Role of Radiomics in Parotid Malignant Disease: A Scoping Review
Simple Summary
Abstract
1. Introduction
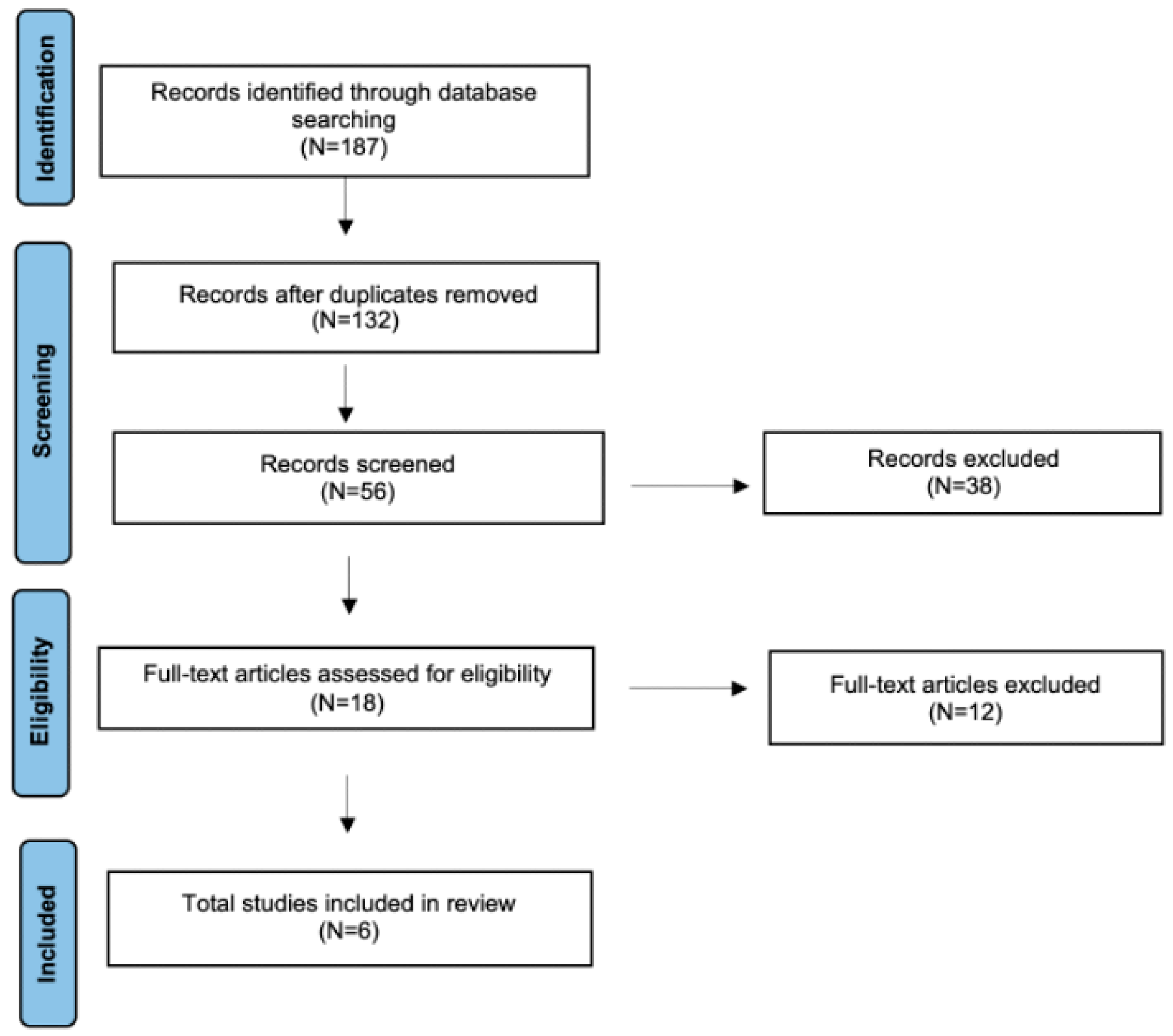
2. Materials and Methods
3. Results
3.1. MRI and Radiomics
3.2. CT-PET/CT and Radiomics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jegadeesh, N.; Liu, Y.; Prabhu, R.S.; Magliocca, K.R.; Marcus, D.M.; Higgins, K.A.; Vainshtein, J.M.; Wadsworth, J.T.; Beitler, J.J. Outcomes and Prognostic Factors in Modern Era Management of Major Salivary Gland Cancer. Oral. Oncol. 2015, 51, 770–777. [Google Scholar] [CrossRef]
- Elhusseiny, K.M.; Abd-Elhay, F.A.; Kamel, M.G.; Abd El Hamid Hassan, H.H.; El Tanany, H.H.M.; Hieu, T.H.; Tieu, T.M.; Low, S.K.; Hou, V.; Dibas, M.; et al. Examined and Positive Lymph Nodes Counts and Lymph Nodes Ratio Are Associated with Survival in Major Salivary Gland Cancer. Head. Neck 2019, 41, 2625–2635. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, R. Malignant salivary gland tumors: A short review. Oral. Maxillofac. Res. 2021, 7, 1–5. [Google Scholar] [CrossRef]
- El-Naggar, A.K.; Chan, J.K.C.; Grandis, J.R.; Takata, T.S.P. WHO Classification of Head and Neck Tumours, 4th ed.; IARC Publication: Lyon, France, 2017; pp. 159–202. [Google Scholar]
- Peravali, R.K.; Bhat, H.H.; Upadya, V.H.; Agarwal, A.; Naag, S. Salivary Gland Tumors: A Diagnostic Dilemma! J. Maxillofac. Oral. Surg. 2015, 14 (Suppl. S1), 438–442. [Google Scholar] [CrossRef] [PubMed]
- Ronchi, A.; Montella, M.; Zito Marino, F.; Panarese, I.; Pagliuca, F.; Colella, G.; Franco, R.; Cozzolino, I. Diagnostic Accuracy of FNA Cytology for Diagnosis of Salivary Gland Tumors in Pediatric Patients. Cancer Cytopathol. 2019, 127, 529–538. [Google Scholar] [CrossRef]
- Dell’Aversana Orabona, G.; Salzano, G.; Abbate, V.; Bonavolontà, P.; Committeri, U.; Seidita, F.; Petrocelli, M.; Somma, T.; Improta, G.; Vaira, L.A.; et al. Malignant Tumours of the Parotid Gland: Management of the Neck (Including the Clinically Negative Neck) and a Literature Review. Br. J. Oral. Maxillofac. Surg. 2021, 59, 665–671. [Google Scholar] [CrossRef]
- Bianchini, C.; Brugali, M.; Migliorelli, A.; Corazzi, V.; Cammaroto, G.; Meccariello, G.; Stomeo, F.; Ciorba, A.; Pelucchi, S. Basal cell adenoma and pleomorphic adenoma of the parotid gland: A single center experience. Minerva Surg. 2023, 78, 626–632. [Google Scholar] [CrossRef]
- Rossi, E.D.; Faquin, W.C. The Milan system for reporting salivary gland cytopathology (MSRSGC): An international effort toward improved patient care—When the roots might be inspired by Leonardo da Vinci. Cancer Cytopathol. 2018, 126, 756–766. [Google Scholar] [CrossRef]
- Geiger, J.L.; Ismaila, N.; Beadle, B.; Caudell, J.J.; Chau, N.; Deschler, D.; Glastonbury, C.; Kaufman, M.; Lamarre, E.; Lau, H.Y.; et al. Management of Salivary Gland Malignancy: ASCO Guideline. J. Clin. Oncol. 2021, 39, 1909–1941. [Google Scholar] [CrossRef]
- Migliorelli, A.; Manuelli, M.; Ciorba, A.; Stomeo, F.; Pelucchi, S.; Bianchini, C. The Role of Blood Inflammatory Markers in Salivary Gland Carcinoma: A Scoping Review. J. Clin. Med. 2025, 14, 1762. [Google Scholar] [CrossRef]
- Alsanie, I.; Shephard, A.; Azarmehr, N.; Vargas, P.; Pring, M.; Rajpoot, N.M.; Khurram, S.A. Exploring the Feasibility of AI-Based Analysis of Histopathological Variability in Salivary Gland Tumours. Sci. Rep. 2025, 15, 29171. [Google Scholar] [CrossRef]
- Lambin, P.; Rios-Velazquez, E.; Leijenaar, R.; Carvalho, S.; van Stiphout, R.G.; Granton, P.; Zegers, C.M.; Gillies, R.; Boellard, R.; Dekker, A.; et al. Radiomics: Extracting More Information from Medical Images Using Advanced Feature Analysis. Eur. J. Cancer 2012, 48, 441–446. [Google Scholar] [CrossRef]
- Kumar, V.; Gu, Y.; Basu, S.; Berglund, A.; Eschrich, S.A.; Schabath, M.B.; Forster, K.; Aerts, H.J.; Dekker, A.; Fenstermacher, D.; et al. Radiomics: The Process and the Challenges. Magn. Reson. Imaging 2012, 30, 1234–1248. [Google Scholar] [CrossRef] [PubMed]
- Bajwa, J.; Munir, U.; Nori, A.; Williams, B. Artificial Intelligence in Healthcare: Transforming the Practice of Medicine. Future Healthc. J. 2021, 8, e188–e194. [Google Scholar] [CrossRef] [PubMed]
- Migliorelli, A.; Manuelli, M.; Ciorba, A.; Stomeo, F.; Pelucchi, S.; Bianchini, C. Role of Artificial Intelligence in Human Papillomavirus Status Prediction for Oropharyngeal Cancer: A Scoping Review. Cancers 2024, 16, 4040. [Google Scholar] [CrossRef] [PubMed]
- Mayo-Yáñez, M.; Rameau, A.; Vaira, L.A.; Louvrier, M.; Sanchez Barrueco, A.; Alcalá-Rueda, I.; García-Curdi, F.; Mejuto-Torreiro, L.; Klein-Rodríguez, A.; Herranz-Larrañeta, J.; et al. Patient Perceptions of Artificial Intelligence in Otolaryngology-Head and Neck Surgery: An International Study. Ear Nose Throat J. 2025, 1455613251351774. [Google Scholar] [CrossRef]
- Cammaroto, G.; Migliorelli, A.; Pelucchi, S.; Meccariello, G.; De Vito, A. Social (Chats), Websites, and ChatGPT in Eagle Syndrome. In EAGLE Syndrome: The Many Faces of the Elongated Styloid Process; Springer Nature Switzerland: Cham, Switzerland, 2025; pp. 33–42. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M.; the QUADAS-2 Group. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Vernuccio, F.; Arnone, F.; Cannella, R.; Verro, B.; Comelli, A.; Agnello, F.; Stefano, A.; Gargano, R.; Rodolico, V.; Salvaggio, G.; et al. Diagnostic Performance of Qualitative and Radiomics Approach to Parotid Gland Tumors: Which Is the Added Benefit of Texture Analysis? Br. J. Radiol. 2021, 94, 20210340. [Google Scholar] [CrossRef]
- Piludu, F.; Marzi, S.; Ravanelli, M.; Pellini, R.; Covello, R.; Terrenato, I.; Farina, D.; Campora, R.; Ferrazzoli, V.; Vidiri, A. MRI-Based Radiomics to Differentiate between Benign and Malignant Parotid Tumors with External Validation. Front. Oncol. 2021, 11, 656918. [Google Scholar] [CrossRef]
- Zheng, Y.M.; Xu, W.J.; Hao, D.P.; Liu, X.J.; Gao, C.P.; Tang, G.Z.; Li, J.; Wang, H.X.; Dong, C. A CT-Based Radiomics Nomogram for Differentiation of Lympho-Associated Benign and Malignant Lesions of the Parotid Gland. Eur. Radiol. 2021, 31, 2886–2895. [Google Scholar] [CrossRef]
- Zheng, Y.M.; Li, J.; Liu, S.; Cui, J.F.; Zhan, J.F.; Pang, J.; Zhou, R.Z.; Li, X.L.; Dong, C. MRI-Based Radiomics Nomogram for Differentiation of Benign and Malignant Lesions of the Parotid Gland. Eur. Radiol. 2021, 31, 4042–4052. [Google Scholar] [CrossRef] [PubMed]
- Ammari, S.; Quillent, A.; Elvira, V.; Bidault, F.; Garcia, G.C.T.E.; Hartl, D.M.; Balleyguier, C.; Lassau, N.; Chouzenoux, É. Using Machine Learning on MRI Radiomics to Diagnose Parotid Tumours before Comparing Performance with Radiologists: A Pilot Study. J. Imaging Inform. Med. 2025, 38, 1496–1508. [Google Scholar] [CrossRef] [PubMed]
- Nakajo, M.; Hirahara, D.; Jinguji, M.; Hirahara, M.; Tani, A.; Nagano, H.; Takumi, K.; Kamimura, K.; Kanzaki, F.; Yamashita, M.; et al. Applying Deep Learning-Based Ensemble Model to [18F]-FDG-PET-Radiomic Features for Differentiating Benign from Malignant Parotid Gland Diseases. Jpn. J. Radiol. 2025, 43, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Takumi, K.; Nagano, H.; Kikuno, H.; Kumagae, Y.; Fukukura, Y.; Yoshiura, T. Differentiating Malignant from Benign Salivary Gland Lesions: A Multiparametric Non-Contrast MR Imaging Approach. Sci. Rep. 2021, 11, 2780. [Google Scholar] [CrossRef]
- Eravcı, F.C.; Sözmen Cılız, D.; Özcan, K.M.; Çolak, M.; Çavuşoğlu, M.; Karakurt, S.E.; Karakuş, M.F. Conventional and Diffusion-Weighted MR Imaging Findings of Parotid Gland Tumors. Turk. Arch. Otorhinolaryngol. 2020, 58, 174–180. [Google Scholar] [CrossRef]
- Aringhieri, G.; Fanni, S.C.; Febi, M.; Colligiani, L.; Cioni, D.; Neri, E. The Role of Radiomics in Salivary Gland Imaging: A Systematic Review and Radiomics Quality Assessment. Diagnostics 2022, 12, 3002. [Google Scholar] [CrossRef]
- Mao, K.; Wong, L.M.; Zhang, R.; So, T.Y.; Shan, Z.; Hung, K.F.; Ai, Q.Y.H. Radiomics Analysis in Characterization of Salivary Gland Tumors on MRI: A Systematic Review. Cancers 2023, 15, 4918. [Google Scholar] [CrossRef]
- Xue, C.; Zhou, Y.; Lo, G.G.; Wong, O.L.; Yu, S.K.; Cheung, K.Y.; Yuan, J. Reliability of Radiomics Features Due to Image Reconstruction Using a Standardized T2-Weighted Pulse Sequence for MR-Guided Radiotherapy: An Anthropomorphic Phantom Study. Magn. Reson. Med. 2021, 85, 3434–3446. [Google Scholar] [CrossRef]
- Noortman, W.A.; Aide, N.; Vriens, D.; Arkes, L.S.; Slump, C.H.; Boellaard, R.; Goeman, J.J.; Deroose, C.M.; Machiels, J.P.; Licitra, L.F.; et al. Development and External Validation of a PET Radiomic Model for Prognostication of Head and Neck Cancer. Cancers 2023, 15, 2681. [Google Scholar] [CrossRef]
- Bianchini, C.; Caracciolo, M.; Urso, L.; Ciorba, A.; Bonsembiante, A.; Migliorelli, A.; Corazzi, V.; Carandina, I.; Ortolan, N.; Cittanti, C.; et al. Role of 18F-FDG PET/CT in Evaluating Lymph Node Status in Patients with Head and Neck Squamous Cell Carcinoma. Acta Otorhinolaryngol. Ital. 2023, 43, 235–244. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, L.V.; Langendijk, J.A.; Zhai, T.T.; Vedelaar, T.A.; Noordzij, W.; Steenbakkers, R.J.H.M.; Sijtsema, N.M. Delta-Radiomics Features during Radiotherapy Improve the Prediction of Late Xerostomia. Sci. Rep. 2019, 9, 12483. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, K.; Lee, S.H.; Cheng, Z.; Lakshminarayanan, P.; Peng, L.; Han, P.; McNutt, T.R.; Quon, H.; Lee, J. Predicting Acute Radiation Induced Xerostomia in Head and Neck Cancer Using MR and CT Radiomics of Parotid and Submandibular Glands. Radiat. Oncol. 2019, 14, 131. [Google Scholar] [CrossRef] [PubMed]
- Vukicevic, A.M.; Milic, V.; Zabotti, A.; Hocevar, A.; De Lucia, O.; Filippou, G.; Frangi, A.F.; Tzioufas, A.; De Vita, S.; Filipovic, N. Radiomics-Based Assessment of Primary Sjögren’s Syndrome from Salivary Gland Ultrasonography Images. IEEE J. Biomed. Health Inform. 2020, 24, 835–843. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Muraoka, H.; Hirahara, N.; Sawada, E.; Okada, S.; Kaneda, T. Quantitative Assessment of Normal Submandibular Glands and Submandibular Sialadenitis Using CT Texture Analysis: A Retrospective Study. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2021, 132, 112–117. [Google Scholar] [CrossRef]
| Author (Yrs) | Country | Modality | Reference Standard | N Training/N Validation | Segmentation | Software | ICC/Repeatability | Validation Type | AUC (95% CI) | Calibration/Clinical Utility |
|---|---|---|---|---|---|---|---|---|---|---|
| Vernuccio (2021) [21] | Italy | MRI | H | 0/57 | Manual ROI (MRI T1, T2, post-contrast) | Horos/MATLAB | ICC variable (poor–excellent) | Internal (cross-validation) | Best radiomics benign vs. malignant: AUC 0.927; head & neck radiologist AUC 0.970 (95% CI 0.934–1.000) | NA |
| Piludu (2021) [22] | Italy | MRI | H | 69/44 | Lesion delineation | S-IBEX/3D Slicer | ICC used for feature selection | External (independent cohort) | Accuracy 86.7–91.9%; AUC not explicitly stated | Calibration curve + DCA |
| Zheng (2021) [23] | China | CT | H | 70/31 | Semi-automatic | NA | ICC ≥ 0.75 | External (two-center) | Nomogram AUC 0.952 (train), 0.938 (val) | DCA performed; good calibration |
| Zheng (2021) [24] | China | MRI | H | 80/35 | Manual | NA | ICC > 0.80 | External (split-sample) | Radiomics + clinical nomogram AUC 0.983 (train), 0.950 (val) | Good calibration; DCA positive net benefit |
| Ammari (2024) [25] | France | MRI | H | 86/25 | Manual | Olea Sphere 3.0.x | NA | Internal (train/test) | Random Forest multi-class accuracy 0.720; OvR AUC 0.838; benign/malignant AUC 0.769 | NA |
| Nakajo (2025) [26] | Japan | PET/CT | H | 44/19 | VOI | LIFEx v6.00 | NA | Internal (train/test) | Ensemble DL model AUC 0.976 (test) | NA |
| Author (Yrs) | Objective | Major Results |
|---|---|---|
| Vernuccio (2021) [21] | Evaluate whether MRI-based texture analysis improves the differentiation of malignant parotid tumors and distinguishes pleomorphic adenoma from Warthin tumor compared with conventional imaging. | Radiologists showed higher accuracy than radiomics in detecting malignancy, while a T2-weighted texture-based model improved non-specialists’ differentiation of pleomorphic adenoma and Warthin tumor. |
| Piludu (2021) [22] | Assess MRI-based radiomics using T2-weighted images and ADC maps to differentiate parotid lesions, and validate predictive models on an external cohort. | Radiomic analysis of ADC and T2-weighted images, combined with qualitative features such as margins and contrast enhancement, achieved good-to-excellent diagnostic accuracy in differentiating parotid lesions. |
| Zheng (2021) [23] | Develop and externally validate a CT-based radiomics-plus-clinical nomogram to preoperatively differentiate parotid BLEL from MALT lymphoma. | The radiomic nomogram integrating clinical factors and radiomic features effectively differentiated parotid BLEL from MALT lymphoma, achieving high predictive performance (AUC = 0.983 for training and 0.950 for validation). |
| Zheng (2021) [24] | Develop and validate a radiomic nomogram based on magnetic resonance imaging to differentiate between benign and malignant parotid gland tumors preoperatively. | Incorporating clinical factors and the radiomic signature, the radiomic nomogram achieved an AUC value of 0.952 in the training set and 0.938 in the validation set. |
| Ammari (2024) [25] | Present a machine learning algorithm that can classify parotid gland tumors into their respective histopathological subtypes. | The random forest model performed best, achieving a multi-class accuracy of 0.720 and an average OvR AUC of 0.838 on the test set. It achieved OvR accuracies of 0.840 for pleomorphic adenomas and Warthin tumors, and 0.760 for carcinomas (benign/malignant distinction). All features selected by the algorithm originated from the T2w sequence. |
| Nakajo (2025) [26] | Use radiomic features to develop and identify ML models based on PET/CT in order to differentiate between benign and malignant parotid gland diseases. | In the test group, three of the five conventional ML models achieved an AUC greater than 0.80 (range: 0.815–0.929). The DL-based ensemble model achieved the highest AUC value (0.976). |
| Author (Yrs) | Patient Selection | Index Test | Reference Standard | Flow & Timing | Applicability Concerns |
|---|---|---|---|---|---|
| Vernuccio (2021) [21] | High | Low | Unclear | High | Low–Moderate |
| Piludu (2021) [22] | High | Unclear | Low | Unclear | Low |
| Zheng (2021) [23] | Low | Low | Low | Low | Low |
| Zheng (2021) [24] | Low | Low | Low | Low | Low |
| Ammari (2024) [25] | High | Low | Low | Unclear | Moderate |
| Nakajo (2025) [26] | Unclear | Low | Unclear | Unclear | Low–Moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Migliorelli, A.; Manuelli, M.; Ciorba, A.; Stomeo, F.; Pelucchi, S.; Bianchini, C. Role of Radiomics in Parotid Malignant Disease: A Scoping Review. Cancers 2025, 17, 3284. https://doi.org/10.3390/cancers17203284
Migliorelli A, Manuelli M, Ciorba A, Stomeo F, Pelucchi S, Bianchini C. Role of Radiomics in Parotid Malignant Disease: A Scoping Review. Cancers. 2025; 17(20):3284. https://doi.org/10.3390/cancers17203284
Chicago/Turabian StyleMigliorelli, Andrea, Marianna Manuelli, Andrea Ciorba, Francesco Stomeo, Stefano Pelucchi, and Chiara Bianchini. 2025. "Role of Radiomics in Parotid Malignant Disease: A Scoping Review" Cancers 17, no. 20: 3284. https://doi.org/10.3390/cancers17203284
APA StyleMigliorelli, A., Manuelli, M., Ciorba, A., Stomeo, F., Pelucchi, S., & Bianchini, C. (2025). Role of Radiomics in Parotid Malignant Disease: A Scoping Review. Cancers, 17(20), 3284. https://doi.org/10.3390/cancers17203284








