The Relationship Between Patient Activation, Cancer-Related Symptoms, and Job Performance Among Young Adult Cancer Survivors with Low and High Workplace Support: A Cross-Sectional Observational Study
Simple Summary
Abstract
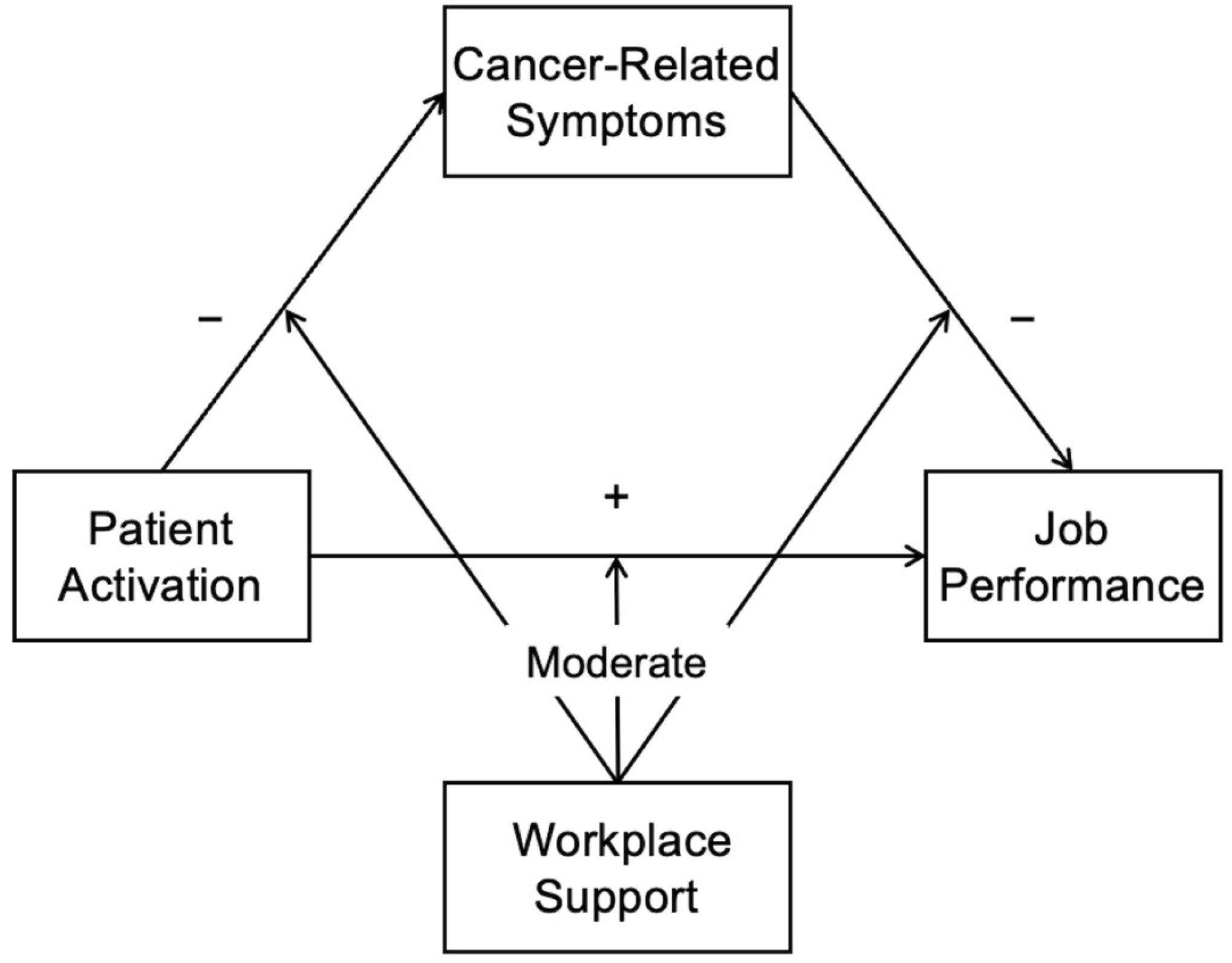
1. Introduction
2. Materials and Methods
2.1. Study Participants and Procedures
2.2. Measures
2.2.1. Demographic and Clinical Characteristics
2.2.2. Patient Activation
2.2.3. Cancer-Related Symptoms
2.2.4. Job Performance
2.3. Statistical Analysis
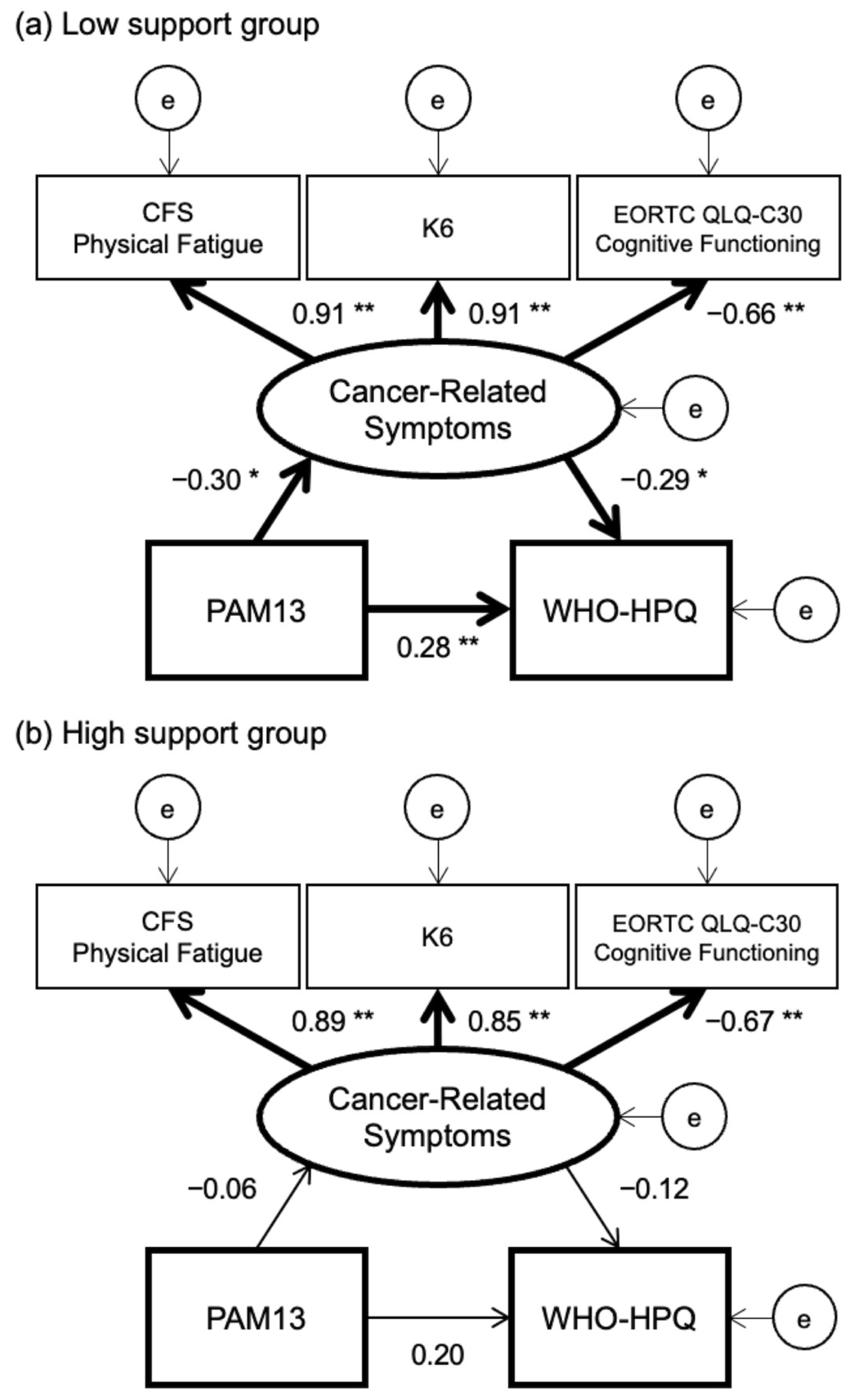
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AGFI | Adjusted Goodness-of-Fit Index |
| CFI | Comparative Fit Index |
| CFS | Cancer Fatigue Scale |
| CMIN | Chi-Square Statistic |
| df | Degrees of Freedom |
| EORTC QLQ-C30 | European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 |
| GFI | Goodness-of-Fit Index |
| IQR | Interquartile Range |
| K6 | Kessler-6 |
| New BJSQ | New Brief Job Stress Questionnaire |
| PAM-13 | 13-item version of Patient Activation Measure |
| RMSEA | Root Mean Square Error of Approximation |
| SEM | Structural Equation Modeling |
| WHO-HPQ | World Health Organization Health and Performance Questionnaire |
References
- Torp, S.; Paraponaris, A.; Van Hoof, E.; Lindbohm, M.L.; Tamminga, S.J.; Alleaume, C.; Campenhout, N.V.; Sharp, L.; de Boer, A.G. Work-related outcomes in self-employed cancer survivors: A European multi-country study. J. Occup. Rehabil. 2019, 29, 361–374. [Google Scholar] [CrossRef]
- Bradley, C.J.; Brown, K.L.; Haan, M.; Glasgow, R.E.; Newman, L.S.; Rabin, B.; Ritzwoller, D.P.; Tenney, L. Cancer survivorship and employment: Intersection of oral agents, changing workforce dynamics, and employers’ perspectives. J. Natl. Cancer Inst. 2018, 110, 1292–1299. [Google Scholar] [CrossRef]
- Desiron, H.A.; Crutzen, R.; Godderis, L.; Van Hoof, E.; de Rijk, A. Bridging health care and the workplace: Formulation of a return-to-work intervention for breast cancer patients using an intervention mapping approach. J. Occup. Rehabil. 2016, 26, 350–365. [Google Scholar] [CrossRef] [PubMed]
- Todd, B.L.; Feuerstein, E.L.; Feuerstein, M. When breast cancer survivors report cognitive problems at work. Int. J. Psychiatry Med. 2011, 42, 279–294. [Google Scholar] [CrossRef] [PubMed]
- Calvio, L.; Peugeot, M.; Bruns, G.L.; Todd, B.L.; Feuerstein, M. Measures of cognitive function and work in occupationally active breast cancer survivors. J. Occup. Environ. Med. 2010, 52, 219–227. [Google Scholar] [CrossRef]
- Bower, J.E. Cancer-related fatigue—Mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 2014, 11, 597–609. [Google Scholar] [CrossRef]
- Smith, H.R. Depression in cancer patients: Pathogenesis, implications and treatment (Review). Oncol. Lett. 2015, 9, 1509–1514. [Google Scholar] [CrossRef] [PubMed]
- Ahles, T.A.; Root, J.C. Cognitive Effects of Cancer and Cancer Treatments. Annu. Rev. Clin. Psychol. 2018, 14, 425–451. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kissane, D.W.; Richardson, G.; Senior, J.; Morgan, J.; Gregory, P.; Birks, S.; Ooi, C.; Lipton, L.; Antill, Y.; et al. The role of depression and other psychological factors in work ability among breast cancer survivors in Australia. Psychooncology 2022, 31, 167–175. [Google Scholar] [CrossRef]
- Dahl, A.A.; Fosså, S.D.; Lie, H.C.; Loge, J.H.; Reinertsen, K.V.; Ruud, E.; Kiserud, C.E. Employment status and work ability in long-term young adult cancer survivors. J. Adolesc. Young Adult Oncol. 2019, 8, 304–311. [Google Scholar] [CrossRef]
- Dorland, H.F.; Abma, F.I.; Van Zon, S.K.R.; Stewart, R.E.; Amick, B.C.; Ranchor, A.V.; Roelen, C.A.M.; Bültmann, U. Fatigue and depressive symptoms improve but remain negatively related to work functioning over 18 months after return to work in cancer patients. J. Cancer Surviv. 2018, 12, 371–378. [Google Scholar] [CrossRef]
- Von Ah, D.; Storey, S.; Crouch, A. Relationship between self-reported cognitive function and work-related outcomes in breast cancer survivors. J. Cancer Surviv. 2018, 12, 246–255. [Google Scholar] [CrossRef] [PubMed]
- van Muijen, P.; Duijts, S.F.A.; Bonefaas-Groenewoud, K.; van der Beek, A.J.; Anema, J.R. Predictors of fatigue and work ability in cancer survivors. Occup. Med. 2017, 67, 703–711. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hydeman, J.A.; Uwazurike, O.C.; Adeyemi, E.I.; Beaupin, L.K. Survivorship needs of adolescent and young adult cancer survivors: A concept mapping analysis. J. Cancer Surviv. 2019, 13, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Act for Eliminating Discrimination Against Persons with Disabilities. Available online: https://www.japaneselawtranslation.go.jp/ja/laws/view/3052 (accessed on 25 May 2024).
- Act to Facilitate the Employment of Persons with Disabilities. Available online: https://www.japaneselawtranslation.go.jp/ja/laws/view/3845 (accessed on 25 May 2024).
- Ishida, Y.; Hayashi, M.; Inoue, F.; Ozawa, M. Recent employment trend of childhood cancer survivors in Japan: A cross-sectional survey. Int. J. Clin. Oncol. 2014, 19, 973–981. [Google Scholar] [CrossRef]
- Jigyojyo ni okeru chiryo to shigoto no ryoritsu shien no tame no gaidorain [Guidelines for Supporting the Balance of Treatment and Work in the Workplace]. Available online: https://chiryoutoshigoto.mhlw.go.jp/dl/download/guideline.pdf (accessed on 10 June 2021).
- Hammond, A.; O’Brien, R.; Woodbridge, S.; Bradshaw, L.; Prior, Y.; Radford, K.; Culley, J.; Whitham, D.; Pulikottil-Jacob, R. Job retention vocational rehabilitation for employed people with inflammatory arthritis (WORK-IA): A feasibility randomized controlled trial. BMC Musculoskelet. Disord. 2017, 18, 315. [Google Scholar] [CrossRef]
- van Vilsteren, M.; Boot, C.R.; Twisk, J.W.; van Schaardenburg, D.; Steenbeek, R.; Voskuyl, A.E.; Anema, J.R. Effectiveness of an integrated care intervention on supervisor support and work functioning of workers with rheumatoid arthritis. Disabil. Rehabil. 2017, 39, 354–362. [Google Scholar] [CrossRef]
- Tamminga, S.J.; Verbeek, J.H.; Bos, M.M.; Fons, G.; Kitzen, J.J.E.M.; Plaisier, P.W.; Frings-Dresen, M.H.W.; de Boer, A.G. Effectiveness of a hospital-based work support intervention for female cancer patients—A multi-centre randomised controlled trial. PLoS ONE 2013, 8, e63271. [Google Scholar] [CrossRef]
- Rabin, C. Cancer-related self-disclosure in the workplace/school by adolescent and young adult cancer survivors. J. Adolesc. Young Adult Oncol. 2020, 9, 528–533. [Google Scholar] [CrossRef]
- Stergiou-Kita, M.; Pritlove, C.; van Eerd, D.; Holness, L.D.; Kirsh, B.; Duncan, A.; Jones, J. The provision of workplace accommodations following cancer: Survivor, provider, and employer perspectives. J. Cancer Surviv. 2016, 10, 489–504. [Google Scholar] [CrossRef]
- Stergiou-Kita, M.; Pritlove, C.; Kirsh, B. The "Big C"-stigma, cancer, and workplace discrimination. J. Cancer Surviv. 2016, 10, 1035–1050. [Google Scholar] [CrossRef] [PubMed]
- Fujisawa, D.; Umezawa, S.; Fujimori, M.; Miyashita, M. Prevalence and associated factors of perceived cancer-related stigma in Japanese cancer survivors. Jpn. J. Clin. Oncol. 2020, 50, 1325–1329. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Tsuchiya, M.; Horio, Y.; Funazaki, H.; Aogi, K.; Miyauchi, K.; Arai, Y. Job resignation after cancer diagnosis among working survivors in Japan: Timing, reasons and change of information needs over time. Jpn. J. Clin. Oncol. 2018, 48, 43–51. [Google Scholar] [CrossRef]
- Soejima, T.; Kamibeppu, K. Are cancer survivors well-performing workers? A systematic review. Asia Pac. J. Clin. Oncol. 2016, 12, e383–e397. [Google Scholar] [CrossRef]
- Hibbard, J.H.; Mahoney, E.R.; Stockard, J.; Tusler, M. Development and testing of a short form of the patient activation measure. Health Serv. Res. 2005, 40, 1918–1930. [Google Scholar] [CrossRef]
- Hibbard, J.H.; Mahoney, E.; Sonet, E. Does patient activation level affect the cancer patient journey? Patient Educ. Couns. 2017, 100, 1276–1279. [Google Scholar] [CrossRef]
- Rijken, M.; Heijmans, M.; Jansen, D.; Rademakers, J. Developments in patient activation of people with chronic illness and the impact of changes in self-reported health: Results of a nationwide longitudinal study in The Netherlands. Patient Educ. Couns. 2014, 97, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Greene, J.; Hibbard, J.H. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J. Gen. Intern. Med. 2012, 27, 520–526. [Google Scholar] [CrossRef]
- van Maarschalkerweerd, P.; Rademakers, J.; Rijken, M. Cancer survivors’ activation to self-management and its relationship with participation in paid work and work-related problems. Psychooncology 2017, 26, 1881–1887. [Google Scholar] [CrossRef]
- Hallgren, E.; Ayers, B.L.; Moore, R.; Purvis, R.S.; McElfish, P.A.; Maraboyina, S.; Bryant-Smith, G. Facilitators and barriers to employment for rural women cancer survivors. J. Cancer Surviv. 2023, 17, 1338–1346. [Google Scholar] [CrossRef]
- Kollerup, A.; Ladenburg, J.; Heinesen, E.; Kolodziejczyk, C. The importance of workplace accommodation for cancer survivors—The role of flexible work schedules and psychological help in returning to work. Econ. Hum. Biol. 2021, 43, 101057. [Google Scholar] [CrossRef]
- Alleaume, C.; Paraponaris, A.; Bendiane, M.K.; Peretti-Watel, P.; Bouhnik, A.D. The positive effect of workplace accommodations on the continued employment of cancer survivors five years after diagnosis. Support. Care Cancer 2020, 28, 4435–4443. [Google Scholar] [CrossRef] [PubMed]
- Bochimoto, H.; Ishimaru, T.; Nakano, A.; Hasegawa, K.; Kimura, E.; Tajima, S.; Yoshikawa, T.; Nemoto, H. Association between workplace social support and use of health-promoting wearable devices: A prospective cohort study of Japanese employees. J. UOEH 2023, 45, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Endo, M.; Muto, G.; Imai, Y.; Mitsui, K.; Nishimura, K.; Hayashi, K. Predictors of post-cancer diagnosis resignation among Japanese cancer survivors. J. Cancer Surviv. 2020, 14, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Inoue, A.; Kawakami, N.; Shimomitsu, T.; Tsutsumi, A.; Haratani, A.; Yoshikawa, T.; Shimazu, A.; Odagiri, Y. Development of a short questionnaire to measure an extended set of job demands, job resources, and positive health outcomes: The new brief job stress questionnaire. Ind. Health 2014, 52, 175–189. [Google Scholar] [CrossRef]
- Fujita, E.; Kuno, E.; Kato, D.; Kokochi, M.; Uehara, K.; Hirayasu, Y. Seishin no Kenko Kanri heno Sekkyokusei Hyoka Syakudo Nihongoban no Kaihatsu [Development and validation of the Japanese version of the patient activation measure 13 for mental health]. Seishin Igaku 2010, 52, 765–772. [Google Scholar] [CrossRef]
- Okuyama, T.; Akechi, T.; Kugaya, A.; Okamura, H.; Shima, Y.; Maruguchi, M.; Hosaka, T.; Uchitomi, Y. Development and validation of the cancer fatigue scale: A brief, three-dimensional, self-rating scale for assessment of fatigue in cancer patients. J. Pain Symptom Manag. 2000, 19, 5–14. [Google Scholar] [CrossRef]
- Furukawa, T.A.; Kawakami, N.; Saitoh, M.; Ono, Y.; Nakane, Y.; Nakamura, Y.; Tachimori, H.; Iwata, N.; Uda, H.; Nakane, H.; et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 2008, 17, 152–158. [Google Scholar] [CrossRef]
- Kobayashi, K.; Takeda, F.; Teramukai, S.; Gotoh, I.; Sakai, H.; Yoneda, S.; Noguchi, Y.; Ogasawara, H.; Yoshida, K. A cross-validation of the European Organization for Research and Treatment of Cancer QLQ-C30 (EORTC QLQ-C30) for Japanese with lung cancer. Eur. J. Cancer 1998, 34, 810–815. [Google Scholar] [CrossRef]
- Mayo, S.J.; Lustberg, M.; Dhillon, H.M.; Nakamura, Z.M.; Allen, D.H.; Von Ah, D.; Janelsins, C.M.; Chan, A.; Olson, K.; Tan, C.J.; et al. Cancer-related cognitive impairment in patients with non-central nervous system malignancies: An overview for oncology providers from the MASCC Neurological Complications Study Group. Support. Care Cancer 2021, 29, 2821–2840. [Google Scholar] [CrossRef]
- Suzuki, T.; Miyaki, K.; Song, Y.; Tsutsumi, A.; Kawakami, N.; Shimazu, A.; Takahashi, M.; Inoue, A.; Kurioka, S. Relationship between sickness presenteeism (WHO-HPQ) with depression and sickness absence due to mental disease in a cohort of Japanese workers. J. Affect. Disord. 2015, 180, 14–20. [Google Scholar] [CrossRef]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. Online 2003, 8, 23–74. [Google Scholar] [CrossRef]
- Fowles, J.B.; Terry, P.; Xi, M.; Hibbard, J.; Bloom, C.T.; Harvey, L. Measuring self-management of patients’ and employees’ health: Further validation of the Patient Activation Measure (PAM) based on its relation to employee characteristics. Patient Educ. Couns. 2009, 77, 116–122. [Google Scholar] [CrossRef]
- Cousins, R.; MacKay, C.J.; Clarke, S.D.; Kelly, C.; Kelly, P.J.; McCaig, R.H. ‘Management Standards’ work-related stress in the UK: Practical development. Work Stress 2004, 18, 113–136. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Lindbohm, M.L. Work engagement among breast cancer survivors and the referents: The importance of optimism and social resources at work. J. Cancer Surviv. 2008, 2, 283–295. [Google Scholar] [CrossRef]
- Yang, T.; Ma, T.; Liu, P.; Liu, Y.; Chen, Q.; Guo, Y.; Zhang, S.; Deng, J. Perceived social support and presenteeism among healthcare workers in China: The mediating role of organizational commitment. Environ. Health Prev. Med. 2019, 24, 55. [Google Scholar] [CrossRef] [PubMed]
- Baeriswyl, S.; Krause, A.; Elfering, A.; Berset, M. How workload and coworker support relate to emotional exhaustion: The mediating role of sickness presenteeism. Int. J. Stress Manag. 2017, 24, 52–73. [Google Scholar] [CrossRef]
- Overview of the Basic Plan to Promote Cancer Control Programs. Available online: https://www.mhlw.go.jp/english/wp/wp-hw3/dl/2-078.pdf (accessed on 5 December 2022).
- Yahaya, N.A.; Abdullah, K.L.; Ramoo, V.; Zainal, N.Z.; Wong, L.P.; Danaee, M. Effects of Self-Care Education Intervention Program (SCEIP) on activation level, psychological distress, and treatment-related information. Healthcare 2022, 10, 1572. [Google Scholar] [CrossRef]
- Knoerl, R.; Lee, D.; Yang, J.; Bridges, C.; Kanzawa-Lee, G.; Smith, L.G.; Smith, L.E.M. Examining the impact of a web-based intervention to promote patient activation in chemotherapy-induced peripheral neuropathy assessment and management. J. Cancer Educ. 2018, 33, 1027–1035. [Google Scholar] [CrossRef]
- National Cancer Center Japan. Cancer Statistics in Japan 2021. Available online: https://ganjoho.jp/public/qa_links/report/statistics/2021_en.html (accessed on 25 November 2021).
- Education at Glance 2021: OECD Indicators. Available online: https://www.oecd-ilibrary.org/sites/1426642c-en/index.html?itemId=/content/component/1426642c-en (accessed on 5 December 2022).
- Lerner, D.; Amick, B.C., 3rd; Rogers, W.H.; Malspeis, S.; Bungay, K.; Cynn, D. The work limitations questionnaire. Med. Care 2001, 39, 72–85. [Google Scholar] [CrossRef]
| N = 202 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Low Support Group (n = 97) | High Support Group (n = 105) | WHO-HPQ | ||||||||
| n | % | n | % | n | % | p a | Median | IQR | η2 b | p b | |
| Age | 0.07 | 0.14 | 0.29 | ||||||||
| 20–24 years | 7 | 3 | 2 | 2 | 5 | 5 | 50.0 | 30.0–80.0 | |||
| 25–29 years | 27 | 13 | 19 | 20 | 8 | 8 | 60.0 | 50.0–80.0 | |||
| 30–34 years | 61 | 30 | 28 | 29 | 33 | 31 | 70.0 | 50.0–80.0 | |||
| 35–39 years | 107 | 53 | 48 | 49 | 59 | 56 | 60.0 | 50.0–70.0 | |||
| Gender | 0.06 | 0.06 | 0.40 | ||||||||
| Male | 45 | 22 | 16 | 16 | 29 | 28 | 70.0 | 50.0–80.0 | |||
| Female | 157 | 78 | 81 | 84 | 76 | 72 | 60.0 | 50.0–80.0 | |||
| Educational level | 0.89 | 0.19 | 0.11 | ||||||||
| Junior-high school | 4 | 2 | 2 | 2 | 2 | 2 | 65.0 | 52.5–70.0 | |||
| High school | 43 | 21 | 20 | 21 | 23 | 22 | 60.0 | 50.0–70.0 | |||
| College/Vocational school | 42 | 21 | 18 | 19 | 24 | 23 | 60.0 | 50.0–70.0 | |||
| University/Graduate school | 110 | 54 | 56 | 58 | 54 | 51 | 70.0 | 50.0–80.0 | |||
| Others | 3 | 1 | 1 | 1 | 2 | 2 | 60.0 | 50.0–60.0 | |||
| Type of employment | 0.01 | 0.07 | 0.66 | ||||||||
| Permanent | 135 | 67 | 55 | 57 | 80 | 76 | 60.0 | 50.0–80.0 | |||
| Temporary | 58 | 29 | 37 | 38 | 21 | 20 | 60.0 | 50.0–72.5 | |||
| Self-employed | 9 | 4 | 5 | 5 | 4 | 4 | 70.0 | 60.0–75.0 | |||
| Type of occupation | 0.80 | 0.18 | 0.37 | ||||||||
| Technical | 38 | 19 | 17 | 18 | 21 | 20 | 60.0 | 50.0–80.0 | |||
| Managerial | 17 | 8 | 8 | 8 | 9 | 9 | 70.0 | 60.0–80.0 | |||
| Clerical | 76 | 38 | 35 | 36 | 41 | 39 | 70.0 | 50.0–80.0 | |||
| Sales | 20 | 10 | 9 | 9 | 11 | 10 | 60.0 | 50.0–70.0 | |||
| Production | 16 | 8 | 7 | 7 | 9 | 9 | 70.0 | 52.5–80.0 | |||
| Services | 25 | 12 | 14 | 14 | 11 | 10 | 60.0 | 50.0–70.0 | |||
| Others | 10 | 5 | 7 | 7 | 3 | 3 | 60.0 | 50.0–75.0 | |||
| Cancer sites | 0.04 | 0.24 | 0.07 | ||||||||
| Gastric cancer | 16 | 8 | 6 | 6 | 10 | 10 | 70.0 | 52.5–80.0 | |||
| Colorectal cancer | 16 | 8 | 8 | 8 | 8 | 8 | 65.0 | 50.0–77.5 | |||
| Breast cancer | 18 | 9 | 11 | 11 | 7 | 7 | 70.0 | 60.0–72.5 | |||
| Female genital cancer | 85 | 42 | 50 | 52 | 35 | 33 | 60.0 | 50.0–80.0 | |||
| Thyroid cancer | 17 | 8 | 7 | 7 | 10 | 10 | 50.0 | 50.0–70.0 | |||
| Lymphoma/leukemia | 15 | 7 | 4 | 4 | 11 | 10 | 70.0 | 50.0–80.0 | |||
| Others | 35 | 17 | 11 | 11 | 24 | 23 | 70.0 | 40.0–70.0 | |||
| Period from diagnosis | 0.02 | 0.11 | 0.27 | ||||||||
| <1 year | 32 | 16 | 15 | 15 | 17 | 16 | 70.0 | 40.0–80.0 | |||
| 1– <5 years | 98 | 49 | 38 | 39 | 60 | 57 | 60.0 | 50.0–80.0 | |||
| ≥5 years | 72 | 36 | 44 | 45 | 28 | 27 | 70.0 | 50.0–77.5 | |||
| Surgery | 0.19 | 0.00 | 0.97 | ||||||||
| Yes | 122 | 60 | 54 | 56 | 68 | 65 | 60.0 | 50.0–80.0 | |||
| No | 80 | 40 | 43 | 44 | 37 | 35 | 60.0 | 50.0–72.5 | |||
| Chemotherapy | 0.51 | 0.02 | 0.76 | ||||||||
| Yes | 50 | 25 | 22 | 23 | 28 | 27 | 60.0 | 50.0–80.0 | |||
| No | 152 | 75 | 75 | 77 | 77 | 73 | 70.0 | 50.0–80.0 | |||
| Radiation | 0.14 | 0.01 | 0.87 | ||||||||
| Yes | 26 | 13 | 9 | 9 | 17 | 16 | 60.0 | 50.0–80.0 | |||
| No | 176 | 87 | 88 | 91 | 88 | 84 | 60.0 | 50.0–70.0 | |||
| Hormone therapy | 0.50 | 0.05 | 0.44 | ||||||||
| Yes | 18 | 9 | 10 | 10 | 8 | 8 | 60.0 | 50.0–80.0 | |||
| No | 184 | 91 | 87 | 90 | 97 | 92 | 70.0 | 60.0–80.0 | |||
| Median | IQR | Median | IQR | Median | IQR | p a | Median | IQR | r c | p c | |
| Job demands on New BJSQ | 2.7 | 2.2–3.2 | 2.5 | 2.0–3.1 | 2.7 | 2.2–3.2 | 0.18 | - | - | −0.08 | 0.25 |
| Workplace support on New BJSQ | 2.3 | 2.0–2.8 | 2.0 | 1.5–2.8 | 2.3 | 2.0–2.9 | 0.03 | - | - | 0.27 | <0.01 |
| Patient activation score on PAM13 | 51.0 | 45.3–63.1 | 51.0 | 45.3–60.6 | 53.2 | 45.3–63.1 | 0.58 | - | - | 0.31 | <0.01 |
| CFS Physical Fatigue subscale | 7.0 | 3.0–13.3 | 7.0 | 3.0–13.5 | 7.0 | 2.5–13.5 | 0.99 | - | - | −0.16 | 0.02 |
| K6 | 5.0 | 1.0–11.0 | 6.0 | 0.0–10.5 | 4.0 | 1.0–11.5 | 0.71 | - | - | −0.16 | 0.02 |
| EORTC QLQ-C30 Cognitive Functioning subscale | 66.7 | 50.0–83.3 | 66.7 | 50.0–100.0 | 66.7 | 50.0–83.3 | 0.37 | - | - | 0.18 | <0.01 |
| WHO-HPQ | 60.0 | 50.0–80.0 | 60.0 | 50.0–70.0 | 70.0 | 60.0–80.0 | <0.01 | - | - | - | - |
| N = 202 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Models a | CMIN | Change b | p c | CMIN/df | CFI | GFI | AGFI | RMSEA | AIC |
| Model without any path constraints | 3.11 | NA | NA | 0.389 | 1.000 | 0.994 | 0.977 | <0.001 | 47.112 |
| Model with path constraints | |||||||||
| PAM13 to cancer-related symptoms | 5.11 | 2.00 | 0.16 | 0.567 | 1.000 | 0.974 | 0.954 | <0.001 | 47.107 |
| PAM13 to WHO-HPQ | 3.26 | 0.15 | 0.70 | 0.362 | 1.000 | 0.978 | 0.961 | <0.001 | 45.261 |
| Cancer-related symptoms to WHO-HPQ | 4.55 | 1.43 | 0.23 | 0.505 | 1.000 | 0.975 | 0.956 | <0.001 | 46.545 |
| All paths | 7.02 | 3.91 | 0.27 | 0.638 | 1.000 | 0.971 | 0.954 | <0.001 | 45.201 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soejima, T.; Tokita, M.; Kitao, M. The Relationship Between Patient Activation, Cancer-Related Symptoms, and Job Performance Among Young Adult Cancer Survivors with Low and High Workplace Support: A Cross-Sectional Observational Study. Cancers 2025, 17, 1742. https://doi.org/10.3390/cancers17111742
Soejima T, Tokita M, Kitao M. The Relationship Between Patient Activation, Cancer-Related Symptoms, and Job Performance Among Young Adult Cancer Survivors with Low and High Workplace Support: A Cross-Sectional Observational Study. Cancers. 2025; 17(11):1742. https://doi.org/10.3390/cancers17111742
Chicago/Turabian StyleSoejima, Takafumi, Masahito Tokita, and Mari Kitao. 2025. "The Relationship Between Patient Activation, Cancer-Related Symptoms, and Job Performance Among Young Adult Cancer Survivors with Low and High Workplace Support: A Cross-Sectional Observational Study" Cancers 17, no. 11: 1742. https://doi.org/10.3390/cancers17111742
APA StyleSoejima, T., Tokita, M., & Kitao, M. (2025). The Relationship Between Patient Activation, Cancer-Related Symptoms, and Job Performance Among Young Adult Cancer Survivors with Low and High Workplace Support: A Cross-Sectional Observational Study. Cancers, 17(11), 1742. https://doi.org/10.3390/cancers17111742






