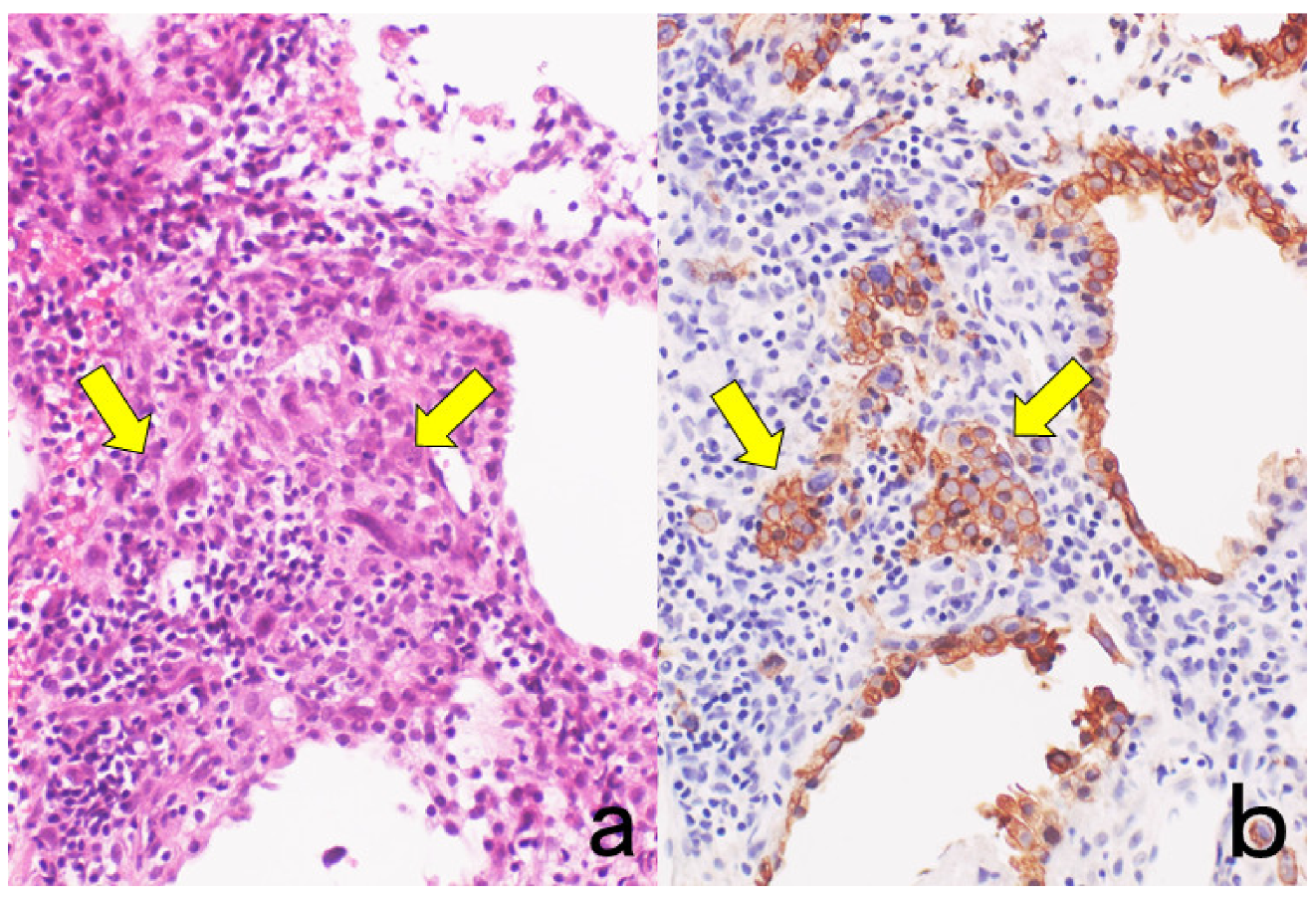
Figure 1.
Cytokeratin for identifying intermediate trophoblasts in the placenta. (a): H&E, (b): cytokeratin immunostaining. Intermediate trophoblasts (arrows) are observed in the stroma of the placental tissue sampled by curettage. Cytokeratin immunoreactivity with a monoclonal antibody CAM5.2 clearly illustrates their distribution.
Figure 1.
Cytokeratin for identifying intermediate trophoblasts in the placenta. (a): H&E, (b): cytokeratin immunostaining. Intermediate trophoblasts (arrows) are observed in the stroma of the placental tissue sampled by curettage. Cytokeratin immunoreactivity with a monoclonal antibody CAM5.2 clearly illustrates their distribution.
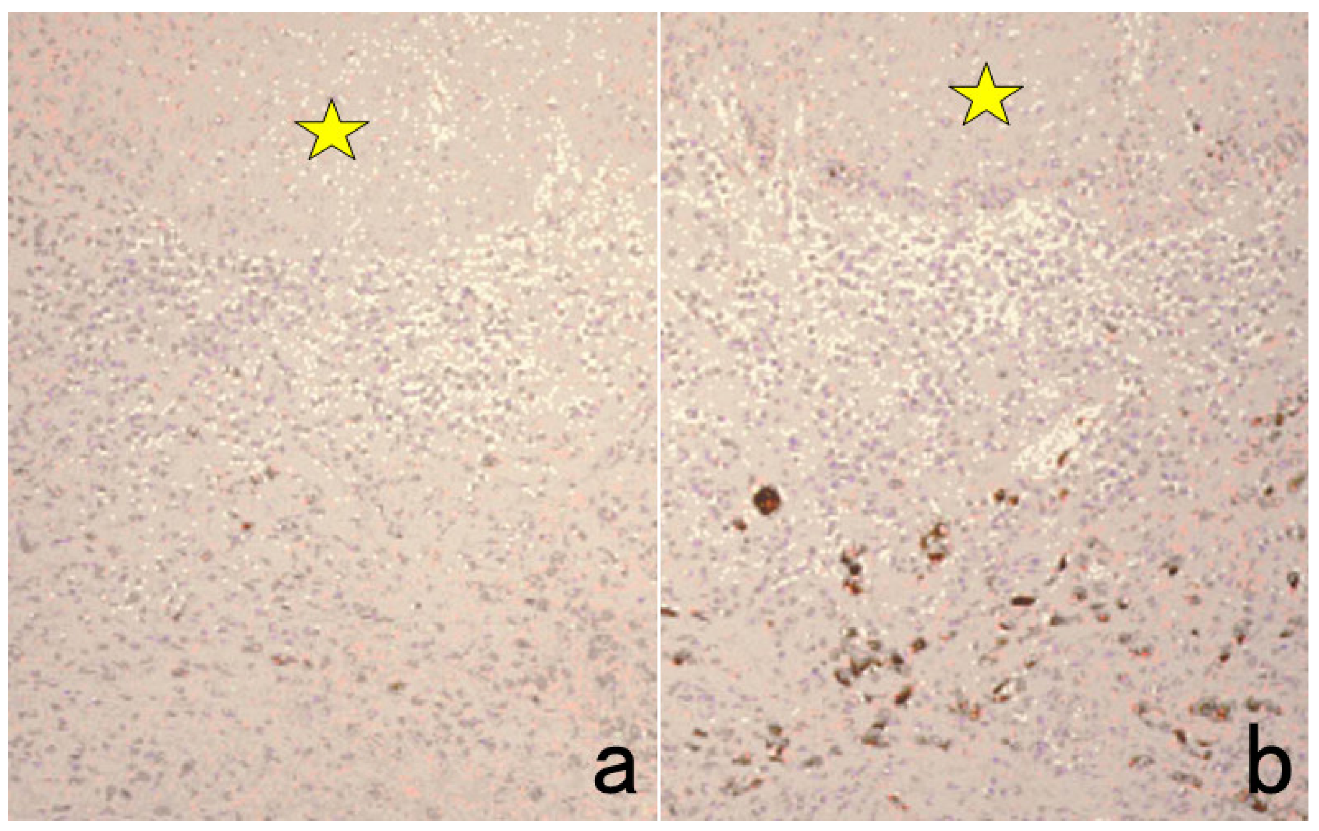
Figure 2.
p53 immunostaining without HIER in esophageal squamous cell carcinoma. (a): Polymer method (EnVision) and (b): catalyzed signal amplification (CSA)-II method. Submucosally invading cancer cells express p53 in the nuclei. The immunoreactivity is significantly enhanced by the CSA-II method using FITC tyramide as an amplifier. Stars indicate non-cancerous esophageal squamous mucosa.
Figure 2.
p53 immunostaining without HIER in esophageal squamous cell carcinoma. (a): Polymer method (EnVision) and (b): catalyzed signal amplification (CSA)-II method. Submucosally invading cancer cells express p53 in the nuclei. The immunoreactivity is significantly enhanced by the CSA-II method using FITC tyramide as an amplifier. Stars indicate non-cancerous esophageal squamous mucosa.
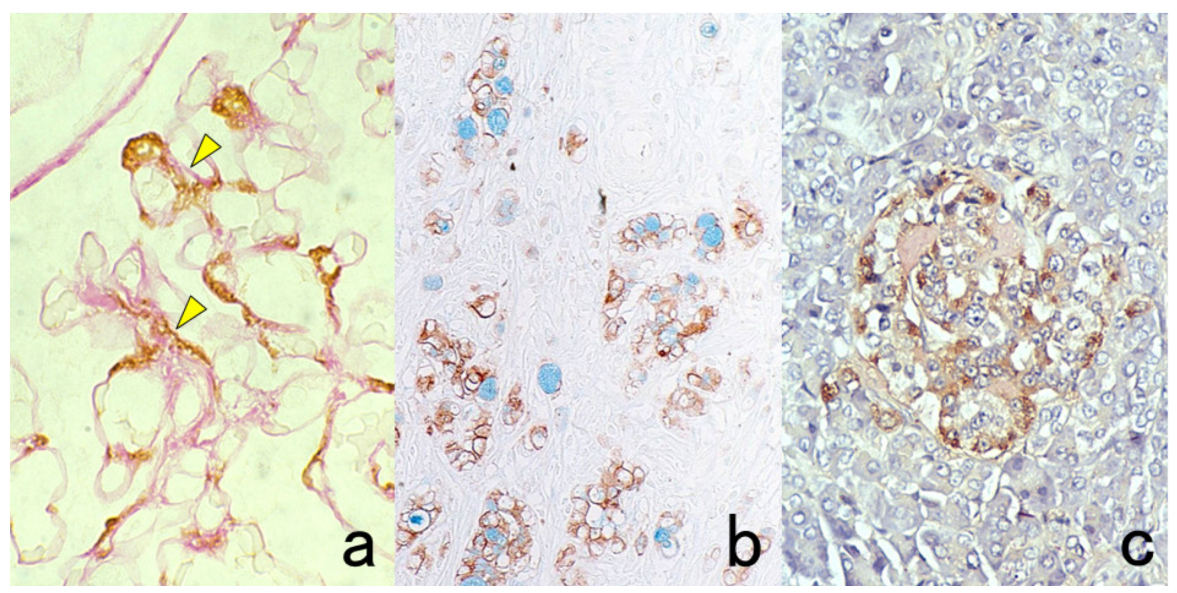
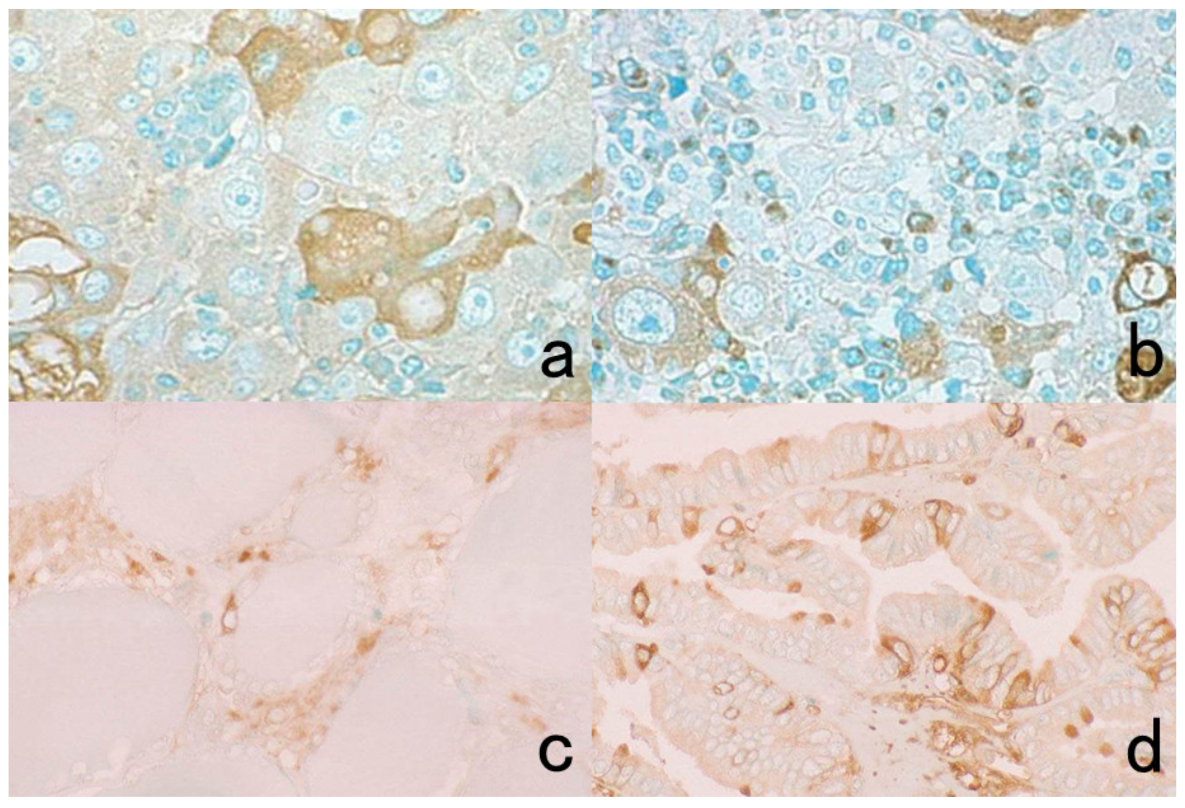
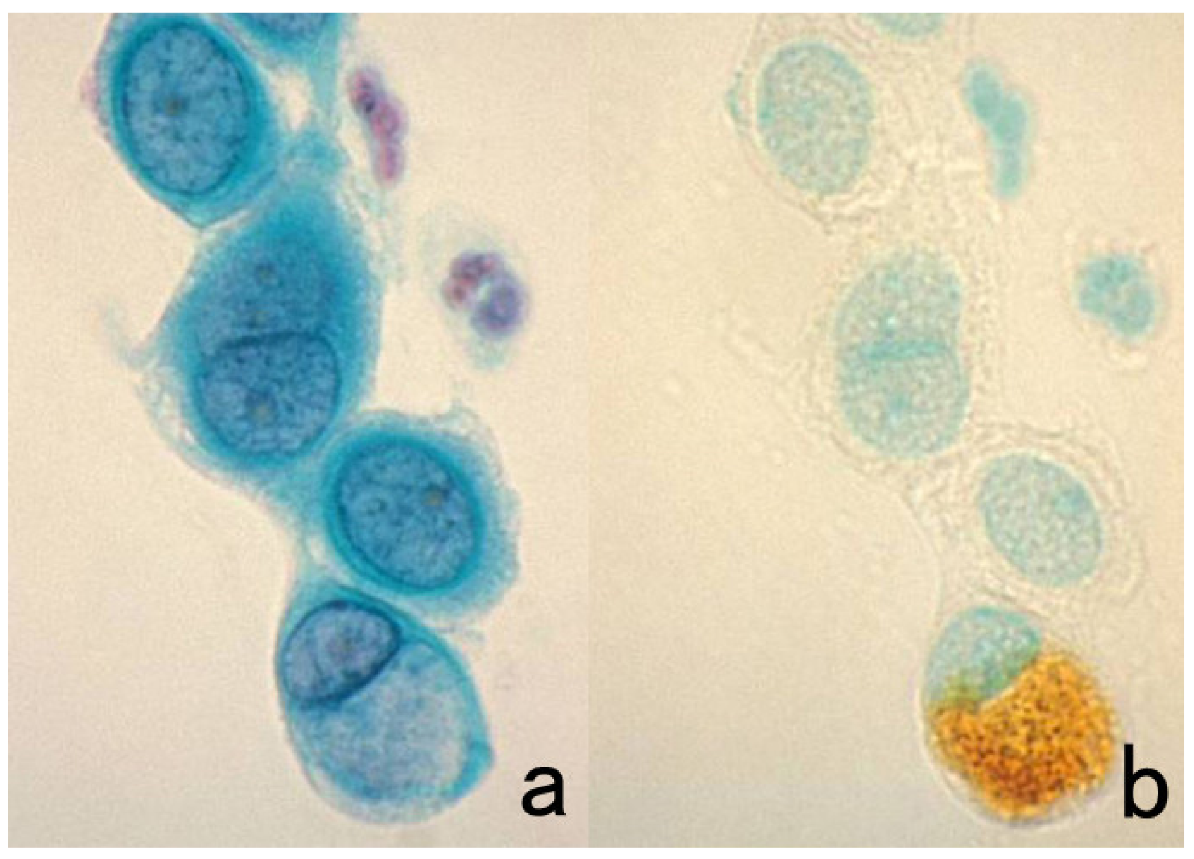
Figure 3.
Chromogenic double immunostaining. (a): Ki-67 (nuclei of proliferative cells are blue) and cleaved cytokeratin 18 (cytoplasm of apoptotic columnar cells is brown) in FFPE colonic adenocarcinoma after neoadjuvant chemotherapy. In colon cancer, some proliferative cells are apoptotic, as the arrows indicate. Cleaved cytokeratin 18 functions as an excellent marker for apoptotic columnar cells. (b): HER2-positive plasma membranes in blue and p53-positive nuclei in brown in an ethanol-fixed aspiration cytology specimen of breast cancer. In this high-grade breast cancer, the atypical ductal cells overexpress both HER2 and p53.
Figure 3.
Chromogenic double immunostaining. (a): Ki-67 (nuclei of proliferative cells are blue) and cleaved cytokeratin 18 (cytoplasm of apoptotic columnar cells is brown) in FFPE colonic adenocarcinoma after neoadjuvant chemotherapy. In colon cancer, some proliferative cells are apoptotic, as the arrows indicate. Cleaved cytokeratin 18 functions as an excellent marker for apoptotic columnar cells. (b): HER2-positive plasma membranes in blue and p53-positive nuclei in brown in an ethanol-fixed aspiration cytology specimen of breast cancer. In this high-grade breast cancer, the atypical ductal cells overexpress both HER2 and p53.
Figure 4.
Double labeling of immuno- and conventional staining. (a): IgA and PAS in renal biopsy of IgA nephropathy. The PAS-reactive basement membrane surrounds mesangial deposition of IgA visualized after prolonged trypsin digestion (arrowheads). (b): Carcinoembryonic antigen (CEA) and alcian blue in gastric signet ring cell carcinoma. CEA expression of mucin-containing cancer cells appears weaker. (c): Insulin and Congo red in a pancreatic islet in type 2 diabetes mellitus. Orange-colored amyloid deposition is seen among the insulin-positive β-cells.
Figure 4.
Double labeling of immuno- and conventional staining. (a): IgA and PAS in renal biopsy of IgA nephropathy. The PAS-reactive basement membrane surrounds mesangial deposition of IgA visualized after prolonged trypsin digestion (arrowheads). (b): Carcinoembryonic antigen (CEA) and alcian blue in gastric signet ring cell carcinoma. CEA expression of mucin-containing cancer cells appears weaker. (c): Insulin and Congo red in a pancreatic islet in type 2 diabetes mellitus. Orange-colored amyloid deposition is seen among the insulin-positive β-cells.
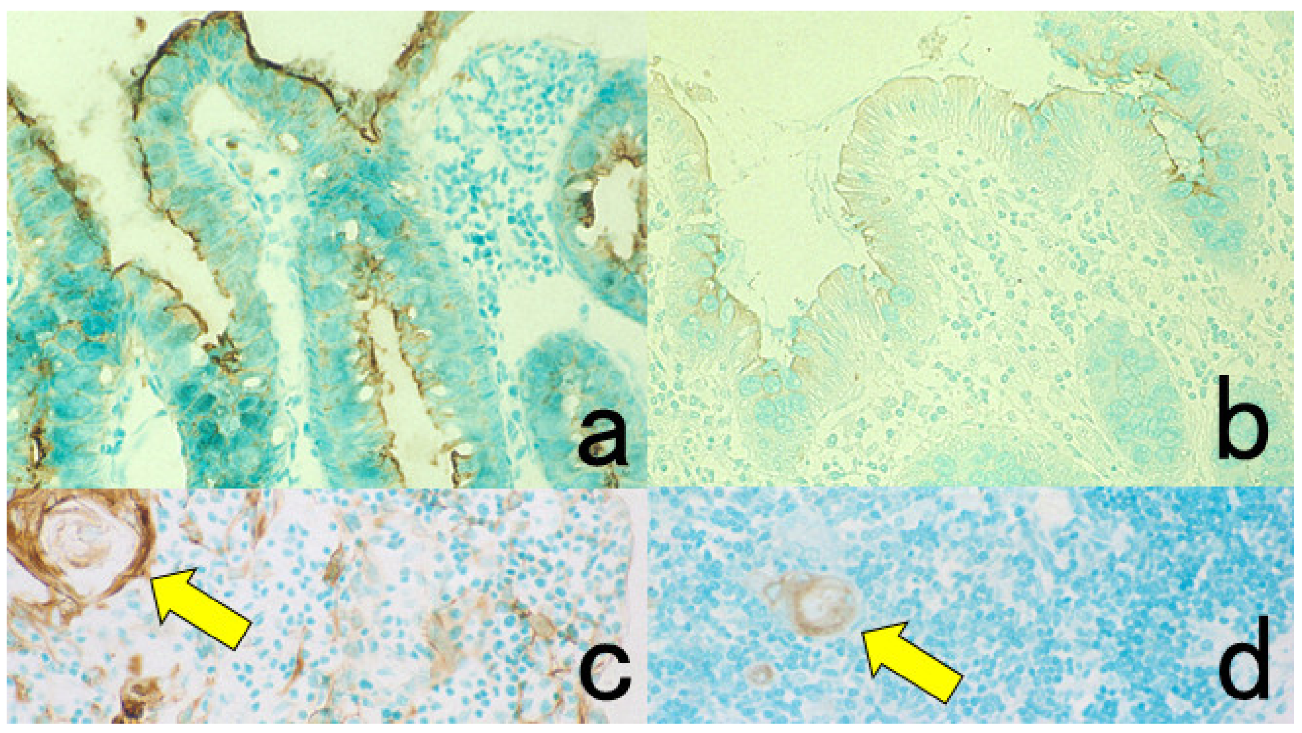
Figure 5.
Antigenic deterioration in FFPE sections. Top panels (a,b): CEA in normal gastric mucosa. Bottom panels (c,d): Cytokeratin in normal infantile thymus. Left (a,c): paraformaldehyde-fixed frozen sections. Right (b,d): FFPE sections. Antigenicities of CEA and cytokeratin detected by polyclonal antibodies are evidently weakened after the FFPE process. Arrows indicate Hassall’s corpuscles in the thymic medulla. The nuclei are counterstained with methyl green.
Figure 5.
Antigenic deterioration in FFPE sections. Top panels (a,b): CEA in normal gastric mucosa. Bottom panels (c,d): Cytokeratin in normal infantile thymus. Left (a,c): paraformaldehyde-fixed frozen sections. Right (b,d): FFPE sections. Antigenicities of CEA and cytokeratin detected by polyclonal antibodies are evidently weakened after the FFPE process. Arrows indicate Hassall’s corpuscles in the thymic medulla. The nuclei are counterstained with methyl green.
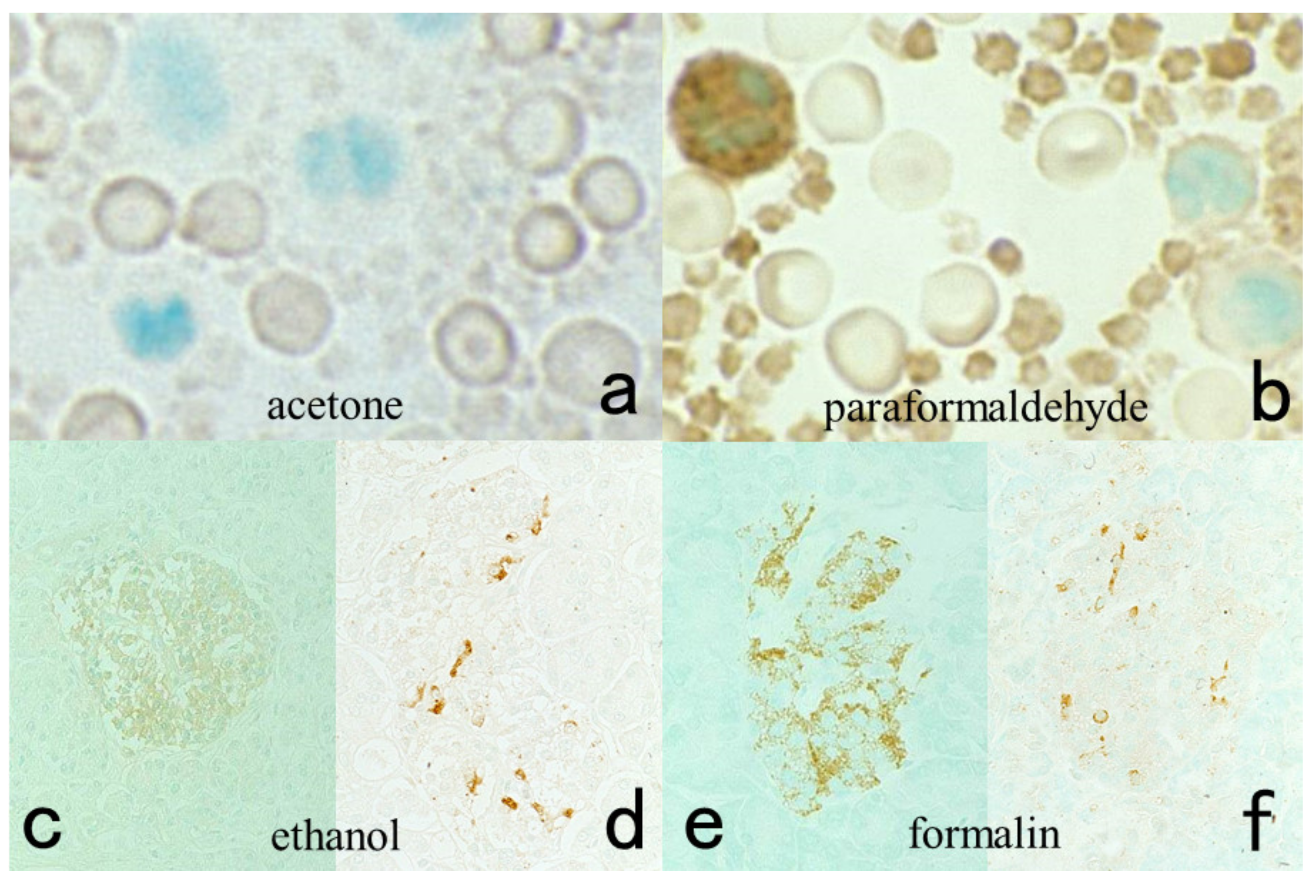
Figure 6.
Antigenic loss by fixation in organic solvent. Top panels (a,b): Immunostaining for platelet factor 4 in a smeared buffy coat of the peripheral blood. Bottom panels (c–f): Immunostaining for insulin (c,e) and somatostatin (d,f) in paraffin-embedded pancreas. Left (a,c,d): Fixation in acetone or ethanol. Right (b,e,f): Fixation in 4% paraformaldehyde or in formalin. Platelet factor 4 and insulin show false negative findings when fixed in the organic solvent. Somatostatin is resistant to ethanol fixation to be clearly immunolocalized. The nuclei are counterstained with methyl green.
Figure 6.
Antigenic loss by fixation in organic solvent. Top panels (a,b): Immunostaining for platelet factor 4 in a smeared buffy coat of the peripheral blood. Bottom panels (c–f): Immunostaining for insulin (c,e) and somatostatin (d,f) in paraffin-embedded pancreas. Left (a,c,d): Fixation in acetone or ethanol. Right (b,e,f): Fixation in 4% paraformaldehyde or in formalin. Platelet factor 4 and insulin show false negative findings when fixed in the organic solvent. Somatostatin is resistant to ethanol fixation to be clearly immunolocalized. The nuclei are counterstained with methyl green.
Figure 7.
Demonstration of HBs antigen and HCV genome in archival specimens of liver cirrhosis fixed for up to 110 years. (a): Azan stain, (b): Nested reverse transcription-PCR for detecting the C-region of the HCV genome, (c); Immunostaining for HBs antigen. HCV-RNA subtype 1b was detected with nested RT-PCR (lane 1), and the same cirrhotic specimen in 1909 was immunoreactive for HBs antigen. Double infection of HBV and HCV was proven. Another specimen in 1914 (lane 5) was also double-positive for HCV, 1b-type, and HBs antigen.
Figure 7.
Demonstration of HBs antigen and HCV genome in archival specimens of liver cirrhosis fixed for up to 110 years. (a): Azan stain, (b): Nested reverse transcription-PCR for detecting the C-region of the HCV genome, (c); Immunostaining for HBs antigen. HCV-RNA subtype 1b was detected with nested RT-PCR (lane 1), and the same cirrhotic specimen in 1909 was immunoreactive for HBs antigen. Double infection of HBV and HCV was proven. Another specimen in 1914 (lane 5) was also double-positive for HCV, 1b-type, and HBs antigen.
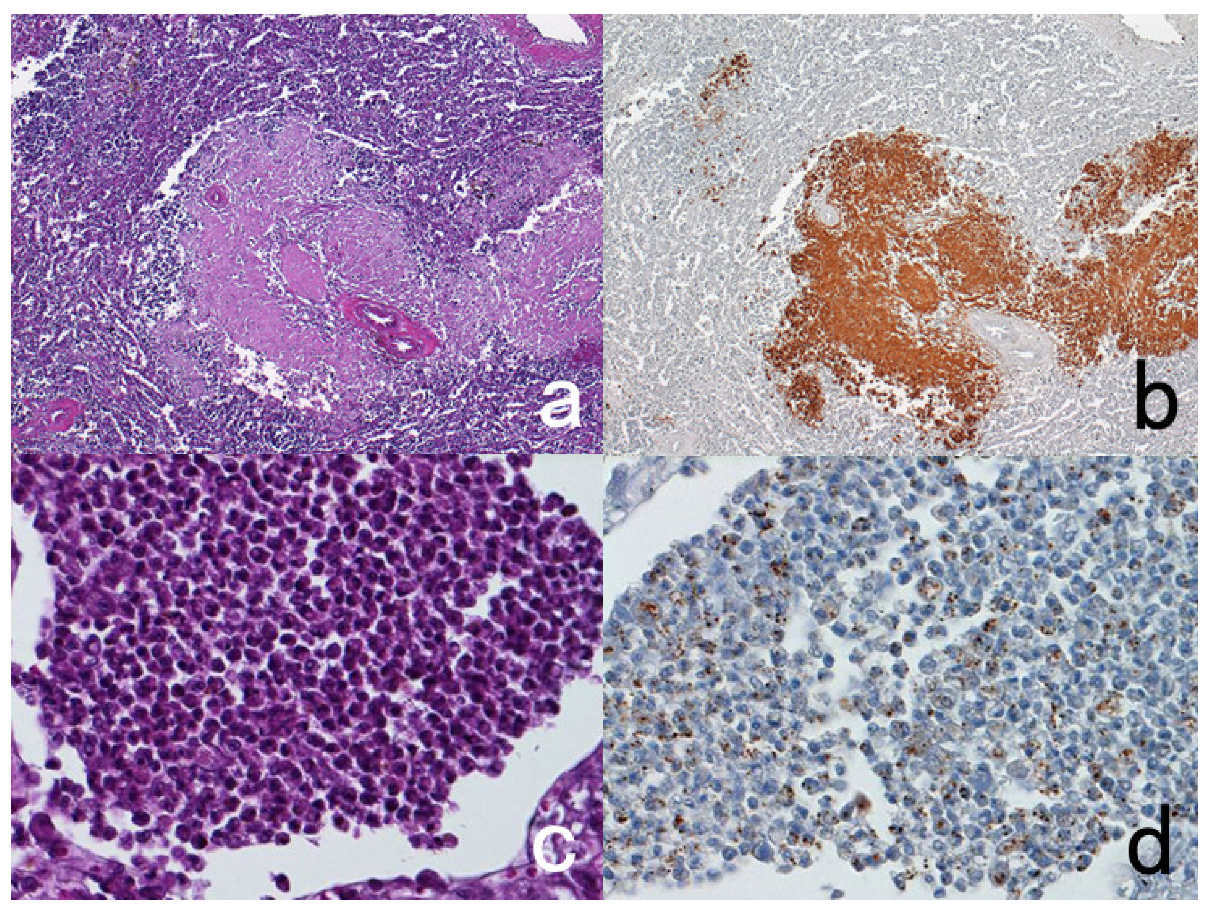
Figure 8.
Demonstration of CD15 and EBER in Hodgkin’s lymphoma in a male patient in his 50s autopsied by Dr. Thomas Hodgkin himself 170 years ago. Top panels: H&E. Only one unstained slide of the liver available was stained with H&E. After photographing, the section was transferred to two silane-coated glass slides (a). Infiltration of Reed-Sternberg cells or Hodgkin’s cells is microscopically recognized (b). Bottom panels: Immunostaining for CD15 (c) and in situ hybridization for EBER (d) gave positive signals on the plasma membrane and in the nucleus, respectively, as indicated by yellow and red arrows.
Figure 8.
Demonstration of CD15 and EBER in Hodgkin’s lymphoma in a male patient in his 50s autopsied by Dr. Thomas Hodgkin himself 170 years ago. Top panels: H&E. Only one unstained slide of the liver available was stained with H&E. After photographing, the section was transferred to two silane-coated glass slides (a). Infiltration of Reed-Sternberg cells or Hodgkin’s cells is microscopically recognized (b). Bottom panels: Immunostaining for CD15 (c) and in situ hybridization for EBER (d) gave positive signals on the plasma membrane and in the nucleus, respectively, as indicated by yellow and red arrows.
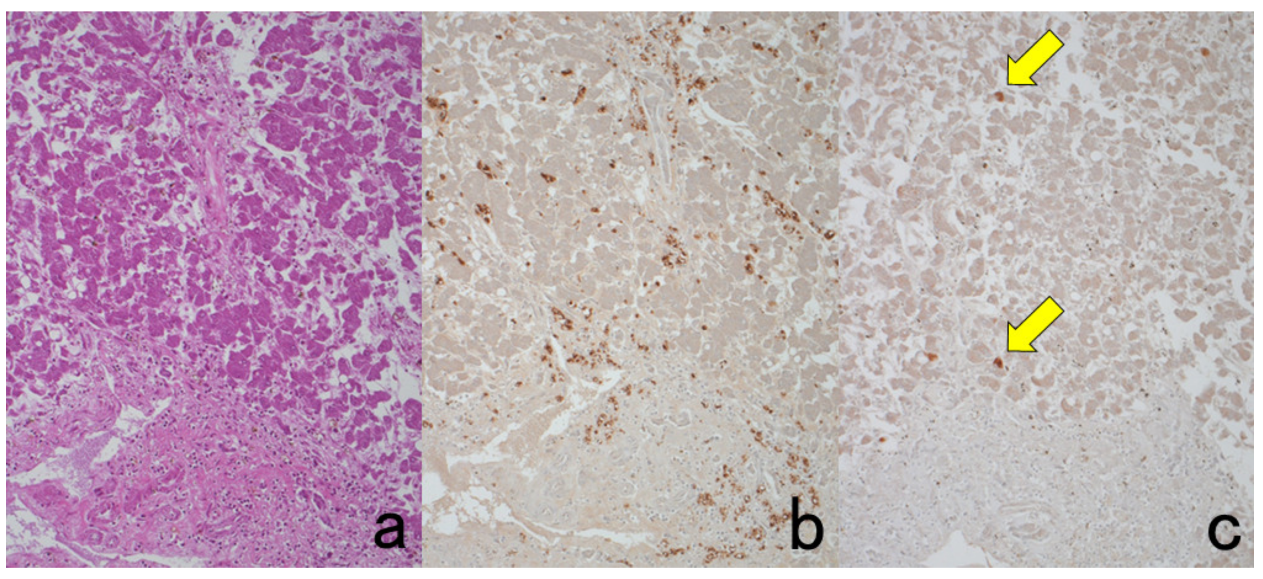
Figure 9.
Demonstration of amyloid A in secondary amyloidosis and pneumococcal antigens in lobar pneumonia in archival material. Top panels (a,b): Splenic white pulp with amyloid A deposition. Bottom panels (c,d): pneumococcal antigens in lobar pneumonia showing diffuse neutrophilic infiltration. Left (a,c): H&E and Right (b,d): chromogenic immunostaining. The specimens were fixed in formalin for 70 years. Deposition of amyloid A protein is evident in the splenic white pulp (no pretreatment needed). Pneumococci phagocytized by neutrophils are visualized immunohistochemically after HIER.
Figure 9.
Demonstration of amyloid A in secondary amyloidosis and pneumococcal antigens in lobar pneumonia in archival material. Top panels (a,b): Splenic white pulp with amyloid A deposition. Bottom panels (c,d): pneumococcal antigens in lobar pneumonia showing diffuse neutrophilic infiltration. Left (a,c): H&E and Right (b,d): chromogenic immunostaining. The specimens were fixed in formalin for 70 years. Deposition of amyloid A protein is evident in the splenic white pulp (no pretreatment needed). Pneumococci phagocytized by neutrophils are visualized immunohistochemically after HIER.
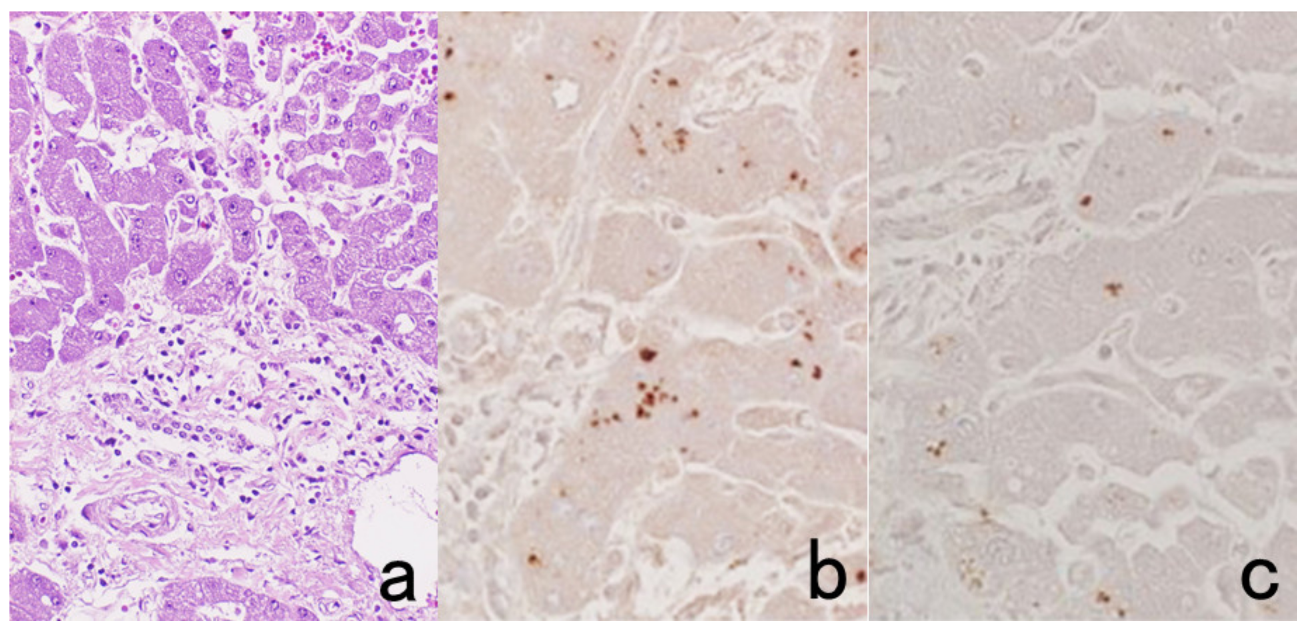
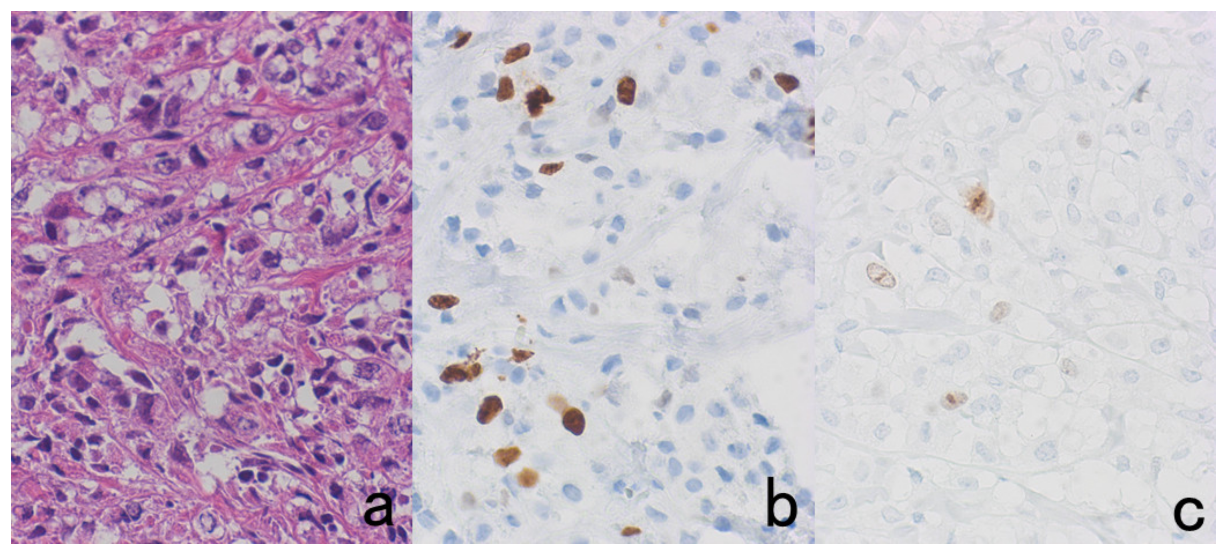
Figure 10.
Demonstration of HCV antigens in an archival liver specimen of chronic hepatitis after HIER. (a): H&E, (b): monoclonal antibody against the NS3 region of HCV and (c): monoclonal antibody against the E1 region. Dot-like immunoreactivity of HCV antigens is seen in the cytoplasm of hepatocytes. The specimen was kept in formalin for 40 years.
Figure 10.
Demonstration of HCV antigens in an archival liver specimen of chronic hepatitis after HIER. (a): H&E, (b): monoclonal antibody against the NS3 region of HCV and (c): monoclonal antibody against the E1 region. Dot-like immunoreactivity of HCV antigens is seen in the cytoplasm of hepatocytes. The specimen was kept in formalin for 40 years.
Figure 11.
Diffusion artifact (I). Hodgkin’s lymphoma. The cytoplasm of Reed-Sternberg cells or Hodgkin’s cells is polyclonally positive for both kappa (a) and lambda (b) chains. The nuclei are negative. This represents an example of diffusion artifact of plasma proteins in FFPE preparations. The nuclei are counterstained with methyl green.
Figure 11.
Diffusion artifact (I). Hodgkin’s lymphoma. The cytoplasm of Reed-Sternberg cells or Hodgkin’s cells is polyclonally positive for both kappa (a) and lambda (b) chains. The nuclei are negative. This represents an example of diffusion artifact of plasma proteins in FFPE preparations. The nuclei are counterstained with methyl green.
Figure 12.
Diffusion artifact (II). Top panels: Albumin (a) and IgG (b) immunoreactivities in hepatocellular carcinoma metastatic to the hepatic hilar lymph node. Bottom panels: IgA immunostaining in normal (c) and neoplastic (d) thyroid. Hepatocellular carcinoma cells, normal thyroid follicular cells, and papillary thyroid carcinoma cells reveal diffuse cytoplasmic staining for the plasma proteins (albumin, IgG, and IgA) in some cells. The nuclei remain negative. The Golgi area of plasma cells is immunoreactive for IgG in panel (b). The nuclei are counterstained with methyl green.
Figure 12.
Diffusion artifact (II). Top panels: Albumin (a) and IgG (b) immunoreactivities in hepatocellular carcinoma metastatic to the hepatic hilar lymph node. Bottom panels: IgA immunostaining in normal (c) and neoplastic (d) thyroid. Hepatocellular carcinoma cells, normal thyroid follicular cells, and papillary thyroid carcinoma cells reveal diffuse cytoplasmic staining for the plasma proteins (albumin, IgG, and IgA) in some cells. The nuclei remain negative. The Golgi area of plasma cells is immunoreactive for IgG in panel (b). The nuclei are counterstained with methyl green.
Figure 13.
Diffusion artifact (III). Albumin immunoreactivity in FFPE autopsied pancreas. Ductular cells (a), acinar cells (b), and islet cells and peripheral nerve (c) show diffuse cytoplasmic staining. The signals are randomly observed in different cells in different parts of the pancreas. The nuclei, counterstained with methyl green, remain negative.
Figure 13.
Diffusion artifact (III). Albumin immunoreactivity in FFPE autopsied pancreas. Ductular cells (a), acinar cells (b), and islet cells and peripheral nerve (c) show diffuse cytoplasmic staining. The signals are randomly observed in different cells in different parts of the pancreas. The nuclei, counterstained with methyl green, remain negative.
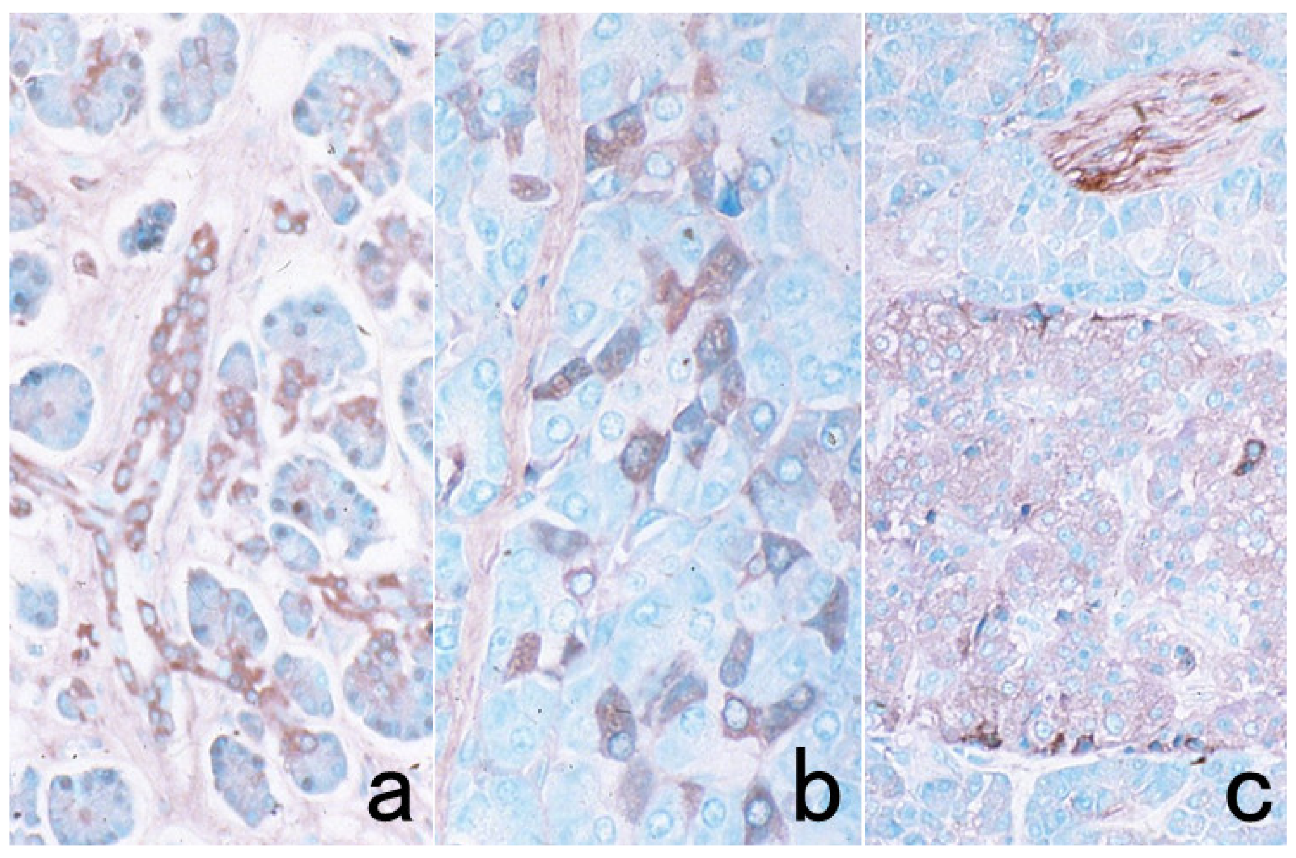
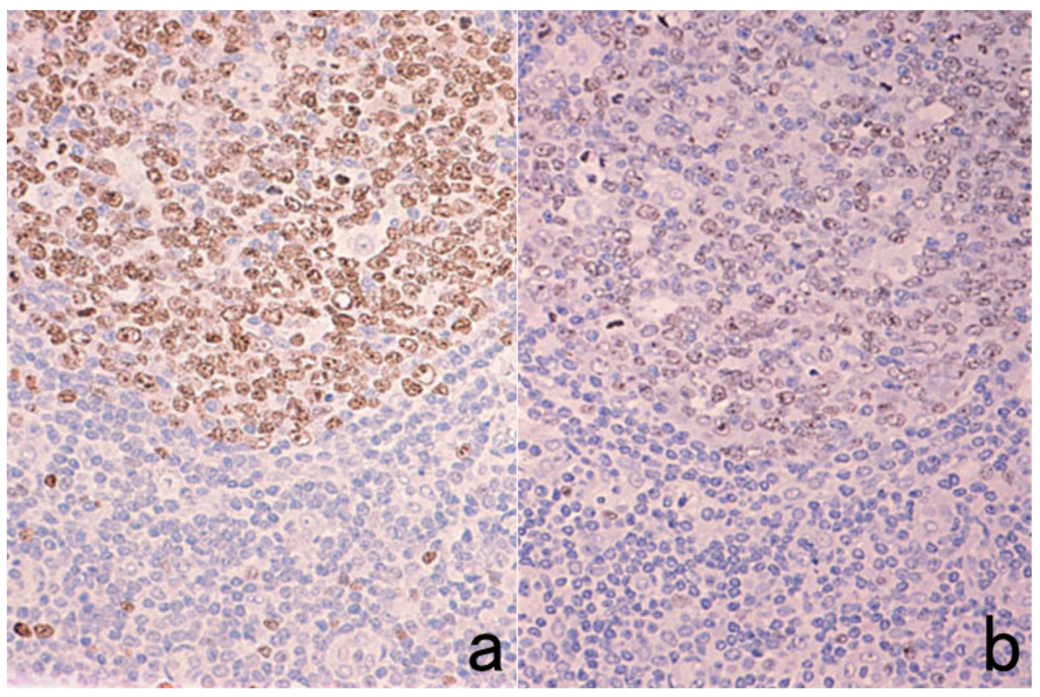
Figure 14.
Vimentin internal control. Diffuse large B-cell lymphoma. (a): Vimentin and (b): CD20. The poorly fixed central part (representing the lower half of the panels) is false negative for both vimentin and CD20. The expression of lymphocyte surface markers should be judged based on the positivity in the appropriately fixed peripheral area (the upper half of the panels).
Figure 14.
Vimentin internal control. Diffuse large B-cell lymphoma. (a): Vimentin and (b): CD20. The poorly fixed central part (representing the lower half of the panels) is false negative for both vimentin and CD20. The expression of lymphocyte surface markers should be judged based on the positivity in the appropriately fixed peripheral area (the upper half of the panels).
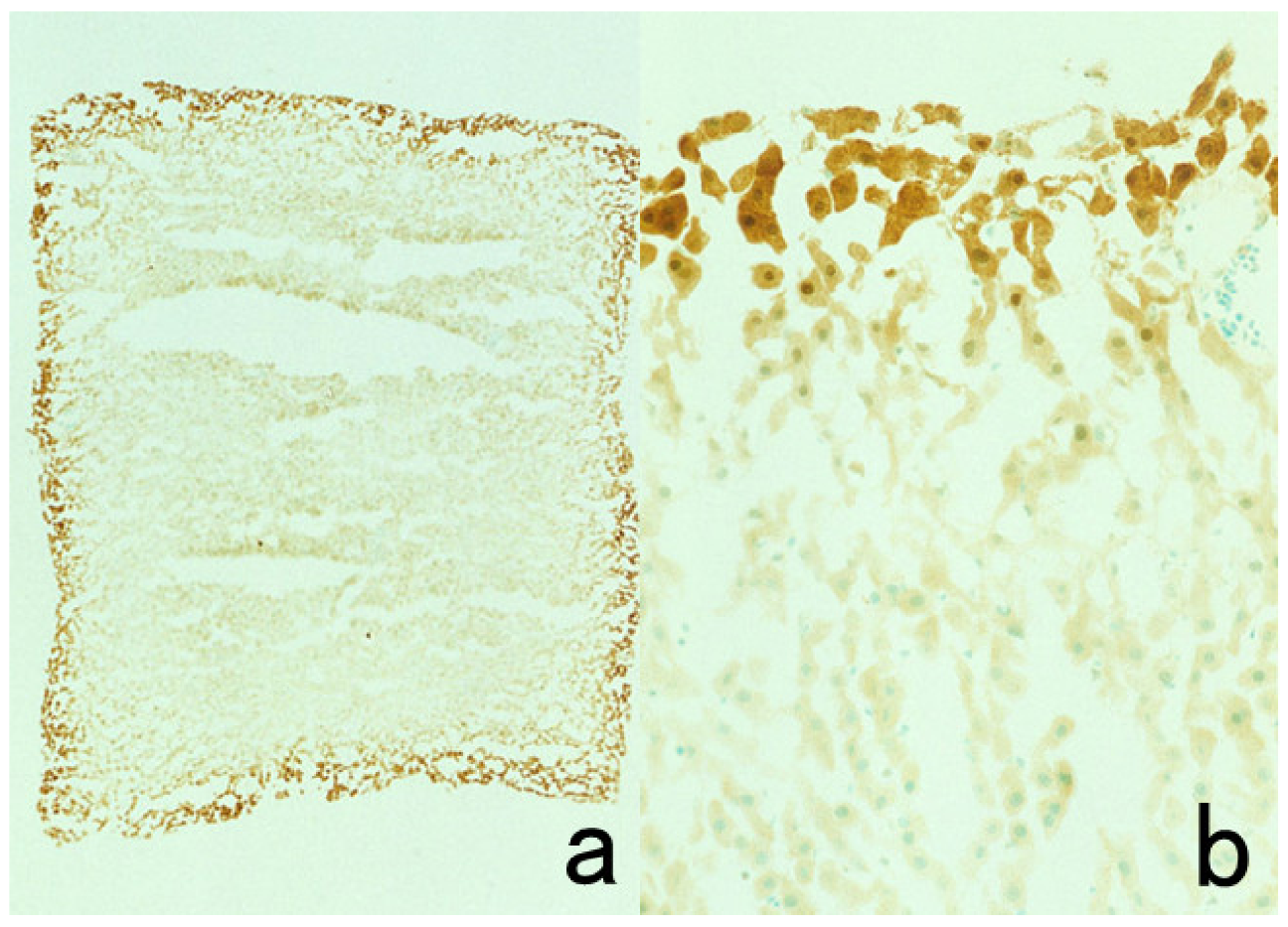
Figure 15.
Glutathione peroxidase immunostaining using a frozen section prepared from 4% paraformaldehyde-fixed rat liver tissue (a): low power, (b): high power. Positive immunoreactivity in the cytoplasm and nucleus of the hepatocytes is seen just at the outermost part of the section.
Figure 15.
Glutathione peroxidase immunostaining using a frozen section prepared from 4% paraformaldehyde-fixed rat liver tissue (a): low power, (b): high power. Positive immunoreactivity in the cytoplasm and nucleus of the hepatocytes is seen just at the outermost part of the section.
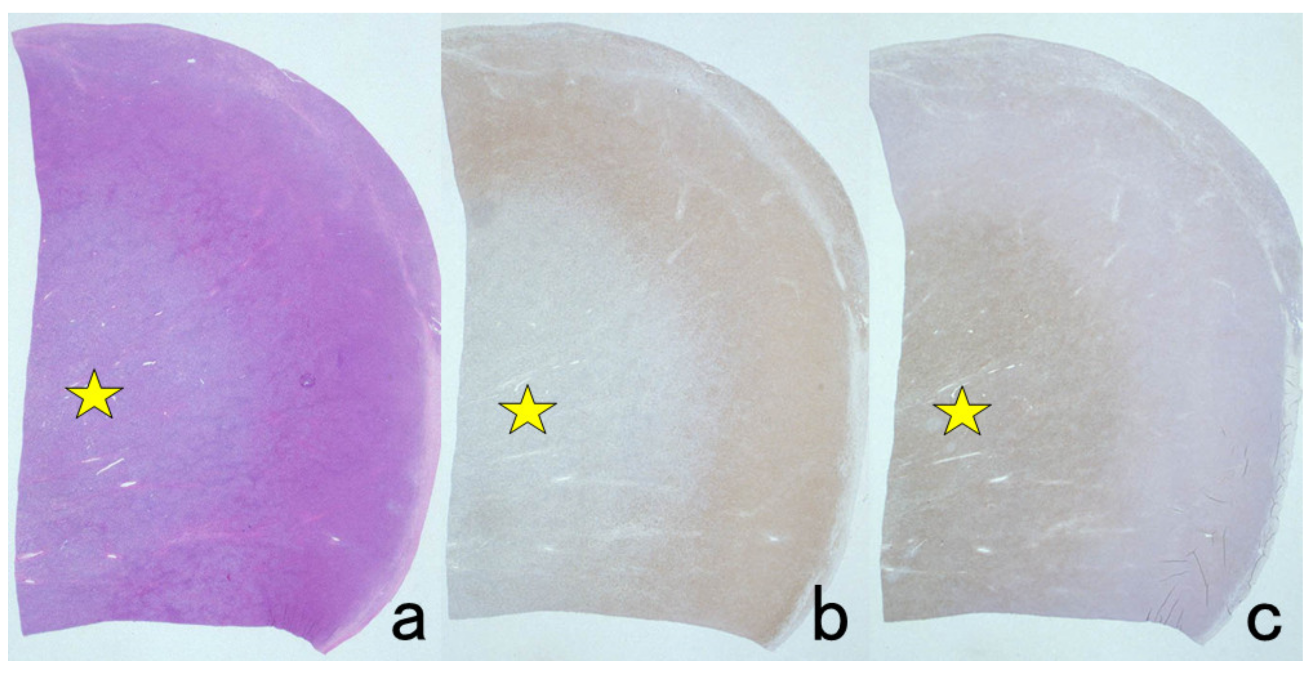
Figure 16.
Paradoxical localization of CD45 and vimentin in FFPE malignant lymphoma tissue. (a): H&E, (b): vimentin and (c): CD45 (leukocyte common antigen: LCA). Vimentin is positive in the peripheral zone but negative in the poorly fixed central area (stars). A reversed pattern is recognizable for CD45 localization. The over-fixed outer zone is negative for CD45.
Figure 16.
Paradoxical localization of CD45 and vimentin in FFPE malignant lymphoma tissue. (a): H&E, (b): vimentin and (c): CD45 (leukocyte common antigen: LCA). Vimentin is positive in the peripheral zone but negative in the poorly fixed central area (stars). A reversed pattern is recognizable for CD45 localization. The over-fixed outer zone is negative for CD45.
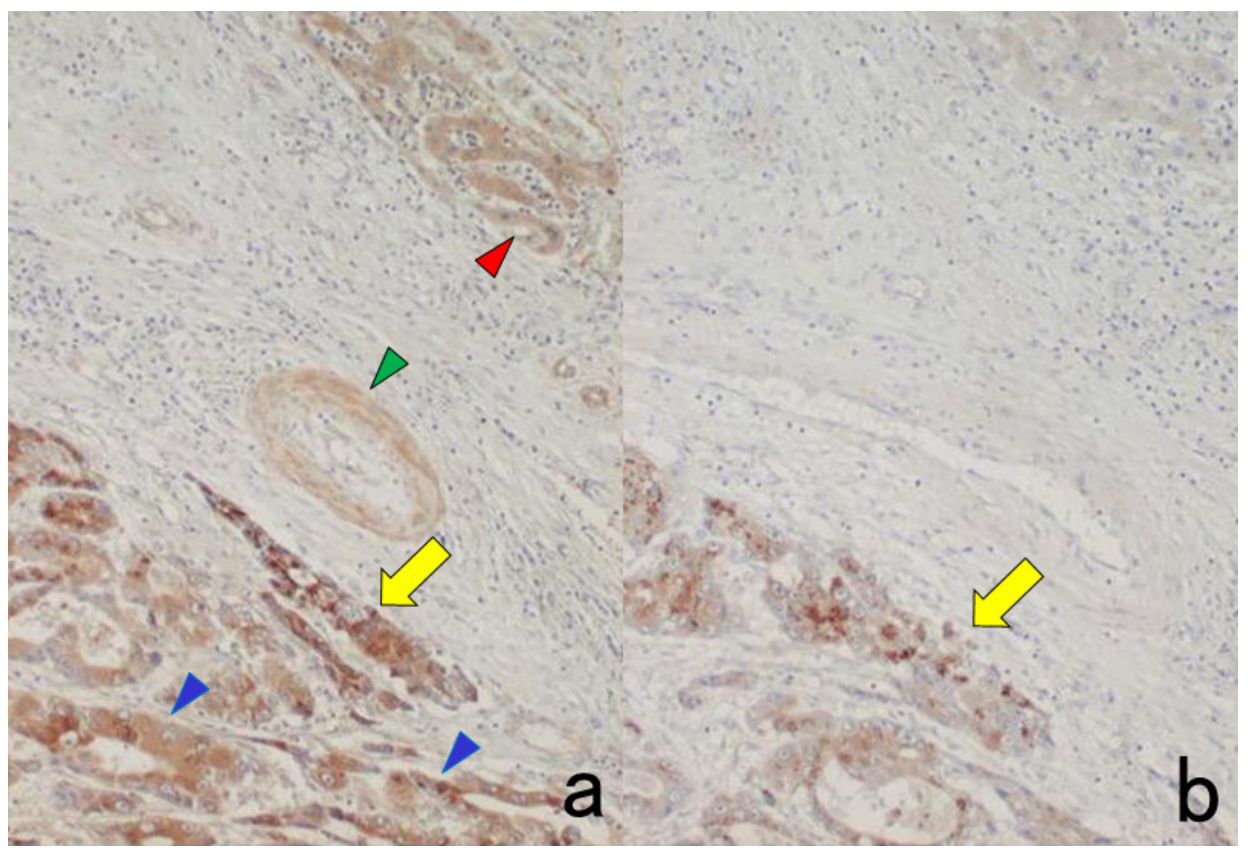
Figure 17.
The need for appropriate dilution of the primary rabbit antiserum. Alpha-fetoprotein (AFP) immunostaining (using the polymer method) for hepatocellular carcinoma. (a): 1:400 dilution, (b): 1:3200 dilution. With 1:400 diluted antiserum, non-neoplastic hepatocytes (blue arrowheads), bile ducts (red arrowhead) and arterial wall (green arrowhead) reveal nonspecific staining. At an appropriate dilution (1:3200), positive signals of AFP are seen only in the hepatoma cells (yellow arrows).
Figure 17.
The need for appropriate dilution of the primary rabbit antiserum. Alpha-fetoprotein (AFP) immunostaining (using the polymer method) for hepatocellular carcinoma. (a): 1:400 dilution, (b): 1:3200 dilution. With 1:400 diluted antiserum, non-neoplastic hepatocytes (blue arrowheads), bile ducts (red arrowhead) and arterial wall (green arrowhead) reveal nonspecific staining. At an appropriate dilution (1:3200), positive signals of AFP are seen only in the hepatoma cells (yellow arrows).
Figure 18.
Antigenic loss of surface markers by endogenous peroxidase blockage in fresh-frozen sections. Aspirated bone marrow clot of essential thrombocythemia. Immunostaining for glycoprotein IIb/IIIa (CD41/CD61), a megakaryocytic marker. (a): Without endogenous peroxidase blockage and (b): with endogenous peroxidase blockage, inset: H&E. Endogenous peroxidase blockage in 0.3% hydrogen peroxide in methanol significantly hampers the immunoreactivity. The nuclei are counterstained with methyl green.
Figure 18.
Antigenic loss of surface markers by endogenous peroxidase blockage in fresh-frozen sections. Aspirated bone marrow clot of essential thrombocythemia. Immunostaining for glycoprotein IIb/IIIa (CD41/CD61), a megakaryocytic marker. (a): Without endogenous peroxidase blockage and (b): with endogenous peroxidase blockage, inset: H&E. Endogenous peroxidase blockage in 0.3% hydrogen peroxide in methanol significantly hampers the immunoreactivity. The nuclei are counterstained with methyl green.
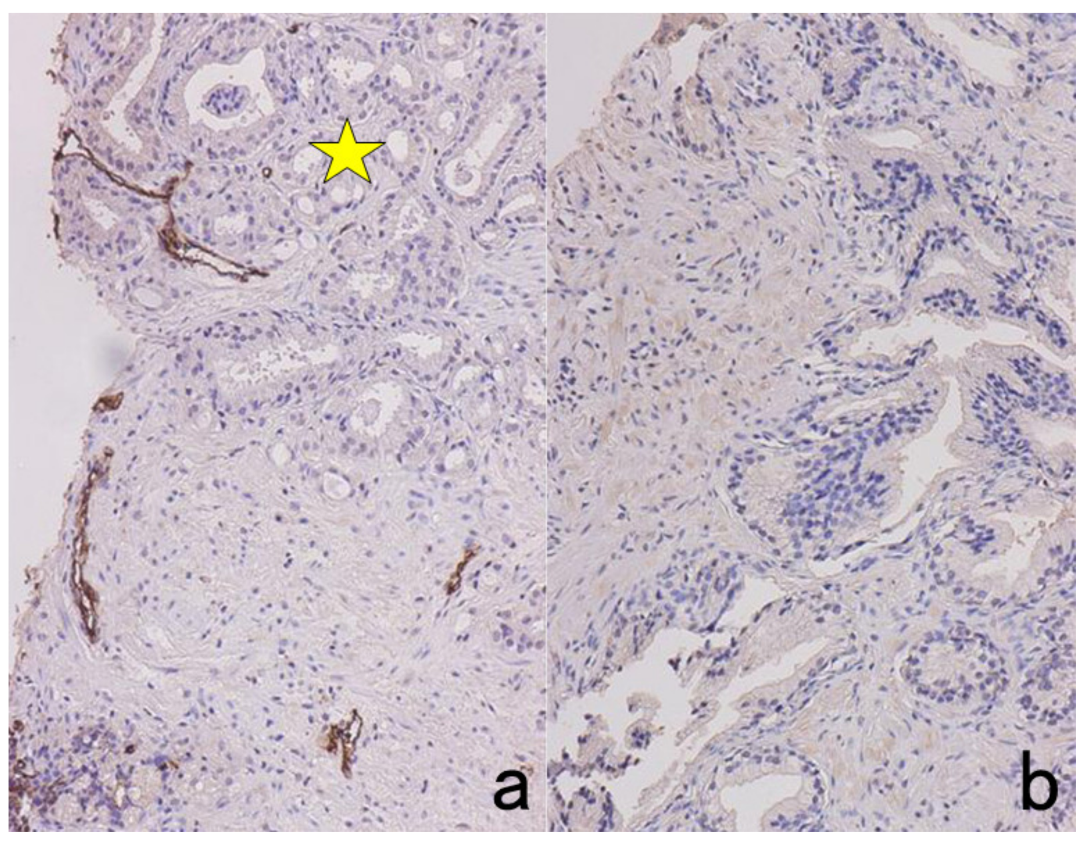
Figure 19.
Retrieval of endogenous biotin activity by heating pretreatment (LSAB immunostaining for villin in the normal kidney with pressure pan heating in 10 mM citrate buffer, pH 6 (a), 10 mM citrate buffer, pH 7 (b) and 10 mM citrate buffer, pH 7, without primary antibody (c). The brush border of proximal renal tubules is immunoreactive for villin. Hydrated heating in citrate buffer, pH 7, enhances retrieval of endogenous biotin activity, as typically represented in panel (c). Coarse granular (mitochondrial) positivity is observed in the cytoplasm. Stars indicate a glomerulus.
Figure 19.
Retrieval of endogenous biotin activity by heating pretreatment (LSAB immunostaining for villin in the normal kidney with pressure pan heating in 10 mM citrate buffer, pH 6 (a), 10 mM citrate buffer, pH 7 (b) and 10 mM citrate buffer, pH 7, without primary antibody (c). The brush border of proximal renal tubules is immunoreactive for villin. Hydrated heating in citrate buffer, pH 7, enhances retrieval of endogenous biotin activity, as typically represented in panel (c). Coarse granular (mitochondrial) positivity is observed in the cytoplasm. Stars indicate a glomerulus.
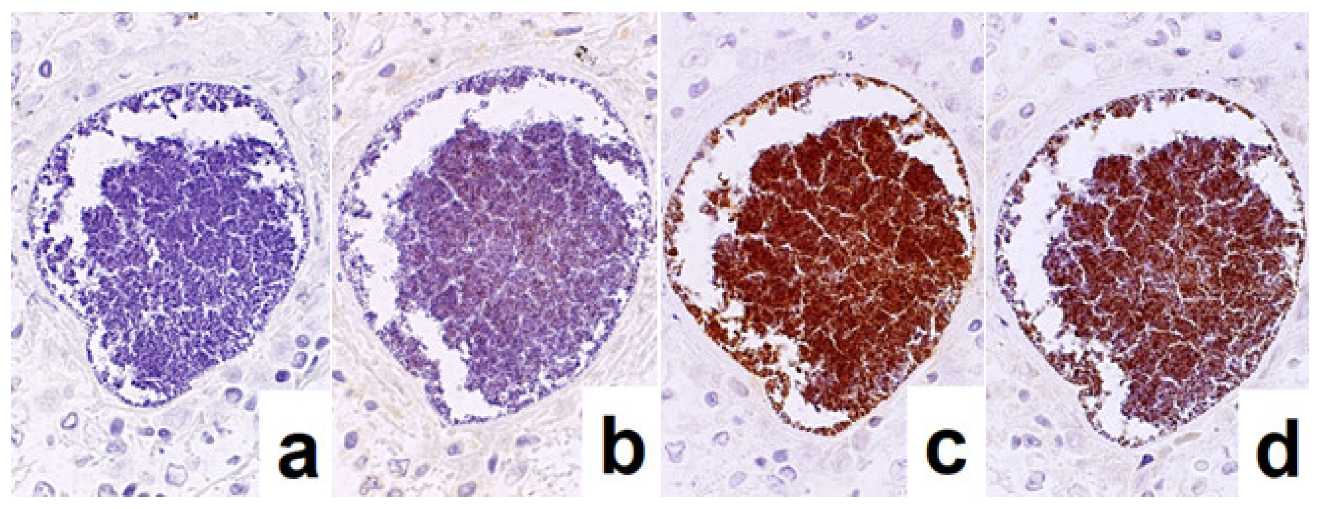
Figure 20.
Retrieval of protein A activity on methicillin-resistant Staphylococcus aureus (MRSA) by heating pretreatment in 1 mM EDTA, pH 8. MRSA infection in the lung. (a): Without primary antibody (negative control), (b): incubation with rabbit antibody, F(ab’)2 fragments, against mouse immunoglobulins, (c): incubation with rabbit antibody, whole IgG, against mouse immunoglobulins and (d): incubation with mouse monoclonal antibody against Pseudomonas aeruginosa as an indifferent antibody. It is evident that the MRSA colony in the lung binds to rabbit and mouse IgG, as shown in panels c and d, respectively. The F(ab’)2 fragments of IgG lack this binding (b), so the nonspecific binding is caused through the Fc portion of IgG.
Figure 20.
Retrieval of protein A activity on methicillin-resistant Staphylococcus aureus (MRSA) by heating pretreatment in 1 mM EDTA, pH 8. MRSA infection in the lung. (a): Without primary antibody (negative control), (b): incubation with rabbit antibody, F(ab’)2 fragments, against mouse immunoglobulins, (c): incubation with rabbit antibody, whole IgG, against mouse immunoglobulins and (d): incubation with mouse monoclonal antibody against Pseudomonas aeruginosa as an indifferent antibody. It is evident that the MRSA colony in the lung binds to rabbit and mouse IgG, as shown in panels c and d, respectively. The F(ab’)2 fragments of IgG lack this binding (b), so the nonspecific binding is caused through the Fc portion of IgG.
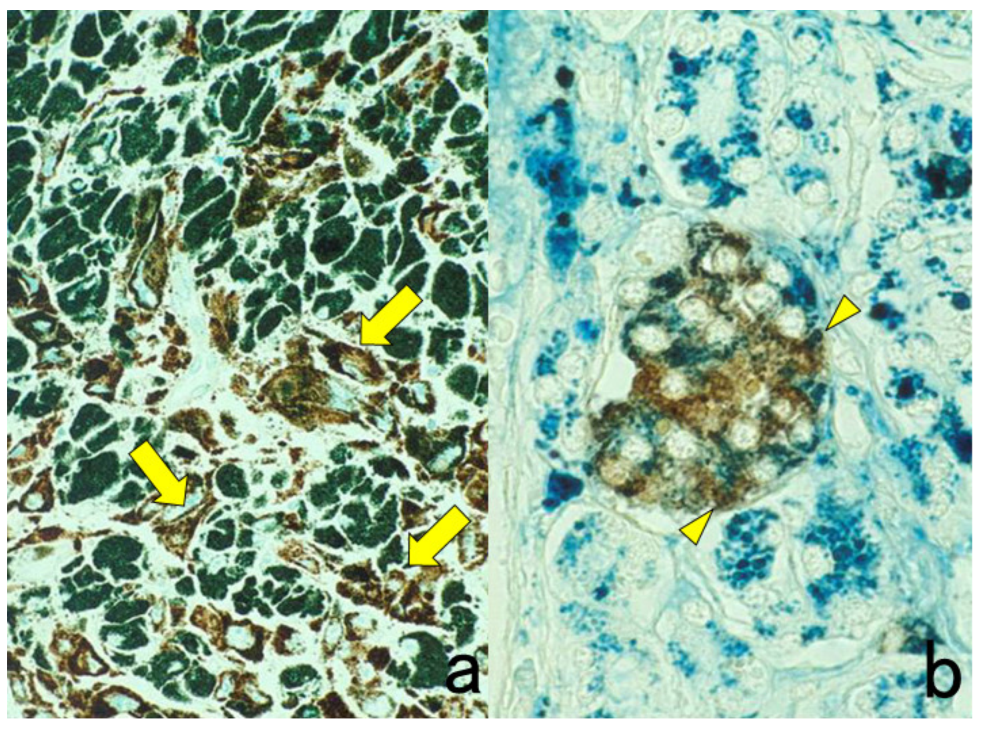
Figure 21.
Metachromasia of melanin by methyl green counterstaining in heavily pigmented nasal malignant melanoma (a) immunostaining for HMB45 and Berlin blue counterstaining for hemosiderin in pancreatic hemochromatosis (b) immunostaining for insulin. Brown-colored pigments such as melanin and hemosiderin hamper the judgment of DAB coloration. Counterstaining with methyl green and Berlin blue is quite effective for distinguishing the DAB color from the endogenous pigments. The rich distribution of HMB45-negative metachromatic melanophages is noted in panel (a). Arrows indicate HMB45-positive melanoma cells. In panel (b), hemosiderin deposition is observed in insulin-positive β-cells of the pancreatic islet (arrowheads).
Figure 21.
Metachromasia of melanin by methyl green counterstaining in heavily pigmented nasal malignant melanoma (a) immunostaining for HMB45 and Berlin blue counterstaining for hemosiderin in pancreatic hemochromatosis (b) immunostaining for insulin. Brown-colored pigments such as melanin and hemosiderin hamper the judgment of DAB coloration. Counterstaining with methyl green and Berlin blue is quite effective for distinguishing the DAB color from the endogenous pigments. The rich distribution of HMB45-negative metachromatic melanophages is noted in panel (a). Arrows indicate HMB45-positive melanoma cells. In panel (b), hemosiderin deposition is observed in insulin-positive β-cells of the pancreatic islet (arrowheads).
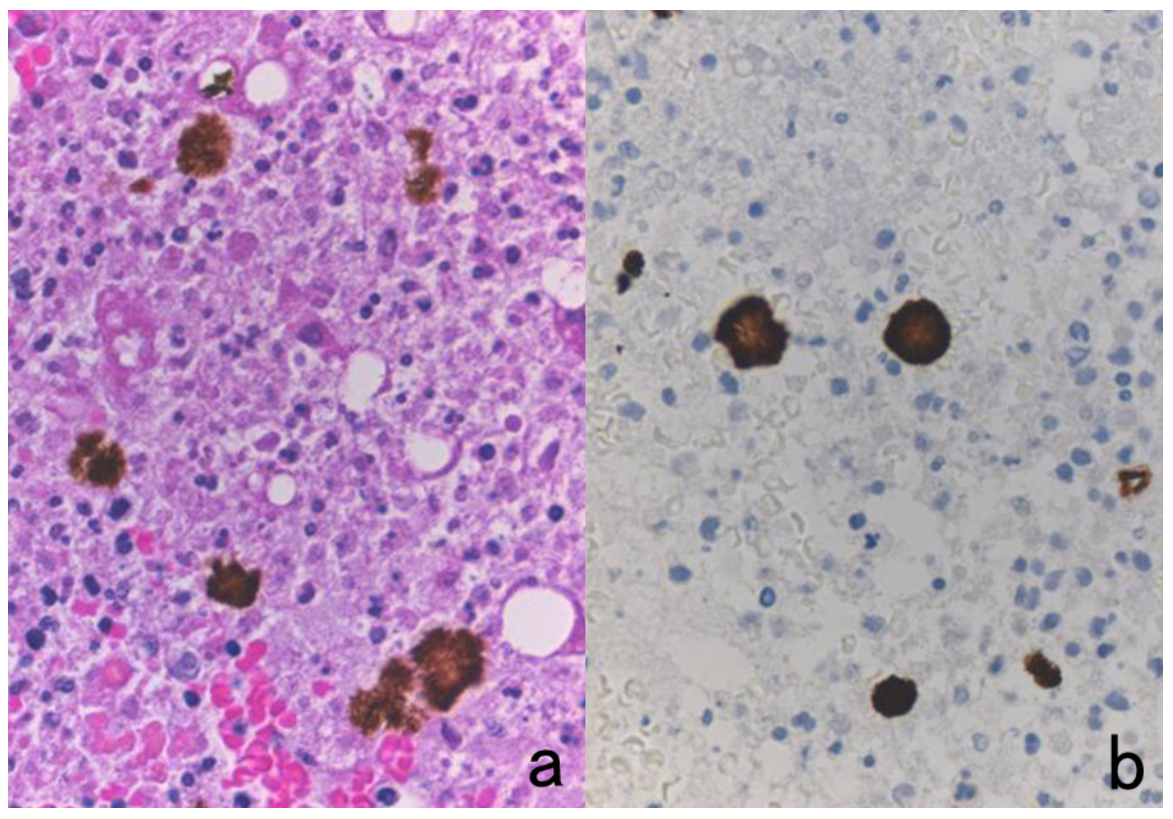
Figure 22.
Concentrated bile pigments in a cell block preparation of liver abscess clinically suspected of being amebic infection. (a): H&E and (b): immunostaining using a monoclonal antibody EHK153 against Entamoeba histolytica. Brown-colored structures of concentrated bile pigments somewhat resemble strongly immunoreactive amebic trophozoites. The entamoeba antigen must be judged as negative in this case. Careful comparison with H&E histology is needed to avoid falsely judging these as positive immunohistochemical signals.
Figure 22.
Concentrated bile pigments in a cell block preparation of liver abscess clinically suspected of being amebic infection. (a): H&E and (b): immunostaining using a monoclonal antibody EHK153 against Entamoeba histolytica. Brown-colored structures of concentrated bile pigments somewhat resemble strongly immunoreactive amebic trophozoites. The entamoeba antigen must be judged as negative in this case. Careful comparison with H&E histology is needed to avoid falsely judging these as positive immunohistochemical signals.
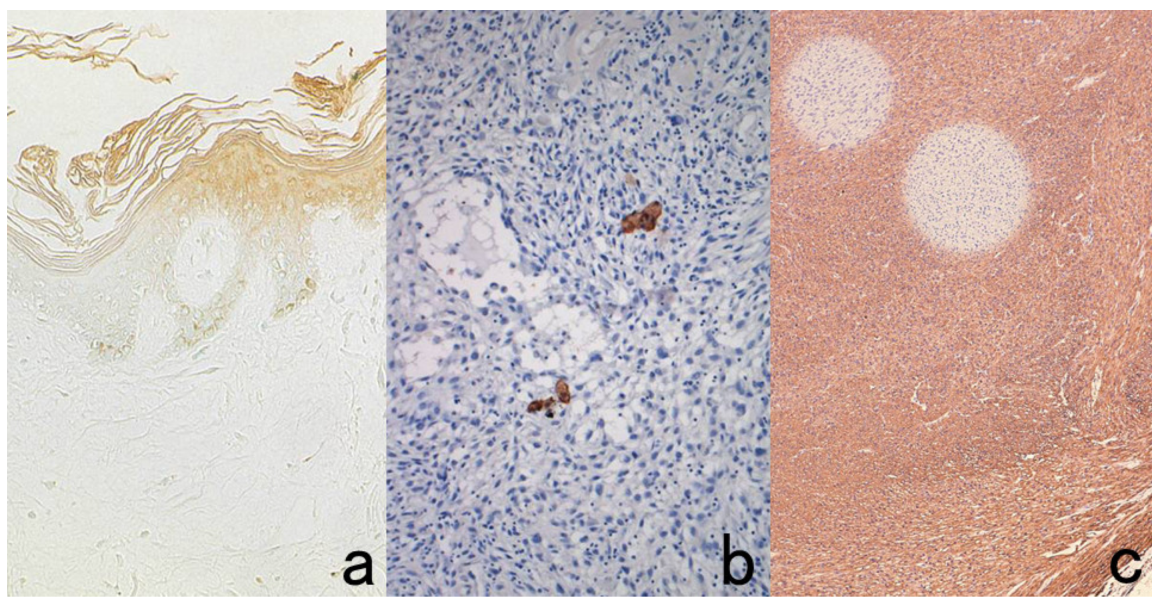
Figure 23.
Technical artifacts. Effects of drying. (a): surfactant apoprotein immunostaining for the skins, contamination of cytokeratin-positive scales. (b): cytokeratin immunostaining for spindle cell sarcoma and insufficient deparaffinization (c): smooth muscle actin immunostaining for leiomyosarcoma. Drying of sections during antibody incubation causes nonspecific binding in the dried area (a). Contaminated cytokeratin-positive scales on the section should be distinguished from true positivity (b). False-negative rounded areas result from insufficient deparaffinization. (c).
Figure 23.
Technical artifacts. Effects of drying. (a): surfactant apoprotein immunostaining for the skins, contamination of cytokeratin-positive scales. (b): cytokeratin immunostaining for spindle cell sarcoma and insufficient deparaffinization (c): smooth muscle actin immunostaining for leiomyosarcoma. Drying of sections during antibody incubation causes nonspecific binding in the dried area (a). Contaminated cytokeratin-positive scales on the section should be distinguished from true positivity (b). False-negative rounded areas result from insufficient deparaffinization. (c).
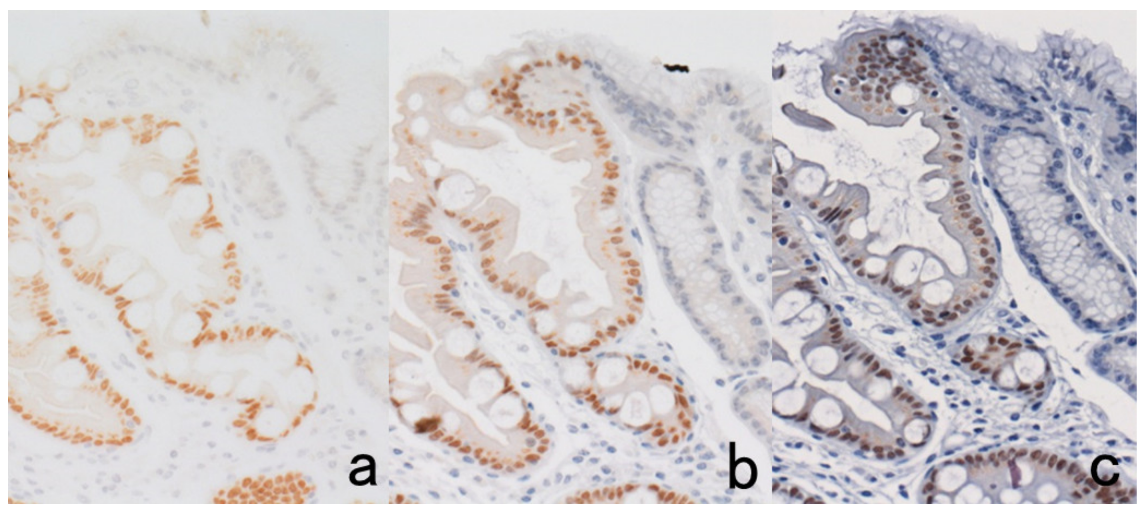
Figure 24.
Effect of prolonged storage of unstained sections (HIER-assisted ER immunostaining for breast cancer). Immunostaining just after cutting (a) and immunostaining after prolonged storage for 6 months in a −20 °C freezer (b) or at room temperature. (c). The prolonged storage at room temperature severely deteriorates the immunoreactivity of nuclear antigens such as ER. Storage in a freezer is effective for avoiding such false negativity.
Figure 24.
Effect of prolonged storage of unstained sections (HIER-assisted ER immunostaining for breast cancer). Immunostaining just after cutting (a) and immunostaining after prolonged storage for 6 months in a −20 °C freezer (b) or at room temperature. (c). The prolonged storage at room temperature severely deteriorates the immunoreactivity of nuclear antigens such as ER. Storage in a freezer is effective for avoiding such false negativity.
Figure 25.
Antigenic loss by stretching sections on a hot plate. Immunostaining for glutathione-S-transferase (GST)-π in the normal liver after stretching on a hot plate at 50 °C for 10 s (a) and at 70 °C for 3 s (b). The cytoplasmic immunoreactivity of GST-π in the bile duct cells is completely lost by high-temperature stretching at 70 °C for even a very short period.
Figure 25.
Antigenic loss by stretching sections on a hot plate. Immunostaining for glutathione-S-transferase (GST)-π in the normal liver after stretching on a hot plate at 50 °C for 10 s (a) and at 70 °C for 3 s (b). The cytoplasmic immunoreactivity of GST-π in the bile duct cells is completely lost by high-temperature stretching at 70 °C for even a very short period.
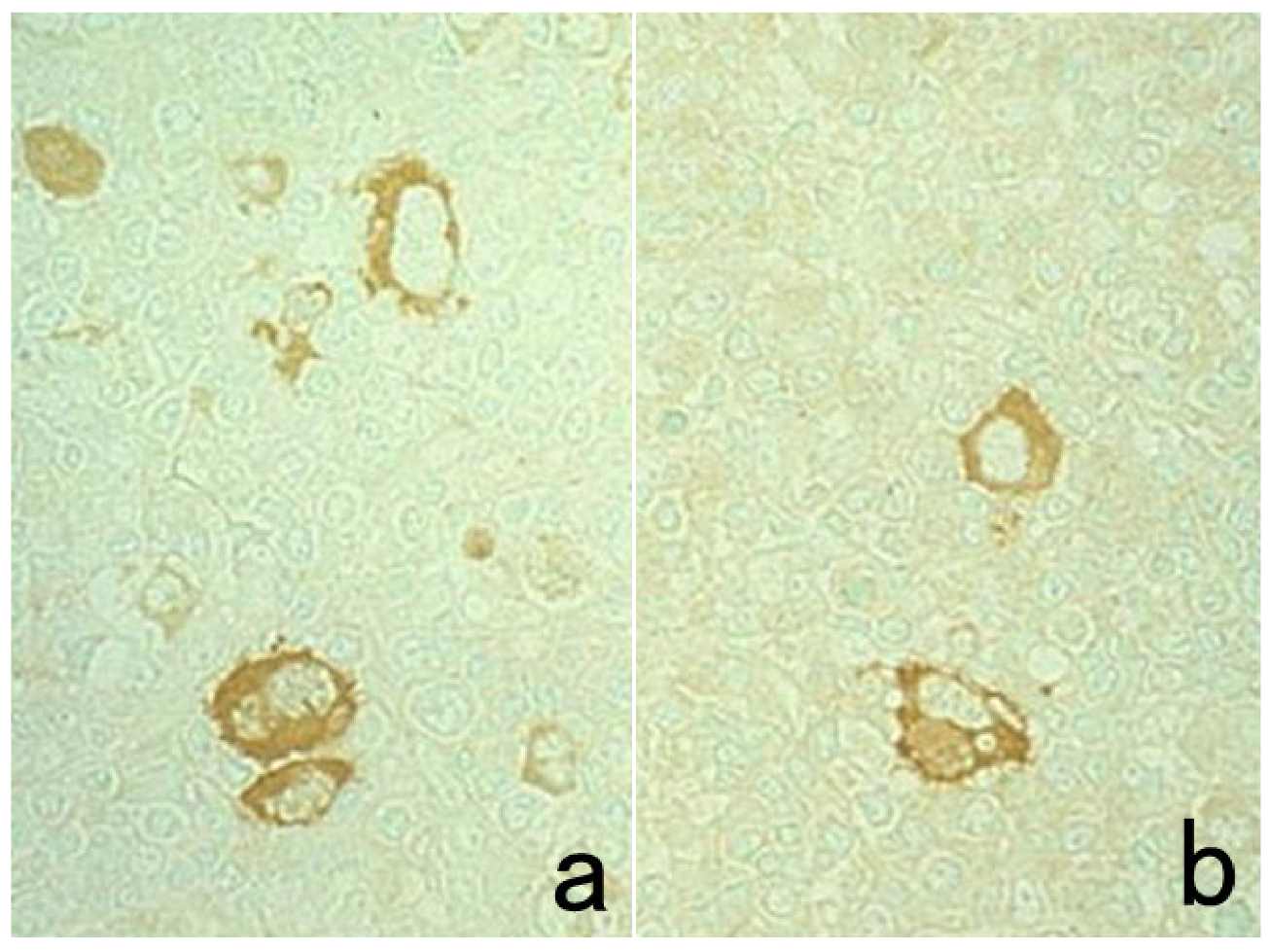
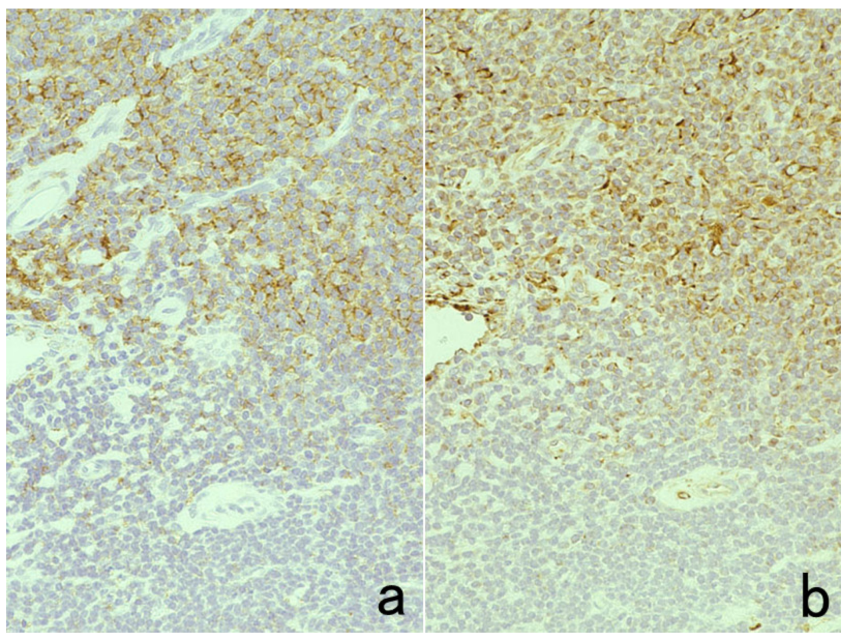
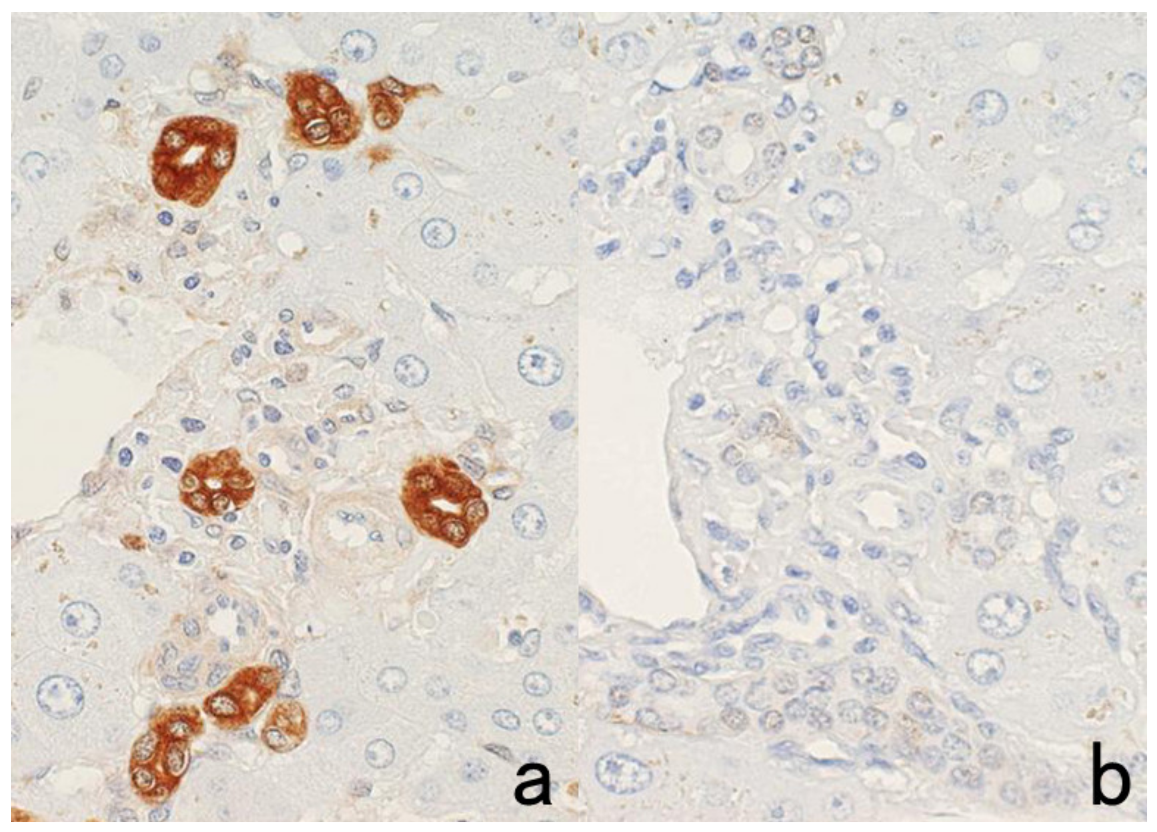
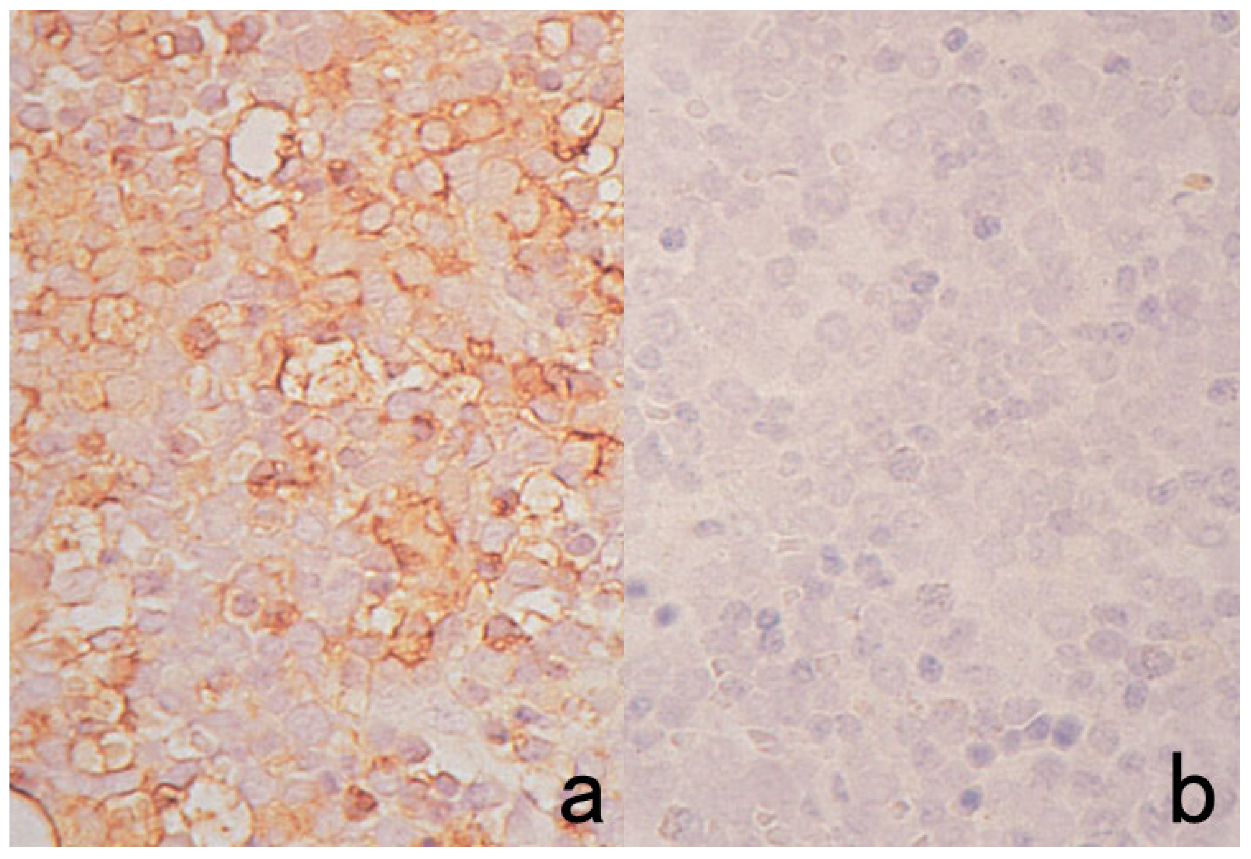
Figure 26.
Weakened HER2 immunoreactivity in breast cancer cells by prolonged drying of unstained sections. Drying in an incubator at 40 °C for 1 h (a) and for 3 days (b). The intensity of HER2 immunostaining is considerably weakened after prolonged drying in an incubator over a weekend.
Figure 26.
Weakened HER2 immunoreactivity in breast cancer cells by prolonged drying of unstained sections. Drying in an incubator at 40 °C for 1 h (a) and for 3 days (b). The intensity of HER2 immunostaining is considerably weakened after prolonged drying in an incubator over a weekend.
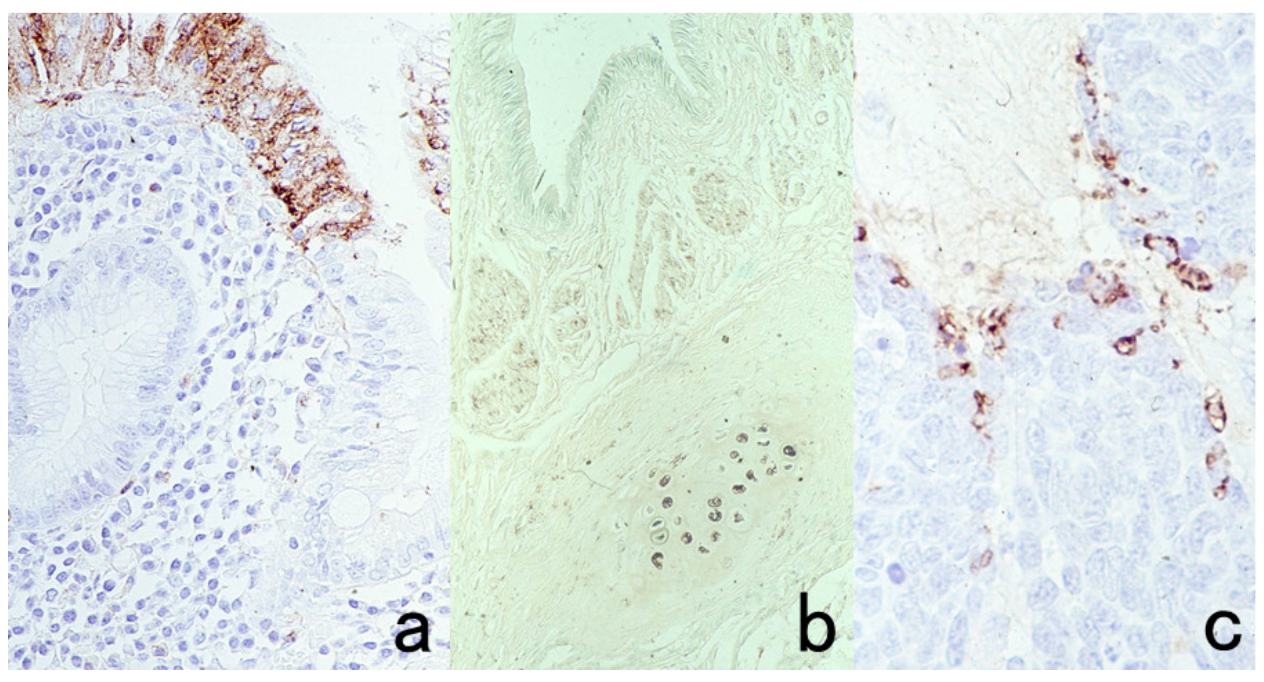
Figure 27.
Loss of Ki-67 immunoreactivity in breast cancer (with foci of dystrophic calcification) by surface decalcification with 5% trichloroacetic acid for 1 h. (a): H&E, (b): Immunostaining without surface decalcification and (c): Immunostaining after surface decalcification with trichloroacetic acid. Surface decalcification significantly deteriorates Ki-67 immunoreactivity.
Figure 27.
Loss of Ki-67 immunoreactivity in breast cancer (with foci of dystrophic calcification) by surface decalcification with 5% trichloroacetic acid for 1 h. (a): H&E, (b): Immunostaining without surface decalcification and (c): Immunostaining after surface decalcification with trichloroacetic acid. Surface decalcification significantly deteriorates Ki-67 immunoreactivity.
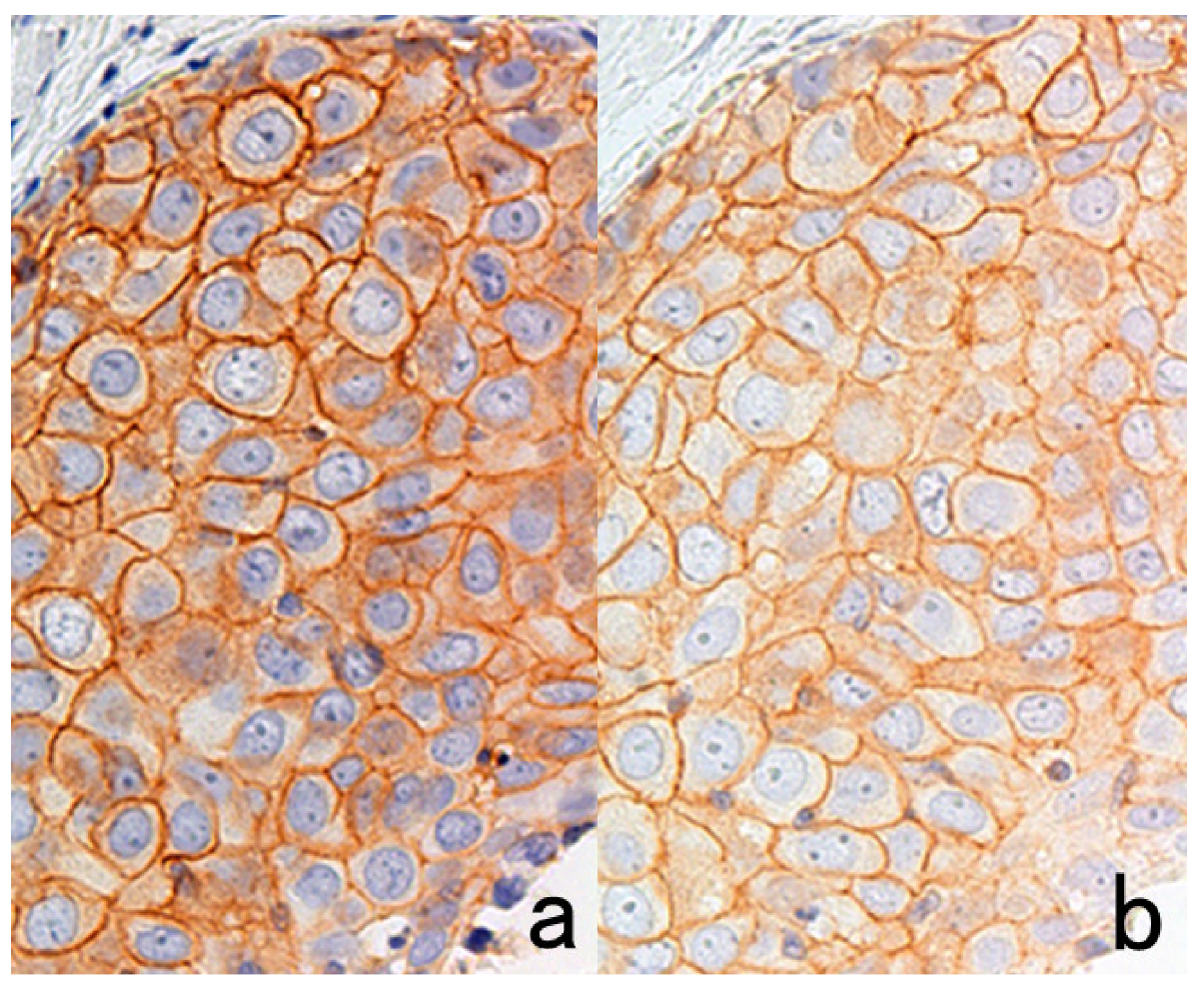
Figure 28.
PharmDxTM for EGFR immunostaining in colonic adenocarcinoma. The kit supplied from Agilent/Dako provides faint immunoreactivity (a), which may affect appropriate judgment. However, when replacing EnVision (as the secondary reagent) with CSA-II (available from the same company), very strong EGFR immunoreactivity can be observed (b).
Figure 28.
PharmDxTM for EGFR immunostaining in colonic adenocarcinoma. The kit supplied from Agilent/Dako provides faint immunoreactivity (a), which may affect appropriate judgment. However, when replacing EnVision (as the secondary reagent) with CSA-II (available from the same company), very strong EGFR immunoreactivity can be observed (b).
Figure 29.
Paradoxical weakening of the antigenicity in CSA-II-mediated chromogenic immunostaining when the primary antibody concentration is high. CD4 immunostaining of the pharyngeal tonsil after HIER using CD4 monoclonal antibody diluted at 1:500 (a) and 1:50 (b). Equivocal CD4 staining on the plasma membrane with a high background occurs when the primary antibody concentration is 10 times higher. The background staining was caused by artificial diffusion of the membrane antigen into the cytoplasm.
Figure 29.
Paradoxical weakening of the antigenicity in CSA-II-mediated chromogenic immunostaining when the primary antibody concentration is high. CD4 immunostaining of the pharyngeal tonsil after HIER using CD4 monoclonal antibody diluted at 1:500 (a) and 1:50 (b). Equivocal CD4 staining on the plasma membrane with a high background occurs when the primary antibody concentration is 10 times higher. The background staining was caused by artificial diffusion of the membrane antigen into the cytoplasm.
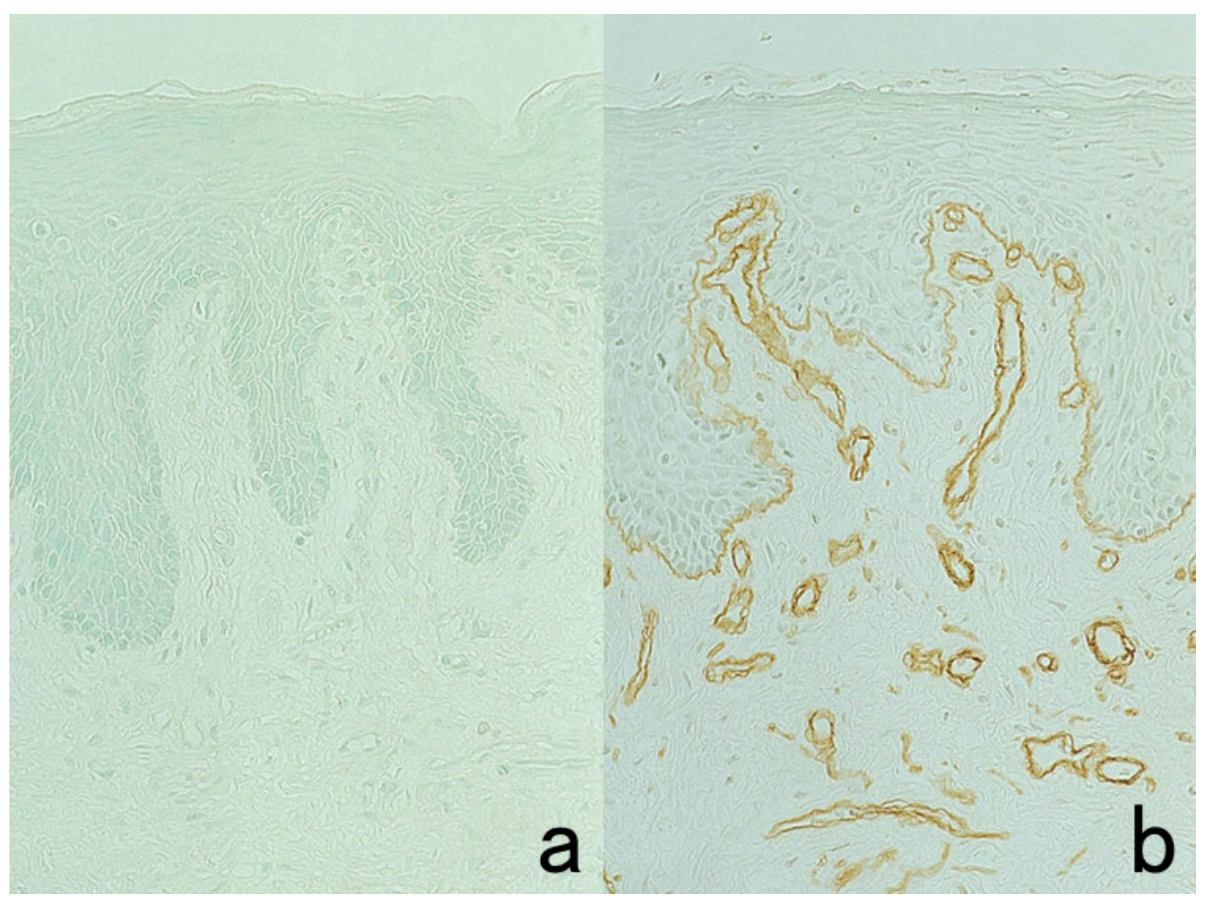
Figure 30.
Effect of trypsin digestion in immunostaining for type 4 collagen in the normal skin. (a): Immunostaining without treatment and (b): after 0.1% trypsin digestion at 37 °C for 30 min. Type 4 collagen immunoreactivity in the basement membrane is clearly visualized after trypsin digestion. The nuclei are counterstained with methyl green.
Figure 30.
Effect of trypsin digestion in immunostaining for type 4 collagen in the normal skin. (a): Immunostaining without treatment and (b): after 0.1% trypsin digestion at 37 °C for 30 min. Type 4 collagen immunoreactivity in the basement membrane is clearly visualized after trypsin digestion. The nuclei are counterstained with methyl green.
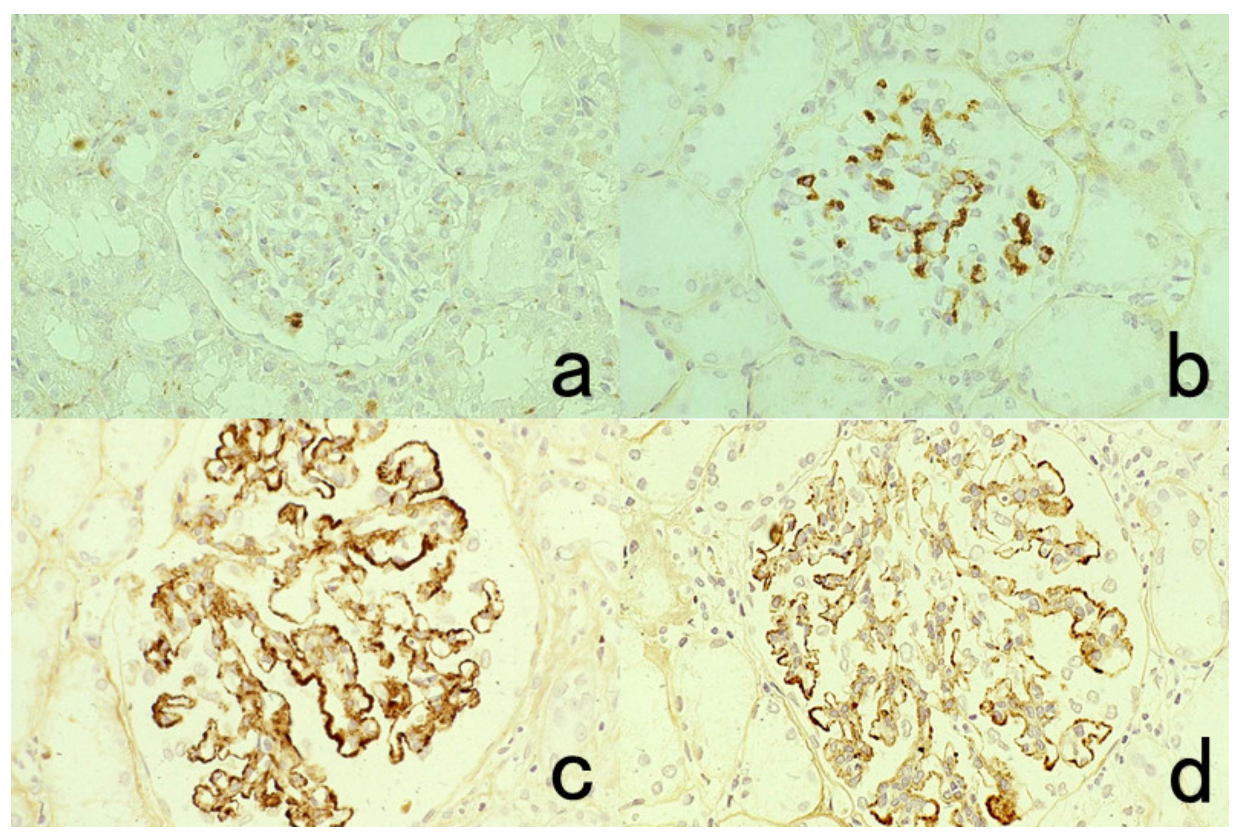
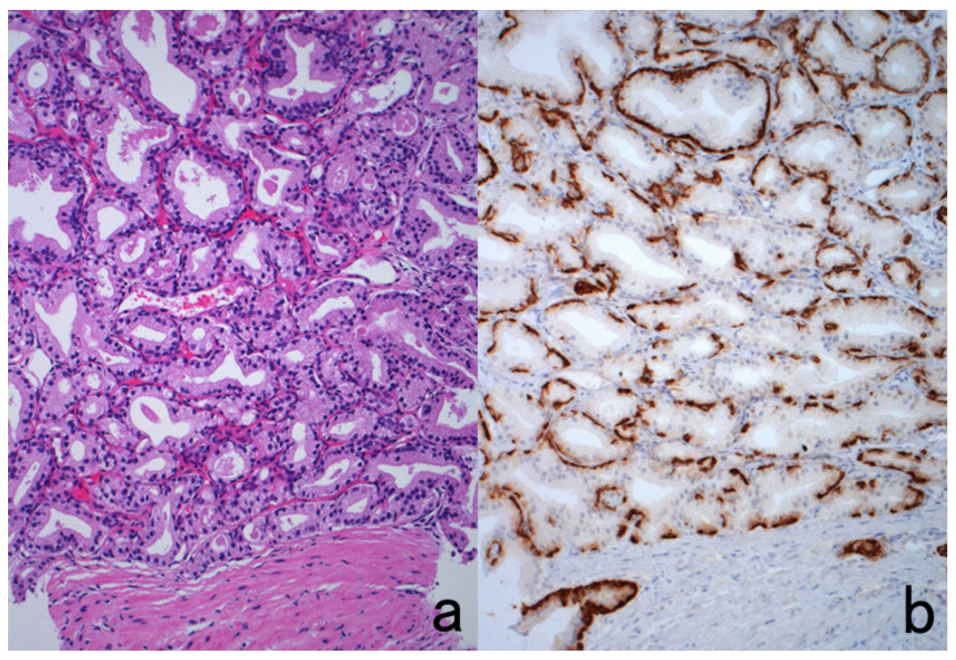
Figure 31.
Detection of glomerular deposits of immunoglobulins and complement in FFPE renal biopsy sections with the aid of prolonged 0.1% trypsin digestion for 120 min. (a,b): IgA nephropathy (IgA staining, (a): without digestion, (b): after digestion). Mesangial deposition of IgA is evident in (b). (c,d): Membranous nephropathy after 0.1% trypsin digestion for 120 min ((c): IgG, (d): C3). Granular deposition of IgG and C3 is observed along the capillary loop, a diagnostic feature of membranous nephropathy.
Figure 31.
Detection of glomerular deposits of immunoglobulins and complement in FFPE renal biopsy sections with the aid of prolonged 0.1% trypsin digestion for 120 min. (a,b): IgA nephropathy (IgA staining, (a): without digestion, (b): after digestion). Mesangial deposition of IgA is evident in (b). (c,d): Membranous nephropathy after 0.1% trypsin digestion for 120 min ((c): IgG, (d): C3). Granular deposition of IgG and C3 is observed along the capillary loop, a diagnostic feature of membranous nephropathy.
Figure 32.
Deterioration of antigenicity by protease pretreatment. Top panels (a,b): substance P in the myenteric plexus of the small bowel. Bottom panels (c,d): IgD in the mantle zone of the pharyngeal tonsil. Left (a,c): without treatment and Right (b,d): after trypsin digestion for 15 min. Immunoreactivities of substance P and IgD are lost or markedly decreased by the enzymatic pretreatment.
Figure 32.
Deterioration of antigenicity by protease pretreatment. Top panels (a,b): substance P in the myenteric plexus of the small bowel. Bottom panels (c,d): IgD in the mantle zone of the pharyngeal tonsil. Left (a,c): without treatment and Right (b,d): after trypsin digestion for 15 min. Immunoreactivities of substance P and IgD are lost or markedly decreased by the enzymatic pretreatment.
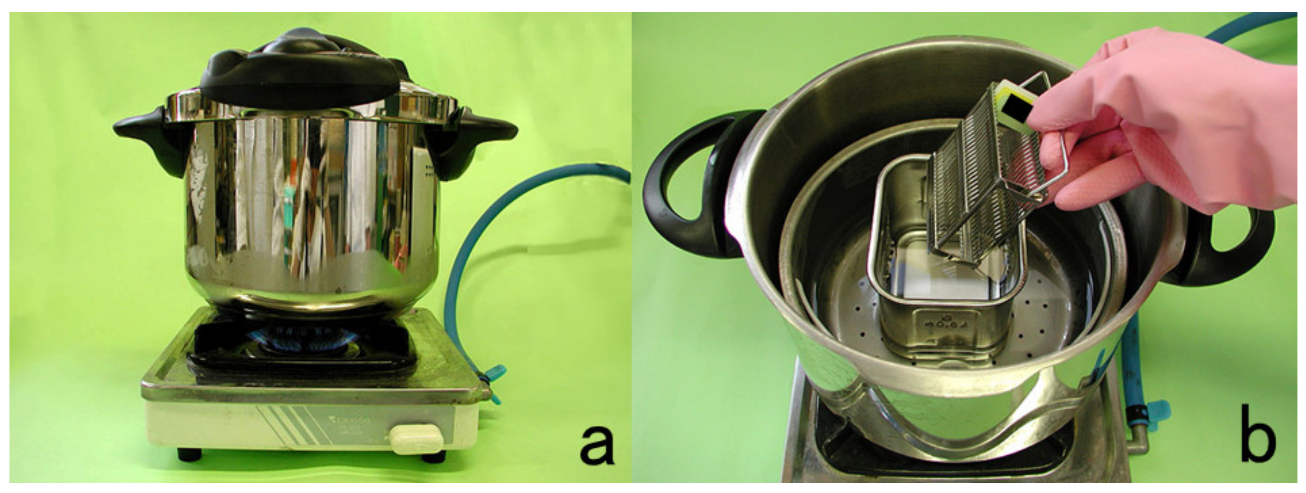
Figure 33.
Recommendation of a pot typically used in French cuisine for use as a pressure pan (a,b). The pressure pan made by T-Fal (Rumilly, Haute-Savoie, France) is easy to handle and use for HIER in a diagnostic pathology laboratory.
Figure 33.
Recommendation of a pot typically used in French cuisine for use as a pressure pan (a,b). The pressure pan made by T-Fal (Rumilly, Haute-Savoie, France) is easy to handle and use for HIER in a diagnostic pathology laboratory.
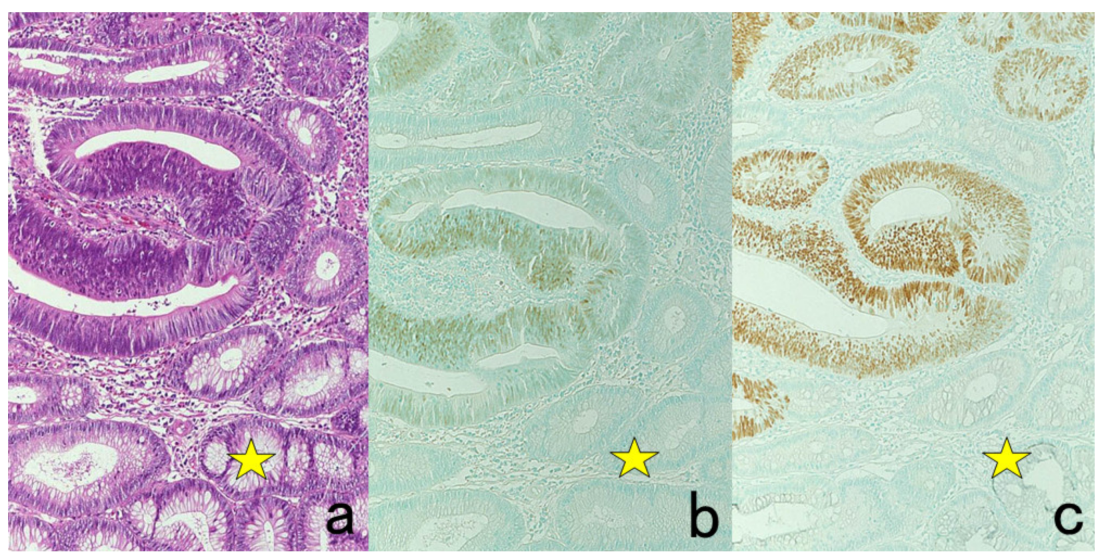
Figure 34.
Application of HIER (I). p53 expression in cancer in adenoma of the colon. (a): H&E, (b): immunostaining without HIER and (c): immunostaining after HIER with autoclaving at 121 °C for 10 min in 10 mM citrate buffer, pH 6.0. The nuclei of adenocarcinoma cells express p53, whereas the surrounding adenoma cells (stars) remain negative. The nuclei are counterstained with methyl green.
Figure 34.
Application of HIER (I). p53 expression in cancer in adenoma of the colon. (a): H&E, (b): immunostaining without HIER and (c): immunostaining after HIER with autoclaving at 121 °C for 10 min in 10 mM citrate buffer, pH 6.0. The nuclei of adenocarcinoma cells express p53, whereas the surrounding adenoma cells (stars) remain negative. The nuclei are counterstained with methyl green.
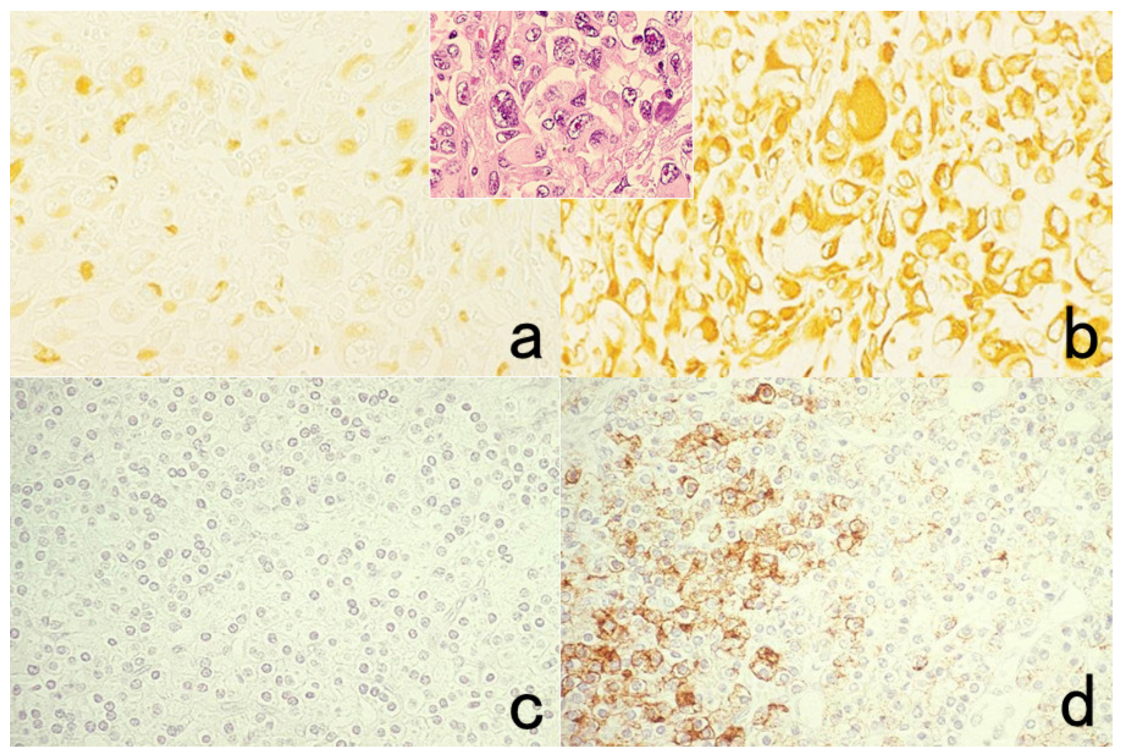
Figure 35.
Application of HIER (II). Top panels (a,b): Vimentin in lung metastasis of anaplastic thyroid carcinoma (inset: H&E). Bottom panels (c,d): Parathyroid hormone in normal parathyroid gland. Left (a,c): Without HIER treatment and Right (b,d): after HIER with autoclaving at 121 °C for 10 min in 10 mM citrate buffer, pH 6. Immunoreactivities of vimentin and parathyroid hormone are significantly retrieved by the hydrated heating pretreatment.
Figure 35.
Application of HIER (II). Top panels (a,b): Vimentin in lung metastasis of anaplastic thyroid carcinoma (inset: H&E). Bottom panels (c,d): Parathyroid hormone in normal parathyroid gland. Left (a,c): Without HIER treatment and Right (b,d): after HIER with autoclaving at 121 °C for 10 min in 10 mM citrate buffer, pH 6. Immunoreactivities of vimentin and parathyroid hormone are significantly retrieved by the hydrated heating pretreatment.
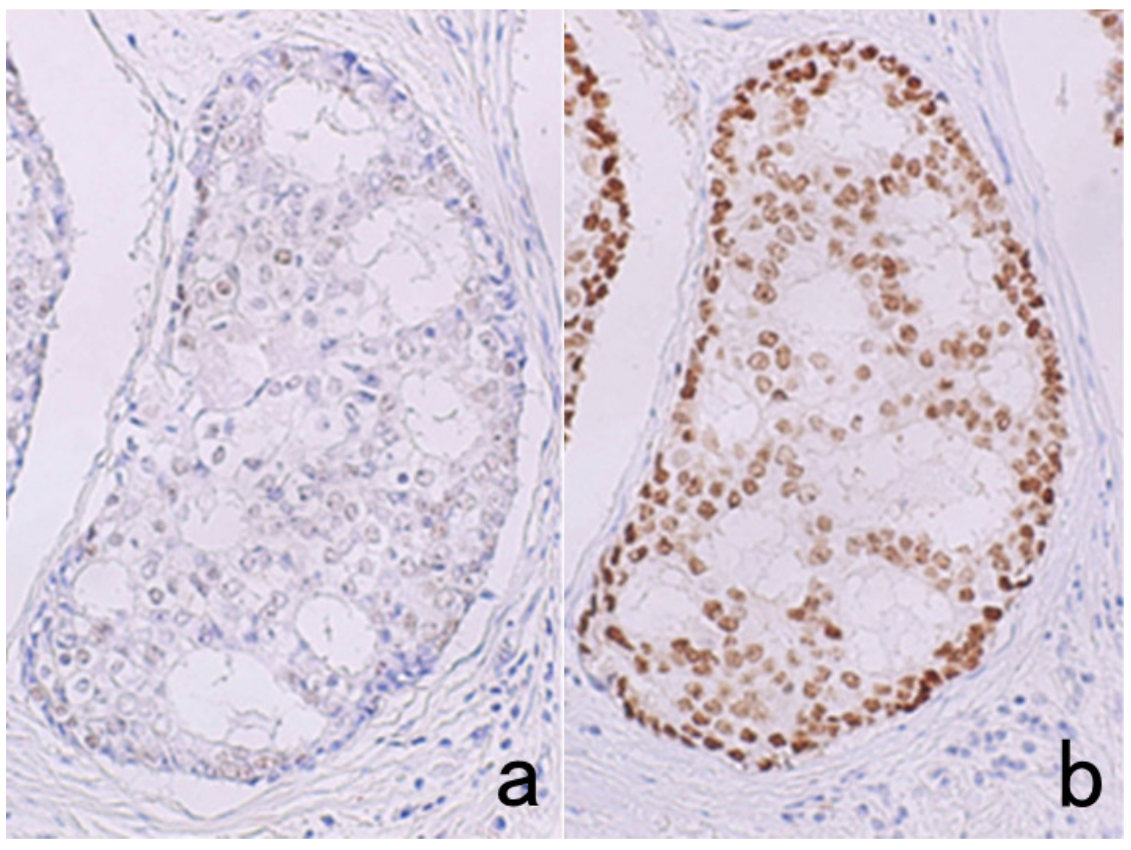
Figure 36.
Selection of the aqueous solution for appropriate HIER. ER immunostaining for breast cancer after pressure pan heating at 121 °C for 10 min. (a): 10 mM citrate buffer, pH 6.0, (b): 1 mM EDTA, pH 8.0. ER in cribriform ductal carcinoma in situ is effectively retrieved by HIER in 1 mM EDTA solution, pH 8.0.
Figure 36.
Selection of the aqueous solution for appropriate HIER. ER immunostaining for breast cancer after pressure pan heating at 121 °C for 10 min. (a): 10 mM citrate buffer, pH 6.0, (b): 1 mM EDTA, pH 8.0. ER in cribriform ductal carcinoma in situ is effectively retrieved by HIER in 1 mM EDTA solution, pH 8.0.
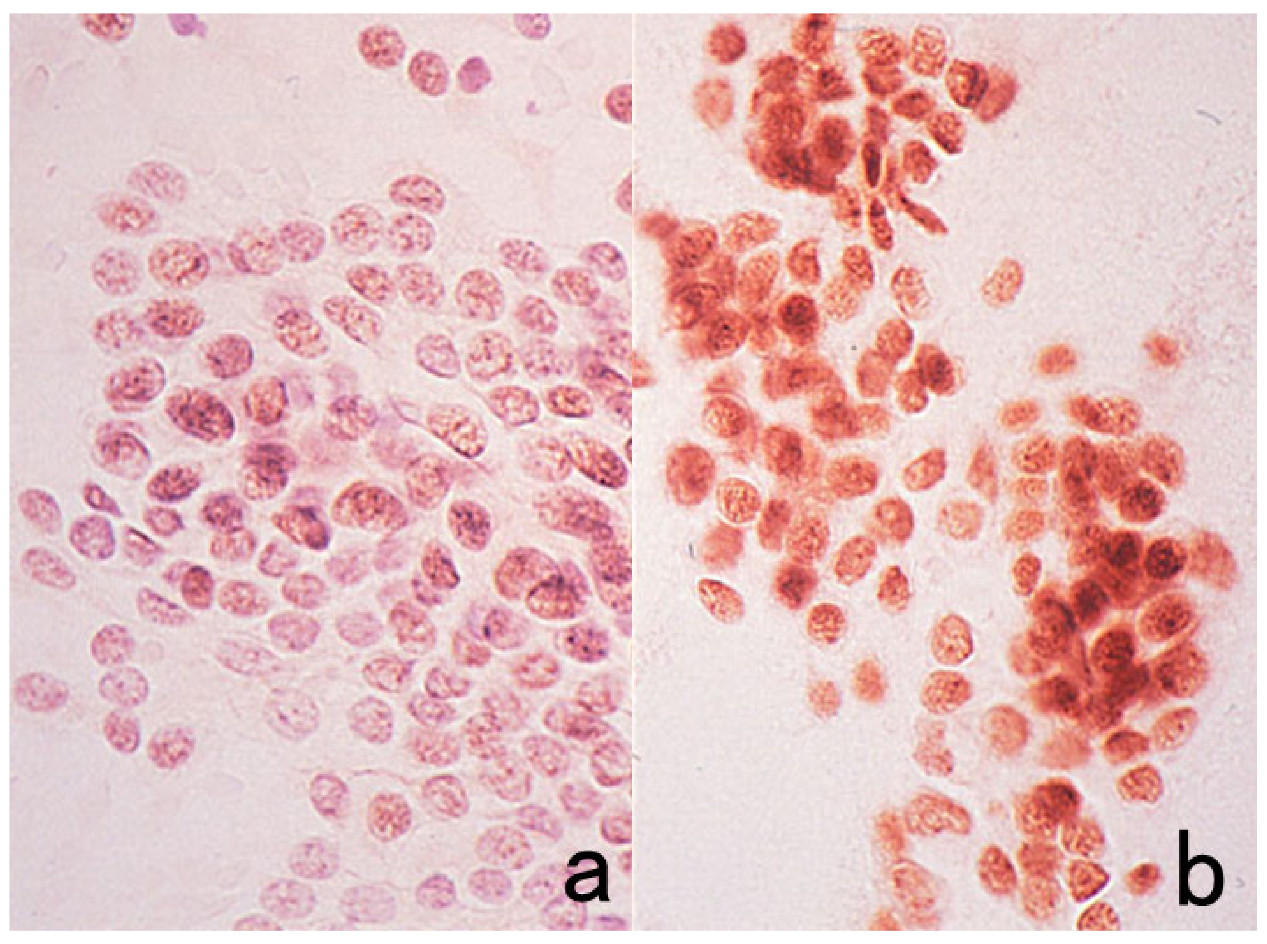
Figure 37.
ER immunostaining for an aspiration cytology preparation after ethanol fixation. (a): Without pretreatment and (b): HIER with pressure pan heating at 121 °C for 10 min in 10 mM citrate buffer, pH 7.0. HIER is effective for ER immunolocalization even in cytology specimens.
Figure 37.
ER immunostaining for an aspiration cytology preparation after ethanol fixation. (a): Without pretreatment and (b): HIER with pressure pan heating at 121 °C for 10 min in 10 mM citrate buffer, pH 7.0. HIER is effective for ER immunolocalization even in cytology specimens.
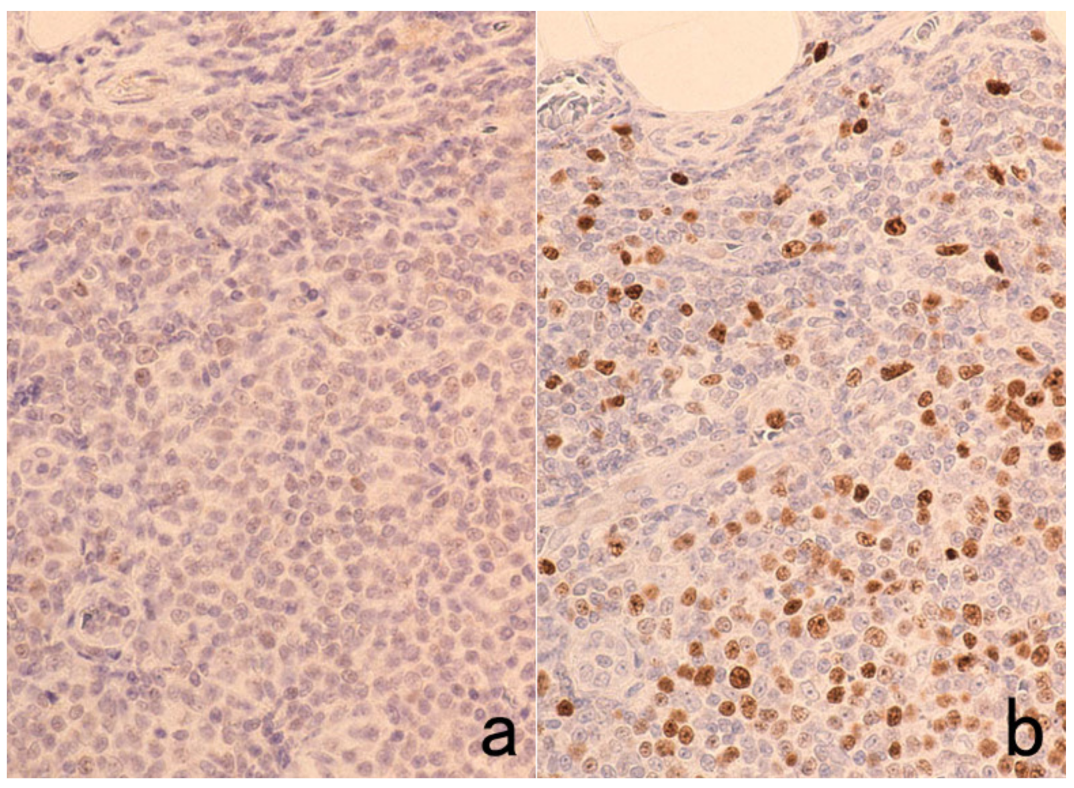
Figure 38.
Weakening of Ki-67 immunoreactivity by overnight antibody incubation after HIER with pressure pan heating at 121 °C for 10 min in 10 mM citrate buffer, pH 6.0. (a): One-hour antibody incubation and (b): overnight incubation. Ki-67 labeling in the germinal center lymphocytes of the pharyngeal tonsil, clearly seen in the 1-h antibody incubation, is significantly weakened after overnight incubation.
Figure 38.
Weakening of Ki-67 immunoreactivity by overnight antibody incubation after HIER with pressure pan heating at 121 °C for 10 min in 10 mM citrate buffer, pH 6.0. (a): One-hour antibody incubation and (b): overnight incubation. Ki-67 labeling in the germinal center lymphocytes of the pharyngeal tonsil, clearly seen in the 1-h antibody incubation, is significantly weakened after overnight incubation.
Figure 39.
Poor nuclear stainability by hematoxylin after EDTA-mediated HIER. CDX2 (a nuclear marker for intestinal-type epithelial cells) immunoreactivity in intestinal metaplasia of the stomach. Mayer’s hematoxylin staining for 10 s (a), 1 min (b), and 3 min (c). Prolonged nuclear staining is necessary after HIER in 1 mM EDTA solution, pH 8.0.
Figure 39.
Poor nuclear stainability by hematoxylin after EDTA-mediated HIER. CDX2 (a nuclear marker for intestinal-type epithelial cells) immunoreactivity in intestinal metaplasia of the stomach. Mayer’s hematoxylin staining for 10 s (a), 1 min (b), and 3 min (c). Prolonged nuclear staining is necessary after HIER in 1 mM EDTA solution, pH 8.0.
Figure 40.
Antigenic loss by HIER in 10 mM citrate buffer, pH 6.0. BM-1 (a myeloid marker) in FFPE bone marrow aspiration. (a): Without HIER and (b): after HIER with pressure pan heating at 121 °C for 10 min. BM-1 immunoreactivity is quite susceptible to the heating pretreatment.
Figure 40.
Antigenic loss by HIER in 10 mM citrate buffer, pH 6.0. BM-1 (a myeloid marker) in FFPE bone marrow aspiration. (a): Without HIER and (b): after HIER with pressure pan heating at 121 °C for 10 min. BM-1 immunoreactivity is quite susceptible to the heating pretreatment.
Figure 41.
How to cool down after HIER. (a): Rapid cooling by soaking in tap water and (b): gradual cooling by leaving the slide container in the heating solution after it reaches room temperature. Ki-67 antigenicity in reactive lymphadenopathy becomes undetectable after rapid cooling. Sections after gradual cooling reveal distinct nuclear labeling.
Figure 41.
How to cool down after HIER. (a): Rapid cooling by soaking in tap water and (b): gradual cooling by leaving the slide container in the heating solution after it reaches room temperature. Ki-67 antigenicity in reactive lymphadenopathy becomes undetectable after rapid cooling. Sections after gradual cooling reveal distinct nuclear labeling.
Figure 42.
Labeling of mitotic cells by Ki-67 immunostaining in the pharyngeal tonsil (inset: high-power view). A high-molecular-weight polymer reagent in the EnVision system provokes a false-negative result for Ki-67 nuclear labeling of proliferative cells. Only mitotic cells are labeled. It seems that the huge molecules of the secondary reagent cannot reach the non-mitotic proliferative cells but do reach the mitotic cells lacking the nuclear membrane.
Figure 42.
Labeling of mitotic cells by Ki-67 immunostaining in the pharyngeal tonsil (inset: high-power view). A high-molecular-weight polymer reagent in the EnVision system provokes a false-negative result for Ki-67 nuclear labeling of proliferative cells. Only mitotic cells are labeled. It seems that the huge molecules of the secondary reagent cannot reach the non-mitotic proliferative cells but do reach the mitotic cells lacking the nuclear membrane.
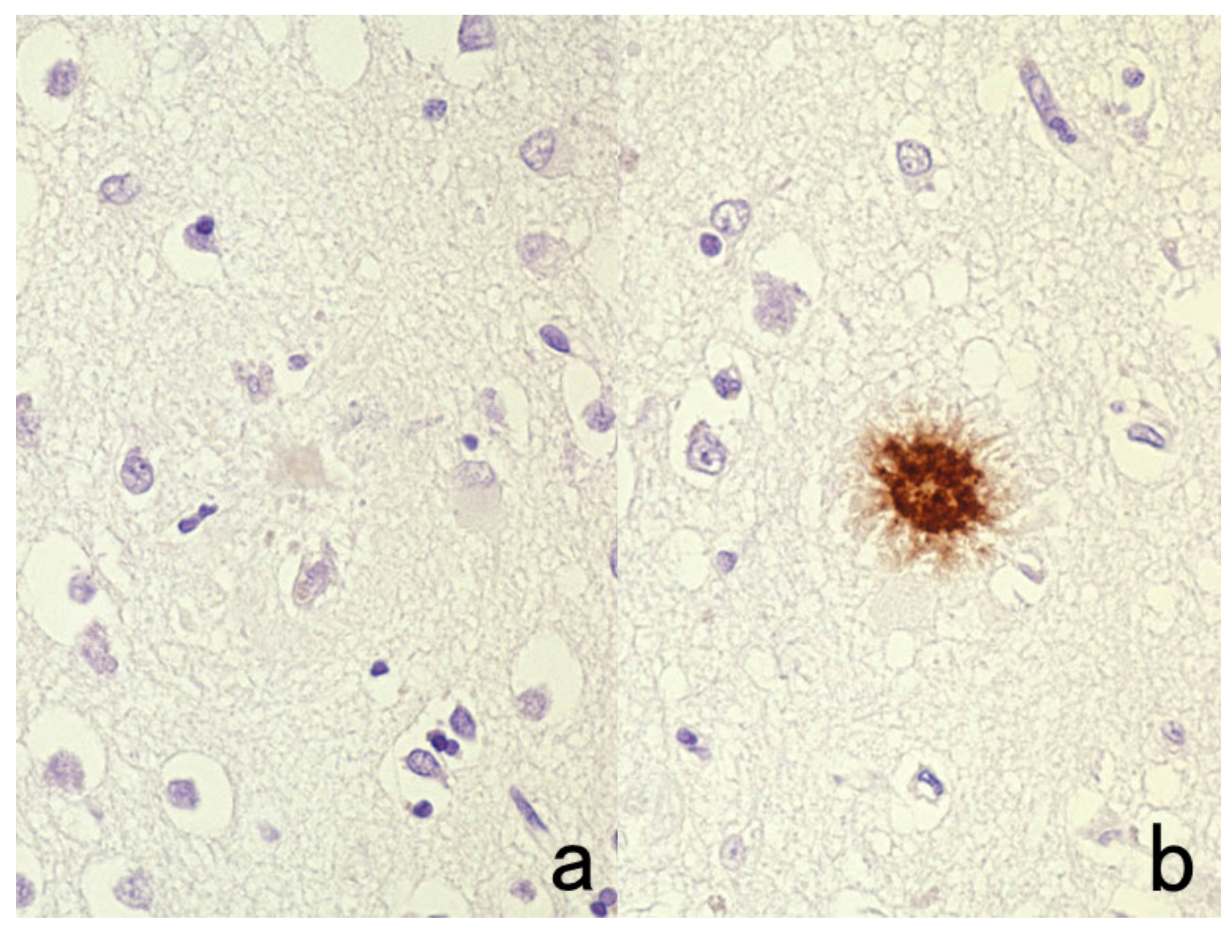
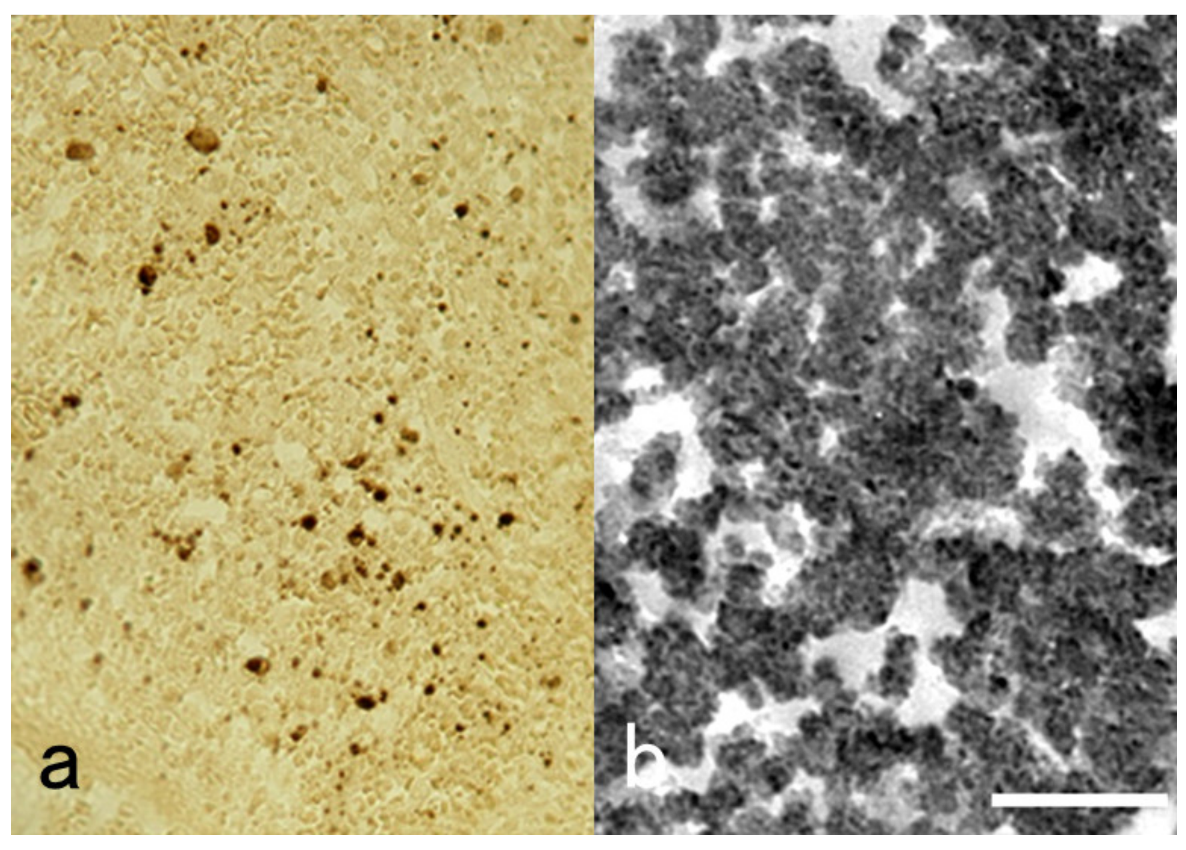
Figure 43.
Retrieval of β-amyloid immunoreactivity in the brain by formic acid pretreatment. (a): Without treatment and (b): with 100% formic acid treatment for 5 min. Brief soaking in formic acid retrieves β-amyloid immunoreactivity of senile plaques in Alzheimer’s disease. A polyclonal antibody available from Agilent Co., Santa Clara, CA, USA, was used.
Figure 43.
Retrieval of β-amyloid immunoreactivity in the brain by formic acid pretreatment. (a): Without treatment and (b): with 100% formic acid treatment for 5 min. Brief soaking in formic acid retrieves β-amyloid immunoreactivity of senile plaques in Alzheimer’s disease. A polyclonal antibody available from Agilent Co., Santa Clara, CA, USA, was used.
Figure 44.
Schematic illustration of intracellular localization of antigens. The specificity of immunostaining can be judged by the intracellular localization pattern of the antigenic substances as either membranous, diffuse cytoplasmic, granular/vesicular cytoplasmic or nuclear.
Figure 44.
Schematic illustration of intracellular localization of antigens. The specificity of immunostaining can be judged by the intracellular localization pattern of the antigenic substances as either membranous, diffuse cytoplasmic, granular/vesicular cytoplasmic or nuclear.
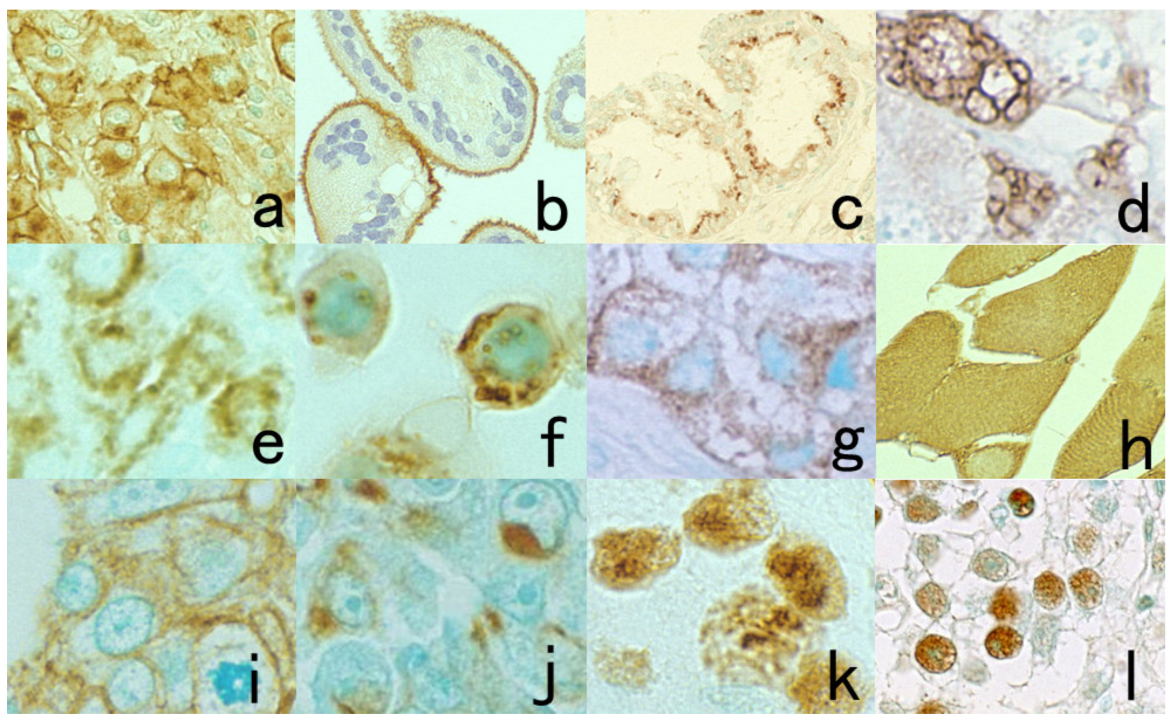
Figure 45.
Representative immunohistochemical markers showing various intracellular localization patterns. (a): CD30 in anaplastic large cell (Ki-1) lymphoma (plasma membrane plus Golgi area), (b): placental ALP on the villi of normal placenta (apical plasma membrane), (c): CA125 in ovarian serous adenocarcinoma (mainly seen in the Golgi area), (d): IgG in plasmacytoma (coarse vesicles), (e): intrinsic factor in parietal cells in the oxyntic gastric mucosa (fine vesicles), (f): nonspecific cross-reacting antigen in lysosomes of lung adenocarcinoma cells (cell line PC-9) (coarse granular), (g): insulin in pancreatic insulinoma (fine granular), (h): creatine kinase-MM isozyme in normal striated muscle (diffuse cytoplasmic), (i): cytokeratin in well-differentiated gastric adenocarcinoma (along the plasma membrane), (j): cytokeratin in poorly differentiated gastric adenocarcinoma (concentrated in the Golgi area), (k): Ki-67 in breast cancer (nucleolar accentuation) and (l): proliferating cell nuclear antigen in testicular seminoma (diffuse nuclear).
Figure 45.
Representative immunohistochemical markers showing various intracellular localization patterns. (a): CD30 in anaplastic large cell (Ki-1) lymphoma (plasma membrane plus Golgi area), (b): placental ALP on the villi of normal placenta (apical plasma membrane), (c): CA125 in ovarian serous adenocarcinoma (mainly seen in the Golgi area), (d): IgG in plasmacytoma (coarse vesicles), (e): intrinsic factor in parietal cells in the oxyntic gastric mucosa (fine vesicles), (f): nonspecific cross-reacting antigen in lysosomes of lung adenocarcinoma cells (cell line PC-9) (coarse granular), (g): insulin in pancreatic insulinoma (fine granular), (h): creatine kinase-MM isozyme in normal striated muscle (diffuse cytoplasmic), (i): cytokeratin in well-differentiated gastric adenocarcinoma (along the plasma membrane), (j): cytokeratin in poorly differentiated gastric adenocarcinoma (concentrated in the Golgi area), (k): Ki-67 in breast cancer (nucleolar accentuation) and (l): proliferating cell nuclear antigen in testicular seminoma (diffuse nuclear).
![Cells 10 01501 g045 Cells 10 01501 g045]()
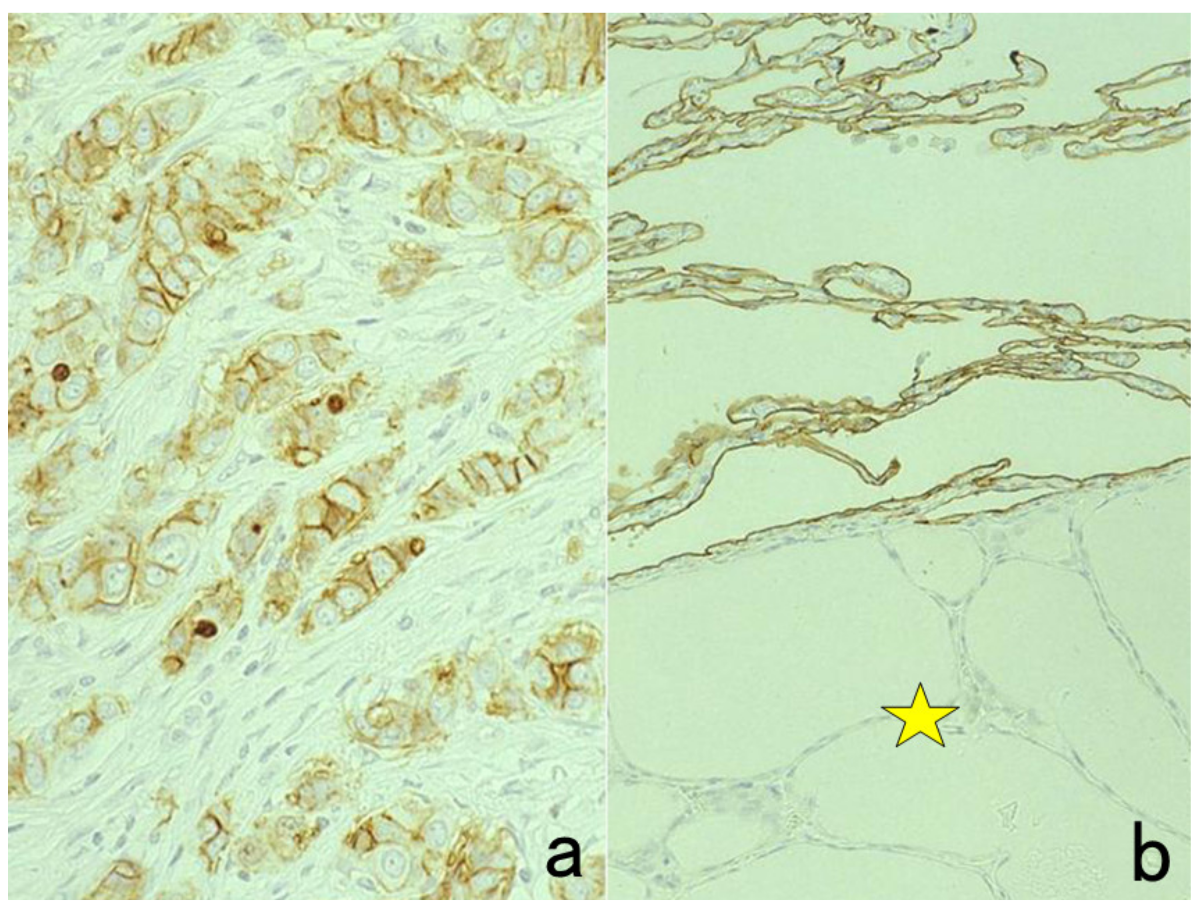
Figure 46.
Plasma membrane localization of Ki-67. (a): Breast cancer and (b): lung with ectopic thyroid tissue. Ki-67 may show strange, cross-reactive localization on the plasma membrane. Membranous positivity in invasive ductal carcinoma cells and alveolar type I pneumocytes is unique but nonspecific. The star indicates ectopic thyroid tissue in the lung.
Figure 46.
Plasma membrane localization of Ki-67. (a): Breast cancer and (b): lung with ectopic thyroid tissue. Ki-67 may show strange, cross-reactive localization on the plasma membrane. Membranous positivity in invasive ductal carcinoma cells and alveolar type I pneumocytes is unique but nonspecific. The star indicates ectopic thyroid tissue in the lung.
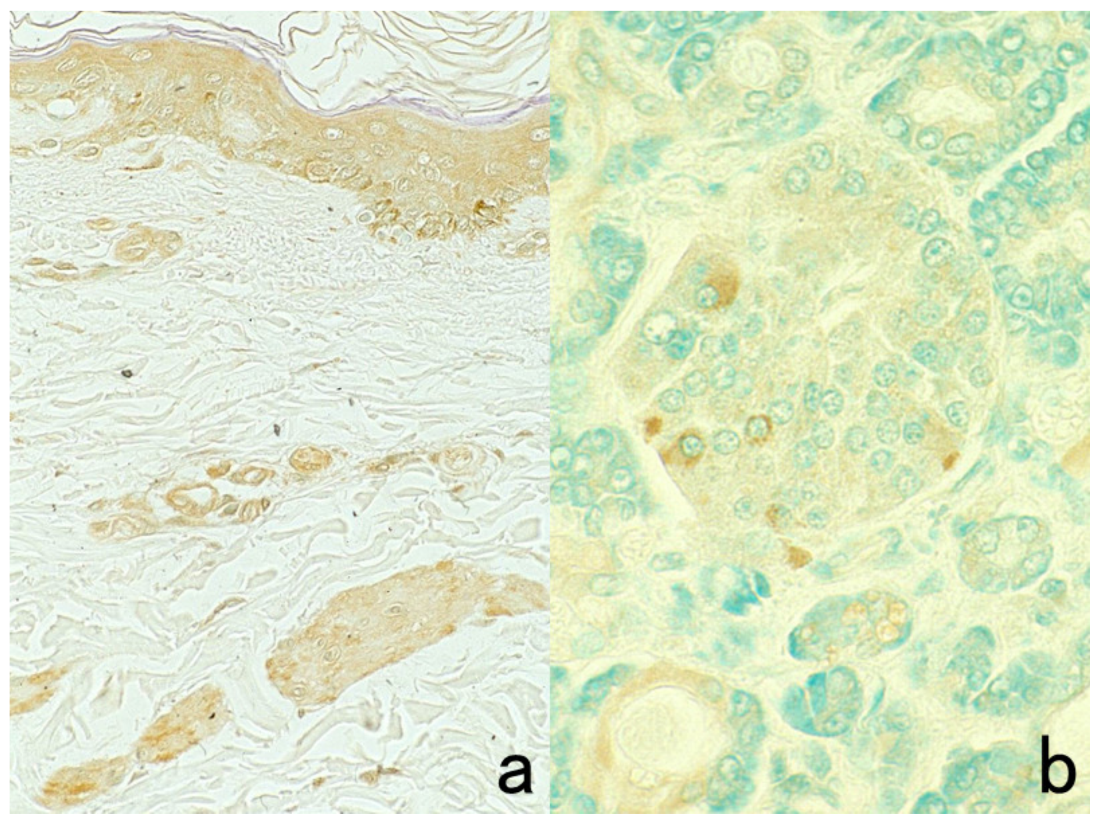
Figure 47.
Examples of nonspecific immunostaining. (a): Membranous positivity of PgR in breast cancer and (b): nuclear positivity of CD45RO (UCHL1) in nasal NK-cell lymphoma. The intracellular localization pattern is unusual, so the results must be regarded as nonspecific. The nuclei in panel (b) are counterstained with methyl green.
Figure 47.
Examples of nonspecific immunostaining. (a): Membranous positivity of PgR in breast cancer and (b): nuclear positivity of CD45RO (UCHL1) in nasal NK-cell lymphoma. The intracellular localization pattern is unusual, so the results must be regarded as nonspecific. The nuclei in panel (b) are counterstained with methyl green.
Figure 48.
Myoglobin immunostaining in the skin (a) and pancreas (b) using a commercial rabbit antiserum. Rabbit antiserum available from Agilent/Dako may contain natural antibodies against intermediate filament proteins. In the skin, epidermal keratinocytes, vascular endothelial cells, and smooth muscle cells of erector pili are weakly stained. In the pancreas, some islet cells are faintly immunostained by the incidentally contaminating antibodies. The nuclei in panel (b) are counterstained with methyl green.
Figure 48.
Myoglobin immunostaining in the skin (a) and pancreas (b) using a commercial rabbit antiserum. Rabbit antiserum available from Agilent/Dako may contain natural antibodies against intermediate filament proteins. In the skin, epidermal keratinocytes, vascular endothelial cells, and smooth muscle cells of erector pili are weakly stained. In the pancreas, some islet cells are faintly immunostained by the incidentally contaminating antibodies. The nuclei in panel (b) are counterstained with methyl green.
Figure 49.
Cross-reactive antibodies against the carrier protein. Cholecystokinin (CCK) is a polypeptide with 33 amino acid residues. The CCK antiserum was raised in a rabbit by using the Ascaris extract as carrier proteins. Ascaris protein-like (cross-reactive) immunoreactivities are observed in the gastric foveolar cells (a), smooth muscle cells and cartilage in the bronchial wall (b), and small cell lung carcinoma cells (c). One must not judge as CCK-producing small cell carcinoma of the lung. Note the vesicular cytoplasmic staining in panel (c) rather than fine granular staining.
Figure 49.
Cross-reactive antibodies against the carrier protein. Cholecystokinin (CCK) is a polypeptide with 33 amino acid residues. The CCK antiserum was raised in a rabbit by using the Ascaris extract as carrier proteins. Ascaris protein-like (cross-reactive) immunoreactivities are observed in the gastric foveolar cells (a), smooth muscle cells and cartilage in the bronchial wall (b), and small cell lung carcinoma cells (c). One must not judge as CCK-producing small cell carcinoma of the lung. Note the vesicular cytoplasmic staining in panel (c) rather than fine granular staining.
Figure 50.
Cross-reactive immunostaining of Mycobacterium leprae in the liver with a rabbit anti-HBs antiserum, immunized with complete adjuvant containing the extract of M. tuberculosis. (a): H&E, (b): anti-HBs rabbit antiserum, (c): anti-HBs monoclonal antibody. Leproma is seen mainly in the portal area. The antiserum visualizes M. leprae in the cytoplasm of macrophages richly distributed both in the portal triad (leproma cells) and in the sinusoid (Kupffer cells). The monoclonal antibody detects HBs antigen-positive hepatocytes (arrows) without background cross-reactivity.
Figure 50.
Cross-reactive immunostaining of Mycobacterium leprae in the liver with a rabbit anti-HBs antiserum, immunized with complete adjuvant containing the extract of M. tuberculosis. (a): H&E, (b): anti-HBs rabbit antiserum, (c): anti-HBs monoclonal antibody. Leproma is seen mainly in the portal area. The antiserum visualizes M. leprae in the cytoplasm of macrophages richly distributed both in the portal triad (leproma cells) and in the sinusoid (Kupffer cells). The monoclonal antibody detects HBs antigen-positive hepatocytes (arrows) without background cross-reactivity.
Figure 51.
Diagnostic utility and pitfalls of cytokeratin immunostaining. Top panels (a,b): Spindle cell carcinoma of the skin and Bottom panels (c,d): anaplastic large cell (Ki-1) lymphoma. Left panels (a,c): H&E and Right panels (b,d): immunostaining with wide-spectrum anti-cytokeratin antiserum. Cytokeratin expression confirms the epithelial nature of the spindle cells in the skin. Because of the epithelioid morphology and cytokeratin expression in Ki-1 lymphoma, diagnostic confusion with metastatic undifferentiated carcinoma may occur. The nuclei in panel (b) are counterstained with methyl green.
Figure 51.
Diagnostic utility and pitfalls of cytokeratin immunostaining. Top panels (a,b): Spindle cell carcinoma of the skin and Bottom panels (c,d): anaplastic large cell (Ki-1) lymphoma. Left panels (a,c): H&E and Right panels (b,d): immunostaining with wide-spectrum anti-cytokeratin antiserum. Cytokeratin expression confirms the epithelial nature of the spindle cells in the skin. Because of the epithelioid morphology and cytokeratin expression in Ki-1 lymphoma, diagnostic confusion with metastatic undifferentiated carcinoma may occur. The nuclei in panel (b) are counterstained with methyl green.
Figure 52.
Post-atrophic hyperplasia of the prostate. (a): H&E and (b): immunostaining for cytokeratin 5/6. H&E histology resembles well-differentiated prostatic adenocarcinoma. Immunostaining for cytokeratin 5/6, a basal cell marker, clearly shows the consistent association of basal cells around the acini, definitely indicating a benign lesion.
Figure 52.
Post-atrophic hyperplasia of the prostate. (a): H&E and (b): immunostaining for cytokeratin 5/6. H&E histology resembles well-differentiated prostatic adenocarcinoma. Immunostaining for cytokeratin 5/6, a basal cell marker, clearly shows the consistent association of basal cells around the acini, definitely indicating a benign lesion.
Figure 53.
Expression of specific markers in unrelated cells. (a): Neuron-specific enolase (NSE) in the normal pancreas, (b): glial fibrillary acidic protein (GFAP) in the normal salivary gland, (c): prostate-specific antigen (PSA) in the normal salivary gland and (d): prostatic acid phosphatase (PAcP) in rectal carcinoid tumor. NSE is expressed not only in islets but also pancreatic ductal cells (a). In the salivary gland, GFAP immunostains some of the myoepithelial cells (b), and PSA antiserum decorates the apical cytoplasm of the ductal cells (c). Rectal carcinoid tumor cells are frequently immunoreactive for PAcP (d). The nuclei are counterstained with methyl green.
Figure 53.
Expression of specific markers in unrelated cells. (a): Neuron-specific enolase (NSE) in the normal pancreas, (b): glial fibrillary acidic protein (GFAP) in the normal salivary gland, (c): prostate-specific antigen (PSA) in the normal salivary gland and (d): prostatic acid phosphatase (PAcP) in rectal carcinoid tumor. NSE is expressed not only in islets but also pancreatic ductal cells (a). In the salivary gland, GFAP immunostains some of the myoepithelial cells (b), and PSA antiserum decorates the apical cytoplasm of the ductal cells (c). Rectal carcinoid tumor cells are frequently immunoreactive for PAcP (d). The nuclei are counterstained with methyl green.
Figure 54.
Nonspecific binding of IgG in certain cells in FFPE sections. (a): Glicentin (enteroglucagon equivalent) immunoreactivity in gastric parietal cells and (b): motilin immunoreactivity in rectal carcinoid tumor. Certain cells may adsorb the antibody molecules nonspecifically, causing false-positive immunostaining. The nuclei are counterstained with methyl green.
Figure 54.
Nonspecific binding of IgG in certain cells in FFPE sections. (a): Glicentin (enteroglucagon equivalent) immunoreactivity in gastric parietal cells and (b): motilin immunoreactivity in rectal carcinoid tumor. Certain cells may adsorb the antibody molecules nonspecifically, causing false-positive immunostaining. The nuclei are counterstained with methyl green.
Figure 55.
Epithelial membrane antigen (EMA) expression in normal (a,c) and neoplastic (b,d) perineurial cells (top panels: (a,b)) and plasma cells (bottom panels: (c,d)). It should be noted that EMA is positive in certain non-epithelial cells and their tumors (perineurioma and multiple myeloma). Perineurial cells surrounding the peripheral nerve sheath represent peripheral meningothelial cells. Chronic cervicitis containing numerous plasma cells is covered with EMA-positive columnar epithelial cells.
Figure 55.
Epithelial membrane antigen (EMA) expression in normal (a,c) and neoplastic (b,d) perineurial cells (top panels: (a,b)) and plasma cells (bottom panels: (c,d)). It should be noted that EMA is positive in certain non-epithelial cells and their tumors (perineurioma and multiple myeloma). Perineurial cells surrounding the peripheral nerve sheath represent peripheral meningothelial cells. Chronic cervicitis containing numerous plasma cells is covered with EMA-positive columnar epithelial cells.
Figure 56.
Immunohistochemical blood typing in needle biopsy specimens of the prostate. Specimens from two patients were mixed up in one tissue container. The blood group was type A in one patient and type O in the other. Immunostaining for type A substance is positive in endothelial cells in panel (a) but negative in panel (b). It is evident that the specimen of the patient with type A blood group contains well-differentiated adenocarcinoma (star).
Figure 56.
Immunohistochemical blood typing in needle biopsy specimens of the prostate. Specimens from two patients were mixed up in one tissue container. The blood group was type A in one patient and type O in the other. Immunostaining for type A substance is positive in endothelial cells in panel (a) but negative in panel (b). It is evident that the specimen of the patient with type A blood group contains well-differentiated adenocarcinoma (star).
Figure 57.
Re-staining of a cytology specimen with Chlamydia trachomatis infection. (a): Papanicolaou and (b): immunostaining with a mouse monoclonal antibody B104.1 after removal of the cover glass and decoloration. A cytoplasmic nevular inclusion body in a cervical columnar cell is clearly immunoreactive for the C. trachomatis antigen, confirming the cytodiagnosis of chlamydiasis. The nuclei in panel (b) are counterstained with methyl green.
Figure 57.
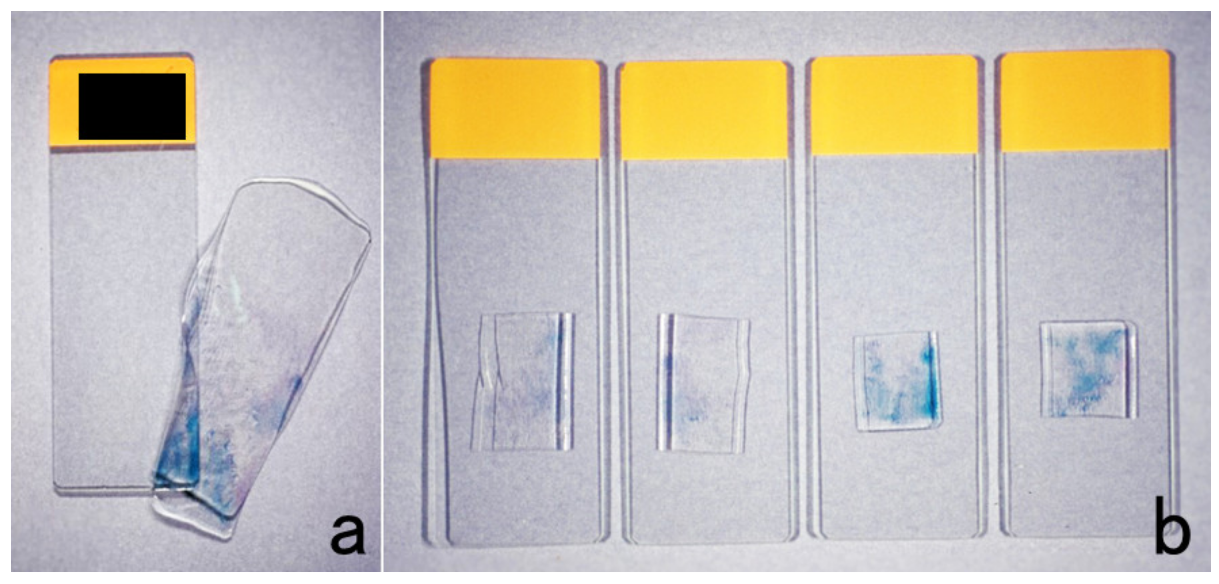
Re-staining of a cytology specimen with Chlamydia trachomatis infection. (a): Papanicolaou and (b): immunostaining with a mouse monoclonal antibody B104.1 after removal of the cover glass and decoloration. A cytoplasmic nevular inclusion body in a cervical columnar cell is clearly immunoreactive for the C. trachomatis antigen, confirming the cytodiagnosis of chlamydiasis. The nuclei in panel (b) are counterstained with methyl green.
Figure 58.
The cell transfer technique. After removal of the cover glass, the cell preparation is covered with mounting resin solution that solidifies to become a thick membrane sheet. Cells are transferred to the solidified resin (a). After cutting the resin membrane into several pieces, they are placed onto silane-coated glass slides, which should be fully dried in an incubator (b). The resin component can easily be removed by dipping the specimens in xylene. Now, the specimens are ready for immunostaining using HIER.
Figure 58.
The cell transfer technique. After removal of the cover glass, the cell preparation is covered with mounting resin solution that solidifies to become a thick membrane sheet. Cells are transferred to the solidified resin (a). After cutting the resin membrane into several pieces, they are placed onto silane-coated glass slides, which should be fully dried in an incubator (b). The resin component can easily be removed by dipping the specimens in xylene. Now, the specimens are ready for immunostaining using HIER.
Figure 59.
Pre-embedding immunoelectron microscopy for SFTS virus using a TACAS glass slide. (a): Light microscopic chromogenic immunostaining and (b): immunoreactive round-shaped viral particles, around 100 nm in size, at the ultrastructural level. The FFPE splenic red pulp from an autopsy case was immunostained with a monoclonal antibody to SFTS virus after HIER. For pre-embedding immunoelectron microscopy, the immunostained section was peeled off for transfer to an Epon-embedded block by the inverted beam capsule method. The miraculous TACAS glass slide prevents detachment of sections during immunostaining and allows cell transfer after immunostaining. Bar indicates 500 nm.
Figure 59.
Pre-embedding immunoelectron microscopy for SFTS virus using a TACAS glass slide. (a): Light microscopic chromogenic immunostaining and (b): immunoreactive round-shaped viral particles, around 100 nm in size, at the ultrastructural level. The FFPE splenic red pulp from an autopsy case was immunostained with a monoclonal antibody to SFTS virus after HIER. For pre-embedding immunoelectron microscopy, the immunostained section was peeled off for transfer to an Epon-embedded block by the inverted beam capsule method. The miraculous TACAS glass slide prevents detachment of sections during immunostaining and allows cell transfer after immunostaining. Bar indicates 500 nm.
Figure 60.
Visualization of bacteria in infectious lesions using cross-reactive antisera. Left panels (a,d): Corynebacterium kroppenstedtii-induced granulomatous mastitis, Central panels (b,e): leptospirosis (Leptospira interrogans infection or Weil’s disease) in the liver and Right panels (c,f): Haemophilus pertussis-induced pneumonia. Top (a–c): H&E, Bottom (d–f): immunostaining using commercially available antiserum against Treponema pallidum (d), Escherichia coli (e), and Bacillus cereus (f). The causative bacteria are visible through the cross-reactivity of the antisera. Bacteria are not recognizable in H&E preparations.
Figure 60.
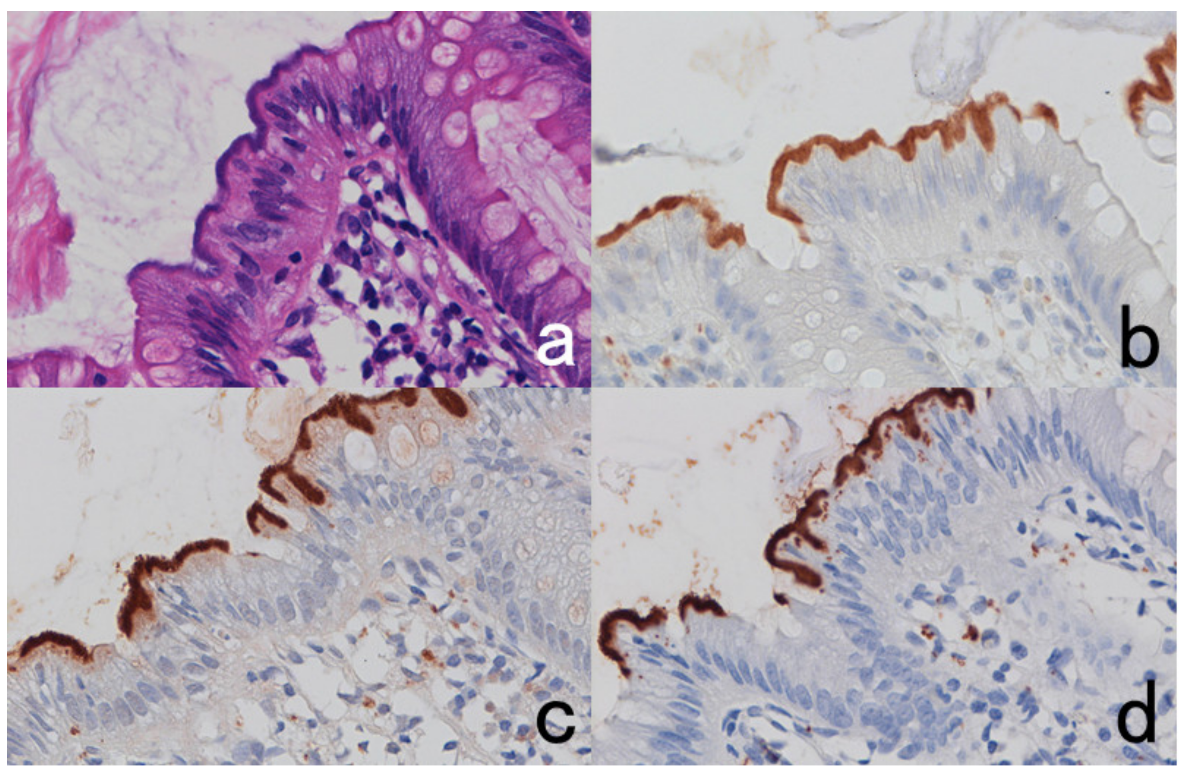
Visualization of bacteria in infectious lesions using cross-reactive antisera. Left panels (a,d): Corynebacterium kroppenstedtii-induced granulomatous mastitis, Central panels (b,e): leptospirosis (Leptospira interrogans infection or Weil’s disease) in the liver and Right panels (c,f): Haemophilus pertussis-induced pneumonia. Top (a–c): H&E, Bottom (d–f): immunostaining using commercially available antiserum against Treponema pallidum (d), Escherichia coli (e), and Bacillus cereus (f). The causative bacteria are visible through the cross-reactivity of the antisera. Bacteria are not recognizable in H&E preparations.
Figure 61.
Intestinal spirochetosis caused by colonization of Brachyspira aalborgi. (a): H&E, (b–d): immunostaining using Treponema pallidum antiserum (b), BCG antiserum, (c) and E. coli antiserum (d). Long and basophilic spiral bacteria closely attach onto the apical surface of the colonic columnar cells (a). They are clearly immunostained with antisera to T. pallidum, BCG, and E. coli (b–d).
Figure 61.
Intestinal spirochetosis caused by colonization of Brachyspira aalborgi. (a): H&E, (b–d): immunostaining using Treponema pallidum antiserum (b), BCG antiserum, (c) and E. coli antiserum (d). Long and basophilic spiral bacteria closely attach onto the apical surface of the colonic columnar cells (a). They are clearly immunostained with antisera to T. pallidum, BCG, and E. coli (b–d).
Figure 62.
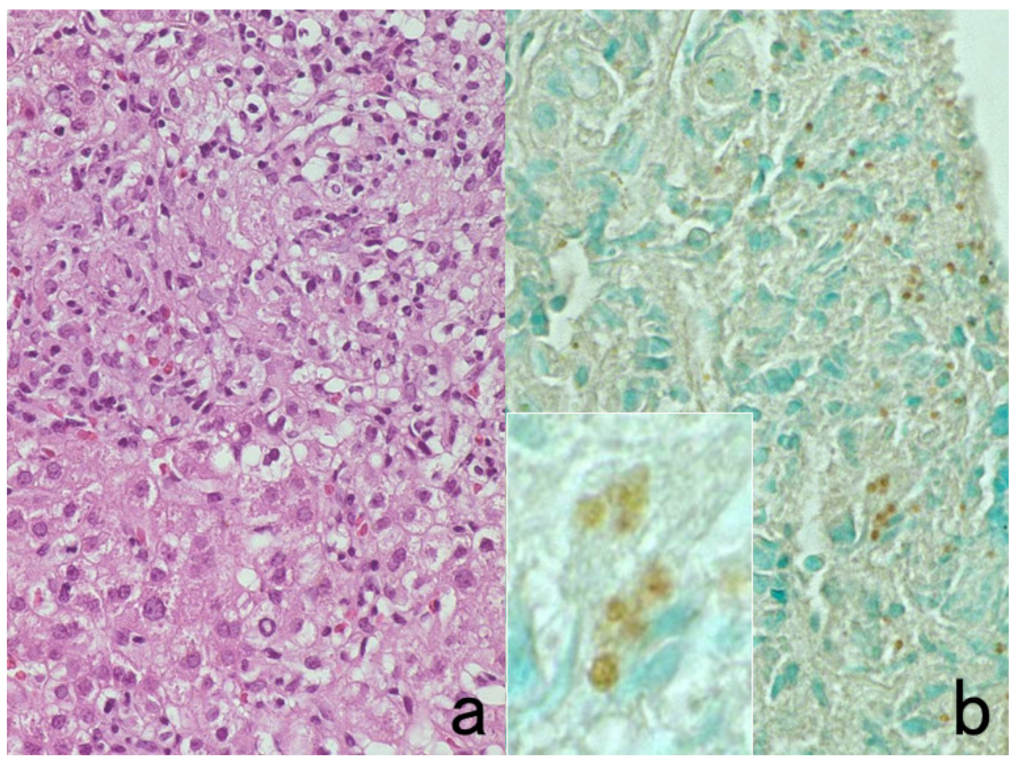
Immunostaining with the patient’s serum (I). Liver biopsy of visceral leishmaniasis (kala azar). (a): H&E and (b): 1:500 dilution of the patient’s own serum (inset: high-power view). Non-caseous epithelioid granulomas are dispersed in the liver parenchyma. Antibodies in the patients’ own serum identify red cell-sized positive signals in the cytoplasm of epithelioid cells and Kupffer cells. Although the specificity of the patient’s serum is totally unknown in this case, it significantly contributed to suggest the causative pathogens to be protozoa. The nuclei in panel (b) are counterstained with methyl green.
Figure 62.
Immunostaining with the patient’s serum (I). Liver biopsy of visceral leishmaniasis (kala azar). (a): H&E and (b): 1:500 dilution of the patient’s own serum (inset: high-power view). Non-caseous epithelioid granulomas are dispersed in the liver parenchyma. Antibodies in the patients’ own serum identify red cell-sized positive signals in the cytoplasm of epithelioid cells and Kupffer cells. Although the specificity of the patient’s serum is totally unknown in this case, it significantly contributed to suggest the causative pathogens to be protozoa. The nuclei in panel (b) are counterstained with methyl green.
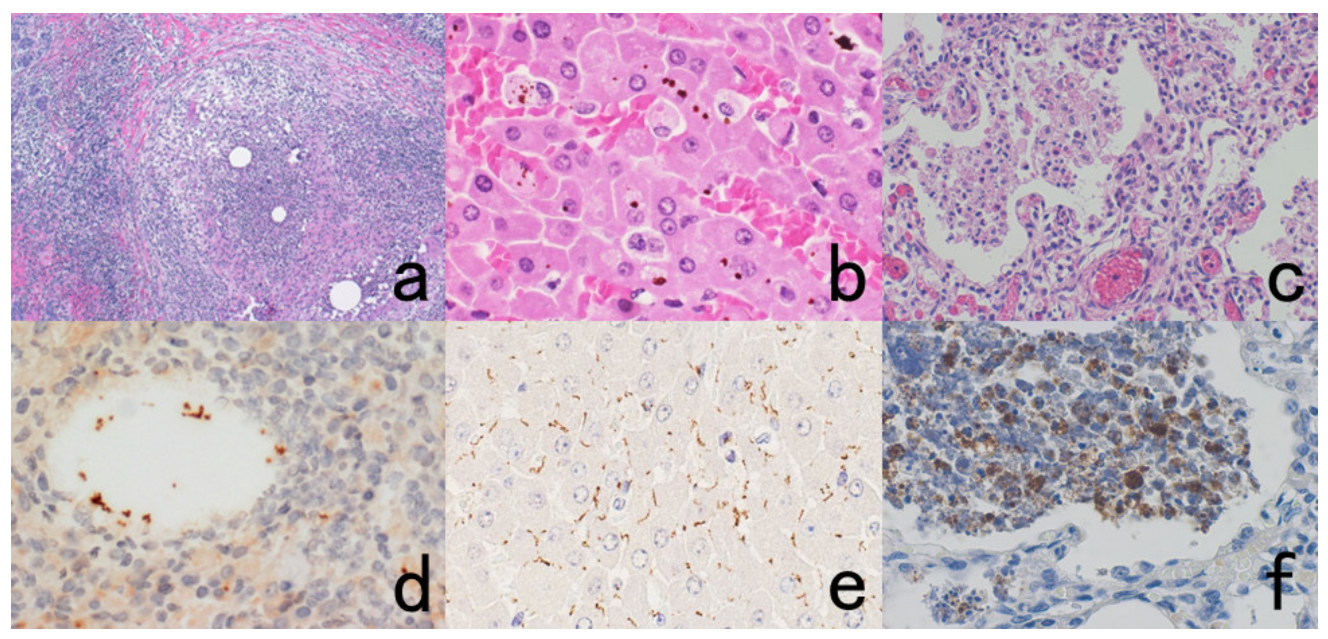
Figure 63.
Immunostaining with another patient’s serum (II). Left (a,c): H&E and Right (b,d): immunostaining with 1:500 dilution of serum from another case of balamuthiasis. Balamuthia mandrillaris infection in the skin (top panels: (a,b)) and brain (bottom panels: (c,d)) of the same patient. Trophozoites are visible in H&E-stained cutaneous panniculitis and chronic encephalitis, and they are strongly immunoreactive with the serum from another patient who suffered Balamuthia encephalitis.
Figure 63.
Immunostaining with another patient’s serum (II). Left (a,c): H&E and Right (b,d): immunostaining with 1:500 dilution of serum from another case of balamuthiasis. Balamuthia mandrillaris infection in the skin (top panels: (a,b)) and brain (bottom panels: (c,d)) of the same patient. Trophozoites are visible in H&E-stained cutaneous panniculitis and chronic encephalitis, and they are strongly immunoreactive with the serum from another patient who suffered Balamuthia encephalitis.
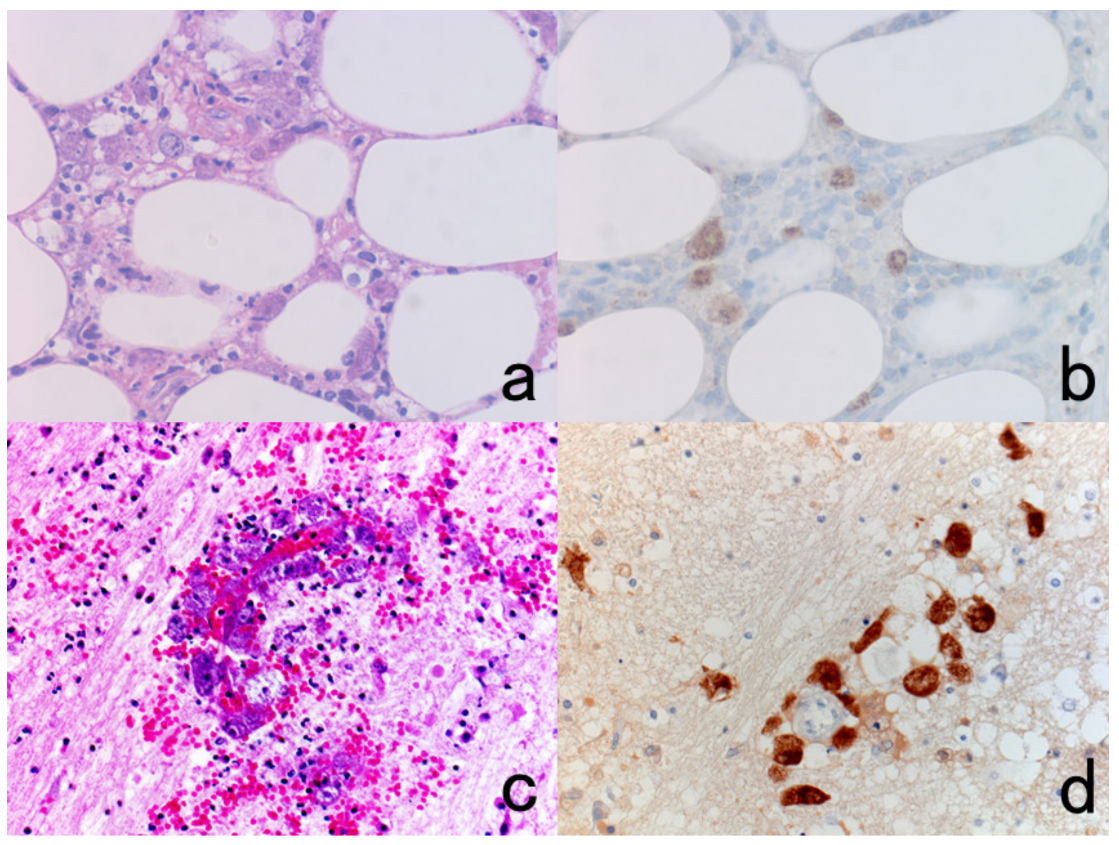
Figure 64.
Images of gastric parietal cells in FFPE sections with the serum of a patient with type A (autoimmune) gastritis ((a): low power, (b): high power). The patient’s 1:20 diluted serum, containing autoantibodies against proton pump (H+, K+-ATPase) molecules, decorates C-shaped intracytoplasmic structures (secretory canaliculi) in the acid-secreting parietal cells. The nuclei were counterstained with methyl green.
Figure 64.
Images of gastric parietal cells in FFPE sections with the serum of a patient with type A (autoimmune) gastritis ((a): low power, (b): high power). The patient’s 1:20 diluted serum, containing autoantibodies against proton pump (H+, K+-ATPase) molecules, decorates C-shaped intracytoplasmic structures (secretory canaliculi) in the acid-secreting parietal cells. The nuclei were counterstained with methyl green.
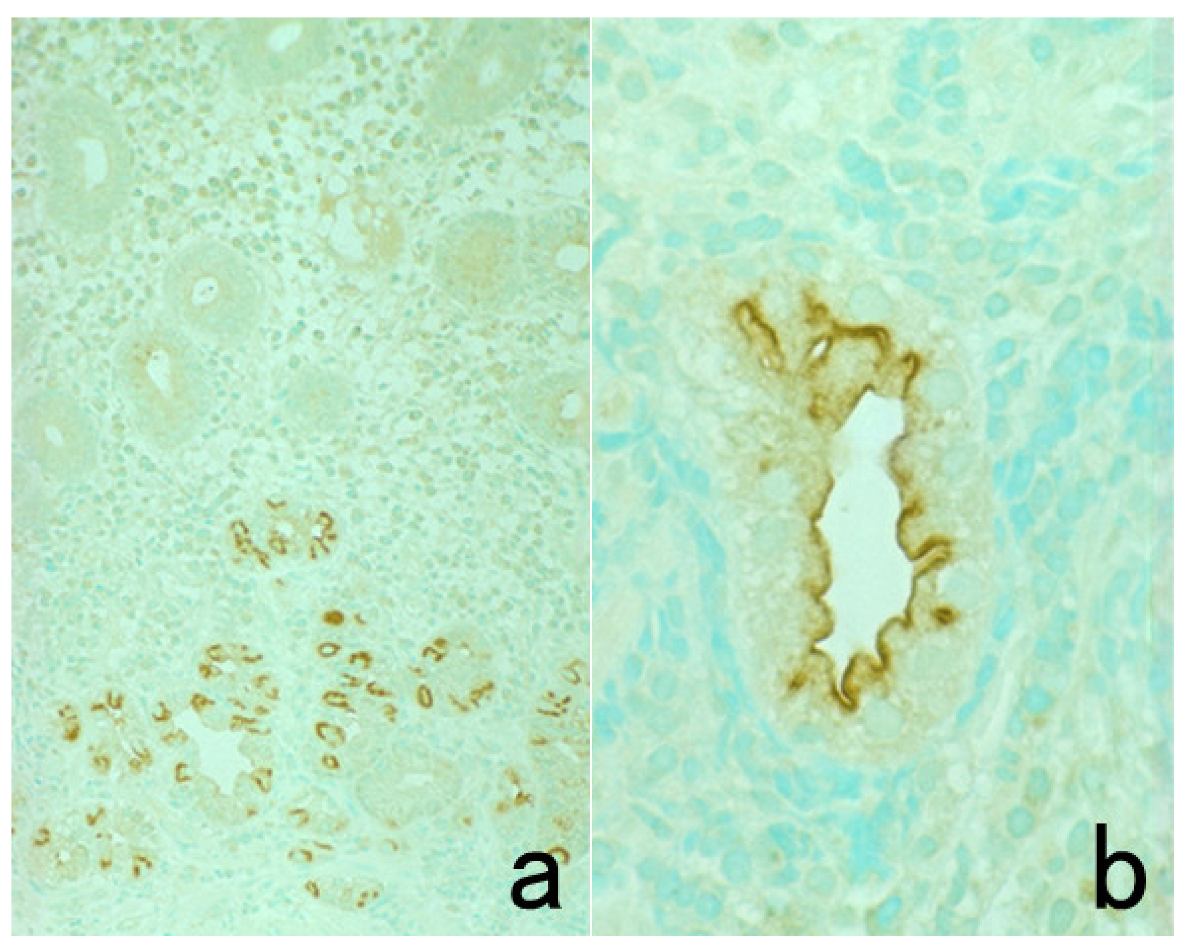
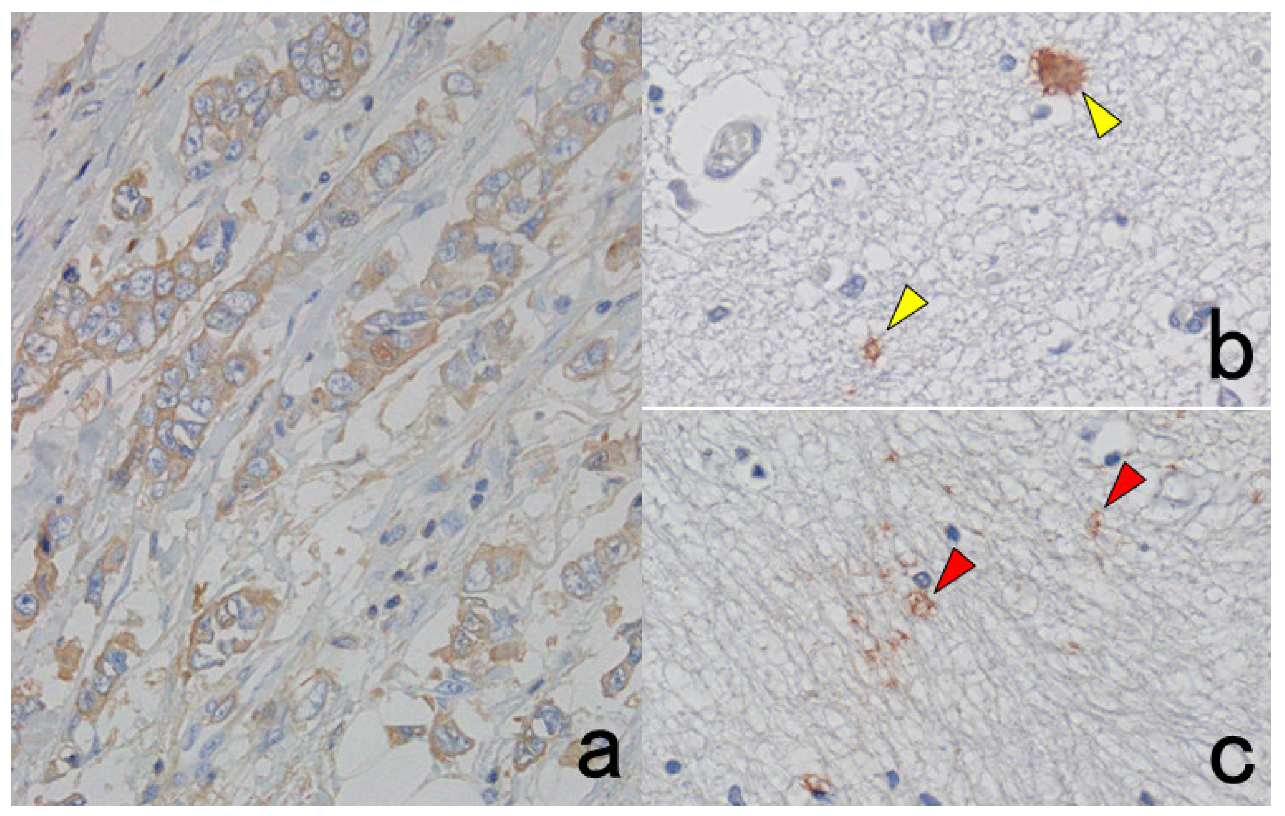
Figure 65.
Immunostaining with the serum of two patients with autoimmune encephalitis. (a): Paraneoplastic (breast cancer-associated) autoimmune encephalitis (Stiff-Man syndrome) with autoantibodies to amphiphysin, a 128-kDa presynaptic protein. (b,c): Autoimmune limbic encephalitis. The patient’s 1:20 diluted serum immunostains her own FFPE breast cancer cells (a). The 1:20 diluted serum of limbic encephalitis decorates astroglia (yellow arrowheads in panel (b)) and their glial processes (red arrowheads in panel (c)) in normal basal ganglia embedded in paraffin from another autopsy case.
Figure 65.
Immunostaining with the serum of two patients with autoimmune encephalitis. (a): Paraneoplastic (breast cancer-associated) autoimmune encephalitis (Stiff-Man syndrome) with autoantibodies to amphiphysin, a 128-kDa presynaptic protein. (b,c): Autoimmune limbic encephalitis. The patient’s 1:20 diluted serum immunostains her own FFPE breast cancer cells (a). The 1:20 diluted serum of limbic encephalitis decorates astroglia (yellow arrowheads in panel (b)) and their glial processes (red arrowheads in panel (c)) in normal basal ganglia embedded in paraffin from another autopsy case.