Sexual Function After Laser Therapy for Penile Cancer: A Systematic Review
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Outcome Measures
2.3. Search Strategy
2.4. Selection Process
2.5. Data Collection Process
2.6. Data Items
- Primary outcomes included erectile function, sexual satisfaction, libido, penetration, cosmetic outcome, function retention, oncological control, and patient satisfaction. When outcomes were not assessed with validated tools (e.g., the International Index of Erectile Function), they were extracted but considered low-certainty.
- Secondary variables included participant characteristics (age and stage of penile cancer), intervention details (type of laser, make, and mode), and study characteristics (year, design, sample size, and follow-up duration). Assumptions for missing data were clearly stated in the manuscripts.
2.7. Risk of Bias and Quality Assessment, Effect Measures, and Data Synthesis
3. Results
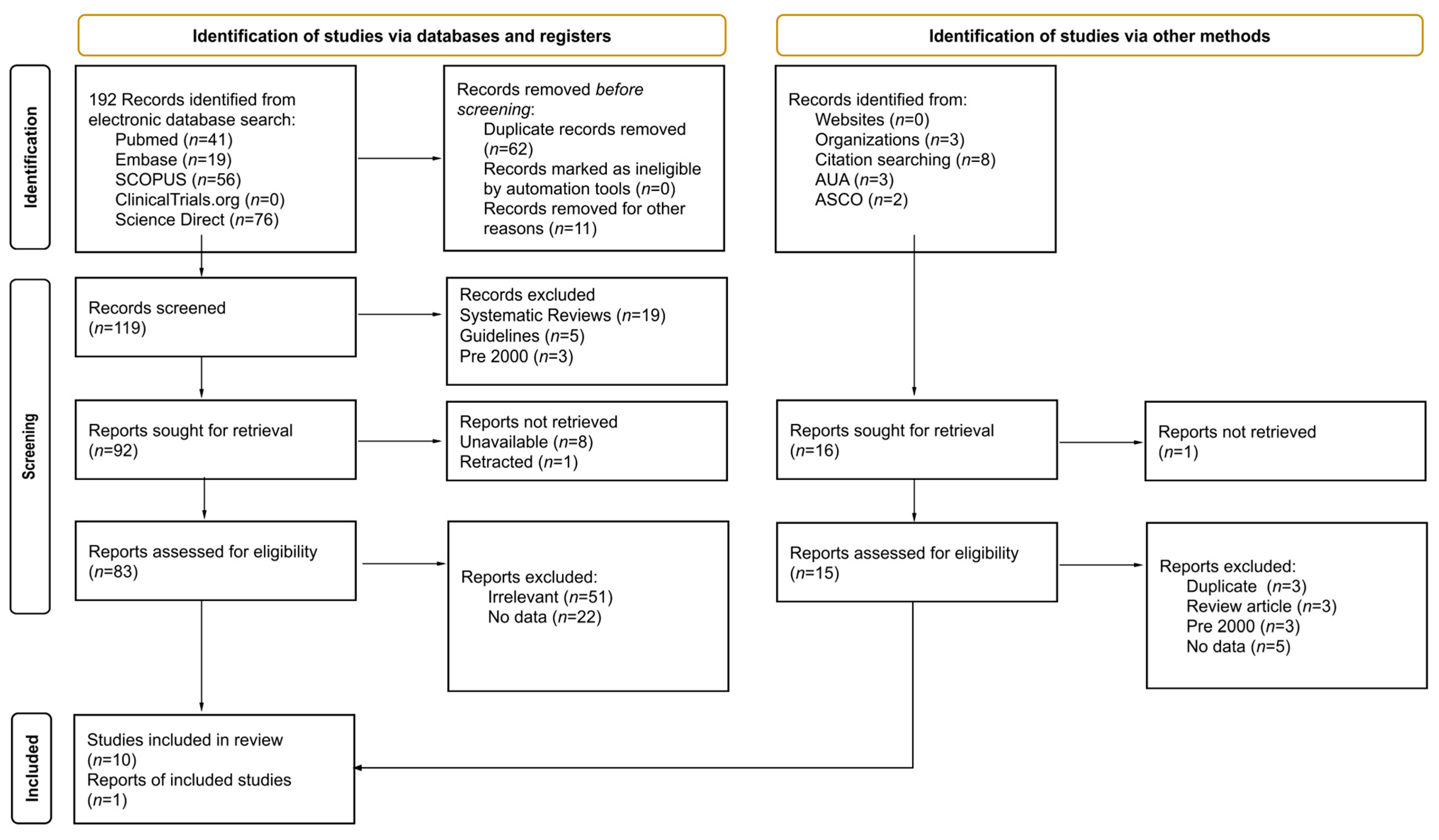
3.1. Study Selection
3.2. Study Characteristics
Risk of Bias in Studies
3.3. Results of Individual Studies
3.3.1. Heterogeneity
3.3.2. Erectile Function Outcomes by Laser Type
3.3.3. Sexual Function
3.3.4. Cosmetic Outcomes and Body Image Issues
3.3.5. Extent of Tissue Preservation
3.3.6. Clinical Outcomes
3.3.7. Postoperative Pain and Complications
3.4. Reporting Biases
3.4.1. CO2 Laser Therapy Studies
3.4.2. Nd:YAG Laser Therapy Studies
3.4.3. Tm:YAG Laser Therapy Study
3.4.4. Other Studies
3.5. Certainty of Evidence
4. Discussion
4.1. General Interpretation
4.2. Conclusions
5. Other Information
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Fu, L.; Tian, T.; Yao, K.; Chen, X.F.; Luo, G.; Gao, Y.; Lin, Y.F.; Wang, B.; Sun, Y.; Zheng, W.; et al. Global Pattern and Trends in Penile Cancer Incidence: Population-Based Study. JMIR Public Health Surveill. 2022, 8, e34874. [Google Scholar] [CrossRef]
- American Cancer Society About Penile Cancer. Available online: https://www.cancer.org/content/dam/CRC/PDF/Public/9756.00.pdf (accessed on 1 September 2025).
- Bleeker, M.C.G.; Heideman, D.A.M.; Snijders, P.J.F.; Horenblas, S.; Dillner, J.; Meijer, C.J.L.M. Penile Cancer: Epidemiology, Pathogenesis and Prevention. World J. Urol. 2009, 27, 141–150. [Google Scholar] [CrossRef]
- Horenblas, S. Penis Cancer Management: Insight into the Future. BJU Int. 2016, 117, 206–207. [Google Scholar] [CrossRef]
- Sri, D.; Sujenthiran, A.; Lam, W.; Minter, J.; Tinwell, B.E.; Corbishley, C.M.; Yap, T.; Sharma, D.M.; Ayres, B.E.; Watkin, N.W. A Study into the Association between Local Recurrence Rates and Surgical Resection Margins in Organ-Sparing Surgery for Penile Squamous Cell Cancer. BJU Int. 2018, 122, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Fallara, G.; Basile, G.; Poterek, A.; Tozzi, M.; Pang, K.; Cakir, O.; Bandini, M.; Ferro, M.; Musi, G.; Satchi, M.; et al. Oncological and Functional Outcomes of Penile Shaft Sparing Surgery for Localised Penile Cancer: A Systematic Review. Eur. Urol. Focus 2024, 11, 46–61. [Google Scholar] [CrossRef] [PubMed]
- Bandi, G.; Nakada, S.Y. Chapter 18—Complications of Lasers in Urologic Surgery. In Complications of Urologic Surgery, 4th ed.; Taneja, S.S., Ed.; W.B. Saunders: Philadelphia, PA, USA, 2010; pp. 199–209. ISBN 978-1-4160-4572-4. [Google Scholar]
- Cencic, B.; Lukac, M.; Marincek, M.; Vizintin, Z. High Fluence, High Beam Quality Q-Switched Nd:YAG Laser with Optoflex Delivery System for Treating Benign Pigmented Lesions and Tattoos. J. Laser Health Acad. 2010, 2010, 9–18. [Google Scholar]
- Giulioni, C.; Pirola, G.M.; Maggi, M.; Brocca, C.; Tramanzoli, P.; Stramucci, S.; Mantovan, M.; Perpepaj, L.; Cicconofri, A.; Gauhar, V.; et al. Current Evidence on Utility, Outcomes, and Limitations of Endoscopic Laser Ablation for Localized Upper Urinary Tract Urothelial Carcinoma: Results from a Scoping Review. Eur. Urol. Open Sci. 2024, 59, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Proietti, S.; Rodríguez-Socarrás, M.E.; Eisner, B.H.; Lucianò, R.; Basulto Martinez, M.J.; Yeow, Y.; Rapallo, I.; Saitta, G.; Scarfò, F.; Gaboardi, F.; et al. Thulium:Yag versus Holmium:Yag Laser Effect on Upper Urinary Tract Soft Tissue: Evidence from an Ex Vivo Experimental Study. J. Endourol. 2021, 35, 544–551. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Yin, G.; Fang, J.; Gu, S.; Ma, M.; Wang, W. Successful Application of Aminolevulinic Acid/Photodynamic Therapy in the Treatment of Giant Condyloma Acuminatum in an 87-Year-Old Patient. Photodiagnosis Photodyn. Ther. 2024, 45, 103980. [Google Scholar] [CrossRef]
- Sosnowski, R.; Kuligowski, M.; Kuczkiewicz, O.; Moskal, K.; Wolski, J.K.; Bjurlin, M.A.; Wysock, J.S.; Pęczkowski, P.; Protzel, C.; Demkow, T. Primary Penile Cancer Organ Sparing Treatment. Cent. Eur. J. Urol. 2016, 69, 377–383. [Google Scholar]
- Hakenberg, O.W.; Compérat, E.M.; Minhas, S.; Necchi, A.; Protzel, C.; Watkin, N. EAU Guidelines on Penile Cancer: 2014 Update. Eur. Urol. 2015, 67, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Bandieramonte, G.; Colecchia, M.; Mariani, L.; Lo Vullo, S.; Pizzocaro, G.; Piva, L.; Nicolai, N.; Salvioni, R.; Lezzi, V.; Stefanon, B.; et al. Peniscopically Controlled CO2 Laser Excision for Conservative Treatment of In Situ and T1 Penile Carcinoma: Report on 224 Patients. Eur. Urol. 2008, 54, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Conejo-Mir, J.; Muñoz, M.; Linares, M.; Rodríguez, L.; Serrano, A. Carbon Dioxide Laser Treatment of erythroplasia of Queyrat: A Revisited to This Condition. J. Eur. Acad. Dermatol. Venereol. 2005, 19, 642–643. [Google Scholar] [CrossRef]
- Schlenker, B.; Tilki, D.; Seitz, M.; Bader, M.J.; Reich, O.; Schneede, P.; Hungerhuber, E.; Stief, C.G.; Gratzke, C. Organ-Preserving Neodymium-Yttrium-Aluminium-Garnet Laser Therapy for Penile Carcinoma: A Long-Term Follow-Up. BJU Int. 2010, 106, 786–790. [Google Scholar] [CrossRef]
- Tewari, M.; Kumar, M.; Shukla, H.S. Nd:YAG Laser Treatment of Early Stage Carcinoma of the Penis Preserves Form and Function of Penis. Asian J. Surg. 2007, 30, 126–130. [Google Scholar] [CrossRef]
- Frimberger, D.; Hungerhuber, E.; Zaak, D.; Waidelich, R.; Hofstetter, A.; Schneede, P. Penile Carcinoma. Is Nd:YAG laser therapy radical enough? J. Urol. 2002, 168, 2418–2421. [Google Scholar] [CrossRef]
- Musi, G.; Russo, A.; Conti, A.; Mistretta, F.A.; Di Trapani, E.; Luzzago, S.; Bianchi, R.; Renne, G.; Ramoni, S.; Ferro, M.; et al. Thulium–Yttrium–Aluminium–Garnet (Tm:YAG) Laser Treatment of Penile Cancer: Oncological Results, Functional Outcomes, and Quality of Life. World J. Urol. 2018, 36, 265–270. [Google Scholar] [CrossRef]
- Skeppner, E.; Windahl, T.; Andersson, S.O.; Fugl-Meyer, K.S. Treatment-Seeking, Aspects of Sexual Activity and Life Satisfaction in Men with Laser-Treated Penile Carcinoma. Eur. Urol. 2008, 54, 631–639. [Google Scholar] [CrossRef]
- Skeppner, E.; Fugl-Meyer, K. Dyadic Aspects of Sexual Well-Being in Men with Laser-Treated Penile Carcinoma. Sex. Med. 2015, 3, 67–75. [Google Scholar] [CrossRef]
- Windahl, T.; Skeppner, E.; Andersson, S.O.; Fugl-Meyer, K.S. Sexual Function and Satisfaction in Men after Laser Treatment for Penile Carcinoma. J. Urol. 2004, 172, 648–651. [Google Scholar] [CrossRef] [PubMed]
- Kokorovic, A.; Duplisea, J.; Qiao, W.; McCormick, B.; Adibi, M.; Papadopoulos, J.; Ramirez, G.; Rao, P.; Tamboli, P.; Pettaway, C. Oncologic Outcomes and Subsequent Treatment Following Organ Sparing Surgery for Penile Carcinoma: The University of Texas M.D. Anderson Cancer Center Experience. Urol. Oncol. Semin. Orig. Investig. 2021, 39, 302.e19–302.e27. [Google Scholar] [CrossRef] [PubMed]
- Shaker, M.; Shaker, G. Saving More Than Just Skin: A Study of Penile Sparing Approaches in Cancer Treatment. Proc. Eur. Urol. Open Sci. 2023, 57 (Suppl. 1), S18. [Google Scholar] [CrossRef]
- Korzeniowski, M.A.; Crook, J.M. Contemporary Role of Radiotherapy in the Management of Penile Cancer. Transl. Androl. Urol. 2017, 6, 855–867. [Google Scholar] [CrossRef]
- Sansalone, S.; Silvani, M.; Leonardi, R.; Vespasiani, G.; Iacovelli, V. Sexual Outcomes after Partial Penectomy for Penile Cancer: Results from a Multi-Institutional Study. Asian J. Androl. 2017, 19, 57–61. [Google Scholar] [CrossRef]
- Audenet, F.; Sfakianos, J.P. Psychosocial Impact of Penile Carcinoma. Transl. Androl. Urol. 2017, 6, 874–878. [Google Scholar] [CrossRef]
- Pang, K.H.; Muneer, A.; Alnajjar, H.M. Glansectomy and Reconstruction for Penile Cancer: A Systematic Review. Eur. Urol. Focus 2022, 8, 1318–1322. [Google Scholar] [CrossRef]
- Martz, N.; Bodokh, Y.; Gautier, M.; Thamphya, B.; Schiappa, R.; Lam Cham Kee, D.; Chevallier, D.; Hannoun, A.; Chand, M.E.; Hannoun-Levi, J.M. High-Dose Rate Brachytherapy in Localized Penile Cancer: 5-Year Clinical Outcome Analysis. Clin. Transl. Radiat. Oncol. 2021, 27, 89–95. [Google Scholar] [CrossRef]
| Penile Cancer | (AND) Laser | AND Sexual Function | NOT | |
|---|---|---|---|---|
| PubMed | ((penile cancer) OR (penile carcinoma) OR (penile neoplasm) OR (penile squamous cell carcinoma) OR (penile SCC) OR (penile tumor) OR (penile malignancy) OR (penile lesion) OR (malignant penile neoplasm) OR (penile intraepithelial neoplasia) OR (PeIN) OR (penile squamous carcinoma) OR (carcinoma of the penis)) | ((laser therapy) OR (laser ablation) OR (CO2 laser) OR (Nd:YAG laser) OR (diode laser) OR (Holmium laser) OR (Thulium laser)) | ((sexual function) OR (erectile dysfunction) OR (sexual health) OR (sexual outcomes) OR (libido) OR (orgasm function) OR (penile sensitivity) OR (penetrative ability) OR (sexual quality of life) OR (SQoL) OR (quality of life) OR (sexual recovery) OR (post-treatment sexual function)) | ((prostate) OR (prostatic) OR (prostate cancer) OR (prostatic neoplasm) OR (prostate carcinoma) OR (BPH) OR (benign prostatic hyperplasia) OR (pearly)) |
| Embase | (‘penile cancer’ OR ‘penile carcinoma’ OR ‘penile neoplasm’ OR ‘penile squamous cell carcinoma’ OR ‘penile SCC’ OR ‘penile tumor’ OR ‘penile malignancy’ OR ‘penile lesion’ OR ‘malignant penile neoplasm’ OR ‘penile intraepithelial neoplasia’ OR ‘PeIN’ OR ‘penile squamous carcinoma’ OR ‘carcinoma of the penis’) | (‘laser therapy’ OR ‘laser ablation’ OR ‘CO2 laser’ OR ‘Nd:YAG laser’ OR ‘diode laser’ OR ‘Holmium laser’ OR ‘Thulium laser’) | (‘sexual function’ OR ‘erectile dysfunction’ OR ‘sexual health’ OR ‘sexual outcomes’ OR ‘libido’ OR ‘orgasmic function’ OR ‘penile sensitivity’ OR ‘penetrative ability’ OR ‘sexual quality of life’ OR ‘SQoL’ OR ‘quality of life’ OR ‘sexual recovery’ OR ‘post-treatment sexual function’) | (‘prostate’ OR ‘prostatic’ OR ‘prostate cancer’ OR ‘prostatic neoplasm’ OR ‘prostate carcinoma’ OR ‘BPH’ OR ‘benign prostatic hyperplasia’ OR ‘pearly’) |
| Scopus | (TITLE-ABS-KEY(“penile cancer” OR “penile carcinoma” OR “penile neoplasm” OR “penile squamous cell carcinoma” OR “penile SCC” OR “penile tumor” OR “penile malignancy” OR “penile lesion” OR “malignant penile neoplasm” OR “penile intraepithelial neoplasia” OR “PeIN” OR “penile squamous carcinoma” OR “carcinoma of the penis”)) | (TITLE-ABS-KEY(“laser therapy” OR “laser ablation” OR “CO2 laser” OR “Nd:YAG laser” OR “diode laser” OR “Holmium laser” OR “Thulium laser”)) | (TITLE-ABS-KEY(“sexual function” OR “erectile dysfunction” OR “sexual health” OR “sexual outcomes” OR “libido” OR “orgasmic function” OR “penile sensitivity” OR “penetrative ability” OR “sexual quality of life” OR “SQoL” OR “quality of life” OR “sexual recovery” OR “post-treatment sexual function”)) | (TITLE-ABS-KEY(“prostate” OR “prostatic” OR “prostate cancer” OR “prostatic neoplasm” OR “prostate carcinoma” OR “BPH” OR “benign prostatic hyperplasia” OR “pearly”)) |
| ScienceDirect | (“penile cancer” OR “penile carcinoma”) | (“laser” OR “laser Therapy”) | (“sexual function” OR “satisfaction” OR “quality of life”) | (“prostate” OR “penectomy”) |
| ClinicalTrial.gov, ASCO, EAU, AUA | Penile cancer | Laser | Sexual Function | N/A |
| Google Scholar | Penile cancer | Laser | Sexual Function | Prostate |
| Author | Study Design | Sample Size | Laser Type | Age (Mean/Median) | Cancer Stage | Main Findings |
|---|---|---|---|---|---|---|
| Bandieramonte (2008) [15] | Retrospective Study | 224 | CO2 | 57 (range 20–83) | Tis (47.3%), T1 (52.7%) | CO2 laser excision under peniscopic control provides excellent oncological and functional outcomes for early-stage penile carcinoma |
| Conejo-Mir (2005) [16] | Retrospective Study | 8 | CO2 | 64 (range: 44–70) | Tis (100%) | CO2 laser therapy is an effective, safe, and cosmetically favorable treatment for erythroplasia of Queyrat |
| Schlenker (2010) [17] | Retrospective Case Series | 54 | Nd:YAG | 57.6 (range: 25–89) | Tis (20.3%)), T1 (72.2%), T2 (7.4%) | Laser therapy offers organ preservation with functional benefits but carries a high recurrence rate |
| Tewari (2007) [18] | Retrospective Study | 32 | Nd:YAG | 47 (range 32–67) | T1 (78.1%), T2 (21.9%) | Nd:YAG laser treatment for early-stage penile cancer provides good oncological control while preserving function |
| Frimberger (2002) [19] | Retrospective Study | 29 | Nd:YAG | 55.1 (range: 30–93) | Tis (58.6%), T1 (34.5%), T2 (6.8%) | Nd:YAG laser therapy is an effective alternative to amputation for early-stage penile carcinoma. Excellent cosmetic and functional results |
| Musi (2018) [20] | Retrospective Study | 26 | Tm:YAG | 61 (range: 54–72) | Tis (42.3%), T1 (30.7%), T2 (11.0%), T3 (0.7%) | Tm:YAG laser therapy preserves penile structure and function while providing effective oncological control. Good functional outcome, with a minor impact on patient’s quality of life |
| Skeppner (2008) [21] | Retrospective Interview Study | 46 | Combined CO2, Nd:YAG | 63.5 (range: 34–90) | Tis (28.3%), T1 (30.4%), T2 (41.3%) | Laser treatment preserves function and quality of life; patients maintain sexual activity and life satisfaction |
| Skeppner (2015) [22] | Prospective Observational Study | 29 | Combined CO2, Nd:YAG | 60 (range: 37–73) | T1 (41.4%), T2 (48.3%) | Life satisfaction matched the general population, but health and sexual satisfaction declined |
| Windahl (2004) [23] | Retrospective Study | 67 | Combined CO2, Nd:YAG | 64 (range: 34–90) | Tis (31.3%), T1 (37.3%), T2 (31.3%), | Laser therapy provides high rates of functional and aesthetic satisfaction while preserving sexual function |
| Kokorovic (2021) [24] | Retrospective Cohort Study | 58 | KTP/CO2 or OSS + KTP | 61.5 (range: 53.1–70.2) | Tis (25.8%), T1a (60.3%), T2 (13.8%) | Laser treatment allows organ preservation but can lead to reduced sexual function and satisfaction |
| Shaker (2023) [25] | Retrospective Review | 20 | Combined CO2, Nd:YAG | N/A | T1, T2 | Laser ablation offers strong local control with better quality of life compared to more invasive procedures |
| Study | Representativeness of Exposed Cohort | Selection of Non -Exposed Cohort | Ascertainment of Exposure | Outcome not Present at Start | Comparability (Design/Analysis) | Assessment of Outcome | Follow-Up Long Enough | Adequacy of Follow-Up | Total Stars | Risk of Bias | Comments |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bandieramonte 2008 [15] | + | − | + | + | − | + | + | + | 7 | Low-Moderate | Large consecutive series of early-stage penile cancer; clear CO2 laser protocol, long follow-up, minimal attrition; lacks comparator or confounder adjustment. |
| Conejo-Mir 2005 [16] | + | − | + | + | − | + | − | + | 6 | Moderate | Small retrospective case series of 8 EQ patients; standardized CO2 laser protocol; complete follow-up reporting but no comparator and unclear follow-up duration for all cases. |
| Schlenker 2010 [17] | + | − | + | + | − | + | + | + | 6 | Moderate | Retrospective single-center series; no comparator group and no confounder adjustment but strong long-term follow-up and outcome assessment. |
| Tewari 2007 [18] | + | − | + | + | − | + | + | + | 6 | Moderate | Retrospective single-center cohort; no comparator group or confounder adjustment but adequate follow-up and standardized exposure. |
| Frimberger 2002 [19] | + | − | + | + | − | + | + | + | 6 | Moderate | Retrospective single-center cohort; no comparator group or confounder adjustment but standardized laser protocol and long-term follow-up. |
| Musi 2018 [20] | + | − | + | + | − | + | − | + | 6 | Moderate | Retrospective consecutive case series; standardized Tm:YAG protocol; complete follow-up but relatively short median follow-up (24 months) and no comparator group or confounder adjustment. |
| Skeppner 2008 [21] | + | − | + | + | − | + | + | + | 7 | Low-Moderate | Consecutive localized penile cancer cases treated with laser; clear exposure documentation, adequate follow-up, minimal attrition; no comparator or confounder adjustment. |
| Skeppner 2015 [22] | + | + | + | + | ++ | + | + | + | 9 | Low | Prospective cohort with partner comparator group; controlled for major confounders; complete follow-up; low risk of bias. |
| Windahl 2004 [23] | + | − | + | + | − | + | + | + | 7 | Low-Moderate | Consecutive localized penile cancer cases treated with combined CO2 and Nd:YAG laser therapy; validated outcome measures; adequate follow-up; no comparator or confounder adjustment. |
| Kokorovic 2021 [24] | + | − | + | + | − | + | + | + | 7 | Low-Moderate | Large single-center OSS series with standardized protocols and histological confirmation; long-term follow-up subset; lacks comparator and multivariable confounder adjustment. |
| Shaker 2023 [25] | + | + | + | + | − | + | + | + | 8 | Low | Retrospective comparative cohort with three penile-sparing approaches; strong follow-up and complete data capture; no confounder adjustment. |
| Author (Year) | Outcome Tool(s) | Instrument Type | Domains Evaluated |
|---|---|---|---|
| Bandieramonte et al. (2008) [15] | Clinical and peniscopic evaluation; patient interviews | Non-validated/Qualitative | Erectile function, sexual activity, cosmetic satisfaction |
| Conejo-Mir et al. (2005) [16] | Clinical observation; patient interview | Non-validated/Qualitative | Sexual and urinary function, cosmetic outcome |
| Schlenker et al. (2010) [17] | Structured follow-up interview | Non-validated/Qualitative | Erectile function, sexual activity, glans sensitivity |
| Tewari et al. (2007 [18] | Postoperative patient questionnaire | Non-validated/Qualitative | Erectile function, penetration ability, urinary and cosmetic outcomes |
| Frimberger et al. (2002) [19] | Physician-conducted interviews | Non-validated/Qualitative | Sexual activity, erectile function, satisfaction |
| Musi et al. (2018) [20] | Author-developed questionnaire | Non-validated/Semi-quantitative | Erectile function, satisfaction, penile length, sensitivity, cosmetic perception |
| Skeppner et al. (2008) [21] | Structured interview including LiSat-11 | Partially validated/Mixed | Sexual activity, satisfaction, life satisfaction |
| Skeppner et al. (2015) [22] | IIEF-5, LiSat-11, HADS | Validated/Quantitative | Erectile and sexual function, psychological well-being |
| Windahl et al. (2004) [23] | 53-item structured interview including IIEF-5 and LiSat-11 items | Partially validated/Mixed | Erectile function, sexual satisfaction, ejaculation, dyspareunia, cosmetic perception |
| Kokorovic et al. (2021) [24] | Institutional questionnaire | Non-validated/Quantitative | Penile preservation, recurrence, functional status |
| Shaker et al. (2023) [25] | Patient interview | Non-validated/Qualitative | Erectile function, sexual activity |
| Study | Schlenker Study (2010) [17] | Tewari Study (2007) [18] | Frimberger Study (2002) [19] | Conejo-Mir Study (2005) [16] | Skeppner Study (2015) [22] | Skeppner Study (2008) [21] | Bandieramonte Study (2008) [15] | Musi Study (2018) [20] | Shaker Study (2023) [25] | Windahl Study (2004) [23] | Kokorovic Study (2021) [24] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size | 54 | 32 | 29 | 8 | 29 | 46 | 224 | 26 | 20 | 67 | 58 |
| Laser Type | Nd:YAG | Nd:YAG | Nd:YAG | CO2 | Combined CO2, Nd:YAG | Combined CO2, Nd:YAG | CO2 | Tm:YAG | Combined CO2, Nd:YAG | Combined CO2, Nd:YAG | KTP/CO2 or OSS + KTP |
| Treatment Protocol | (30–50 W power, 100 s, 3 mm margin), acetic-acid mapping, circumcision in all cases. | laser coagulation of tumor bed, circumcision in all cases | coagulation with 3 mm safety margin; acetic acid mapping before treatment. | Super-pulsed mode, 5–8 watts; 8–10 mm margin | N/A | N/A | Peniscopically controlled, with adjunctive vaporization of lesion margins | RevoLix 200 W continuous-wave laser, 360 μm fiber, 15–20 W power; safety margin of 3 mm vaporized | N/A | N/A | Laser monotherapy or combination used with acetic acid mapping |
| Functional Outcome | N/A | 100% could urinate in standing posture | N/A | 100% preserved urinary function. | 47.6% dyspareunia before treatment, reduced to 12% at follow-up | N/A | Reported “excellent” | N/A | N/A | N/A | N/A |
| Scarring and Discoloration | Minimal | Minimal | Minimal | No hyperplastic scars | N/A | Minimal | Minimal | Minimal | N/A | No hyperplastic scars or gross deformities. | Minimal |
| Satisfaction with Cosmetic Outcome | 80% | 100% | 100% | “High” satisfaction with cosmetic results “excellent cosmetic outcome” (physicians’ opinion) | N/A | Reported “High” | Reported “Excellent”; | N/A | N/A | 78% satisfied/very satisfied; 100% retained a normal-appearing glans and meatus. | N/A |
| Tissue Preservation | N/A | 100% | 100% | 100% | Penile preservation achieved in “most” cases | 100% | 96.0%; 4.0% required amputation. | 100% | 100% | 100% | 100% |
| Body Image Issues | “Superior” psychological outcomes compared to penectomy | 100% satisfied | “Superior” psychological outcomes compared to penectomy | N/A | Comparable to general population | N/A | N/A | N/A | N/A | N/A | |
| Penile Length Changes | “Superior” than in penectomy. | N/A | N/A | N/A | N/A | N/A | preserved penile form and curvature | 78.2% no change | N/A | N/A | N/A |
| Outcomes Related to Sexual Satisfaction | |||||||||||
| Sexual Satisfaction | 59.3% of sexually active patients before surgery remained active post-treatment; “Superior” compared to amputation | 75% reporting normal sexual satisfaction. | “Excellent” orgasmic function; 66.7% patients reported regular sexual activity | “High” | 61% satisfied with sexual life before treatment, 32% after treatment (p = 0.039). 19% of patients stopped penetrative sex, but engaged in other forms of sexual activity Patient’s sexual partner satisfaction: low sexual desire before and after (8/29 then 9/29), decreased female lubrication (5/29 to 2/29), and partner sexual satisfaction remained the same. | 65% of sexually active men before treatment resumed sexual activity Decreased manual stimulation/caressing and fellatio; 13.0% were sexually inactive; 21.7% did not resume sexual activities; 50.0% resumed intercourse; 95.7% did not change masturbation habits | “Satisfactory” | 82.6% resumed intercourse; 13% did not continue intercourse 56.5% reported an impact; 43.5% reported no change | “Higher” in laser ablation and circumcision groups compared to glans excision | 50% satisfied/very satisfied; 72% considered their sexual life to be as good as they wanted | N/A |
| Libido Changes | N/A | N/A | 33% had no desire | N/A | Decreased libido in 45% before treatment, 34% after treatment | N/A | N/A | N/A | N/A | Unchanged in 80%, decreased in 17%, increased in 2.2%. | N/A |
| Time to Sexual Activity Resumption | N/A | N/A | N/A | N/A | Within one year 53% resumed intercourse; 19% resumed non penetrative sex. | 6% within weeks; 59% within months. | N/A | 60% had sexual intercourse within a month. 52.2% resumed erections within a week; 15.4% resumed erections after a month | N/A | 75% had resumed sexual activity within the median 3-year follow-up | N/A |
| Erectile Function | 59.3% | 71.9% reported normal erectile function | 33% reported erectile dysfunction | No erectile dysfunction reported. | IIEF-5 score ≥22 in 48.3% before, after: 34.5% at 1-year follow-up. | Reduced | No erectile dysfunction reported. | Unaltered post-treatment | N/A | 72% unaltered; 22% decreased; 6% improved. | N/A |
| Penile Sensation | Self-reported sensitivity not or only slightly impaired | N/A | N/A | N/A | 51.7% of patients reported decreased | N/A | Preserved in 100% | 26.1% maintained; 56.5% improved; 17.4% worsened | N/A | N/A | N/A |
| Outcomes Related to Life Satisfaction | |||||||||||
| Mental Health | Some patients experienced psychological distress due to recurrence | N/A | No suicidal thoughts reported | N/A | Factors of life satisfaction either improved slightly or remained unchanged. Anxiety in 17% of partners before treatment, 0% at follow-up | 50.0% of patients satisfied with whole life, comparable to the general population | N/A | N/A | N/A | N/A | N/A |
| Psychological Counseling Received | N/A | N/A | None of the patients required | N/A | 24.1% of patients and 17.2 partners discussed sexual issues | None. “Patients were somewhat less satisfied with their psychological health” | N/A | N/A | N/A | N/A | N/A |
| Post-Treatment Complications and Adverse Effects | |||||||||||
| Post-Treatment Pain or Complication | N/A | No reported need for parenteral analgesics | No major complication. | Minimal; No major complications. Full re-epithelialization within 14–28 days | N/A | No major complications. | Minimal; pain resolved within 3 days post-op. No infections reported, minor local edema | Mild discomfort in external meatus cases. Minimal; mild edema of the prepuce and | No major complications or adverse effects reported | Dyspareunia reported in 10.4%. | N/A |
| Short vs. Long-Term Recovery | Fast recovery but required long-term follow-up due to late recurrences | Fast healing with epithelialization completed in 7–9 weeks | N/A | Full healing within 14–28 days | N/A | N/A | Healing completed in 6 weeks; no need for additional treatment in most cases | Healing by secondary intention in 5 weeks; no major complications | N/A | Full healing typically within 3 months | N/A |
| Adverse Effects and Complications | N/A | N/A | No major adverse effects reported. | Recurrence reported in the meatal area | Dyspareunia (11.8%) | No major adverse effects reported. | No major adverse effects reported. | Mild pain while urinating for a week | No major adverse effects reported. | N/A | N/A |
| Additional Treatments | Radical circumcision for additional safety and hygiene | None specified | Groin dissection in 10 of 12 patients (83%) with invasive tumors | None specified | None specified | Lymph node dissection in 16/46 patients (34.8%). Chemotherapy in 1/46 patients (2.2%). Radiotherapy in 1/46 patients (2.2%) | Reductive chemotherapy in select cases (exophytic tumors) | None specified | None specified | 17/46 (37.0%) bilateral inguinal lymph node dissection; 1/46 (2.2%) received adjuvant chemotherapy | Inguinal lymphadenectomy in high-risk cases |
| Outcomes Related to Oncological Control | |||||||||||
| Recurrence Rate | 16/39 patients (42%); mean: 53 months | 2/32 patients; 6.25%, occurring at 48–60 months | T1: 1 patient; CIS: 1 patient (2/29 patients; 6.9%) | 12.5% (1/8 patients); at 1 year | N/A | 8/46 patients (17.4%) | 39/224 patients; (17.5%) at 10 years | 17.4% (4/23 patients), including 13.0% invasive recurrence | recurrence: 4/20 patients (20.0%). | 13/67 patients (19.4%); (10 successfully re-treated with laser | KTP/CO2—2/8 patients; 25.0% OSS + KTP—10/50 patients (20.0%) |
| Follow-Up Duration mean/median | 87 months (range: 9–366) | 70 months (range: 6–120) | 46.7 months (range: 6–180) | 120 months | 12 months | 54 months (range: 6–180) | 66 months (range: 35–132) | 24 months (range: 15–30) | 57 months | 36 months (range: 6–15) | 28 months (range: 0.2–188) |
| Laser Therapy | Sexual Function Reporting Bias | Recurrence Reporting Bias | Other Bias Concerns | Overall Risk of Reporting Bias |
|---|---|---|---|---|
| CO2 Laser | No quantitative sexual function data | Inconsistent recurrence tracking | Short follow-up in some studies | Moderate to High |
| Nd:YAG Laser | No standardized assessments | Large variation in recurrence rates | High variability in follow-ups | High |
| Tm:YAG Laser | Only one study, qualitative function data | Short follow-up, underestimation likely | No control group | Very High |
| Miscellaneous | Sexual function data inconsistently reported | Wide variation in follow-up (12 months–15 years) | Subjective interviews | Moderate to High |
| Outcome | Certainty of Evidence | Justification |
|---|---|---|
| Erectile function preservation | Low | No standardized assessments, inconsistent self-reported data |
| Libido changes | Very Low | Only qualitatively reported in select studies, no objective measures |
| Orgasmic function | Very Low | No direct measurement in any study |
| Penile preservation success | Moderate | Consistently reported across studies (96–100%) |
| Time to resumption of sexual activity | Very Low | Reported inconsistently, no standardized measurement |
| Short-term recurrence (<2 years) | Moderate to Low | Reasonably well reported but varies across studies |
| Long-term recurrence (>5 years) | Low | Follow-up durations are inconsistent; late recurrences may be underreported |
| Overall recurrence-free survival | Low | Large variation in recurrence estimates across laser therapies |
| 5-year overall survival | Moderate | Reported in some but limited data |
| 5-year disease-free survival | Low | Inconsistently reported across studies |
| 10-year survival | Very Low | No study systematically tracked survival beyond 5 years |
| Overall patient satisfaction | Low | Reported qualitatively but inconsistently |
| Quality of life post-treatment | Very Low | Lack of structured QoL assessments |
| Partner satisfaction | Very Low | No data available in most studies |
| Sexual function | Low | No standardized assessments, qualitative data mostly |
| Recurrence rates | Low | High variability, inconsistent follow-up durations |
| Oncologic control | Low to Moderate | Few survival data points, no long-term tracking |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ariamanesh, P.; Czajkowski, M.; Matuszewski, M. Sexual Function After Laser Therapy for Penile Cancer: A Systematic Review. Cancers 2025, 17, 3737. https://doi.org/10.3390/cancers17233737
Ariamanesh P, Czajkowski M, Matuszewski M. Sexual Function After Laser Therapy for Penile Cancer: A Systematic Review. Cancers. 2025; 17(23):3737. https://doi.org/10.3390/cancers17233737
Chicago/Turabian StyleAriamanesh, Pouya, Mateusz Czajkowski, and Marcin Matuszewski. 2025. "Sexual Function After Laser Therapy for Penile Cancer: A Systematic Review" Cancers 17, no. 23: 3737. https://doi.org/10.3390/cancers17233737
APA StyleAriamanesh, P., Czajkowski, M., & Matuszewski, M. (2025). Sexual Function After Laser Therapy for Penile Cancer: A Systematic Review. Cancers, 17(23), 3737. https://doi.org/10.3390/cancers17233737







