these biological activities are different. References for A circled: [17,18,19,20,21,22,23,25,26,28,29,30,31], References for B circled: [49,121,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159], References for “?”: [22,25,26,27,28,30,31].
Recently, a research group has highlighted the importance of autophagy-mediated bioactivity by spermidine on life span extension [77]. Autophagy is a natural regulatory mechanism within the cells to remove degenerated or dysfunctional components from the cell. If autophagy function is inhibited, these unwanted components accumulate in cells, inhibit cellular homeostasis, and provoke various pathological changes [160]. Animal experiments using organ-specific conditional autophagy-deficient mice have revealed a close relationship between decreased autophagy and aging-associated pathologies [161,162].
Given that the increases in the incidence of aging-associated diseases with aging, we can speculate that autophagy activity decreases with aging [163]. In addition, decreased autophagy with aging has been reported in various studies [161,164,165,166]. However, other investigators have demonstrated that autophagy does not necessarily decline with age [167,168]. Yamamoto et al. even demonstrated substantial upregulation of autophagy in the aged kidney, suggesting compensatory activation of basal autophagy in response to the increased number of unwanted components with aging-associated accumulation [169].
Experiments using several primitive organisms confirm that inactivation of an autophagy gene suppressed the lifespan extension of long-lived mutant worms and slightly shortened the lifespan of wild-type worms [170,171,172,173,174,175,176]. However, the relationship between autophagy and longevity is not straightforward. Other investigators have shown that the inhibition of autophagy genes in several organisms does not always reduce normal lifespan [163,175,177]. Hashimoto et al. have systematically examined the effect of suppression of 14 autophagy genes on life span using RNAi. They reported that the suppression of autophagy genes can extend, but not shorten, the lifespan of Caenorhabditis elegans. These results indicate that autophagy activation is not necessarily beneficial for longevity and functions to shorten, or at least not extend, lifespan in several nematodes and flies [178]. Additionally, it has also been suggested that physiological levels of autophagy promote survival, while inadequate or excessive levels of autophagy promote death [179]. Because there is little scientific evidence indicating that autophagy activation helps extend the life span of mammals and aging is a complex process in highly developed mammals, the simple relationship between autophagy and aging observed in certain primitive organisms with short life spans is not straightforward in mammals, especially humans.
From these scientific facts, the biological activities described above are not enough to achieve the life span extension and inhibit the progression of senescence in mammals, especially humans, even if the mechanism and/or the pathway by which polyamines and polyphenols elicit these biological activities are different (Figure 2).
7. Aging, Proinflammatory Status, and DNA Methylation
Mammals are composed of countless numbers of cells and are made up of a complex interplay of various tissues and organs (nervous system, endocrine function, respiratory system, digestive system, immune functions, etc.). In humans, aging is associated with increased susceptibility to numerous different kinds of pathological conditions such as anemia, decreased kidney function, physical function impairment, sarcopenia, metabolic syndrome, diabetes, impaired cognitive function, neurodegenerative diseases, cardiovascular diseases, and cancer. Therefore, the type of disease they suffer from, the organ where pathology develops, and the progression of the disease affect their lifespan.
When considering that aging is associated with an increased incidence of these various diseases, the changes in the body environment that develop with aging play an important role in triggering these various diseases. Among changes, the increased pro-inflammatory status is considered a typical change associated with aging and triggering aging-associated diseases because inflammation and the resulting increase in oxidative stress have been shown to be involved in many aging-associated diseases [180]. Chronic, low-level elevation of proinflammatory cytokines and chemokines, and the resulting increases in inflammatory biomarkers, are associated with age-related declines in function and increased risks of morbidity and mortality [181]. Although the biological background of aging-associated increase in pro-inflammatory status is not fully clarified, one of the typical changes associated with aging responsible for increased pro-inflammatory status is the aging-associated increase in LFA-1 expression in immune cells. [182,183,184,185].
LFA-1 is an important protein involved in the induction of inflammation. The immune cells are activated when they recognize substances to be eliminated, and inflammation is generally the result of immune cell activation to eliminate harmful pathogens. The first step in this process is the binding of LFA-1 on immune cell membranes to intercellular adhesion molecules on endothelial cells lining the innermost layer of blood vessels. The increase in persistent inflammation associated with aging is likely the result of continuously weak stimulation by originally non-stimulatory degraded cells and substances and the increased response of aged immune cells with increased LFA-1 expression [186]. The activation of immune cells results in the production of proinflammatory cytokines, and aging is accompanied by progressive increases in the blood levels of proinflammatory mediators, including tumor necrosis factor α, interleukin-1, and interleukin-6 [187,188,189,190]. All three of these cytokines inhibit erythropoiesis [191], accelerate muscle wasting [192], induce insulin resistance [193], promote vascular dysfunction [194], and the resulting chronic inflammation provoked by cytokine production has also been linked to neurodegenerative diseases such as Alzheimer’s disease [195] and carcinogenesis [196].
The amount of LFA-1 protein on immune cells’ membrane is regulated by two main mechanisms. One is the intracellular signaling pathways, which result in rapid redistribution of LFA-1 to the cell membrane, regulating LFA-1 levels [197]. Apart from that, the alteration of DNA methylation status of the responsible part of LFA-1 expression, called ITGAL, also regulate LFA-1 expression. DNA methylation is a mechanism to regulate gene expression by modulating methylation in genomic regions that are either distal or proximal to the transcription start site of a gene. It has been reported that increases in LFA-1 protein levels in immune cells with aging are associated with enhanced demethylation of the ITGAL (LFA-1 promoter area) and increased LFA-1 protein levels [49,56,198,199].
A growing number of recent studies have shown a close relationship between aging and DNA methylation [198,200,201]. Aging is associated with enhanced demethylation of DNA in various organs and tissues in several animals and humans [202,203,204]. However, increased methylation (hypermethylation) associated with age has also been reported in other genes [205,206]. The condition in which demethylation and hypermethylation are present in various parts of the entire gene is called the aberrant DNA methylation. The progression of aberrant DNA methylation changes are key regulators of the aging process and contributors to the development of aging-associated diseases [207,208,209,210,211,212,213], including neoplastic growth [214,215,216,217,218] and senescence [219,220,221,222].
DNA methylation is susceptible to various lifestyle and living environments, such as environmental air pollution [223,224,225,226,227], smoking [218,228,229,230,231,232], and excessive alcohol consumption [233,234,235,236]. It has been reported that the changes observed on DNA methylation induced by these environmental factors with negative health effects have similarities to those associated with aging-associated diseases, such as malignant transformation [218,232,237], CVDs [231,238], and the acceleration of senescence [229,230,239]. Contrarily, lifestyle habits considered having favorable consequences for health, such as exercise [240,241,242,243] and dietary restriction for obesity [244], also alter DNA methylation status, which is the opposite of the changes observed during aging.
8. Polyamine, DNA Methylation, and LFA-1
Age-related genome-wide aberrant DNA methylation status [222,245], enhanced demethylation of the LFA-1 promoter area [199], and increases in LFA-1 protein levels [49,56,185,198] are accompanied by decreases in ODC [70,246,247] and DNA methyltransferases (DNMTs) activities [248,249,250,251]. There is a close relationship between ODC, a rate-limiting enzyme for polyamine synthesis, and DNMTs involved in DNA methylation. Ornithine and SAM are two crucial substrates for polyamine synthesis. Ornithine is converted to putrescine by ODC, and SAM is converted to dcSAM by AdoMetDC. Putrescine receives the aminopropyl group from dcSAM and is sequentially synthesized into spermidine and spermine. DNA methylation is the conversion of cytosine residues to 5-methylcytosine by the addition of the methyl group to a cytosine residue at the C-5 position. DNMTs regulate methylation of DNA in the presence of SAM, while dcSAM is a strong inhibitor of DNMTs [252]. The activity of DNMT is closely associated with the concentration of SAM [253] and dcSAM [254,255], and with the dcSAM to SAM ratio [252,255] (Figure 3).
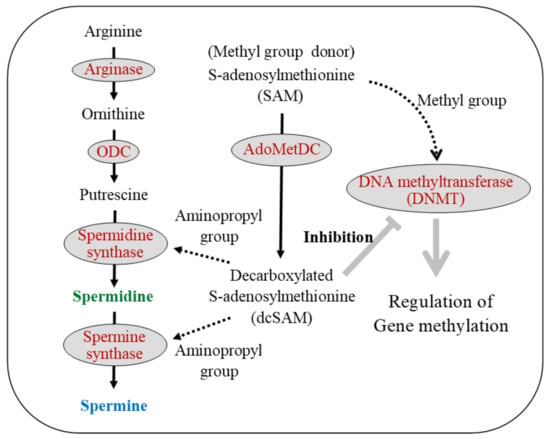
Figure 3.
Polyamine metabolism and gene methylation. The relationship between polyamine metabolism (left side) and gene methylation (right side) is indicated. S-adenosylmethionine (SAM), an amino acid, is a substrate for polyamine synthesis and a donor of methyl groups. During polyamine synthesis, spermidine and spermine synthase require an aminopropyl group from decarboxylated s-adenosylmethionine (dcSAM), which is converted from SAM by the enzymatic action of adenosylmethionine decarboxylase (AdoMetDC). DNA methyltransferases (DNMTs) regulate gene methylation status by receiving a supply of the methyl group from SAM. SAM is essential as a source of methyl groups in gene methylation reactions, and dcSAM is a strong inhibitor of DNMTs. Black text indicates the substance name, while spermidine and spermine are shown in green and blue, respectively. Red letters indicate enzyme names. The solid black arrows indicate the metabolic pathway, and the dashed black arrows indicate the transfer of some material from the upstream material. The thick gray arrow indicates activity on the target, and thick gray T-bar indicates the inhibitory activity on target. ODC: Ornithine decarboxylase; SAM: S-adenosylmethionine; AdoMetDC: Adenosylmethionine decarboxylase; dcSAM: Decarboxylated S-adenosylmethionine; DNMT: DNA methyltransferase.
Intracellular concentrations of dcSAM rise in cells when the addition of aminopropyl groups for polyamine synthesis is no longer necessary. This condition is observed when ODC activity is decreased due to the overexpression of antizyme that degrade ODC or treatment with α-D,L-difluoromethylornithine hydrochloride (DFMO), which inhibits ODC activity [252,255,256,257]. An increase in dcSAM induced by inhibition of ODC activity decreases DNMT activity [254,255,258]. We also showed that ODC inhibition by DFMO increased dcSAM concentrations and the dcSAM/SAM ratio and decreased activities of DNMT 1, 3a, and 3b in Jurkat cells [55]. We initially speculated that decreased DNMT activity and decreased donation of methyl groups to cytosine residues would lead to progressive demethylation of the entire genome, but in fact, aberrant methylation of the entire genome was promoted. The decline in DNMT activity induced by the inhibition of polyamine synthesis both increased demethylation in certain areas and increased hypermethylation in other areas, resulting in genome-wide aberrant methylation status [53,259,260,261,262,263]. Simultaneously, polyamine-deprivation enhanced demethylation of ITGAL region and increased LFA-1 protein levels [54]. The changes in methylation status in the ITGAL region were similar to those observed in the entire genome, i.e., aberrant methylation. In other words, some sites in ITGAL were demethylated, some were hypermethylated, and sites important for LFA-1 expression in immune cells were demethylated upon polyamine deprivation, increasing LFA-1 protein levels. The increase in LFA-1 expression associated with aging has been reported in animals and humans [53,182,183,184,185]. In addition, the age-dependent increase in the LFA-1 expression is associated with the age-dependent methylation changes in ITGAL region [53,198,264].
As we have shown in our animal experiments and human intervention studies, increased polyamine intake (spermidine content is much higher than spermine content) elevates blood spermine levels [52,53,56,93]. Many reports have shown that the biological activities of spermine are much stronger than those of spermidine [49,87,98,123]. Therefore, spermine was employed to study its effects on enzyme activities and substance concentrations involved in polyamine synthesis and DNA methylation. In cells with or without suppressed ODC activity by DFMO, spermine supplementation inhibited AdoMetDC activity and decreased dcSAM concentrations with a decreased dcSAM/SAM ratio. Decreasing dcSAM concentration or decreasing dcSAM/SAM ratio by spermine supplementation weakened the inhibitory effect of dcSAM on DNMT3a and 3b and activated these two enzymes (Figure 4), but did not reactivate DNMT1, which was inhibited by polyamine deprivation by DFMO [55]. Similarly, it has been reported that the presence or absence of methyl donors affects the expression of DNMT3a and 3b by other researchers [253]. DNMT3a and 3b are involved in de novo methylation and DNMT1 is involved in the maintenance of gene methylation status. Spermine supplementation reversed the changes in methylation status, i.e., a reversal of increased demethylation, in ITGAL induced by polyamine deprivation, resulting in decreased LFA-1 protein levels [54] (Figure 4).
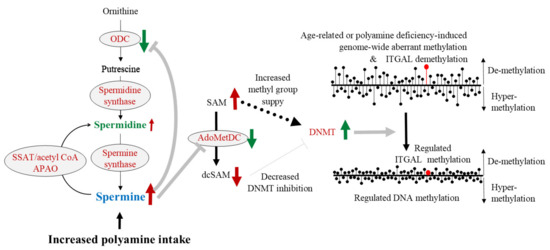
Figure 4.
The effects of increased polyamine intake on enzyme activities and substance levels related to polyamine metabolism and gene methylation. Increased polyamine intake elevates blood spermine levels and inhibits ODC activity. Increased spermine concentration strongly suppresses AdoMetDC activity, resulting in an increased amount of SAM and reduced amount of dcSAM. Since SAM is a methyl group donor for DNA methylation and dcSAM inhibits the activity of DNMTs, DNMTs are activated. As a result, enhanced aberrant methylation of entire genome and increased demethylation of ITGAL are reversed and regulated. Black text indicates the substance name, while spermidine and spermine are shown in green and blue, respectively. Red letters indicate enzyme names. The solid black arrows indicate the metabolic pathway, and the dashed black arrows indicate the transfer of the methyl group from SAM. The brown arrows indicate the conditions of enzymatic activities (upward and downward arrows). Upward arrows indicate activation of the enzyme, and downward arrows indicate the inhibition of enzyme activity. Green arrows indicate the change in material quantity and enzymatic activity. The thick gray arrows indicate the stimulus given to the target by the upstream enzyme activity, and the thick gray T-bars indicate the inhibitory activities on the target. The right figures show the condition and changes in DNA methylation status. The length of the line of black circles with bars indicates the progression of demethylation and hyper-methylation. The upward line indicates the progression of demethylation, and the downward lines indicate the progression of hyper-methylation. ODC: ornithine decarboxylase; SSAT: Spermidine/spermine N1-acetyltransferase; APAO: N1-acetylpolyamine oxidase; SAM: S-adenosylmethionine; AdoMetDC: Adenosylmethionine decarboxylase; dcSAM: Decarboxylated S-adenosylmethionine; DNMT: DNA methyltransferase; ITGAL: gene promoter area that is responsible for the LFA-1 expression.
Spermine can reverse the methylation status of ITGAL in several cells. However, spermine seems not to be able to reverse all the methylation changes associated with aging. In our earlier report, we noticed that the effects of spermine on LFA-1 expression are different from those of aging [49]. And, in our latest intervention study, we observed that the group of cells in which LFA-1 expression increases with age is different from the group of cells in which LFA-1 expression decreases by spermine supplementation, suggesting that the sites and cells in which spermine alters methylation status are different from those affected with aging [56]. Additionally, both abnormal genome-wide methylation and elevated LFA-1 protein levels observed in aged mice fed a normal chow were significantly suppressed, though not completely restored, in mice fed a high-polyamine diet [53]. Based on these results, spermine does not necessarily have effects on chronologically induced methylation changes. However, the regulation of DNA methylation by spermine may inhibit the onset and progression of various pathological changes and lifestyle-related diseases and consequently to slowing down the progression of senescence.
9. Possible Role of Polyamine in Cognitive Function
The role of polyamines in cancer progression is well known. Polyamine accelerates neoplastic growth and enhance metastatic spread [69]. However, it is controversial whether polyamines act as an initiator of carcinogenesis in normal cells that do not have existing carcinogenic elements (genetic abnormalities leading to carcinogenesis, exposure to preceding carcinogens and carcinogenic stimuli, etc.). There are several reports suggesting that increased polyamine intake does not increase carcinogenesis but has a suppressive effect on carcinogenesis in healthy individuals [53,265,266]. I have discussed the issues in my previous review [267].
In this section, I will discuss the possible role of polyamine in the inhibition of cognitive decline or the improvement of cognitive function. One of the major risk factors for poor health and shortened life expectancy among the elderly is the incidence and progression of diseases associated with cognitive decline and impaired cognitive function [268,269,270]. Individuals with cognitive impairment with or without definite neurodegenerative diseases have a higher mortality risk than healthy controls [270,271,272,273,274]. Therefore, it would make sense to investigate the possible role of increased polyamine intake, which extends the lifespan, in these aging-associated changes.
The possibility that spermidine is involved in memory function through a mechanism involving a novel memory-related molecule has been reported in insects such as Drosophila [275]. It cannot be completely ruled out the possibility of these mechanisms to function in the learning memory of higher animals such as mammals including humans. However, differences in basic biological background between insect memory and human memory are not known in detail, and the biological activities of spermidine in insects are not similar to its role in humans (described in Section 2. Polyamine). Additionally, because polyamines cannot cross the BBB under otherwise normal conditions, it is not expected that spermidine or spermine supplied from the intestinal lumen enters brain cells and exert their biological activities. Moreover, the role of autophagy activation in memory function and life span extension of mammals, especially humans, is not known (described in Section 6. Biological activities of polyamine). Therefore, I think it is difficult to believe that the effects on cognitive functions confirmed in some insects can be demonstrated in humans.
While polyamines cannot cross the BBB under normal conditions, reports have indicated that BBB dysfunction is associated with the pathogenesis of various neurodegenerative disorders such as Alzheimer’s disease [276,277], Parkinson’s disease [278,279], multiple sclerosis [280,281,282], and amyotrophic lateral sclerosis [283,284], in addition to typical cerebrovascular disorders such as stroke and vascular dementia [285,286]. However, it is incomprehensible how an increase in spermidine, which is so minuscule that it cannot elicit or enhance a physiological function, can exert any physiological activities. The effects of the stimulation of autophagy by the substances on cognitive function are also not clearly defined in humans. Moreover, even when the disruption of the BBB found in patients with cognitive impairment allows spermidine to enter brain tissue, patients with impaired cognitive function already have higher spermidine levels in the brain and blood than normal volunteers. Inoue et al. showed that patients with neurodegenerative diseases such as Alzheimer’s disease have increased spermidine levels in the frontal and parietal lobes of the brain [287]. Although polyamines cannot cross the BBB, their brain concentrations can be reflected in the blood via cerebrospinal fluid [288]. Sternberg et al. showed that serum levels of spermidine in patients with mild cognitive function are higher than those of healthy controls. Additionally, they reported that high spermidine level is associated with impaired cognitive function [89]. Similarly, the mean value of blood SPD levels in the Parkinson’s disease group was 134% higher than those of the controls [289]. Moreover, Graham et al. reported that spermidine plasma levels in patients with mild cognitive function who subsequently converted to Alzheimer’s disease were higher than those who did not [290]. Elevated spermidine levels in neurodegenerative diseases are consistent with reports of decreased spermine/spermidine ratios in patients with such diseases. Saiki et al. reported that spermine and the spermine/spermidine ratio is decreased in patients with Parkinson’s disease and Alzheimer’s disease [87].
There is evidence indicating a close relationship between chronic inflammation and neurodegenerative diseases [195,291,292,293]. Inflammation activates SSAT, an enzyme that breaks down spermine to spermidine and spermidine to putrescine, decreasing polyamine levels (Figure 1 and Figure 5). Increased polyamine degradation and decreased concentrations of spermine and spermidine activate polyamine recycling pathway, i.e., the activation of enzymes for polyamine synthesis. It is unclear how these metabolic changes affect polyamine concentrations, but it can be inferred by their effects on spermine and spermidine concentrations under different pathological conditions. In cancer tissues, inflammation and autonomous, but not stimulation-induced, increases in polyamine synthesis are observed. In cancer tissues, increases in spermidine concentrations are more prominent than spermine [65,67]. Similarly, in patients with neurodegenerative diseases, there are decreased spermine/spermidine ratios or increased spermidine concentrations [87,89,287,290]. These findings further support that inflammation-induced changes in polyamine metabolism are involved in the background of neurodegenerative diseases and cognitive decline. Our latest research also shows that the spermine/spermidine ratio in the blood of elderly people who can live independently is higher, i.e., increased spermidine concentrations relative to spermine, than that of older people who compelled to live in the elderly care facilities for assistance (manuscript is being prepared).
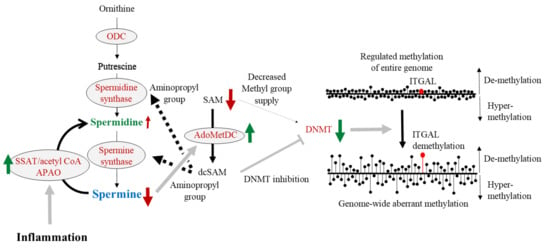
Figure 5.
The effects of chronic inflammation on enzyme activities and substance levels related to polyamine metabolism and gene methylation. Age-associated chronic inflammation activates SSAT. SSAT activation enhances spermine degradation and results in decreased spermine concentration. Polyamine synthesis is activated as a compensation for polyamine degradation, resulting in an activation of AdoMetDC. AdoMetDC consumes SAM for polyamine synthesis and results in a decreased supply of methyl groups for DNA methylation. The lack of a methyl group supply results in aberrant methylation of the entire genome and increased demethylation of ITGAL. Black text indicates the substance name, while spermidine and spermine are shown in green and blue, respectively. Red letters indicate enzyme names. The solid black arrows indicate the metabolic pathway, and the dashed black arrows indicate the transfer of the aminopropyl group from dcSAM. The brown arrows indicate the conditions of enzymatic activities (upward and downward arrows). Upward arrows indicate the activation of the enzyme, and downward arrows indicate the inhibition of enzyme activity. Green arrows indicate the change in enzymatic activity. The thick gray arrows indicate the stimulus given to the target by the upstream substance or enzyme activity, and the thick gray T-bars indicate the inhibitory activities on the target. The right figures show the condition and changes in DNA methylation status. The length of the line of black circles with bars indicates the progression of demethylation and hyper-methylation. The upward line indicates the progression of demethylation and the downward lines indicate the progression of hyper-methylation. ODC: ornithine decarboxylase; SSAT: Spermidine/spermine N1-acetyltransferase; APAO: N1-acetylpolyamine oxidase; SAM: S-adenosylmethionine; AdoMetDC: Adenosylmethionine decarboxylase; dcSAM: Decarboxylated S-adenosylmethionine; DNMT: DNA methyltransferase; ITGAL: gene promoter area that is responsible for the LFA-1 expression.
Due to the feedback mechanism, the activation of polyamine degradation by inflammation stimulates the enzymes of polyamine synthesis, and one of these enzymes, AdoMetDC, is also stimulated (Figure 5). Morrison LD et al. reported that autopsied brain of patients suffered Alzheimer’s disease showed an increase in the activity of AdoMetDC [294], also suggesting the involvement of chronic inflammation in the pathogenesis of the disease. AdoMetDC converts SAM to dSAM, and dSAM is used for polyamine synthesis. Thus, increased AdoMetDC activity decreases the SAM available for DNA methylation (Figure 5). Over the long term, this condition results in the progression of aberrant DNA methylation in the entire genome [295].
Continuously long-term increases in polyamine intake increased only spermine levels in the blood and suppressed aging-associated increases in proinflammatory conditions in humans and mice [53,56], i.e., suppression of LFA-1 protein levels on immune cells, and suppressed aging-associated enhancement of aberrant methylation of the entire genome and extended life span of mice [53]. These changes were associated with increases in blood spermine levels, and the degree of increase in the concentration of spermine was sufficient to make it biologically active in vivo. Increases in blood spermine levels are also sufficient to strongly suppress AdoMetDC activity, resulting in decreased dcSAM concentrations and increased SAM availability (Figure 4). The increase in SAM and the decrease in dcSAM that accompanies increases in spermine concentration activate DNA methyltransferase, which in turn regulates the DNA methylation status of the entire genome of brain tissue, tilting the LFA-1 promoter region toward hypermethylation and leading to a less pro-inflammatory state, i.e., reduced expression of LFA-1.
In both humans and rodents, the global changes in DNA methylation with normal aging are found in various tissues, including the brain [296,297,298,299]. Gene-specific DNA methylation changes are essential for memory formation, neurogenesis, and neuronal plasticity [300,301]. Unlike polyamines, which are difficult to pass through the BBB, SAM and dcSAM can pass through the BBB. It is reasonable to assume that changes in the concentration of substances related to DNA methylation and changes in enzyme activity caused by increased polyamine intake can help improve cognitive dysfunction via the regulation of methylation status and the suppression of proinflammatory condition. Very interestingly, the possible role of SAM supplementation in cognitive function and neuropsychiatric disorders has been discussed [302,303,304]. Our in vitro experiments showed that SAM supplementation reversed polyamine-deficient induced increase in LFA-1 expression, indicating a reversal of aberrant methylation status of the entire genome induced by polyamine deficiency [54]. Spermine supplementation not only reversed polyamine-deficient induced increase in LFA-1 but also further decreased LFA-1 expression, suggesting its potent effect on the regulation of DNA methylation [54].
10. Conclusions
We started our experiments to investigate the role of polyamines in extending the lifespan and health of mice, when we first discovered that spermine selectively suppresses LFA-1 expression in immune cells in 2005 [49]. After repeated experiments on mice, we confirmed the effect of increased polyamine intake on life span. After a long period of non-responsive and silent review of a submitted paper, we could publish for the first time the effect of increased polyamine intake on the lifespan of mice [52]. I hope this review will be helpful to scientists who are investigating the health and longevity of mammals, especially humans. I summarized the bioactivities and mechanisms of polyamines contributing to the extension of healthy life span (Figure 6).
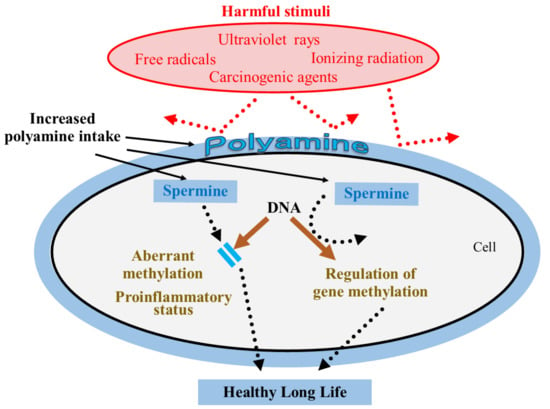
Figure 6.
Bioactivities and mechanism of polyamines contributing to healthy long life. The mechanism by which increased polyamine intake inhibits onset or progression of aging-associated diseases and senescence. Increased polyamine intake elevates blood spermine levels in humans, in spite the fact that many foods contain spermidine much more than spermine. Polyamine binds to the cell membrane, proteins, and genes by electric charge. Polyamine (spermine and spermidine) protects cells and genes from harmful stimuli indicated in red. Spermine inhibits aberrant DNA methylation and regulates DNA methylation status. These biological activities contribute to a healthy longevity.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The author declares no conflict of interest.
References
- Nagata, C.; Wada, K.; Tamura, T.; Konishi, K.; Goto, Y.; Koda, S.; Kawachi, T.; Tsuji, M.; Nakamura, K. Dietary soy and natto intake and cardiovascular disease mortality in Japanese adults: The Takayama study. Am. J. Clin. Nutr. 2017, 105, 426–431. [Google Scholar] [CrossRef] [Green Version]
- Erdman, J.W., Jr. AHA Science Advisory: Soy protein and cardiovascular disease: A statement for healthcare professionals from the Nutrition Committee of the AHA. Circulation 2000, 102, 2555–2559. [Google Scholar] [CrossRef] [Green Version]
- Trock, B.J.; Hilakivi-Clarke, L.; Clarke, R. Meta-analysis of soy intake and breast cancer risk. J. Natl. Cancer Inst. 2006, 98, 459–471. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.K.; Kim, J.H.; Nam, S.J.; Ryu, S.; Kong, G. Dietary intake of soy protein and tofu in association with breast cancer risk based on a case-control study. Nutr. Cancer 2008, 60, 568–576. [Google Scholar] [CrossRef]
- Wu, A.H.; Yu, M.C.; Tseng, C.C.; Pike, M.C. Epidemiology of soy exposures and breast cancer risk. Br. J. Cancer 2008, 98, 9–14. [Google Scholar] [CrossRef] [Green Version]
- Yan, L.; Spitznagel, E.L.; Bosland, M.C. Soy consumption and colorectal cancer risk in humans: A meta-analysis. Cancer Epidemiol. Biomark. Prev. 2010, 19, 148–158. [Google Scholar] [CrossRef] [Green Version]
- Yang, G.; Shu, X.O.; Li, H.; Chow, W.H.; Cai, H.; Zhang, X.; Gao, Y.T.; Zheng, W. Prospective cohort study of soy food intake and colorectal cancer risk in women. Am. J. Clin. Nutr. 2009, 89, 577–583. [Google Scholar] [CrossRef] [Green Version]
- Oba, S.; Nagata, C.; Shimizu, N.; Shimizu, H.; Kametani, M.; Takeyama, N.; Ohnuma, T.; Matsushita, S. Soy product consumption and the risk of colon cancer: A prospective study in Takayama, Japan. Nutr. Cancer 2007, 57, 151–157. [Google Scholar] [CrossRef]
- Spector, D.; Anthony, M.; Alexander, D.; Arab, L. Soy consumption and colorectal cancer. Nutr. Cancer 2003, 47, 1–12. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvado, J.; Covas, M.I.; Corella, D.; Aros, F.; Gomez-Gracia, E.; Ruiz-Gutierrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Kris-Etherton, P.; Eckel, R.H.; Howard, B.V.; St Jeor, S.; Bazzarre, T.L.; Nutrition Committee Population Science Committee; Clinical Science Committee of the American Heart Association. AHA Science Advisory: Lyon Diet Heart Study. Benefits of a Mediterranean-style, National Cholesterol Education Program/American Heart Association Step I Dietary Pattern on Cardiovascular Disease. Circulation 2001, 103, 1823–1825. [Google Scholar] [CrossRef] [Green Version]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [Green Version]
- Benetou, V.; Trichopoulou, A.; Orfanos, P.; Naska, A.; Lagiou, P.; Boffetta, P.; Trichopoulos, D. Conformity to traditional Mediterranean diet and cancer incidence: The Greek EPIC cohort. Br. J. Cancer 2008, 99, 191–195. [Google Scholar] [CrossRef] [Green Version]
- Couto, E.; Boffetta, P.; Lagiou, P.; Ferrari, P.; Buckland, G.; Overvad, K.; Dahm, C.C.; Tjonneland, A.; Olsen, A.; Clavel-Chapelon, F.; et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br. J. Cancer 2011, 104, 1493–1499. [Google Scholar] [CrossRef] [Green Version]
- Fung, T.T.; Hu, F.B.; McCullough, M.L.; Newby, P.K.; Willett, W.C.; Holmes, M.D. Diet quality is associated with the risk of estrogen receptor-negative breast cancer in postmenopausal women. J. Nutr. 2006, 136, 466–472. [Google Scholar] [CrossRef] [Green Version]
- Trichopoulou, A.; Bamia, C.; Lagiou, P.; Trichopoulos, D. Conformity to traditional Mediterranean diet and breast cancer risk in the Greek EPIC (European Prospective Investigation into Cancer and Nutrition) cohort. Am. J. Clin. Nutr. 2010, 92, 620–625. [Google Scholar] [CrossRef] [Green Version]
- Ferraresi, A.; Phadngam, S.; Morani, F.; Galetto, A.; Alabiso, O.; Chiorino, G.; Isidoro, C. Resveratrol inhibits IL-6-induced ovarian cancer cell migration through epigenetic up-regulation of autophagy. Mol. Carcinog. 2017, 56, 1164–1181. [Google Scholar] [CrossRef]
- George, V.C.; Dellaire, G.; Rupasinghe, H.P.V. Plant flavonoids in cancer chemoprevention: Role in genome stability. J. Nutr. Biochem. 2017, 45, 1–14. [Google Scholar] [CrossRef]
- Joseph, S.V.; Edirisinghe, I.; Burton-Freeman, B.M. Berries: Anti-inflammatory effects in humans. J. Agric. Food Chem. 2014, 62, 3886–3903. [Google Scholar] [CrossRef]
- Maleki, S.J.; Crespo, J.F.; Cabanillas, B. Anti-inflammatory effects of flavonoids. Food Chem. 2019, 299, 125124. [Google Scholar] [CrossRef]
- Wisnuwardani, R.W.; De Henauw, S.; Ferrari, M.; Forsner, M.; Gottrand, F.; Huybrechts, I.; Kafatos, A.G.; Kersting, M.; Knaze, V.; Manios, Y.; et al. Total Polyphenol Intake Is Inversely Associated with a Pro/Anti-Inflammatory Biomarker Ratio in European Adolescents of the HELENA Study. J. Nutr. 2020, 150, 1610–1618. [Google Scholar] [CrossRef]
- Elmaidomy, A.H.; Alhadrami, H.A.; Amin, E.; Aly, H.F.; Othman, A.M.; Rateb, M.E.; Hetta, M.H.; Abdelmohsen, U.R.; Hassan, M.H. Anti-Inflammatory and Antioxidant Activities of Terpene- and Polyphenol-Rich Premna odorata Leaves on Alcohol-Inflamed Female Wistar Albino Rat Liver. Molecules 2020, 25, 3116. [Google Scholar] [CrossRef]
- Guthrie, A.R.; Chow, H.S.; Martinez, J.A. Effects of resveratrol on drug- and carcinogen-metabolizing enzymes, implications for cancer prevention. Pharmacol. Res. Perspect. 2017, 5, e00294. [Google Scholar] [CrossRef]
- Jayasena, T.; Poljak, A.; Smythe, G.; Braidy, N.; Munch, G.; Sachdev, P. The role of polyphenols in the modulation of sirtuins and other pathways involved in Alzheimer’s disease. Ageing Res. Rev. 2013, 12, 867–883. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Y.; Zhang, T.; Chi, Y.; Liu, M.; Liu, Y. Genistein and Myd88 Activate Autophagy in High Glucose-Induced Renal Podocytes In Vitro. Med. Sci. Monit. 2018, 24, 4823–4831. [Google Scholar] [CrossRef]
- Zhang, B.; Yin, X.; Sui, S. Resveratrol inhibited the progression of human hepatocellular carcinoma by inducing autophagy via regulating p53 and the phosphoinositide 3kinase/protein kinase B pathway. Oncol. Rep. 2018, 40, 2758–2765. [Google Scholar]
- Sacks, F.M.; Lichtenstein, A.; Van Horn, L.; Harris, W.; Kris-Etherton, P.; Winston, M. Soy protein, isoflavones, and cardiovascular health: An American Heart Association Science Advisory for professionals from the Nutrition Committee. Circulation 2006, 113, 1034–1044. [Google Scholar] [CrossRef] [Green Version]
- Ding, S.; Jiang, J.; Yu, P.; Zhang, G.; Zhang, G.; Liu, X. Green tea polyphenol treatment attenuates atherosclerosis in high-fat diet-fed apolipoprotein E-knockout mice via alleviating dyslipidemia and up-regulating autophagy. PLoS ONE 2017, 12, e0181666. [Google Scholar] [CrossRef] [Green Version]
- Park, D.; Jeong, H.; Lee, M.N.; Koh, A.; Kwon, O.; Yang, Y.R.; Noh, J.; Suh, P.G.; Park, H.; Ryu, S.H. Resveratrol induces autophagy by directly inhibiting mTOR through ATP competition. Sci. Rep. 2016, 6, 21772. [Google Scholar] [CrossRef] [Green Version]
- Tang, L.; Yang, F.; Fang, Z.; Hu, C. Resveratrol Ameliorates Alcoholic Fatty Liver by Inducing Autophagy. Am. J. Chin. Med. 2016, 44, 1207–1220. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, J.; Xu, J.; Lu, Y.; Jiang, J.; Wang, L.; Shen, H.M.; Xia, D. Curcumin targets the TFEB-lysosome pathway for induction of autophagy. Oncotarget 2016, 7, 75659–75671. [Google Scholar] [CrossRef] [Green Version]
- Mancuso, R.; del Valle, J.; Modol, L.; Martinez, A.; Granado-Serrano, A.B.; Ramirez-Nunez, O.; Pallas, M.; Portero-Otin, M.; Osta, R.; Navarro, X. Resveratrol improves motoneuron function and extends survival in SOD1(G93A) ALS mice. Neurotherapeutics 2014, 11, 419–432. [Google Scholar]
- Baur, J.A.; Pearson, K.J.; Price, N.L.; Jamieson, H.A.; Lerin, C.; Kalra, A.; Prabhu, V.V.; Allard, J.S.; Lopez-Lluch, G.; Lewis, K.; et al. Resveratrol improves health and survival of mice on a high-calorie diet. Nature 2006, 444, 337–342. [Google Scholar] [CrossRef]
- Burnett, C.; Valentini, S.; Cabreiro, F.; Goss, M.; Somogyvari, M.; Piper, M.D.; Hoddinott, M.; Sutphin, G.L.; Leko, V.; McElwee, J.J.; et al. Absence of effects of Sir2 overexpression on lifespan in C. elegans and Drosophila. Nature 2011, 477, 482–485. [Google Scholar] [CrossRef] [Green Version]
- Johnson, A.A.; Riehle, M.A. Resveratrol Fails to Extend Life Span in the Mosquito Anopheles stephensi. Rejuvenation Res. 2015, 18, 473–478. [Google Scholar] [CrossRef]
- Kaeberlein, M.; McDonagh, T.; Heltweg, B.; Hixon, J.; Westman, E.A.; Caldwell, S.D.; Napper, A.; Curtis, R.; DiStefano, P.S.; Fields, S.; et al. Substrate-specific activation of sirtuins by resveratrol. J. Biol. Chem. 2005, 280, 17038–17045. [Google Scholar] [CrossRef] [Green Version]
- Miller, R.A.; Harrison, D.E.; Astle, C.M.; Baur, J.A.; Boyd, A.R.; de Cabo, R.; Fernandez, E.; Flurkey, K.; Javors, M.A.; Nelson, J.F.; et al. Rapamycin, but not resveratrol or simvastatin, extends life span of genetically heterogeneous mice. J. Gerontol. Biol. Sci. Med. Sci. 2011, 66, 191–201. [Google Scholar] [CrossRef]
- Pearson, K.J.; Baur, J.A.; Lewis, K.N.; Peshkin, L.; Price, N.L.; Labinskyy, N.; Swindell, W.R.; Kamara, D.; Minor, R.K.; Perez, E.; et al. Resveratrol delays age-related deterioration and mimics transcriptional aspects of dietary restriction without extending life span. Cell Metab. 2008, 8, 157–168. [Google Scholar] [CrossRef] [Green Version]
- Staats, S.; Wagner, A.E.; Kowalewski, B.; Rieck, F.T.; Soukup, S.T.; Kulling, S.E.; Rimbach, G. Dietary Resveratrol Does Not Affect Life Span, Body Composition, Stress Response, and Longevity-Related Gene Expression in Drosophila melanogaster. Int. J. Mol. Sci. 2018, 19, 223. [Google Scholar] [CrossRef] [Green Version]
- Strong, R.; Miller, R.A.; Astle, C.M.; Baur, J.A.; de Cabo, R.; Fernandez, E.; Guo, W.; Javors, M.; Kirkland, J.L.; Nelson, J.F.; et al. Evaluation of resveratrol, green tea extract, curcumin, oxaloacetic acid, and medium-chain triglyceride oil on life span of genetically heterogeneous mice. J. Gerontol. Biol. Sci. Med. Sci. 2013, 68, 6–16. [Google Scholar] [CrossRef] [Green Version]
- Cook, N.R.; Albert, C.M.; Gaziano, J.M.; Zaharris, E.; MacFadyen, J.; Danielson, E.; Buring, J.E.; Manson, J.E. A randomized factorial trial of vitamins C and E and beta carotene in the secondary prevention of cardiovascular events in women: Results from the Women’s Antioxidant Cardiovascular Study. Arch. Intern. Med. 2007, 167, 1610–1618. [Google Scholar] [CrossRef] [Green Version]
- Ernst, I.M.; Pallauf, K.; Bendall, J.K.; Paulsen, L.; Nikolai, S.; Huebbe, P.; Roeder, T.; Rimbach, G. Vitamin E supplementation and lifespan in model organisms. Ageing Res. Rev. 2013, 12, 365–375. [Google Scholar] [CrossRef]
- Hsieh, C.C.; Lin, B.F. Opposite effects of low and high dose supplementation of vitamin E on survival of MRL/lpr mice. Nutrition 2005, 21, 940–948. [Google Scholar] [CrossRef]
- Karim, M.R.; Fujimura, S.; Kadowaki, M. Vitamin E as a novel enhancer of macroautophagy in rat hepatocytes and H4-II-E cells. Biochem. Biophys. Res. Commun. 2010, 394, 981–987. [Google Scholar] [CrossRef]
- Miller, E.R., 3rd; Pastor-Barriuso, R.; Dalal, D.; Riemersma, R.A.; Appel, L.J.; Guallar, E. Meta-analysis: High-dosage vitamin E supplementation may increase all-cause mortality. Ann. Intern. Med. 2005, 142, 37–46. [Google Scholar] [CrossRef] [Green Version]
- Morley, A.A.; Trainor, K.J. Lack of an effect of vitamin E on lifespan of mice. Biogerontology 2001, 2, 109–112. [Google Scholar] [CrossRef]
- Selman, C.; McLaren, J.S.; Meyer, C.; Duncan, J.S.; Redman, P.; Collins, A.R.; Duthie, G.G.; Speakman, J.R. Life-long vitamin C supplementation in combination with cold exposure does not affect oxidative damage or lifespan in mice, but decreases expression of antioxidant protection genes. Mech. Ageing Dev. 2006, 127, 897–904. [Google Scholar] [CrossRef]
- Vivekananthan, D.P.; Penn, M.S.; Sapp, S.K.; Hsu, A.; Topol, E.J. Use of antioxidant vitamins for the prevention of cardiovascular disease: Meta-analysis of randomised trials. Lancet 2003, 361, 2017–2023. [Google Scholar] [CrossRef]
- Soda, K.; Kano, Y.; Nakamura, T.; Kasono, K.; Kawakami, M.; Konishi, F. Spermine, a natural polyamine, suppresses LFA-1 expression on human lymphocyte. J. Immunol. 2005, 175, 237–245. [Google Scholar] [CrossRef] [Green Version]
- Soda, K.; Kano, Y.; Chiba, F. Food polyamine and cardiovascular disease—An epidemiological study. Glob. J. Health Sci. 2012, 4, 170–178. [Google Scholar] [CrossRef]
- Binh, P.N.T.; Soda, K.; Kawakami, M. Mediterranean diet and polyamine intake: Possible contribution of increased polyamine intake to inhibition of age-associated disease. Nutr. Diet. Suppl. 2011, 3, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Soda, K.; Dobashi, Y.; Kano, Y.; Tsujinaka, S.; Konishi, F. Polyamine-rich food decreases age-associated pathology and mortality in aged mice. Exp. Gerontol. 2009, 44, 727–732. [Google Scholar] [CrossRef]
- Soda, K.; Kano, Y.; Chiba, F.; Koizumi, K.; Miyaki, Y. Increased polyamine intake inhibits age-associated alteration in global DNA methylation and 1,2-dimethylhydrazine-induced tumorigenesis. PLoS ONE 2013, 8, e64357. [Google Scholar] [CrossRef] [Green Version]
- Kano, Y.; Soda, K.; Konishi, F. Suppression of LFA-1 expression by spermine is associated with enhanced methylation of ITGAL, the LFA-1 promoter area. PLoS ONE 2013, 8, e56056. [Google Scholar]
- Fukui, T.; Soda, K.; Takao, K.; Rikiyama, T. Extracellular Spermine Activates DNA Methyltransferase 3A and 3B. Int. J. Mol. Sci. 2019, 20, 1254. [Google Scholar] [CrossRef] [Green Version]
- Soda, K.; Uemura, T.; Sanayama, H.; Igarashi, K.; Fukui, T. Polyamine-Rich Diet Elevates Blood Spermine Levels and Inhibits Pro-Inflammatory Status: An Interventional Study. Med. Sci. 2021, 9, 22. [Google Scholar] [CrossRef]
- Inouye, M.; Pardee, A.B. Requirement of polyamines for bacterial division. J. Bacteriol. 1970, 101, 770–776. [Google Scholar] [CrossRef] [Green Version]
- Miyamoto, S.; Kashiwagi, K.; Ito, K.; Watanabe, S.; Igarashi, K. Estimation of polyamine distribution and polyamine stimulation of protein synthesis in Escherichia coli. Arch. Biochem. Biophys. 1993, 300, 63–68. [Google Scholar] [CrossRef]
- Nickerson, K.W.; Dunkle, L.D.; Van Etten, J.L. Absence of spermine in filamentous fungi. J. Bacteriol. 1977, 129, 173–176. [Google Scholar] [CrossRef] [Green Version]
- Raina, A.; Jansen, M.; Cohen, S.S. Polyamines and the accumulation of ribonucleic acid in some polyauxotrophic strains of Escherichia coli. J. Bacteriol. 1967, 94, 1684–1696. [Google Scholar] [CrossRef] [Green Version]
- Wortham, B.W.; Patel, C.N.; Oliveira, M.A. Polyamines in bacteria: Pleiotropic effects yet specific mechanisms. Adv. Exp. Med. Biol. 2007, 603, 106–115. [Google Scholar]
- Hamasaki-Katagiri, N.; Katagiri, Y.; Tabor, C.W.; Tabor, H. Spermine is not essential for growth of Saccharomyces cerevisiae: Identification of the SPE4 gene (spermine synthase) and characterization of a spe4 deletion mutant. Gene 1998, 210, 195–201. [Google Scholar] [CrossRef]
- Gordon, R.; Cornect, M.; Walters, B.M.; Hall, D.E.; Brosnan, M.E. Polyamine Synthesis by the Mermithid Nematode Romanomermis culicivorax. J. Nematol. 1989, 21, 81–86. [Google Scholar]
- Pegg, A.E.; Michael, A.J. Spermine synthase. Cell. Mol. Life Sci. 2010, 67, 113–121. [Google Scholar] [CrossRef]
- Becciolini, A.; Porciani, S.; Lanini, A.; Balzi, M.; Cionini, L.; Bandettini, L. Polyamine levels in healthy and tumor tissues of patients with colon adenocarcinoma. Dis. Colon Rectum 1991, 34, 167–173. [Google Scholar] [CrossRef]
- Gallesio, C.; Colombatto, S.; Modica, R. Free and acetylated polyamines as markers of oral cavity tumors. Oral Surg. Oral Med. Oral Pathol. 1994, 77, 167–171. [Google Scholar] [CrossRef]
- Upp, J.R., Jr.; Saydjari, R.; Townsend, C.M., Jr.; Singh, P.; Barranco, S.C.; Thompson, J.C. Polyamine levels and gastrin receptors in colon cancers. Ann. Surg. 1988, 207, 662–669. [Google Scholar] [CrossRef]
- Loser, C.; Folsch, U.R.; Paprotny, C.; Creutzfeldt, W. Polyamines in colorectal cancer. Evaluation of polyamine concentrations in the colon tissue, serum, and urine of 50 patients with colorectal cancer. Cancer 1990, 65, 958–966. [Google Scholar] [CrossRef]
- Soda, K. The mechanisms by which polyamines accelerate tumor spread. J. Exp. Clin. Cancer Res. 2011, 30, 95. [Google Scholar] [CrossRef] [Green Version]
- Das, R.; Kanungo, M.S. Activity and modulation of ornithine decarboxylase and concentrations of polyamines in various tissues of rats as a function of age. Exp. Gerontol. 1982, 17, 95–103. [Google Scholar] [CrossRef]
- Ferioli, M.E.; Ceruti, G.; Comolli, R. Changes in rat liver ornithine decarboxylase activity during ageing and effect of stimulation by dexamethasone. Exp. Gerontol. 1976, 11, 153–156. [Google Scholar] [CrossRef]
- Yoshinaga, K.; Ishizuka, J.; Evers, B.M.; Townsend, C.M., Jr.; Thompson, J.C. Age-related changes in polyamine biosynthesis after fasting and refeeding. Exp. Gerontol. 1993, 28, 565–572. [Google Scholar] [CrossRef]
- Janne, J.; Raina, A. On the stimulation of ornithine decarboxylase and RNA polymerase activity in rat liver after treatment with growth hormone. Biochim. Biophys. Acta 1969, 174, 769–772. [Google Scholar] [CrossRef]
- Bedford, M.R.; Smith, T.K.; Summers, J.D. Effect of dietary ornithine on renal and hepatic polyamine synthesis. Ann. Nutr. Metab. 1988, 32, 265–270. [Google Scholar] [CrossRef]
- Schleiffer, R.; Duranton, B.; Gosse, F.; Hasselmann, M.; Raul, F. Blood polyamine levels after oral ornithine load, a diagnostic marker of hyperproliferative premalignant and malignant stages in a model of colon carcinogenesis. Cancer Detect. Prev. 2000, 24, 542–548. [Google Scholar]
- Teixeira, D.; Santaolaria, M.L.; Meneu, V.; Alonso, E. Dietary arginine slightly and variably affects tissue polyamine levels in male swiss albino mice. J. Nutr. 2002, 132, 3715–3720. [Google Scholar] [CrossRef] [Green Version]
- Madeo, F.; Bauer, M.A.; Carmona-Gutierrez, D.; Kroemer, G. Spermidine: A physiological autophagy inducer acting as an anti-aging vitamin in humans? Autophagy 2019, 15, 165–168. [Google Scholar] [CrossRef]
- Jaenne, J.; Raina, A.; Siimes, M. Spermidine and Spermine in Rat Tissues at Different Ages. Acta Physiol. Scand. 1964, 62, 352–358. [Google Scholar] [CrossRef]
- Nishimura, K.; Shiina, R.; Kashiwagi, K.; Igarashi, K. Decrease in polyamines with aging and their ingestion from food and drink. J. Biochem. 2006, 139, 81–90. [Google Scholar] [CrossRef]
- Morrison, L.D.; Becker, L.; Ang, L.C.; Kish, S.J. Polyamines in human brain: Regional distribution and influence of aging. J. Neurochem. 1995, 65, 636–642. [Google Scholar] [CrossRef]
- Dezortova, M.; Jiru, F.; Skoch, A.; Capek, V.; Ryznarova, Z.; Vik, V.; Hajek, M. The aging effect on prostate metabolite concentrations measured by (1)H MR spectroscopy. MAGMA 2017, 30, 65–74. [Google Scholar] [CrossRef]
- Rui, H.; Thomassen, Y.; Oldereid, N.B.; Purvis, K. Accessory sex gland function in normal young (20–25 years) and middle-aged (50–55 years) men. J. Androl. 1986, 7, 93–99. [Google Scholar] [CrossRef]
- Elworthy, P.; Hitchcock, E. Polyamine levels in red blood cells from patient groups of different sex and age. Biochim. Biophys. Acta 1989, 993, 212–216. [Google Scholar] [CrossRef]
- Chaisiri, P.; Harper, M.E.; Blamey, R.W.; Peeling, W.B.; Griffiths, K. Plasma spermidine concentrations in patients with tumours of the breast or prostate or testis. Clin. Chim. Acta 1980, 104, 367–375. [Google Scholar] [CrossRef]
- Van den Berg, G.A.; Muskiet, F.A.; Kingma, A.W.; van der Slik, W.; Halie, M.R. Simultaneous gas-chromatographic determination of free and acetyl-conjugated polyamines in urine. Clin. Chem. 1986, 32, 1930–1937. [Google Scholar] [CrossRef]
- Yodfat, Y.; Weiser, M.; Kreisel, M.; Bachrach, U. Diamine and polyamine levels in the urine of healthy adults. Clin. Chim. Acta 1988, 176, 107–113. [Google Scholar] [CrossRef]
- Saiki, S.; Sasazawa, Y.; Fujimaki, M.; Kamagata, K.; Kaga, N.; Taka, H.; Li, Y.; Souma, S.; Hatano, T.; Imamichi, Y.; et al. A metabolic profile of polyamines in parkinson disease: A promising biomarker. Ann. Neurol. 2019, 86, 251–263. [Google Scholar] [CrossRef] [Green Version]
- Pekar, T.; Wendzel, A.; Flak, W.; Kremer, A.; Pauschenwein-Frantsich, S.; Gschaider, A.; Wantke, F.; Jarisch, R. Spermidine in dementia : Relation to age and memory performance. Wien. Klin. Wochenschr. 2020, 132, 42–46. [Google Scholar] [CrossRef] [Green Version]
- Sternberg, Z.; Podolsky, R.; Nir, A.; Yu, J.; Nir, R.; Halvorsen, S.W.; Quinn, J.F.; Kaye, J.; Kolb, C. The Utility of Spermidine Serum Levels as a Biomarker of Alzheimer’s Disease a Pilot Study. Alzheimers Dis. Dement. 2021, 5, 119–125. [Google Scholar]
- Cipolla, B.; Guilli, F.; Moulinoux, J.P. Polyamine-reduced diet in metastatic hormone-refractory prostate cancer (HRPC) patients. Biochem. Soc. Trans. 2003, 31, 384–387. [Google Scholar] [CrossRef]
- Nishimura, K.; Araki, N.; Ohnishi, Y.; Kozaki, S. Effects of dietary polyamine deficiency on Trypanosoma gambiense infection in rats. Exp. Parasitol. 2001, 97, 95–101. [Google Scholar] [CrossRef]
- Sarhan, S.; Knodgen, B.; Seiler, N. The gastrointestinal tract as polyamine source for tumor growth. Anticancer Res. 1989, 9, 215–223. [Google Scholar]
- Soda, K.; Kano, Y.; Sakuragi, M.; Takao, K.; Lefor, A.; Konishi, F. Long-term oral polyamine intake increases blood polyamine concentrations. J. Nutr. Sci. Vitaminol. 2009, 55, 361–366. [Google Scholar] [CrossRef] [Green Version]
- Cipolla, B.G.; Havouis, R.; Moulinoux, J.P. Polyamine contents in current foods: A basis for polyamine reduced diet and a study of its long term observance and tolerance in prostate carcinoma patients. Amino Acids 2007, 33, 203–212. [Google Scholar] [CrossRef]
- Nishibori, N.; Fujihara, S.; Akatuki, T. Amounts of polyamines in foods in Japan and intake by Japanese. Food Chem. 2006, 100, 491–497. [Google Scholar] [CrossRef]
- Soda, K.; Mogi, S.; Shiina, M.; Kawabata, N. The Polyamine Content in Various Foods on a Calorie Basis. Jacobs J. Food Nutr. 2017, 4, 029. [Google Scholar]
- Watanabe, S.; Sato, S.; Nagase, S.; Shimosato, K.; Ohkuma, S. Effects of methotrexate and cyclophosphamide on polyamine levels in various tissues of rats. J. Drug Target. 1999, 7, 197–205. [Google Scholar] [CrossRef]
- Brodal, B.P.; Eliassen, K.A.; Ronning, H.; Osmundsen, H. Effects of dietary polyamines and clofibrate on metabolism of polyamines in the rat. J. Nutr. Biochem. 1999, 10, 700–708. [Google Scholar] [CrossRef]
- Schwarz, C.; Stekovic, S.; Wirth, M.; Benson, G.; Royer, P.; Sigrist, S.J.; Pieber, T.; Dammbrueck, C.; Magnes, C.; Eisenberg, T.; et al. Safety and tolerability of spermidine supplementation in mice and older adults with subjective cognitive decline. Aging Albany NY 2018, 10, 19–33. [Google Scholar] [CrossRef] [Green Version]
- Eisenberg, T.; Abdellatif, M.; Schroeder, S.; Primessnig, U.; Stekovic, S.; Pendl, T.; Harger, A.; Schipke, J.; Zimmermann, A.; Schmidt, A.; et al. Cardioprotection and lifespan extension by the natural polyamine spermidine. Nat. Med. 2016, 22, 1428–1438. [Google Scholar] [CrossRef]
- Wirth, M.; Benson, G.; Schwarz, C.; Kobe, T.; Grittner, U.; Schmitz, D.; Sigrist, S.J.; Bohlken, J.; Stekovic, S.; Madeo, F.; et al. The effect of spermidine on memory performance in older adults at risk for dementia: A randomized controlled trial. Cortex 2018, 109, 181–188. [Google Scholar] [CrossRef]
- Wirth, M.; Schwarz, C.; Benson, G.; Horn, N.; Buchert, R.; Lange, C.; Kobe, T.; Hetzer, S.; Maglione, M.; Michael, E.; et al. Effects of spermidine supplementation on cognition and biomarkers in older adults with subjective cognitive decline (SmartAge)-study protocol for a randomized controlled trial. Alzheimers Res. Ther. 2019, 11, 36. [Google Scholar] [CrossRef]
- Kibe, R.; Kurihara, S.; Sakai, Y.; Suzuki, H.; Ooga, T.; Sawaki, E.; Muramatsu, K.; Nakamura, A.; Yamashita, A.; Kitada, Y.; et al. Upregulation of colonic luminal polyamines produced by intestinal microbiota delays senescence in mice. Sci. Rep. 2014, 4, 4548. [Google Scholar] [CrossRef]
- Matsumoto, M.; Ohishi, H.; Benno, Y. Impact of LKM512 yogurt on improvement of intestinal environment of the elderly. FEMS Immunol. Med. Microbiol. 2001, 31, 181–186. [Google Scholar] [CrossRef]
- Matsumoto, M.; Kurihara, S.; Kibe, R.; Ashida, H.; Benno, Y. Longevity in mice is promoted by probiotic-induced suppression of colonic senescence dependent on upregulation of gut bacterial polyamine production. PLoS ONE 2011, 6, e23652. [Google Scholar] [CrossRef] [Green Version]
- Igarashi, K.; Kashiwagi, K. Polyamines: Mysterious modulators of cellular functions. Biochem. Biophys. Res. Commun. 2000, 271, 559–564. [Google Scholar] [CrossRef]
- Watanabe, S.; Kusama-Eguchi, K.; Kobayashi, H.; Igarashi, K. Estimation of polyamine binding to macromolecules and ATP in bovine lymphocytes and rat liver. J. Biol. Chem. 1991, 266, 20803–20809. [Google Scholar] [CrossRef]
- Cooper, K.D.; Shukla, J.B.; Rennert, O.M. Polyamine distribution in cellular compartments of blood and in aging erythrocytes. Clin. Chim. Acta 1976, 73, 71–88. [Google Scholar] [CrossRef]
- Matsumoto, M.; Kitada, Y.; Naito, Y. Endothelial Function is improved by Inducing Microbial Polyamine Production in the Gut: A Randomized Placebo-Controlled Trial. Nutrients 2019, 11, 1188. [Google Scholar] [CrossRef] [Green Version]
- Kremzner, L.T. Metabolism of polyamines in the nervous system. Fed. Proc. 1970, 29, 1583–1588. [Google Scholar]
- Shin, W.W.; Fong, W.F.; Pang, S.F.; Wong, P.C. Limited blood-brain barrier transport of polyamines. J. Neurochem. 1985, 44, 1056–1059. [Google Scholar] [CrossRef]
- Koenig, H.; Goldstone, A.D.; Lu, C.Y. Blood brain barrier breakdown in brain edema following cold injury is mediated by microvascular polyamines. Biochem. Biophys. Res. Commun. 1983, 116, 1039–1048. [Google Scholar] [CrossRef]
- Paschen, W. Polyamine metabolism in different pathological states of the brain. Mol. Chem. Neuropathol. 1992, 16, 241–271. [Google Scholar] [CrossRef]
- Schmitz, M.P.; Combs, D.J.; Dempsey, R.J. Difluoromethylornithine decreases postischemic brain edema and blood-brain barrier breakdown. Neurosurgery 1993, 33, 882–887; discussion 887–888. [Google Scholar]
- Sears, E.S.; McCandless, D.W.; Chandler, M.D. Disruption of the blood-brain barrier in hyperammonemic coma and the pharmacologic effects of dexamethasone and difluoromethyl ornithine. J. Neurosci. Res. 1985, 14, 255–261. [Google Scholar] [CrossRef]
- Trout, J.J.; Koenig, H.; Goldstone, A.D.; Lu, C.Y. Blood-brain barrier breakdown by cold injury. Polyamine signals mediate acute stimulation of endocytosis, vesicular transport, and microvillus formation in rat cerebral capillaries. Lab. Investig. 1986, 55, 622–631. [Google Scholar]
- Diler, A.S.; Ziylan, Y.Z.; Uzum, G.; Lefauconnier, J.M.; Seylaz, J.; Pinard, E. Passage of spermidine across the blood-brain barrier in short recirculation periods following global cerebral ischemia: Effects of mild hyperthermia. Neurosci. Res. 2002, 43, 335–342. [Google Scholar] [CrossRef]
- Winter, C.; Bell, C.; Whyte, T.; Cardinal, J.; Macfarlane, D.; Rose, S. Blood-brain barrier dysfunction following traumatic brain injury: Correlation of K(trans) (DCE-MRI) and SUVR (99mTc-DTPA SPECT) but not serum S100B. Neurol. Res. 2015, 37, 599–606. [Google Scholar] [CrossRef]
- Baskaya, M.K.; Rao, A.M.; Dogan, A.; Donaldson, D.; Gellin, G.; Dempsey, R.J. Regional brain polyamine levels in permanent focal cerebral ischemia. Brain Res. 1997, 744, 302–308. [Google Scholar] [CrossRef]
- Uda, K.; Tsujikawa, T.; Fujiyama, Y.; Bamba, T. Rapid absorption of luminal polyamines in a rat small intestine ex vivo model. J. Gastroenterol. Hepatol. 2003, 18, 554–559. [Google Scholar] [CrossRef]
- Zhang, M.; Caragine, T.; Wang, H.; Cohen, P.S.; Botchkina, G.; Soda, K.; Bianchi, M.; Ulrich, P.; Cerami, A.; Sherry, B.; et al. Spermine inhibits proinflammatory cytokine synthesis in human mononuclear cells: A counterregulatory mechanism that restrains the immune response. J. Exp. Med. 1997, 185, 1759–1768. [Google Scholar] [CrossRef] [Green Version]
- Bardocz, S.; Brown, D.S.; Grant, G.; Pusztai, A. Luminal and basolateral polyamine uptake by rat small intestine stimulated to grow by Phaseolus vulgaris lectin phytohaemagglutinin in vivo. Biochim. Biophys. Acta 1990, 1034, 46–52. [Google Scholar] [CrossRef]
- Yuan, Q.; Ray, R.M.; Viar, M.J.; Johnson, L.R. Polyamine regulation of ornithine decarboxylase and its antizyme in intestinal epithelial cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2001, 280, G130–G138. [Google Scholar] [CrossRef]
- Choi, Y.H.; Park, H.Y. Anti-inflammatory effects of spermidine in lipopolysaccharide-stimulated BV2 microglial cells. J. Biomed. Sci. 2012, 19, 31. [Google Scholar] [CrossRef] [Green Version]
- Lagishetty, C.V.; Naik, S.R. Polyamines: Potential anti-inflammatory agents and their possible mechanism of action. Indian J. Pharmacol. 2008, 40, 121–125. [Google Scholar]
- Lovaas, E.; Carlin, G. Spermine: An anti-oxidant and anti-inflammatory agent. Free Radic. Biol. Med. 1991, 11, 455–461. [Google Scholar] [CrossRef]
- Paul, S.; Kang, S.C. Natural polyamine inhibits mouse skin inflammation and macrophage activation. Inflamm. Res. 2013, 62, 681–688. [Google Scholar] [CrossRef]
- Zhou, S.; Gu, J.; Liu, R.; Wei, S.; Wang, Q.; Shen, H.; Dai, Y.; Zhou, H.; Zhang, F.; Lu, L. Spermine Alleviates Acute Liver Injury by Inhibiting Liver-Resident Macrophage Pro-Inflammatory Response through ATG5-Dependent Autophagy. Front. Immunol. 2018, 9, 948. [Google Scholar] [CrossRef]
- Belle, N.A.; Dalmolin, G.D.; Fonini, G.; Rubin, M.A.; Rocha, J.B. Polyamines reduces lipid peroxidation induced by different pro-oxidant agents. Brain Res. 2004, 1008, 245–251. [Google Scholar] [CrossRef]
- Chattopadhyay, M.K.; Tabor, C.W.; Tabor, H. Polyamines protect Escherichia coli cells from the toxic effect of oxygen. Proc. Natl. Acad. Sci. USA 2003, 100, 2261–2265. [Google Scholar] [CrossRef] [Green Version]
- Fujisawa, S.; Kadoma, Y. Kinetic evaluation of polyamines as radical scavengers. Anticancer Res. 2005, 25, 965–969. [Google Scholar]
- Gaboriau, F.; Vaultier, M.; Moulinoux, J.P.; Delcros, J.G. Antioxidative properties of natural polyamines and dimethylsilane analogues. Redox. Rep. 2005, 10, 9–18. [Google Scholar] [CrossRef]
- Jeong, J.W.; Cha, H.J.; Han, M.H.; Hwang, S.J.; Lee, D.S.; Yoo, J.S.; Choi, I.W.; Kim, S.; Kim, H.S.; Kim, G.Y.; et al. Spermidine Protects against Oxidative Stress in Inflammation Models Using Macrophages and Zebrafish. Biomol. Ther. 2018, 26, 146–156. [Google Scholar] [CrossRef] [Green Version]
- Jung, I.L.; Oh, T.J.; Kim, I.G. Abnormal growth of polyamine-deficient Escherichia coli mutant is partially caused by oxidative stress-induced damage. Arch. Biochem. Biophys. 2003, 418, 125–132. [Google Scholar] [CrossRef]
- Nayvelt, I.; Hyvonen, M.T.; Alhonen, L.; Pandya, I.; Thomas, T.; Khomutov, A.R.; Vepsalainen, J.; Patel, R.; Keinanen, T.A.; Thomas, T.J. DNA condensation by chiral alpha-methylated polyamine analogues and protection of cellular DNA from oxidative damage. Biomacromolecules 2010, 11, 97–105. [Google Scholar] [CrossRef]
- Rider, J.E.; Hacker, A.; Mackintosh, C.A.; Pegg, A.E.; Woster, P.M.; Casero, R.A., Jr. Spermine and spermidine mediate protection against oxidative damage caused by hydrogen peroxide. Amino Acids 2007, 33, 231–240. [Google Scholar] [CrossRef]
- Sava, I.G.; Battaglia, V.; Rossi, C.A.; Salvi, M.; Toninello, A. Free radical scavenging action of the natural polyamine spermine in rat liver mitochondria. Free Radic. Biol. Med. 2006, 41, 1272–1281. [Google Scholar] [CrossRef]
- von Deutsch, A.W.; Mitchell, C.D.; Williams, C.E.; Dutt, K.; Silvestrov, N.A.; Klement, B.J.; Abukhalaf, I.K.; von Deutsch, D.A. Polyamines protect against radiation-induced oxidative stress. Gravit. Space Biol. Bull. 2005, 18, 109–110. [Google Scholar]
- Arundel, C.M.; Nishioka, K.; Tofilon, P.J. Effects of alpha-difluoromethylornithine-induced polyamine depletion on the radiosensitivity of a human colon carcinoma cell line. Radiat. Res. 1988, 114, 634–640. [Google Scholar] [CrossRef]
- Chiu, S.; Oleinick, N.L. Radioprotection of cellular chromatin by the polyamines spermine and putrescine: Preferential action against formation of DNA-protein crosslinks. Radiat. Res. 1998, 149, 543–549. [Google Scholar] [CrossRef]
- Courdi, A.; Milano, G.; Bouclier, M.; Lalanne, C.M. Radiosensitization of human tumor cells by alpha-difluoromethylornithine. Int. J. Cancer 1986, 38, 103–107. [Google Scholar] [CrossRef]
- Douki, T.; Bretonniere, Y.; Cadet, J. Protection against radiation-induced degradation of DNA bases by polyamines. Radiat. Res. 2000, 153, 29–35. [Google Scholar] [CrossRef]
- Held, K.D.; Awad, S. Effects of polyamines and thiols on the radiation sensitivity of bacterial transforming DNA. Int. J. Radiat. Biol. 1991, 59, 699–710. [Google Scholar] [CrossRef]
- Newton, G.L.; Aguilera, J.A.; Ward, J.F.; Fahey, R.C. Polyamine-induced compaction and aggregation of DNA—A major factor in radioprotection of chromatin under physiological conditions. Radiat. Res. 1996, 145, 776–780. [Google Scholar] [CrossRef]
- Snyder, R.D.; Schroeder, K.K. Radiosensitivity of polyamine-depleted HeLa cells and modulation by the aminothiol WR-1065. Radiat. Res. 1994, 137, 67–75. [Google Scholar] [CrossRef]
- Sy, D.; Hugot, S.; Savoye, C.; Ruiz, S.; Charlier, M.; Spotheim-Maurizot, M. Radioprotection of DNA by spermine: A molecular modelling approach. Int. J. Radiat. Biol. 1999, 75, 953–961. [Google Scholar]
- Warters, R.L.; Newton, G.L.; Olive, P.L.; Fahey, R.C. Radioprotection of human cell nuclear DNA by polyamines: Radiosensitivity of chromatin is influenced by tightly bound spermine. Radiat. Res. 1999, 151, 354–362. [Google Scholar] [CrossRef]
- Pothipongsa, A.; Jantaro, S.; Incharoensakdi, A. Polyamines induced by osmotic stress protect Synechocystis sp. PCC 6803 cells and arginine decarboxylase transcripts against UV-B radiation. Appl. Biochem. Biotechnol. 2012, 168, 1476–1488. [Google Scholar] [CrossRef]
- Snyder, R.D.; Sunkara, P.S. Effect of polyamine depletion on DNA damage and repair following UV irradiation of HeLa cells. Photochem. Photobiol. 1990, 52, 525–532. [Google Scholar] [CrossRef]
- Williams, J.R.; Casero, R.A.; Dillehay, L.E. The effect of polyamine depletion on the cytotoxic response to PUVA, gamma rays and UVC in V79 cells in vitro. Biochem. Biophys. Res. Commun. 1994, 201, 1–7. [Google Scholar] [CrossRef]
- Chauhan, S.D.; Seggara, G.; Vo, P.A.; Macallister, R.J.; Hobbs, A.J.; Ahluwalia, A. Protection against lipopolysaccharide-induced endothelial dysfunction in resistance and conduit vasculature of iNOS knockout mice. FASEB J. 2003, 17, 773–775. [Google Scholar] [CrossRef]
- Di Mascio, P.; Teixeira, P.C.; Onuki, J.; Medeiros, M.H.; Dornemann, D.; Douki, T.; Cadet, J. DNA damage by 5-aminolevulinic and 4,5-dioxovaleric acids in the presence of ferritin. Arch. Biochem. Biophys. 2000, 373, 368–374. [Google Scholar] [CrossRef]
- Mackintosh, C.A.; Pegg, A.E. Effect of spermine synthase deficiency on polyamine biosynthesis and content in mice and embryonic fibroblasts, and the sensitivity of fibroblasts to 1,3-bis-(2-chloroethyl)-N-nitrosourea. Biochem. J. 2000, 351 Pt 2, 439–447. [Google Scholar] [CrossRef]
- Rajalakshmi, S.; Rao, P.M.; Sarma, D.S. Studies on carcinogen chromatin--DNA interaction: Inhibition of N-methyl-N-nitrosourea-induced methylation of chromatin—DNA by spermine and distamycin A. Biochemistry 1978, 17, 4515–4518. [Google Scholar] [CrossRef]
- Gugliucci, A.; Menini, T. The polyamines spermine and spermidine protect proteins from structural and functional damage by AGE precursors: A new role for old molecules? Life Sci. 2003, 72, 2603–2616. [Google Scholar] [CrossRef]
- Okumura, S.; Teratani, T.; Fujimoto, Y.; Zhao, X.; Tsuruyama, T.; Masano, Y.; Kasahara, N.; Iida, T.; Yagi, S.; Uemura, T.; et al. Oral administration of polyamines ameliorates liver ischemia/reperfusion injury and promotes liver regeneration in rats. Liver Transpl. 2016, 22, 1231–1244. [Google Scholar] [CrossRef] [Green Version]
- Sagor, G.H.; Berberich, T.; Takahashi, Y.; Niitsu, M.; Kusano, T. The polyamine spermine protects Arabidopsis from heat stress-induced damage by increasing expression of heat shock-related genes. Transgenic Res. 2013, 22, 595–605. [Google Scholar] [CrossRef]
- Sacitharan, P.K.; Lwin, S.; Gharios, G.B.; Edwards, J.R. Spermidine restores dysregulated autophagy and polyamine synthesis in aged and osteoarthritic chondrocytes via EP300. Exp. Mol. Med. 2018, 50, 123. [Google Scholar] [CrossRef] [Green Version]
- Chae, Y.B.; Kim, M.M. Activation of p53 by spermine mediates induction of autophagy in HT1080 cells. Int. J. Biol. Macromol. 2014, 63, 56–63. [Google Scholar] [CrossRef]
- Djajadikerta, A.; Keshri, S.; Pavel, M.; Prestil, R.; Ryan, L.; Rubinsztein, D.C. Autophagy Induction as a Therapeutic Strategy for Neurodegenerative Diseases. J. Mol. Biol. 2020, 432, 2799–2821. [Google Scholar] [CrossRef]
- Rubinsztein, D.C.; Marino, G.; Kroemer, G. Autophagy and aging. Cell 2011, 146, 682–695. [Google Scholar] [CrossRef] [Green Version]
- Takabatake, Y.; Kimura, T.; Takahashi, A.; Isaka, Y. Autophagy and the kidney: Health and disease. Nephrol. Dial. Transplant. 2014, 29, 1639–1647. [Google Scholar] [CrossRef] [Green Version]
- Cuervo, A.M. Autophagy and aging: Keeping that old broom working. Trends Genet. 2008, 24, 604–612. [Google Scholar] [CrossRef] [Green Version]
- Cui, J.; Bai, X.Y.; Shi, S.; Cui, S.; Hong, Q.; Cai, G.; Chen, X. Age-related changes in the function of autophagy in rat kidneys. Age 2012, 34, 329–339. [Google Scholar] [CrossRef] [Green Version]
- Del Roso, A.; Vittorini, S.; Cavallini, G.; Donati, A.; Gori, Z.; Masini, M.; Pollera, M.; Bergamini, E. Ageing-related changes in the in vivo function of rat liver macroautophagy and proteolysis. Exp. Gerontol. 2003, 38, 519–527. [Google Scholar] [CrossRef]
- Lipinski, M.M.; Zheng, B.; Lu, T.; Yan, Z.; Py, B.F.; Ng, A.; Xavier, R.J.; Li, C.; Yankner, B.A.; Scherzer, C.R.; et al. Genome-wide analysis reveals mechanisms modulating autophagy in normal brain aging and in Alzheimer’s disease. Proc. Natl. Acad. Sci. USA 2010, 107, 14164–14169. [Google Scholar] [CrossRef] [Green Version]
- Demirovic, D.; Nizard, C.; Rattan, S.I. Basal level of autophagy is increased in aging human skin fibroblasts in vitro, but not in old skin. PLoS ONE 2015, 10, e0126546. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.S.; Park, S.Y.; Moon, S.H.; Lee, J.D.; Kim, S. Autophagy in Human Skin Fibroblasts: Impact of Age. Int. J. Mol. Sci. 2018, 19, 2254. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, T.; Takabatake, Y.; Kimura, T.; Takahashi, A.; Namba, T.; Matsuda, J.; Minami, S.; Kaimori, J.Y.; Matsui, I.; Kitamura, H.; et al. Time-dependent dysregulation of autophagy: Implications in aging and mitochondrial homeostasis in the kidney proximal tubule. Autophagy 2016, 12, 801–813. [Google Scholar] [CrossRef] [Green Version]
- Melendez, A.; Talloczy, Z.; Seaman, M.; Eskelinen, E.L.; Hall, D.H.; Levine, B. Autophagy genes are essential for dauer development and life-span extension in C. elegans. Science 2003, 301, 1387–1391. [Google Scholar] [CrossRef] [Green Version]
- Apfeld, J.; Kenyon, C. Cell nonautonomy of C. elegans daf-2 function in the regulation of diapause and life span. Cell 1998, 95, 199–210. [Google Scholar] [CrossRef] [Green Version]
- Hars, E.S.; Qi, H.; Ryazanov, A.G.; Jin, S.; Cai, L.; Hu, C.; Liu, L.F. Autophagy regulates ageing in C. elegans. Autophagy 2007, 3, 93–95. [Google Scholar] [CrossRef] [Green Version]
- Toth, M.L.; Sigmond, T.; Borsos, E.; Barna, J.; Erdelyi, P.; Takacs-Vellai, K.; Orosz, L.; Kovacs, A.L.; Csikos, G.; Sass, M.; et al. Longevity pathways converge on autophagy genes to regulate life span in Caenorhabditis elegans. Autophagy 2008, 4, 330–338. [Google Scholar] [CrossRef] [Green Version]
- Tavernarakis, N.; Pasparaki, A.; Tasdemir, E.; Maiuri, M.C.; Kroemer, G. The effects of p53 on whole organism longevity are mediated by autophagy. Autophagy 2008, 4, 870–873. [Google Scholar] [CrossRef] [Green Version]
- Hansen, M.; Chandra, A.; Mitic, L.L.; Onken, B.; Driscoll, M.; Kenyon, C. A role for autophagy in the extension of lifespan by dietary restriction in C. elegans. PLoS Genet. 2008, 4, e24. [Google Scholar] [CrossRef] [Green Version]
- Jia, K.; Levine, B. Autophagy is required for dietary restriction-mediated life span extension in C. elegans. Autophagy 2007, 3, 597–599. [Google Scholar] [CrossRef] [Green Version]
- Ren, C.; Finkel, S.E.; Tower, J. Conditional inhibition of autophagy genes in adult Drosophila impairs immunity without compromising longevity. Exp. Gerontol. 2009, 44, 228–235. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, Y.; Ookuma, S.; Nishida, E. Lifespan extension by suppression of autophagy genes in Caenorhabditis elegans. Genes Cells 2009, 14, 717–726. [Google Scholar] [CrossRef]
- Kang, C.; You, Y.J.; Avery, L. Dual roles of autophagy in the survival of Caenorhabditis elegans during starvation. Genes Dev. 2007, 21, 2161–2171. [Google Scholar] [CrossRef] [Green Version]
- Stepanova, M.; Rodriguez, E.; Birerdinc, A.; Baranova, A. Age-independent rise of inflammatory scores may contribute to accelerated aging in multi-morbidity. Oncotarget 2015, 6, 1414–1421. [Google Scholar] [CrossRef] [Green Version]
- Franceschi, C.; Campisi, J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J. Gerontol. Biol. Sci. Med. Sci. 2014, 69 (Suppl. S1), S4–S9. [Google Scholar] [CrossRef]
- Powers, D.C.; Morley, J.E.; Flood, J.F. Age-related changes in LFA-1 expression, cell adhesion, and PHA-induced proliferation by lymphocytes from senescence-accelerated mouse (SAM)-P/8 and SAM-R/1 substrains. Cell Immunol. 1992, 141, 444–456. [Google Scholar] [CrossRef]
- Pallis, M.; Robins, A.; Powell, R. Quantitative analysis of lymphocyte CD11a using standardized flow cytometry. Scand. J. Immunol. 1993, 38, 559–564. [Google Scholar] [CrossRef]
- Okumura, M.; Fujii, Y.; Takeuchi, Y.; Inada, K.; Nakahara, K.; Matsuda, H. Age-related accumulation of LFA-1high cells in a CD8+CD45RAhigh T cell population. Eur. J. Immunol. 1993, 23, 1057–1063. [Google Scholar] [CrossRef]
- Chiricolo, M.; Morini, M.C.; Mancini, R.; Beltrandi, E.; Belletti, D.; Conte, R. Cell adhesion molecules CD11a and CD18 in blood monocytes in old age and the consequences for immunological dysfunction. Preliminary results. Gerontology 1995, 41, 227–234. [Google Scholar] [CrossRef]
- Fulop, T.; Larbi, A.; Pawelec, G. Human T cell aging and the impact of persistent viral infections. Front. Immunol. 2013, 4, 271. [Google Scholar] [CrossRef] [Green Version]
- Franceschi, C.; Bonafe, M.; Valensin, S.; Olivieri, F.; De Luca, M.; Ottaviani, E.; De Benedictis, G. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann. N. Y. Acad. Sci. 2000, 908, 244–254. [Google Scholar] [CrossRef]
- Flesher, D.L.; Sun, X.; Behrens, T.W.; Graham, R.R.; Criswell, L.A. Recent advances in the genetics of systemic lupus erythematosus. Expert Rev. Clin. Immunol. 2010, 6, 461–479. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, A.; Sridharan, A.; Prakash, S.; Agrawal, H. Dendritic cells and aging: Consequences for autoimmunity. Expert Rev. Clin. Immunol. 2012, 8, 73–80. [Google Scholar] [CrossRef] [Green Version]
- Prasad, S.; Sung, B.; Aggarwal, B.B. Age-associated chronic diseases require age-old medicine: Role of chronic inflammation. Prev. Med. 2012, 54, S29–S37. [Google Scholar] [CrossRef] [Green Version]
- La Ferla, K.; Reimann, C.; Jelkmann, W.; Hellwig-Burgel, T. Inhibition of erythropoietin gene expression signaling involves the transcription factors GATA-2 and NF-kappaB. FASEB J. 2002, 16, 1811–1813. [Google Scholar] [CrossRef]
- Munoz-Canoves, P.; Scheele, C.; Pedersen, B.K.; Serrano, A.L. Interleukin-6 myokine signaling in skeletal muscle: A double-edged sword? FEBS J. 2013, 280, 4131–4148. [Google Scholar] [CrossRef]
- De Luca, C.; Olefsky, J.M. Inflammation and insulin resistance. FEBS Lett. 2008, 582, 97–105. [Google Scholar] [CrossRef] [Green Version]
- Sprague, A.H.; Khalil, R.A. Inflammatory cytokines in vascular dysfunction and vascular disease. Biochem. Pharmacol. 2009, 78, 539–552. [Google Scholar] [CrossRef] [Green Version]
- Akiyama, H.; Barger, S.; Barnum, S.; Bradt, B.; Bauer, J.; Cole, G.M.; Cooper, N.R.; Eikelenboom, P.; Emmerling, M.; Fiebich, B.L.; et al. Inflammation and Alzheimer’s disease. Neurobiol. Aging 2000, 21, 383–421. [Google Scholar] [CrossRef]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef]
- Lum, A.F.; Green, C.E.; Lee, G.R.; Staunton, D.E.; Simon, S.I. Dynamic regulation of LFA-1 activation and neutrophil arrest on intercellular adhesion molecule 1 (ICAM-1) in shear flow. J. Biol. Chem. 2002, 277, 20660–20670. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Deng, C.; Lu, Q.; Richardson, B. Age-dependent DNA methylation changes in the ITGAL (CD11a) promoter. Mech. Ageing Dev. 2002, 123, 1257–1268. [Google Scholar] [CrossRef]
- Lu, Q.; Kaplan, M.; Ray, D.; Ray, D.; Zacharek, S.; Gutsch, D.; Richardson, B. Demethylation of ITGAL (CD11a) regulatory sequences in systemic lupus erythematosus. Arthritis Rheum. 2002, 46, 1282–1291. [Google Scholar] [CrossRef]
- Kochmanski, J.; Marchlewicz, E.H.; Cavalcante, R.G.; Sartor, M.A.; Dolinoy, D.C. Age-related Epigenome-wide DNA Methylation and Hydroxymethylation in Longitudinal Mouse Blood. Epigenetics 2018, 13, 779–792. [Google Scholar] [CrossRef] [Green Version]
- Guevara, E.E.; Lawler, R.R.; Staes, N.; White, C.M.; Sherwood, C.C.; Ely, J.J.; Hopkins, W.D.; Bradley, B.J. Age-associated epigenetic change in chimpanzees and humans. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2020, 375, 20190616. [Google Scholar] [CrossRef]
- Avrahami, D.; Li, C.; Zhang, J.; Schug, J.; Avrahami, R.; Rao, S.; Stadler, M.B.; Burger, L.; Schubeler, D.; Glaser, B.; et al. Aging-Dependent Demethylation of Regulatory Elements Correlates with Chromatin State and Improved beta Cell Function. Cell Metab. 2015, 22, 619–632. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, A.; Leblond, F.; Mamarbachi, M.; Geoffroy, S.; Thorin, E. Age-Dependent Demethylation of Sod2 Promoter in the Mouse Femoral Artery. Oxid. Med. Cell. Longev. 2016, 2016, 8627384. [Google Scholar] [CrossRef] [Green Version]
- Takasugi, M.; Hayakawa, K.; Arai, D.; Shiota, K. Age- and sex-dependent DNA hypomethylation controlled by growth hormone in mouse liver. Mech. Ageing Dev. 2013, 134, 331–337. [Google Scholar] [CrossRef]
- Khalil, H.; Tazi, M.; Caution, K.; Ahmed, A.; Kanneganti, A.; Assani, K.; Kopp, B.; Marsh, C.; Dakhlallah, D.; Amer, A.O. Aging is associated with hypermethylation of autophagy genes in macrophages. Epigenetics 2016, 11, 381–388. [Google Scholar] [CrossRef] [Green Version]
- Thalheim, T.; Herberg, M.; Galle, J. Linking DNA Damage and Age-Related Promoter DNA Hyper-Methylation in the Intestine. Genes 2018, 9, 17. [Google Scholar] [CrossRef] [Green Version]
- Cruickshanks, H.A.; McBryan, T.; Nelson, D.M.; Vanderkraats, N.D.; Shah, P.P.; van Tuyn, J.; Singh Rai, T.; Brock, C.; Donahue, G.; Dunican, D.S.; et al. Senescent cells harbour features of the cancer epigenome. Nat. Cell Biol. 2013, 15, 1495–1506. [Google Scholar] [CrossRef]
- Horvath, S. DNA methylation age of human tissues and cell types. Genome Biol. 2013, 14, R115. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Guo, Z.; Guo, Y.; Li, M.; Yan, H.; Cheng, J.; Wang, C.; Hong, G. Common DNA methylation alterations of Alzheimer’s disease and aging in peripheral whole blood. Oncotarget 2016, 7, 19089–19098. [Google Scholar] [CrossRef] [Green Version]
- Lopez-Otin, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef] [Green Version]
- Marioni, R.E.; Shah, S.; McRae, A.F.; Chen, B.H.; Colicino, E.; Harris, S.E.; Gibson, J.; Henders, A.K.; Redmond, P.; Cox, S.R.; et al. DNA methylation age of blood predicts all-cause mortality in later life. Genome Biol. 2015, 16, 25. [Google Scholar] [CrossRef] [Green Version]
- Ramos, R.B.; Fabris, V.; Lecke, S.B.; Maturana, M.A.; Spritzer, P.M. Association between global leukocyte DNA methylation and cardiovascular risk in postmenopausal women. BMC Med. Genet. 2016, 17, 71. [Google Scholar] [CrossRef] [Green Version]
- Watson, C.T.; Roussos, P.; Garg, P.; Ho, D.J.; Azam, N.; Katsel, P.L.; Haroutunian, V.; Sharp, A.J. Genome-wide DNA methylation profiling in the superior temporal gyrus reveals epigenetic signatures associated with Alzheimer’s disease. Genome Med. 2016, 8, 5. [Google Scholar] [CrossRef] [Green Version]
- Joyce, B.T.; Gao, T.; Zheng, Y.; Liu, L.; Zhang, W.; Dai, Q.; Shrubsole, M.J.; Hibler, E.A.; Cristofanilli, M.; Zhang, H.; et al. Prospective changes in global DNA methylation and cancer incidence and mortality. Br. J. Cancer 2016, 115, 465–472. [Google Scholar] [CrossRef] [Green Version]
- Kresovich, J.K.; Joyce, B.T.; Gao, T.; Zheng, Y.; Zhang, Z.; Achenbach, C.J.; Murphy, R.L.; Just, A.C.; Shen, J.; Yang, H.; et al. Promoter methylation of PGC1A and PGC1B predicts cancer incidence in a veteran cohort. Epigenomics 2018, 10, 733–743. [Google Scholar] [CrossRef]
- Maeda, M.; Nakajima, T.; Oda, I.; Shimazu, T.; Yamamichi, N.; Maekita, T.; Asada, K.; Yokoi, C.; Ando, T.; Yoshida, T.; et al. High impact of methylation accumulation on metachronous gastric cancer: 5-year follow-up of a multicentre prospective cohort study. Gut 2017, 66, 1721–1723. [Google Scholar] [CrossRef] [Green Version]
- Nishida, N.; Iwanishi, M.; Minami, T.; Chishina, H.; Arizumi, T.; Takita, M.; Kitai, S.; Yada, N.; Ida, H.; Hagiwara, S.; et al. Hepatic DNA Methylation Is Affected by Hepatocellular Carcinoma Risk in Patients with and without Hepatitis Virus. Dig. Dis. 2015, 33, 745–750. [Google Scholar] [CrossRef]
- Vaz, M.; Hwang, S.Y.; Kagiampakis, I.; Phallen, J.; Patil, A.; O’Hagan, H.M.; Murphy, L.; Zahnow, C.A.; Gabrielson, E.; Velculescu, V.E.; et al. Chronic Cigarette Smoke-Induced Epigenomic Changes Precede Sensitization of Bronchial Epithelial Cells to Single-Step Transformation by KRAS Mutations. Cancer Cell 2017, 32, 360–376.e6. [Google Scholar] [CrossRef] [Green Version]
- Ianov, L.; Riva, A.; Kumar, A.; Foster, T.C. DNA Methylation of Synaptic Genes in the Prefrontal Cortex Is Associated with Aging and Age-Related Cognitive Impairment. Front. Aging Neurosci. 2017, 9, 249. [Google Scholar] [CrossRef]
- Jin, L.; Jiang, Z.; Xia, Y.; Lou, P.; Chen, L.; Wang, H.; Bai, L.; Xie, Y.; Liu, Y.; Li, W.; et al. Genome-wide DNA methylation changes in skeletal muscle between young and middle-aged pigs. BMC Genom. 2014, 15, 653. [Google Scholar] [CrossRef] [Green Version]
- Kananen, L.; Marttila, S.; Nevalainen, T.; Jylhava, J.; Mononen, N.; Kahonen, M.; Raitakari, O.T.; Lehtimaki, T.; Hurme, M. Aging-associated DNA methylation changes in middle-aged individuals: The Young Finns study. BMC Genom. 2016, 17, 103. [Google Scholar] [CrossRef] [Green Version]
- Spiers, H.; Hannon, E.; Wells, S.; Williams, B.; Fernandes, C.; Mill, J. Age-associated changes in DNA methylation across multiple tissues in an inbred mouse model. Mech. Ageing Dev. 2016, 154, 20–23. [Google Scholar] [CrossRef]
- De, F.C.L.A.J.; van der Plaat, D.A.; de Jong, K.; van Diemen, C.C.; Postma, D.S.; Nedeljkovic, I.; van Duijn, C.M.; Amin, N.; la Bastide-van Gemert, S.; de Vries, M.; et al. Long-term Air Pollution Exposure, Genome-wide DNA Methylation and Lung Function in the LifeLines Cohort Study. Environ. Health Perspect. 2018, 126, 027004. [Google Scholar]
- Nwanaji-Enwerem, J.C.; Colicino, E.; Dai, L.; Cayir, A.; Sanchez-Guerra, M.; Laue, H.E.; Nguyen, V.T.; Di, Q.; Just, A.C.; Hou, L.; et al. Impacts of the Mitochondrial Genome on the Relationship of Long-Term Ambient Fine Particle Exposure with Blood DNA Methylation Age. Environ. Sci. Technol. 2017, 51, 8185–8195. [Google Scholar] [CrossRef]
- Panni, T.; Mehta, A.J.; Schwartz, J.D.; Baccarelli, A.A.; Just, A.C.; Wolf, K.; Wahl, S.; Cyrys, J.; Kunze, S.; Strauch, K.; et al. Genome-Wide Analysis of DNA Methylation and Fine Particulate Matter Air Pollution in Three Study Populations: KORA F3, KORA F4, and the Normative Aging Study. Environ. Health Perspect. 2016, 124, 983–990. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Chen, R.; Shi, M.; Cai, J.; Shi, J.; Yang, C.; Li, H.; Lin, Z.; Meng, X.; Liu, C.; et al. Possible Mediation by Methylation in Acute Inflammation Following Personal Exposure to Fine Particulate Air Pollution. Am. J. Epidemiol. 2018, 187, 484–493. [Google Scholar] [CrossRef] [Green Version]
- Ward-Caviness, C.K.; Nwanaji-Enwerem, J.C.; Wolf, K.; Wahl, S.; Colicino, E.; Trevisi, L.; Kloog, I.; Just, A.C.; Vokonas, P.; Cyrys, J.; et al. Long-term exposure to air pollution is associated with biological aging. Oncotarget 2016, 7, 74510–74525. [Google Scholar] [CrossRef] [Green Version]
- Bauer, M.; Fink, B.; Thurmann, L.; Eszlinger, M.; Herberth, G.; Lehmann, I. Tobacco smoking differently influences cell types of the innate and adaptive immune system-indications from CpG site methylation. Clin. Epigenetics 2015, 7, 83. [Google Scholar] [CrossRef] [Green Version]
- Gao, X.; Zhang, Y.; Saum, K.U.; Schottker, B.; Breitling, L.P.; Brenner, H. Tobacco smoking and smoking-related DNA methylation are associated with the development of frailty among older adults. Epigenetics 2017, 12, 149–156. [Google Scholar] [CrossRef] [Green Version]
- Ligthart, S.; Steenaard, R.V.; Peters, M.J.; van Meurs, J.B.; Sijbrands, E.J.; Uitterlinden, A.G.; Bonder, M.J.; consortium, B.; Hofman, A.; Franco, O.H.; et al. Tobacco smoking is associated with DNA methylation of diabetes susceptibility genes. Diabetologia 2016, 59, 998–1006. [Google Scholar] [CrossRef] [Green Version]
- Steenaard, R.V.; Ligthart, S.; Stolk, L.; Peters, M.J.; van Meurs, J.B.; Uitterlinden, A.G.; Hofman, A.; Franco, O.H.; Dehghan, A. Tobacco smoking is associated with methylation of genes related to coronary artery disease. Clin. Epigenetics 2015, 7, 54. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Schottker, B.; Florath, I.; Stock, C.; Butterbach, K.; Holleczek, B.; Mons, U.; Brenner, H. Smoking-Associated DNA Methylation Biomarkers and Their Predictive Value for All-Cause and Cardiovascular Mortality. Environ. Health Perspect. 2016, 124, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Marioni, R.E.; Hedman, A.K.; Pfeiffer, L.; Tsai, P.C.; Reynolds, L.M.; Just, A.C.; Duan, Q.; Boer, C.G.; Tanaka, T.; et al. A DNA methylation biomarker of alcohol consumption. Mol. Psychiatry 2018, 23, 422–433. [Google Scholar] [CrossRef]
- Dugue, P.A.; Wilson, R.; Lehne, B.; Jayasekara, H.; Wang, X.; Jung, C.H.; Joo, J.E.; Makalic, E.; Schmidt, D.F.; Baglietto, L.; et al. Alcohol consumption is associated with widespread changes in blood DNA methylation: Analysis of cross-sectional and longitudinal data. Addict. Biol. 2021, 26, e12855. [Google Scholar] [CrossRef]
- Friedel, E.; Walter, H.; Veer, I.M.; Zimmermann, U.S.; Heinz, A.; Frieling, H.; Zindler, T. Impact of Long-Term Alcohol Consumption and Relapse on Genome-Wide DNA Methylation Changes in Alcohol-Dependent Subjects: A Longitudinal Study. Alcohol. Clin. Exp. Res. 2020, 44, 1356–1365. [Google Scholar] [CrossRef]
- Lu, M.; Xueying, Q.; Hexiang, P.; Wenjing, G.; Hagg, S.; Weihua, C.; Chunxiao, L.; Canqing, Y.; Jun, L.; Zengchang, P.; et al. Genome-wide associations between alcohol consumption and blood DNA methylation: Evidence from twin study. Epigenomics 2021, 13, 939–951. [Google Scholar] [CrossRef]
- O’Hagan, H.M.; Wang, W.; Sen, S.; Destefano Shields, C.; Lee, S.S.; Zhang, Y.W.; Clements, E.G.; Cai, Y.; Van Neste, L.; Easwaran, H.; et al. Oxidative damage targets complexes containing DNA methyltransferases, SIRT1, and polycomb members to promoter CpG Islands. Cancer Cell 2011, 20, 606–619. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Elgizouli, M.; Schottker, B.; Holleczek, B.; Nieters, A.; Brenner, H. Smoking-associated DNA methylation markers predict lung cancer incidence. Clin. Epigenetics 2016, 8, 127. [Google Scholar] [CrossRef] [Green Version]
- Gao, X.; Zhang, Y.; Breitling, L.P.; Brenner, H. Relationship of tobacco smoking and smoking-related DNA methylation with epigenetic age acceleration. Oncotarget 2016, 7, 46878–46889. [Google Scholar] [CrossRef] [Green Version]
- Barres, R.; Yan, J.; Egan, B.; Treebak, J.T.; Rasmussen, M.; Fritz, T.; Caidahl, K.; Krook, A.; O’Gorman, D.J.; Zierath, J.R. Acute exercise remodels promoter methylation in human skeletal muscle. Cell Metab. 2012, 15, 405–411. [Google Scholar] [CrossRef] [Green Version]
- Denham, J.; O’Brien, B.J.; Harvey, J.T.; Charchar, F.J. Genome-wide sperm DNA methylation changes after 3 months of exercise training in humans. Epigenomics 2015, 7, 717–731. [Google Scholar] [CrossRef]
- Maejima, H.; Kanemura, N.; Kokubun, T.; Murata, K.; Takayanagi, K. Exercise enhances cognitive function and neurotrophin expression in the hippocampus accompanied by changes in epigenetic programming in senescence-accelerated mice. Neurosci. Lett. 2018, 665, 67–73. [Google Scholar] [CrossRef]
- Ronn, T.; Volkov, P.; Davegardh, C.; Dayeh, T.; Hall, E.; Olsson, A.H.; Nilsson, E.; Tornberg, A.; Dekker Nitert, M.; Eriksson, K.F.; et al. A six months exercise intervention influences the genome-wide DNA methylation pattern in human adipose tissue. PLoS Genet. 2013, 9, e1003572. [Google Scholar] [CrossRef]
- Barres, R.; Kirchner, H.; Rasmussen, M.; Yan, J.; Kantor, F.R.; Krook, A.; Naslund, E.; Zierath, J.R. Weight loss after gastric bypass surgery in human obesity remodels promoter methylation. Cell Rep. 2013, 3, 1020–1027. [Google Scholar] [CrossRef] [Green Version]
- Chen, B.H.; Marioni, R.E.; Colicino, E.; Peters, M.J.; Ward-Caviness, C.K.; Tsai, P.C.; Roetker, N.S.; Just, A.C.; Demerath, E.W.; Guan, W.; et al. DNA methylation-based measures of biological age: Meta-analysis predicting time to death. Aging Albany NY 2016, 8, 1844–1865. [Google Scholar] [CrossRef] [Green Version]
- Minois, N.; Carmona-Gutierrez, D.; Madeo, F. Polyamines in aging and disease. Aging Albany NY 2011, 3, 716–732. [Google Scholar] [CrossRef] [Green Version]
- Shain, S.A.; Schultz, J.J.; Lancaster, C.M. Aging in the AXC/SSh rat: Diminished prostate L-ornithine decarboxylase (ODC) activity reflects diminished prostate ODC protein and transcript content. Endocrinology 1986, 119, 1830–1838. [Google Scholar] [CrossRef]
- Casillas, M.A., Jr.; Lopatina, N.; Andrews, L.G.; Tollefsbol, T.O. Transcriptional control of the DNA methyltransferases is altered in aging and neoplastically-transformed human fibroblasts. Mol. Cell. Biochem. 2003, 252, 33–43. [Google Scholar] [CrossRef]
- Lopatina, N.; Haskell, J.F.; Andrews, L.G.; Poole, J.C.; Saldanha, S.; Tollefsbol, T. Differential maintenance and de novo methylating activity by three DNA methyltransferases in aging and immortalized fibroblasts. J. Cell. Biochem. 2002, 84, 324–334. [Google Scholar] [CrossRef]
- Oliveira, A.M.; Hemstedt, T.J.; Bading, H. Rescue of aging-associated decline in Dnmt3a2 expression restores cognitive abilities. Nat. Neurosci. 2012, 15, 1111–1113. [Google Scholar] [CrossRef]
- Romanenko, E.B.; Demidenko, Z.N.; Vanyushin, B.F. RNA-polymerase, DNA-polymerase, DNA-methyltransferase and sphingomyelinase activities in liver nuclei of rats of different Age. Biochemistry 1998, 63, 159–163. [Google Scholar]
- Frostesjo, L.; Holm, I.; Grahn, B.; Page, A.W.; Bestor, T.H.; Heby, O. Interference with DNA methyltransferase activity and genome methylation during F9 teratocarcinoma stem cell differentiation induced by polyamine depletion. J. Biol. Chem. 1997, 272, 4359–4366. [Google Scholar] [CrossRef] [Green Version]
- Poomipark, N.; Flatley, J.E.; Hill, M.H.; Mangnall, B.; Azar, E.; Grabowski, P.; Powers, H.J. Methyl Donor Status Influences DNMT Expression and Global DNA Methylation in Cervical Cancer Cells. Asian Pac. J. Cancer Prev. 2016, 17, 3213–3222. [Google Scholar]
- Tsuji, T.; Usui, S.; Aida, T.; Tachikawa, T.; Hu, G.F.; Sasaki, A.; Matsumura, T.; Todd, R.; Wong, D.T. Induction of epithelial differentiation and DNA demethylation in hamster malignant oral keratinocyte by ornithine decarboxylase antizyme. Oncogene 2001, 20, 24–33. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, D.; Shima, K.; Matsuo, K.; Nishioka, T.; Chen, C.Y.; Hu, G.F.; Sasaki, A.; Tsuji, T. Ornithine decarboxylase antizyme induces hypomethylation of genome DNA and histone H3 lysine 9 dimethylation (H3K9me2) in human oral cancer cell line. PLoS ONE 2010, 5, e12554. [Google Scholar] [CrossRef] [Green Version]
- Pegg, A.E.; Wang, X.; Schwartz, C.E.; McCloskey, D.E. Spermine synthase activity affects the content of decarboxylated S-adenosylmethionine. Biochem. J. 2011, 433, 139–144. [Google Scholar] [CrossRef] [Green Version]
- Shantz, L.M.; Holm, I.; Janne, O.A.; Pegg, A.E. Regulation of S-adenosylmethionine decarboxylase activity by alterations in the intracellular polyamine content. Biochem. J. 1992, 288 Pt 2, 511–518. [Google Scholar] [CrossRef] [Green Version]
- Papazafiri, P.; Osborne, H.B. Effect of alpha-difluoromethylornithine on DNA methylation in murine erythroleukaemic cells. Relationship to stimulation of induced differentiation. Biochem. J. 1987, 242, 479–483. [Google Scholar] [CrossRef]
- Bell, J.T.; Tsai, P.C.; Yang, T.P.; Pidsley, R.; Nisbet, J.; Glass, D.; Mangino, M.; Zhai, G.; Zhang, F.; Valdes, A.; et al. Epigenome-wide scans identify differentially methylated regions for age and age-related phenotypes in a healthy ageing population. PLoS Genet. 2012, 8, e1002629. [Google Scholar] [CrossRef] [Green Version]
- Florath, I.; Butterbach, K.; Muller, H.; Bewerunge-Hudler, M.; Brenner, H. Cross-sectional and longitudinal changes in DNA methylation with age: An epigenome-wide analysis revealing over 60 novel age-associated CpG sites. Hum. Mol. Genet. 2014, 23, 1186–1201. [Google Scholar] [CrossRef]
- McClay, J.L.; Aberg, K.A.; Clark, S.L.; Nerella, S.; Kumar, G.; Xie, L.Y.; Hudson, A.D.; Harada, A.; Hultman, C.M.; Magnusson, P.K.; et al. A methylome-wide study of aging using massively parallel sequencing of the methyl-CpG-enriched genomic fraction from blood in over 700 subjects. Hum. Mol. Genet. 2014, 23, 1175–1185. [Google Scholar] [CrossRef] [Green Version]
- Perez, R.F.; Tejedor, J.R.; Bayon, G.F.; Fernandez, A.F.; Fraga, M.F. Distinct chromatin signatures of DNA hypomethylation in aging and cancer. Aging Cell 2018, 17, e12744. [Google Scholar] [CrossRef]
- Zeng, Q.; Chen, X.; Ning, C.; Zhu, Q.; Yao, Y.; Zhao, Y.; Luan, F. Methylation of the genes ROD1, NLRC5, and HKR1 is associated with aging in Hainan centenarians. BMC Med. Genom. 2018, 11, 7. [Google Scholar] [CrossRef] [Green Version]
- Lu, Q.; Ray, D.; Gutsch, D.; Richardson, B. Effect of DNA methylation and chromatin structure on ITGAL expression. Blood 2002, 99, 4503–4508. [Google Scholar] [CrossRef] [Green Version]
- Vargas, A.J.; Ashbeck, E.L.; Wertheim, B.C.; Wallace, R.B.; Neuhouser, M.L.; Thomson, C.A.; Thompson, P.A. Dietary polyamine intake and colorectal cancer risk in postmenopausal women. Am. J. Clin. Nutr. 2015, 102, 411–419. [Google Scholar] [CrossRef] [Green Version]
- Wada, M.; Funada-Wada, U.; Mano, H.; Udaka, S. Effects of Dietary Polyamines on the Promotion of Mammary Tumor in Rats. J. Health Sci. 2002, 48, 376–380. [Google Scholar] [CrossRef] [Green Version]
- Soda, K. Polyamine Metabolism and Gene Methylation in Conjunction with One-Carbon Metabolism. Int. J. Mol. Sci. 2018, 19, 3106. [Google Scholar] [CrossRef] [Green Version]
- Hao, Q.; Dong, B.; Yang, M.; Dong, B.; Wei, Y. Frailty and Cognitive Impairment in Predicting Mortality among Oldest-Old People. Front. Aging Neurosci. 2018, 10, 295. [Google Scholar] [CrossRef] [Green Version]
- Langa, K.M.; Larson, E.B.; Karlawish, J.H.; Cutler, D.M.; Kabeto, M.U.; Kim, S.Y.; Rosen, A.B. Trends in the prevalence and mortality of cognitive impairment in the United States: Is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 2008, 4, 134–144. [Google Scholar] [CrossRef] [Green Version]
- Perna, L.; Wahl, H.W.; Mons, U.; Saum, K.U.; Holleczek, B.; Brenner, H. Cognitive impairment, all-cause and cause-specific mortality among non-demented older adults. Age Ageing 2015, 44, 445–451. [Google Scholar] [CrossRef] [Green Version]
- Park, M.H.; Kwon, D.Y.; Jung, J.M.; Han, C.; Jo, I.; Jo, S.A. Mini-Mental Status Examination as predictors of mortality in the elderly. Acta Psychiatr. Scand. 2013, 127, 298–304. [Google Scholar] [CrossRef]
- Sachs, G.A.; Carter, R.; Holtz, L.R.; Smith, F.; Stump, T.E.; Tu, W.; Callahan, C.M. Cognitive impairment: An independent predictor of excess mortality: A cohort study. Ann. Intern. Med. 2011, 155, 300–308. [Google Scholar] [CrossRef]
- Santabarbara, J.; Gracia-Garcia, P.; Pirez, G.; Lopez-Anton, R.; De La Camara, C.; Ventura, T.; Perez-Sastre, M.; Lobo, E.; Saz, P.; Marcos, G.; et al. Mortality in Mild Cognitive Impairment Diagnosed with DSM-5 Criteria and with Petersen’s Criteria: A 17-Year Follow-Up in a Community Study. Am. J. Geriatr. Psychiatry 2016, 24, 977–986. [Google Scholar] [CrossRef]
- Vassilaki, M.; Cha, R.H.; Aakre, J.A.; Therneau, T.M.; Geda, Y.E.; Mielke, M.M.; Knopman, D.S.; Petersen, R.C.; Roberts, R.O. Mortality in mild cognitive impairment varies by subtype, sex, and lifestyle factors: The Mayo Clinic Study of Aging. J. Alzheimers Dis. 2015, 45, 1237–1245. [Google Scholar] [CrossRef] [Green Version]
- Gupta, V.K.; Scheunemann, L.; Eisenberg, T.; Mertel, S.; Bhukel, A.; Koemans, T.S.; Kramer, J.M.; Liu, K.S.; Schroeder, S.; Stunnenberg, H.G.; et al. Restoring polyamines protects from age-induced memory impairment in an autophagy-dependent manner. Nat. Neurosci. 2013, 16, 1453–1460. [Google Scholar] [CrossRef]
- Bell, R.D.; Zlokovic, B.V. Neurovascular mechanisms and blood-brain barrier disorder in Alzheimer’s disease. Acta Neuropathol. 2009, 118, 103–113. [Google Scholar] [CrossRef] [Green Version]
- Zlokovic, B.V. Neurovascular pathways to neurodegeneration in Alzheimer’s disease and other disorders. Nat. Rev. Neurosci. 2011, 12, 723–738. [Google Scholar] [CrossRef]
- Bartels, A.L. Blood-brain barrier P-glycoprotein function in neurodegenerative disease. Curr. Pharm. Des. 2011, 17, 2771–2777. [Google Scholar] [CrossRef]
- Chung, Y.C.; Ko, H.W.; Bok, E.; Park, E.S.; Huh, S.H.; Nam, J.H.; Jin, B.K. The role of neuroinflammation on the pathogenesis of Parkinson’s disease. BMB Rep. 2010, 43, 225–232. [Google Scholar] [CrossRef] [Green Version]
- Lassmann, H.; van Horssen, J.; Mahad, D. Progressive multiple sclerosis: Pathology and pathogenesis. Nat. Rev. Neurol. 2012, 8, 647–656. [Google Scholar] [CrossRef]
- Prineas, J.W.; Parratt, J.D. Oligodendrocytes and the early multiple sclerosis lesion. Ann. Neurol. 2012, 72, 18–31. [Google Scholar] [CrossRef]
- Tourdias, T.; Dousset, V. Neuroinflammatory imaging biomarkers: Relevance to multiple sclerosis and its therapy. Neurotherapeutics 2013, 10, 111–123. [Google Scholar] [CrossRef] [Green Version]
- Garbuzova-Davis, S.; Sanberg, P.R. Blood-CNS Barrier Impairment in ALS patients versus an animal model. Front. Cell. Neurosci. 2014, 8, 21. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, M.C.; Hernandez-Ontiveros, D.G.; Louis, M.K.; Willing, A.E.; Borlongan, C.V.; Sanberg, P.R.; Voltarelli, J.C.; Garbuzova-Davis, S. Neurovascular aspects of amyotrophic lateral sclerosis. Int. Rev. Neurobiol. 2012, 102, 91–106. [Google Scholar]
- Iadecola, C. The pathobiology of vascular dementia. Neuron 2013, 80, 844–866. [Google Scholar] [CrossRef] [Green Version]
- Wardlaw, J.M.; Sandercock, P.A.; Dennis, M.S.; Starr, J. Is breakdown of the blood-brain barrier responsible for lacunar stroke, leukoaraiosis, and dementia? Stroke 2003, 34, 806–812. [Google Scholar] [CrossRef]
- Inoue, K.; Tsutsui, H.; Akatsu, H.; Hashizume, Y.; Matsukawa, N.; Yamamoto, T.; Toyo’oka, T. Metabolic profiling of Alzheimer’s disease brains. Sci. Rep. 2013, 3, 2364. [Google Scholar] [CrossRef] [Green Version]
- Akanuma, S.I.; Shimada, H.; Kubo, Y.; Hosoya, K.I. Involvement of Carrier-Mediated Transport at the Blood-Cerebrospinal Fluid Barrier in Spermine Clearance from Rat Brain. Biol. Pharm. Bull. 2017, 40, 1599–1603. [Google Scholar] [CrossRef] [Green Version]
- Gomes-Trolin, C.; Nygren, I.; Aquilonius, S.M.; Askmark, H. Increased red blood cell polyamines in ALS and Parkinson’s disease. Exp. Neurol. 2002, 177, 515–520. [Google Scholar] [CrossRef]
- Graham, S.F.; Chevallier, O.P.; Elliott, C.T.; Holscher, C.; Johnston, J.; McGuinness, B.; Kehoe, P.G.; Passmore, A.P.; Green, B.D. Untargeted metabolomic analysis of human plasma indicates differentially affected polyamine and L-arginine metabolism in mild cognitive impairment subjects converting to Alzheimer’s disease. PLoS ONE 2015, 10, e0119452. [Google Scholar] [CrossRef]
- Holmes, C.; Butchart, J. Systemic inflammation and Alzheimer’s disease. Biochem. Soc. Trans. 2011, 39, 898–901. [Google Scholar] [CrossRef]
- Lee, Y.J.; Han, S.B.; Nam, S.Y.; Oh, K.W.; Hong, J.T. Inflammation and Alzheimer’s disease. Arch. Pharm. Res. 2010, 33, 1539–1556. [Google Scholar] [CrossRef]
- Tao, Q.; Ang, T.F.A.; DeCarli, C.; Auerbach, S.H.; Devine, S.; Stein, T.D.; Zhang, X.; Massaro, J.; Au, R.; Qiu, W.Q. Association of Chronic Low-grade Inflammation With Risk of Alzheimer Disease in ApoE4 Carriers. JAMA Netw. Open 2018, 1, e183597. [Google Scholar] [CrossRef] [Green Version]
- Morrison, L.D.; Bergeron, C.; Kish, S.J. Brain S-adenosylmethionine decarboxylase activity is increased in Alzheimer’s disease. Neurosci. Lett. 1993, 154, 141–144. [Google Scholar] [CrossRef]
- Karouzakis, E.; Gay, R.E.; Michel, B.A.; Gay, S.; Neidhart, M. DNA hypomethylation in rheumatoid arthritis synovial fibroblasts. Arthritis. Rheum. 2009, 60, 3613–3622. [Google Scholar] [CrossRef] [Green Version]
- Jones, M.J.; Goodman, S.J.; Kobor, M.S. DNA methylation and healthy human aging. Aging Cell 2015, 14, 924–932. [Google Scholar] [CrossRef]
- Murgatroyd, C.; Wu, Y.; Bockmuhl, Y.; Spengler, D. The Janus face of DNA methylation in aging. Aging Albany NY 2010, 2, 107–110. [Google Scholar]
- Vanyushin, B.F.; Nemirovsky, L.E.; Klimenko, V.V.; Vasiliev, V.K.; Belozersky, A.N. The 5-methylcytosine in DNA of rats. Tissue and age specificity and the changes induced by hydrocortisone and other agents. Gerontologia 1973, 19, 138–152. [Google Scholar] [CrossRef]
- Wilson, V.L.; Smith, R.A.; Ma, S.; Cutler, R.G. Genomic 5-methyldeoxycytidine decreases with age. J. Biol. Chem. 1987, 262, 9948–9951. [Google Scholar] [CrossRef]
- Day, J.J.; Sweatt, J.D. DNA methylation and memory formation. Nat. Neurosci. 2010, 13, 1319–1323. [Google Scholar] [CrossRef]
- Day, J.J.; Childs, D.; Guzman-Karlsson, M.C.; Kibe, M.; Moulden, J.; Song, E.; Tahir, A.; Sweatt, J.D. DNA methylation regulates associative reward learning. Nat. Neurosci. 2013, 16, 1445–1452. [Google Scholar] [CrossRef]
- Rosenbaum, J.F.; Fava, M.; Falk, W.E.; Pollack, M.H.; Cohen, L.S.; Cohen, B.M.; Zubenko, G.S. The antidepressant potential of oral S-adenosyl-l-methionine. Acta Psychiatr. Scand. 1990, 81, 432–436. [Google Scholar] [CrossRef]
- Chan, A.; Shea, T.B. Effects of dietary supplementation with N-acetyl cysteine, acetyl-L-carnitine and S-adenosyl methionine on cognitive performance and aggression in normal mice and mice expressing human ApoE4. Neuromol. Med. 2007, 9, 264–269. [Google Scholar] [CrossRef]
- Tchantchou, F.; Graves, M.; Ortiz, D.; Rogers, E.; Shea, T.B. Dietary supplementation with 3-deaza adenosine, N-acetyl cysteine, and S-adenosyl methionine provide neuroprotection against multiple consequences of vitamin deficiency and oxidative challenge: Relevance to age-related neurodegeneration. Neuromol. Med. 2004, 6, 93–103. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).