Glass Fiber Post Pretreated with Neodymium-Doped Yttrium Orthovanadate, Toluidine Blue Activated Low-Level Laser Therapy, and Bioactive Glass: An In Vitro Analysis of SEM, Bond Strength, and Surface Roughness
Abstract
1. Introduction
2. Materials and Methods
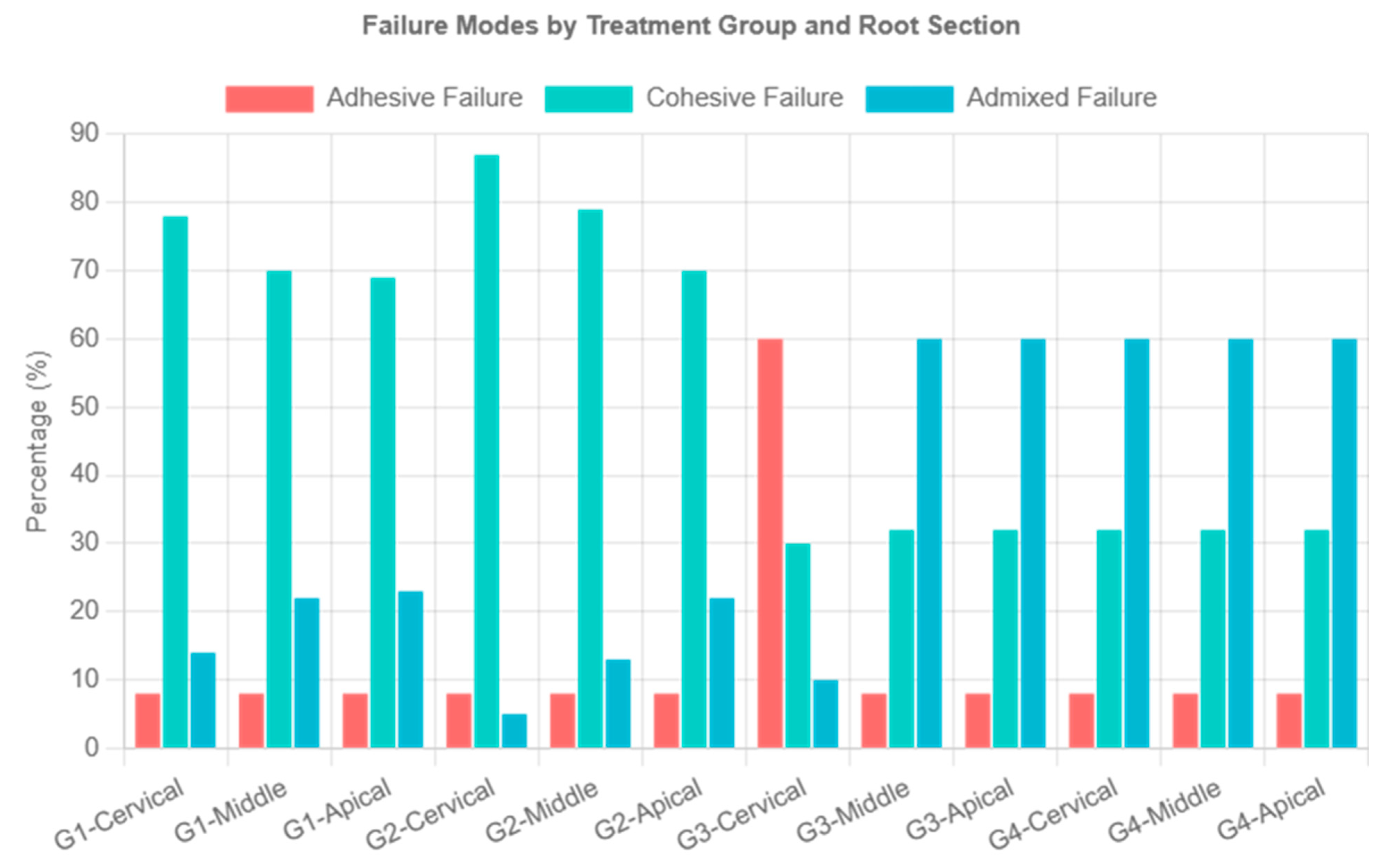
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wan, S.; Tan, Y.; Xie, J.; Huang, X.; Guo, L. The Effect of a Root-Dentin Pretreatment Technique Combining PIPS with MTAD Aiming to Improve the Bond Strength of Glass Fiber Post. Microsc. Res. Tech. 2020, 83, 824–833. [Google Scholar] [CrossRef] [PubMed]
- Maawadh, A.M.; Al Ahdal, K.; Al Deeb, L.; Alshamrani, A.S.; Almohareb, T.; Alrahlah, A. Effectiveness of Final Cavity Disinfectant Terminalia Chebula, Malachite, and Indocyanine Green, against E. Faecalis and on the Bond Interface of Fiber Post to Radicular Dentin. Photodiagn. Photodyn. Ther. 2023, 42, 103538. [Google Scholar] [CrossRef]
- Alshahrani, A.; Albaqami, M.; Naji, Z.; Al-Khunein, Y.; Alsubaie, K.; Alqahtani, A.; Al-Thobity, A.M. Impact of Different Surface Treatment Methods on Bond Strength between Fiber Post and Composite Core Material. Saudi Dent. J. 2021, 33, 334–341. [Google Scholar] [CrossRef]
- Santos, L.R.D.; Lima, D.M.; Carvalho, E.M.; Rodrigues, V.P.; Alves, C.M.C. Effect of Glass Fiber Post Surface Treatment on Bond Strength of a Self-Adhesive Resin Cement: An “in Vitro” Study. Int. J. Dent. 2021, 2021, 8856657. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.R.; Kim, K.N.; Kim, K.M. The Disinfection of Impression Materials by Using Microwave Irradiation and Hydrogen Peroxide. J. Prosthet. Dent. 2014, 112, 981–987. [Google Scholar] [CrossRef]
- Li, X.; Xu, N.; Dong, M.; Zuo, E.; Ren, X.; Hu, S. Effect of Different Surface Treatments on Bond Strength of Glass Fiber Post to Root Dentin an in Vitro Study. J. Dalian Med. Univ. 2013, 35, 424–429. [Google Scholar] [CrossRef]
- Mishra, L.; Khan, A.S.; Velo, M.M.d.A.C.; Panda, S.; Zavattini, A.; Rizzante, F.A.P.; Arbildo Vega, H.I.; Sauro, S.; Lukomska-Szymanska, M. Effects of Surface Treatments of Glass Fiber-Reinforced Post on Bond Strength to Root Dentine: A Systematic Review. Materials 2020, 13, 1967. [Google Scholar] [CrossRef]
- Punia, S.K.; Kumar, Y.; Kushwaha, S.; Choudhary, D.; Agarwal, S. Impact of Antioxidants on Bond Strength between Resin Composites and Bleached Enamel: An In Vitro Comparative Evaluation. Dent. J. Adv. Stud. 2024, 12, 106–110. [Google Scholar] [CrossRef]
- Qamar, Z.; Abdul, N.S.; Ali, S.; AlSheikh, R.; Alqarawi, F.K.; Niazi, F.H. Assessment of Push-out Bond Strength of Post-Surface Pretreatment before Salinization Using Hydrogen Peroxide, Aluminum Trioxide, and Natural Photosensitizers to Radicular Dentin. Photodiagnosis Photodyn. Ther. 2022, 39, 102859. [Google Scholar] [CrossRef]
- Aljamhan, A.; Alkhudhairy, F. Impact of Hydrofluoric Acid, Ytterbium Fiber Lasers, and Hydroxyapatite Nanoparticles on Surface Roughness and Bonding Strength of Resin Cement with Different Viscosities to Lithium Disilicate Glass Ceramic: SEM and EDX Analysis. Crystals 2025, 15, 661. [Google Scholar] [CrossRef]
- Alkhudhairy, F.; Vohra, F.; Naseem, M. Influence of Er,Cr:YSGG Laser Dentin Conditioning on the Bond Strength of Bioactive and Conventional Bulk-Fill Dental Restorative Material. Photobiomodul. Photomed. Laser Surg. 2020, 38, 30–35. [Google Scholar] [CrossRef]
- Alrabiah, M.; Alsunbul, H.; Almutairi, B.; Aljanakh, M.; Alzahrani, K.M.; Abduljabbar, T. Er, Cr: YSGG, Nd: YVO4, and Ti: Sapphire Lasers for Surface Treatment of Hybrid Ceramics on Bond Durability, Surface Texture, and Debonding to Resin Cement: A Scanning Electron Microscopy (SEM) Analysis. J. Biomater. Tissue Eng. 2023, 13, 792–798. [Google Scholar] [CrossRef]
- Kimura, H.; Tsuka, H.; Morita, K.; Hirata, I.; Nishio, F.; Abekura, H.; Doi, K.; Tsuga, K. Nd:YVO4 Laser Groove Treatment Can Improve the Shear Bond Strength between Dental PEEK and Adhesive Resin Cement with an Adhesive System. Dent. Mater. J. 2022, 41, 382–391. [Google Scholar] [CrossRef]
- Vohra, F.; Bukhari, I.A.; Sheikh, S.A.; Naseem, M.; Hussain, M. Photodynamic Activation of Irrigation (Using Different Laser Prototypes) on Push out Bond Strength of Fiber Posts. Photodiagn. Photodyn. Ther. 2020, 30, 101716. [Google Scholar] [CrossRef]
- Maawadh, A.M.; Almohareb, T.; Al-Hamdan, R.S.; Al Deeb, M.; Naseem, M.; Alhenaki, A.M.; Vohra, F.; Abduljabbar, T. Repair Strength and Surface Topography of Lithium Disilicate and Hybrid Resin Ceramics with LLLT and Photodynamic Therapy in Comparison to Hydrofluoric Acid. J. Appl. Biomater. Funct. Mater. 2020, 18, 2280800020966938. [Google Scholar] [CrossRef] [PubMed]
- Alsunbul, H.; Almutairi, B.; Aljanakh, M.; Abduljabbar, T. Hybrid Ceramic Repair Strength, Surface Roughness, and Bond Failure, Using Methylene Blue-Activated Low-Level Laser Therapy, Carbon Dioxide, and Ti: Al2O3 Laser. Photodiagn. Photodyn. Ther. 2023, 43, 103693. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Gupta, B.; Motwani, B.K.; Binalrimal, S.; Radwan, W.; Robaian, A.; Zidane, B.; Al Wadei, M.H.D.; Veeraraghavan, V.P.; Bhandi, S.; et al. The Effect of Different Surface Conditioning Techniques on the Bonding between Resin Cement & Ceramic. Coatings 2022, 12, 399. [Google Scholar] [CrossRef]
- Dahiya, M.S.; Tomer, V.K.; Duhan, S. Bioactive Glass/Glass Ceramics for Dental Applications. In Applications of Nanocomposite Materials in Dentistry; Woodhead Publishing: Cambridge, UK, 2019; pp. 1–25. ISBN 9780128137420. [Google Scholar]
- Thavornyutikarn, B.; Feltis, B.; Wright, P.F.A.; Turney, T.W. Effect of Pre-Treatment of Crystallized Bioactive Glass with Cell Culture Media on Structure, Degradability, and Biocompatibility. Mater. Sci. Eng. C 2019, 97, 188–197. [Google Scholar] [CrossRef]
- Edelhoff, D.; Liebermann, A.; Beuer, F.; Stimmelmayr, M.; Güth, J.-F. Minimally Invasive Treatment Options in Fixed Prosthodontics. Quintessence Int. 2016, 47, 207–216. [Google Scholar] [CrossRef]
- Kırmalı, Ö.; Üstün, Ö.; Kapdan, A.; Kuştarcı, A. Evaluation of Various Pretreatments to Fiber Post on the Push-out Bond Strength of Root Canal Dentin. J. Endod. 2017, 43, 1180–1185. [Google Scholar] [CrossRef] [PubMed]
- Al-Kheraif, A.A.; Mohamed, B.A.; Sufyan, A.O.H.; Khan, A.A.; Divakar, D.D. Photodynamic Therapy and Other Pretreatment Methods on Epoxy-Based Glass Fiber Post on the Push-out Bond Strength to Radicular Dentin. Photodiagnosis Photodyn. Ther. 2021, 36, 102526. [Google Scholar] [CrossRef]
- Uzun, I.; Keskin, C.; Özsu, D.; Güler, B.; Aydemir, H. Push-out Bond Strength of Oval versus Circular Fiber Posts Irradiated by Erbium-Doped Yttrium Aluminum Garnet Laser. J. Prosthet. Dent. 2016, 116, 425–430. [Google Scholar] [CrossRef]
- Archana, C.H.; Raju, S.M.K.; Yadhav, S.S.; Konagala, R.K.; Manthena, S.R.K.; Teja, P.R. Effect of Surface Pretreatment and Thermal Activation of Silane Coupling Agent on Bond Strength of Fiber Posts to Resin Cement. J. Contemp. Dent. Pract. 2019, 20, 1293–1296. [Google Scholar] [CrossRef] [PubMed]
- Alkahtany, M.F. Extrusion Bond Strength of Glass Fiber Post to Radicular Dentin after Final Irrigation Using MTAD, EDTA, Pineapple Peel Extract, and Riboflavin. Photodiagn. Photodyn. Ther. 2022, 39, 102982. [Google Scholar] [CrossRef] [PubMed]
- Shabib, S. Use of Nd:YVO4 Laser, Photodynamic Therapy, Sulfuric Acid and Sand Blasting on Improving Bond Integrity of PEEK to Resin Cement with Adhesive. Photodiagn. Photodyn. Ther. 2022, 39, 102865. [Google Scholar] [CrossRef]
- Alkhudhairy, F.; Aljamhan, A.S. Surface Conditioning of PEEK Post Using Nd: YVO4 Laser, Photodynamic Therapy, and Sulfuric Acid on the Pushout Bond Strength to Canal Dentin. Photodiagn. Photodyn. Ther. 2023, 42, 103601. [Google Scholar] [CrossRef]
- Mistry, S.; Roy, R.; Kundu, B.; Datta, S.; Kumar, M.; Chanda, A.; Kundu, D. Clinical Outcome of Hydroxyapatite Coated, Bioactive Glass Coated, and Machined Ti6Al4V Threaded Dental Implant in Human Jaws: A Short-Term Comparative Study. Implant Dent. 2016, 25, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Alsunbul, H.; Alfawaz, Y.F.; Alhamdan, E.M.; Farooq, I.; Vohra, F.; Abduljabbar, T. Influence of Carbon and Graphene Oxide Nanoparticle on the Adhesive Properties of Dentin Bonding Polymer: A SEM, EDX, FTIR Study. J. Appl. Biomater. Funct. Mater. 2023, 21, 22808000231159238. [Google Scholar] [CrossRef]
- Mosharraf, R.; Haerian, A. Push-out Bond Strength of a Fiber Post System with Two Resin Cements. Dent. Res. J. 2011, 8, S88–S93. [Google Scholar]
- Saraiva, L.; Aguiar, T.; Costa, L.; Correr-Sobrinho, L.; Muniz, L.; Mathias, P. Effect of Different Adhesion Strategies on Fiber Post Cementation: Push-out Test and Scanning Electron Microscopy Analysis. Contemp. Clin. Dent. 2013, 4, 443–447. [Google Scholar] [CrossRef]
- Pyun, J.H.; Shin, T.B.; Lee, J.H.; Ahn, K.M.; Kim, T.H.; Cha, H.S. Effects of Hydrogen Peroxide Pretreatment and Heat Activation of Silane on the Shear Bond Strength of Fiber-Reinforced Composite Posts to Resin Cement. J. Adv. Prosthodont. 2016, 8, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Gençer, B.K.; Şenol, A.A.; Acar, E.; Atalı, P.Y.; Tarçın, B.; Özcan, M. Effect of Surface Conditioning Protocols on the Repair Bond Strength of Resin Composite to CAD/CAM Blocks: Bioactive-Glass, Silica-Coated Alumina, or Aluminum Oxide? Eur. J. Oral Sci. 2025, 133, e70016. [Google Scholar] [CrossRef] [PubMed]
- Al-Hamdan, R.S.; Almutairi, B.; Abduljabbar, T. Sandblasting, Bioactive Glass Particles, and Phthalocyanine Activated via Low-Level Laser Therapy on the Surface Roughness and Shear Bond Strength of Hybrid Ceramics Bonded to Different Cement Types. Photodiagn. Photodyn. Ther. 2025, 55, 104682. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhairy, F.; Shono, N.N. An Investigation of Y-TZP Surface Characteristics and Adhesive Properties Following Treatment with Tri-Biochemical Silica Coating, Femtosecond Laser, and Nano-Hydroxyapatite: A Scanning Electron Microscopy Evaluation. Pak. J. Med. Sci. 2025, 41, 758. [Google Scholar] [CrossRef]
- Mozayeni, M.A.; Vatandoost, F.; Asnaashari, M.; Shokri, M.; Azari-Marhabi, S.; Asnaashari, N. Comparing the Efficacy of Toluidine Blue, Methylene Blue and Curcumin in Photodynamic Therapy Against Enterococcus Faecalis. J. Lasers Med. Sci. 2020, 11, S49–S54. [Google Scholar] [CrossRef]


| Experimental Groups | Mean ± (SD) Ra (µm) | p-Value ! | |
|---|---|---|---|
| Group 1 | H2O2 | 1027.37 ± 0.066 a | p < 0.05 |
| Group 2 | Nd: YVO4 laser | 1051.54 ± 0.087 a | |
| Group 3 | LLLT-TB | 539.39 ± 0.091 c | |
| Group 4 | BAGP | 793.32 ± 0.058 b | |
| Experimental Groups | Mean ± SD Cervical | Mean ± SD Middle | Mean ± SD Apical | p-Value ! | |
|---|---|---|---|---|---|
| Group 1 | H2O2 | 8.75 ± 0.21 a,A | 8.43 ± 0.15 a,A | 7.13 ± 0.09 a,B | p < 0.05 |
| Group 2 | Nd: YVO4 laser | 8.89 ± 0.12 a,A | 8.57 ± 0.06 a,A | 7.01 ± 0.10 a,B | |
| Group 3 | TB-LLLT | 5.87 ± 0.54 c,A | 5.54 ± 0.43 c,A | 4.94 ± 0.12 c,B | |
| Group 4 | BAGPs | 6.79 ± 0.35 b,A | 6.39 ± 0.41 b,A | 5.94 ± 0.21 b,B | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlRefeai, M.H.; Alkhudhairy, F. Glass Fiber Post Pretreated with Neodymium-Doped Yttrium Orthovanadate, Toluidine Blue Activated Low-Level Laser Therapy, and Bioactive Glass: An In Vitro Analysis of SEM, Bond Strength, and Surface Roughness. Crystals 2025, 15, 813. https://doi.org/10.3390/cryst15090813
AlRefeai MH, Alkhudhairy F. Glass Fiber Post Pretreated with Neodymium-Doped Yttrium Orthovanadate, Toluidine Blue Activated Low-Level Laser Therapy, and Bioactive Glass: An In Vitro Analysis of SEM, Bond Strength, and Surface Roughness. Crystals. 2025; 15(9):813. https://doi.org/10.3390/cryst15090813
Chicago/Turabian StyleAlRefeai, Mohammad H., and Fahad Alkhudhairy. 2025. "Glass Fiber Post Pretreated with Neodymium-Doped Yttrium Orthovanadate, Toluidine Blue Activated Low-Level Laser Therapy, and Bioactive Glass: An In Vitro Analysis of SEM, Bond Strength, and Surface Roughness" Crystals 15, no. 9: 813. https://doi.org/10.3390/cryst15090813
APA StyleAlRefeai, M. H., & Alkhudhairy, F. (2025). Glass Fiber Post Pretreated with Neodymium-Doped Yttrium Orthovanadate, Toluidine Blue Activated Low-Level Laser Therapy, and Bioactive Glass: An In Vitro Analysis of SEM, Bond Strength, and Surface Roughness. Crystals, 15(9), 813. https://doi.org/10.3390/cryst15090813






