The Influence of rhBMP-7 Associated with Nanometric Hydroxyapatite Coatings Titanium Implant on the Osseointegration: A Pre-Clinical Study
Abstract
:1. Introduction
2. Materials and Methods
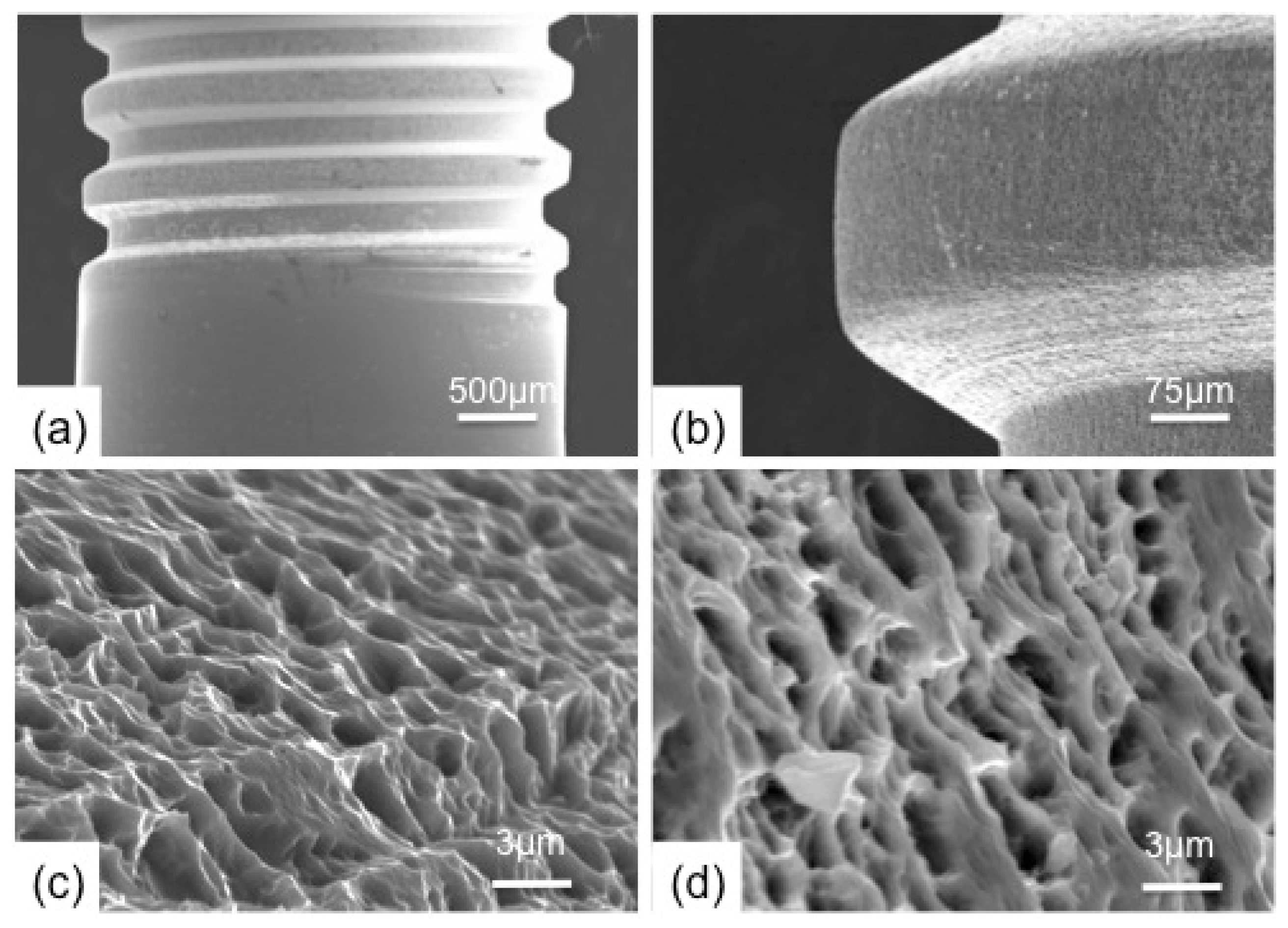
2.1. Implant Surface and Characterization
2.2. In Vivo Experiment
2.3. Histomorphometric Analysis
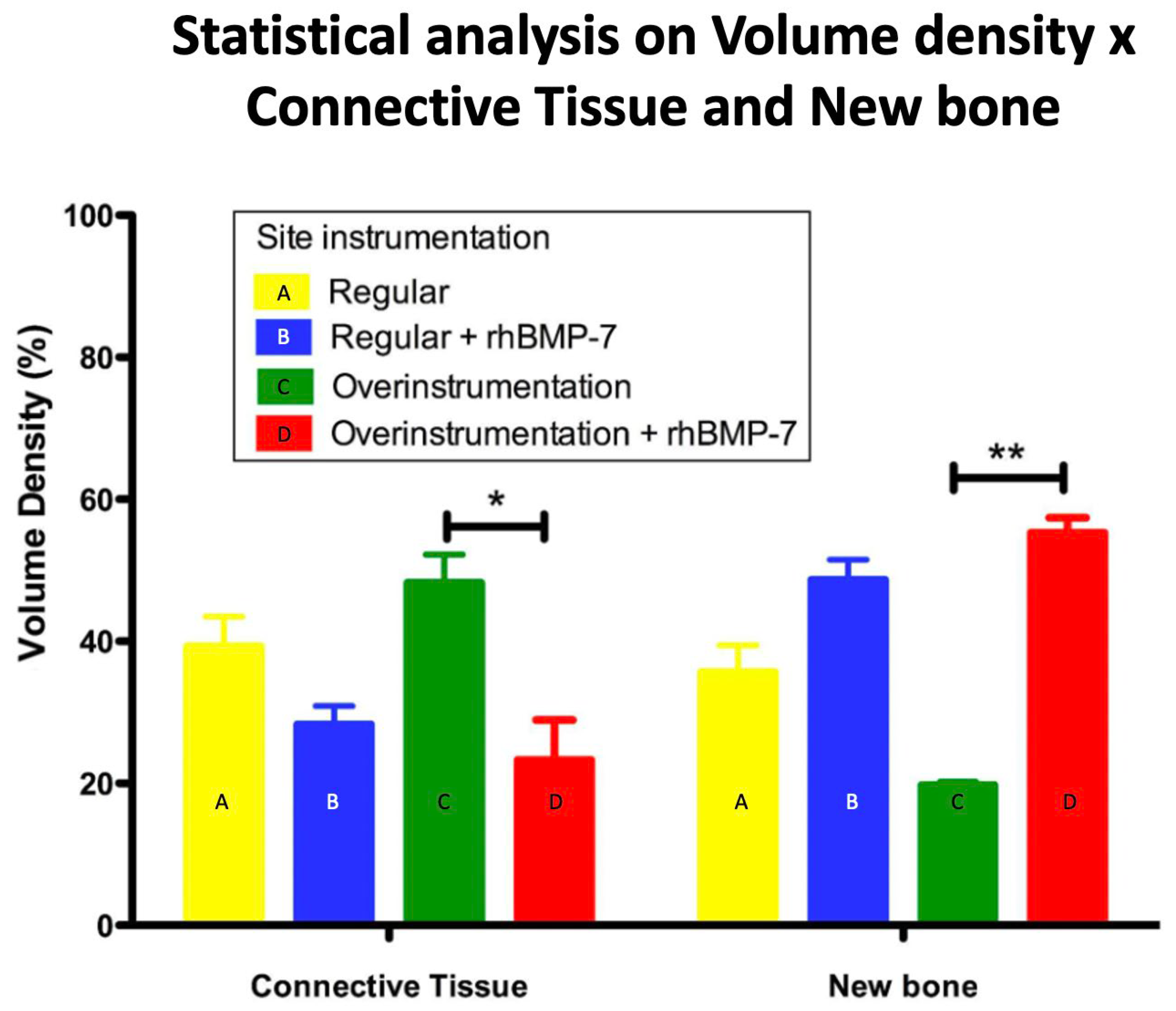
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| BMP | Bone morphogenetic protein |
| BIC | Bone-to-implant contact |
| Calcium and Phosphate | Ca- and P- |
| °C | Celsius degree |
| eV | electron Volts |
| FTIR | Fourier Transform Infrared Spectrophotometry |
| FTIRM-ATR | Fourier Transformed Infrared Attenuated Total Reflectance Microscopy |
| GIXRD | Grazing-incidence X-ray diffraction technique |
| HA | Hydroxyapatite |
| OH | Hydroxide |
| MPa | MegaPascal |
| nm | Nanometer |
| RAMS | Right-angle magnetron sputtering |
| rhBMP-7 | Recombinant human bone morphogenetic protein-7 |
| SEM | Scanning electron microscope |
| XRD | X-ray diffraction |
References
- Borges, H.; Correia, A.R.M.; Castilho, R.M.; Fernandes, G.V.O. Zirconia Implants and Marginal Bone Loss: A Systematic Review and Meta-Analysis of Clinical Studies. Int. J. Oral Maxillofac. Implant. 2020, 35, 707–720. [Google Scholar] [CrossRef] [PubMed]
- Orsini, G.; Piattelli, M.; Scarano, A.; Petrone, G.; Kenealy, J.; Piattelli, A.; Caputi, S. Randomized, controlled histologic and histomorphometric evaluation of implants with nanometer-scale calcium phosphate added to the dual acid-etched surface in the human posterior maxilla. J. Periodontol. 2007, 78, 209. [Google Scholar] [CrossRef] [PubMed]
- Buser, D. 20 Years of Guided Bone Regeneration in Implant Dentistry, 2nd ed.; Quintessence Books: New Malden, Surrey, UK, 2009. [Google Scholar]
- Albrektsson, T.; Wennerberg, A. Oral implant surfaces: Part 1—Review focusing on topographic and chemical properties of different surfaces and in vivo responses to them. Int. J. Prosthodont. 2004, 17, 536. [Google Scholar] [PubMed]
- Coelho, P.G.; Granjeiro, J.M.; Romanos, G.E.; Suzuki, M.; Silva, N.R.F.; Cardaropoli, G.; Thompson, V.P.; Lemons, J.E. Review: Basic Research Methods and Current Trends of Dental Implant Surfaces. J. Biomed. Mater. Res. Part B Appl. Biomater. 2009, 88B, 579–596. [Google Scholar] [CrossRef]
- Buser, D.; Schenk, R.K.; Steinemann, S.; Fiorellini, J.P.; Fox, C.H.; Stich, H. Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs. J. Biomed. Mater. Res. 1991, 25, 889. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Mericske-Stern, R.; Bernard, J.P.; Behneke, A.; Behneke, N.; Hirt, H.P.; Belser, U.C.; Lang, N.P. Long-term evaluation of non-submerged ITI implants. Part I. 8-Year life table analysis of a prospective multi-center study with 2359 implants. Clin. Oral Implant. Res. 1997, 8, 161. [Google Scholar] [CrossRef]
- Trisi, P.; Lazzara, R.; Rebaudi, A.; Rao, W.; Testori, T.; Porter, S.S. Bone–implant contact on machined and dual acid-etched surfaces after 2 months of healing in the human maxilla. J. Periodontol. 2003, 74, 945. [Google Scholar] [CrossRef]
- Cho, S.A.; Jung, S.K. A removal torque of the laser-treated titanium implants in rabbit tibia. Biomaterials 2003, 24, 4859. [Google Scholar] [CrossRef]
- Le Guéhennec, L.; Soueidan, A.; Layrolle, P.; Amouriq, Y. Surface treatments of titanium dental implants for rapid osseointegration. Dent. Mater. 2007, 23, 844–854. [Google Scholar] [CrossRef]
- Damerau, J.; Bierbaum, S.; Wiedemeier, D.; Korn, P.; Smeets, R.; Jenny, G.; Nadalini, J.; Stadlinger, B. A systematic review on the effect of inorganic surface coatings in large animal models and meta-analysis on tricalcium phosphate and hydroxyapatite on periimplant bone formation. J. Biomed. Mater. Res. B Appl. Biomater. 2022, 110, 157–175. [Google Scholar] [CrossRef]
- Hall, J.; Sorensen, R.G.; Wozney, J.M.; Wikesjö, U.M. Bone formation at rhBMP-2-coated titanium implants in the rat ectopic model. J. Clin. Periodontol. 2007, 34, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Marin, C.; Granato, R.; Suzuki, M.; Gil, J.N.; Piattelli, A.; Coelho, P.G. Removal torque and histomorphometric evaluation of bioceramic grit-blasted/acid-etched and dual acid-etched implant surfaces: An experimental study in dogs. J. Periodontol. 2008, 79, 1942–1949. [Google Scholar] [CrossRef] [PubMed]
- Coelho, P.G.; Cardaropoli, G.; Suzuki, M.; Lemons, J.E. Histomorphometric evaluation of a nanothickness bioceramic deposition on endosseous implants: A study in dogs. Clin. Implant. Dent. Relat. Res. 2009, 11, 292–302. [Google Scholar] [CrossRef]
- Silva, R.C.S.; Agrelli, A.; Andrade, A.N.; Mendes-Marques, C.L.; Arruda, I.R.S.; Santos, L.R.L.; Vasconcelos, N.F.; Machado, G. Titanium Dental Implants: An Overview of Applied Nanobiotechnology to Improve Biocompatibility and Prevent Infections. Materials 2022, 15, 3150. [Google Scholar] [CrossRef]
- Lee, J.; Decker, J.F.; Polimeni, G.; Cortella, C.A.; Rohrer, M.D.; Wozney, J.M.; Hall, J.; Susin, C.; Wikesjö, U.M. Evaluation of implants coated with rhBMP-2 using two different coating strategies: A critical-size supraalveolar peri-implant defect study in dogs. J. Clin. Periodontol. 2010, 37, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, C.S.; Choi, K.H.; Jung, U.W.; Yun, J.H.; Choi, S.H.; Cho, K.S. The induction of bone formation in rat calvarial defects and subcutaneous tissues by recombinant human BMP-2, produced in Escherichia coli. Biomaterials 2010, 31, 3512–3519. [Google Scholar] [CrossRef] [PubMed]
- Hägi, T.T.; Wu, G.; Liu, Y.; Hunziker, E.B. Cell-mediated BMP-2 liberation promotes bone formation in a mechanically unstable implant environment. Bone 2010, 46, 1322–1327. [Google Scholar] [CrossRef]
- Mello, A.; Hong, Z.; Rossi, A.M.; Luan, L.; Farina, M.; Querido, W.; Eon, J.; Terra, J.; Balasundaram, G.; Webster, T.; et al. Osteoblast proliferation on hydroxyapatite thin coatings produced by right angle magnetron sputtering. Biomed. Mater. 2007, 2, 67–77. [Google Scholar] [CrossRef]
- Hong, Z.; Mello, A.; Yoshida, T.; Luan, L.; Stern, P.H.; Rossi, A.; Ellis, D.E.; Ketterson, J.B. Osteoblast proliferation on hydroxyapatite coated substrates prepared by right angle magnetron sputtering. J. Biomed. Mater. Res. A 2010, 93, 878–885. [Google Scholar] [CrossRef]
- Vercaigne, S.; Wolke, J.G.; Naert, I.; Jansen, J.A. Bone healing capacity of titanium plasma-sprayed and hydroxylapatite-coated oral implants. Clin. Oral Implant. Res. 1998, 9, 261–271. [Google Scholar] [CrossRef]
- Granjeiro, J.M.; Oliveira, R.C.; Bustos-Valenzuela, J.C.; Sogayar, M.C.; Taga, R. Bone morphogenetic proteins: From structure to clinical use. Braz J. Med. Biol. Res. 2005, 38, 1463–1473. [Google Scholar] [CrossRef] [PubMed]
- Canter, H.I.; Vargel, I.; Korkusuz, P.; Oner, F.; Gungorduk, D.B.; Cil, B.; Karabulut, E.; Sargon, M.F.; Erk, Y. Effect of use of slow release of bone morphogenetic protein-2 and transforming growth factor-Beta-2 in a chitosan gel matrix on cranial bone graft survival in experimental cranial critical size defect model. Ann. Plast. Surg. 2010, 64, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Giannoudis, P.V.; Kanakaris, N.K.; Dimitriou, R.; Gill, I.; Kolimarala, V.; Montgomery, R.J. The synergistic effect of autograft and BMP-7 in the treatment of atrophic nonunions. Clin. Orthop. Relat. Res. 2009, 467, 3239–3248. [Google Scholar] [CrossRef] [PubMed]
- Dawson, E.; Bae, H.W.; Burkus, J.K.; Stambough, J.L.; Glassman, S.D. Recombinant human bone morphogenetic protein-2 on an absorbable collagen sponge with an osteoconductive bulking agent in posterolateral arthrodesis with instrumentation. A prospective randomized trial. J. Bone Joint Surg. Am. 2009, 91, 1604–1613. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Windisch, S.I.; Eggenschwiler, A.M.; Thoma, D.S.; Weber, F.E.; Hammerle, C.H. A randomized-controlled clinical trial evaluating clinical and radiological outcomes after 3 and 5 years of dental implants placed in bone regenerated by means of GBR techniques with or without the addition of BMP-2. Clin. Oral Implant. Res. 2009, 20, 660–666. [Google Scholar] [CrossRef]
- Nemcakova, I.; Litvinec, A.; Mandys, V.; Potocky, S.; Plencner, M.; Doubkova, M.; Nanka, O.; Olejnickova, V.; Sankova, B.; Bartos, M.; et al. Coating Ti6Al4V implants with nanocrystalline diamond functionalized with BMP-7 promotes extracellular matrix mineralization in vitro and faster osseointegration in vivo. Sci. Rep. 2022, 12, 5264. [Google Scholar] [CrossRef]
- Helbig, L.; Omlor, G.W.; Ivanova, A.; Guehring, T.; Sonntag, R.; Kretzer, J.P.; Minkwitz, S.; Wildemann, B.; Schmidmaier, G. Bone morphogenetic proteins −7 and −2 in the treatment of delayed osseous union secondary to bacterial osteitis in a rat model. BMC Musculoskelet. Disord. 2018, 19, 261. [Google Scholar] [CrossRef] [PubMed]
- Bustos-Valenzuela, J.C.; Halcsik, E.; Bassi, E.J.; Demasi, M.A.; Granjeiro, J.M.; Sogayar, M.C. Expression, Purification, Bioactivity, and Partial Characterization of a Recombinant Human Bone Morphogenetic Protein-7 Produced in Human 293T. Cells Mol. Biotechnol. 2010, 46, 118–126. [Google Scholar] [CrossRef]
- Albrektsson, T.; Wennerberg, A. Oral implant surfaces: Part 2—Review focusing on clinical knowledge of different surfaces. Int. J. Prosthodont. 2004, 17, 544. [Google Scholar]
- Fernandes, G.V.O.; Costa, B.M.G.N.; Trindade, H.F.; Castilho, R.M.; Fernandes, J.C.H. Comparative analysis between extra-short implants (≤6 mm) and 6 mm-longer implants: A meta-analysis of randomized controlled trial. Aust. Dental J. 2022, 1–18. [Google Scholar] [CrossRef]
- Schierano, G.; Canuto, R.A.; von Degerfeld, M.M.; Navone, R.; Peirone, B.; Preti, G.; Muzio, G. Role of rhBMP-7, Fibronectin, And Type I Collagen in Dental Implant Osseointegration Process: An Initial Pilot Study on Minipig Animals. Materials 2021, 14, 2185. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Kim, K.H.; Ong, J.L. A review on calcium phosphate coatings produced using a sputtering process–an alternative to plasma spraying. Biomaterials 2005, 26, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Daugaard, H.; Elmengaard, B.; Bechtold, J.E.; Jensen, T.; Soballe, K. The effect on bone growth enhancement of implant coatings with hydroxyapatite and collagen deposited electrochemically and by plasma spray. J. Biomed. Mater. Res. 2010, 92A, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Misch, C.E. Density of bone: Effect on treatment plans, surgical approach, healing, and progressive bone loading. Int. J. Oral Implantol. 1990, 6, 23–31. [Google Scholar] [PubMed]
- Esposito, M.; Murray-Curtis, L.; Grusovin, M.G.; Coulthard, P.; Worthington, H.V. Interventions for replacing missing teeth: Different types of dental implants. Cochrane Database Syst. Rev. 2007, 17, CD003815. [Google Scholar]
- Hsu, S.-H.; Liu, B.-S.; Lin, W.-H.; Chiang, H.-C.; Huang, S.-C.; Cheng, S.-S. Characterization and biocompatibility of a titanium dental implant with a laser irradiated and dual-acid etched surface. Biomed. Mater. Eng. 2007, 17, 53–68. [Google Scholar]
- Anselme, K.; Linez, P.; Bigerelle, M.; Le Maguer, D.; Le Maguer, A.; Hardouin, P.; Hildebrand, H.F.; Iost, A.; Leroy, J.M. The relative influence of the topography and chemistry of TiAl6V4 surfaces on osteoblastic cell behavior. Biomaterials 2000, 21, 1567–1577. [Google Scholar] [CrossRef]
- Matsuzaka, K.; Walboomers, X.F.; Yoshinari, M.; Inoue, T.; Jansen, J.A. The attachment and growth behavior of osteoblast-like cells on microtextured surfaces. Biomaterials 2003, 24, 2711–2719. [Google Scholar] [CrossRef]
- Sader, M.S.; Balduino, A.; Soares, G.A.; Borojevic, R. Effect of three distinct treatments of titanium surface on osteoblast attachment, proliferation, and differentiation. Clin. Oral Implant. Res. 2005, 16, 667–675. [Google Scholar] [CrossRef]
- Lemons, J.; Dietch-Misch, F. Biomaterials for Dental Implants. In Contemporary Implant Denstistry; Carl, E.M., Ed.; Mosby, Inc.: Saint Louis, MO, USA, 1999; pp. 271–302. [Google Scholar]
- Ong, J.L.; Carnes, D.L.; Bessho, K. Evaluation of titanium plasma-sprayed and plasma-sprayed hydroxyapatite implants in vivo. Biomaterials 2004, 25, 4601–4606. [Google Scholar] [CrossRef]
- Liu, Y.; Layrolle, P.; de Bruijn, J.; van Blitterswijk, C.; de Groot, K. Biomimetic coprecipitation of calcium phosphate and bovine serum albumin on titanium alloy. J. Biomed. Mater. Res. 2001, 57, 327–335. [Google Scholar] [CrossRef]
- Sul, Y.T.; Jönsson, J.; Yoon, G.S.; Johansson, C. Resonance frequency measurements in vivo and related surface properties of magnesium-incorporated, micropatterned and magnesium-incorporated TiUnite, Osseotite, SLA and TiOblast implants. Clin. Oral Implant. Res. 2009, 20, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Gedrange, T.; Gredes, T.; Gredes, M.; Allegrini, M.R.; Borsos, G.; Vegh, A.; Salles, M.B.; Heinemann, F.; Dominiak, M.; Allegrini, S., Jr. Comparative animal study on hard tissue integration and bone formation of different Nobel Biocare implants. J. Physiol. Pharmacol. 2009, 60 (Suppl. S8), 117–121. [Google Scholar] [PubMed]
- Susin, C.; Qahash, M.; Polimeni, G.; Lu, P.H.; Prasad, H.S.; Rohrer, M.D.; Hall, J.; Wikesjö, U.M. Alveolar ridge augmentation using implants coated with recombinant human bone morphogenetic protein-7 (rhBMP-7/rhOP-1), histological observations. J. Clin. Periodontol. 2010, 37, 574–581. [Google Scholar] [CrossRef]
- Wikesjö, U.M.E.; Qahash, M.; Huang, Y.-H.; Xiropaidis, A.; Polimeni, G.; Susin, C. Bone morphogenetic proteins for periodontal and alveolar indications; biological observations–clinical implications. Orthod. Craniofac. Res. 2009, 12, 263–270. [Google Scholar] [CrossRef]
- Freilich, M.; Patel, C.M.; Wei, M.; Shafer, D.; Schleier, P.; Hortschansky, P.; Kompali, R.; Kuhn, L. Growth of new bone guided by implants in a murine calvarial model. Bone 2008, 43, 781–788. [Google Scholar] [CrossRef]
- Leknes, K.N.; Yang, J.; Qahash, M.; Polimeni, G.; Susin, C.; Wikesjo, U.M.E. Alveolar ridge augmentation using implants coated with recombinant human bone morphogenetic protein-7 (rhBMP-7/rhOP-1): Radiographic observations. J. Clin. Periodontol. 2008, 35, 914–919. [Google Scholar] [CrossRef]
- Sachse, A.; Wagner, A.; Keller, M.; Wagner, O.; Wetzel, W.D.; Layher, F.; Venbrocks, R.A.; Hortschansky, P.; Pietraszczyk, M.; Wiederanders, B.; et al. Osteointegration of hydroxyapatite-titanium implants coated with nonglycosylated recombinant human bone morphogenetic protein-2 (BMP-2) in aged sheep. Bone 2005, 37, 699–710. [Google Scholar] [CrossRef]
- Wikesjö, U.M.E.; Qahash, M.; Polimeni, G.; Susin, C.; Shanaman, R.H.; Rohrer, M.D.; Wozney, J.M.; Hall, J. Alveolar ridge augmentation using implants coated with recombinant human bone morphogenetic protein-2 (rhBMP-2). Histologic observations. J. Clin. Periodontol. 2008, 35, 1001–1010. [Google Scholar] [CrossRef]
- Stenport, V.F.; Johansson, C.; Joo Heo, S.; Aspenberg, P.; Albrektsson, T. Titanium implants and BMP-7 in bone: An experimental model in the rabbit. J. Mater. Sci. Mater. Med. 2003, 14, 247–254. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonato, R.S.; Fernandes, G.V.d.O.; Calasans-Maia, M.D.; Mello, A.; Rossi, A.M.; Carreira, A.C.O.; Sogayar, M.C.; Granjeiro, J.M. The Influence of rhBMP-7 Associated with Nanometric Hydroxyapatite Coatings Titanium Implant on the Osseointegration: A Pre-Clinical Study. Polymers 2022, 14, 4030. https://doi.org/10.3390/polym14194030
Bonato RS, Fernandes GVdO, Calasans-Maia MD, Mello A, Rossi AM, Carreira ACO, Sogayar MC, Granjeiro JM. The Influence of rhBMP-7 Associated with Nanometric Hydroxyapatite Coatings Titanium Implant on the Osseointegration: A Pre-Clinical Study. Polymers. 2022; 14(19):4030. https://doi.org/10.3390/polym14194030
Chicago/Turabian StyleBonato, Rafael Silva, Gustavo Vicentis de Oliveira Fernandes, Monica Diuana Calasans-Maia, Alexandre Mello, Alexandre Malta Rossi, Ana Claudia Oliveira Carreira, Mari Cleide Sogayar, and José Mauro Granjeiro. 2022. "The Influence of rhBMP-7 Associated with Nanometric Hydroxyapatite Coatings Titanium Implant on the Osseointegration: A Pre-Clinical Study" Polymers 14, no. 19: 4030. https://doi.org/10.3390/polym14194030
APA StyleBonato, R. S., Fernandes, G. V. d. O., Calasans-Maia, M. D., Mello, A., Rossi, A. M., Carreira, A. C. O., Sogayar, M. C., & Granjeiro, J. M. (2022). The Influence of rhBMP-7 Associated with Nanometric Hydroxyapatite Coatings Titanium Implant on the Osseointegration: A Pre-Clinical Study. Polymers, 14(19), 4030. https://doi.org/10.3390/polym14194030