Effects of Ionizing Radiation on Cardiac Implantable Electronic Devices (CIEDs) in Patients with Esophageal Cancer Undergoing Radiotherapy: A Pilot Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Evaluation
2.2. CIED Details
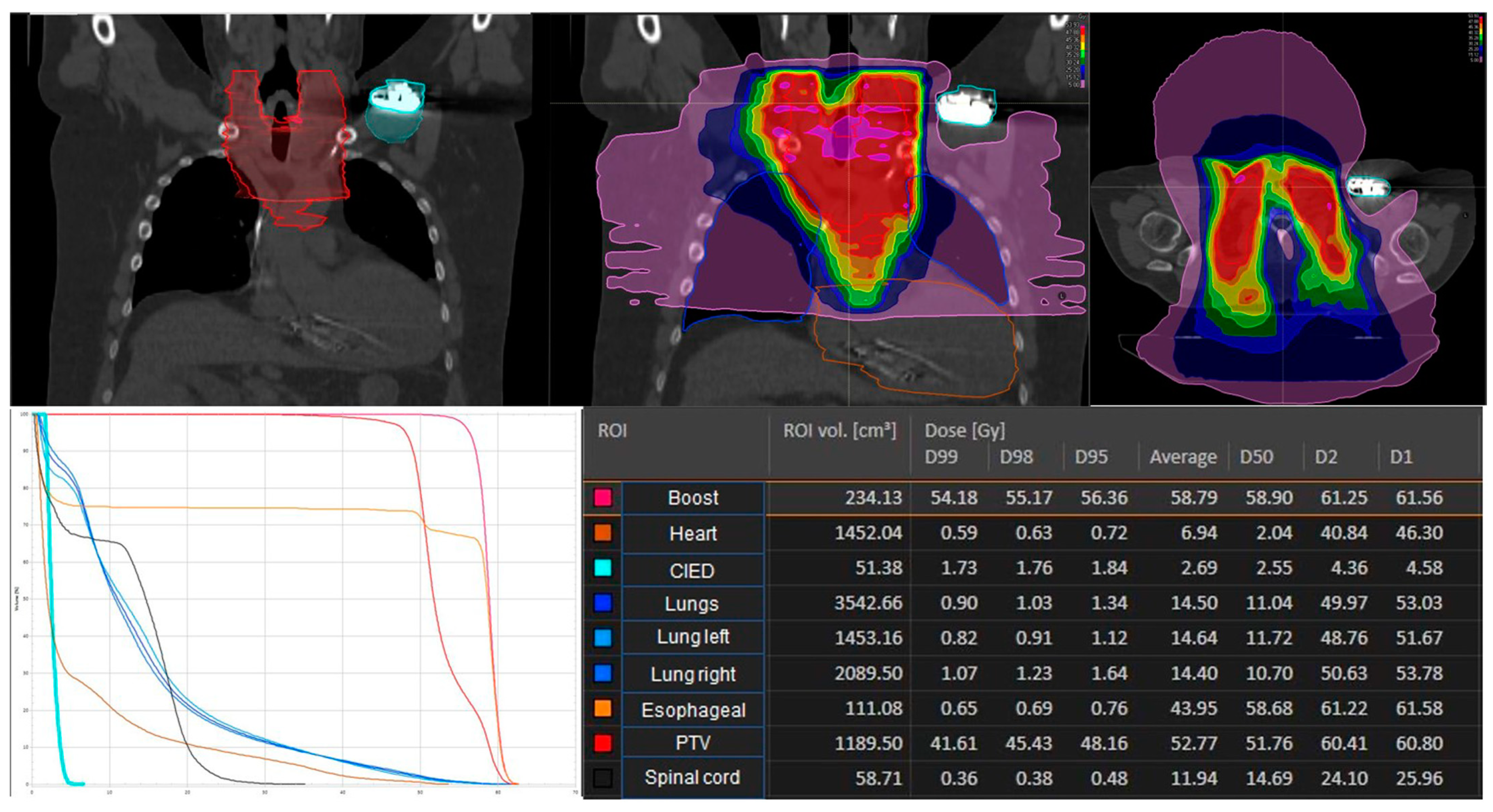
2.3. Treatment Planning and Treatment Characteristics
2.4. CIED Follow-Up
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mond, H.G.; Irwin, M.; Ector, H.; Proclemer, A. The world survey of cardiac pacing and cardioverter-defibrillators: Calendar year 2005 an International Cardiac Pacing and Electrophysiology Society (ICPES) project. Pacing Clin. Electrophysiol. 2008, 31, 1202–1212. [Google Scholar] [CrossRef] [PubMed]
- Lester, J.F.; Evans, L.M.; Yousef, Z.; Penney, A.; Brown, P.N.; Perks, R. A national audit of current cardiac device policies from radiotherapy centres across the UK. Clin. Oncol. (R. Coll. Radiol.) 2014, 26, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Hashii, H.; Hashimoto, T.; Okawa, A.; Shida, K.; Isobe, T.; Hanmura, M.; Nishimura, T.; Aonuma, K.; Sakae, T.; Sakurai, H. Comparison of the effects of high-energy photon beam irradiation (10 and 18 MV) on 2 types of implantable cardioverter-defibrillators. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 840–845. [Google Scholar] [CrossRef]
- Zaremba, T.; Jakobsen, A.R.; Søgaard, M.; Thøgersen, A.M.; Riahi, S. Radiotherapy in patients with pacemakers and implantable cardioverter defibrillators: A literature review. Europace 2016, 18, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Hudson, F.; Coulshed, D.; D’Souza, E.; Baker, C. Effect of radiation therapy on the latest generation of pacemakers and implantable cardioverter defibrillators: A systematic review. J. Med. Imaging Radiat. Oncol. 2010, 54, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Blaes, A.; Prizment, A.; Koene, R.J.; Konety, S. Cardio-oncology Related to Heart Failure: Common Risk Factors Between Cancer and Cardiovascular Disease. Heart Fail. Clin. 2017, 13, 367–380. [Google Scholar] [CrossRef] [PubMed]
- Hasin, T.; Iakobishvili, Z.; Weisz, G. Associated Risk of Malignancy in Patients with Cardiovascular Disease: Evidence and Possible Mechanism. Am. J. Med. 2017, 130, 780–785. [Google Scholar] [CrossRef]
- Hur, C.; Miller, M.; Kong, C.Y.; Dowling, E.C.; Nattinger, K.J.; Dunn, M.; Feuer, E.J. Trends in esophageal adenocarcinoma incidence and mortality. Cancer 2013, 119, 1149–1158. [Google Scholar] [CrossRef]
- Löfdahl, H.E.; Lane, A.; Lu, Y.; Lagergren, P.; Harvey, R.F.; Blazeby, J.M.; Lagergren, J. Increased population prevalence of reflux and obesity in the United Kingdom compared with Sweden: A potential explanation for the difference in incidence of esophageal adenocarcinoma. Eur. J. Gastroenterol. Hepatol. 2011, 23, 128–132. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef]
- Kranzfelder, M.; Schuster, T.; Geinitz, H.; Friess, H.; Büchler, P. Meta-analysis of neoadjuvant treatment modalities and definitive non-surgical therapy for oesophageal squamous cell cancer. Br. J. Surg. 2011, 98, 768–783. [Google Scholar] [CrossRef]
- van Hagen, P.; Hulshof, M.C.; van Lanschot, J.J.; Steyerberg, E.W.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.; Richel, D.J.; Nieuwenhuijzen, G.A.; Hospers, G.A.; Bonenkamp, J.J.; et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N. Engl. J. Med. 2012, 366, 2074–2084. [Google Scholar] [CrossRef] [PubMed]
- Stewart, B.W.; Bray, F.; Forman, D.; Ohgaki, H.; Straif, K.; Ullrich, A.; Wild, C.P. Cancer prevention as part of precision medicine: ‘Plenty to be done’. Carcinogenesis 2016, 37, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Sjoquist, K.M.; Burmeister, B.H.; Smithers, B.M.; Zalcberg, J.R.; Simes, R.J.; Barbour, A.; Gebski, V. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: An updated meta-analysis. Lancet Oncol. 2011, 12, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, J.; van Lanschot, J.J.B.; Hulshof, M.; van Hagen, P.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.L.; van Laarhoven, H.W.M.; Nieuwenhuijzen, G.A.P.; Hospers, G.A.P.; Bonenkamp, J.J.; et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): Long-term results of a randomised controlled trial. Lancet Oncol. 2015, 16, 1090–1098. [Google Scholar] [CrossRef]
- Gauter-Fleckenstein, B.; Israel, C.W.; Dorenkamp, M.; Dunst, J.; Roser, M.; Schimpf, R.; Steil, V.; Schäfer, J.; Höller, U.; Wenz, F. DEGRO/DGK guideline for radiotherapy in patients with cardiac implantable electronic devices. Strahlenther. Onkol. 2015, 191, 393–404. [Google Scholar] [CrossRef]
- Azraai, M.; D’Souza, D.; Lin, Y.H.; Nadurata, V. Current clinical practice in patients with cardiac implantable electronic devices undergoing radiotherapy: A literature review. Europace 2022, 24, 362–374. [Google Scholar] [CrossRef]
- Miften, M.; Mihailidis, D.; Kry, S.F.; Reft, C.; Esquivel, C.; Farr, J.; Followill, D.; Hurkmans, C.; Liu, A.; Gayou, O.; et al. Management of radiotherapy patients with implanted cardiac pacemakers and defibrillators: A Report of the AAPM TG-203(†). Med. Phys. 2019, 46, e757–e788. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Zeppenfeld, K.; Tfelt-Hansen, J.; de Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; de Chillou, C.; et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022, 43, 3997–4126. [Google Scholar] [CrossRef]
- Sundar, S.; Symonds, R.P.; Deehan, C. Radiotherapy to patients with artificial cardiac pacemakers. Cancer Treat. Rev. 2005, 31, 474–486. [Google Scholar] [CrossRef] [PubMed]
- Elders, J.; Kunze-Busch, M.; Smeenk, R.J.; Smeets, J.L. High incidence of implantable cardioverter defibrillator malfunctions during radiation therapy: Neutrons as a probable cause of soft errors. Europace 2013, 15, 60–65. [Google Scholar] [CrossRef]
- Wu, A.J.; Bosch, W.R.; Chang, D.T.; Hong, T.S.; Jabbour, S.K.; Kleinberg, L.R.; Mamon, H.J.; Thomas, C.R., Jr.; Goodman, K.A. Expert Consensus Contouring Guidelines for Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2015, 92, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Zaremba, T.; Jakobsen, A.R.; Thøgersen, A.M.; Riahi, S.; Kjærgaard, B. Effects of high-dose radiotherapy on implantable cardioverter defibrillators: An in vivo porcine study. Pacing Clin. Electrophysiol. 2013, 36, 1558–1563. [Google Scholar] [CrossRef] [PubMed]
- Zecchin, M.; Morea, G.; Severgnini, M.; Sergi, E.; Baratto Roldan, A.; Bianco, E.; Magnani, S.; De Luca, A.; Zorzin Fantasia, A.; Salvatore, L.; et al. Malfunction of cardiac devices after radiotherapy without direct exposure to ionizing radiation: Mechanisms and experimental data. Europace 2016, 18, 288–293. [Google Scholar] [CrossRef]
- Riva, G.; Alessandro, O.; Spoto, R.; Ferrari, A.; Garibaldi, C.; Cattani, F.; Luraschi, R.; Rondi, E.; Colombo, N.; Giovenzana, F.L.F.; et al. Radiotherapy in patients with cardiac implantable electronic devices: Clinical and dosimetric aspects. Med. Oncol. 2018, 35, 73. [Google Scholar] [CrossRef]
- Hudson, F.J.; Ryan, E.A. A review of implantable cardioverter defibrillator failures during radiation therapy in three Sydney hospitals. J. Med. Imaging Radiat. Oncol. 2017, 61, 517–521. [Google Scholar] [CrossRef]
- Zweng, A.; Schuster, R.; Hawlicek, R.; Weber, H.S. Life-threatening pacemaker dysfunction associated with therapeutic radiation: A case report. Angiology 2009, 60, 509–512. [Google Scholar] [CrossRef]
- Nemec, J. Runaway implantable defibrillator—A rare complication of radiation therapy. Pacing Clin. Electrophysiol. 2007, 30, 716–718. [Google Scholar] [CrossRef]
- Hurkmans, C.W.; Knegjens, J.L.; Oei, B.S.; Maas, A.J.; Uiterwaal, G.J.; van der Borden, A.J.; Ploegmakers, M.M.; van Erven, L. Management of radiation oncology patients with a pacemaker or ICD: A new comprehensive practical guideline in The Netherlands. Dutch Society of Radiotherapy and Oncology (NVRO). Radiat. Oncol. 2012, 7, 198. [Google Scholar] [CrossRef]
- Zaremba, T.; Jakobsen, A.R.; Thøgersen, A.M.; Oddershede, L.; Riahi, S. The effect of radiotherapy beam energy on modern cardiac devices: An in vitro study. Europace 2014, 16, 612–616. [Google Scholar] [CrossRef] [PubMed]
- Marbach, J.R.; Sontag, M.R.; Van Dyk, J.; Wolbarst, A.B. Management of radiation oncology patients with implanted cardiac pacemakers: Report of AAPM Task Group No. 34. American Association of Physicists in Medicine. Med. Phys. 1994, 21, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Zaremba, T.; Jakobsen, A.R.; Søgaard, M.; Thøgersen, A.M.; Johansen, M.B.; Madsen, L.B.; Riahi, S. Risk of device malfunction in cancer patients with implantable cardiac device undergoing radiotherapy: A population-based cohort study. Pacing Clin. Electrophysiol. 2015, 38, 343–356. [Google Scholar] [CrossRef] [PubMed]
- Varelas, A.N.; Eggerstedt, M.; Ganti, A.; Tajudeen, B.A. Epidemiologic, prognostic, and treatment factors in sinonasal diffuse large B -cell lymphoma. Laryngoscope 2019, 129, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- Indik, J.H.; Gimbel, J.R.; Abe, H.; Alkmim-Teixeira, R.; Birgersdotter-Green, U.; Clarke, G.D.; Dickfeld, T.L.; Froelich, J.W.; Grant, J.; Hayes, D.L.; et al. 2017 HRS expert consensus statement on magnetic resonance imaging and radiation exposure in patients with cardiovascular implantable electronic devices. Heart Rhythm. 2017, 14, e97–e153. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, H.; Ezura, T.; Hashimoto, Y.; Karasawa, K.; Nishio, T.; Tsuneda, M. Prediction of radiation-induced malfunction for cardiac implantable electronic devices (CIEDs). Med. Phys. 2020, 47, 1489–1498. [Google Scholar] [CrossRef]
- Bourgouin, A.; Varfalvy, N.; Archambault, L. Estimating and reducing dose received by cardiac devices for patients undergoing radiotherapy. J. Appl. Clin. Med. Phys. 2015, 16, 411–422. [Google Scholar] [CrossRef]
- Tajstra, M.; Gadula-Gacek, E.; Buchta, P.; Blamek, S.; Gasior, M.; Kosiuk, J. Effect of Therapeutic Ionizing Radiation on Implantable Electronic Devices: Systematic Review and Practical Guidance. J. Cardiovasc. Electrophysiol. 2016, 27, 1247–1251. [Google Scholar] [CrossRef]
| Characteristics | No of Patients (%) |
|---|---|
| Gender | |
| Male | 14 |
| female | 2 |
| Age at RT | |
| mean (range) | 77 (56–85 years) |
| T-stage | |
| T1 | 1 (6.25%) |
| T2 | 2 (12.5%) |
| T3 | 10 (62.4%) |
| T4 | 3 (18.75%) |
| N-stage | |
| N0 | 2 (12.5%) |
| N+ | 14 (87.5%) |
| Cardiovascular risk factors | |
| Hypertension | 14 (87.5%) |
| Hypercholesterolemia | 8 (50.0%) |
| Diabetes mellitus | 8 (50.0%) |
| Smoking | 11 (68.8%) |
| Coronary artery disease | 11 (68.8%) |
| Heart failure with reduced ejection fraction | 10 (62.5%) |
| Prior percutaneous coronary interventions | 5 (31.3%) |
| Prior aortocoronary bypass grafting | 4 (25.0%) |
| n (%) | |
|---|---|
| RT-technique | |
| 3D-CRT | 1 (6.25%) |
| IMRT | 15 (93.75%) |
| Mean total dose PTV | 58.8 Gy (range:36.0–58.8 Gy) |
| irradiation cervical lymph nodes | |
| yes | 12 (75.0%) |
| No | 4 (25.0%) |
| Mean PTV-volume | 810 ccm (range 207–1539 ccm) |
| Mean total dose CIED | 1.75 Gy (range 0.2–4.81 Gy) |
| Mean total dose ICD | 2.2 Gy (range 0.96–4.81 Gy) |
| Mean total dose PM | 0.6 Gy (range 0.2–2.0 Gy) |
| PTV | 851 ccm (range 207–1539 ccm) |
| Uncertainties on planning dose values | 0.4% (range 0.1–2.1%) |
| n (%) | |
|---|---|
| CIED type | |
| ICD | 7 (43.8%) |
| PM | 6 (37.5%) |
| CRT | 3 (18.8%) |
| PM dependence | |
| Dependent (</= 30 bpm) | 2 (22.2%) |
| Not dependent (>30 bpm) | 7 (77.8%) |
| Missing | 0 (0%) |
| Manufacture | |
| Medtronic | 10 (62.5%) |
| St. Jude Medical | 5 (31.25%) |
| Boston Scientific | 1 (6.25%) |
| Patients | Pacing Threshold (Volt) | Sensing Threshold (mV) | Lead-Impedance (Ohm) | |||
|---|---|---|---|---|---|---|
| before RT | after RT | before RT | after RT | before RT | after RT | |
| 1 | 0.6 | 0.5 | 5.8 | 5.8 | 388 | 390 |
| 2 | 1.0 | 1.12 | 5.3 | 5.3 | 300 | 292 |
| 3 | 0.75 | 0.75 | 20.2 | 21.4 | 478 | 475 |
| 4 | 3 | 3 | 2.3 | 4.2 | 544 | 528 |
| 5 | 0.75 | 0.5 | 9.6 | 7.6 | 350 | 363 |
| 6 | 0.75 | 0.87 | 22.4 | 22.4 | 671 | 689 |
| 7 | 0.75 | 0.75 | 6 | 5.1 | 456 | 456 |
| 8 | 1.0 | 1.25 | 6.8 | 8.0 | 700 | 779 |
| 9 | 1.0 | 1.0 | 11 | 19.9 | 480 | 760 |
| 10 | 0.75 | 0.75 | 11.3 | 12.1 | 475 | 475 |
| 11 | 0.75 | 0.75 | 6.8 | 6.8 | 719 | 674 |
| 12 | 0.5 | 0.5 | 7.2 | 7.3 | 475 | 463 |
| 13 | 0.5 | 0.5 | 22.4 | 22.4 | 848 | 756 |
| 14 | 0.9 | 0.8 | 7.2 | 11.4 | 428 | 459 |
| 15 | 1.0 | 1.0 | 6.3 | 11.8 | 375 | 400 |
| 16 | 0.75 | 0.75 | 5.8 | 5.8 | 380 | 399 |
| Mean/± SD | 0.9 ± 0.6 | 0.9 ± 0.6 | 9.8 ± 6.1 | 11.1 ± 6.5 | 504.2 ± 148.8 | 522.4 ± 152.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uzun, D.D.; Salatzki, J.; Xynogalos, P.; Frey, N.; Debus, J.; Lang, K. Effects of Ionizing Radiation on Cardiac Implantable Electronic Devices (CIEDs) in Patients with Esophageal Cancer Undergoing Radiotherapy: A Pilot Study. Cancers 2024, 16, 555. https://doi.org/10.3390/cancers16030555
Uzun DD, Salatzki J, Xynogalos P, Frey N, Debus J, Lang K. Effects of Ionizing Radiation on Cardiac Implantable Electronic Devices (CIEDs) in Patients with Esophageal Cancer Undergoing Radiotherapy: A Pilot Study. Cancers. 2024; 16(3):555. https://doi.org/10.3390/cancers16030555
Chicago/Turabian StyleUzun, Davut D., Janek Salatzki, Panagiotis Xynogalos, Norbert Frey, Juergen Debus, and Kristin Lang. 2024. "Effects of Ionizing Radiation on Cardiac Implantable Electronic Devices (CIEDs) in Patients with Esophageal Cancer Undergoing Radiotherapy: A Pilot Study" Cancers 16, no. 3: 555. https://doi.org/10.3390/cancers16030555
APA StyleUzun, D. D., Salatzki, J., Xynogalos, P., Frey, N., Debus, J., & Lang, K. (2024). Effects of Ionizing Radiation on Cardiac Implantable Electronic Devices (CIEDs) in Patients with Esophageal Cancer Undergoing Radiotherapy: A Pilot Study. Cancers, 16(3), 555. https://doi.org/10.3390/cancers16030555







