Occurrence Rates of Delirium in Brain Tumor Patients: A Systematic Review and Meta-Analysis
Simple Summary
Abstract
1. Introduction
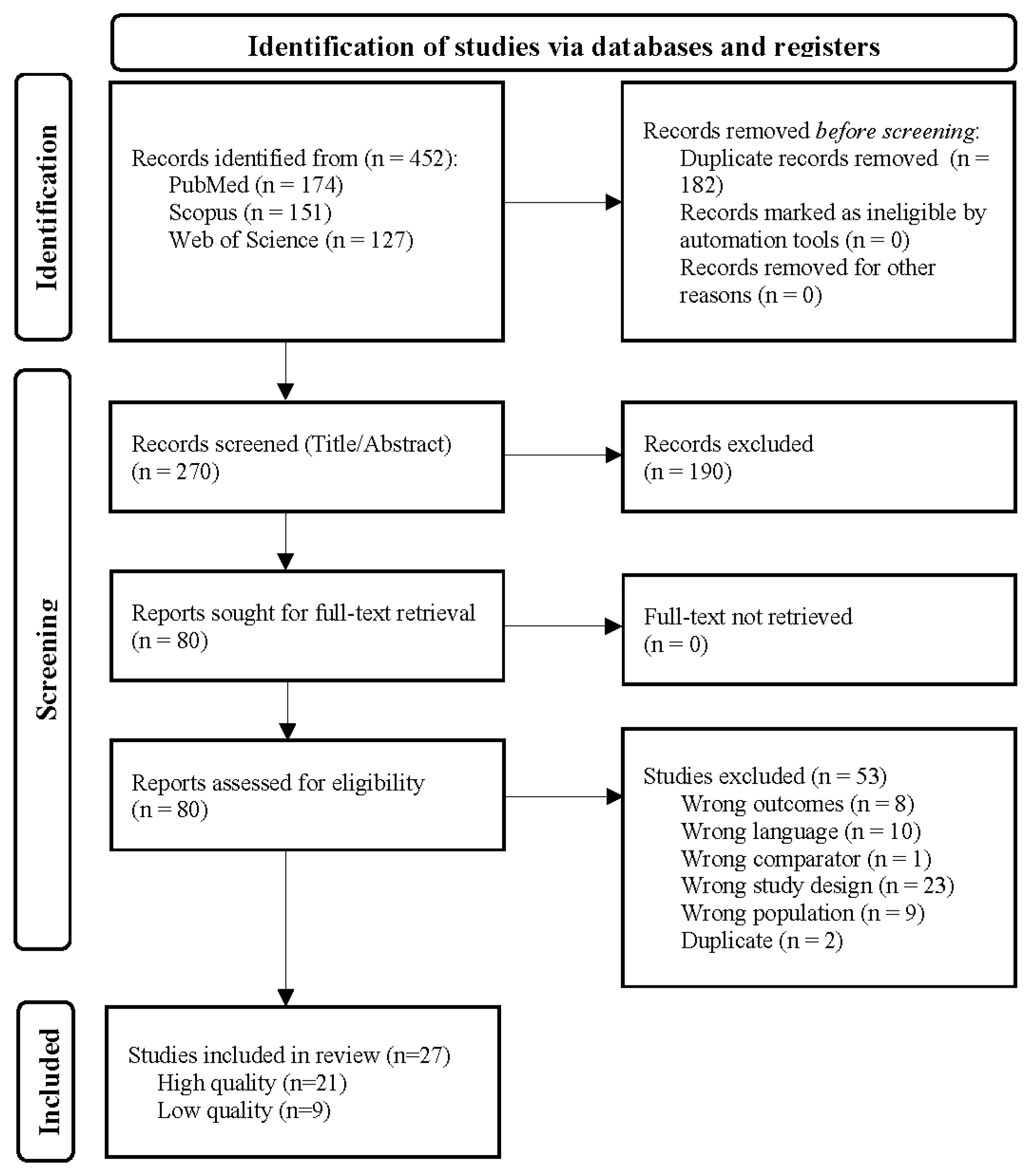
2. Methods
2.1. Search Strategy
2.2. Study Population
2.3. Data Collection and Extraction
2.4. Quality Assessment
2.5. Data Analysis
2.6. Data Availability
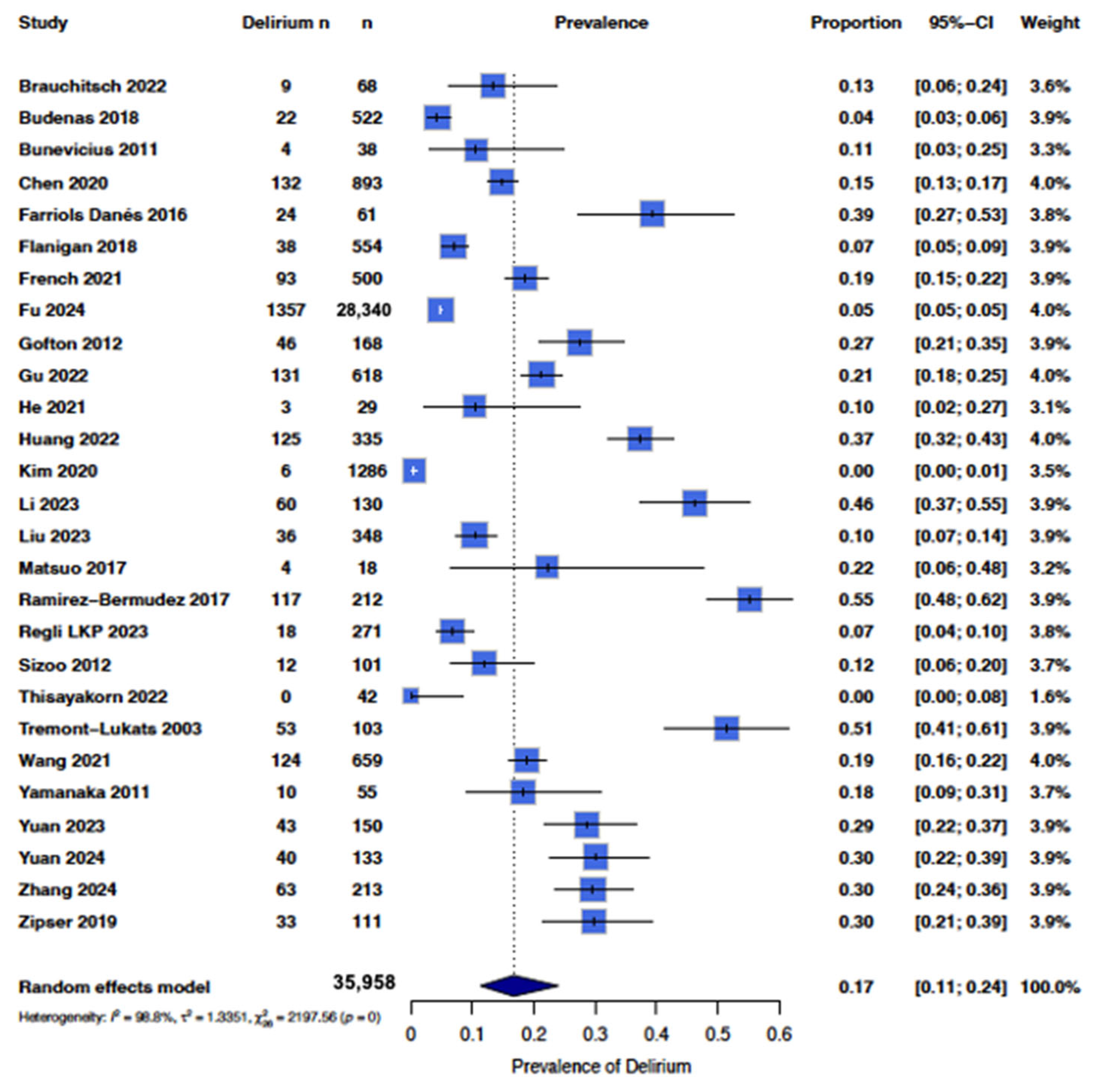
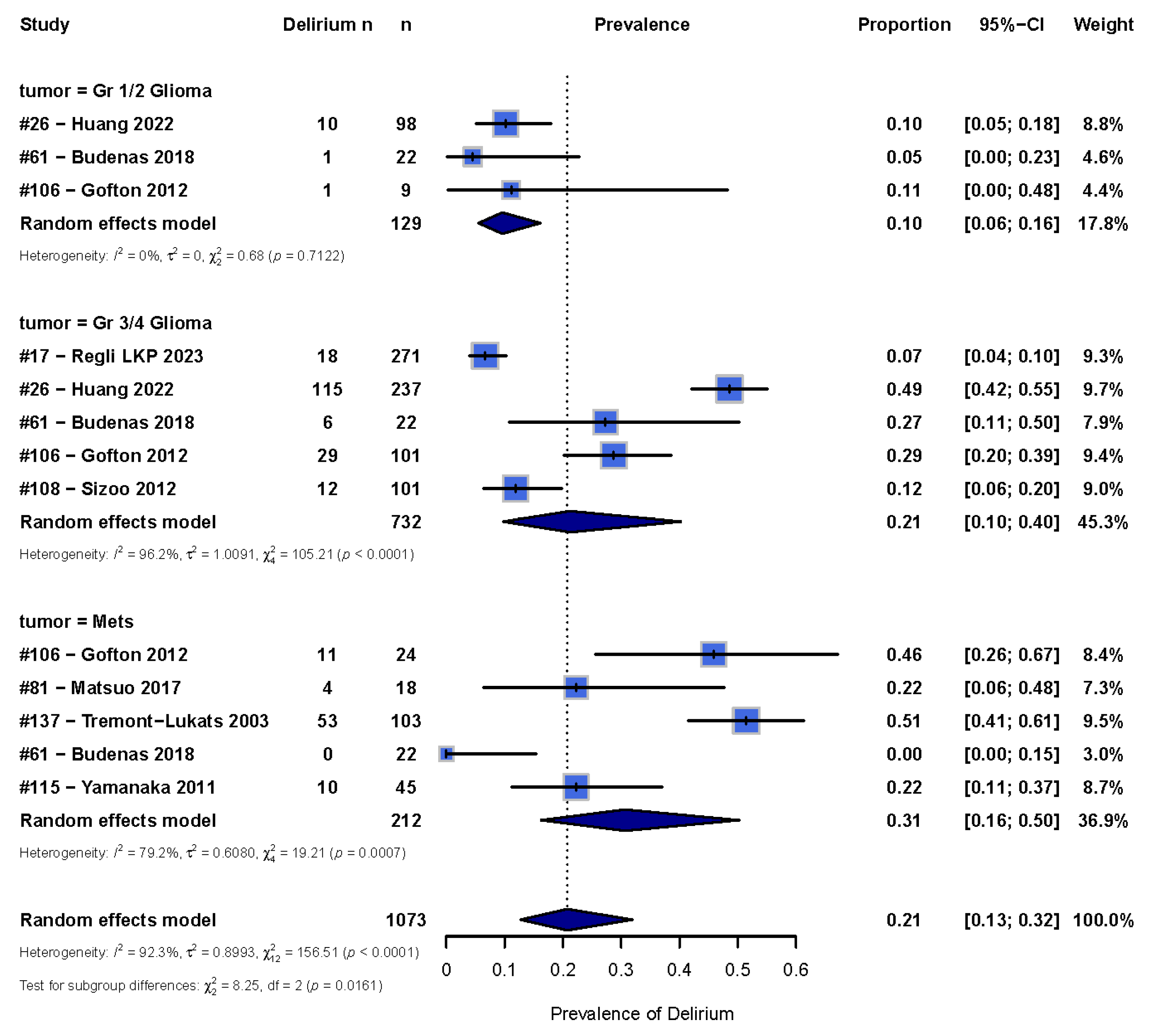
3. Results
3.1. Overall Occurrence
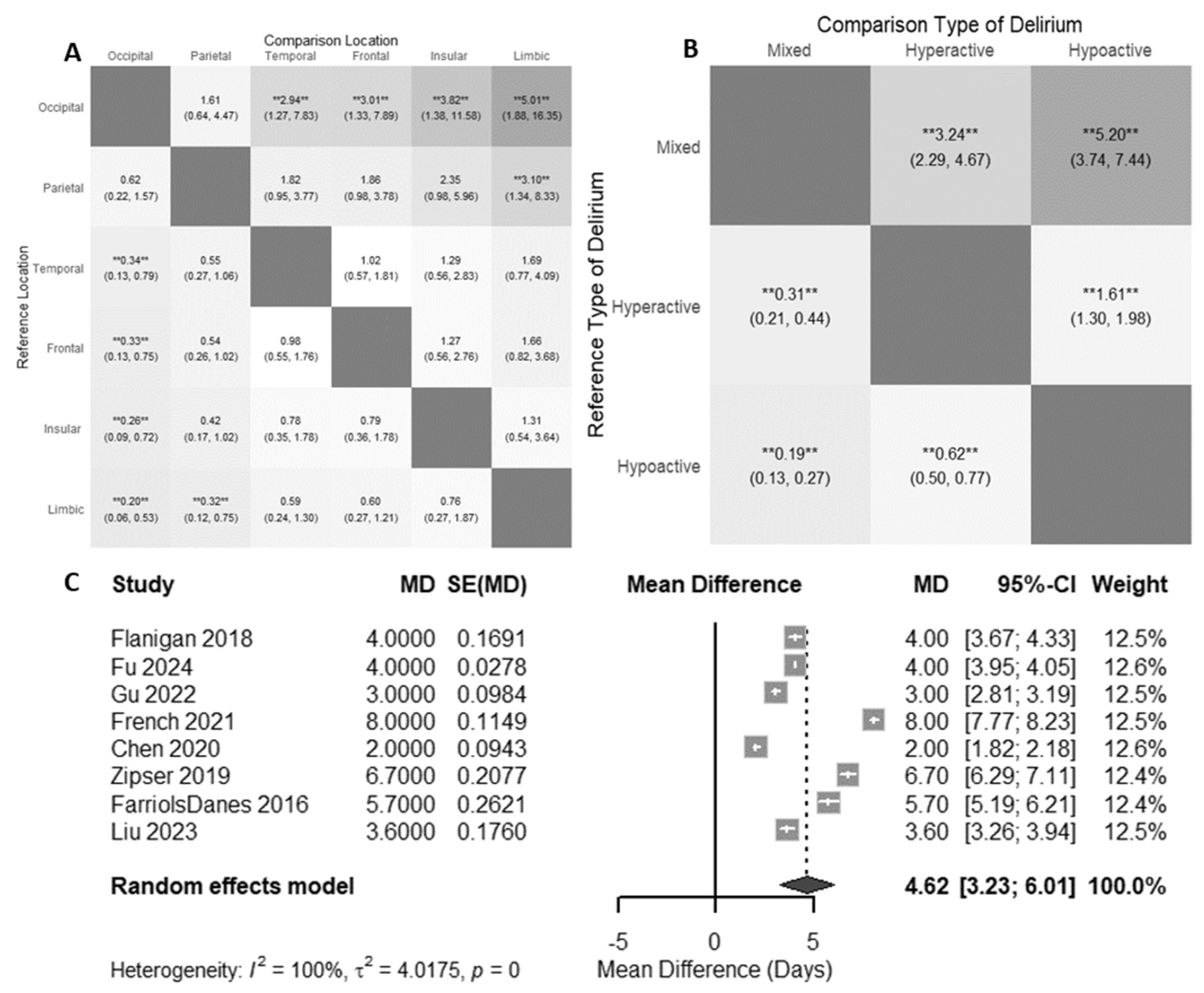
3.2. Tumor Location
3.3. Delirium Subtype
3.4. Length of Stay
3.5. Timepoints and Timeframe
3.6. Publication Bias Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ely, E.W.; Margolin, R.; Francis, J.; May, L.; Truman, B.; Dittus, R.; Speroff, T.; Gautam, S.; Bernard, G.R.; Inouye, S.K. Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit. Care Med. 2001, 29, 1370–1379. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.E.; Mart, M.F.; Cunningham, C.; Shehabi, Y.; Girard, T.D.; MacLullich, A.M.; Slooter, A.J.; Ely, E.W. Delirium. Nat. Rev. Dis. Primers 2020, 6, 90. [Google Scholar] [CrossRef]
- van den Boogaard, M.; Schoonhoven, L.; Evers, A.W.M.; van der Hoeven, J.G.; van Achterberg, T.; Pickkers, P. Delirium in critically ill patients: Impact on long-term health-related quality of life and cognitive functioning. Crit. Care Med. 2012, 40, 112. [Google Scholar] [CrossRef]
- Abelha, F.J.; Luís, C.; Veiga, D.; Parente, D.; Fernandes, V.; Santos, P.; Botelho, M.; Santos, A.; Santos, C. Outcome and quality of life in patients with postoperative delirium during an ICU stay following major surgery. Crit. Care 2013, 17, R257. [Google Scholar] [CrossRef] [PubMed]
- Basinski, J.R.; Alfano, C.M.; Katon, W.J.; Syrjala, K.L.; Fann, J.R. Impact of Delirium on Distress, Health-Related Quality of Life, and Cognition 6 Months and 1 Year after Hematopoietic Cell Transplant. Biol. Blood Marrow Transplant. 2010, 16, 824–831. [Google Scholar] [CrossRef]
- Lobo-Valbuena, B.; Molina, R.; Castañeda-Vozmediano, R.; Lopez de la Oliva Calvo, L.; Abella, A.; Garcia-Arias, M.M.; Salinas Gabiña, I.; Gordo, F. Functional independence, frailty and perceived quality of life in patients who developed delirium during ICU stay: A prospective cohort study. Eur. J. Med. Res. 2023, 28, 560. [Google Scholar] [CrossRef]
- Hofhuis, J.G.M.; Schermer, T.; Spronk, P.E. Mental health-related quality of life is related to delirium in intensive care patients. Intensive Care Med. 2022, 48, 1197–1205. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, C.B.; Collet, M.O.; Samuelson, K. Struggling to return to everyday life—The experiences of quality of life 1 year after delirium in the intensive care unit. Nurs. Crit. Care 2023, 28, 670–678. [Google Scholar] [CrossRef]
- Rhee, J.Y.; Colman, M.A.; Mendu, M.; Shah, S.J.; Fox, M.D.; Rost, N.S.; Kimchi, E.Y. Associations Between Stroke Localization and Delirium: A Systematic Review and Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2022, 31, 106270. [Google Scholar] [CrossRef]
- Shaw, R.C.; Walker, G.; Elliott, E.; Quinn, T.J. Occurrence Rate of Delirium in Acute Stroke Settings: Systematic Review and Meta-Analysis. Stroke 2019, 50, 3028–3036. [Google Scholar] [CrossRef]
- American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. American Geriatrics Society Abstracted Clinical Practice Guideline for Postoperative Delirium in Older Adults. J. Am. Geriatr. Soc. 2015, 63, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Reynish, E.L.; Hapca, S.M.; De Souza, N.; Cvoro, V.; Donnan, P.T.; Guthrie, B. Epidemiology and outcomes of people with dementia, delirium, and unspecified cognitive impairment in the general hospital: Prospective cohort study of 10,014 admissions. BMC Med. 2017, 15, 140. [Google Scholar] [CrossRef]
- Lawson, R.A.; Richardson, S.J.; Yarnall, A.J.; Burn, D.J.; Allan, L.M. Identifying delirium in Parkinson disease: A pilot study. Int. J. Geriatr. Psychiatry 2020, 35, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Green, S.; Perrott, S.L.; McCleary, A.; Sleeman, I.; Maple-Grødem, J.; Counsell, C.E.; Macleod, A.D. First delirium episode in Parkinson’s disease and parkinsonism: Incidence, predictors, and outcomes. npj Park. Dis. 2021, 7, 92. [Google Scholar] [CrossRef]
- Zaal, I.J.; Devlin, J.W.; Peelen, L.M.; Slooter, A.J.C. A Systematic Review of Risk Factors for Delirium in the ICU. Crit. Care Med. 2015, 43, 40–47. [Google Scholar] [CrossRef]
- Yamato, K.; Ikeda, A.; Endo, M.; Filomeno, R.; Kiyohara, K.; Inada, K.; Nishimura, K.; Tanigawa, T. An association between cancer type and delirium incidence in Japanese elderly patients: A retrospective longitudinal study. Cancer Med. 2022, 12, 2407–2416. [Google Scholar] [CrossRef]
- Lawlor, P.G.; Gagnon, B.; Mancini, I.L.; Pereira, J.L.; Hanson, J.; Suarez-Almazor, M.E.; Bruera, E.D. Occurrence, causes, and outcome of delirium in patients with advanced cancer: A prospective study. Arch. Intern. Med. 2000, 160, 786–794. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Kim, N.; Min, K.T.; Kim, E.H.; Oh, H.; Choi, S.H. Sleep disturbance and delirium in patients with acromegaly in the early postoperative period after transsphenoidal pituitary surgery. Medecine 2020, 99, e23157. [Google Scholar] [CrossRef]
- Thisayakorn, P.; Schuermeyer, I. Psychiatric adverse effects of levetiracetam in Malignant glioma populations; a retrospective cohort study. J. Health Sci. Med. Res. 2022, 40, 27–34. [Google Scholar] [CrossRef]
- Ramírez-Bermúdez, J.; Aguilar-Venegas, L.C.; Calero-Moscoso, C.; Ramírez-Abascal, M.; Nente-Chávez, F.; Flores-Reynoso, S.; Dolores-Velasco, F.; Ramos-Tisnado, R. Neurology and psychiatry interphase in patients hospitalized due to central nervous system diseases. Gac. Med. Mex. 2010, 146, 108–111. [Google Scholar]
- Grover, S.; Kate, N. Assessment scales for delirium: A review. World J. Psychiatry 2012, 2, 58–70. [Google Scholar] [CrossRef]
- Al Farsi, R.S.; Al Alawi, A.M.; Al Huraizi, A.R.; Al-Saadi, T.; Al-Hamadani, N.; Al Zeedy, K.; Al-Maqbali, J.S. Delirium in Medically Hospitalized Patients: Prevalence, Recognition and Risk Factors: A Prospective Cohort Study. J. Clin. Med. 2023, 12, 3897. [Google Scholar] [CrossRef]
- Ryan, D.J.; O’Regan, N.A.; Caoimh, R.Ó.; Clare, J.; O’Connor, M.; Leonard, M.; McFarland, J.; Tighe, S.; O’Sullivan, K.; Trzepacz, P.T.; et al. Delirium in an adult acute hospital population: Predictors, prevalence and detection. BMJ Open 2013, 3, e001772. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Chapter 7: Systematic reviews of Aetiology and risk. In JBI Manual for Evidence Synthesis; Aromataris, E., Lockwood, C., Porritt, K., Pilla, B., Jordan, Z., Eds.; JBI: Adelaide, Australia, 2024. [Google Scholar] [CrossRef]
- Gelman, A.; Hill, J.; Yajima, M. Why We (Usually) Don’t Have to Worry About Multiple Comparisons. J. Res. Educ. Eff. 2012, 5, 189–211. [Google Scholar] [CrossRef]
- Brauchitsch, S.V.; Strzelczyk, A.; Rosenow, F.; Neuhaus, E.; Dubinski, D.; Steinbach, J.P.; Voss, M. High end-of-life incidence of seizures and status epilepticus in patients with primary and secondary brain tumors. J. Neurooncol. 2022, 160, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Jiang, H.; Chen, B.; Fan, L.; Shi, W.; Jin, Y.; Ren, X.; Lang, L.; Zhu, F. The Incidence and Predictors of Postoperative Delirium After Brain Tumor Resection in Adults: A Cross-Sectional Survey. World Neurosurg. 2020, 140, e129–e139. [Google Scholar] [CrossRef]
- Farriols Danés, C.; Landa Teran, C.P.; Ruiz Ripoll, A.I.; Planas Domingo, J. Prevalence of delirium in patients with advanced cancer admitted to a palliative care unit. Med. Paliativa. 2016, 23, 165–171. [Google Scholar] [CrossRef]
- Flanigan, P.M.; Jahangiri, A.; Weinstein, D.; Dayani, F.; Chandra, A.; Kanungo, I.; Choi, S.; Sankaran, S.; Molinaro, A.M.; McDermott, M.W.; et al. Postoperative Delirium in Glioblastoma Patients: Risk Factors and Prognostic Implications. Neurosurgery 2018, 83, 1161–1172. [Google Scholar] [CrossRef]
- French, J.; Weber, T.; Ge, B.; Litofsky, N.S. Postoperative Delirium in Patients After Brain Tumor Surgery. World Neurosurg. 2021, 155, e472–e479. [Google Scholar] [CrossRef]
- Fu, W.; Li, Y.; Liu, R.; Li, J. Incidence and Risk Factors of Delirium Following Brain Tumor Resection: A Retrospective National Inpatient Sample Database Study. World Neurosurg. 2024, 189, e533–e543. [Google Scholar] [CrossRef] [PubMed]
- Gofton, T.E.; Graber, J.; Carver, A. Identifying the palliative care needs of patients living with cerebral tumors and metastases: A retrospective analysis. J. Neurooncol. 2012, 108, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Gu, W.J.; Zhou, J.X.; Ji, R.Q.; Zhou, L.Y.; Wang, C.M. Incidence, risk factors, and consequences of emergence delirium after elective brain tumor resection. Surgeon 2022, 20, e214–e220. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Qian, J.; Wang, X.; Lin, J.; Yang, S.; Hu, R.; Xian, J.; Feng, H.; Chen, Y.; Tan, B. Identifying hormones and other perioperative risk factors for postoperative delirium after endoscope-assisted transsphenoidal pituitary adenoma resection: A retrospective, matched cohort study. Brain Behav. 2023, 13, e3041. [Google Scholar] [CrossRef]
- Ramirez-Bermudez, J.; Perez-Esparza, R.; Aguilar-Venegas, L.C.; Sachdev, P. Neuropsychiatry: Towards a Philosophy of Praxis. Rev. Colomb. Psiquiatría 2017, 46, 28–35. [Google Scholar] [CrossRef]
- Regli, L.K.P.; Huijs, S.M.H.; Pasmans, R.C.O.S.; Leue, C.; Dijkstra, J.B.; Eekers, D.B.P.; Hovinga, K.E.; Anten, M.H.M.E.; Hoeben, A.; Broen, M.P.G. Incidence of clinically relevant psychiatric symptoms during glioblastoma treatment: An exploratory study. J. Neurooncol. 2023, 163, 185–194. [Google Scholar] [CrossRef]
- Sizoo, E.M.; Pasman, H.R.W.; Buttolo, J.; Heimans, J.J.; Klein, M.; Deliens, L.; Reijneveld, J.C.; Taphoorn, M.J. Decision-making in the end-of-life phase of high-grade glioma patients. Eur. J. Cancer 2012, 48, 226–232. [Google Scholar] [CrossRef]
- Tremont-Lukats, I.W.; Bobustuc, G.; Lagos, G.K.; Lolas, K.; Kyritsis, A.P.; Puduvalli, V.K. Brain metastasis from prostate carcinoma: The M. D. Anderson Cancer Cent experience. Cancer 2003, 98, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.M.; Ma, Y.L.; Yang, X.Y.; Ji, R.Q.; Gu, W.J.; Zhou, J.X. Association of preoperative frailty with postoperative delirium after elective brain tumor resection: Retrospective analysis of a prospective cohort. Surgery 2021, 170, 1763–1769. [Google Scholar] [CrossRef]
- Yamanaka, R.; Koga, H.; Yamamoto, Y.; Yamada, S.; Sano, T.; Fukushige, T. Characteristics of patients with brain metastases from lung cancer in a palliative care center. Support Care Cancer 2011, 19, 467–473. [Google Scholar] [CrossRef]
- Zhang, S.; Chen, Y.; Wang, X.; Liu, J.; Zhang, G. Related factors of delirium after transsphenoidal endoscopic pituitary adenoma resection-A matched retrospective cohort study. J. Clin. Neurosci. 2024, 123, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.W.; Zhang, X.K.; Li, H.Y.; Wang, Y.G.; Jing, B.; Chen, Y.; Patel, M.B.; Ely, E.W.; Liu, Y.O.; Zhou, J.X.; et al. Higher Grade Glioma Increases the Risk of Postoperative Delirium: Deficient Brain Compensation Might Be a Potential Mechanism of Postoperative Delirium. Front. Aging Neurosci. 2022, 14, 822984. [Google Scholar] [CrossRef]
- Budėnas, A.; Tamašauskas, Š.; Šliaužys, A.; Navickaitė, I.; Sidaraitė, M.; Pranckevičienė, A.; Deltuva, V.P.; Tamašauskas, A.; Bunevičius, A. Incidence and clinical significance of postoperative delirium after brain tumor surgery. Acta Neurochir. 2018, 160, 2327–2337. [Google Scholar] [CrossRef]
- Bunevicius, A.; Deltuva, V.; Tamasauskas, S.; Tamasauskas, A.; Bunevicius, R. Depression, anxiety and delirium are associated with thyroid axis function in brain tumor patients. Eur. Neuropsychopharmacol. 2011, 21, S353–S354. [Google Scholar] [CrossRef]
- He, X.; Cheng, K.M.; Duan, Y.Q.; Xu, S.S.; Gao, H.R.; Miao, M.Y.; Li, H.L.; Chen, K.; Yang, Y.L.; Zhang, L.; et al. Feasibility of low-dose dexmedetomidine for prevention of postoperative delirium after intracranial operations: A pilot randomized controlled trial. BMC Neurol. 2021, 21, 472. [Google Scholar] [CrossRef]
- Li, S.; Li, R.; Li, M.; Cui, Q.; Zhang, X.; Ma, T.; Wang, D.; Zeng, M.; Li, H.; Bao, Z.; et al. Dexmedetomidine administration during brain tumour resection for prevention of postoperative delirium: A randomised trial. Br. J. Anaesth. 2023, 130, e307–e316. [Google Scholar] [CrossRef]
- Matsuo, N.; Morita, T.; Matsuda, Y.; Okamoto, K.; Matsumoto, Y.; Kaneishi, K.; Odagiri, T.; Sakurai, H.; Katayama, H.; Mori, I.; et al. Predictors of Delirium in Corticosteroid-Treated Patients with Advanced Cancer: An Exploratory, Multicenter, Prospective, Observational Study. J. Palliat. Med. 2017, 20, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Gu, Q.; Zhu, M.; Zhang, Y.; Lan, M. Frailty-originated early rehabilitation reduces postoperative delirium in brain tumor patients: Results from a prospective randomized study. Asia Pac. J. Oncol. Nurs. 2023, 10, 100263. [Google Scholar] [CrossRef]
- Yuan, C.; Cheng, Z.; Liu, Y.; You, Y.; Wang, L.; Li, D.; Zhong, L. Incidence and risk factors of post-operative delirium in glioma patients: A prospective cohort study in general wards. J. Clin. Nurs. 2024, 33, 3539–3547. [Google Scholar] [CrossRef]
- Zipser, C.M.; Deuel, J.; Ernst, J.; Schubert, M.; von Känel, R.; Böttger, S. The predisposing and precipitating risk factors for delirium in neurosurgery: A prospective cohort study of 949 patients. Acta Neurochir. 2019, 161, 1307–1315. [Google Scholar] [CrossRef]
- Jawabri, K.H.; Sharma, S. Physiology, Cerebral Cortex Functions. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: http://www.ncbi.nlm.nih.gov/books/NBK538496/ (accessed on 12 September 2024).
- Svokos, K.A.; Salhia, B.; Toms, S.A. Molecular Biology of Brain Metastasis. Int. J. Mol. Sci. 2014, 15, 9519–9530. [Google Scholar] [CrossRef] [PubMed]
- Siam, L.; Bleckmann, A.; Chaung, H.N.; Mohr, A.; Klemm, F.; Barrantes-Freer, A.; Blazquez, R.; Wolff, H.A.; Lüke, F.; Rohde, V.; et al. The metastatic infiltration at the metastasis/brain parenchyma-interface is very heterogeneous and has a significant impact on survival in a prospective study. Oncotarget 2015, 6, 29254–29267. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.; Joo, B.; Park, J.; Park, H.H.; Park, M.; Ahn, S.J.; Suh, S.H.; Kim, J.J.; Oh, J. Delirium-related factors and their prognostic value in patients undergoing craniotomy for brain metastasis. Front. Neurol. 2022, 13, 988293. [Google Scholar] [CrossRef] [PubMed]
- Tafani, M.; Di Vito, M.; Frati, A.; Pellegrini, L.; De Santis, E.; Sette, G.; Eramo, A.; Sale, P.; Mari, E.; Santoro, A.; et al. Pro-inflammatory gene expression in solid glioblastoma microenvironment and in hypoxic stem cells from human glioblastoma. J. Neuroinflamm. 2011, 8, 32. [Google Scholar] [CrossRef]
- Alghamri, M.S.; McClellan, B.L.; Hartlage, C.S.; Haase, S.; Faisal, S.M.; Thalla, R.; Dabaja, A.; Banerjee, K.; Carney, S.V.; Mujeeb, A.A.; et al. Targeting Neuroinflammation in Brain Cancer: Uncovering Mechanisms, Pharmacological Targets, and Neuropharmaceutical Developments. Front. Pharmacol. 2021, 12, 680021. [Google Scholar] [CrossRef]
- Seeley, W.W. The Salience Network: A Neural System for Perceiving and Responding to Homeostatic Demands. J. Neurosci. 2019, 39, 9878–9882. [Google Scholar] [CrossRef]
- Young, J.W.S. The network model of delirium. Med. Hypotheses 2017, 104, 80–85. [Google Scholar] [CrossRef]
- Khan, B.A.; Perkins, A.J.; Gao, S.; Hui, S.L.; Campbell, N.L.; Farber, M.O.; Chlan, L.L.; Boustani, M.A. The CAM-ICU-7 Delirium Severity Scale: A Novel Delirium Severity Instrument for Use in the Intensive Care Unit. Crit. Care Med. 2017, 45, 851–857. [Google Scholar] [CrossRef]
- Thomas, R.I.; Cameron, D.J.; Fahs, M.C. A Prospective Study of Delirium and Prolonged Hospital Stay: Exploratory Study. Arch. Gen. Psychiatry 1988, 45, 937–940. [Google Scholar] [CrossRef]
- da Silva Machado, A.S.; Alves, M.R.T.; Vieira, D.N.; de Sousa, S.E.; Maia, F.R.; da Costa, D.A.; Raider, L. Occurrence of Delirium and Length of Stay of Patients in the Intensive Care Unit. J. Biosci. Med. 2021, 9, 1–9. [Google Scholar] [CrossRef]
- Dziegielewski, C.; Skead, C.; Canturk, T.; Webber, C.; Fernando, S.M.; Thompson, L.H.; Foster, M.; Ristovic, V.; Lawlor, P.G.; Chaudhuri, D.; et al. Delirium and Associated Length of Stay and Costs in Critically Ill Patients. Crit. Care Res. Pract. 2021, 2021, 6612187. [Google Scholar] [CrossRef] [PubMed]
- la Cour, K.N.; Andersen-Ranberg, N.C.; Weihe, S.; Poulsen, L.M.; Mortensen, C.B.; Kjer, C.K.W.; Collet, M.O.; Estrup, S.; Mathiesen, O. Distribution of delirium motor subtypes in the intensive care unit: A systematic scoping review. Crit. Care 2022, 26, 53. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Bakhla, A.K.; Gupta, S.; Raju, B.M.S.V.K.; Prasad, A. Etiologic and Cognitive Differences in Hyperactive and Hypoactive Delirium. Prim. Care Companion CNS Disord. 2015, 17, 26337. [Google Scholar] [CrossRef][Green Version]
- Krewulak, K.D.; Stelfox, H.T.; Ely, E.W.; Fiest, K.M. Risk factors and outcomes among delirium subtypes in adult ICUs: A systematic review. J. Crit. Care 2020, 56, 257–264. [Google Scholar] [CrossRef]
- van Velthuijsen, E.L.; Zwakhalen, S.M.G.; Mulder, W.J.; Verhey, F.R.J.; Kempen, G.I.J.M. Detection and management of hyperactive and hypoactive delirium in older patients during hospitalization: A retrospective cohort study evaluating daily practice. Int. J. Geriatr. Psychiatry 2018, 33, 1521–1529. [Google Scholar] [CrossRef]
- Collet, L.; Lanore, A.; Alaterre, C.; Constantin, J.M.; Martin, G.L.; Caille, A.; James, A.; Dechartres, A. Heterogeneity in the definition of delirium in ICUs and association with the intervention effect in randomized controlled trials: A meta-epidemiological study. Crit. Care 2023, 27, 170. [Google Scholar] [CrossRef]
- Thein, M.Z.A.; Pereira, J.V.; Nitchingham, A.; Caplan, G.A. A call to action for delirium research: Meta-analysis and regression of delirium associated mortality. BMC Geriatr. 2020, 20, 325. [Google Scholar] [CrossRef]
- Naidech, A.M.; Polnaszek, K.L.; Berman, M.D.; Voss, J.L. Hematoma Locations Predicting Delirium Symptoms After Intracerebral Hemorrhage. Neurocrit. Care 2016, 24, 397–403. [Google Scholar] [CrossRef]
- Mitasova, A.; Kostalova, M.; Bednarik, J.; Michalcakova, R.; Kasparek, T.; Balabanova, P.; Dusek, L.; Vohanka, S.; Ely, E.W. Poststroke delirium incidence and outcomes: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit. Care Med. 2012, 40, 484–490. [Google Scholar] [CrossRef]
- Pendlebury, S.T.; Lovett, N.G.; Smith, S.C.; Dutta, N.; Bendon, C.; Lloyd-Lavery, A.; Mehta, Z.; Rothwell, P.M. Observational, longitudinal study of delirium in consecutive unselected acute medical admissions: Age-specific rates and associated factors, mortality and re-admission. BMJ Open 2015, 5, e007808. [Google Scholar] [CrossRef]
| Author, Year | Setting | Number of Patients, n | Delirium Assessment Tool | Post Operative (Yes/No) | Patient Population | Delirium Prevalence (%) | Age (Mean) | Women (%) |
|---|---|---|---|---|---|---|---|---|
| Brauchitsch et al., 2022 [27] | Hospital | 68 | Clinical Judgement | N | Primary, Metastasis | 13.2 | 59.1 | - |
| Budėnas et al., 2018 [44] | Hospital | 522 | CAM-ICU | Y | Primary, Metastasis | 4.2 | 57.23 | 64 |
| Bunevicius et al., 2011 [45] | Hospital | 38 | DSM-IV-TR | Y | Meningioma, Glioma, Pituitary Tumors, Brain Tumors | 11 | - | - |
| Chen et al., 2020 [28] | Hospital | 893 | CAM-ICU | Y | Meningioma, Adenoma, Glioma | 14.3 | - | - |
| Farriols Danés et al., 2016 [29] | Palliative Care Unit | 61 | DSM-IV-TR | N | Primary, Metastasis | 39.3 | - | - |
| Flanigan et al., 2018 [30] | Hospital | 554 | Clinical Judgement | Y | Glioma | 6.8 | 60.8 | 42.8 |
| French et al., 2021 [31] | Hospital | 500 | DSM-V | Y | Primary, Metastasis | 18.6 | - | - |
| Fu et al., 2024 [32] | Hospital | 28,340 | ICD-10-CM | Y | Meningioma, Glioma, Metastasis | 4.79 | 60.3 | 52.8 |
| Gofton et al., 2012 [33] | Hospital | 168 | Clinical Judgement | N | Primary, Metastasis | 27.4 | 60 | 42.9 |
| Gu et al., 2022 [34] | Hospital | 618 | CAM-ICU | Y | Benign, Malignant | 21.2 | 47 | 60.8 |
| He et al., 2021 [46] | Hospital | 29 | CAM-ICU | Y | Not specified | 10.3 | 48 | 50 |
| Huang et al., 2022 [43] | Hospital | 335 | CAM-ICU | Y | Glioma | 37.3 | - | 47.3 |
| Kim et al., 2020 [18] | Hospital | 969 | CAM-ICU | Y | Non-functioning pituitary tumors | 0.6 | 46.68 | 41.9 |
| Kim et al., 2020 (2) [18] | Hospital | 317 | CAM-ICU | Y | Functioning pituitary tumors | 0 | 44.06 | 53.6 |
| Li et al., 2023 [47] | Hospital | 130 | CAM-ICU | Y | Glioma, Meningioma, Others (cholesteatoma, epidermoid cyst, subependymoma, and metastasis) | 46.2 | 45 | 66 |
| Liu et al., 2023 [35] | Hospital | 348 | CAM-ICU | Y | Pituitary Adenoma | 10.34 | 48.3 | 52.2 |
| Matsuo et al., 2017 [48] | Hospital | 18 | CAM-ICU | N | Metastasis | 22 | - | - |
| Ramírez-Bermúdez et al., 2010 [20] | Hospital | 212 | DRS-98 | N | Not specified (Central Neoplasms) | 55.2 | - | - |
| Regli LKP et al., 2023 [37] | Hospital | 271 | Clinical Judgement | N | Glioblastoma | 6.6 | - | - |
| Sizoo et al., 2012 [38] | Hospital | 101 | Clinical Judgement | N | Glioma | 11.8 | - | 28 |
| Thisayakorn et al., 2022 [19] | Hospital | 42 | Clinical Judgement | N | High Grade Glioma | 0 | 58.6 | 47.6 |
| Tremont-Lukats et al., 2003 [39] | Hospital | 103 | Clinical Judgement | N | Metastasis | 51 | - | - |
| Wang et al., 2021 [40] | Hospital | 659 | CAM-ICU | Y | Benign and Malignant | 18.8 | 48 | 59.8 |
| Yamanaka et al., 2011 [41] | Palliative Care Unit | 55 | Clinical Judgement | N | Metastasis | 19 | 60.7 | . |
| Yuan et al., 2023 [49] | Hospital | 150 | Nu-DESC | Y | Meningioma, Glioma, Others | 28.7 | 55 | 54.7 |
| Yuan et al., 2024 [50] | Hospital | 133 | CAM-ICU | Y | Glioma | 31.6 | - | - |
| Zhang et al., 2024 [42] | Hospital | 213 | 4AT | Y | Adenoma | 29.58 | - | - |
| Zipser et al., 2019 [51] | Hospital | 111 | Delirium Observation Screening Scale (DOS) | Y | Not specified (Cerebral Neoplasm) | 29.7 | - | - |
| Averages (%) | 20 | 53 | 51 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tentor, Z.; Finnemore, A.; Miller, P.J.; Davis, J.; Juarez Martinez, E.; Lindvall, C.; Kimchi, E.Y.; Rhee, J.Y. Occurrence Rates of Delirium in Brain Tumor Patients: A Systematic Review and Meta-Analysis. Cancers 2025, 17, 1998. https://doi.org/10.3390/cancers17121998
Tentor Z, Finnemore A, Miller PJ, Davis J, Juarez Martinez E, Lindvall C, Kimchi EY, Rhee JY. Occurrence Rates of Delirium in Brain Tumor Patients: A Systematic Review and Meta-Analysis. Cancers. 2025; 17(12):1998. https://doi.org/10.3390/cancers17121998
Chicago/Turabian StyleTentor, Zachary, Alexander Finnemore, Paul J. Miller, Joshua Davis, Erika Juarez Martinez, Charlotta Lindvall, Eyal Y. Kimchi, and John Y. Rhee. 2025. "Occurrence Rates of Delirium in Brain Tumor Patients: A Systematic Review and Meta-Analysis" Cancers 17, no. 12: 1998. https://doi.org/10.3390/cancers17121998
APA StyleTentor, Z., Finnemore, A., Miller, P. J., Davis, J., Juarez Martinez, E., Lindvall, C., Kimchi, E. Y., & Rhee, J. Y. (2025). Occurrence Rates of Delirium in Brain Tumor Patients: A Systematic Review and Meta-Analysis. Cancers, 17(12), 1998. https://doi.org/10.3390/cancers17121998







