EUS-Guided Gallbladder Drainage of Inoperable Malignant Distal Biliary Obstruction by Lumen-Apposing Metal Stent: Systematic Review and Meta-Analysis
Simple Summary
Abstract
1. Introduction
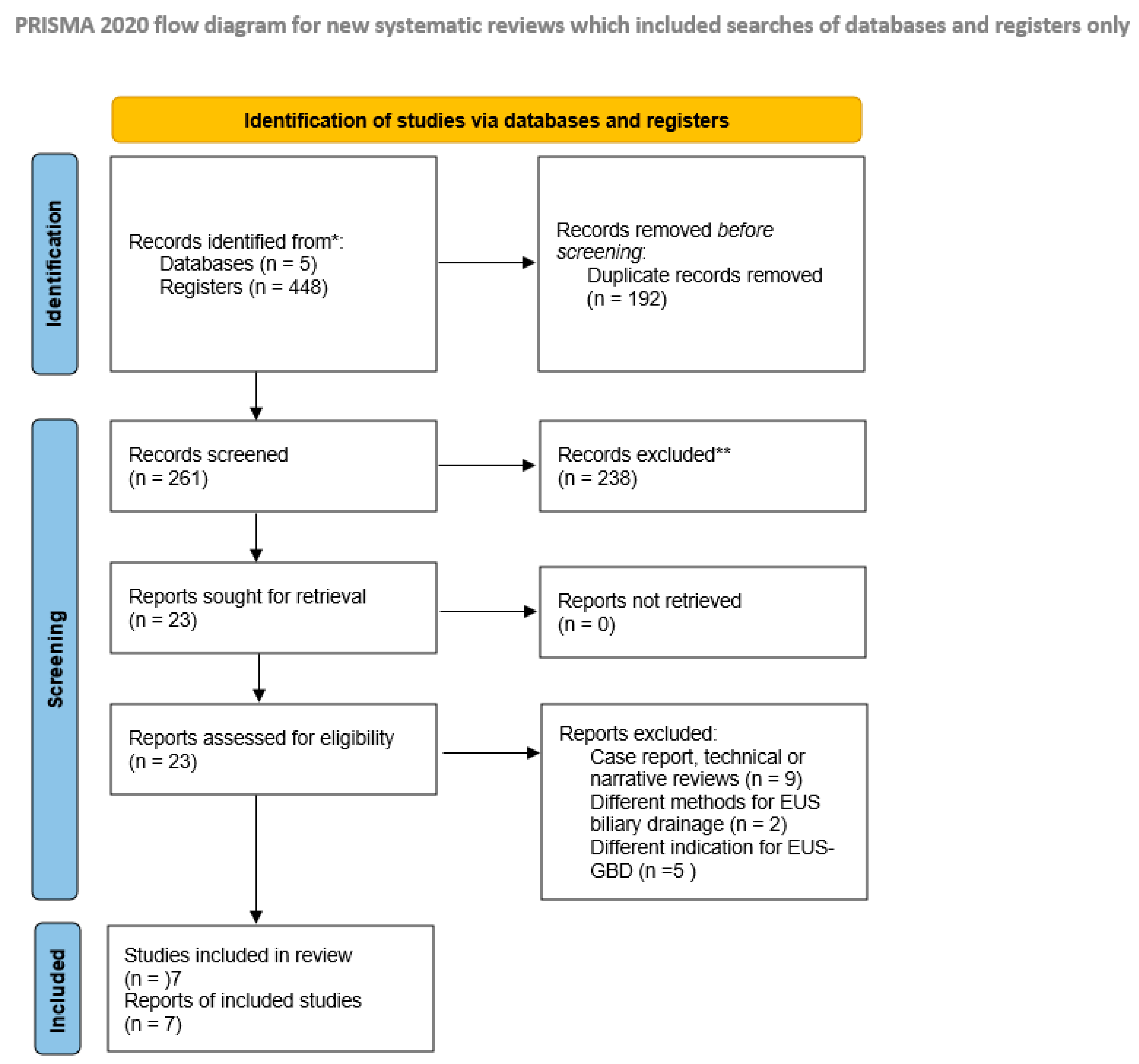
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Methods
2.3. Quality Appraisal
2.4. Data Collection
2.5. Definition of Outcomes
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Dumonceau, J.M.; Deprez, P.H.; Jenssen, C.; Iglesias-Garcia, J.; Larghi, A.; Vanbiervliet, G.; Aithal, G.P.; Arcidiacono, P.G.; Bastos, P.; Carrara, S.; et al. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline—Updated January 2017. Endoscopy 2017, 49, 695–714. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, T.; Itoi, T.; Sofuni, A.; Tonozuka, R.; Mukai, S. Endoscopic ultrasonography-guided rendezvous technique. Dig. Endosc. 2016, 28 (Suppl. S1), 96–101. [Google Scholar] [CrossRef]
- Khoury, T.; Sbeit, W.; Fumex, F.; Marasco, G.; Eusebi, L.H.; Fusaroli, P.; Chan, S.M.; Shahin, A.; Basheer, M.; Gincul, R.; et al. Endoscopic ultrasound- versus ERCP-guided primary drainage of inoperable malignant distal biliary obstruction: Systematic review and meta-analysis of randomized controlled trials. Endoscopy 2024, 56, 955–963. [Google Scholar] [CrossRef]
- Takahara, N.; Nakai, Y.; Noguchi, K.; Suzuki, T.; Sato, T.; Hakuta, R.; Ishigaki, K.; Saito, T.; Hamada, T.; Fujishiro, M. Endoscopic ultrasound-guided hepaticogastrostomy and endoscopic retrograde cholangiopancreatography-guided biliary drainage for distal malignant biliary obstruction due to pancreatic cancer with asymptomatic duodenal invasion: A retrospective, single-center study in Japan. Clin. Endosc. 2025, 58, 134–143. [Google Scholar] [CrossRef]
- Binda, C.; Anderloni, A.; Forti, E.; Fusaroli, P.; Macchiarelli, R.; Manno, M.; Fugazza, A.; Redaelli, A.; Aragona, G.; Lovera, M.; et al. EUS-Guided Gallbladder Drainage Using a Lumen-Apposing Metal Stent for Acute Cholecystitis: Results of a Nationwide Study with Long-Term Follow-Up. Diagnostics 2024, 14, 413. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Cotton, P.B.; Eisen, G.M.; Aabakken, L.; Baron, T.H.; Hutter, M.M.; Jacobson, B.C.; Mergener, K.; Nemcek, A., Jr.; Petersen, B.T.; Petrini, J.L.; et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 2010, 71, 446–454. [Google Scholar] [CrossRef]
- Binda, C.; Anderloni, A.; Fugazza, A.; Amato, A.; de Nucci, G.; Redaelli, A.; Di Mitri, R.; Cugia, L.; Pollino, V.; Macchiarelli, R.; et al. EUS-guided gallbladder drainage using a lumen-apposing metal stent as rescue treatment for malignant distal biliary obstruction: A large multicenter experience. Gastrointest. Endosc. 2023, 98, 765–773. [Google Scholar] [CrossRef]
- Chang, J.I.; Dong, E.; Kwok, K.K. Endoscopic ultrasound-guided transmural gallbladder drainage in ma-lignant obstruction using a novel lumen-apposing stent: A case series (with video). Endosc. Int. Open 2019, 7, E655–E661. [Google Scholar] [CrossRef]
- Chin, J.Y.; Seleq, S.; Weilert, F. Safety and outcomes of endoscopic ultrasound-guided drainage for ma-lignant biliary obstruction using cautery-enabled lumen-apposing metal stent. Endosc. Int. Open 2020, 8, E1633–E1638. [Google Scholar] [CrossRef] [PubMed]
- Debourdeau, A.; Daniel, J.; Caillo, L.; Assenat, E.; Bertrand, M.; Bardol, T.; Souche, F.R.; Pouderoux, P.; Gerard, R.; Lorenzo, D.; et al. Effectiveness of endoscopic ultrasound (EUS)-guided choledochoduodenostomy vs. EUS-guided gallbladder drainage for jaundice in patients with malignant distal biliary obstruction after failed endoscopic retrograde cholangiopancreatography: Retrospective, multicenter study (GALLBLADEUS Study). Dig. Endosc. 2025, 37, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Issa, D.; Irani, S.; Law, R.; Shah, S.; Bhalla, S.; Mahadev, S.; Hajifathalian, K.; Sampath, K.; Mukewar, S.; Carr-Locke, D.L.; et al. Endoscopic ultrasound-guided gallbladder drainage as a rescue therapy for unresectable malignant biliary obstruction: A multicenter experience. Endoscopy 2021, 53, 827–831. [Google Scholar] [CrossRef]
- Lambin, T.B.J.; Privat, J. Efficacy and Safety of Eus-Guided Transmural Gallbladder Drainage in Malignant Biliary Obstruction Using an Electrocau-Tery-Enhanced Lumen Apposing Metal Stent: A French Multicenter Study. Multi-Center, Retrospective. Endoscopy 2021, 53, OP94. [Google Scholar]
- Mangiavillano, B.; Moon, J.H.; Facciorusso, A.; Vargas-Madrigal, J.; Di Matteo, F.; Rizzatti, G.; De Luca, L.; Forti, E.; Mutignani, M.; Al-Lehibi, A.; et al. Endoscopic ultrasound-guided gallbladder drainage as a first approach for jaundice palliation in unresectable malignant distal biliary obstruction: Prospective study. Dig. Endosc. 2024, 36, 351–358. [Google Scholar] [CrossRef]
- Kamal, F.; Khan, M.A.; Lee-Smith, W.; Sharma, S.; Acharya, A.; Farooq, U.; Aziz, M.; Kouanda, A.; Dai, S.C.; Munroe, C.A.; et al. Efficacy and safety of EUS-guided gallbladder drainage for rescue treatment of malignant biliary obstruction: A systematic review and meta-analysis. Endosc. Ultra-Sound 2023, 12, 8–15. [Google Scholar] [CrossRef]
- Rimbas, M.; Crino, S.F.; Rizzatti, G.; Larghi, A. Endoscopic ultrasound-guided gallbladder drainage: A backdoor for biliary decompression? Endoscopy 2021, 53, 873. [Google Scholar] [CrossRef]
- Tarnasky, P.R.; England, R.E.; Lail, L.M.; Pappas, T.N.; Cotton, P.B. Cystic duct patency in malignant ob-structive jaundice. An ERCP-based study relevant to the role of laparoscopic cholecystojejunostomy. Ann. Surg. 1995, 221, 265–271. [Google Scholar] [CrossRef]
- Sobani, Z.A.; Ling, C.; Rustagi, T. Endoscopic Ultrasound-Guided Gallbladder Drainage. Dig. Dis. Sci. 2021, 66, 2154–2161. [Google Scholar] [CrossRef]
- Mangiavillano, B.; Lakhtakia, S.; Samanta, J.; Auriemma, F.; Vargas-Madrigal, J.; Arcidiacono, P.G.; Barbera, C.; Ashhab, H.; Song, T.J.; Pham, K.D.; et al. Lumen-apposing metal stents for the treatment of pancreatic and peripancreatic fluid collections and bleeding risk: A propensity matched study. Endoscopy 2024, 56, 249–257. [Google Scholar] [CrossRef]
- van der Merwe, S.W.; van Wanrooij, R.L.J.; Bronswijk, M.; Everett, S.; Lakhtakia, S.; Rimbas, M.; Hucl, T.; Kunda, R.; Badaoui, A.; Law, R.; et al. Therapeutic endoscopic ultrasound: Eu-ropean Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2022, 54, 185–205. [Google Scholar] [CrossRef] [PubMed]
- Lisotti, A.; Linguerri, R.; Bacchilega, I.; Cominardi, A.; Marocchi, G.; Fusaroli, P. EUS-guided gallbladder drainage in high-risk surgical patients with acute cholecystitis-procedure outcomes and evaluation of mortality predictors. Surg. Endosc. 2022, 36, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Moreno, B.; Lopez-Roldan, G.; Martinez-Sempere, J.; de-Madaria, E.; Jover, R.; Aparicio, J.R. Long-term results after EUS gallbladder drainage in high-surgical-risk patients with acute cholecystitis: A 3-year follow-up registry. Endosc. Int. Open 2023, 11, E1063–E1068. [Google Scholar] [CrossRef]
- Baron, T.H.; Jorge, I.; Husnain, A.; Benias, P.C.; Reames, B.N.; Bhanushali, A.; Docimo, S., Jr.; Bloom, M.; Salem, R.; Murphy, P.; et al. Comprehensive Review of the Management of Patients with Acute Cholecystitis Who Are Ineligible for Surgery. Ann. Surg. 2025, 10, 1097. [Google Scholar] [CrossRef]
- Arayakarnkul, S.; Blomker, J.; Seid, A.S.; Afraz, I.; Theis-Mahon, N.; Wilson, N.; Karna, R.; Bilal, M. Outcomes of interval cholecystectomy after EUS-guided gallbladder drainage: A systematic review and meta-analysis. Gastrointest. Endosc. 2025, in press. [CrossRef]
- David, Y.; Kakked, G.; Confer, B.; Shah, R.; Khara, H.; Diehl, D.L.; Krafft, M.R.; Shah-Khan, S.M.; Nasr, J.Y.; Benias, P.; et al. US multicenter outcomes of endoscopic ultrasound-guided gallbladder drainage with lumen-apposing metal stents for acute cholecystitis. Endosc. Int. Open 2025, 13, a24955542. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nakai, Y.; Sato, T.; Hakuta, R.; Ishigaki, K.; Saito, K.; Saito, T.; Takahara, N.; Hamada, T.; Mizuno, S.; Kogure, H.; et al. Long-term outcomes of a long, partially covered metal stent for EUS-guided hepaticogastrostomy in patients with malignant biliary obstruction (with video). Gastrointest. Endosc. 2020, 92, 623–631.e1. [Google Scholar] [CrossRef]
- Marasco, M.; Signoretti, M.; Esposito, G.; Crinò, S.F.; Panzuto, F.; Galasso, D. Endoscopic ultrasonography guided gallbladder drainage: “how and when”. Expert. Rev. Gastroenterol. Hepatol. 2025, 19, 399–412. [Google Scholar] [CrossRef]
- Dell’Anna, G.; Nunziata, R.; Delogu, C.; Porta, P.; Grassini, M.V.; Dhar, J.; Barà, R.; Bencardino, S.; Fanizza, J.; Mandarino, F.V.; et al. The Role of Therapeutic Endoscopic Ultrasound in Management of Malignant Double Obstruction (Biliary and Gastric Outlet): A Comprehensive Review with Clinical Scenarios. J. Clin. Med. 2024, 13, 7731. [Google Scholar] [CrossRef]
- Hayat, M.; Xiao, Y.; Arain, M.A.; Yang, D. Endoscopic Gallbladder Drainage EUS LAMS vs. ERCP Trans-Papillary Drainage. Curr. Gastroenterol. Rep. 2025, 27, 5. [Google Scholar] [CrossRef]
| Variables | Binda et al. [9] | Debourdeau et al. [12] | Issa et al. [13] | Mangiavillano et al. [15] | Chang et al. [10] | Lambin et al. [14] | Chin et al. [11] |
|---|---|---|---|---|---|---|---|
| Journal | Gastrointestinal endoscopy | Digestive endoscopy | Endoscopy | Digestive endoscopy | Endoscopy international open | Abstract | Endoscopy international open |
| Year published | 2023 | 2024 | 2021 | 2024 | 2018 | 2021 | 2020 |
| Design of study | Retrospective | Retrospective | Retrospective | Prospective | Retrospective | Retrospective | Retrospective |
| Cause of MDBO | Pancreatic cancer Cholangiocarcinoma Ampullary cancer Others | Pancreatic cancer Cholangiocarcinoma Ampullary cancer Others | NR | Pancreatic cancer Cholangiocarcinoma Ampullary cancer | Pancreatic cancer | Pancreatic cancer Cholangiocarcinoma Others | NR |
| Patients, n | 48 | 41 | 26 | 37 | 9 | 28 | 4 |
| Type of LAMS | Hot Axios | Hot Axios | Hot Axios | Hot Spaxus | Hot Axios | Hot Axios | Hot Axios |
| Route of drainage | Trans-gastric (58.3%) Trans-duodenal (41.7%) | Trans-gastric (100%) | Trans-gastric (46%) Trans-duodenal (54%) | Trans-gastric (40.6%) Trans-duodenal (59.4%) | Trans-gastric (44.4%) Trans-duodenal (55.6%) | NR | Trans-duodenal (100%) |
| Follow-up (median) | 122 | 170 | 990 | 120 | 130.7 | 108 | 237 |
| Reference | Selection | Comparability | Outcome | Overall |
|---|---|---|---|---|
| Binda et al. [9] | Medium | Not assessable | High | Medium |
| Debourdeau et al. [12] | High | Not assessable | High | Medium |
| Issa et al. [13] | High | Not assessable | High | Medium |
| Mangiavillano et al. [15] | High | Not assessable | High | Medium |
| Chang et al. [10] | Medium | Not assessable | High | Medium |
| Lambin t et al. [14] | Medium | Not assessable | Medium | Low |
| Chin et al. [11] | Medium | Not assessable | Medium | Low |
| Reference | Selection Bias | Performance Bias | Detection Bias | Attribution Bias |
|---|---|---|---|---|
| Binda et al. [9] | Moderate | Moderate | Moderate | Moderate |
| Debourdeau et al. [12] | Moderate | High | Moderate | Moderate |
| Issa et al. [13] | Moderate | Moderate | Moderate | Moderate |
| Mangiavillano et al. [15] | Low | Low | Low | Moderate |
| Chang et al. [10] | High | High | High | High |
| Lambin t et al. [14] | Moderate | Moderate | Low | Moderate |
| Chin et al. [11] | Moderate | Moderate | Low | Moderate |
| No. Studies (Population) | Pooled Estimates [95% CI] Random Effect Model | Heterogeneity (I2) | Egger’s Test (p Value) | |
|---|---|---|---|---|
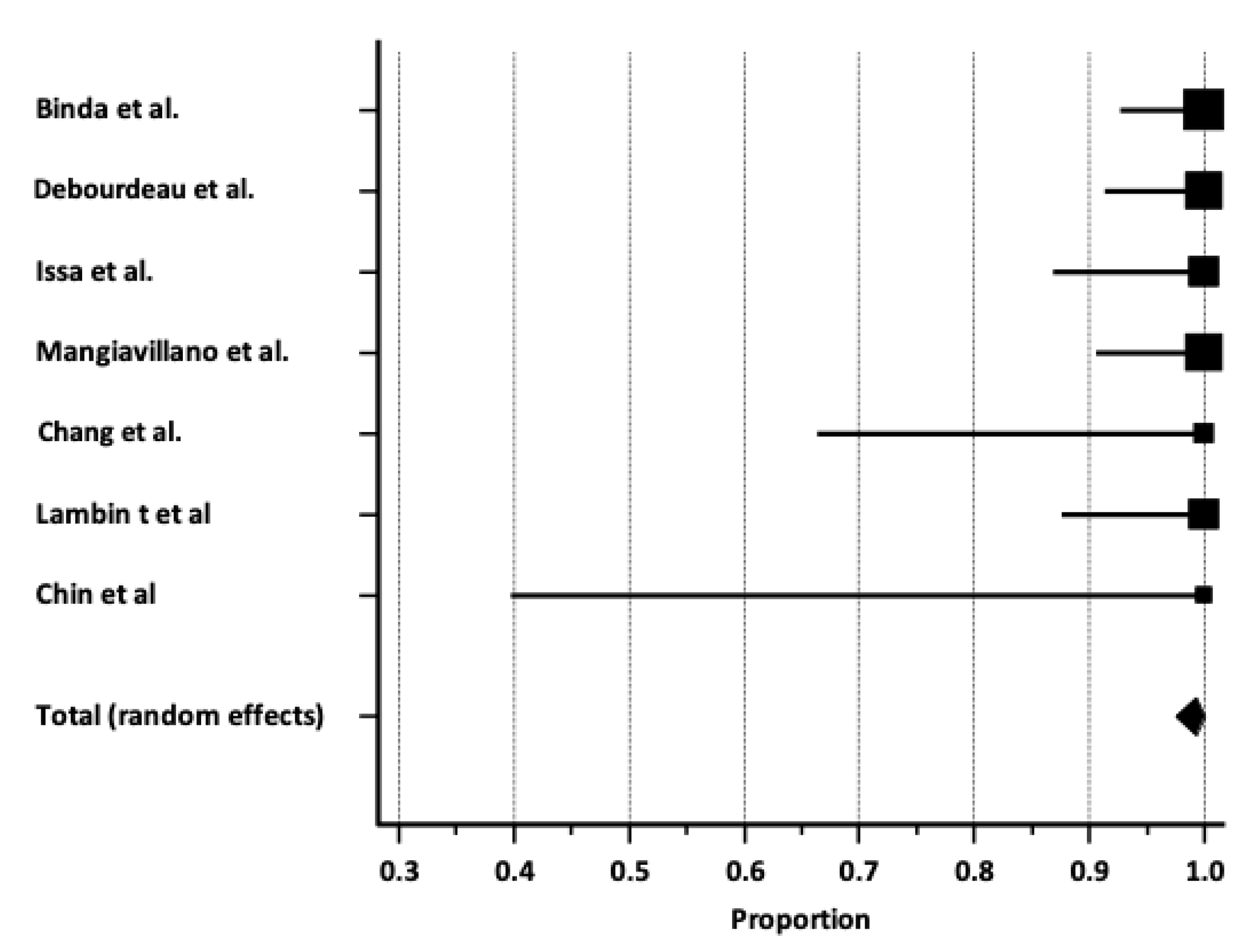
| Technical success rate | 7 studies (193 patients) | 99.2% [97.5–100%] | 0.0% | <0.001 |
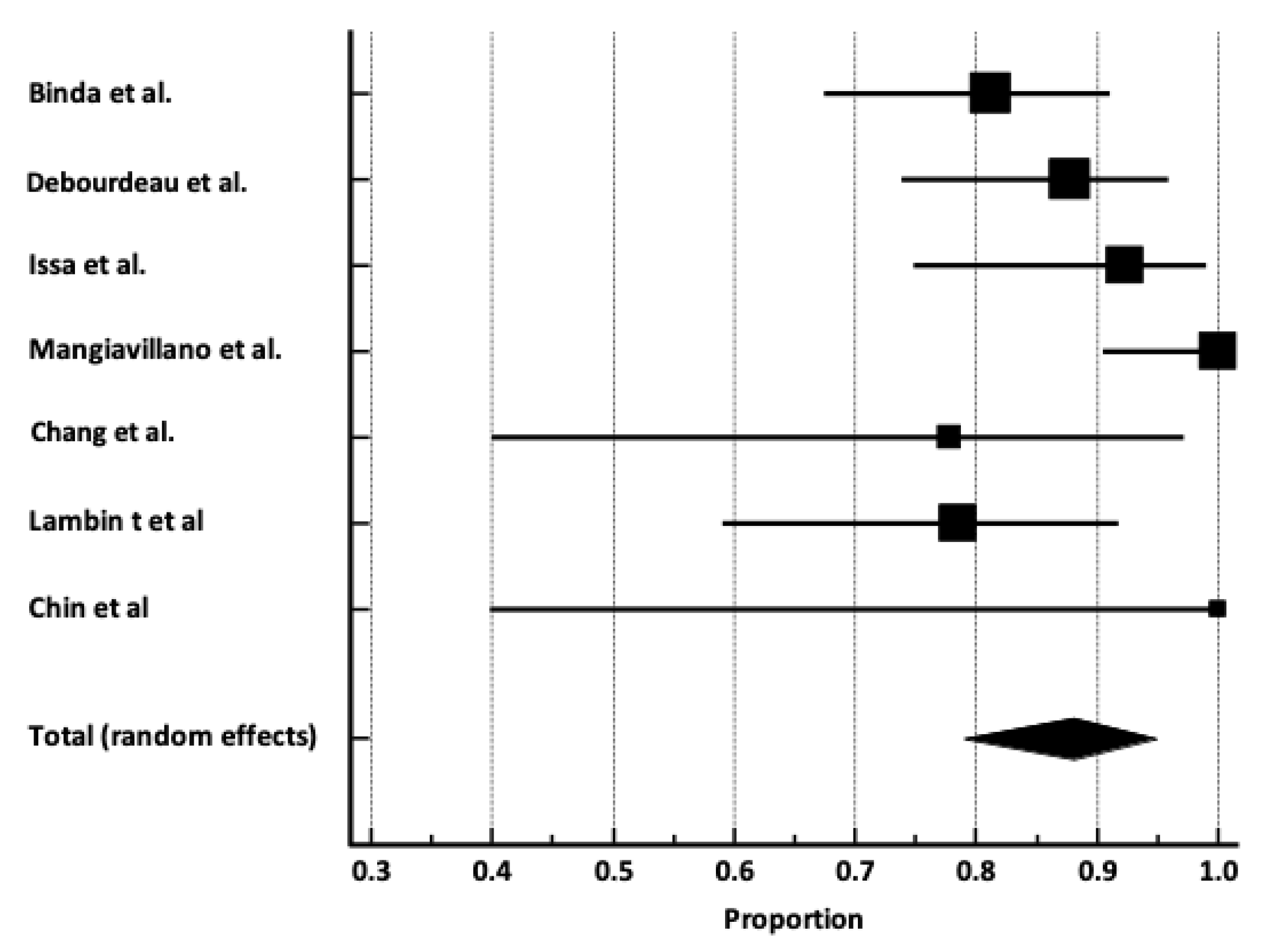
| Clinical success rate | 7 studies (193 patients) | 88.1% [78.9–94.9%] | 65.2% | 0.95 |
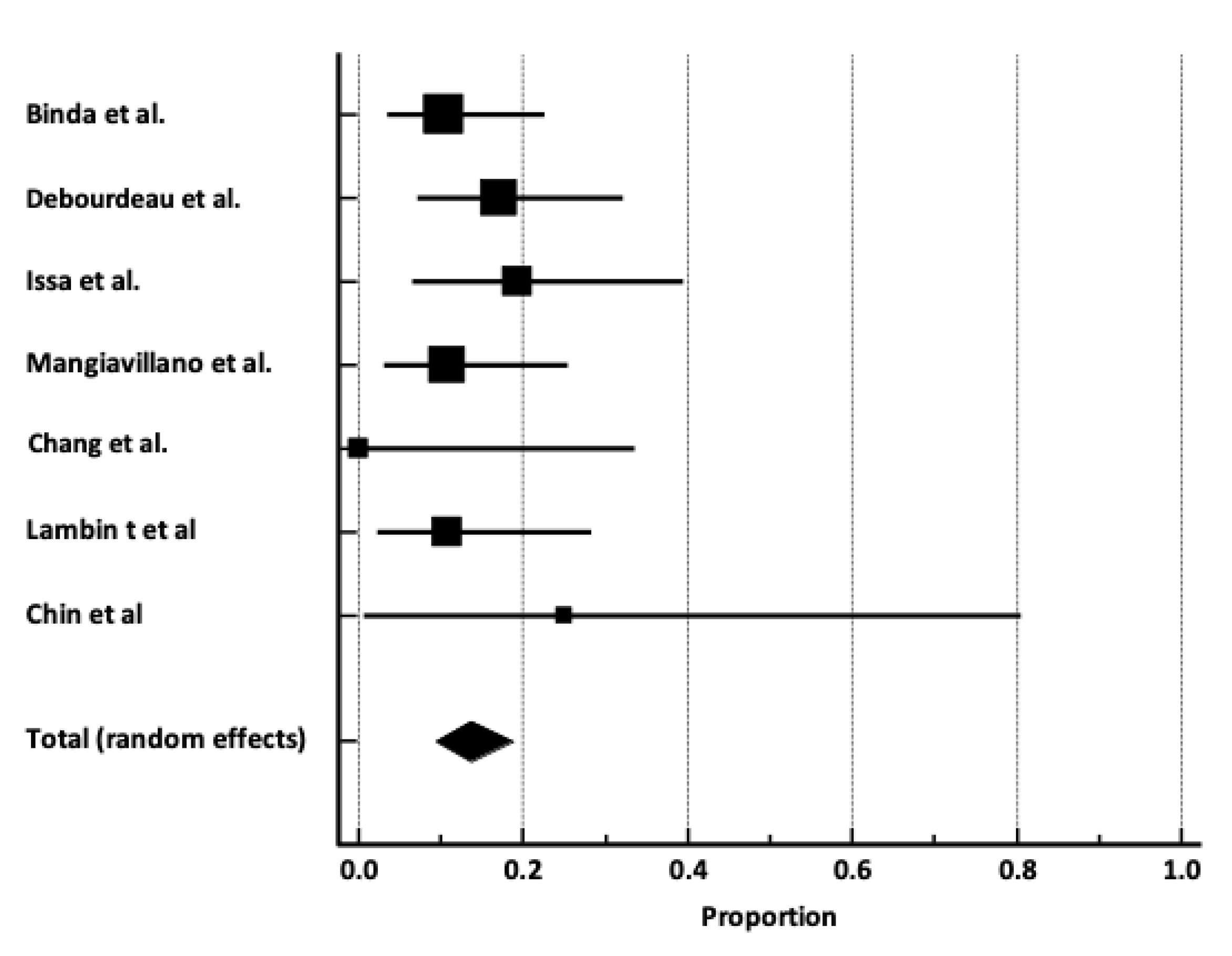
| Adverse event rate | 7 studies (193 patients) | 13.7% [9.3–18.8%] | 0.0% | 0.97 |
| AEs timing | ||||
| • Early AEs rate | 7 studies (193 patients) | 4.5% [2.0–7.9%] | 5.1% | 0.48 |
| • Delayed AEs rate | 7 studies (193 patients) | 9.5% [5.7–14.3%] | 9.2% | 0.42 |
| AEs severity | ||||
| • Mild AEs rate | 7 studies (193 patients) | 4.2% [0.4–11.8%] | 73.8% | 0.67 |
| • Moderate AEs rate | 7 studies (193 patients) | 7.6% [4.3–11.6%] | 0.0% | 0.32 |
| • Severe AEs rate | 7 studies (193 patients) | 1.1% [0.1–3.1%] | 0.0% | 0.16 |
| Random Effect Model | No. Studies (Population) | Pooled Estimates [95% Confidence Interval] | Heterogeneity (I2) |
|---|---|---|---|
| Study population | |||
| Study population < 35 patients | 4 studies (67 patients) | 84.3% [74.8–91.8%] | 1.9% |
| Study population ≥ 35 patients | 3 studies (126 patients) | 91.0% [75.1–99.2%] | 84.2% |
| Study design | |||
| Retrospective design | 6 studies (156 patients) | 83.9% [77.9–89.2%] | 0.0% |
| Prospective design | 1 study (37 patients) | 100% [90.5–100%%] | N/A |
| Publication type | |||
| Full-text article | 6 studies (165 patients) | 86.5% [79.1–90.3%] | 3.2% |
| Study period | |||
| Before 2023 | 4 studies (67 patients) | 84.3% [74.8–91.8%] | 1.9% |
| 2023–2024 | 3 studies (126 patients) | 91.0% [75.1–99.2%] | 84.2% |
| LAMS type | |||
| Hot-Axios stent | 6 studies (156 patients) | 83.9% [77.9–89.2%] | 0.0% |
| Hot-Spaxus stent | 1 study (37 patients) | 100% [90.5–100%%] | N/A |
| LAMS diameter | |||
| Large (≥15 mm) LAMS | 3 studies (76 patients) | 87.1% [78.8–93.5%] | 0.0% |
| Small (<15 mm) LAMS | 3 studies (89 patients) | 93.3% [72.4–99.9%] | 83.4% |
| Gallbladder drainage intention | |||
| After ERCP failure | 5 studies (147 patients) | 84.4% [78.3–89.7%] | 0.0% |
| EUS-GBD primary drainage | 2 studies (46 patients) | 92.3% [57.5–97.8%] | 83.7% |
| No. Studies (Population) | Incidence of AEs [95% CI] Random Effect Model | |
|---|---|---|
| Study population | ||
| Study population < 35 patients | 4 studies (67 patients) | 14.0% [6.2–24.3%] |
| Study population ≥ 35 patients | 3 studies (126 patients) | 13.4% [8.1–19.8%] |
| LAMS type | ||
| Hot-Axios stent | 6 studies (156 patients) | 14.1% [9.2–19.9%] |
| Hot-Spaxus stent | 1 study (37 patients) | 10.8% [3.0–18.8%%] |
| LAMS diameter | ||
| Large (≥15 mm) LAMS | 3 studies (76 patients) | 15.2% [6.5–26.6%] |
| Small (<15 mm) LAMS | 3 studies (89 patients) | 12.3% [6.4–19.7%] |
| Gallbladder drainage intention | ||
| After ERCP failure | 5 studies (147 patients) | 15.2% [9.9–21.3%] |
| EUS-GBD primary drainage | 2 studies (46 patients) | 9.0% [2.1–20.1%] |
| Reference | Number of AEs | Type of AEs | Severity |
|---|---|---|---|
| Binda et al. [9] | |||
| Early (intraprocedural) | 3 | Bleeding (2), dislodgment (1) | Mild–moderate |
| Late (>15 days) | 2 | Buried stent (1), occlusion (1) | Moderate |
| Debourdeau et al. [12] | |||
| Early (within 24 h) | 4 | Bleeding (2), dislodgment (1), bacteremia (1) | Mild–severe |
| Late (after 24 h) | 3 | Bleeding (1), stent obstruction (2) | Moderate |
| Issa et al. [13] | |||
| Early (within 24 h) | 0 | - | - |
| Late (after 24 h) | 5 | Food impaction (3), bleeding (2) | Moderate |
| Mangiavillano et al. [15] | |||
| Early (within 48 h) | 1 | Bleeding (1) | Moderate |
| Late (after 48 h) | 3 | Occlusion (1), cystic duct occlusion by tumor (2) | Moderate |
| Chang et al. [10] | NR | NR | NR |
| Early | |||
| Late | |||
| Lambin T et al. [14] | |||
| Early (periprocedural) | 0 | - | - |
| Late (within 30 days) | 3 | Obstruction (1), cholangitis (1), septic shock (1) | Moderate |
| Chin et al. [11] | |||
| Early (<30 days) | 0 | - | - |
| Late (>30 days) | 1 | Migration (1) | Moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khoury, T.; Farraj, M.; Sbeit, W.; Fusaroli, P.; Barbara, G.; Binda, C.; Fabbri, C.; Basheer, M.; Leblanc, S.; Fumex, F.; et al. EUS-Guided Gallbladder Drainage of Inoperable Malignant Distal Biliary Obstruction by Lumen-Apposing Metal Stent: Systematic Review and Meta-Analysis. Cancers 2025, 17, 1983. https://doi.org/10.3390/cancers17121983
Khoury T, Farraj M, Sbeit W, Fusaroli P, Barbara G, Binda C, Fabbri C, Basheer M, Leblanc S, Fumex F, et al. EUS-Guided Gallbladder Drainage of Inoperable Malignant Distal Biliary Obstruction by Lumen-Apposing Metal Stent: Systematic Review and Meta-Analysis. Cancers. 2025; 17(12):1983. https://doi.org/10.3390/cancers17121983
Chicago/Turabian StyleKhoury, Tawfik, Moaad Farraj, Wisam Sbeit, Pietro Fusaroli, Giovanni Barbara, Cecilia Binda, Carlo Fabbri, Maamoun Basheer, Sarah Leblanc, Fabien Fumex, and et al. 2025. "EUS-Guided Gallbladder Drainage of Inoperable Malignant Distal Biliary Obstruction by Lumen-Apposing Metal Stent: Systematic Review and Meta-Analysis" Cancers 17, no. 12: 1983. https://doi.org/10.3390/cancers17121983
APA StyleKhoury, T., Farraj, M., Sbeit, W., Fusaroli, P., Barbara, G., Binda, C., Fabbri, C., Basheer, M., Leblanc, S., Fumex, F., Gincul, R., Teoh, A. Y. B., Jacques, J., Napoléon, B., & Lisotti, A. (2025). EUS-Guided Gallbladder Drainage of Inoperable Malignant Distal Biliary Obstruction by Lumen-Apposing Metal Stent: Systematic Review and Meta-Analysis. Cancers, 17(12), 1983. https://doi.org/10.3390/cancers17121983