Collagen Fibril Diameter Distribution of Sheep Anterior Cruciate Ligament
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. ACL Tissue Isolation
2.3. Transmission Electron Microscopy
2.4. Measurements of Fibril Diameter
2.5. Fabrication of PCL Constructs
2.6. Mechanical Properties and Injured ACL Model
2.7. SEM Characterization
2.8. Statistical Analysis
3. Results
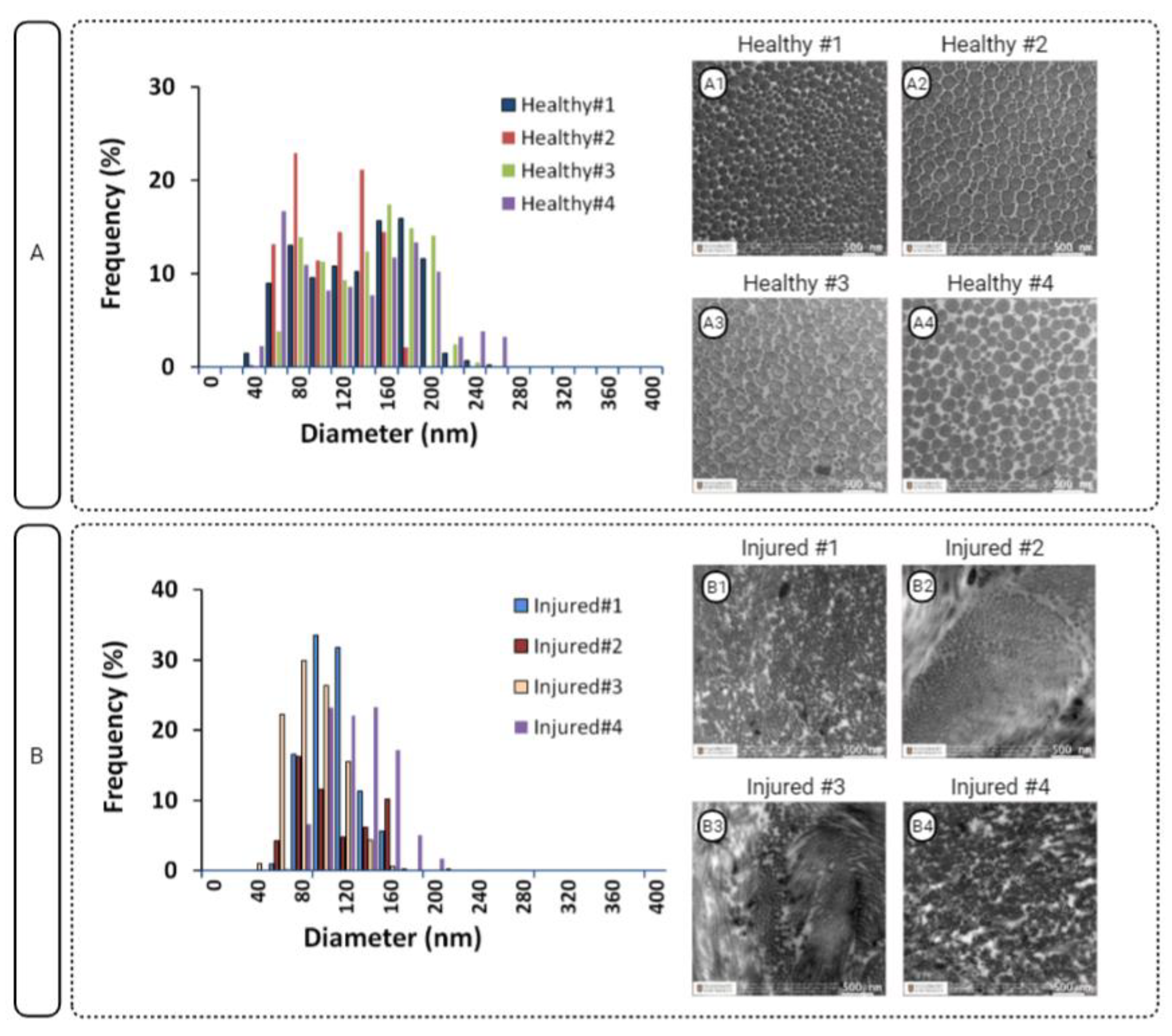
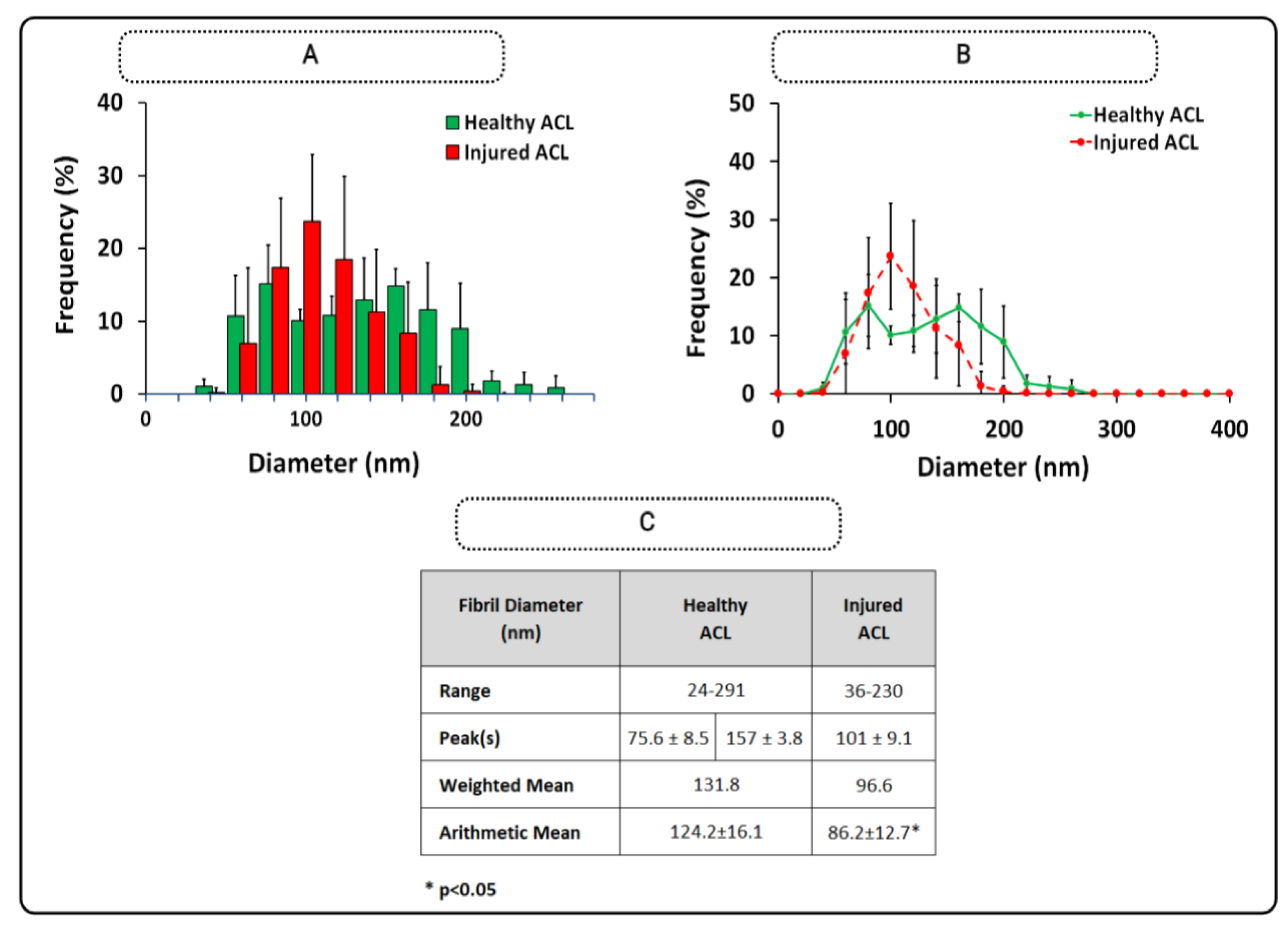
3.1. ACL Fibril Diameter
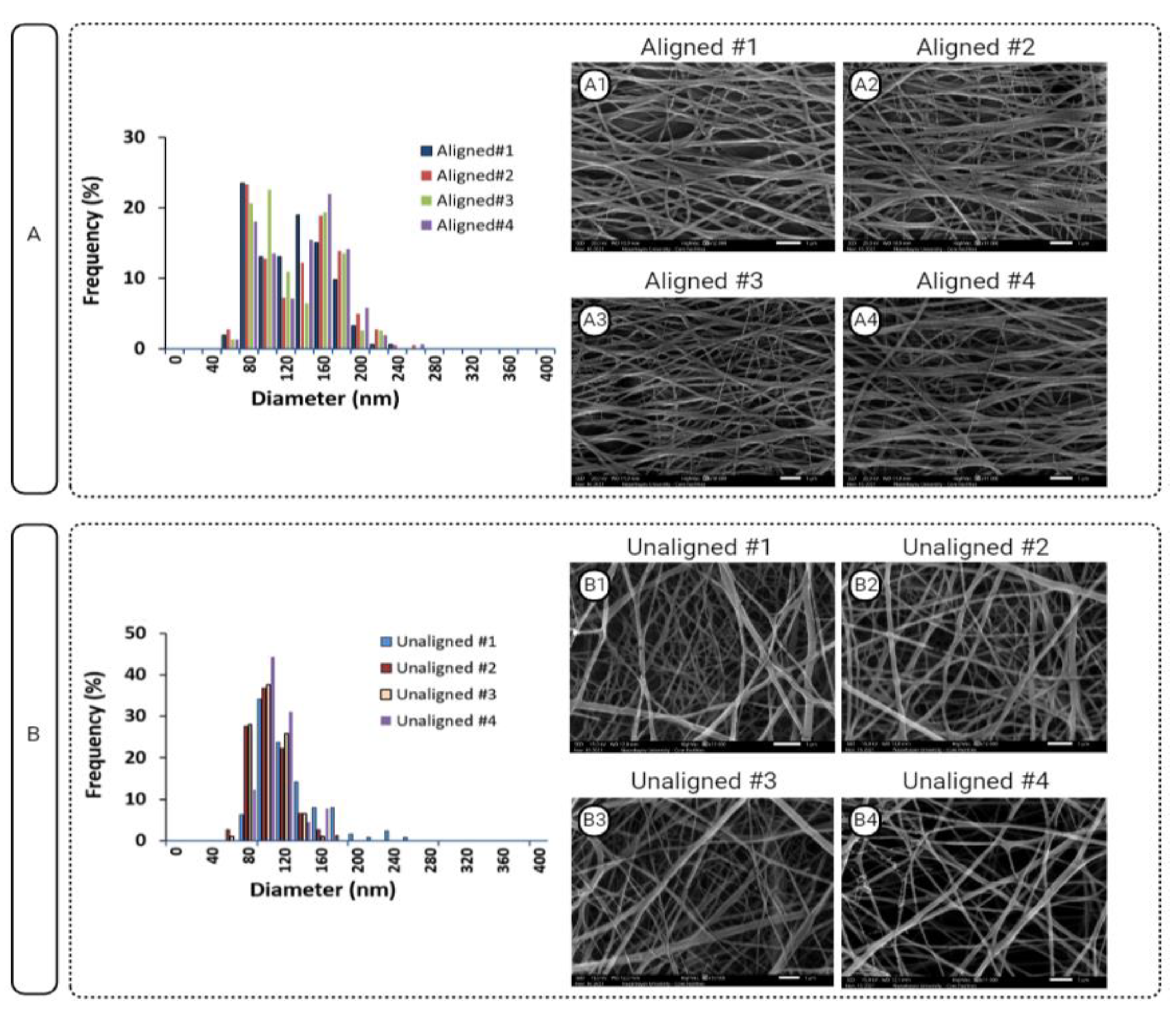
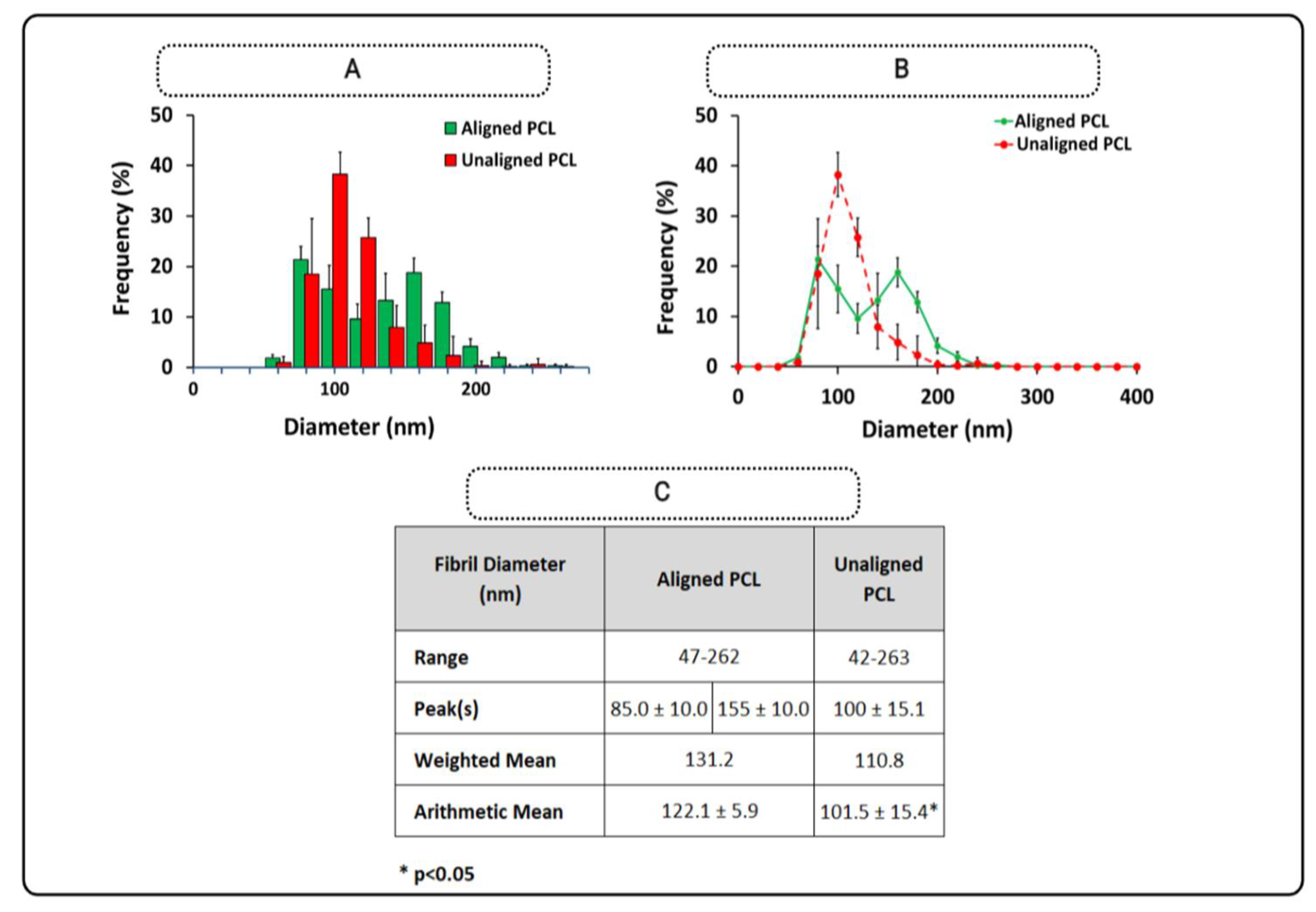
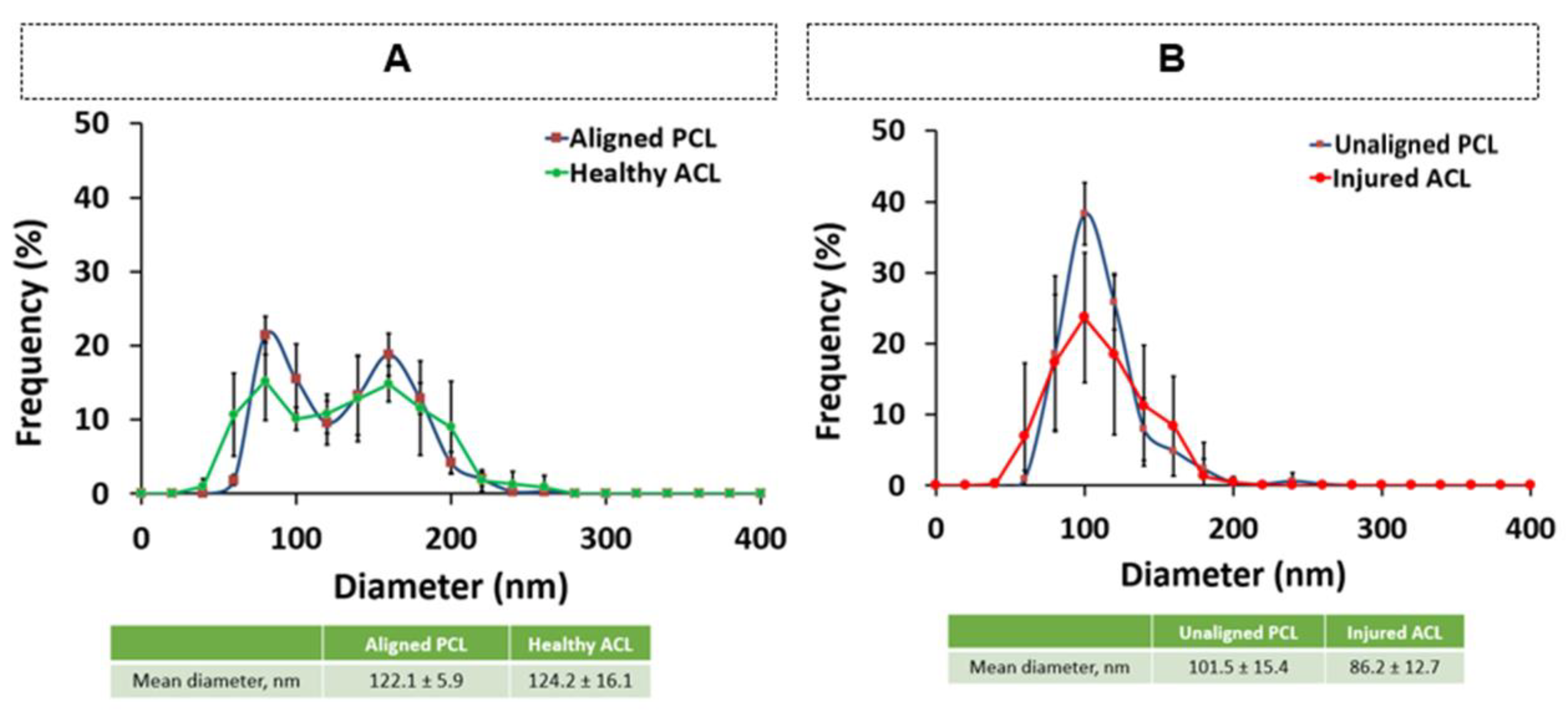
3.2. Fiber Diameter of PCL Constructs
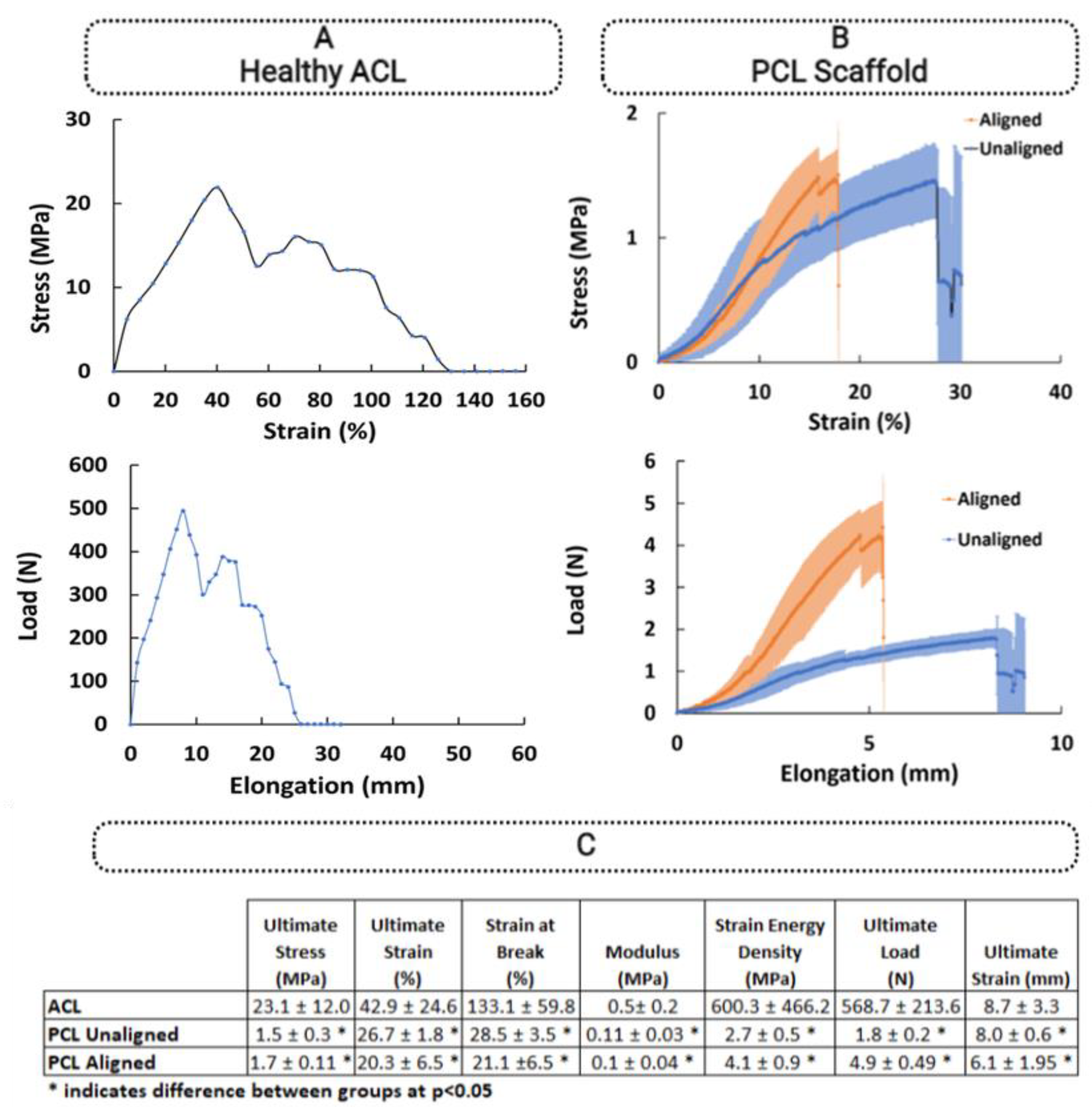
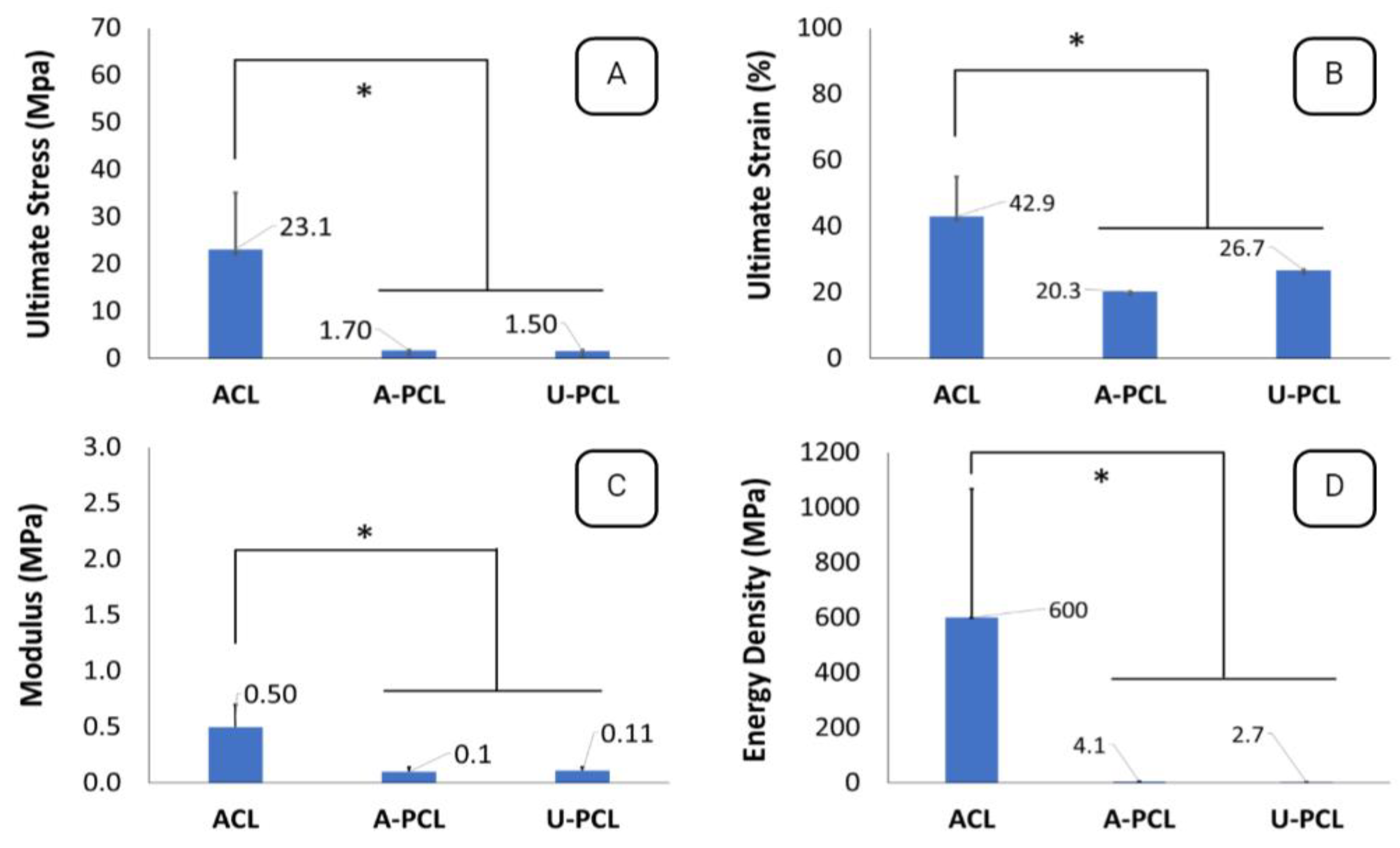
3.3. Comparison of Biomechanical Properties of ACL Tissue and PCL Constructs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lim, W.L.; Liau, L.L.; Ng, M.H.; Chowdhury, S.R.; Law, J.X. Current Progress in Tendon and Ligament Tissue Engineering. Tissue Eng. Regen. Med. 2019, 16, 549–571. [Google Scholar] [CrossRef] [PubMed]
- Zbrojkiewicz, D.; Vertullo, C.; Grayson, J.E. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2005. Med. J. Aust. 2018, 208, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Abram, S.G.; Judge, A.; Beard, D.J.; Price, A.J. Rates of Adverse Outcomes and Revision Surgery After Anterior Cruciate Ligament Reconstruction: A Study of 104,255 Procedures Using the National Hospital Episode Statistics Database for England, UK. Am. J. Sports Med. 2019, 47, 2533–2542. [Google Scholar] [CrossRef] [PubMed]
- Hootman, J.M.; Dick, R.; Agel, J. Epidemiology of collegiate injuries for 15 sports: Summary and recommendations for injury prevention initiatives. J. Athl. Train. 2007, 42, 311–319. [Google Scholar]
- Zhang, C.; Zhu, J.; Zhou, Y.; Thampatty, B.P.; Wang, J.H.-C. Tendon Stem/Progenitor Cells and Their Interactions with Extracellular Matrix and Mechanical Loading. Stem Cells Int. 2019, 2019, 3674647. [Google Scholar] [CrossRef]
- Frank, C.B. Ligament structure, physiology and function. J. Musculoskelet. Neuronal Interact. 2004, 4, 199–201. [Google Scholar]
- Duthon, V.L.A.; Barea, C.; Abrassart, S.; Fasel, J.H.; Fritschy, D.; Menetrey, J. Anatomy of the anterior cruciate ligament. Knee Surg. Sport. Traumatol. Arthrosc. 2005, 14, 204–213. [Google Scholar] [CrossRef]
- Marieswaran, M.; Jain, I.; Garg, B.; Sharma, V.; Kalyanasundaram, D. A Review on Biomechanics of Anterior Cruciate Ligament and Materials for Reconstruction. Appl. Bionics Biomech. 2018, 2018, 4657824. [Google Scholar] [CrossRef]
- Fujie, H. Mechanical properties and biomechanical function of the ACL. In ACL Injury and Its Treatment; Springer: Tokyo, Japan, 2016; pp. 69–77. [Google Scholar] [CrossRef]
- Adeoye, A.O.; Mukasheva, F.; Smatov, S.; Khumyrzakh, B.; Kadyr, S.; Shulgau, Z.; Erisken, C. A biomimetic synthetic nanofiber-based model for anterior cruciate ligament regeneration. Front. Bioeng. Biotechnol. 2022, 10, 969282. [Google Scholar] [CrossRef]
- Hart, R.A.; Akeson, W.H.; Spratt, K.; Amiel, D. Collagen fibril diameter distributions in rabbit anterior cruciate and medial collateral ligaments: Changes with maturation. Iowa Orthop. J. 1999, 19, 66–70. [Google Scholar]
- Rumian, A.P.; Wallace, A.L.; Birch, H. Tendons and ligaments are anatomically distinct but overlap in molecular and morphological features—A comparative study in an ovine model. J. Orthop. Res. 2007, 25, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Beisbayeva, Z.; Zhanbassynova, A.; Kulzhanova, G.; Mukasheva, F.; Erisken, C. Change in Collagen Fibril Diameter Distribution of Bovine Anterior Cruciate Ligament upon Injury Can Be Mimicked in a Nanostructured Scaffold. Molecules 2021, 26, 1204. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Zhang, X.; Ma, Y.; Zhou, C.; Ao, Y. Ultrastructural and Morphological Characteristics of Human Anterior Cruciate Ligament and Hamstring Tendons. Anat. Rec. 2012, 295, 1430–1436. [Google Scholar] [CrossRef] [PubMed]
- Friedrich Neurath, M.; Stofft, E.; Neurath, M.F.; Stofft, E. Collagen ultrastructure in ruptured cruciate ligaments: An electron microscopic investigation. Acta Orthop. 1992, 63, 507–510. [Google Scholar] [CrossRef] [PubMed]
- Samavedi, S.; Vaidya, P.; Gaddam, P.; Whittington, A.R.; Goldstein, A.S. Electrospun meshes possessing region-wise differences in fiber orientation, diameter, chemistry and mechanical properties for engineering bone-ligament-bone tissues. Biotechnol. Bioeng. 2014, 111, 2549–2559. [Google Scholar] [CrossRef] [PubMed]
- Criscenti, G.; Longoni, A.; Di Luca, A.; De Maria, C.; Van Blitterswijk, C.A.; Vozzi, G.; Moroni, L. Triphasic scaffolds for the regeneration of the bone–ligament interface. Biofabrication 2016, 8, 015009. [Google Scholar] [CrossRef]
- Deng, T.; Lv, J.; Pang, J.; Liu, B.; Ke, J. Construction of tissue-engineered osteochondral composites and repair of large joint defects in rabbit. J. Tissue Eng. Regen. Med. 2012, 8, 546–556. [Google Scholar] [CrossRef]
- He, J.; Jiang, N.; Qin, T.; Zhang, W.; Liu, Z.; Liu, Y.; Li, D. Microfiber-reinforced nanofibrous scaffolds with structural and material gradients to mimic ligament-to-bone interface. J. Mater. Chem. B 2017, 5, 8579–8590. [Google Scholar] [CrossRef]
- Samavedi, S.; Horton, C.O.; Guelcher, S.A.; Goldstein, A.S.; Whittington, A.R. Fabrication of a model continuously graded co-electrospun mesh for regeneration of the ligament–bone interface. Acta Biomater. 2011, 7, 4131–4138. [Google Scholar] [CrossRef]
- Samavedi, S.; Guelcher, S.A.; Goldstein, A.S.; Whittington, A. Response of bone marrow stromal cells to graded co-electrospun scaffolds and its implications for engineering the ligament-bone interface. Biomaterials 2012, 33, 7727–7735. [Google Scholar] [CrossRef]
- Robi, K.; Jakob, N.; Matevz, K.; Matjaz, V. The Physiology of Sports Injuries and Repair Processes; Hamlin, M., Draper, N.K.Y., Eds.; IntechOpen: London, UK, 2013. [Google Scholar] [CrossRef]
- Kano, T.; Kokubun, T.; Murata, K.; Oka, Y.; Ozone, K.; Arakawa, K.; Morishita, Y.; Takayanagi, K.; Kanemura, N. Influence of the site of injury on the spontaneous healing response in a rat model of total rupture of the anterior cruciate ligament. Connect. Tissue Res. 2021, 63, 138–150. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Zhao, X.; Chen, S.; Du, C. Osteogenic and tenogenic induction of hBMSCs by an integrated nanofibrous scaffold with chemical and structural mimicry of the bone–ligament connection. J. Mater. Chem. B 2016, 5, 1015–1027. [Google Scholar] [CrossRef]
- Olvera, D.; Sathy, B.N.; Carroll, S.F.; Kelly, D.J. Modulating microfibrillar alignment and growth factor stimulation to regulate mesenchymal stem cell differentiation. Acta Biomater. 2017, 64, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Olvera, D.; Sathy, B.N.; Kelly, D.J. Spatial Presentation of Tissue-Specific Extracellular Matrix Components along Electrospun Scaffolds for Tissue Engineering the Bone–Ligament Interface. ACS Biomater. Sci. Eng. 2020, 6, 5145–5161. [Google Scholar] [CrossRef] [PubMed]
- Erisken, C.; Kalyon, D.M.; Wang, H. A hybrid twin screw extrusion/electrospinning method to process nanoparticle-incorporatedelectrospun nanofibres. Nanotechnology 2008, 19, 165302. [Google Scholar] [CrossRef] [PubMed]
- Lindboe, C.F.; Fjeld, T.O.; Steen, H. Morphological changes in continuously stretched skeletal muscles in sheep. Eur. J. Appl. Physiol. 1985, 54, 184–190. [Google Scholar] [CrossRef]
- Muellner, T.; Kwasny, O.; Loehnert, V.; Mallinger, R.; Unfried, G.; Schabus, R.; Plenk, H., Jr. Light and electron microscopic study of stress-shielding effects on rat patellar tendon. Arch. Orthop. Trauma Surg. 2001, 121, 561–565. [Google Scholar] [CrossRef]
- Lee, J.B.; Ko, Y.-G.; Cho, D.; Park, W.H.; Kim, B.N.; Lee, B.C.; Kang, I.-K.; Kwon, O.H. Modification of PLGA Nanofibrous Mats by Electron Beam Irradiation for Soft Tissue Regeneration. J. Nanomater. 2015, 2015, 295807. [Google Scholar] [CrossRef]
- Erisken, C.; Tsiantis, A.; Papathanasiou, T.; Karvelas, E. Collagen fibril diameter distribution affects permeability of ligament tissue: A computational study on healthy and injured tissues. Comput. Methods Programs Biomed. 2020, 196, 105554. [Google Scholar] [CrossRef]
- Mahajan, P.S.; Chandra, P.; Negi, V.C.; Jayaram, A.P.; Hussein, S.A. Smaller Anterior Cruciate Ligament Diameter Is a Predictor of Subjects Prone to Ligament Injuries: An Ultrasound Study. BioMed Res. Int. 2015, 2015, 845689. [Google Scholar] [CrossRef]
- Johnston, J.M.; Connizzo, B.K.; Shetye, S.S.; Robinson, K.A.; Huegel, J.; Rodriguez, A.B.; Sun, M.; Adams, S.M.; Birk, D.E.; Soslowsky, L.J. Collagen V haploinsufficiency in a murine model of classic Ehlers-Danlos syndrome is associated with deficient structural and mechanical healing in tendons. J. Orthop. Res. 2017, 35, 2707–2715. [Google Scholar] [CrossRef] [PubMed]
- Proffen, B.L.; McElfresh, M.; Fleming, B.C.; Murray, M.M. A comparative anatomical study of the human knee and six animal species. Knee 2011, 19, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, E.C.; Chin, M.; Aoyama, J.T.; Ganley, T.J.; Shea, K.G.; Hast, M.W. Mechanical and Microstructural Properties of Native Pediatric Posterior Cruciate and Collateral Ligaments. Orthop. J. Sports Med. 2019, 7, 2325967118824400. [Google Scholar] [CrossRef] [PubMed]
- Asai, K.; Nakase, J.; Ishikawa, T.; Yoshimizu, R.; Kimura, M.; Ozaki, N.; Tsuchiya, H. Differences in cellular and microstructural properties of the semitendinosus muscle tendon between young and adult patients. J. Orthop. Sci. 2021, 27, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Gurlek, A.C.; Sevinc, B.; Bayrak, E.; Erisken, C. Synthesis and characterization of polycaprolactone for anterior cruciate ligament regeneration. Mater. Sci. Eng. C 2017, 71, 820–826. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Garrett, W.E. Mechanisms of non-contact ACL injuries. Br. J. Sports Med. 2007, 41 (Suppl. S1), i47–i51. [Google Scholar] [CrossRef]

| Specie | Peak for Healthy Tissue (nm) | Range Healthy (nm) | Peak Value for Injured Tissue (nm) | Range Injured (nm) | Reference | |
|---|---|---|---|---|---|---|
| Smaller | Larger | |||||
| Rat ACL | ~60 | ~150 | 20–260 | ~125 | 20–220 | [10] |
| Rabbit ACL | ~20 | ~250 | 10–320 | NR | NR | [11] |
| Sheep ACL | ~60 | ~200 | 20–300 | NR | NR | [12] |
| Bovine ACL | ~73 | ~210 | 20–320 | ~100 | 40–200 | [13] |
| Human ACL | ~50 | ~150 | 20–200 | NR | NR | [14] |
| Human ACL | ~75 | NR | 20–185 | 71 | 20–290 | [15] |
| Thickness mm | Width mm | Area (mm2) | Length (mm) | |
|---|---|---|---|---|
| Joint#1 | 3.59 | 6.05 | 21.74 | 21.30 |
| Joint#2 | 3.77 | 4.51 | 16.99 | 15.67 |
| Joint#3 | 4.69 | 6.11 | 28.64 | 16.09 |
| Joint#4 | 4.30 | 5.34 | 22.99 | 25.14 |
| PCL 11% | Thickness mm | Width mm | Area (mm2) | Length mm |
|---|---|---|---|---|
| Scaffold#1 | 0.09 | 10.00 | 0.90 | 30.00 |
| Scaffold#2 | 0.14 | 10.00 | 1.37 | 30.00 |
| Scaffold#3 | 0.12 | 10.00 | 1.23 | 30.00 |
| Scaffold#4 | 0.13 | 10.00 | 1.27 | 30.00 |
| Scaffold#5 | 0.16 | 10.00 | 1.57 | 30.00 |
| PCL 8% + 15% | Thickness mm | Width mm | Area (mm2) | Length mm |
|---|---|---|---|---|
| Scaffold#1 | 0.23 | 10.00 | 2.33 | 30.00 |
| Scaffold#2 | 0.29 | 10.00 | 2.93 | 30.00 |
| Scaffold#3 | 0.29 | 10.00 | 2.93 | 30.00 |
| Scaffold#4 | 0.30 | 10.00 | 2.97 | 30.00 |
| Scaffold#5 | 0.26 | 10.00 | 2.60 | 30.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smatov, S.; Mukasheva, F.; Erisken, C. Collagen Fibril Diameter Distribution of Sheep Anterior Cruciate Ligament. Polymers 2023, 15, 752. https://doi.org/10.3390/polym15030752
Smatov S, Mukasheva F, Erisken C. Collagen Fibril Diameter Distribution of Sheep Anterior Cruciate Ligament. Polymers. 2023; 15(3):752. https://doi.org/10.3390/polym15030752
Chicago/Turabian StyleSmatov, Smail, Fariza Mukasheva, and Cevat Erisken. 2023. "Collagen Fibril Diameter Distribution of Sheep Anterior Cruciate Ligament" Polymers 15, no. 3: 752. https://doi.org/10.3390/polym15030752
APA StyleSmatov, S., Mukasheva, F., & Erisken, C. (2023). Collagen Fibril Diameter Distribution of Sheep Anterior Cruciate Ligament. Polymers, 15(3), 752. https://doi.org/10.3390/polym15030752







