Simple Summary
Pituitary tumours are slowly growing tumours of the pituitary gland, and they can cause damage due to the invasion or compression of surrounding tissues, such as the nerves responsible for vision, and/or due to altered hormone production. The treatment of pituitary tumours is complex and requires a wide range of medical specialists, including neurosurgeons, endocrinologists, neuropathologists, neuroradiologists, neuro-ophthalmologists, and otorhinolaryngologists, among others. Thus, optimal management of patients with pituitary tumours is best provided in the context of a dedicated multidisciplinary team with expertise in treating such conditions.
Abstract
The optimal care for patients with pituitary tumours is best provided in a multidisciplinary and collaborative environment, which requires the contribution of multiple medical specialties working together. The benefits and advantages of the pituitary multidisciplinary team (MDT) are broad, and all relevant international consensus and guidelines in the field recommend that patients with pituitary tumours should always be managed in a MDT. Endocrinologists and neurosurgeons are normally the leading specialties within the pituitary MDT, supported by many other specialties with significant contributions to the diagnosis and management of pituitary tumours, including neuropathology, neuroradiology, neuro-ophthalmology, and otorhinolaryngology, among others. Here, we review the literature concerning the concepts of Pituitary MDT/Pituitary Tumour Centre of Excellence (PTCOE) in terms of their mission, goals, benefits, structure, proposed models of function, and barriers, and we also provide the views of different specialists involved in our Pituitary MDT.
1. Introduction
The concept of multidisciplinary team (MDT) and multidisciplinary medical care is recognised as best practice and has been increasingly used for a wide variety of conditions [1,2]. The contemporaneous management of complex and/or rare disorders relies mainly on MDT meetings and discussions among experienced healthcare professionals, which ensure timely, appropriate, specialized, and multidisciplinary decision-making, thus improving outcomes. Moreover, MDT meetings provide unique opportunities for improved medical communication and development of cohesive management plans, learning platforms, and knowledge for research projects [1,3].
Pituitary tumours arise from the adenohypophysis and account for 10–15% of all intracranial neoplasms. Although these tumours are usually benign, up to 30–45% invade the cavernous or sphenoid sinus [4,5,6]. Less frequently, they may behave aggressively, recur multiple times and/or become resistant to conventional treatments, or more rarely, metastasize [6,7]. From a histological standpoint, pituitary tumours are classified on the basis of the respective cell lineage determined by the expression of pituitary hormones, transcription factors, or other biomarkers as: PIT1-lineage tumours (somatotroph tumours, lactotroph tumours, mammosomatotroph tumours, thyrotroph tumours, mature/immature PIT1 lineage tumours, acidophil stem cell tumours, and mixed somatotroph and lactotroph tumours); TPIT-lineage tumours (corticotroph tumours including densely granulated, sparsely granulated, and Crooke cell tumours); SF1-lineage tumours (i.e., gonadotroph tumours); tumours with no distinct cell lineage (plurihormonal tumours); and null cell tumours [8]. Pituitary tumours may cause syndromes related to excessive hormone secretion, such as Cushing’s disease or acromegaly, or hypopituitarism-related symptoms due to the compression of the normal pituitary. Also, presentation can include neurological symptoms such as visual defects, diplopia, or headache. Moreover, approximately 5% of pituitary tumours may be familial, occurring in isolation or as part of a genetic syndrome such as multiple endocrine neoplasia type 1 or Carney complex [6,9].
The above-mentioned aspects, together with the challenging anatomical location of the pituitary and its relationship with key structures such as the optic chiasm, impose several difficulties on the management of patients with pituitary tumours. Hence, the best care for pituitary tumour patients is provided by an experienced MDT working in an interdisciplinary and collaborative manner within the frame of a Pituitary MDT or Pituitary Tumour Centre of Excellence (PTCOE) [10,11,12].
Here, we reviewed the literature concerning Pituitary MDT and PTCOE, and we are also providing the views and perspectives of different medical specialists involved in Pituitary MDT in our centre.
2. Concept and Mission of the Pituitary Multidisciplinary Team (MDT)/Pituitary Tumour Centres of Excellence (PTCOE)
The concept of a Centre of Excellence is disseminating in several fields of medicine to address public and professional concerns regarding the quality of care for patients suffering from a certain condition. This concept is useful for conditions demanding an interdisciplinary management approach, and thus, a dedicated MDT composed by different experts in surgery, medical treatments, radiotherapy, or diagnostic procedures [10,13]. The concepts of MDT, or Centres of Excellence, are relevant in several cancers and rare diseases, as well as in many endocrine conditions, including thyroid diseases [14,15], obesity [16,17,18], diabetes [19,20], and neuroendocrine tumours [21].
The pursuit of excellence in delivering the best care to patients with pituitary tumours and other sellar lesions, including craniopharyngiomas or Rathke’s cleft cysts, has led to the implementation of Pituitary MDT/PTCOE. Pituitary MDT/PTCOE are now widely recommended by different guidelines and medical societies relevant in the field [2,10,11,22,23]. The definition criteria of PTCOE have been proposed [10], and further validated in a survey of several internationally recognised tertiary centres [11]. Organising and delivering multidisciplinary management by experienced pituitary neurosurgeons and endocrinologists, with the support of other key specialists, is critical to the definition of Pituitary MDT/PTCOE [10,11,12].
Management of patients with pituitary diseases has much improved since the implementation of PTCOE, or Pituitary MDT, with a “patient-centric” philosophy where the patient is at the core of its mission, and all activities and goals are aimed at improving the patient’s experience and outcomes [2,10]. The mission and main clinical goals of the Pituitary MDT/PTCOE are summarised in Table 1. Ultimately, the key goal is to eliminate, or at least reduce, the excess morbidity and mortality due to pituitary tumours, pituitary hypersecretion syndromes, and other disorders affecting the pituitary, as well as manage the anterior or posterior pituitary hormone deficiencies [8,10,11,24,25,26,27,28,29,30,31]. For most patients, this requires the establishment of a complex program of care and the need for long-term follow-up [10,11].

Table 1.
Mission and main clinical goals of the Pituitary Multidisciplinary Team (MDT)/Pituitary Tumour Centres of Excellence (PTCOE).
3. Benefits of the Pituitary MDT/PTCOE
As in other cancers, the dissemination of Pituitary MDT accompanied the improvement of the standards of care and outcomes of pituitary tumour patients over recent years [32,33,34], and it has relied on the notion of being beneficial for patients and healthcare systems, while there has been little evidence supporting their establishment. MDT benefits are partly attributable to better engagement of the relevant medical specialties involved in the management of such patients, while close collaboration prevents complications and facilitates the utilisation of the latest developments, guidelines, and technologies [2,35]. On the other hand, Pituitary MDT for healthcare professionals may be beneficial for professional fulfillment, and may result in closer relationships between different specialists and the development of new skills, knowledge, and learning opportunities while providing some medico-legal protection [3]. Although substantive evidence is still limited, few studies comparing the outcomes of patients treated before and after the implementation of Pituitary MDT (Table 2) highlight some of the benefits [2,36,37].

Table 2.
Overview of the studies comparing the outcomes/complications of patients with pituitary diseases treated before and after implementing of a Pituitary MDT or multidisciplinary protocols.
Grayson and coworkers showed that since the introduction of a Pituitary MDT there has been a reduction in inpatient hospital days, transient diabetes insipidus, a syndrome of inappropriate antidiuretic hormone, hypothyroidism, an unexpected residual tumor, and peri- and post-operative complications [2]. Previously, Carminucci et al. reported that the introduction of Pituitary MDT reduced the length of hospital stay post-operatively from a median of 3 to 2 days without compromising outcomes [37]. Other studies showed that post-operative follow-up by an endocrinologist reduced the risk of 30-day readmission after surgery [38,39]. Cerebrospinal fluid leakage rates after transsphenoidal surgery have decreased since the introduction of a multidisciplinary surgical skull base team in a high-volume Swedish centre [40]. Pituitary MDT benefits have also been highlighted in a series of four women with sellar lesions during pregnancy [41]. Benjamin et al. assessed the cost effectiveness of a post-operative protocol after resection of pituitary tumours implemented by their MDT, concluding that there was a significant cost reduction in laboratory studies (of USD 255.95 per patient); there was also a decrease in the number of patients treated with desmopressin post-operatively after the protocol implementation [36]. Such MDT-based protocols may reduce hospital stays and readmissions, and improve the outcomes and safety of surgical patients [36,37,42,43].
The multidisciplinary management of functioning pituitary tumours, including prolactin, growth hormone (GH)- or adrenocorticotropic hormone (ACTH)-secreting tumours, is crucial for improving clinical outcomes and the prognosis of patients [22,23,44,45,46,47,48]. Experienced neurosurgeons working in Pituitary MDT/PTCOE have better results [49,50,51,52]. Pituitary neurosurgeons achieve higher rates of biochemical cure in acromegaly or Cushing’s disease [51,53,54,55,56,57,58,59]. Moreover, the expertise of neurosurgeons and endocrinologists is crucial in reducing post-operative complications and decreasing the length of hospital stay after operation [33,37], as shown in a surgical series for Cushing’s disease [34].
4. Characteristics, Composition and Requirements of the Pituitary MDT/PTCOE
The features, structure, and mode of operation of the MDT vary across the globe and across different conditions [1,2]. Pituitary MDT/PTCOE have only been implemented in recent years; thus, formal definitions are still controversial. However, defining the scope and structure of Pituitary MDT/PTCOE has been addressed by relevant societies in the field, including the Pituitary Society [10,11], and the European Reference Network on Rare Endocrine Conditions (Endo-ERN) [26,27].
The endo-ERN subthematic group of hypothalamic and pituitary conditions is based on different MDT and diagnostic and treatment approaches in three key domains: pituitary tumours, congenital hypopituitarism, and acquired hypopituitarism [26,27]. The general characteristics of a Pituitary MDT/PTCOE as defined by the Pituitary Society includes: (i) provide the best care for pituitary tumour patients and pituitary/sellar related disorders; (ii) be independent from health authorities, administrations and for-profit organisations; (iii) be recognised amongst endocrinologists and pituitary surgeons locally, nationally and/or internationally within the endocrine and neurosurgical communities and societies; (iv) advance the science and knowledge in the field of pituitary; (v) provide adequate patient education and community outreach; and (vi) serve as training centre for doctors aiming to specialise in the diagnosis and treatment of pituitary diseases [10].
The general structure of a Pituitary MDT/PTCOE relies on a core team composed of experienced pituitary neurosurgeons and endocrinologists (leading team), supported by specialists in other areas, including neuroradiologists, neuropathologists, neuro-ophthalmologists, otorhinolaryngologists, radiation oncologists, and endocrine nurses [10,60]. More recently, the involvement of neuro-oncologists has also been suggested (Figure 1) [12].
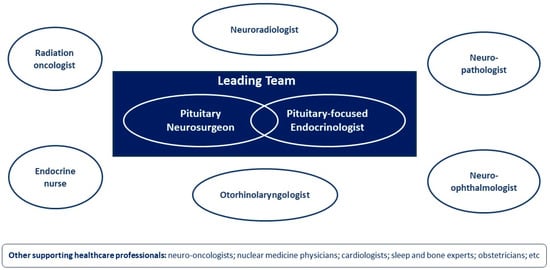
Figure 1.
General composition of a Pituitary Multidisciplinary Team (MDT)/Pituitary Tumour Centres of Excellence (PTCOE).
4.1. Pituitary Neurosurgeons and Neurosurgery Units
Despite recent advances in medical therapy, surgery remains the first choice for pituitary tumours, except for prolactinomas, where dopamine agonists are recommended as primary treatment. Thus, it is unquestionable that the Pituitary MDT/PTCOE depends on an experienced neurosurgeon able to perform endonasal transsphenoidal or transcranial surgical approaches effectively and safely [10,50]. Surgery is the most effective procedure for acromegaly, Cushing’s disease, thyrotrophinomas, resistant prolactinomas, and non-functioning pituitary tumours causing mass effects. It is also recommended for selected cases of apoplexy, Rathke’s cleft cysts, or craniopharyngiomas [10].
Being an excellent pituitary neurosurgeon requires solid training and knowledge of the hypothalamic-pituitary and skull base anatomy and physiology, plus continuous practice in a high-volume centre to maintain the expertise. Basic knowledge of neurosurgery relies on a residency program that should cover all neurosurgery-related fields, and not only pituitary [61,62]. Such programs provide limited experience in transsphenoidal pituitary surgery due to the small number of surgeries per year in most centres, as well as insufficient interaction with endocrinologists and other specialists in the Pituitary MDT, which in turn does not allow graduates to obtain enough experience to manage pituitary tumour patients after completing the residency [10,63]. Thus, after the residency, a neurosurgeon seeking to specialise in pituitary should have an additional postgraduate fellowship at an excellent high-volume centre [10,50].
Experienced pituitary neurosurgeons have better outcomes and fewer (and less severe) complications; hence, the number of surgeries performed per year on a continuous basis in a high-volume centre is critical [49,51,52,53,54,55,64,65]. A typical high-volume centre should encounter more than 1000 patients with pituitary diseases per year, with 850 being regarded as the minimal threshold. As defining criteria for a PTCOE, it has been considered 100 pituitary operations per centre per year as the preferred threshold, although 50 surgeries/year are acceptable [11]. Acute post-operative complications, including mortality and readmission rates, should preferably be negligible or nonexistent, with a preferred and acceptable criterion being respectively <2% and <10% of operated patients with complications requiring readmission [11]. However, the reality across European neurosurgical centres is far from such recommendations, with a recent study showing that only 8% of the centres perform more than 100 surgeries per year, whereas more than 40% of centres operate less than 30 patients per year [63]; moreover, most centres operate only 1–5 hormone-secreting tumours per year [66].
The surgeon workload depends on the population size served by the centre and on the number of surgeons existing in the centre. The ideal number of pituitary neurosurgeons per centre has been proposed as 3. However, one surgeon may be acceptable, but this scenario may lead to several issues, such as the centre will be uncovered when that surgeon is absent, the training of fellows may be more difficult, and performing research projects may be impeded or biased [10,11,50]. To avoid these problems while ensuring sufficient workload, the population covered by the centre may be expanded instead of reducing the number of surgeons performing pituitary surgeries; alternatively, neurosurgeons available in a certain region can be concentrated in a single centre [10,11,50]. The preferred population size per PTCOE has been suggested as 3.7 million, while a population of 1.5 million may be acceptable [11]. However, a previous study assessing the optimal numerosity of the referral population defined a PTCOE as a centre where a surgeon would serve a population of at least 9.5 million, which was the size allowing the minimal surgical experience threshold to be reached within 1 years’ time [50].
4.2. Endocrinologists and Endocrine Units
Endocrinologists provide high-quality, timely, cost-effective, equitable, accessible, and culturally sensitive health care to patients with endocrine disorders while taking part in the education of patients, families, communities, and authorities to ensure adequate health literacy and decisions/policies [67,68]. Pituitary-focused endocrinologists are crucial to the Pituitary MDT/PTCOE and play a key “holistic” role in the diagnosis, treatment, and follow-up of patients with pituitary disorders. The challenges of pituitary tumours are not only of a surgical nature but encompass a wide range of other issues, such as long-term management of the tumour, treatment-related secondary effects, including hypopituitarism, or diabetes insipidus, and/or morbidity and mortality associated with hormone hypersecretion. Moreover, many pituitary disorders are primarily managed by endocrinologists, such as prolactinomas, congenital hypopituitarism, or acquired hypopituitarism (e.g., after trauma or radiotherapy). Endocrinologists are also crucial in providing support in peri- and post-operative settings, specifically in hormone replacement and water–sodium imbalances [2,10,11,23,39,42,47,69].
Dedicated endocrinologists participating in the Pituitary MDT/PTCOE should have received basic training in internal medicine and endocrinology through the residency, and then performed postgraduate training for at least 12 months in a pituitary tertiary centre. Key skills and competences of a pituitary-focused endocrinologist include: experience in evaluating and managing patients with pituitary diseases, namely those that may impose challenges in the differential diagnosis [46,70,71,72]; thorough knowledge of the laboratory techniques for hormone analysis and capacity to interpret results, including those from dynamic testing; ability to interpret pituitary magnetic resonance imaging (MRI); understand the basics of pituitary pathology [8,73]; awareness of the new developments in the pituitary field in terms of molecular/genetic testing, and in treatment options [28,29]; participation in scientific meetings, and in national or international surveys and registries [27,74,75,76]; willingness to present results at scientific meetings, and advance pituitary science by conducting research, publishing on peer-reviewed journals or textbooks [10,11,42].
The criteria to define the expertise of a pituitary-focused endocrinologist/endocrine unit in an MDT/PTCOE may be more difficult to establish than for pituitary neurosurgeons. However, a recent study encompassing nine PTCOEs highlighted some aspects. The median number of pituitary-focused endocrinologists was 6, ranging from 4 up to a maximum of 17, and the median number of patients managed by the endocrine unit annually was estimated at 1403, varying from 855 up to 1874 patients. These data led to the recommendation of including 6 pituitary-dedicated endocrinologists (4 acceptable) in a Pituitary MDT/PTCOE, overseeing a total of patients that should not be lower than 850 (preferably 1400 patients) [11]. The number of dynamic tests performed by each endocrine unit ranged from 342 up to 4230 (median of 1335) [11].
4.3. Neuroradiologists and Radiology Units
MRI is the primary imaging modality for the pituitary gland. An experienced neuroradiologist with deep knowledge of the normal anatomy and MRI appearance of the normal pituitary and hypothalamic regions, as well as of pituitary tumours, neoplasms other than pituitary tumours, pituitary tumour-mimicking lesions, and inflammatory/infiltrative stalk processes, is crucial to the Pituitary MDT/PTCOE [77,78]. At least one dedicated neuroradiologist should exist in a Pituitary MDT/PTCOE, although 7 may be preferred [11].
The optimal MRI technique relies on thin section T1-weighted sequences in the sagittal and coronal planes before and after gadolinium contrast enhancement; T2-weighted sequences may add useful information in some cases but do not substitute for T1-weighted sequences [79]. A high-field MRI machine with at least 1.5T (or above) and high-resolution should be available at the radiology unit [10,11]. The centre should have access to digital subtraction angiography and bilateral venous sampling of the inferior petrosal sinus, which is critical for many cases of ACTH-dependent Cushing’s syndrome [10,11,46]. The median annual number of pituitary MRI scans and inferior petrosal sinus sampling reported by 9 PTCOE were respectively 810 (range: 125–3411) and 3 (range: 0–20) [11].
4.4. Neuropathologists and Pathology Units
Pathology is essential for the diagnosis, management, and follow-up of patients with pituitary tumours and related disorders; thus, one dedicated neuropathologist (preferably three) should be included in the Pituitary MDT/PTCOE [11]. The pathological assessment is crucial to establishing the final diagnosis, and may help guide or determine response to treatment, particularly with the emergence of new molecular biomarkers and targeted therapies [7,28,80,81], as well as in predicting the patient’s prognosis [82,83]. Pathology is key for the differential diagnosis of non-pituitary neoplasms, such as Rathke’s cleft cysts, craniopharyngiomas, pituicytomas, spindle cell oncocytomas, granular cell tumours, meningiomas, or germinomas. Pathology can also establish the diagnosis of infiltrative disorders, such as lymphocytic hypophysitis or Langerhans cell histiocytosis [84].
One or two experienced neuropathologists should be integrated into the Pituitary MDT/PTCOE and provide the final diagnosis for each case using the most updated WHO guidelines [8]. Routine assessment should include information concerning pleomorphism, giant cells, inclusions, inflammatory changes, stroma, hemorrhage, vascular features, granulation patterns, Ki-67, mitotic count, staining for pituitary hormones and transcription factors, and in selected cases, alpha subunit, chromogranin, P53, hormone receptors, or somatostatin receptors [8,10,11].
4.5. Neuro-Ophthalmologists and Ophthalmology Units
Dedicated neuro-ophthalmologists are required for the diagnosis and follow-up of visual impairment in patients with pituitary tumours; thus, it is recommended to include one neuro-ophthalmologist (preferably two) in the Pituitary MDT/PTCOE [11]. A pre-operative evaluation should be offered to patients with visual symptoms or tumours compressing the optic chiasma, and typically include examination of visual acuity, pupil and ocular motility, eye fundus, automated perimetry, and optical coherence tomography [42,85].
A complete neuro-ophthalmological examination may help predict the likelihood of visual acuity and visual field deficit improvement, which may occur in 68% and 81% of patients undergoing pituitary tumour resection [86]. Such examination is often useful in establishing the need and urgency of the operation in patients with large tumours, as well as to assess visual outcomes after surgery [42,87,88]. Moreover, a careful examination may identify other causes of visual impairment, such as cataracts, preventing unnecessary pituitary operations or superfluous cataract surgeries [89]. Neuro-ophthalmologists are also essential in the follow-up of pregnant women with macroprolactinomas [90].
4.6. Otorhinolaryngologist and Otorhinolaryngology Units
Otorhinolaryngologists are not widely involved in Pituitary MDT/PTCOE, and there is considerable variability regarding their participation among different centres. In 29 of 60 (48.4%) German neurosurgical centres, otorhinolaryngologists are never involved in pituitary surgeries, whereas in only 8 centres (13.3%) surgeries are always performed together with an otorhinolaryngologist [91]. Nevertheless, the collaboration between pituitary neurosurgeons and otorhinolaryngologists during endonasal and other skull base surgical approaches is of extreme value, allowing higher tumour resection rates and fewer post-operative complications, particularly cerebrospinal fluid leakages [39,40,92,93].
Pre-operative assessment by an otorhinolaryngologist is important considering that the surgical approach to the sella is typically performed endonasally (through the nostrils). Hence, anticipating anatomical difficulties or nasal pathologies is relevant for better surgical planning. Moreover, the evaluation of symptoms such as nasal obstruction, rhinorrhoea, or hyposmia, as well as the performance of other tests including nasofibroscopy, nasal function tests, rhinometry, rhinomanometry, and smell tests, may be useful in some cases. Most patients will benefit from endonasal post-operative care, such as crust removal or minor procedures to speed up healing processes and obtain a faster return to a normal quality of life regarding breathing and smelling. Also, these observations should allow early diagnosis of complications such as cerebrospinal fluid leak, sinusitis, reconstruction flap necrosis, or mucocele [42].
4.7. Radiation Neuro-Oncologists and Radiotherapy Units
Radiation therapy may be needed to treat pituitary tumour remnants or functioning tumours resistant to medical treatment, as well as other parasellar tumours such as craniopharyngiomas or meningiomas; patients refusing or with contra-indications to surgery may also be eligible for primary irradiation treatment [94,95,96,97,98]. Radiation neuro-oncologists or radiotherapists managing patients with pituitary tumours must have a deep knowledge of the tolerance of the optic system, cranial nerves in the cavernous sinus, temporal lobes, and normal pituitary, and should be available in the Pituitary MDT/PTCOE [10,11].
In a survey across 9 PTCOE, it was reported that there was a median number of radiotherapists/radiation oncologists of 3 (range: 2–5), and a relatively low median number of stereotactic radiotherapy and radiosurgery interventions on an annual basis of respectively 5.3 (range: 2–35) and 4.3 (range: 0–60), while conventional radiotherapy was almost fully abandoned [11], likely due to the negative risk:benefit ratio, particularly when compared to newer and more effective techniques [99]. Computer-assisted irradiation techniques should be available at centres of excellence as they remain important tools for selected cases, with rates of local control at 5 years estimated at 94–97% in patients with non-functioning tumour remnants [96], and a likelihood of 50–75% in controlling hormone excess in acromegaly or Cushing’s disease [94,100,101,102].
4.8. Other Healthcare Professionals and Units
Recently, the inclusion of neuro-oncologists in the Pituitary MDT/PTCOE has been advocated based on recent molecular and therapeutic advancements, in particular the emergence of new systemic therapies for aggressive or metastatic pituitary tumours such as temozolomide, tyrosine kinase inhibitors, mTOR inhibitors, bevacizumab, or immune checkpoint inhibitors [12]. A median of 3 neuro-oncologists (range: 1–30) have been recently self-reported by 9 PTCOE [11].
Pituitary MDT/PTCOE should include at least one endocrine nurse (preferably 3) [11], considering the importance of nursing care in the pre-, peri-, and post-operative management of pituitary tumour patients, as well as in the long-term follow-up and education of patients with hypopituitarism [10,11,103]. Endocrine nurses are key in facilitating communication between patients and clinicians [104,105]. However, in some pituitary tumour centres of excellence, there are no nurses available [11].
There is an emerging role for nuclear medicine in the management of pituitary tumours. Positron emission tomography-computed tomography (PET-CT) with 18F-fluorodeoxyglucose may be helpful for differential diagnosis and pre-operative characterization of some sellar lesions. Other tracers are currently used in the pituitary setting [23]. PET-CT with 68Ga-labeled somatostatin analogues may localize and determine response to surgical, medical, or radiation treatment, as well as aid in selecting aggressive or metastatic pituitary cases suitable for peptide receptor radionuclide therapy [31]. PET-CT with 11carbon-methionine plays an important role in identifying a target not visible (or equivocal) on MRI that might be amenable for surgery or radiotherapy [106,107,108].
Other collaborating medical specialties may be involved in the care of pituitary tumour patients, such as cardiologists, sleep experts, and bone experts, particularly in syndromes related to pituitary hormone excess such as acromegaly or Cushing’s disease [11]. Gynaecologists, and obstetricians might also be crucial in managing cases of pregnant women with pituitary tumours or other sellar lesions [41,109].
5. Barriers to the Pituitary MDT/PTCOE
Although the best care model for pituitary tumour patients relies on the Pituitary MDT/PTCOE, its application in the real world often encounters several barriers. Data from a large survey study including 254 neurosurgical centres performing pituitary surgeries across 34 European countries showed that regular pituitary board meetings were held in only 56.3% of them [63]. Hence, more needs to be done to overcome such barriers and to widely implement Pituitary MDT/PTCOE across healthcare systems.
The MDT model is associated with marked consumption of time and resources, and significant costs [3]. In the UK, the estimated cost to the health system of a 2 h monthly Pituitary MDT meeting ranges from £9000 up to £12,000 per year [2]. While such direct costs are easier to calculate based on the time spent and number of physicians involved in such meetings, the indirect financial benefits and cost-effectiveness for high-quality decision making and more efficacious management of pituitary tumours are more difficult to assess, and remain poorly described [2,110]. Recent studies showed that the creation of a Pituitary MDT reduced inpatient hospital days [2,37], decreased post-operative complications [2,40], lowered the risk of readmission after surgery [39], and reduced costs in laboratory studies [36], while at the same time improving clinical outcomes [36,37,42,43]. Multidisciplinary management of patients with functioning tumours achieves higher rates of biochemical cure [51,53,54,55,56,57,58,59], allowing significant savings in terms of their long-term management associated with the costs of medications to treat hormone excess in persistent or recurrent disease. In acromegaly, the costs of somatostatin analogue therapy range between EUR 7900–19,800 per patient depending on dose and country, whereas the annual cost for pegvisomant treatment per patient may vary between EUR 28,300–84,900 in Europe, or be higher than USD 100,000 in the United States [111,112,113]. Also, there is a financial burden associated with the management of pituitary hormone excess-related comorbidities, such as diabetes, hypertension, cardiovascular disease, or mental illness [112,114,115,116,117]. Thus, efficacious and cost-effective care for pituitary tumour patients reduces costs, leading to significant savings aspects often overlooked in the discussions around the Pituitary MDT/PTCOE.
Efficient communication between the different healthcare professionals involved in an MDT is crucial. The creation of a non-hierarchical and collaborative highly specialised environment, the presentation of the case in a concise and high-quality manner, scheduling structured meetings on a regular basis (once a week, biweekly or monthly, depending on the volume of cases in the centre), and ensuring these meetings are always well-attended by the core members, are key factors for the success of a Pituitary MDT/PTCOE [1,3,10]. The establishment of local guidelines or institutional protocols, and the maintenance of local registries and electronic clinical files are important tools to monitor outcomes and improve when necessary, while also providing a reliable tool to conduct research and communicate scientific results [10].
Another barrier to optimal care for pituitary patients is that health care systems are often too fragmented, lack clinical information capabilities, duplicate services, are not properly designed for chronic care, and may be challenging to modify. In some institutions, the initiatives by endocrinologists or administrators to concentrate procedures on a single neurosurgeon may encounter firm opposition in the Neurosurgery department, situation unlikely to be modifiable given the lack of external guidelines or policies endorsed by authoritative bodies [10]. Moreover, small groups or groups that perform poorly never present or publish their results, thus making it difficult to run audits or independent assessments, which in turn, may also impact scientific advancements [10,27]. There are also demographic factors and disparities related to payer status, insurance, admission types, or geography, imposing barriers to high-quality care that must be overcome to improve the access of patients to centres of excellence [118].
6. Perspectives of the Different Specialists Involved in our Pituitary MDT
In order to provide additional insights and reflections around this topic from the different medical specialists involved in our Pituitary MDT, we answered two questions: (i) What is the major contribution that your specialty can provide to the Pituitary MDT? (ii) What are the major contributions that other specialties can provide to your clinical practice when managing a pituitary tumour patient? Replies to each question can be found in Supplementary Tables S1 and S2. Overall, the main message emerging from the replies is that this interdisciplinary and collaborative teamwork between the different specialists is crucial for the best decision-making process and delivering high-quality and effective treatment to patients with pituitary diseases.
7. Conclusions
The optimal care for patients with pituitary tumours is best provided in a multidisciplinary and collaborative environment, which requires the contribution of multiple medical specialties working together within the scope of a Pituitary MDT/PTCOE. There are several benefits to providing care to pituitary tumour patients through the pituitary MDT/PTCOE, and this model of delivering care is highly recommended by all relevant societies and international guidelines in the pituitary field.
Pituitary neurosurgeons and pituitary-focused endocrinologists are normally the leading specialties in the Pituitary MDT and should be supported by other specialties with significant contributions to the diagnosis and management of pituitary diseases, including neuropathology, neuroradiology, neuro-ophthalmology, otorhinolaryngology, and radiation neuro-oncologists, among others. Despite the barriers that may arise when setting up a Pituitary MDT/PTCOE, efforts should be made to overcome them, aiming to deliver high-quality, cost-effective, and safe medical care for all patients with pituitary disorders.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers16050950/s1, Table S1: The perspectives of different specialists involved in our Pituitary MDT regarding the question “What is the major contribution that your specialty can provide to the Pituitary Multidisciplinary Team?”; Table S2: The perspectives of different specialists involved in our Pituitary MDT regarding the question “What are the major contributions that other specialties can provide to your clinical practice when managing a pituitary tumour patient?”.
Author Contributions
P.M., A.S., F.T., L.N., J.T.F., J.S., A.P., D.D. and I.S. contributed to the literature review, manuscript draft preparation, and revision of the final version. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Anokwute, M.C.; Preda, V.; Di Ieva, A. Determining Contemporary Barriers to Effective Multidisciplinary Team Meetings in Neurological Surgery: A Review of the Literature. World Neurosurg. 2023, 172, 73–80. [Google Scholar] [CrossRef]
- Grayson, J.W.; Nayak, A.; Winder, M.; Jonker, B.; Alvarado, R.; Barham, H.; McCormack, A.; Harvey, R.J. Multidisciplinary Team Care in the Surgical Management of Pituitary Adenoma. J. Neurol. Surg. B Skull Base 2021, 82, 295–302. [Google Scholar] [CrossRef]
- Walraven, J.E.W.; van der Hel, O.L.; van der Hoeven, J.J.M.; Lemmens, V.; Verhoeven, R.H.A.; Desar, I.M.E. Factors influencing the quality and functioning of oncological multidisciplinary team meetings: Results of a systematic review. BMC Health Serv. Res. 2022, 22, 829. [Google Scholar] [CrossRef]
- Meij, B.P.; Lopes, M.B.; Ellegala, D.B.; Alden, T.D.; Laws, E.R., Jr. The long-term significance of microscopic dural invasion in 354 patients with pituitary adenomas treated with transsphenoidal surgery. J. Neurosurg. 2002, 96, 195–208. [Google Scholar] [CrossRef]
- Zada, G.; Woodmansee, W.W.; Ramkissoon, S.; Amadio, J.; Nose, V.; Laws, E.R., Jr. Atypical pituitary adenomas: Incidence, clinical characteristics, and implications. J. Neurosurg. 2011, 114, 336–344. [Google Scholar] [CrossRef]
- Melmed, S.; Kaiser, U.B.; Lopes, M.B.; Bertherat, J.; Syro, L.V.; Raverot, G.; Reincke, M.; Johannsson, G.; Beckers, A.; Fleseriu, M.; et al. Clinical Biology of the Pituitary Adenoma. Endocr. Rev. 2022, 43, 1003–1037. [Google Scholar] [CrossRef]
- Raverot, G.; Ilie, M.D.; Lasolle, H.; Amodru, V.; Trouillas, J.; Castinetti, F.; Brue, T. Aggressive pituitary tumours and pituitary carcinomas. Nat. Rev. Endocrinol. 2021, 17, 671–684. [Google Scholar] [CrossRef] [PubMed]
- Asa, S.L.; Mete, O.; Perry, A.; Osamura, R.Y. Overview of the 2022 WHO Classification of Pituitary Tumors. Endocr. Pathol. 2022, 33, 6–26. [Google Scholar] [CrossRef] [PubMed]
- Marques, P.; Korbonits, M. Genetic Aspects of Pituitary Adenomas. Endocrinol. Metab. Clin. N. Am. 2017, 46, 335–374. [Google Scholar] [CrossRef]
- Casanueva, F.F.; Barkan, A.L.; Buchfelder, M.; Klibanski, A.; Laws, E.R.; Loeffler, J.S.; Melmed, S.; Mortini, P.; Wass, J.; Giustina, A.; et al. Criteria for the definition of Pituitary Tumor Centers of Excellence (PTCOE): A Pituitary Society Statement. Pituitary. 2017, 20, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Giustina, A.; Uygur, M.M.; Frara, S.; Barkan, A.; Biermasz, N.R.; Chanson, P.; Freda, P.; Gadelha, M.; Kaiser, U.B.; Lamberts, S.; et al. Pilot study to define criteria for Pituitary Tumors Centers of Excellence (PTCOE): Results of an audit of leading international centers. Pituitary 2023, 26, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Jouanneau, E.; Calvanese, F.; Ducray, F.; Raverot, G. Pituitary Tumor Centers of Excellence (PTCOE) should now include neuro-oncologic input. Pituitary 2023, 26, 642–643. [Google Scholar] [CrossRef] [PubMed]
- Fountas, A.; Hamblin, R.; Criseno, S.; Karavitaki, N. Chapter 51-Multidisciplinary team perspective: A model of care for patients with pituitary tumors. In Pituitary Tumors: A Comprehensive and Interdisciplinary Approach; Academic Press: Cambridge, MA, USA, 2021; pp. 679–685. [Google Scholar]
- Selwyn, A.; Davis, J.; Hone, R. The United Kingdom thyroid multi-disciplinary team: A national survey of services and comparison to guidelines. Clin. Otolaryngol. 2022, 47, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Wesson, D.E.; Johnson, B.L.; Barclay, C.; Vogel, A.M.; Chelius, D.C.; Dimachkieh, A.L.; Athanassaki, I.D.; Karaviti, L.P.; Sher, A.C.; Hernandez, J.A.; et al. Thyroid surgery outcomes at a children’s hospital: The value of a multidisciplinary team approach. J. Pediatr. Surg. 2022, 57, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Champion, J.K.; Pories, W.J. Centers of Excellence for Bariatric Surgery. Surg. Obes. Relat. Dis. 2005, 1, 148–151. [Google Scholar] [CrossRef]
- de Weerd, L.; Weum, S.; Florholmen, J. A multidisciplinary team for treatment of patients with morbid obesity should include a plastic surgeon. Eur. J. Intern. Med. 2009, 20, e19. [Google Scholar] [CrossRef]
- Pratt, G.M.; McLees, B.; Pories, W.J. The ASBS Bariatric Surgery Centers of Excellence program: A blueprint for quality improvement. Surg. Obes. Relat. Dis. 2006, 2, 497–503; discussion 503. [Google Scholar] [CrossRef]
- Cai, J.; Islam, M.S. Interventions incorporating a multi-disciplinary team approach and a dedicated care team can help reduce preventable hospital readmissions of people with type 2 diabetes mellitus: A scoping review of current literature. Diabet Med. 2023, 40, e14957. [Google Scholar] [CrossRef]
- Taieb, A.; Gaelle, L.; Roxane, D.; Perrine, W.; Marion, A.; Fleur, B.; Zoe, L.; Aurelie, L.; Solen, D.; Patricia, D.; et al. Efficiency of a multidisciplinary team care approach through a short hospitalization of patients with poorly controlled diabetes mellitus: A 12 months prospective monocentric study. Pan. Afr. Med. J. 2022, 41, 192. [Google Scholar]
- Metz, D.C.; Choi, J.; Strosberg, J.; Heaney, A.P.; Howden, C.W.; Klimstra, D.; Yao, J.C. A rationale for multidisciplinary care in treating neuroendocrine tumours. Curr. Opin. Endocrinol. Diabetes Obes. 2012, 19, 306–313. [Google Scholar] [CrossRef]
- Raverot, G.; Burman, P.; McCormack, A.; Heaney, A.; Petersenn, S.; Popovic, V.; Trouillas, J.; Dekkers, O.M.; European Society of Endocrinology. European Society of Endocrinology Clinical Practice Guidelines for the management of aggressive pituitary tumours and carcinomas. Eur. J. Endocrinol. 2018, 178, G1–G24. [Google Scholar] [CrossRef]
- Bianchi, A.; Chiloiro, S.; Giampietro, A.; Gaudino, S.; Calandrelli, R.; Mazzarella, C.; Caldarella, C.; Rigante, M.; Gessi, M.; Lauretti, L.; et al. Multidisciplinary management of difficult/aggressive growth-hormone pituitary neuro-endocrine tumors. Front. Endocrinol. 2023, 14, 1123267. [Google Scholar] [CrossRef] [PubMed]
- Gheorghe, A.M.; Trandafir, A.I.; Ionovici, N.; Carsote, M.; Nistor, C.; Popa, F.L.; Stanciu, M. Pituitary Apoplexy in Patients with Pituitary Neuroendocrine Tumors (PitNET). Biomedicines 2023, 11, 680. [Google Scholar] [CrossRef] [PubMed]
- Pekic, S.; Miljic, D.; Popovic, V. Infections of the Hypothalamic-Pituitary Region. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Pereira, A.M.; Hiort, O. Introduction to Endo-ERN-scope and mission. Endocrine 2021, 71, 537–538. [Google Scholar] [CrossRef] [PubMed]
- Zamanipoor Najafabadi, A.H.; van der Meulen, M.; Priego Zurita, A.L.; Faisal Ahmed, S.; van Furth, W.R.; Charmandari, E.; Hiort, O.; Pereira, A.M.; Dattani, M.; Vitali, D.; et al. Starting point for benchmarking outcomes and reporting of pituitary adenoma surgery within the European Reference Network on Rare Endocrine Conditions (Endo-ERN): Results from a meta-analysis and survey study. Endocr. Connect. 2023, 12, e220349. [Google Scholar] [CrossRef] [PubMed]
- Ilie, M.D.; Vasiljevic, A.; Bertolino, P.; Raverot, G. Biological and Therapeutic Implications of the Tumor Microenvironment in Pituitary Adenomas. Endocr. Rev. 2022, 44, 297–311. [Google Scholar] [CrossRef] [PubMed]
- Ilie, M.D.; Vasiljevic, A.; Jouanneau, E.; Raverot, G. Immunotherapy in aggressive pituitary tumors and carcinomas: A systematic review. Endocr. Relat. Cancer 2022, 29, 415–426. [Google Scholar] [CrossRef]
- Khan, D.Z.; Hanrahan, J.G.; Baldeweg, S.E.; Dorward, N.L.; Stoyanov, D.; Marcus, H.J. Current and Future Advances in Surgical Therapy for Pituitary Adenoma. Endocr. Rev. 2023, 44, 947–959. [Google Scholar] [CrossRef]
- Marques, P. The Effects of Peptide Receptor Radionuclide Therapy on the Neoplastic and Normal Pituitary. Cancers 2023, 15, 2710. [Google Scholar] [CrossRef] [PubMed]
- Villwock, J.A.; Villwock, M.; Deshaies, E.; Goyal, P. Significant increases of pituitary tumors and resections from 1993 to 2011. Int. Forum. Allergy Rhinol. 2014, 4, 767–770. [Google Scholar] [CrossRef]
- Barker, F.G., 2nd; Klibanski, A.; Swearingen, B. Transsphenoidal surgery for pituitary tumors in the United States, 1996–2000: Mortality, morbidity, and the effects of hospital and surgeon volume. J. Clin. Endocrinol. Metab. 2003, 88, 4709–4719. [Google Scholar] [CrossRef]
- Patil, C.G.; Lad, S.P.; Harsh, G.R.; Laws, E.R., Jr.; Boakye, M. National trends, complications, and outcomes following transsphenoidal surgery for Cushing’s disease from 1993 to 2002. Neurosurg. Focus 2007, 23, E7. [Google Scholar] [CrossRef]
- Iacovazzo, D.; Bianchi, A.; Lugli, F.; Milardi, D.; Giampietro, A.; Lucci-Cordisco, E.; Doglietto, F.; Lauriola, L.; De Marinis, L. Double pituitary adenomas. Endocrine 2013, 43, 452–457. [Google Scholar] [CrossRef]
- Benjamin, C.G.; Dastagirzada, Y.; Bevilacqua, J.; Kurland, D.B.; Fujita, K.; Sen, C.; Golfinos, J.G.; Placantonakis, D.G.; Jafar, J.J.; Lieberman, S.; et al. The Cost Effectiveness of Implementation of a Postoperative Endocrinopathy Management Protocol after Resection of Pituitary Adenomas. J. Neurol. Surg. B Skull Base 2022, 83, 618–625. [Google Scholar] [CrossRef]
- Carminucci, A.S.; Ausiello, J.C.; Page-Wilson, G.; Lee, M.; Good, L.; Bruce, J.N.; Freda, P.U. Outcome of Implementation of a Multidisciplinary Team Approach to the Care of Patients after Transsphenoidal Surgery. Endocr. Pract. 2016, 22, 36–44. [Google Scholar] [CrossRef]
- Ghiam, M.K.; Ali, I.A.; Dable, C.L.; Ayala, A.R.; Kargi, A.Y.; Komotar, R.J.; Levine, C.G.; Sargi, Z. Multidisciplinary Postoperative Care Pathway to Reduce Readmissions following Endoscopic Transsphenoidal Pituitary Surgery: Improving Quality of Patient Care. J. Neurol. Surg. B Skull Base 2022, 83, 626–634. [Google Scholar] [CrossRef]
- Ghiam, M.K.; Chyou, D.E.; Dable, C.L.; Katz, A.P.; Eichberg, D.G.; Zhang, H.; Ayala, A.R.; Kargi, A.Y.; Komotar, R.J.; Sargi, Z. 30-Day Readmissions and Coordination of Care Following Endoscopic Transsphenoidal Pituitary Surgery: Experience with 409 Patients. J. Neurol. Surg. B Skull Base 2022, 83 (Suppl. S2), e410–e418. [Google Scholar] [CrossRef]
- Bengtsson, O.F.; Sunnergren, O.; Segerhammar, I.; Forander, P.; Olsson, M.; Hulting, A.L.; Stjarne, P. Remission, complications, and overall survival in transsphenoidal pituitary surgery-a Swedish single-center experience of 578 patients. Acta Neurochir. 2023, 165, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Zhong, H.P.; Tang, H.; Zhang, Y.; Luo, Y.; Yao, H.; Cheng, Y.; Gu, W.T.; Wei, Y.X.; Wu, Z.B. Multidisciplinary team efforts improve the surgical outcomes of sellar region lesions during pregnancy. Endocrine 2019, 66, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Araujo-Castro, M.; Pascual-Corrales, E.; Martinez San Millan, J.; Rebolleda, G.; Pian, H.; Ruz-Caracuel, I.; De Los Santos Granados, G.; Ley Urzaiz, L.; Escobar-Morreale, H.F.; Rodriguez Berrocal, V. Multidisciplinary protocol of preoperative and surgical management of patients with pituitary tumors candidates to pituitary surgery. Ann. Endocrinol. 2021, 82, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Burke, W.T.; Cote, D.J.; Iuliano, S.I.; Zaidi, H.A.; Laws, E.R. A practical method for prevention of readmission for symptomatic hyponatremia following transsphenoidal surgery. Pituitary 2018, 21, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Fleseriu, M.; Biller, B.M.K.; Freda, P.U.; Gadelha, M.R.; Giustina, A.; Katznelson, L.; Molitch, M.E.; Samson, S.L.; Strasburger, C.J.; van der Lely, A.J.; et al. A Pituitary Society update to acromegaly management guidelines. Pituitary 2021, 24, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Nieman, L.K.; Biller, B.M.; Findling, J.W.; Murad, M.H.; Newell-Price, J.; Savage, M.O.; Tabarin, A.; Endocrine, S. Treatment of Cushing’s Syndrome: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2015, 100, 2807–2831. [Google Scholar] [CrossRef] [PubMed]
- Fleseriu, M.; Auchus, R.; Bancos, I.; Ben-Shlomo, A.; Bertherat, J.; Biermasz, N.R.; Boguszewski, C.L.; Bronstein, M.D.; Buchfelder, M.; Carmichael, J.D.; et al. Consensus on diagnosis and management of Cushing’s disease: A guideline update. Lancet Diabetes Endocrinol. 2021, 9, 847–875. [Google Scholar] [CrossRef] [PubMed]
- Petersenn, S.; Fleseriu, M.; Casanueva, F.F.; Giustina, A.; Biermasz, N.; Biller, B.M.K.; Bronstein, M.; Chanson, P.; Fukuoka, H.; Gadelha, M.; et al. Diagnosis and management of prolactin-secreting pituitary adenomas: A Pituitary Society international Consensus Statement. Nat. Rev. Endocrinol. 2023, 19, 722–740. [Google Scholar] [CrossRef]
- Giustina, A.; Barkhoudarian, G.; Beckers, A.; Ben-Shlomo, A.; Biermasz, N.; Biller, B.; Boguszewski, C.; Bolanowski, M.; Bollerslev, J.; Bonert, V.; et al. Multidisciplinary management of acromegaly: A consensus. Rev. Endocr. Metab. Disord. 2020, 21, 667–678. [Google Scholar] [CrossRef] [PubMed]
- Ciric, I.; Ragin, A.; Baumgartner, C.; Pierce, D. Complications of transsphenoidal surgery: Results of a national survey, review of the literature, and personal experience. Neurosurgery. 1997, 40, 225–236; discussion 236–237. [Google Scholar] [CrossRef]
- Mortini, P.; Nocera, G.; Roncelli, F.; Losa, M.; Formenti, A.M.; Giustina, A. The optimal numerosity of the referral population of pituitary tumors centers of excellence (PTCOE): A surgical perspective. Rev. Endocr. Metab. Disord. 2020, 21, 527–536. [Google Scholar] [CrossRef]
- Honegger, J.; Grimm, F. The experience with transsphenoidal surgery and its importance to outcomes. Pituitary 2018, 21, 545–555. [Google Scholar] [CrossRef]
- Perry, A.; Graffeo, C.S.; Meyer, J.; Carlstrom, L.P.; Oushy, S.; Driscoll, C.L.W.; Meyer, F.B. Beyond the Learning Curve: Comparison of Microscopic and Endoscopic Incidences of Internal Carotid Injury in a Series of Highly Experienced Operators. World Neurosurg. 2019, 131, e128–e135. [Google Scholar] [CrossRef]
- Bates, P.R.; Carson, M.N.; Trainer, P.J.; Wass, J.A.; Group, U.K.N.A.R.S. Wide variation in surgical outcomes for acromegaly in the UK. Clin. Endocrinol. 2008, 68, 136–142. [Google Scholar] [CrossRef]
- Erturk, E.; Tuncel, E.; Kiyici, S.; Ersoy, C.; Duran, C.; Imamoglu, S. Outcome of surgery for acromegaly performed by different surgeons: Importance of surgical experience. Pituitary 2005, 8, 93–97. [Google Scholar] [CrossRef]
- Gittoes, N.J.; Sheppard, M.C.; Johnson, A.P.; Stewart, P.M. Outcome of surgery for acromegaly—The experience of a dedicated pituitary surgeon. QJM 1999, 92, 741–745. [Google Scholar] [CrossRef]
- Lissett, C.A.; Peacey, S.R.; Laing, I.; Tetlow, L.; Davis, J.R.; Shalet, S.M. The outcome of surgery for acromegaly: The need for a specialist pituitary surgeon for all types of growth hormone (GH) secreting adenoma. Clin. Endocrinol. 1998, 49, 653–657. [Google Scholar] [CrossRef]
- Wang, Y.Y.; Higham, C.; Kearney, T.; Davis, J.R.; Trainer, P.; Gnanalingham, K.K. Acromegaly surgery in Manchester revisited--the impact of reducing surgeon numbers and the 2010 consensus guidelines for disease remission. Clin. Endocrinol. 2012, 76, 399–406. [Google Scholar] [CrossRef]
- Mancini, T.; Porcelli, T.; Giustina, A. Treatment of Cushing disease: Overview and recent findings. Ther. Clin. Risk Manag. 2010, 6, 505–516. [Google Scholar] [PubMed]
- Rees, D.A.; Hanna, F.W.; Davies, J.S.; Mills, R.G.; Vafidis, J.; Scanlon, M.F. Long-term follow-up results of transsphenoidal surgery for Cushing’s disease in a single centre using strict criteria for remission. Clin. Endocrinol. 2002, 56, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Frara, S.; Rodriguez-Carnero, G.; Formenti, A.M.; Martinez-Olmos, M.A.; Giustina, A.; Casanueva, F.F. Pituitary Tumors Centers of Excellence. Endocrinol. Metab. Clin. N. Am. 2020, 49, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Koc, K.; Anik, I.; Ozdamar, D.; Cabuk, B.; Keskin, G.; Ceylan, S. The learning curve in endoscopic pituitary surgery and our experience. Neurosurg. Rev. 2006, 29, 298–305; discussion 305. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Snyderman, C.; Kassam, A.; Carrau, R.; Mintz, A.; Gardner, P.; Prevedello, D.M. Acquisition of surgical skills for endonasal skull base surgery: A training program. Laryngoscope 2007, 117, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Netuka, D.; Grotenhuis, A.; Foroglou, N.; Zenga, F.; Froehlich, S.; Ringel, F.; Sampron, N.; Thomas, N.; Komarc, M.; Majovsky, M. Pituitary Adenoma Surgery Survey: Neurosurgical Centers and Pituitary Adenomas. Int. J. Endocrinol. 2022, 2022, 7206713. [Google Scholar] [CrossRef] [PubMed]
- Knutzen, R. Pituitary centers of excellence: For patients it is life or death. Neurosurgery 2014, 74, E143. [Google Scholar] [CrossRef]
- Jane, J.A., Jr.; Laws, E.R., Jr. The surgical management of pituitary adenomas in a series of 3093 patients. J. Am. Coll. Surg. 2001, 193, 651–659. [Google Scholar]
- Netuka, D.; Grotenhuis, A.; Foroglou, N.; Zenga, F.; Froehlich, S.; Ringel, F.; Sampron, N.; Thomas, N.; Komarc, M.; Kosak, M.; et al. Endocrinological aspects of pituitary adenoma surgery in Europe. Sci. Rep. 2022, 12, 6529. [Google Scholar] [CrossRef]
- Elders, M.J. Role of endocrinologists in eliminating health care disparities. Endocr. Pract. 2009, 15, 612–623. [Google Scholar] [CrossRef] [PubMed]
- Vigersky, R.A.; Fish, L.; Hogan, P.; Stewart, A.; Kutler, S.; Ladenson, P.W.; McDermott, M.; Hupart, K.H. The clinical endocrinology workforce: Current status and future projections of supply and demand. J. Clin. Endocrinol. Metab. 2014, 99, 3112–3121. [Google Scholar] [CrossRef] [PubMed]
- Mercado, M.; Gonzalez, B.; Vargas, G.; Ramirez, C.; de los Monteros, A.L.; Sosa, E.; Jervis, P.; Roldan, P.; Mendoza, V.; Lopez-Felix, B.; et al. Successful mortality reduction and control of comorbidities in patients with acromegaly followed at a highly specialized multidisciplinary clinic. J. Clin. Endocrinol. Metab. 2014, 99, 4438–4446. [Google Scholar] [CrossRef]
- Marques, P.; Korbonits, M. Pseudoacromegaly. Front. Neuroendocrinol. 2019, 52, 113–143. [Google Scholar] [CrossRef]
- Nieman, L.K.; Biller, B.M.; Findling, J.W.; Newell-Price, J.; Savage, M.O.; Stewart, P.M.; Montori, V.M. The diagnosis of Cushing’s syndrome: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2008, 93, 1526–1540. [Google Scholar] [CrossRef]
- Peixe, C.; Sanchez-Garcia, M.; Grossman, A.B.; Korbonits, M.; Marques, P. Biochemical discrepancies in the evaluation of the somatotroph axis: Elevated GH or IGF-1 levels do not always diagnose acromegaly. Growth Horm. IGF Res. 2022, 64, 101467. [Google Scholar] [CrossRef]
- Drummond, J.; Roncaroli, F.; Grossman, A.B.; Korbonits, M. Clinical and Pathological Aspects of Silent Pituitary Adenomas. J. Clin. Endocrinol. Metab. 2019, 104, 2473–2489. [Google Scholar] [CrossRef] [PubMed]
- Badia, X.; Roset, M.; Valassi, E.; Franz, H.; Forsythe, A.; Webb, S.M. Mapping CushingQOL scores to EQ-5D utility values using data from the European Registry on Cushing’s syndrome (ERCUSYN). Qual. Life Res. 2013, 22, 2941–2950. [Google Scholar] [CrossRef] [PubMed]
- Valassi, E. Clinical presentation and etiology of Cushing’s syndrome: Data from ERCUSYN. J. Neuroendocrinol. 2022, 34, e13114. [Google Scholar] [CrossRef] [PubMed]
- Luger, A.; Feldt-Rasmussen, U.; Abs, R.; Gaillard, R.C.; Buchfelder, M.; Trainer, P.; Brue, T. Lessons learned from 15 years of KIMS and 5 years of ACROSTUDY. Horm. Res. Paediatr. 2011, 76 (Suppl. S1), 33–38. [Google Scholar] [CrossRef]
- Tsukamoto, T.; Miki, Y. Imaging of pituitary tumors: An update with the 5th WHO Classifications-part 2. Neoplasms other than PitNET and tumor-mimicking lesions. Jpn. J. Radiol. 2023, 41, 808–829. [Google Scholar] [CrossRef]
- Tsukamoto, T.; Miki, Y. Imaging of pituitary tumors: An update with the 5th WHO Classifications-part 1. Pituitary neuroendocrine tumor (PitNET)/pituitary adenoma. Jpn. J. Radiol. 2023, 41, 789–806. [Google Scholar] [CrossRef]
- Evanson, J. Radiology of the Pituitary. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Marques, P.; Silva, A.L.; Lopez-Presa, D.; Faria, C.; Bugalho, M.J. The microenvironment of pituitary adenomas: Biological, clinical and therapeutical implications. Pituitary 2022, 25, 363–382. [Google Scholar] [CrossRef]
- Burman, P.; Casar-Borota, O.; Perez-Rivas, L.G.; Dekkers, O.M. Aggressive pituitary tumors and pituitary carcinomas: From pathology to treatment. J. Clin. Endocrinol. Metab. 2023, 108, 1585–1601. [Google Scholar] [CrossRef]
- Trouillas, J.; Roy, P.; Sturm, N.; Dantony, E.; Cortet-Rudelli, C.; Viennet, G.; Bonneville, J.F.; Assaker, R.; Auger, C.; Brue, T.; et al. A new prognostic clinicopathological classification of pituitary adenomas: A multicentric case-control study of 410 patients with 8 years post-operative follow-up. Acta Neuropathol. 2013, 126, 123–135. [Google Scholar] [CrossRef]
- Peixe, C.; Alexandre, M.I.; Gomes, A.R.; Nobre, E.; Silva, A.L.; Oliveira, T.; Lopez-Presa, D.; Faria, C.C.; Miguens, J.; Bugalho, M.J.; et al. Usefulness of a clinicopathological classification in predicting treatment-related outcomes and multimodal therapeutic approaches in pituitary adenoma patients: Retrospective analysis on a Portuguese cohort of 129 patients from a tertiary pituitary center. Pituitary 2023, 26, 352–363. [Google Scholar] [CrossRef]
- Kobalka, P.J.; Huntoon, K.; Becker, A.P. Neuropathology of Pituitary Adenomas and Sellar Lesions. Neurosurgery 2021, 88, 900–918. [Google Scholar] [CrossRef]
- Danesh-Meyer, H.V.; Wong, A.; Papchenko, T.; Matheos, K.; Stylli, S.; Nichols, A.; Frampton, C.; Daniell, M.; Savino, P.J.; Kaye, A.H. Optical coherence tomography predicts visual outcome for pituitary tumors. J. Clin. Neurosci. 2015, 22, 1098–1104. [Google Scholar] [CrossRef]
- Muskens, I.S.; Zamanipoor Najafabadi, A.H.; Briceno, V.; Lamba, N.; Senders, J.T.; van Furth, W.R.; Verstegen, M.J.T.; Smith, T.R.S.; Mekary, R.A.; Eenhorst, C.A.E.; et al. Visual outcomes after endoscopic endonasal pituitary adenoma resection: A systematic review and meta-analysis. Pituitary 2017, 20, 539–552. [Google Scholar] [CrossRef]
- Castle-Kirszbaum, M.; Wang, Y.Y.; King, J.; Goldschlager, T. Predictors of visual and endocrine outcomes after endoscopic transsphenoidal surgery for pituitary adenomas. Neurosurg. Rev. 2022, 45, 843–853. [Google Scholar] [CrossRef]
- van Essen, M.J.; Muskens, I.S.; Lamba, N.; Belunek, S.F.J.; van der Boog, A.T.J.; Amelink, G.J.; Gosselaar, P.H.; van Doormaal, T.P.C.; Stades, A.M.E.; Verhoeff, J.J.C.; et al. Visual Outcomes after Endoscopic Endonasal Transsphenoidal Resection of Pituitary Adenomas: Our Institutional Experience. J. Neurol. Surg. B Skull Base 2021, 82 (Suppl. S3), e79–e87. [Google Scholar] [CrossRef]
- Gerges, M.M.; Arnaout, M.M.; El Asri, A.C.; Cummock, M.D.; Roshdy, A.; Anand, V.K.; Dinkin, M.J.; Oliveira, C.; Schwartz, T.H. Increased frequency of cataract surgery in patients over age 50 with pituitary macroadenomas and chiasmal compression. Pituitary 2019, 22, 405–410. [Google Scholar] [CrossRef]
- Luger, A.; Broersen, L.H.A.; Biermasz, N.R.; Biller, B.M.K.; Buchfelder, M.; Chanson, P.; Jorgensen, J.O.L.; Kelestimur, F.; Llahana, S.; Maiter, D.; et al. ESE Clinical Practice Guideline on functioning and nonfunctioning pituitary adenomas in pregnancy. Eur. J. Endocrinol. 2021, 185, G1–G33. [Google Scholar] [CrossRef]
- Ottenhausen, M.; Conrad, J.; Kalasauskas, D.; Netuka, D.; Ringel, F. Pituitary Surgery in Germany-Findings from the European Pituitary Adenoma Surgery Survey. Exp. Clin. Endocrinol. Diabetes 2023, 131, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, R.; Toda, M.; Tomita, T.; Ogawa, K.; Yoshida, K. Surgical Outcome of Endoscopic Endonasal Surgery for Non-Functional Pituitary Adenoma by a Team of Neurosurgeons and Otolaryngologists Adenoma by a Team of Neurosurgeons and Otolaryngologists. Turk. Neurosurg. 2017, 27, 1–7. [Google Scholar] [PubMed]
- Fang, C.H.; Agarwal, V.; Liu, J.K.; Eloy, J.A. Overview of Pituitary Surgery. Otolaryngol. Clin. N. Am. 2022, 55, 205–221. [Google Scholar] [CrossRef] [PubMed]
- Knappe, U.J.; Petroff, D.; Quinkler, M.; Schmid, S.M.; Schofl, C.; Schopohl, J.; Stieg, M.R.; Tonjes, A.; participants of the German Acromegaly, R. Fractionated radiotherapy and radiosurgery in acromegaly: Analysis of 352 patients from the German Acromegaly Registry. Eur. J. Endocrinol. 2020, 182, 275–284. [Google Scholar] [CrossRef]
- Fong, K.Y.; Lim, M.J.R.; Fu, S.; Low, C.E.; Chan, Y.H.; Deepak, D.S.; Xu, X.; Thong, M.; Jain, S.; Teo, K.; et al. Postsurgical outcomes of nonfunctioning pituitary adenomas: A patient-level meta-analysis. Pituitary 2023, 26, 461–473. [Google Scholar] [CrossRef]
- Kotecha, R.; Sahgal, A.; Rubens, M.; De Salles, A.; Fariselli, L.; Pollock, B.E.; Levivier, M.; Ma, L.; Paddick, I.; Regis, J.; et al. Stereotactic radiosurgery for non-functioning pituitary adenomas: Meta-analysis and International Stereotactic Radiosurgery Society practice opinion. Neuro Oncol. 2020, 22, 318–332. [Google Scholar] [CrossRef]
- Loeffler, J.S.; Shih, H.A. Radiation therapy in the management of pituitary adenomas. J. Clin. Endocrinol. Metab. 2011, 96, 1992–2003. [Google Scholar] [CrossRef] [PubMed]
- Albano, L.; Losa, M.; Flickinger, J.; Mortini, P.; Minniti, G. Radiotherapy of Parasellar Tumours. Neuroendocrinology 2020, 110, 848–858. [Google Scholar] [CrossRef] [PubMed]
- Minniti, G.; Flickinger, J. The risk/benefit ratio of radiotherapy in pituitary tumors. Best Pract. Res. Clin. Endocrinol. Metab. 2019, 33, 101269. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiu, M.L. Updates in outcomes of stereotactic radiation therapy in acromegaly. Pituitary 2017, 20, 154–168. [Google Scholar] [CrossRef] [PubMed]
- Gheorghiu, M.L. Updates in the outcomes of radiation therapy for Cushing’s disease. Best Pract. Res. Clin. Endocrinol. Metab. 2021, 35, 101514. [Google Scholar] [CrossRef] [PubMed]
- Losa, M.; Picozzi, P.; Redaelli, M.G.; Laurenzi, A.; Mortini, P. Pituitary radiotherapy for Cushing’s disease. Neuroendocrinology 2010, 92 (Suppl. S1), 107–110. [Google Scholar] [CrossRef] [PubMed]
- Llahana, S.; Mulligan, K.; Hirani, S.P.; Wilson, S.; Baldeweg, S.E.; Grossman, A.; Norton, C.; Sharman, P.; McBride, P.; Newman, S. Using the behaviour change wheel and person-based approach to develop a digital self-management intervention for patients with adrenal insufficiency: The Support AI study protocol. Front. Endocrinol. 2023, 14, 1207715. [Google Scholar] [CrossRef] [PubMed]
- Fleseriu, M.; Dekkers, O.M.; Karavitaki, N. Endocrinology in the time of COVID-19: Management of pituitary tumours. Eur. J. Endocrinol. 2020, 183, G17–G23. [Google Scholar] [CrossRef]
- Barbot, M.; Ceccato, F.; Lizzul, L.; Daniele, A.; Zilio, M.; Gardiman, M.P.; Denaro, L.; Emanuelli, E.; Vianello, F.; Lombardi, G.; et al. Perioperative multidisciplinary management of endoscopic transsphenoidal surgery for sellar lesions: Practical suggestions from the Padova model. Neurosurg. Rev. 2020, 43, 1109–1116. [Google Scholar] [CrossRef]
- Bakker, L.E.H.; Verstegen, M.J.T.; Ghariq, E.; Verbist, B.M.; Schutte, P.J.; Bashari, W.A.; Kruit, M.C.; Pereira, A.M.; Gurnell, M.; Biermasz, N.R.; et al. Implementation of functional imaging using (11)C-methionine PET-CT co-registered with MRI for advanced surgical planning and decision making in prolactinoma surgery. Pituitary 2022, 25, 587–601. [Google Scholar] [CrossRef]
- Gillett, D.; Senanayake, R.; MacFarlane, J.; van der Meulen, M.; Koulouri, O.; Powlson, A.S.; Crawford, R.; Gillett, B.; Bird, N.; Heard, S.; et al. Localization of TSH-secreting pituitary adenoma using 11C-methionine image subtraction. EJNMMI Res. 2022, 12, 26. [Google Scholar] [CrossRef]
- Koulouri, O.; Steuwe, A.; Gillett, D.; Hoole, A.C.; Powlson, A.S.; Donnelly, N.A.; Burnet, N.G.; Antoun, N.M.; Cheow, H.; Mannion, R.J.; et al. A role for 11C-methionine PET imaging in ACTH-dependent Cushing’s syndrome. Eur. J. Endocrinol. 2015, 173, M107–M120. [Google Scholar] [CrossRef]
- Zoia, C.; Cattalani, A.; Turpini, E.; Custodi, V.M.; Benazzo, M.; Pagella, F.; Carena, P.; Lovati, E.; Lucotti, P.; Gaetani, P. Haemorrhagic presentation of a craniopharyngioma in a pregnant woman. Case Rep. Neurol. Med. 2014, 2014, 435208. [Google Scholar] [CrossRef] [PubMed]
- Inder, W.J.; Alford, F.P. Pituitary masses: The importance of a multidisciplinary approach. Med. J. Aust. 2007, 187, 522–523. [Google Scholar] [CrossRef] [PubMed]
- Biermasz, N.R.; Roelfsema, F.; Pereira, A.M.; Romijn, J.A. Cost-effectiveness of lanreotide Autogel in treatment algorithms of acromegaly. Expert. Rev. Pharmacoecon. Outcomes Res. 2009, 9, 223–234. [Google Scholar] [CrossRef]
- Elbaum, M.; Mizera, L.; Bolanowski, M. The real costs of acromegaly: Analysis of different therapies. Endokrynol. Pol. 2019, 70, 74–85. [Google Scholar] [CrossRef]
- Knutzen, R.; Ezzat, S. The cost of medical care for the acromegalic patient. Neuroendocrinology 2006, 83, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Fleseriu, M.; Barkan, A.; Del Pilar Schneider, M.; Darhi, Y.; de Pierrefeu, A.; Ribeiro-Oliveira, A., Jr.; Petersenn, S.; Neggers, S.; Melmed, S. Prevalence of comorbidities and concomitant medication use in acromegaly: Analysis of real-world data from the United States. Pituitary 2022, 25, 296–307. [Google Scholar] [CrossRef] [PubMed]
- Burton, T.; Le Nestour, E.; Bancroft, T.; Neary, M. Real-world comorbidities and treatment patterns of patients with acromegaly in two large US health plan databases. Pituitary 2013, 16, 354–362. [Google Scholar] [CrossRef]
- Broder, M.S.; Neary, M.P.; Chang, E.; Cherepanov, D.; Ludlam, W.H. Burden of illness, annual healthcare utilization, and costs associated with commercially insured patients with Cushing disease in the United States. Endocr. Pract. 2015, 21, 77–86. [Google Scholar] [CrossRef]
- Swearingen, B.; Wu, N.; Chen, S.Y.; Pulgar, S.; Biller, B.M. Health care resource use and costs among patients with cushing disease. Endocr. Pract. 2011, 17, 681–690. [Google Scholar] [CrossRef]
- Wilson, D.; Jin, D.L.; Wen, T.; Carmichael, J.D.; Cen, S.; Mack, W.J.; Zada, G. Demographic factors, outcomes, and patient access to transsphenoidal surgery for Cushing’s disease: Analysis of the Nationwide Inpatient Sample from 2002 to 2010. Neurosurg. Focus. 2015, 38, E2. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).