Simulation Models for Suicide Prevention: A Survey of the State-of-the-Art
Abstract
1. Introduction
- Which interventions are supported by previous models? Reviews of simulation models in public health occasionally show that groups of practitioners work in silos, possibly being unaware of existing tools [47]. As a result, several models may independently be developed to answer the same what-if scenarios, and none may be available for other scenarios of interest. Thus, a thorough inventory of the support offered by prior models can foster synergies across teams, provide a concrete toolbox for practitioners, and reveal areas in need of further efforts.
- How much confidence can we place in models? Although a simulation model is ultimately an instrument [51], its intended users need to know the extent to which it can be trusted in a given application setting. Perfect trust does not exist, as a simulation is necessarily a simplification of reality; hence, the emphasis here is on knowing the limitations of a model and addressing them where possible.
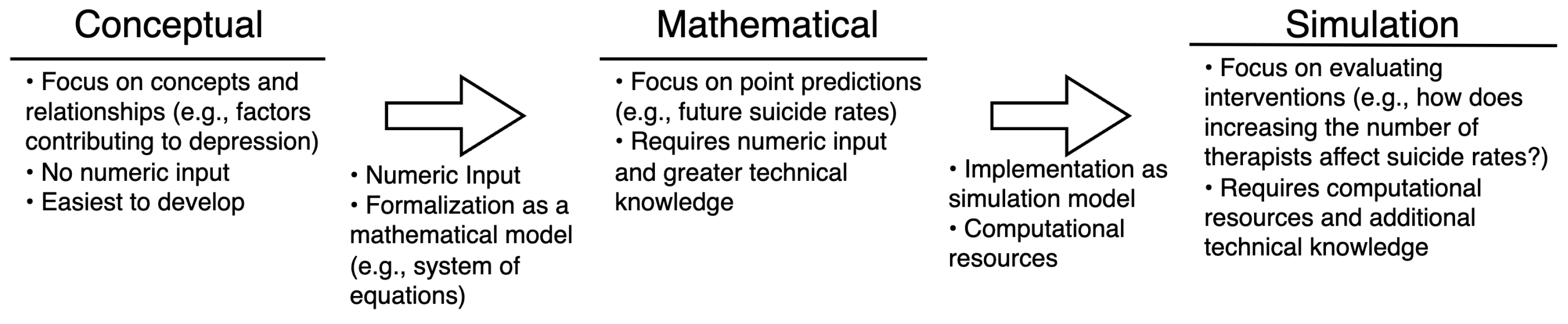
2. Background
2.1. Agent-Based Models
2.2. System Dynamics
2.3. Microsimulation, Network Simulation, and Discrete Event Simulation
3. RQ1: Which Interventions Are Supported by Previous Models?
4. RQ2: What Are the Obstacles Preventing Model Application?
5. RQ3: How Much Confidence Can We Place in the Models?
6. Discussion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| ABM | Agent-Based Models |
| DES | Discrete Event Simulation |
| M&S | Modeling and Simulation |
| MDD | Major Depressive Disorder |
| SD | System Dynamics |
References
- Centers for Disease Control and Prevention and National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). In Fatal Injury and Violence Data; Centers for Disease Control and Prevention and National Center for Injury Prevention and Control: Atlanta, GA, USA, 2023. [Google Scholar]
- World Health Organization. Suicide Worldwide in 2019: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Ilic, M.; Ilic, I. Worldwide suicide mortality trends (2000–2019): A joinpoint regression analysis. World J. Psychiatry 2022, 12, 1044. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Deaths in Australia; AIHW, Australian Government: Canberra, ACT, Australia, 2022.
- Aleman, A.; Denys, D. Mental health: A road map for suicide research and prevention. Nature 2014, 509, 421–423. [Google Scholar] [CrossRef] [PubMed]
- Bilsen, J. Suicide and youth: Risk factors. Front. Psychiatry 2018, 9, 540. [Google Scholar] [CrossRef] [PubMed]
- Gili, M.; Castellví, P.; Vives, M.; de la Torre-Luque, A.; Almenara, J.; Blasco, M.J.; Cebrià, A.I.; Gabilondo, A.; Pérez-Ara, M.A.; Miranda-Mendizabal, A.; et al. Mental disorders as risk factors for suicidal behavior in young people: A meta-analysis and systematic review of longitudinal studies. J. Affect. Disord. 2019, 245, 152–162. [Google Scholar] [CrossRef]
- Hawton, K.; i Comabella, C.C.; Haw, C.; Saunders, K. Risk factors for suicide in individuals with depression: A systematic review. J. Affect. Disord. 2013, 147, 17–28. [Google Scholar] [CrossRef]
- National Mental Health Commission (Australia). Monitoring Mental Health and Suicide Prevention Reform: National Report 2019; Commonwealth of Australia (National Mental Health Commission): Sydney, Australia, 2019.
- Petrosky, E.; Harpaz, R.; Fowler, K.A.; Bohm, M.K.; Helmick, C.G.; Yuan, K.; Betz, C.J. Chronic pain among suicide decedents, 2003 to 2014: Findings from the national violent death reporting system. Ann. Intern. Med. 2018, 169, 448–455. [Google Scholar] [CrossRef]
- Racine, M. Chronic pain and suicide risk: A comprehensive review. Prog.-Neuro-Psychopharmacol. Biol. Psychiatry 2018, 87, 269–280. [Google Scholar] [CrossRef]
- Baiden, P.; LaBrenz, C.A.; Onyeaka, H.K.; Muoghalu, C.; Nicholas, J.K.; Spoor, S.P.; Bock, E.; Taliaferro, L.A. Perceived racial discrimination and suicidal behaviors among racial and ethnic minority adolescents in the United States: Findings from the 2021 Adolescent Behaviors and Experiences Survey. Psychiatry Res. 2022, 317, 114877. [Google Scholar] [CrossRef]
- Pollock, N.J.; Naicker, K.; Loro, A.; Mulay, S.; Colman, I. Global incidence of suicide among Indigenous peoples: A systematic review. BMC Med. 2018, 16, 145. [Google Scholar] [CrossRef]
- Allen, J.; Levintova, M.; Mohatt, G. Suicide and alcohol-related disorders in the US Arctic: Boosting research to address a primary determinant of health disparities. Int. J. Circumpolar Health 2011, 70, 473–487. [Google Scholar] [CrossRef]
- Olfson, M.; Blanco, C.; Wall, M.; Liu, S.M.; Saha, T.D.; Pickering, R.P.; Grant, B.F. National trends in suicide attempts among adults in the United States. JAMA Psychiatry 2017, 74, 1095–1103. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N.; Segal, S.P. Adverse childhood experiences and suicide attempts among those with mental and substance use disorders. Child Abus. Negl. 2017, 69, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.P.; Kingree, J.; Lamis, D. Associations of adverse childhood experiences and suicidal behaviors in adulthood in a US nationally representative sample. Child Care Health Dev. 2019, 45, 121–128. [Google Scholar] [CrossRef]
- Calati, R.; Ferrari, C.; Brittner, M.; Oasi, O.; Olié, E.; Carvalho, A.F.; Courtet, P. Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. J. Affect. Disord. 2019, 245, 653–667. [Google Scholar] [CrossRef]
- Heuser, C.; Howe, J. The relation between social isolation and increasing suicide rates in the elderly. Qual. Ageing Older Adults 2019, 20, 2–9. [Google Scholar] [CrossRef]
- Gould, M.; Jamieson, P.; Romer, D. Media contagion and suicide among the young. Am. Behav. Sci. 2003, 46, 1269–1284. [Google Scholar] [CrossRef]
- Swedo, E.A.; Beauregard, J.L.; de Fijter, S.; Werhan, L.; Norris, K.; Montgomery, M.P.; Rose, E.B.; David-Ferdon, C.; Massetti, G.M.; Hillis, S.D.; et al. Associations between social media and suicidal behaviors during a youth suicide cluster in Ohio. J. Adolesc. Health 2021, 68, 308–316. [Google Scholar] [CrossRef]
- Walling, M.A. Suicide contagion. Curr. Trauma Rep. 2021, 7, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Allchin, A.; Chaplin, V.; Horwitz, J. Limiting access to lethal means: Applying the social ecological model for firearm suicide prevention. Inj. Prev. 2019, 25, i44–i48. [Google Scholar] [CrossRef]
- Milner, A.; Witt, K.; Maheen, H.; LaMontagne, A.D. Access to means of suicide, occupation and the risk of suicide: A national study over 12 years of coronial data. BMC Psychiatry 2017, 17, 125. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention and National Center for Injury Prevention and Control. The Social-Ecological Model: A Framework for Prevention; Division of Violence Prevention: Atlanta, GA, USA, 2023.
- Hox, J.J. Computational social science methodology, anyone? Methodology 2017, 13, 3–12. [Google Scholar] [CrossRef]
- Gilbert, N.; Ahrweiler, P.; Barbrook-Johnson, P.; Narasimhan, K.P.; Wilkinson, H. Computational modelling of public policy: Reflections on practice. J. Artif. Soc. Soc. Simul. 2018, 21, 14. [Google Scholar] [CrossRef]
- Jalali, M.S.; DiGennaro, C.; Guitar, A.; Lew, K.; Rahmandad, H. Evolution and reproducibility of simulation modeling in epidemiology and health policy over half a century. Epidemiol. Rev. 2021, 43, 166–175. [Google Scholar] [CrossRef]
- Luke, D.A.; Stamatakis, K.A. Systems Science Methods in Public Health: Dynamics, Networks, and Agents. Annu. Rev. Public Health 2012, 33, 357–376. [Google Scholar] [CrossRef] [PubMed]
- Giabbanelli, P.J.; Torsney-Weir, T.; Mago, V.K. A fuzzy cognitive map of the psychosocial determinants of obesity. Appl. Soft Comput. 2012, 12, 3711–3724. [Google Scholar] [CrossRef]
- Giabbanelli, P.J.; Alimadad, A.; Dabbaghian, V.; Finegood, D.T. Modeling the influence of social networks and environment on energy balance and obesity. J. Comput. Sci. 2012, 3, 17–27. [Google Scholar] [CrossRef]
- Fone, D.; Hollinghurst, S.; Temple, M.; Round, A.; Lester, N.; Weightman, A.; Roberts, K.; Coyle, E.; Bevan, G.; Palmer, S. Systematic review of the use and value of computer simulation modelling in population health and health care delivery. J. Public Health 2003, 25, 325–335. [Google Scholar] [CrossRef]
- Thompson, R.N.; Hollingsworth, T.D.; Isham, V.; Arribas-Bel, D.; Ashby, B.; Britton, T.; Challenor, P.; Chappell, L.H.K.; Clapham, H.; Cunniffe, N.J.; et al. Key questions for modelling COVID-19 exit strategies. Proc. R. Soc. B Biol. Sci. 2020, 287, 20201405. [Google Scholar] [CrossRef]
- Spelta, A.; Flori, A.; Pierri, F.; Bonaccorsi, G.; Pammolli, F. After the lockdown: Simulating mobility, public health and economic recovery scenarios. Sci. Rep. 2020, 10, 16950. [Google Scholar] [CrossRef]
- Li, J.; Giabbanelli, P. Returning to a normal life via COVID-19 vaccines in the United States: A large-scale agent-based simulation study. JMIR Med. Inform. 2021, 9, e27419. [Google Scholar] [CrossRef]
- Giabbanelli, P.J.; Galgoczy, M.C.; Nguyen, D.M.; Foy, R.; Rice, K.L.; Nataraj, N.; Brown, M.M.; Harper, C.R. Mapping the Complexity of Suicide by Combining Participatory Modeling and Network Science. In Proceedings of the 2021 IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining, ASONAM ’21, Virtual Event, 8–11 November 2021; Association for Computing Machinery: New York, NY, USA, 2022; pp. 339–342. [Google Scholar] [CrossRef]
- Giabbanelli, P.J.; Rice, K.L.; Nataraj, N.; Brown, M.M.; Harper, C.R. A systems science approach to identifying data gaps in national data sources on adolescent suicidal ideation and suicide attempt in the United States. BMC Public Health 2023, 23, 627. [Google Scholar] [CrossRef]
- Giabbanelli, P.J.; Rice, K.L.; Galgoczy, M.C.; Nataraj, N.; Brown, M.M.; Harper, C.R.; Nguyen, M.D.; Foy, R. Pathways to suicide or collections of vicious cycles? Understanding the complexity of suicide through causal mapping. Soc. Netw. Anal. Min. 2022, 12, 60. [Google Scholar] [CrossRef]
- Gijzen, M.W.; Rasing, S.P.; Creemers, D.H.; Smit, F.; Engels, R.C.; De Beurs, D. Suicide ideation as a symptom of adolescent depression. a network analysis. J. Affect. Disord. 2021, 278, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Oakey-Frost, N.; Cowan, T.; Moscardini, E.H.; Pardue-Bourgeois, S.; de Beurs, D.; Cohen, A.; Bryan, C.J.; Tucker, R.P. Examining the Interrelationships Among Suicide Cognitions, Suicidal Ideation, and Theoretically Derived Protective Factors. Arch. Suicide Res. 2022, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Pelton, M.; Crawford, H.; Bul, K.; Robertson, A.E.; de Beurs, D.; Rodgers, J.; Baron-Cohen, S.; Cassidy, S. The role of anxiety and depression in suicidal thoughts for autistic and non-autistic people: A theory-driven network analysis. Suicide Life Threat. Behav. 2022, 53, 426–442. [Google Scholar] [CrossRef] [PubMed]
- De la Poza, E.; Jódar Sánchez, L.A.; Douklia, G. Modeling the Spread of Suicide in Greece. Complex Syst. 2019, 28, 475–489. [Google Scholar] [CrossRef]
- Folly, W.S.D. The Threshold Bias Model: A Mathematical Model for the Nomothetic Approach of Suicide. PLoS ONE 2011, 6, e24414. [Google Scholar] [CrossRef]
- Skinner, A.; Occhipinti, J.A.; Song, Y.J.C.; Hickie, I.B. Regional suicide prevention planning: A dynamic simulation modelling analysis. BJPsych Open 2021, 7, e157. [Google Scholar] [CrossRef]
- Occhipinti, J.A.; Skinner, A.; Iorfino, F.; Lawson, K.; Sturgess, J.; Burgess, W.; Davenport, T.; Hudson, D.; Hickie, I. Reducing youth suicide: Systems modelling and simulation to guide targeted investments across the determinants. BMC Med. 2021, 19, 61. [Google Scholar] [CrossRef]
- Cerdá, M.; Hamilton, A.D.; Tracy, M.; Branas, C.; Fink, D.; Keyes, K.M. Would restricting firearm purchases due to alcohol-and drug-related misdemeanor offenses reduce firearm homicide and suicide? An agent-based simulation. Inj. Epidemiol. 2022, 9, 17. [Google Scholar] [CrossRef]
- Giabbanelli, P.J.; Tison, B.; Keith, J. The application of modeling and simulation to public health: Assessing the quality of agent-based models for obesity. Simul. Model. Pract. Theory 2021, 108, 102268. [Google Scholar] [CrossRef]
- Janssen, M.; Wimmer, M.A.; Deljoo, A. Policy Practice and Digital Science: Integrating Complex Systems, Social Simulation and Public Administration in Policy Research; Springer: Berlin/Heidelberg, Germany, 2015; Volume 10. [Google Scholar]
- Giabbanelli, P.J.; Vesuvala, C.X. Human Factors in Leveraging Systems Science to Shape Public Policy for Obesity: A Usability Study. Information 2023, 14, 196. [Google Scholar] [CrossRef]
- Ahrweiler, P.; Gilbert, N.; Pyka, A. Policy Modeling for Large Scale Social Systems; Routledge: London, UK, 2015; pp. 229–246. [Google Scholar]
- Alvarado, R. Computer simulations as scientific instruments. Found. Sci. 2022, 27, 1183–1205. [Google Scholar] [CrossRef]
- Badham, J. A Compendium of Modelling Techniques; The Australian National University: Canberra, ACT, Australia, 2010. [Google Scholar]
- Badham, J.; Chattoe-Brown, E.; Gilbert, N.; Chalabi, Z.; Kee, F.; Hunter, R.F. Developing agent-based models of complex health behaviour. Health Place 2018, 54, 170–177. [Google Scholar] [CrossRef]
- Nianogo, R.A.; Arah, O.A. Agent-based modeling of noncommunicable diseases: A systematic review. Am. J. Public Health 2015, 105, e20–e31. [Google Scholar] [CrossRef] [PubMed]
- Maglio, P.P.; Mabry, P.L. Agent-based models and systems science approaches to public health. Am. J. Prev. Med. 2011, 40, 392–394. [Google Scholar] [CrossRef]
- Voinov, A.; Jenni, K.; Gray, S.; Kolagani, N.; Glynn, P.D.; Bommel, P.; Prell, C.; Zellner, M.; Paolisso, M.; Jordan, R.; et al. Tools and methods in participatory modeling: Selecting the right tool for the job. Environ. Model. Softw. 2018, 109, 232–255. [Google Scholar] [CrossRef]
- Mesoudi, A. The cultural dynamics of copycat suicide. PLoS ONE 2009, 4, e7252. [Google Scholar] [CrossRef]
- Morabito, P.N.; Cook, A.V.; Homan, C.M.; Long, M.E. Agent-based models of copycat suicide. In Proceedings of the Social Computing, Behavioral-Cultural Modeling, and Prediction: 8th International Conference, SBP 2015, Washington, DC, USA, 31 March–3 April 2015; Proceedings 8. Springer: Berlin/Heidelberg, Germany, 2015; pp. 369–374. [Google Scholar]
- Keyes, K.M.; Hamilton, A.; Swanson, J.; Tracy, M.; Cerdá, M. Simulating the suicide prevention effects of firearms restrictions based on psychiatric hospitalization and treatment records: Social benefits and unintended adverse consequences. Am. J. Public Health 2019, 109, S236–S243. [Google Scholar] [CrossRef]
- Khademi, A.; Zhang, D.; Giabbanelli, P.J.; Timmons, S.; Luo, C.; Shi, L. An agent-based model of healthy eating with applications to hypertension. In Advanced Data Analytics in Health; Springer: Cham, Switzerland, 2018; pp. 43–58. [Google Scholar]
- Homer, J.B.; Hirsch, G.B. System Dynamics Modeling for Public Health: Background and Opportunities. Am. J. Public Health 2006, 96, 452–458. [Google Scholar] [CrossRef]
- Atkinson, J.A.; Wells, R.; Page, A.; Dominello, A.; Haines, M.; Wilson, A. Applications of system dynamics modelling to support health policy. Public Health Res. Pract. 2015, 25, e2531531. [Google Scholar] [CrossRef]
- Wittenborn, A.K.; Hosseinichimeh, N. Exploring personalized psychotherapy for depression: A system dynamics approach. PLoS ONE 2022, 17, e0276441. [Google Scholar] [CrossRef]
- Hosseinichimeh, N.; Wittenborn, A.K.; Rick, J.; Jalali, M.S.; Rahmandad, H. Modeling and estimating the feedback mechanisms among depression, rumination, and stressors in adolescents. PLoS ONE 2018, 13, e0204389. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, M.C. Socio-economic statistics and public policy: A new role for microsimulation modeling. In Statistics Canada Working Paper; Statistics Canada: Ottawa, ON, Canada, 1995; Available online: https://ideas.repec.org/p/stc/stcp3e/1995081e.html (accessed on 1 June 2023).
- Kim, D. Applications of Microsimulation Models to the Social Determinants of Health and Public Health. In New Horizons in Modeling and Simulation for Social Epidemiology and Public Health; Wiley: Hoboken, NJ, USA, 2021. [Google Scholar]
- Smith, D.M.; Heppenstall, A.; Campbell, M. Estimating Health over Space and Time: A Review of Spatial Microsimulation Applied to Public Health. J 2021, 4, 182–192. [Google Scholar] [CrossRef]
- Huddleston, J.; Galgoczy, M.C.; Ghumrawi, K.A.; Giabbanelli, P.J.; Rice, K.L.; Nataraj, N.; Brown, M.M.; Harper, C.R.; Florence, C.S. Design and Deployment of a Simulation Platform: Case Study of an Agent-Based Model for Youth Suicide Prevention. In Proceedings of the 2022 Winter Simulation Conference (WSC), Singapore, 11–14 December 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 2582–2593. [Google Scholar]
- Liu, J.; Li, L.; Russell, K. What becomes of the broken hearted? An agent-based approach to self-evaluation, interpersonal loss, and suicide ideation. In Proceedings of the 16th Conference on Autonomous Agents and MultiAgent Systems, São Paulo, Brazil, 8–12 May 2017; pp. 436–445. [Google Scholar]
- Silenzio, V.M.B.; Duberstein, P.R.; Tu, X.; Tang, W.; Lu, N.; Homan, C.M. Connecting the invisible dots: Network-based methods to reach a hidden population at risk for suicide. Soc. Sci. Med. 2009, 69, 469. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Castroman, J.; Moulahi, B.; Azé, J.; Bringay, S.; Deninotti, J.; Guillaume, S.; Baca-Garcia, E. Mining social networks to improve suicide prevention: A scoping review. J. Neurosci. Res. 2020, 98, 616–625. [Google Scholar] [CrossRef]
- Martínez, V.; Jiménez-Molina, Á.; Gerber, M.M. Social contagion, violence, and suicide among adolescents. Curr. Opin. Psychiatry 2023, 36, 237. [Google Scholar] [CrossRef]
- Le Lay, A.; Despiegel, N.; François, C.; Duru, G. Can discrete event simulation be of use in modelling major depression? Cost Eff. Resour. Alloc. 2006, 4, 1–11. [Google Scholar] [CrossRef]
- McKinley, K.W.; Rickard, K.N.; Latif, F.; Wavra, T.; Berg, J.; Morrison, S.; Chamberlain, J.M.; Patel, S.J. Impact of universal suicide risk screening in a pediatric emergency department: A discrete event simulation approach. Healthc. Inform. Res. 2022, 28, 25–34. [Google Scholar] [CrossRef]
- World Health Organization. Live Life: An Implementation Guide for Suicide Prevention in Countries; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Page, A.; Atkinson, J.A.; Heffernan, M.; McDonnell, G.; Hickie, I. A decision-support tool to inform Australian strategies for preventing suicide and suicidal behaviour. Public Health Res. Pract. 2017, 27, 2721717. [Google Scholar] [CrossRef]
- Atkinson, J.A.; Page, A.; Skinner, A.; Heffernan, M.; Prodan, A.; Hickie, I.B. The impact of reducing psychiatric beds on suicide rates. Front. Psychiatry 2019, 10, 448. [Google Scholar] [CrossRef] [PubMed]
- Occhipinti, J.A.; Rose, D.; Skinner, A.; Rock, D.; Song, Y.J.C.; Prodan, A.; Rosenberg, S.; Freebairn, L.; Vacher, C.; Hickie, I.B. Sound decision making in uncertain times: Can systems modelling be useful for informing policy and planning for suicide prevention? Int. J. Environ. Res. Public Health 2022, 19, 1468. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, J.A.; Skinner, A.; Hackney, S.; Mason, L.; Heffernan, M.; Currier, D.; King, K.; Pirkis, J. Systems modelling and simulation to inform strategic decision making for suicide prevention in rural New South Wales (Australia). Aust. N. Z. J. Psychiatry 2020, 54, 892–901. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Zafari, Z.; Slejko, J.F.; Castillo, W.C.; Reeves, G.M.; Dosreis, S. Impact of undertreatment of depression on suicide risk among children and adolescents with major depressive disorder: A microsimulation study. Am. J. Epidemiol. 2023, 192, 929–938. [Google Scholar] [CrossRef]
- Romeo, R.; Byford, S.; Knapp, M. Annotation: Economic evaluations of child and adolescent mental health interventions: A systematic review. J. Child Psychol. Psychiatry 2005, 46, 919–930. [Google Scholar] [CrossRef] [PubMed]
- Ahern, S.; Burke, L.A.; McElroy, B.; Corcoran, P.; McMahon, E.M.; Keeley, H.; Carli, V.; Wasserman, C.; Hoven, C.W.; Sarchiapone, M.; et al. A cost-effectiveness analysis of school-based suicide prevention programmes. Eur. Child Adolesc. Psychiatry 2018, 27, 1295–1304. [Google Scholar] [CrossRef]
- Hashemian, M.; Qian, W.; Stanley, K.G.; Osgood, N.D. Temporal aggregation impacts on epidemiological simulations employing microcontact data. BMC Med. Inform. Decis. Mak. 2012, 12, 132. [Google Scholar] [CrossRef]
- Giabbanelli, P.J.; Voinov, A.A.; Castellani, B.; Törnberg, P. Ideal, best, and emerging practices in creating artificial societies. In Proceedings of the 2019 Spring Simulation Conference (SpringSim), Tucson, AZ, USA, 29 April–2 May 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 1–12. [Google Scholar]
- Kaplan, M.S.; McFarland, B.; Huguet, N. Characteristics of adult male and female firearm suicide decedents: Findings from the National Violent Death Reporting System. Inj. Prev. 2009, 15, 322–327. [Google Scholar] [CrossRef]



| NYC ABM | Australia SD | Micro | DES | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | [59] | [46] | [76] | [77] | [45] | [78] | [44] | [79] | [80] | [74] |
| Five-year firearm ownership disqualification for anyone with a psychiatric hospitalization | ✓ | |||||||||
| Five-year firearm ownership disqualification for anyone receiving psychiatric treatment | ✓ | |||||||||
| Firearms removed for five years after one alcohol-related misdemeanor conviction | ✓ | |||||||||
| Firearms removed for five years after one alcohol-related arrest | ✓ | |||||||||
| Firearms removed for five years after one drug-related misdemeanor conviction | ✓ | |||||||||
| Firearms removed for five years after one drug-related arrest | ✓ | |||||||||
| Firearms removed for 10 years after one alcohol-related misdemeanor conviction | ✓ | |||||||||
| Firearms removed for 10 years after one alcohol-related arrest | ✓ | |||||||||
| Firearms removed for 10 years after one drug-related misdemeanor conviction | ✓ | |||||||||
| Firearms removed for 10 years after one drug-related arrest | ✓ | |||||||||
| Firearms removed for five years after two or more alcohol-related misdemeanor convictions in five years | ✓ | |||||||||
| Firearms removed for five years after two or more alcohol-related arrest in five years | ✓ | |||||||||
| Firearms removed for five years after two or more drug-related misdemeanor convictions in five years | ✓ | |||||||||
| Firearms removed for five years after two or more drug-related arrests in five years | ✓ | |||||||||
| General practitioner training | ✓ | ✓ | ✓ | ✓ | ||||||
| Coordinated aftercare in those who have attempted suicide | ✓ | |||||||||
| School-based mental health literacy programs | ✓ | |||||||||
| Brief-contact interventions in hospital settings | ✓ | |||||||||
| Psychosocial treatment approaches | ✓ | |||||||||
| 20% reduction in the lethality of means | ✓ | |||||||||
| Reducing psychiatric beds | ✓ | |||||||||
| Increasing the capacity of community-based services | ✓ | ✓ | ✓ | ✓ | ||||||
| Post-attempt assertive aftercare | ✓ | ✓ | ✓ | ✓ | ||||||
| Social connectedness programs | ✓ | ✓ | ✓ | ✓ | ||||||
| Community-based acute care services | ✓ | ✓ | ✓ | |||||||
| Technology-enabled crisis response | ✓ | |||||||||
| Technology-enabled coordinated care | ✓ | ✓ | ✓ | |||||||
| Post-discharge peer support | ✓ | |||||||||
| Reducing childhood adversity by 20% or 50% | ✓ | |||||||||
| Increasing youth employment by 20% or 50% | ✓ | |||||||||
| Reducing total unemployment by 20% or 50% | ✓ | |||||||||
| Reducing domestic violence by 20% or 50% | ✓ | |||||||||
| Reducing homelessness by 20% or 50% | ✓ | |||||||||
| Community-based education programs | ✓ | |||||||||
| Family psychoeducation and support | ✓ | ✓ | ||||||||
| Safety planning | ✓ | ✓ | ||||||||
| Safe space services | ✓ | ✓ | ||||||||
| General practitioner services capacity increase | ✓ | ✓ | ||||||||
| Psychiatrist and allied health services capacity increase | ✓ | ✓ | ||||||||
| Psychiatric hospital capacity increase | ✓ | ✓ | ||||||||
| Awareness campaigns | ✓ | |||||||||
| Suicide helpline services | ✓ | |||||||||
| Community management of severe disorders | ✓ | |||||||||
| Mental health education programs | ✓ | |||||||||
| Services re-engagement programs | ✓ | |||||||||
| Online services | ✓ | |||||||||
| Hospital staff training | ✓ | |||||||||
| Services capacity increase | ✓ | |||||||||
| 12 week antidepressant treatment | ✓ | |||||||||
| 36 week antidepressant treatment | ✓ | |||||||||
| 52 week antidepressant treatment | ✓ | |||||||||
| Emergency department suicide risk screening for patients at least 10 years old | ✓ | |||||||||
| Hospital suicide risk screening for patients at least 12 years old | ✓ | |||||||||
| Category | Interventions | % |
|---|---|---|
| Limit access to the means of suicide | n = 15 | 31.9% |
| Interact with the media for responsible reporting of suicide | n = 1 | 2.1% |
| Foster socio-emotional life skills in adolescents | n = 5 | 10.6% |
| Early identification, assessment, management and follow up of anyone who is affected by suicidal behaviours | n = 26 | 55.3% |
| Total | 47 | 100.0% |
| Model Group | Time Frame and Granularity | Sensitivity Analysis | Heterogeneity | Several Data Sources |
|---|---|---|---|---|
| NYC ABM | Y | Y | Y | Y |
| SD Australia | Y | Y | Y | Y |
| Micro | Y | Y | Y | Y |
| DES | Provided time frame but not granularity | Y | N/A | N/A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schuerkamp, R.; Liang, L.; Rice, K.L.; Giabbanelli, P.J. Simulation Models for Suicide Prevention: A Survey of the State-of-the-Art. Computers 2023, 12, 132. https://doi.org/10.3390/computers12070132
Schuerkamp R, Liang L, Rice KL, Giabbanelli PJ. Simulation Models for Suicide Prevention: A Survey of the State-of-the-Art. Computers. 2023; 12(7):132. https://doi.org/10.3390/computers12070132
Chicago/Turabian StyleSchuerkamp, Ryan, Luke Liang, Ketra L. Rice, and Philippe J. Giabbanelli. 2023. "Simulation Models for Suicide Prevention: A Survey of the State-of-the-Art" Computers 12, no. 7: 132. https://doi.org/10.3390/computers12070132
APA StyleSchuerkamp, R., Liang, L., Rice, K. L., & Giabbanelli, P. J. (2023). Simulation Models for Suicide Prevention: A Survey of the State-of-the-Art. Computers, 12(7), 132. https://doi.org/10.3390/computers12070132







