The Association Between Clinical Outcome and Expression of DNMT1, 3A, and 3B in Locally Advanced Laryngeal Carcinomas Treated by Definitive Radiotherapy
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Treatment and Follow-Up
2.3. Analysis of Publicly Available Data
2.4. Immunohistochemistry and Scoring
2.5. Statistical Analysis
3. Results
3.1. Analysis on Publicly Available Data
3.2. Demographic and Clinical Data
3.3. Locoregional Recurrence
3.4. Disease-Specific Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ebrahimi, H.; Aryan, Z.; Moghaddam, S.S.; Bisignano, C.; Rezaei, S.; Pishgar, F.; Force, L.M.; Abolhassani, H.; Abu-Gharbieh, E.; Advani, S.M.; et al. Global, regional, and national burden of respiratory tracancers and associated risk factors from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Respir Med. 2021, 9, 1030–1049. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Wang, H.; Zhao, Q.; Zhang, Y.; Zheng, Z.; Liu, S.; Liu, Z.; Meng, L.; Xin, Y.; Jiang, X. Evaluation of Risk Factors for Laryngeal Squamous Cell Carcinoma: A Single-Center Retrospective Study. Front. Oncol. 2021, 11, 606010. [Google Scholar] [CrossRef] [PubMed]
- Forastiere, A.A.; Ismaila, N.; Lewin, J.S.; Nathan, C.A.; Adelstein, D.J.; Eisbruch, A.; Fass, G.; Fisher, S.G.; Laurie, S.A.; Le, Q.-T.; et al. Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2018, 36, 1143–1169. [Google Scholar] [CrossRef]
- Brandstorp-Boesen, J.; Falk, R.S.; Boysen, M.; Brøndbo, K. Impact of stage, management and recurrence on survival rates in laryngeal cancer. PLoS ONE 2017, 12, e0179371. [Google Scholar] [CrossRef]
- Rajgor, A.D.; Cowley, J.; Gillespie, C.; Lee, C.W.; O’Hara, J.; Iqbal, M.S.; Hamilton, D.W. Outcomes of the modern management approach for locally advanced (T3-T4) laryngeal cancer: A retrospective cohort study. J. Laryngol. Otol. 2024, 138, 1154–1160. [Google Scholar] [CrossRef]
- Elbers, J.B.W.; Veldhuis, L.I.; Bhairosing, P.A.; Smeele, L.E.; Jóźwiak, K.; Brekel, M.W.M.v.D.; Verheij, M.; Al-Mamgani, A.; Zuur, C.L. Salvage surgery for advanced stage head and neck squamous cell carcinoma following radiotherapy or chemoradiation. Eur. Arch. Oto-Rhino-Laryngol. 2019, 276, 647–655. [Google Scholar] [CrossRef]
- Hermann, R.M.; Christiansen, H.; Rödel, R.M. Lymph node positive head and neck carcinoma after curative radiochemotherapy: A long lasting debate on elective post-therapeutic neck dissections comes to a conclusion. Cancer/Radiotherapie 2013, 17, 323–331. [Google Scholar] [CrossRef]
- Lavertu, P.; Bonafede, J.P.; Adelstein, D.J.; Saxton, J.P.; Strome, M.; Wanamaker, J.R.; Eliachar, I.; Wood, B.G. Comparison of surgical complications after organ-preservation therapy in patients with stage III or IV squamous cell head and neck cancer. Arch. Otolaryngol. Head. Neck Surg. 1998, 124, 401–406. [Google Scholar] [CrossRef]
- Schwartz, S.R.; Yueh, B.; Maynard, C.; Daley, J.; Henderson, W.; Khuri, S.F. Predictors of wound complications after laryngectomy: A study of over 2000 patients. Otolaryngol. Neck Surg. Off. J. Am. Acad. Otolaryngol. Neck Surg. 2004, 131, 61–68. [Google Scholar] [CrossRef]
- Chen, C.; Chen, W.; Wang, W.; Lu, C.; Lin, P.; Lee, K.; Chen, M. Role of DNA methyltransferase 1 in pharyngeal cancer related to treatment resistance. Head Neck 2011, 33, 1132–1143. [Google Scholar] [CrossRef]
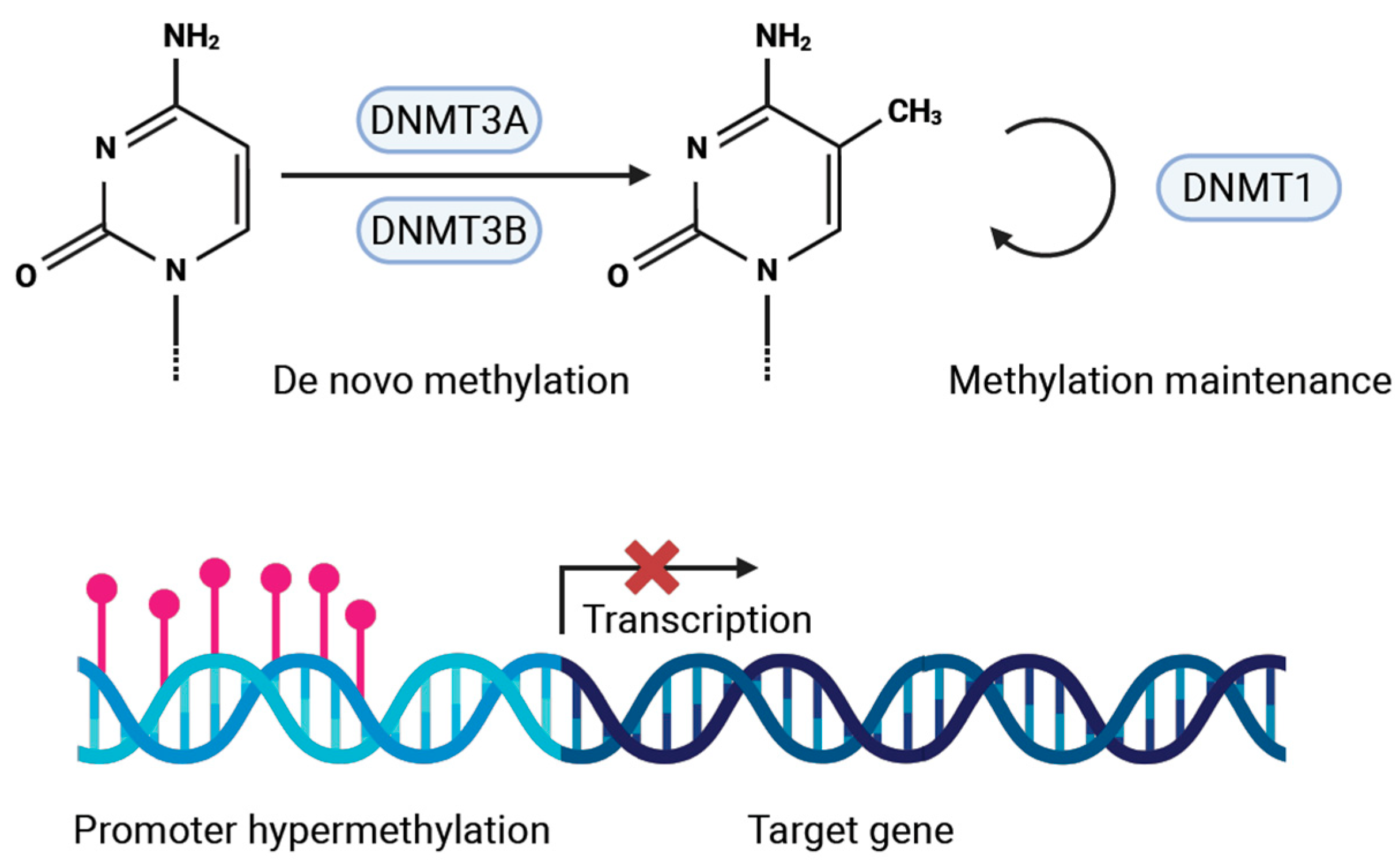
- Herman, J.G.; Baylin, S.B. Gene silencing in cancer in association with promoter hypermethylation. N. Engl. J. Med. 2003, 349, 2042–2054. [Google Scholar] [CrossRef]
- Robertson, K.D. DNA methylation and chromatin—Unraveling the tangled web. Oncogene 2002, 21, 5361–5379. [Google Scholar] [CrossRef]
- Hodge, D.R.; Peng, B.; Cherry, J.C.; Hurt, E.M.; Fox, S.D.; Kelley, J.A.; Munroe, D.J.; Farrar, W.L. Interleukin 6 supports the maintenance of p53 tumor suppressor gene promoter methylation. Cancer Res. 2005, 65, 4673–4682. [Google Scholar] [CrossRef]
- Momparler, R.L.; Bovenzi, V. DNA methylation and cancer. J. Cell Physiol. 2000, 183, 145–154. [Google Scholar] [CrossRef]
- Gujar, H.; Weisenberger, D.J.; Liang, G. The roles of human DNA methyltransferases and their isoforms in shaping the epigenome. Genes 2019, 10, 172. [Google Scholar] [CrossRef]
- Abdelfatah, E.; Kerner, Z.; Nanda, N.; Ahuja, N. Epigenetic therapy in gastrointestinal cancer: The right combination. Ther. Adv. Gastroenterol. 2016, 9, 560–579. [Google Scholar] [CrossRef]
- Esteller, M. Epigenetics in cancer. N. Engl. J. Med. 2008, 358, 1148–1159. [Google Scholar] [CrossRef]
- Zhang, W.; Xu, J. DNA methyltransferases and their roles in tumorigenesis. Biomark. Res. 2017, 5, 1. [Google Scholar] [CrossRef]
- Mishra, M.V.; Bisht, K.S.; Sun, L.; Muldoon-Jacobs, K.; Awwad, R.; Kaushal, A.; Nguyen, P.; Huang, L.; Pennington, J.D.; Markovina, S.; et al. DNMT1 as a molecular target in a multimodality-resistant phenotype in tumor cells. Mol. Cancer Res. 2008, 6, 243–249. [Google Scholar] [CrossRef]
- de Bruin, L.B.; Clausen, M.J.A.M.; Slagter-Menkema, L.; de Bock, G.H.; Langendijk, J.A.; van der Vegt, B.; van der Laan, B.F.A.M.; Schuuring, E. High DNMT1 Is Associated With Worse Local Control in Early-Stage Laryngeal Squamous Cell Carcinoma. Laryngoscope 2022, 132, 801–805. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, X.; Liu, L.; Mims, J.; Punska, E.C.; Williams, K.E.; Zhao, W.; Arcaro, K.F.; Tsang, A.W.; Zhou, X.; Furdui, C.M. Analysis of DNA methylation and gene expression in radiation-resistant head and neck tumors. Epigenetics 2015, 10, 545–561. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Wang, Y.; Tan, L.; Fu, X. The pivotal role of DNA methylation in the radio-sensitivity of tumor radiotherapy. Cancer Med. 2018, 7, 3812–3819. [Google Scholar] [CrossRef] [PubMed]
- Chi, H.-C.; Tsai, C.-Y.; Tsai, M.-M.; Lin, K.-H. Impact of DNA and RNA Methylation on Radiobiology and Cancer Progression. Int. J. Mol. Sci. 2018, 19, 555. [Google Scholar] [CrossRef]
- Bovenkamp, K.v.D.; van der Vegt, B.; Halmos, G.B.; Slagter-Menkema, L.; Langendijk, J.A.; van Dijk, B.A.C.; Schuuring, E.; van der Laan, B.F.A.M. The relation between hypoxia and proliferation biomarkers with radiosensitivity in locally advanced laryngeal cancer. Eur. Arch. Oto-Rhino-Laryngol. 2023, 280, 3801–3809. [Google Scholar] [CrossRef]
- Dutch Head and Neck Society (NWHHT) Guideline: Follow-up After Treatment of Head and Neck Tumours. 2014. Richtlijnendatabase (In Dutch). Available online: https://richtlijnendatabase.nl/richtlijn/hoofd-halstumoren_sept_2023/startpagina_-_hoofd-halstumoren_2023.html (accessed on 7 April 2023).
- Adhikari, B.R.; Uehara, O.; Matsuoka, H.; Takai, R.; Harada, F.; Utsunomiya, M.; Chujo, T.; Morikawa, T.; Shakya, M.; Yoshida, K.; et al. Immunohistochemical evaluation of Klotho and DNA methyltransferase 3a in oral squamous cell carcinomas. Med. Mol. Morphol. 2017, 50, 155–160. [Google Scholar] [CrossRef]
- Daniel, F.I.; Rivero, E.R.C.; Modolo, F.; Lopes, T.G.; Salum, F.G. Immunohistochemical expression of DNA methyltransferases 1, 3a and 3b in oral leukoplakias and squamous cell carcinomas. Arch. Oral. Biol. 2010, 55, 1024–1030. [Google Scholar] [CrossRef]
- Flausino, C.S.; Daniel, F.I.; Modolo, F. DNA methylation in oral squamous cell carcinoma: From its role in carcinogenesis to potential inhibitor drugs. Crit. Rev. Oncol. Hematol. 2021, 164, 103399. [Google Scholar] [CrossRef]
- Choi, M.S.; Shim, Y.-H.; Hwa, J.Y.; Lee, S.K.; Ro, J.Y.; Kim, J.-S.; Yu, E. Expression of DNA methyltransferases in multistep hepatocarcinogenesis. Hum. Pathol. 2003, 34, 11–17. [Google Scholar] [CrossRef]
- Chen, J.; Yang, J.; Wei, X.; Wu, Q.; Xu, Z.; Gu, D.; Jin, Y.; Shen, Y.; Huang, H.; Fan, H. Clinical significance of the expression of DNA methyltransferase proteins in gastric cancer. Mol. Med. Rep. 2011, 4, 1139–1143. [Google Scholar] [CrossRef]
- Ding, W.-J.; Fang, J.-Y.; Chen, X.-Y.; Peng, Y.-S. The expression and clinical significance of DNA methyltransferase proteins in human gastric cancer. Dig. Dis. Sci. 2008, 53, 2083–2089. [Google Scholar] [CrossRef]
- Camero, S.; Vitali, G.; Pontecorvi, P.; Ceccarelli, S.; Anastasiadou, E.; Cicchetti, F.; Flex, E.; Pomella, S.; Cassandri, M.; Rota, R.; et al. DNMT3A and DNMT3B Targeting as an Effective Radiosensitizing Strategy in Embryonal Rhabdomyosarcoma. Cells 2021, 10, 2956. [Google Scholar] [CrossRef] [PubMed]
- Cui, J.; Zheng, L.; Zhang, Y.; Xue, M. Bioinformatics analysis of DNMT1 expression and its role in head and neck squamous cell carcinoma prognosis. Sci. Rep. 2021, 11, 2267. [Google Scholar] [CrossRef]
- Liu, P.; Yang, F.; Zhang, L.; Hu, Y.; Chen, B.; Wang, J.; Su, L.; Wu, M.; Chen, W. Emerging role of different DNA methyltransferases in the pathogenesis of cancer. Front. Pharmacol. 2022, 13, 958146. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, J.H.; Chie, E.K.; Young, P.; Da Kim, I.A.; Kim, I.H. DNMT (DNA methyltransferase) inhibitors radiosensitize human cancer cells by suppressing DNA repair activity. Radiat. Oncol. 2012, 7, 39. [Google Scholar] [CrossRef]
- Kang, H.-C.; Chie, E.K.; Kim, H.J.; Kim, J.H.; Kim, I.H.; Kim, K.; Shin, B.S.; Ma, E. A phthalimidoalkanamide derived novel DNMT inhibitor enhanced radiosensitivity of A549 cells by inhibition of homologous recombination of DNA damage. Investig. New Drugs 2019, 37, 1158–1165. [Google Scholar] [CrossRef]

| Characteristic | Number of Patients (Row %) |
|---|---|
| Total N | 58 (100) |
| Age, y | |
| Median | 68.8 |
| Range | 41.7–84.9 |
| Age, y | |
| <65 | 24 (41) |
| ≥65 | 34 (59) |
| Sex | |
| Male | 51 (88) |
| Female | 7 (12) |
| Clinical T-classification | |
| T3 | 35 (60) |
| T4 | 23 (40) |
| Clinical N-classification | |
| N0 | 43 (74) |
| N1 | 10 (17) |
| N2 | 3 (5) |
| N3 | 2 (4) |
| Follow-up, mo | |
| Median | 51.9 |
| Range | 1.9–145.9 |
| Locoregional recurrence | |
| Yes | 16 (28) |
| No | 42 (72) |
| Disease-specific mortality | |
| Yes | 10 (17) |
| No | 48 (83) |
| Characteristic | Locoregional Recurrence | Disease-Specific Mortality | |||
|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | ||
| DNMT1 | <80% | 1 | 0.766 | 1 | 0.228 |
| ≥80% | 0.86 (0.31–2.36) | 0.39 (0.08–1.82) | |||
| DNMT3A | <70% | 1 | 0.031 | 1 | 0.029 |
| ≥70% | 0.29 (0.09–0.89) | 0.10 (0.01–0.80) | |||
| DNMT3B | <85% | 1 | 0.282 | 1 | 0.047 |
| ≥85% | 0.58 (0.22–1.56) | 0.25 (0.07–0.98) | |||
| Sex | Female | 1 | 0.455 | 1 | 0.081 |
| Male | 0.62 (0.18–2.18) | 0.30 (0.08–1.16) | |||
| Age, y | <65 | 1 | 0.402 | 1 | 0.606 |
| ≥65 | 0.66 (0.25–1.75) | 0.72 (0.21–2.49) | |||
| T-status | T3 | 1 | 0.344 | 1 | 0.502 |
| T4 | 1.61 (0.60–4.28) | 1.53 (0.44–5.30) | |||
| N-status | N0 | 1 | <0.001 | 1 | 0.001 |
| N+ | 6.46 (2.38–17.51) | 9.94 (2.56–38.64) | |||
| Characteristic | Locoregional Recurrence | ||
|---|---|---|---|
| HR (95% CI) | p | ||
| DNMT3A | <70% | 1 | 0.076 |
| ≥70% | 0.36 (0.11–1.11) | ||
| N-status | N0 | 1 | <0.001 |
| N+ | 5.63 (2.06–15.39) | ||
| Characteristic | Disease-Specific Mortality | ||
|---|---|---|---|
| HR (95% CI) | p | ||
| DNMT3A | <70% | 1 | 0.045 |
| >70% | 0.12 (0.02–0.96) | ||
| N-status | N0 | 1 | 0.002 |
| N+ | 8.70 (2.21–34.22) | ||
| Characteristic | Disease-Specific Mortality | ||
|---|---|---|---|
| HR (95% CI) | p | ||
| DNMT3B | <85% | 1 | 0.122 |
| ≥85% | 0.34 (0.09–1.34) | ||
| N-status | N0 | 1 | 0.002 |
| N+ | 8.46 (2.15–33.32) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van den Bovenkamp, K.; Halmos, G.B.; Slagter-Menkema, L.; van Dijk, B.A.C.; Yu, S.; Langendijk, J.A.; van der Laan, B.F.A.M.; Schuuring, E.; van der Vegt, B. The Association Between Clinical Outcome and Expression of DNMT1, 3A, and 3B in Locally Advanced Laryngeal Carcinomas Treated by Definitive Radiotherapy. Cancers 2025, 17, 1741. https://doi.org/10.3390/cancers17111741
van den Bovenkamp K, Halmos GB, Slagter-Menkema L, van Dijk BAC, Yu S, Langendijk JA, van der Laan BFAM, Schuuring E, van der Vegt B. The Association Between Clinical Outcome and Expression of DNMT1, 3A, and 3B in Locally Advanced Laryngeal Carcinomas Treated by Definitive Radiotherapy. Cancers. 2025; 17(11):1741. https://doi.org/10.3390/cancers17111741
Chicago/Turabian Stylevan den Bovenkamp, Karlijn, Gyorgy B. Halmos, Lorian Slagter-Menkema, Boukje A. C. van Dijk, Shibo Yu, Johannes A. Langendijk, Bernard F. A. M. van der Laan, Ed Schuuring, and Bert van der Vegt. 2025. "The Association Between Clinical Outcome and Expression of DNMT1, 3A, and 3B in Locally Advanced Laryngeal Carcinomas Treated by Definitive Radiotherapy" Cancers 17, no. 11: 1741. https://doi.org/10.3390/cancers17111741
APA Stylevan den Bovenkamp, K., Halmos, G. B., Slagter-Menkema, L., van Dijk, B. A. C., Yu, S., Langendijk, J. A., van der Laan, B. F. A. M., Schuuring, E., & van der Vegt, B. (2025). The Association Between Clinical Outcome and Expression of DNMT1, 3A, and 3B in Locally Advanced Laryngeal Carcinomas Treated by Definitive Radiotherapy. Cancers, 17(11), 1741. https://doi.org/10.3390/cancers17111741








