Simple Summary
This research focuses on understanding a rare, benign tumor that derives from the autonomic nervous system, called ganglioneuroma (GN). Our study reports a unique case of a woman with GN originating in her larynx, which caused dysphonia and dysphagia. After an evaluation of the neck imaging, surgical intervention was proposed, and the tumor was successfully removed via a cervical approach. We hope to raise awareness about this unusual tumor location, improve early diagnosis, and guide future treatment.
Abstract
Introduction: Ganglioneuroma (GN) is a rare, benign tumor of the autonomic nervous system. It is seldom located in the head and neck (HN) region. GN typically presents as a slow-growing, painless mass, often leading to delayed diagnosis. Case report: We report a unique case of laryngeal-originating GN in a 43-year-old female who presented with worsening dysphonia and dyspnea. Imaging revealed a large mass originating from the larynx. Histological examination confirmed the diagnosis. The tumor was surgically excised with preservation of key structures in the neck. At the follow-up, the patient experienced a significant improvement in symptoms. Material and methods: A systematic literature review following PRISMA guidelines was conducted in January 2024 to investigate the common sites of GN in the HN region and the complications associated with its treatment. Results: In a total of 58 articles, we studied 65 patients, mostly under 30 years old. Surgical excision remains the primary treatment, and post-operative complications were mostly neurological. Discussion: GNs are generally slow-growing and asymptomatic, but they can reveal themselves when compressing nearby structures, especially in the HN region. In symptomatic cases or when the tumor exhibits significant growth or hormonal activity, surgical resection is required. The lateral cervical approach is the most common one. The risk of postoperative complications and recurrence underscores the need for careful surgical planning and long-term follow-up. Conclusion: This unique laryngeal GN case highlights the importance of considering GN in the differential diagnosis of HN masses. Further large-scale studies are warranted to establish evidence-based protocols for their management, especially in the HN region.
1. Introduction
Ganglioneuroma (GN) is a rare, benign, and encapsulated tumor of nervous tissue originating from the sympathetic ganglion [1]. GN is classified as part of the neuroblastic tumor family, and it is composed of Schwann and ganglion cells [2]. First described by Loretz in 1870 and later by Stout in 1947, this tumor has a higher prevalence in females. It is rarely associated with Von Recklinghausen disease [3].
This neoplasm is commonly localized in the posterior mediastinum, retroperitoneum, and adrenal glands, and it rarely occurs in the head and neck (HN) region, where it typically presents as a painless neck mass [1,2,3]. Due to the indolent and slow-growing nature of these lesions, early detection is challenging, and diagnosis is often delayed until symptoms arise from the compression of surrounding structures. It is typically identified either as a noticeable neck swelling or mass or through incidental findings during radiological investigations performed for unrelated reasons.
Various imaging techniques are useful for cervical masses because they provide information on their size, location, composition, and relation to adjacent structures, but they often lack specificity in distinguishing GN from other neurogenic tumors, so they are mostly used for the follow-up. Fine-needle aspiration biopsy (FNAB) can yield useful diagnostic details, although histopathologic confirmation may not always conclusively identify the condition.
As a result, the definitive diagnosis of GN is generally established only after surgical resection, which allows for thorough histopathological examination. Surgery represents the first therapeutic choice, but complications can occur due to the proximity of these tumors to vascular and nervous structures in the cervical region [4].
Herein, we describe a case of GN in an adult patient with worsening dysphonia and dyspnea that manifested as a swollen mass in the left lateral neck region. She underwent surgical resection of the mass, and subsequent histopathological analysis confirmed the diagnosis of larynx-originating GN. In light of this case, we also provide a comprehensive review of the existing literature, highlighting current approaches to the diagnosis, management, and prognosis of these tumors in the HN region.
2. Case Report
A 43-year-old Caucasian female, with a smoking history of 20 pack-years and no comorbidities, reported worsening dysphonia associated with dyspnea for approximately one year.
Fibrolaryngoscopy (FLS) evaluation revealed a voluminous right-sided mass at the hypopharyngeal level, obstructing visualization of the glottic plane and covered by intact mucosa. No cervical lymphadenopathies were clinically evident (Figure 1).
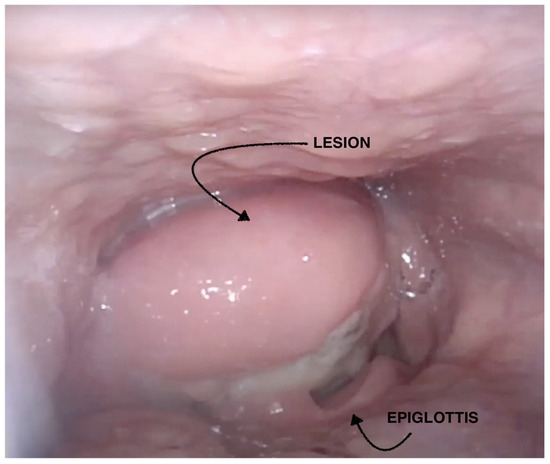
Figure 1.
Preoperative fibrolaryngoscopy.
Although Magnetic Resonance Imaging (MRI) of the neck was recommended, the patient underwent computed tomography (CT) with and without contrast because of claustrophobia. CT revealed a voluminous, round, heterogeneous solid mass measuring 44 × 33 mm in the axial planes, extending cranially by 65 mm, localized in the paramedian right-sided hypopharynx, and involving the posterolateral parapharyngeal space (Figure 2). It abutted the right epiglottis without a cleavage plan and extended inferiorly, displacing the glottic plane and aryepiglottic fold and infiltrating the cricoid cartilage and the right thyroid oblique lamina. The upper right pole of the thyroid gland was not cleavable. Enlarged ipsilateral lymph nodes (LNs) were noted.
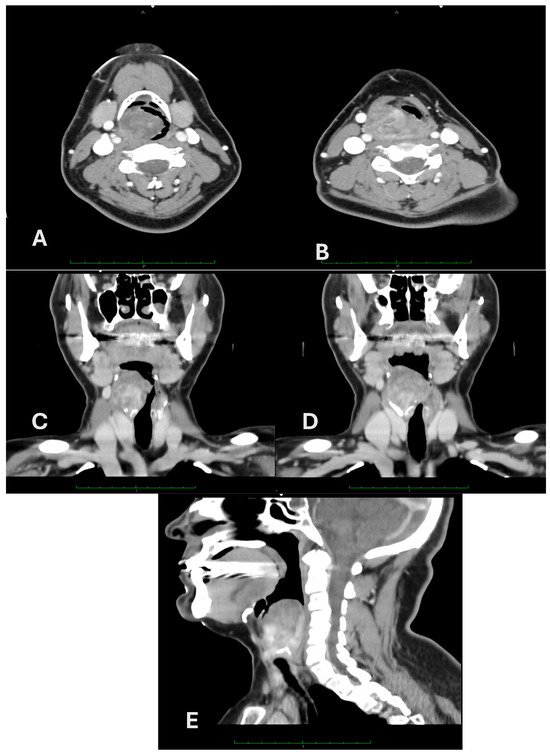
Figure 2.
Axial (A,B), coronal (C,D), and sagittal (E) contrast-enhanced CT scan of the neck.
Diagnostic microlaryngoscopy with multiple biopsies of the lesion and tracheotomy was performed under general anesthesia. Histological examination showed a paracellular neoplasm composed of spindle elements without atypia, with positive immunohistochemistry for S100 and SOX10. The findings were suggestive of a nerve sheath neoplasm without histological features of aggressiveness.
Therefore, we performed a surgical excision through a right cervical access. We removed the upper part of the right thyroid cartilage, including its superior horn, and the homolateral pharyngeal constrictor muscles were removed; this allowed the complete removal of the encapsulated, oval (50 × 30 × 30 mm), yellowish-white mass, with its origin at the cricothyroid notch and the epiglottis. The glottis and both arytenoids were preserved.
At the microscopic examination (Figure 3), the predominant portion of the neoplasm consisted of spindle cells with sporadic cytological atypia, while a minor portion was represented by epithelioid cellularity with a neuroendocrine immunophenotype. Positive staining was observed with S-100, CD56, chromogranin, and synaptophysin. Some elements exhibited abundant polygonal cytoplasm with evident nucleoli and cytoplasmic extensions (ganglion cells). Mitosis, lymphatic/vascular invasion, and necrosis were not documented. Ki-67 was expressed in 5–8% of the neoplastic population. A pathological diagnosis of GN was established.

Figure 3.
Histological findings of laryngeal ganglioneuroma. (a) Hematoxylin and eosin ×25; (b) hematoxylin and eosin ×200; (c) synaptophysin stain.
The tracheal cannula and a nasogastric tube were maintained until the 7th post-operative day, and she was discharged on the 10th post-operative day. The FLS examination showed mild arytenoid edema and reduced mobility of the right arytenoid with preserved airway space and an absence of pathological stasis in the hypopharynx. She underwent speech therapy rehabilitation for the first 3 months post-surgery.
At the 6-month follow-up evaluation, the patient reported a major improvement in dysphonia and an absence of dysphagia. The FLS showed no recurrence and persisting hypomobility of the right vocal cord with good compensation by the contralateral one.
3. Material and Methods
3.1. Searching Strategy and Selection Criteria
This review was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and has not been registered. We conducted a literature search using the PubMed and Embase databases in order to identify the relevant studies.
The following keywords were used:
- Ganglioneuroma AND head and neck (160 articles in English, Italian, or Chinese);
- Ganglioneuroma AND larynx (7 articles in English, Italian, or Chinese);
Only studies describing the localization, symptoms, and therapeutic management of patients with HN GN were included; articles were excluded based on the following criteria: localization outside the HN region, papers with incomplete data and reviews, and those that were not written in English, Italian, or Chinese.
3.2. Data Collection
The title and abstract of the selected papers were carefully read according to the inclusion and exclusion criteria, and duplicates were removed. Two reviewers (S.J., A.G.) independently extracted data from each study, which were reviewed for consistency among the authors, and any discrepancies were resolved by consensus. The full text of the included studies was then read in order to extract the following data:
- Reference: first author, year of publication;
- Age and sex;
- Localization and size;
- Symptoms;
- Therapeutic iter and surgical complications;
- Follow-up duration.
3.3. Quality Assessment and Statistical Methods
The quality and the risk of bias of the articles included in the systematic review were evaluated by the Quality In Prognosis Studies (QUIPS) tool, with any discrepancies resolved by consensus by the first two authors (S.J., A.G.). Visualization of the risk-of-bias assessments was performed by creating a traffic lights plot and a weighted bar plot using the Robvis tool.
4. Results
We systematically reviewed cases of HN GN reported in the literature up to January 2024, following the PRISMA guidelines.
A total of 160 records for HN GN were identified from a primary literature search. After the removal of duplicates and by applying the aforementioned criteria, a total of 66 publications were selected. Papers were then screened by reading the titles and abstracts, and 58 manuscripts were deemed eligible for possible inclusion. After reading the full texts, 4 articles were excluded because of insufficient or incomplete data, and 1 review and 3 articles were excluded because of the GN localization; only 58 studies eventually met the inclusion criteria. The flowchart presenting our literature search strategy is shown in Figure 4. The included studies are summarized with their main characteristics in Table 1.

Figure 4.
PRISMA 2020 flow diagram for new systematic reviews.

Table 1.
Clinicopathological features of cervical ganglioneuromas described in the literature. NA Not Available.
The majority of the population included in our study (N = 65) was under 30 (67.69%). The average age at presentation was 24 years old, with a median of 19 years, with the maximum reported age in the literature being 71 years. There were no differences between males and females (M = 31, F = 33, NA = 0). In the cervical region, the left side was more frequently involved; the localizations described in the literature were laterocervical, oropharyngeal, and the retropharyngeal space [11,16,30,33,40]. HN GN is usually a single, monolateral lesion, but a case of bilateral neck GN was also reported [44]. None described a laryngeal localization. Patients presented predominantly with cervical swelling, rarely with dysphagia or pain.
The postoperative complications were mostly neurological: the most frequently described one was Horner’s syndrome (33.85%), particularly if the chosen surgical approach was transcervical. Less frequently, paralysis of mixed cranial nerves (IX, X, XI, XII) occurred, resulting in symptoms such as dysphonia, dysphagia, and shoulder motor difficulty [2,12,21,22,29,30,34,35,36]. In one case, surgical intervention led to the onset of first-bite syndrome [18].
Their overall risk of bias was judged to be low to moderate, and the traffic lights plot and the weighted bar plot for each domain considered in the QUIPS tool are given in Figure 5 and Figure 6, respectively.
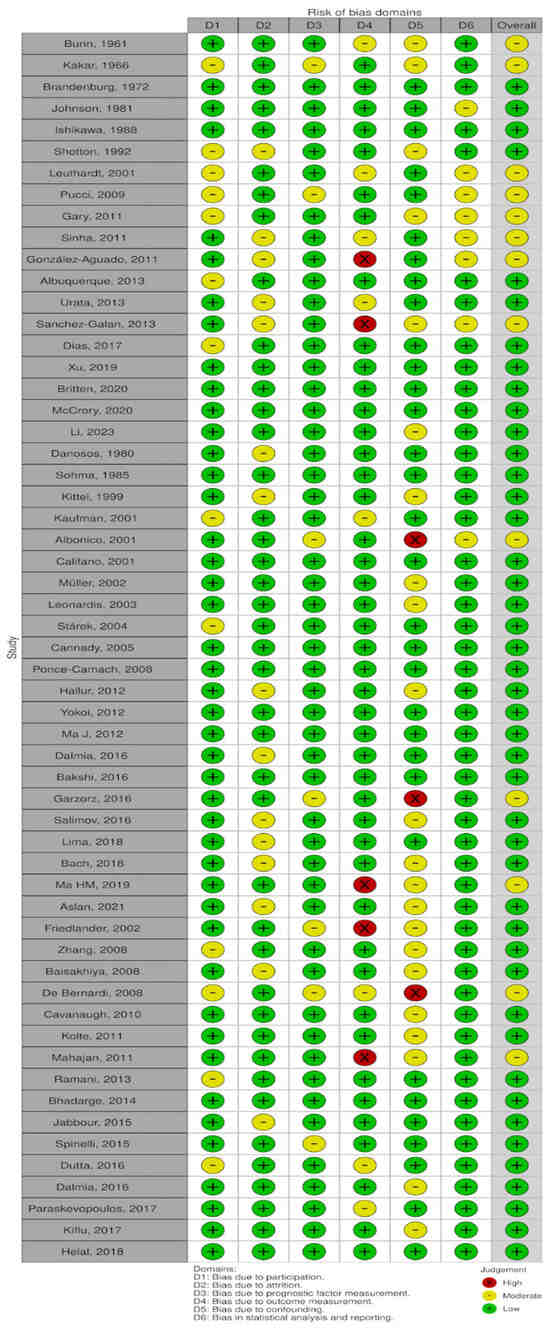
Figure 5.
Traffic lights plot [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57].
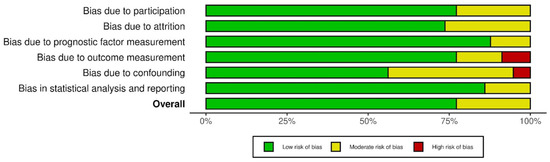
Figure 6.
Weighted bar plot.
5. Discussion
GN is a rare, benign tumor originating from the sympathetic ganglion, composed of Schwann and ganglion cells. It is more common in females and is only rarely linked to Von Recklinghausen disease [1].
GNs are slow-growing, well-differentiated tumors of the autonomic nervous system [24]. They are usually located in the thoracic cavity (60–80%, mainly in the posterior mediastinum), abdominal cavity (10–15%, adrenal gland, retroperitoneum, pelvic, sacral, and coccygeal sympathetic ganglia, and the organ of Zuckerkandl), and less commonly in the cervical region (5%). Other rare locations include the middle ear, parapharyngeal space, skin, orbital space, and gastrointestinal tract [25,26]. To the best of our knowledge, there are not any described cases of laryngeal GNs.
Although Stout (1947) recorded a predominance of this tumor in females [3], the current literature data show no incidence prevalence of the condition based on gender, with a male-to-female ratio of 1:1.
Our results indicate that this condition typically affects young adults, with 67.69% of the patients described as under 30 years old. The average age at presentation was 24 years, with a median age of 19 years, and the oldest age reported in the literature was 71 years.
Typically, GNs grow slowly and cause symptoms only when they reach a considerable size or compress nearby structures. In cases where they exhibit low neuroendocrine activity, they may lead to symptoms such as diarrhea, hypertension, virilization, and myasthenia gravis. Tumors located in the HN region usually present with neck swelling, hoarseness, and dysphagia; large GNs can compress peripheral nerves in the cervical area, resulting in Horner’s syndrome [23].
This symptomatology may be common to other expansive head–neck pathologies that cause compression of the lateral–cervical structures. The differential diagnosis, in fact, includes paragangliomas, lymphomas, carcinomas, thyroid masses, neurofibromas, and salivary gland tumors. Therefore, a thorough medical history examination is essential to rule out systemic symptoms that could indicate lymphatic neoplasms or syndromic conditions (such as neurofibromatosis). Additionally, laboratory testing to exclude abnormalities in thyroid hormone levels is indispensable [18].
The largest GN reported in the literature measured 160 × 60 × 190 mm, and the patient reported neck swelling and sleep apnea [15]. The symptoms and the localization of our patient were uncommon: she reported worsening dysphonia and dyspnea due to its laryngeal origin.
Advanced imaging techniques play a crucial role in assessing the extent and characteristics of GN, providing information on mass size, location, composition, and its relation to adjacent structures. A combination of imaging modalities, including ultrasound (US), CT, MRI, positron emission tomography-computed tomography (PET-CT), and fine-needle aspiration biopsy (FNAB), helps in accurate diagnosis and treatment planning [20]. US provides an initial evaluation and can identify the location and size of the tumor, while FNAB, although not always definitive, may provide valuable diagnostic information in some cases. CT scans offer detailed visualization of the tumor’s location, size, and morphology, typically presenting as well-defined, low- or medium-density masses with calcifications. MRI is particularly useful for soft tissue characterization, delineating the tumor’s relationship with surrounding structures and depicting features such as the “vortex sign” on T2-weighted images. PET-CT may offer insights into the metabolic activity of the tumor. However, it is essential to note that characteristic features of GNs can overlap with other neurogenic tumors, requiring a comprehensive approach that combines clinical findings, imaging studies, and histopathological evaluation for accurate diagnosis and treatment decision-making [58].
Making an accurate preoperative histological diagnosis of GNs poses challenges since FNAB is not consistently definitive. Histologically, GNs are composed of ganglion cells, Schwann cells, and fibrous tissues. Their differential diagnosis includes neuroblastoma and ganglioneuroblastoma based on neuroblastic differentiation and Schwannian stroma development [17].
The treatment strategy for GN remains controversial. Surgical resection is not mandatory because the prognosis is generally favorable and post-operative complications may occur, mostly neurological, albeit being resolved within months. It should be considered in cases that occur with neurological symptoms, hormonal imbalances, or significant physical deformities. And in some cases when a neurogenic tumor with malignant potential is suspected, surgery represents the only way to obtain a definitive diagnosis.
Surgical resection is the mainstay of treatment for parapharyngeal space tumors, with various surgical approaches developed to balance maximal tumor removal with minimal damage to surrounding structures [4]. The lateral cervical approach is commonly employed due to its wide surgical field and better exposure to important neck structures. In our review, three cases preferred the transoral approach, while in two cases, a combined approach was used.
When deciding between surgical intervention and a “wait and see” approach, it is important to consider the most common postoperative complications. Postoperative complications are primarily neurological, with Horner’s syndrome being the most commonly reported (33.85%), especially when a transcervical surgical approach is used. Less commonly, paralysis of mixed cranial nerves (IX, X, XI, XII) has been observed, leading to symptoms such as dysphonia, dysphagia, and shoulder motor difficulties [2,12,21,22,29,30,34,35,36]. In one instance, surgery resulted in the development of first-bite syndrome [18].
Recurrence, although rare, can happen, emphasizing the importance of thorough surgical management and long-term follow-up [35].
6. Conclusions
GN is a benign tumor that can occur in various parts of the body. The HN region is an uncommon site and, to the best of our knowledge, the laryngeal location has not been previously reported. Due to its indolent nature, GN often presents as an incidental finding or as a symptomatic mass due to its size or compression of surrounding structures. Imaging and FNAB help us with the diagnosis. Surgery should only be considered in cases with neurological symptoms, hormonal imbalances, or significant physical deformities because it is associated with potential postoperative neurological complications. Although recurrence is rare, it underscores the importance of vigilant follow-up.
Given the rarity of GN in the HN region, particularly in the laryngeal region, we conducted a systematic search of the literature to establish treatment strategies, but large-scale studies are necessary to assess evidence-based protocols.
Written consent was obtained from the patient for the publication of this study. Our research was conducted in full accordance with ethical principles, including the World Medical Association Declaration of Helsinki (version 2002).
Author Contributions
Conceptualization: O.G., S.J., A.G., and R.M.; data curation: A.G. and S.J.; formal analysis: S.J. and A.G.; investigation: O.G., T.T. and R.M.; methodology: S.J.; supervision: O.G. and R.M.; validation: O.G. and R.M.; visualization: O.G., T.T. and R.M.; writing—original draft: A.G. and S.J.; Writing—review and editing: O.G., S.J., and A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The present case report is conceived as an educational activity and it did not need the approval of the Institutional Review Board of AOU Careggi for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available in the Pubmed and Embase databases.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chikuie, N.; Hamamoto, T.; Ishino, T.; Nagasawa, A.; Kuniyasu, H.; Rina TA, N.I.; Takeno, S. Ganglioneuroma in The Neck Region: A Case Report. Hiroshima J. Med. Sci. 2019, 68, 49–53. [Google Scholar] [CrossRef]
- Ishikawa, K.; Hanazawa, S.; Togawa, K. Neurogenic Neoplasms in the Head and Neck Region. Auris Nasus Larynx 1988, 15, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Kakar, P.K.; Sawhney, K.L.; Saharia, P.S. Peripheral Ganglioneuroma of Neck. J. Laryngol. Otol. 1966, 80, 1260–1263. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Galán, A.; Barrena, S.; Vilanova-Sánchez, A.; Martín, S.H.A.; Lopez-Fernandez, S.; García, P.; Lopez-Santamaria, M.; Martínez, L.; Tovar, J.A. Ganglioneuroma: To Operate or Not to Operate. Eur. J. Pediatr. Surg. 2014, 24, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Bunn, N.D., Jr.; King, A.B. Cervical ganglioneuroma. A case report and review of the literature. Guthrie Clin. Bull. 1961, 30, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Brandenburg, J.H. Symposium on malignancy. IV. Neurogenic. Tumors of the parapharyngeal space. Laryngoscope 1972, 82, 1292–1305. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.C.; Teleg, M.; Eberle, R.C. Simultaneous Occurrence of a Ganglioneuroma and a Neurilemmoma of the Vagus Nerve: A Case Report. Otolaryngol.-Head Neck Surg. 1981, 89, 75–76. [Google Scholar] [CrossRef] [PubMed]
- Shotton, J.C.; Milton, C.M.; Allen, J.P. Multiple ganglioneuroma of the neck. J. Laryngol. Otol. 1992, 106, 277–278. [Google Scholar] [CrossRef] [PubMed]
- Leuthardt, R.; Petralli, C.; Lütschg, J.; von Schweinitz, D.; Kaiser, G. Cortical blindness: An unusual complication after removal of a ganglioneuroma of the neck. Child’s Nerv. Syst. 2001, 17, 356–358. [Google Scholar] [CrossRef] [PubMed]
- Pucci, A.; Pucci, E.; Santini, F.; Altea, M.A.; Faviana, P.; Basolo, F.; Pinchera, A.; Iacconi, P.; Vitti, P. A Ganglioneuroma with Features of a Thyroid Nodule: Intense Pain on Fine Needle Biopsy as a Diagnostic Clue. Thyroid® 2009, 19, 201–204. [Google Scholar] [CrossRef]
- Gary, C.; Robertson, H.; Ruiz, B.; Zuzukin, V.; Walvekar, R.R. Retropharyngeal Ganglioneuroma Presenting with Neck Stiffness: Report of a Case and Review of the Literature. Laryngoscope 2010, 120 (Suppl. S4), S148. [Google Scholar] [CrossRef] [PubMed]
- Sinha, P.; Sharma, S.C.; Agarwal, S.; Gupta, S.D. Parapharyngeal Ganglioneuroma with Neurofibromatosis: An Unusual Presentation. Ann. Otol. Rhinol. Laryngol. 2011, 120, 769–774. [Google Scholar] [CrossRef] [PubMed]
- González-Aguado, R.; Morales-Angulo, C.; Obeso-Agüera, S.; Longarela-Herrero, Y.; García-Zornoza, R.; Cervera, L.A. Síndrome de Horner secundario a cirugía cervical. Acta Otorrinolaringol. Esp. 2012, 63, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, B.S.; Farias, T.P.; Dias, F.L.; Torman, D. Surgical Management of Parapharyngeal Ganglioneuroma: Case Report and Review of the Literature. ORL J. Otorhinolaryngol. Relat. Spec. 2013, 75, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Urata, S.; Yoshida, M.; Ebihara, Y.; Asakage, T. Surgical management of a giant cervical ganglioneuroma. Auris Nasus Larynx 2013, 40, 577–580. [Google Scholar] [CrossRef] [PubMed]
- Dias, R.B.; Rosa, D.; Rito, M.; Borges, A. Ganglioneuroma of the retropharyngeal space in a patient with glottic cancer. BMJ Case Rep. 2017, 2017. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xu, T.; Zhu, W.; Wang, P. Cervical ganglioneuroma: A case report and review of the literature. Medicine 2019, 98, e15203. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Britten, A.G.; Entezami, P.; A Chang, B. Cervical ganglioneuroma mimicking a carotid body tumour. BMJ Case Rep. 2020, 13, e238469. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- McCrory, D.; Kelly, A.; Korda, M. Postoperative Horner’s syndrome following excision of incidental cervical ganglioneuroma during hemithyroidectomy and parathyroid gland exploration. BMJ Case Rep. 2020, 13, e231514. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, F.; Feng, H.; Liao, J.; Bao, Y.; Xu, S.; Qin, G. Parapharyngeal Space Ganglioneuroma: Clinical Experience and Review of the Literature. Ear Nose Throat J. 2023, 102, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Danosos, D.A.; Santos, V.B.; Ruffy, M.L.; A Polisar, I.; Torno, R. Ganglioneuroma of the parapharyngeal space. Bull. N. Y. Acad. Med. 1980, 56, 616–622. [Google Scholar] [PubMed]
- Sohma, S.; Azuma, E.; Asakura, K. A case of ganglioneuroma of the parapharyngeal space. Nippon. Jibiinkoka Gakkai Kaiho 1985, 88, 41–47. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kittel, K.; Hornung, J.; Wolf, S. Parapharyngealer Tumor. HNO 1999, 47, 56–57. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, M.R.; Rhee, J.S.; Fuegelman, L.J.; Costantino, P.D. Ganglioneuroma of the Parapharyngeal Space in a Pediatric Patient. Otolaryngol. Neck Surg. 2001, 124, 702–704. [Google Scholar] [CrossRef] [PubMed]
- Albonico, G.; Pellegrino, B.G.; Maisano, M.; Kardon, D.E. Ganglioneuroma of Parapharyngeal Region. Arch. Pathol. Lab. Med. 2001, 125, 1217–1218. [Google Scholar] [CrossRef] [PubMed]
- Califano, L.; Zupi, A.; Mangone, G.M.; Long, F. Cervical Ganglioneuroma: Report of a Case. Otolaryngol.-Head Neck Surg. 2001, 124, 115–116. [Google Scholar] [CrossRef]
- Müller, A.; Förster, G.; Behrendt, W.; Kosmehl, H. Headache as an unusual presenting symptom of retropharyngeal ganglioneuroma. Acta Otolaryngol. 2002, 122, 565–568. [Google Scholar] [CrossRef]
- Leonardis, M.; Sperb, D.; Alster, C.; Campisi, C.; Herter, N. Ganglioneuroma of the neck, masquerading as a goiter. Eur. J. Surg. Oncol. 2003, 29, 929–930. [Google Scholar] [CrossRef]
- Stárek, I.; Mihál, V.; Novák, Z.; Pospíšilová, D.; Vomáčka, J.; Vokurka, J. Pediatric tumors of the parapharyngeal space. Three case reports and a literature review. Int. J. Pediatr. Otorhinolaryngol. 2004, 68, 601–606. [Google Scholar] [CrossRef]
- Cannady, S.B.; Chung, B.J.; Hirose, K.; Garabedian, N.; Abbeele, T.V.D.; Koltai, P.J. Surgical management of cervical ganglioneuromas in children. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 287–294. [Google Scholar] [CrossRef]
- Ponce-Camacho, M.A.; De Leon-Medina, R.D.; Miranda-Maldonado, I.; Garza-Guajardo, R.; Hernandez-Salazar, J.; Barboza-Quintana, O. A 5-year-old girl with a congenital ganglioneuroma diagnosed by fine needle aspiration biopsy: A case report. CytoJournal 2008, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Hallur, N.; Sikkerimath, B.C.; Gudi, S.S.; Chour, G.; Ginimav, S.; Nidoni, M. Parapharyngeal Ganglioneuroma of Hypoglossal Nerve in a 4 Year Old Girl: A Rare Case Report. J. Maxillofac. Oral Surg. 2012, 11, 343–346. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yokoi, H.; Arakawa, A.; Inoshita, A.; Ikeda, K. Novel use of a Weerda laryngoscope for transoral excision of a cervical ganglioneuroma: A case report. J. Med. Case Rep. 2012, 6, 88. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Liang, L.; Liu, H. Multiple cervical ganglioneuroma: A case report and review of the literature. Oncol. Lett. 2012, 4, 509–512. [Google Scholar] [CrossRef]
- Dalmia, D.; Behera, S.K.; Motiwala, M.A.; Rekhi, B. Cervical vagal nerve ganglioneuroma: A rare case report. Int. J. Otorhinolaryngol. Head Neck Surg. 2016, 2, 274–276. [Google Scholar] [CrossRef][Green Version]
- Bakshi, J.; Mohammed, A.W.; Lele, S.; Nada, R. Ganglioneuromas Involving the Hypoglossal Nerve and the Vagus Nerve in a Child: Surgical Difficulties. Ear Nose Throat J. 2016, 95, E22–E24. [Google Scholar] [CrossRef]
- Garzorz, N.; Diercks, G.R.; Lin, H.W.; Faquin, W.C.; Romo, L.V.; Hartnick, C.J. A case of pediatric parapharyngeal space ganglioneuroma. Ear Nose Throat J. 2016, 95, E16–E20. [Google Scholar]
- Salimov, A.; Süslü, N.; Kuşçu, O.; Süslü, A.E.; Akyol, M.U.; Gököz, Ö.; Özoğul, E. Parapharyngeal giant ganglioneuroma with multifocal bone involvement in a pediatric female patient. Turk. J. Pediatr. 2016, 58, 669–674. [Google Scholar] [CrossRef]
- Lima, A.F.; Moreira, F.C.; Menezes, A.; Dias, L. Cervical Ganglioneuroma in Pediatric Age: A Case Report. Turk. Arch. Otolaryngol. 2018, 56, 237–240. [Google Scholar] [CrossRef]
- Bach, J.; Azher, Q.; Salih, A. Paediatric parapharyngeal ganglioneuroma. BMJ Case Rep. 2018, 2018. [Google Scholar] [CrossRef]
- Ma, H.M.; Zhao, Y.Q.; Zhao, Y.; Zhou, J.H.; Zhang, J.R.; Wei, H.Q. Ganglioneuroma in poststyloid space removed under endoscope through transoral approach: A case report. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2019, 33, 468–469; 473. [Google Scholar] [CrossRef]
- Aslan, M.; Dogukan, F.M. A Rare Cause of Dysphagia: A Giant Ganglioneuroma in Parapharyngeal Space. J. Maxillofac. Oral Surg. 2022, 21, 99–101. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, P.L.; Hunt, J.P.; Palacios, E. Ganglioneuroma of the neck. Ear Nose Throat J. 2002, 81, 435. [Google Scholar] [CrossRef] [PubMed]
- Zebing, Z.; Jianwei, S.; Yan, C.; Yan, G. Clinicopathological characteristics of neck ganglioneuroma. Oral Med. Pathol. 2008, 12, 131–134. [Google Scholar] [CrossRef][Green Version]
- Baisakhiya, N.K.; Mukundan, S. Ganglioneuroma of the neck. J. Pak. Med. Assoc. 2008, 58, 699–701. [Google Scholar] [PubMed]
- De Bernardi, B.; Gambini, C.; Haupt, R.; Granata, C.; Rizzo, A.; Conte, M.; Tonini, G.P.; Bianchi, M.; Giuliano, M.; Luksch, R.; et al. Retrospective Study of Childhood Ganglioneuroma. J. Clin. Oncol. 2008, 26, 1710–1716. [Google Scholar] [CrossRef]
- Cavanaugh, D.A.; Jawahar, A.; Harper, J.; McLaren, B.K.; Wooten, T.; Kerr, E.J.; Nunley, P.D. Cervical ganglioneuroma in an adult man: Case report and literature review of a rare occurrence. J. LA State Med. Soc. 2010, 162, 218–221. [Google Scholar]
- Kolte, S.S. Ganglioneuroma presenting as a neck mass diagnosed by fine needle aspiration cytology. Cytopathology 2011, 22, 205–206. [Google Scholar] [CrossRef]
- Mahajan, N.; Aggarwal, S.; Khurana, N.; Jain, S.; Gulati, A. Ganglioneuroma in the neck masquerading as a benign mesenchymal lesion on cytology: A morphological mimic. Cytopathology 2013, 24, 65–67. [Google Scholar] [CrossRef]
- Ramani, M.; Krishna, O.R.; Reddy, K.R.; Sowjanya, R. An interesting case of differentiated neuroblastoma-ganglioneuroma of the neck in a 5 year old female child. J. Evol. Med. Dent. Sci. 2013, 2, 4298–4302. [Google Scholar]
- Bhadarge, P.; Poflee, S. Aspiration cytology in the preoperative diagnosis of ganglioneuroma presenting as a neck mass. J. Cytol. 2014, 31, 57–58. [Google Scholar] [CrossRef] [PubMed]
- Jabbour, M.; Zaatari, G.; Salem, Z.; Khalifeh, I. Cervical ganglioneuroma in collision with a metastatic undifferentiated carcinoma. J. Oral Maxillofac. Pathol. 2015, 19, 88–91. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Spinelli, C.; Rossi, L.; Barbetta, A.; Ugolini, C.; Strambi, S. Incidental ganglioneuromas: A presentation of 14 surgical cases and literature review. J. Endocrinol. Investig. 2015, 38, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Dutta, H.K. Cervical ganglioneuroma in a child. SM J. Pediatr. Surg 2016, 2, 1013–1015. [Google Scholar]
- Paraskevopoulos, K.; Cheva, A.; Papaemmanuil, S.; Vahtsevanos, K.; Antoniades, K. Synchronous Ganglioneuroma and Schwannoma Mistaken for Carotid Body Tumor. Case Rep. Otolaryngol. 2017, 2017, 1–2. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kiflu, W.; Nigussie, T. Ganglioneuroma presenting as a neckmass: A case report. Ethiop. Med. J. 2017, 55, 69–71. [Google Scholar]
- Helal, A.A.; Badawy, R.; Mahfouz, M.; Hussien, T. Adjacent cervical ganglioneuromas. J. Pediatr. Surg. Case Rep. 2018, 34, 7–9. [Google Scholar] [CrossRef]
- Yi, W.-L.; Chen, T.-P.; Chiu, N.-T.; Liu, C.-S.; Lin, Y.-H. Parapharyngeal Ganglioneuroma Detected by 18F-FDG PET/CT in a Patient with Hodgkin Lymphoma. Clin. Nucl. Med. 2019, 44, 240–243. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).