Real-World Outcomes of Crizotinib in ROS1-Rearranged Advanced Non-Small-Cell Lung Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Design and Patient Eligibility
2.2. Treatment
2.3. Study Endpoints
2.4. Sample Preparation and Sequencing Analysis
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Efficacy of Crizotinib
3.3. Safety of Crizotinib
3.4. Amplicon-Based Targeted Sequencing of cfTNA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Statistics Korea. Daejeon: Statistics Korea. 2021. Available online: http://kosis.kr (accessed on 25 August 2023).
- Jeon, D.S.; Kim, H.C.; Kim, S.H.; Kim, T.J.; Kim, H.K.; Moon, M.H.; Beck, K.S.; Suh, Y.G.; Song, C.; Ahn, J.S.; et al. Five-Year Overall Survival and Prognostic Factors in Patients with Lung Cancer: Results from the Korean Association of Lung Cancer Registry (KALC-R) 2015. Cancer Res. Treat. 2023, 55, 103–111. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society. Cancer Facts & Figures 2023. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2023/2023-cancer-facts-and-figures.pdf (accessed on 1 September 2023).
- Scagliotti, G.V.; Parikh, P.; Pawel, J.v.; Biesma, B.; Vansteenkiste, J.; Manegold, C.; Serwatowski, P.; Gatzemeier, U.; Digumarti, R.; Zukin, M.; et al. Phase III Study Comparing Cisplatin Plus Gemcitabine With Cisplatin Plus Pemetrexed in Chemotherapy-Naive Patients With Advanced-Stage Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2008, 26, 3543–3551. [Google Scholar] [CrossRef] [PubMed]
- Kelly, K.; Crowley, J.; Bunn, P.A., Jr.; Presant, C.A.; Grevstad, P.K.; Moinpour, C.M.; Ramsey, S.D.; Wozniak, A.J.; Weiss, G.R.; Moore, D.F.; et al. Randomized phase III trial of paclitaxel plus carboplatin versus vinorelbine plus cisplatin in the treatment of patients with advanced non--small-cell lung cancer: A Southwest Oncology Group trial. J. Clin. Oncol. 2001, 19, 3210–3218. [Google Scholar] [CrossRef] [PubMed]
- Schiller, J.H.; Harrington, D.; Belani, C.P.; Langer, C.; Sandler, A.; Krook, J.; Zhu, J.; Johnson, D.H. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N. Engl. J. Med. 2002, 346, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Pao, W.; Girard, N. New driver mutations in non-small-cell lung cancer. Lancet Oncol. 2011, 12, 175–180. [Google Scholar] [CrossRef]
- Chi, S.A.; Yu, H.; Choi, Y.-L.; Park, S.; Sun, J.-M.; Lee, S.-H.; Ahn, J.S.; Ahn, M.-J.; Choi, D.-H.; Kim, K.; et al. Trends in Survival Rates of Non–Small Cell Lung Cancer With Use of Molecular Testing and Targeted Therapy in Korea, 2010–2020. JAMA Netw. Open 2023, 6, e232002. [Google Scholar] [CrossRef]
- Blumenthal, G.M.; Karuri, S.W.; Zhang, H.; Zhang, L.; Khozin, S.; Kazandjian, D.; Tang, S.; Sridhara, R.; Keegan, P.; Pazdur, R. Overall response rate, progression-free survival, and overall survival with targeted and standard therapies in advanced non-small-cell lung cancer: US Food and Drug Administration trial-level and patient-level analyses. J. Clin. Oncol. 2015, 33, 1008–1014. [Google Scholar] [CrossRef]
- Leone, G.M.; Candido, S.; Lavoro, A.; Vivarelli, S.; Gattuso, G.; Calina, D.; Libra, M.; Falzone, L. Clinical Relevance of Targeted Therapy and Immune-Checkpoint Inhibition in Lung Cancer. Pharmaceutics 2023, 15, 1252. [Google Scholar] [CrossRef]
- Le, X.; Elamin, Y.Y.; Zhang, J. New Actions on Actionable Mutations in Lung Cancers. Cancers 2023, 15, 2917. [Google Scholar] [CrossRef]
- Chu, Q.S. Targeting non-small cell lung cancer: Driver mutation beyond epidermal growth factor mutation and anaplastic lymphoma kinase fusion. Ther. Adv. Med. Oncol. 2020, 12, 1758835919895756. [Google Scholar] [CrossRef] [PubMed]
- Araghi, M.; Mannani, R.; Heidarnejad Maleki, A.; Hamidi, A.; Rostami, S.; Safa, S.H.; Faramarzi, F.; Khorasani, S.; Alimohammadi, M.; Tahmasebi, S.; et al. Recent advances in non-small cell lung cancer targeted therapy; an update review. Cancer Cell Int. 2023, 23, 162. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Cordero, R.; Devine, W.P. Targeted Therapy and Checkpoint Immunotherapy in Lung Cancer. Surg. Pathol. Clin. 2020, 13, 17–33. [Google Scholar] [CrossRef] [PubMed]
- Bergethon, K.; Shaw, A.T.; Ou, S.H.; Katayama, R.; Lovly, C.M.; McDonald, N.T.; Massion, P.P.; Siwak-Tapp, C.; Gonzalez, A.; Fang, R.; et al. ROS1 rearrangements define a unique molecular class of lung cancers. J. Clin. Oncol. 2012, 30, 863–870. [Google Scholar] [CrossRef]
- Rikova, K.; Guo, A.; Zeng, Q.; Possemato, A.; Yu, J.; Haack, H.; Nardone, J.; Lee, K.; Reeves, C.; Li, Y.; et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell 2007, 131, 1190–1203. [Google Scholar] [CrossRef] [PubMed]
- Gainor, J.F.; Shaw, A.T. Novel targets in non-small cell lung cancer: ROS1 and RET fusions. Oncologist 2013, 18, 865–875. [Google Scholar] [CrossRef] [PubMed]
- Kohno, T.; Nakaoku, T.; Tsuta, K.; Tsuchihara, K.; Matsumoto, S.; Yoh, K.; Goto, K. Beyond ALK-RET, ROS1 and other oncogene fusions in lung cancer. Transl. Lung Cancer Res. 2015, 4, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Zhan, P.; Zhang, X.; Lv, T.; Song, Y. Clinicopathologic characteristics of patients with ROS1 fusion gene in non-small cell lung cancer: A meta-analysis. Transl. Lung Cancer Res. 2015, 4, 300–309. [Google Scholar] [CrossRef]
- Davies, K.D.; Le, A.T.; Theodoro, M.F.; Skokan, M.C.; Aisner, D.L.; Berge, E.M.; Terracciano, L.M.; Cappuzzo, F.; Incarbone, M.; Roncalli, M.; et al. Identifying and targeting ROS1 gene fusions in non-small cell lung cancer. Clin. Cancer Res. 2012, 18, 4570–4579. [Google Scholar] [CrossRef]
- Ou, S.H. Crizotinib: A novel and first-in-class multitargeted tyrosine kinase inhibitor for the treatment of anaplastic lymphoma kinase rearranged non-small cell lung cancer and beyond. Drug Des. Devel. Ther. 2011, 5, 471–485. [Google Scholar] [CrossRef]
- Shaw, A.T.; Ou, S.H.; Bang, Y.J.; Camidge, D.R.; Solomon, B.J.; Salgia, R.; Riely, G.J.; Varella-Garcia, M.; Shapiro, G.I.; Costa, D.B.; et al. Crizotinib in ROS1-rearranged non-small-cell lung cancer. N. Engl. J. Med. 2014, 371, 1963–1971. [Google Scholar] [CrossRef]
- Wu, Y.L.; Yang, J.C.; Kim, D.W.; Lu, S.; Zhou, J.; Seto, T.; Yang, J.J.; Yamamoto, N.; Ahn, M.J.; Takahashi, T.; et al. Phase II Study of Crizotinib in East Asian Patients With ROS1-Positive Advanced Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2018, 36, 1405–1411. [Google Scholar] [CrossRef] [PubMed]
- Templeton, A.J.; Booth, C.M.; Tannock, I.F. Informing Patients About Expected Outcomes: The Efficacy-Effectiveness Gap. J. Clin. Oncol. 2020, 38, 1651–1654. [Google Scholar] [CrossRef]
- Nordon, C.; Karcher, H.; Groenwold, R.H.; Ankarfeldt, M.Z.; Pichler, F.; Chevrou-Severac, H.; Rossignol, M.; Abbe, A.; Abenhaim, L. The “Efficacy-Effectiveness Gap”: Historical Background and Current Conceptualization. Value Health 2016, 19, 75–81. [Google Scholar] [CrossRef]
- Mazières, J.; Zalcman, G.; Crinò, L.; Biondani, P.; Barlesi, F.; Filleron, T.; Dingemans, A.M.; Léna, H.; Monnet, I.; Rothschild, S.I.; et al. Crizotinib therapy for advanced lung adenocarcinoma and a ROS1 rearrangement: Results from the EUROS1 cohort. J. Clin. Oncol. 2015, 33, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Qiang, T.; Li, Z.; Ding, D.; Yu, Y.; Lu, S. First-line crizotinib versus platinum-pemetrexed chemotherapy in patients with advanced ROS1-rearranged non-small-cell lung cancer. Cancer Med. 2020, 9, 3310–3318. [Google Scholar] [CrossRef] [PubMed]
- Rolfo, C.; Mack, P.; Scagliotti, G.V.; Aggarwal, C.; Arcila, M.E.; Barlesi, F.; Bivona, T.; Diehn, M.; Dive, C.; Dziadziuszko, R.; et al. Liquid Biopsy for Advanced NSCLC: A Consensus Statement From the International Association for the Study of Lung Cancer. J. Thorac. Oncol. 2021, 16, 1647–1662. [Google Scholar] [CrossRef]
- Pérez-Callejo, D.; Romero, A.; Provencio, M.; Torrente, M. Liquid biopsy based biomarkers in non-small cell lung cancer for diagnosis and treatment monitoring. Transl. Lung Cancer Res. 2016, 5, 455–465. [Google Scholar] [CrossRef]
- Gedvilaitė, V.; Schveigert, D.; Cicėnas, S. Cell-free DNA in non-small cell lung cancer. Acta Med. Litu. 2017, 24, 138–144. [Google Scholar] [CrossRef]
- Szpechcinski, A.; Chorostowska-Wynimko, J.; Struniawski, R.; Kupis, W.; Rudzinski, P.; Langfort, R.; Puscinska, E.; Bielen, P.; Sliwinski, P.; Orlowski, T. Cell-free DNA levels in plasma of patients with non-small-cell lung cancer and inflammatory lung disease. Br. J. Cancer 2015, 113, 476–483. [Google Scholar] [CrossRef]
- Leighl, N.B.; Page, R.D.; Raymond, V.M.; Daniel, D.B.; Divers, S.G.; Reckamp, K.L.; Villalona-Calero, M.A.; Dix, D.; Odegaard, J.I.; Lanman, R.B.; et al. Clinical Utility of Comprehensive Cell-free DNA Analysis to Identify Genomic Biomarkers in Patients with Newly Diagnosed Metastatic Non–small Cell Lung Cancer. Clin. Cancer Res. 2019, 25, 4691–4700. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, N.; Kohsaka, S.; Kurokawa, K.; Shinno, Y.; Takeda Nakamura, I.; Ueno, T.; Kojima, S.; Kawazu, M.; Suehara, Y.; Ishijima, M.; et al. Highly sensitive fusion detection using plasma cell-free RNA in non-small-cell lung cancers. Cancer Sci. 2021, 112, 4393–4403. [Google Scholar] [CrossRef] [PubMed]
- Michels, S.; Massutí, B.; Schildhaus, H.U.; Franklin, J.; Sebastian, M.; Felip, E.; Grohé, C.; Rodriguez-Abreu, D.; Abdulla, D.S.Y.; Bischoff, H.; et al. Safety and Efficacy of Crizotinib in Patients With Advanced or Metastatic ROS1-Rearranged Lung Cancer (EUCROSS): A European Phase II Clinical Trial. J. Thorac. Oncol. 2019, 14, 1266–1276. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Riely, G.J.; Bang, Y.J.; Kim, D.W.; Camidge, D.R.; Solomon, B.J.; Varella-Garcia, M.; Iafrate, A.J.; Shapiro, G.I.; Usari, T.; et al. Crizotinib in ROS1-rearranged advanced non-small-cell lung cancer (NSCLC): Updated results, including overall survival, from PROFILE 1001. Ann. Oncol. 2019, 30, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Landi, L.; Chiari, R.; Tiseo, M.; D’Incà, F.; Dazzi, C.; Chella, A.; Delmonte, A.; Bonanno, L.; Giannarelli, D.; Cortinovis, D.L.; et al. Crizotinib in MET-Deregulated or ROS1-Rearranged Pretreated Non-Small Cell Lung Cancer (METROS): A Phase II, Prospective, Multicenter, Two-Arms Trial. Clin. Cancer Res. 2019, 25, 7312–7319. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Ahn, B.C.; Lim, S.W.; Sun, J.M.; Kim, H.R.; Hong, M.H.; Lee, S.H.; Ahn, J.S.; Park, K.; Choi, Y.; et al. Characteristics and Outcome of ROS1-Positive Non-Small Cell Lung Cancer Patients in Routine Clinical Practice. J. Thorac. Oncol. 2018, 13, 1373–1382. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, X.; Zhang, R.; Xu, Q.; Yang, H.; Lizaso, A.; Xu, C.; Liu, J.; Wang, W.; Ou, S.-H.I.; et al. Clinical and molecular factors that impact the efficacy of first-line crizotinib in ROS1-rearranged non-small-cell lung cancer: A large multicenter retrospective study. BMC Med. 2021, 19, 206. [Google Scholar] [CrossRef] [PubMed]
- Waterhouse, D.; Iadeluca, L.; Sura, S.; Wilner, K.; Emir, B.; Krulewicz, S.; Espirito, J.; Bartolome, L. Real-World Outcomes Among Crizotinib-Treated Patients with ROS1-Positive Advanced Non-Small-Cell Lung Cancer: A Community Oncology-Based Observational Study. Target. Oncol. 2022, 17, 25–33. [Google Scholar] [CrossRef]
- Costa, D.B.; Kobayashi, S.; Pandya, S.S.; Yeo, W.L.; Shen, Z.; Tan, W.; Wilner, K.D. CSF concentration of the anaplastic lymphoma kinase inhibitor crizotinib. J. Clin. Oncol. 2011, 29, e443–e445. [Google Scholar] [CrossRef]
- Peters, S.; Camidge, D.R.; Shaw, A.T.; Gadgeel, S.; Ahn, J.S.; Kim, D.W.; Ou, S.I.; Pérol, M.; Dziadziuszko, R.; Rosell, R.; et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 377, 829–838. [Google Scholar] [CrossRef]
- Bronkhorst, A.J.; Ungerer, V.; Holdenrieder, S. The emerging role of cell-free DNA as a molecular marker for cancer management. Biomol. Detect. Quantif. 2019, 17, 100087. [Google Scholar] [CrossRef] [PubMed]
- Wan, J.C.M.; Massie, C.; Garcia-Corbacho, J.; Mouliere, F.; Brenton, J.D.; Caldas, C.; Pacey, S.; Baird, R.; Rosenfeld, N. Liquid biopsies come of age: Towards implementation of circulating tumour DNA. Nat. Rev. Cancer 2017, 17, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Pasini, L.; Ulivi, P. Liquid Biopsy for the Detection of Resistance Mechanisms in NSCLC: Comparison of Different Blood Biomarkers. J. Clin. Med. 2019, 8, 998. [Google Scholar] [CrossRef] [PubMed]
- Mezquita, L.; Swalduz, A.; Jovelet, C.; Ortiz-Cuaran, S.; Howarth, K.; Planchard, D.; Avrillon, V.; Recondo, G.; Marteau, S.; Benitez, J.C.; et al. Clinical Relevance of an Amplicon-Based Liquid Biopsy for Detecting ALK and ROS1 Fusion and Resistance Mutations in Patients With Non-Small-Cell Lung Cancer. JCO Precis. Oncol. 2020, 4, PO.19.00281. [Google Scholar] [CrossRef]
- Dagogo-Jack, I.; Rooney, M.; Nagy, R.J.; Lin, J.J.; Chin, E.; Ferris, L.A.; Ackil, J.; Lennerz, J.K.; Lanman, R.B.; Gainor, J.F.; et al. Molecular Analysis of Plasma From Patients With ROS1-Positive NSCLC. J. Thorac. Oncol. 2019, 14, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Davies, K.D.; Le, A.T.; Sheren, J.; Nijmeh, H.; Gowan, K.; Jones, K.L.; Varella-Garcia, M.; Aisner, D.L.; Doebele, R.C. Comparison of Molecular Testing Modalities for Detection of ROS1 Rearrangements in a Cohort of Positive Patient Samples. J. Thorac. Oncol. 2018, 13, 1474–1482. [Google Scholar] [CrossRef]
- Awad, M.M.; Katayama, R.; McTigue, M.; Liu, W.; Deng, Y.L.; Brooun, A.; Friboulet, L.; Huang, D.; Falk, M.D.; Timofeevski, S.; et al. Acquired resistance to crizotinib from a mutation in CD74-ROS1. N. Engl. J. Med. 2013, 368, 2395–2401. [Google Scholar] [CrossRef]
- Lin, J.J.; Choudhury, N.J.; Yoda, S.; Zhu, V.W.; Johnson, T.W.; Sakhtemani, R.; Dagogo-Jack, I.; Digumarthy, S.R.; Lee, C.; Do, A.; et al. Spectrum of Mechanisms of Resistance to Crizotinib and Lorlatinib in ROS1 Fusion–Positive Lung Cancer. Clin. Cancer Res. 2021, 27, 2899–2909. [Google Scholar] [CrossRef]
- García-Pardo, M.; Calles, A. ROS-1 NSCLC therapy resistance mechanism. Precis. Cancer Med. 2021, 4, 1–15. [Google Scholar] [CrossRef]
- Watanabe, J.; Furuya, N.; Fujiwara, Y. Appearance of a BRAF Mutation Conferring Resistance to Crizotinib in Non-Small Cell Lung Cancer Harboring Oncogenic ROS1 Fusion. J. Thorac. Oncol. 2018, 13, e66–e69. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.C.; Lin, X.P.; Li, X.F.; Wu, L.X.; Chen, H.F.; Wang, W.X.; Xu, C.W.; Shen, J.F.; Wei, J.G.; Du, K.Q. Concurrent ROS1 gene rearrangement and KRAS mutation in lung adenocarcinoma: A case report and literature review. Thorac. Cancer 2018, 9, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Dziadziuszko, R.; Le, A.T.; Wrona, A.; Jassem, J.; Camidge, D.R.; Varella-Garcia, M.; Aisner, D.L.; Doebele, R.C. An Activating KIT Mutation Induces Crizotinib Resistance in ROS1-Positive Lung Cancer. J. Thorac. Oncol. 2016, 11, 1273–1281. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 40) |
|---|---|
| Median age, years (range) | 60.5 (27–83) |
| Sex (male/female) | 14/26 |
| BMI | 24.3 ± 3.2 |
| Smoking status (n = 39) | |
| Never-smoker | 27 (69.2) |
| Former smoker | 11 (28.2) |
| Current smoker | 1 (2.6) |
| ECOG PS | |
| 0 | 7 (17.5) |
| 1 | 30 (75.0) |
| 2 | 3 (7.5) |
| Stage at initial diagnosis a | |
| IIA | 1 (2.5) |
| IIB | 2 (5.0) |
| IIIA | 3 (7.5) |
| IIIB | 2 (5.0) |
| IVA | 20 (50.0) |
| IVB | 12 (30.0) |
| Location of biopsy b | |
| Lung | 26 (65.0) |
| Lymph node | 16 (40.0) |
| Pleural effusion | 1 (2.5) |
| Histologic type | |
| Adenocarcinoma | 40 (100.0) |
| Metastasis | |
| Yes | 32 (80.0) |
| No | 8 (20.0) |
| Distant metastatic site at initial diagnosis a,b | |
| Brain/central nervous system | 13 (32.5) |
| Lung | 13 (32.5) |
| Bone | 10 (25.0) |
| Pleura | 9 (22.5) |
| Adrenal gland | 6 (15.0) |
| Lymph node | 6 (15.0) |
| Liver | 2 (5.0) |
| Other | 1 (2.5) |
| Number of prior chemotherapeutic regimens | |
| 0 | 20 (50.0) |
| 1 | 12 (30.0) |
| 2 | 4 (10.0) |
| ≥3 | 4 (10.0) |
| ROS1 rearrangement b | 40 (100) |
| RT-qPCR | 38 (95.0) |
| IHC | 8 (20.0) |
| FISH | 3 (7.5) |
| EGFR mutation (n = 39) | 0 |
| ALK rearrangement (n = 37) | 0 |
| Total, No. (%) | |
|---|---|
| Number of patients | 40 |
| Best overall response | |
| Complete response | 0 |
| Partial response | 28 (70.0) |
| Stable disease | 12 (30.0) |
| ORR (n = 40) | 28 (70.0) |
| 95% CI | 53.5–83.4 |
| DCR (n = 40) | 40 (100.0) |
| 95% CI | 91.2–100 |
| DR | |
| Median, months (95% CI) | 27.8 (21.0–34.6) |
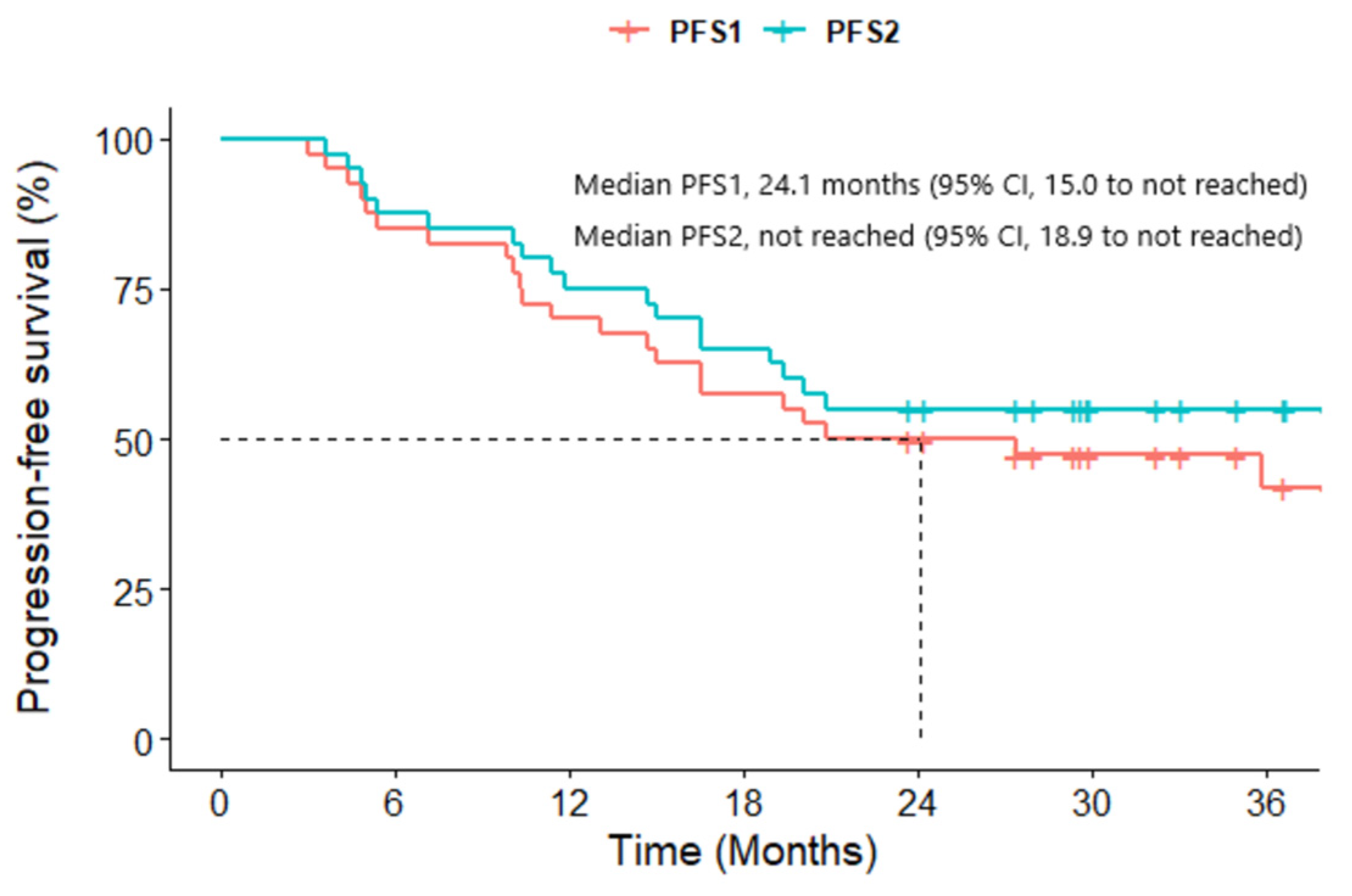
| PFS1 | |
| Number of events | 22 (55.0) |
| Progressive disease | 19 (47.5) |
| Death without objective progression | 3 (7.5) |
| Median, months (95% CI) | 24.1 (15.0–NR) |
| 6 months PFS1 rate, % (95% CI) | 85.0 (74.6–96.8) |
| 12 months PFS1 rate, % (95% CI) | 70.0 (57.1–85.7) |
| 18 months PFS1 rate, % (95% CI) | 57.5 (44.1–75.1) |
| PFS2 | |
| Number of events | 18 (45.0) |
| Median, months (95% CI) | NR (18.9–NR) |
| 6 months PFS2 rate, % (95% CI) | 85.0 (74.6–96.8) |
| 12 months PFS2 rate, % (95% CI) | 72.5 (59.9–87.7) |
| 18 months PFS2 rate, % (95% CI) | 62.5 (49.2–79.5) |
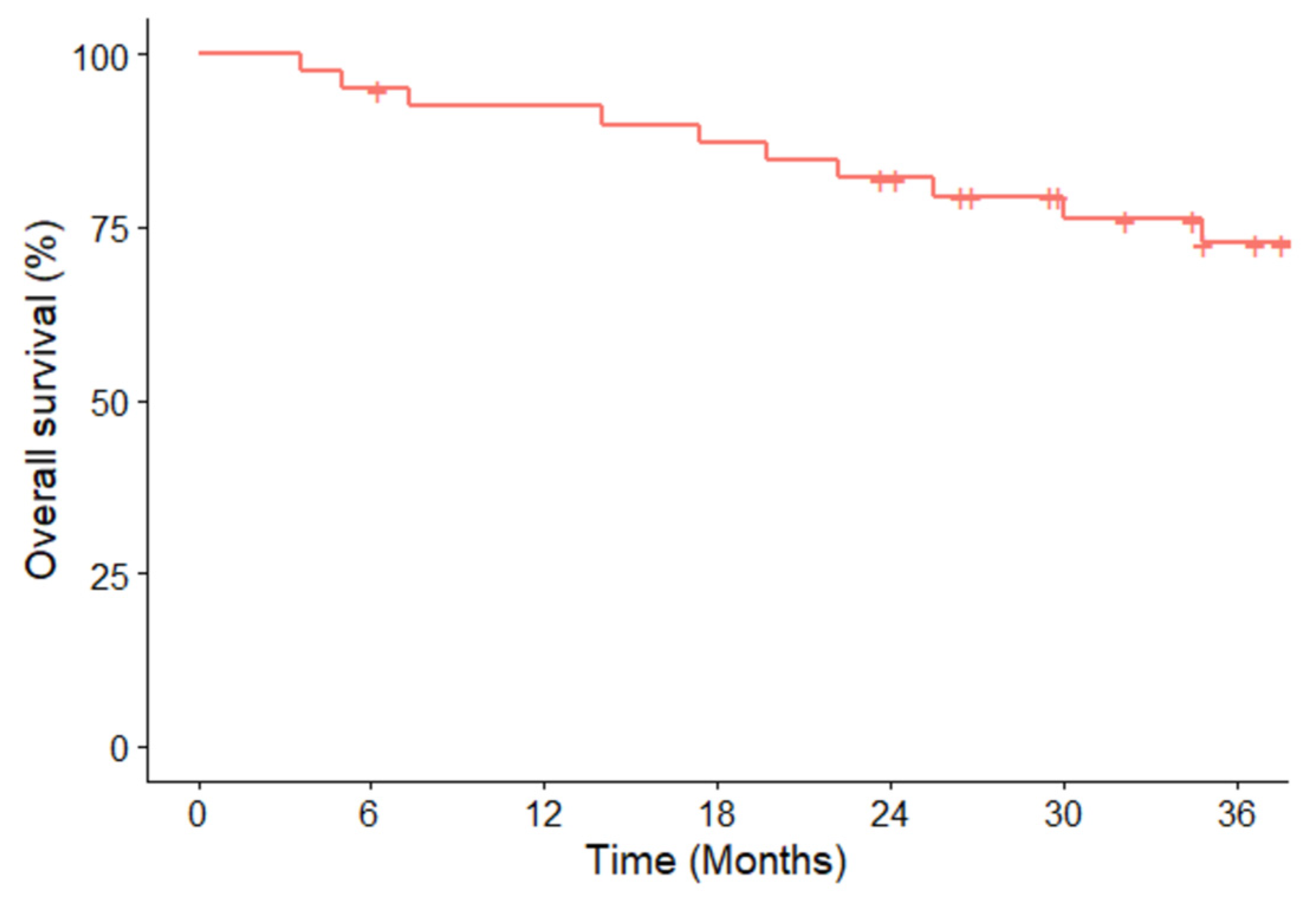
| OS | |
| Number of events | 10 (25.0) |
| Median, months (95% CI) | NR (NR–NR) |
| 6 months OS rate, % (95% CI) | 95.0 (88.5–100.0) |
| 12 months OS rate, % (95% CI) | 92.4 (84.6–100.0) |
| 18 months OS rate, % (95% CI) | 87.3 (77.5–98.4) |
| Adverse Events | Grade | |||||
|---|---|---|---|---|---|---|
| Any, n (%) | 1, n (%) | 2, n (%) | 3, n (%) | 4, n (%) | 5, n (%) | |
| Any | 36 (90.0) | 30 (75.0) | 15 (37.5) | 13 (32.5) | 0 | 1 (2.5) |
| In ≥10% of patients | ||||||
| Elevated ALT | 15 (37.5) | 11 (27.5) | 1 (2.5) | 3 (7.5) | - | - |
| Elevated AST | 13 (32.5) | 10 (25.0) | 2 (5.0) | 1 (2.5) | - | - |
| Nausea | 9 (22.5) | 7 (17.5) | 2 (5.0) | - | - | - |
| Diarrhea | 8 (20.0) | 6 (15.0) | 2 (5.0) | - | - | - |
| Elevated ALP | 7 (17.5) | 3 (7.5) | 2 (5.0) | 2 (5.0) | - | - |
| Paresthesia | 7 (17.5) | 3 (7.5) | 4 (10.0) | - | - | - |
| Constipation | 6 (15.0) | 5 (12.5) | 1 (2.5) | - | - | - |
| Skin rash | 5 (12.5) | 1 (2.5) | 4 (10.0) | - | - | - |
| Edema | 5 (12.5) | 3 (7.5) | 2 (5.0) | - | - | - |
| Visual disturbance | 5 (12.5) | 5 (12.5) | - | - | - | - |
| Vomiting | 4 (10.0) | 3 (7.5) | 1 (2.5) | - | - | - |
| Asthenia/fatigue | 4 (10.0) | 2 (5.0) | 1 (2.5) | 1 (2.5) | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.H.; Lee, J.C.; Oh, I.-J.; Kim, E.Y.; Yoon, S.H.; Lee, S.Y.; Lee, M.K.; Lee, J.E.; Park, C.K.; Lee, K.Y.; et al. Real-World Outcomes of Crizotinib in ROS1-Rearranged Advanced Non-Small-Cell Lung Cancer. Cancers 2024, 16, 528. https://doi.org/10.3390/cancers16030528
Kim HH, Lee JC, Oh I-J, Kim EY, Yoon SH, Lee SY, Lee MK, Lee JE, Park CK, Lee KY, et al. Real-World Outcomes of Crizotinib in ROS1-Rearranged Advanced Non-Small-Cell Lung Cancer. Cancers. 2024; 16(3):528. https://doi.org/10.3390/cancers16030528
Chicago/Turabian StyleKim, Hyeon Hwa, Jae Cheol Lee, In-Jae Oh, Eun Young Kim, Seong Hoon Yoon, Shin Yup Lee, Min Ki Lee, Jeong Eun Lee, Chan Kwon Park, Kye Young Lee, and et al. 2024. "Real-World Outcomes of Crizotinib in ROS1-Rearranged Advanced Non-Small-Cell Lung Cancer" Cancers 16, no. 3: 528. https://doi.org/10.3390/cancers16030528
APA StyleKim, H. H., Lee, J. C., Oh, I.-J., Kim, E. Y., Yoon, S. H., Lee, S. Y., Lee, M. K., Lee, J. E., Park, C. K., Lee, K. Y., Lee, S. Y., Kim, S. J., Lim, J. H., & Choi, C.-m. (2024). Real-World Outcomes of Crizotinib in ROS1-Rearranged Advanced Non-Small-Cell Lung Cancer. Cancers, 16(3), 528. https://doi.org/10.3390/cancers16030528







