Harnessing the Systemic Biology of Functional Decline and Cachexia to Inform more Holistic Therapies for Incurable Cancers
Abstract
Simple Summary
Abstract
1. Introduction
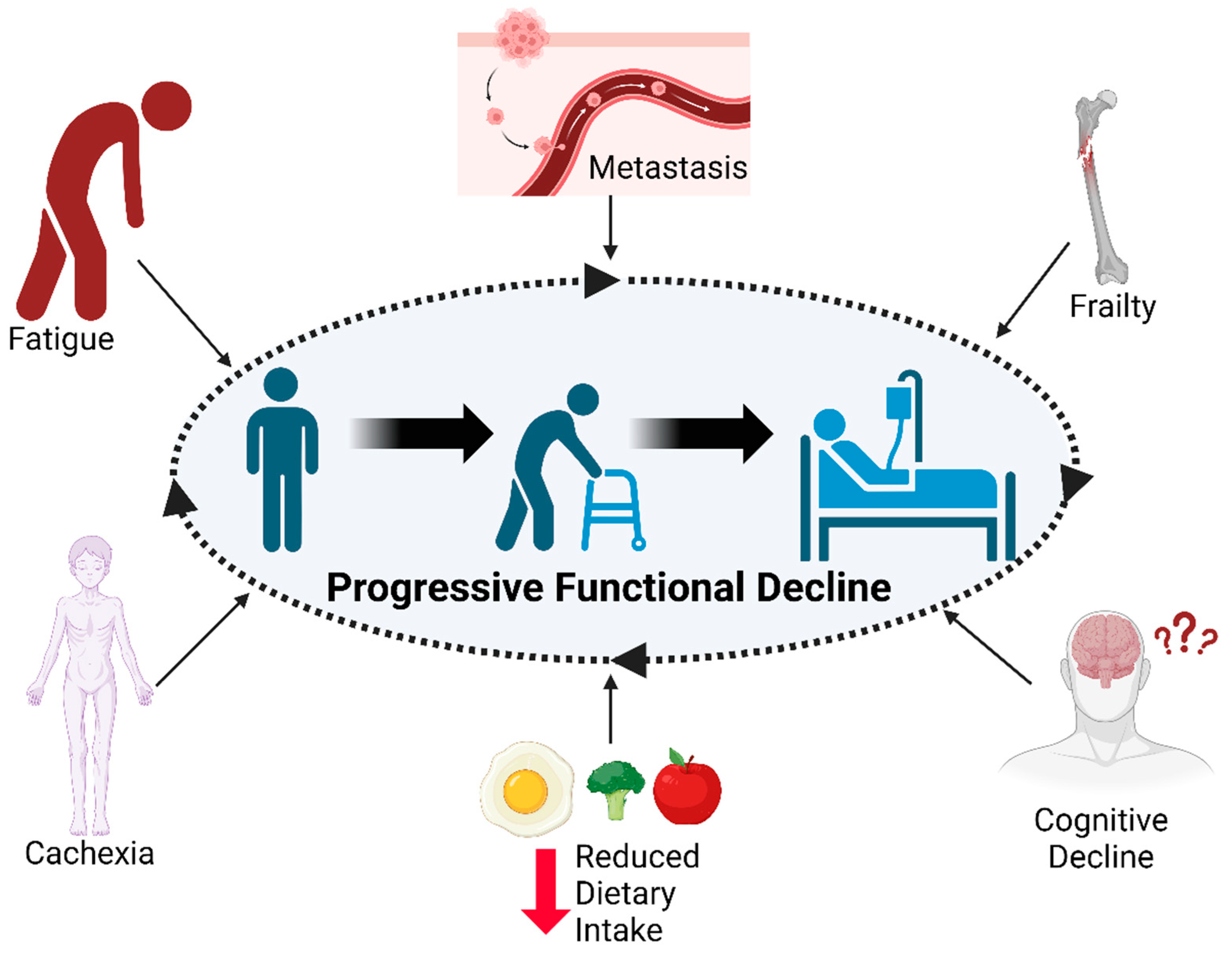
2. Functional Decline and Facilitators of Morbidity in Advanced Cancers
3. Systemic Biology of Advanced Cancers: Extratumoral Mechanisms
4. Pharmaceutical Interventions
5. Nutritional Guidelines and Interventions
6. Rehabilitation and Exercise Interventions
7. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Incidence and Relative Survival by Stage at Diagnosis for Common Cancers. USCS Data Brief. 2021, 25. Available online: https://www.cdc.gov/cancer/uscs/about/data-briefs/no25-incidence-relative-survival-stage-diagnosis.htm (accessed on 15 October 2023).
- Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; Xu, R.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019. JAMA Oncol. 2022, 8, 420. [Google Scholar] [CrossRef] [PubMed]
- Fettes, L.; Neo, J.; Ashford, S.; Higginson, I.J.; Maddocks, M. Trajectories of Disability in Activities of Daily Living in Advanced Cancer or Respiratory Disease: A Systematic Review. Disabil. Rehabil. 2022, 44, 1790–1801. [Google Scholar] [CrossRef] [PubMed]
- Ferrell, B.R.; Temel, J.S.; Temin, S.; Alesi, E.R.; Balboni, T.A.; Basch, E.M.; Firn, J.I.; Paice, J.A.; Peppercorn, J.M.; Phillips, T.; et al. Integration of Palliative Care Into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2017, 35, 96–112. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Bruera, E. Models of Palliative Care Delivery for Patients With Cancer. J. Clin. Oncol. 2020, 38, 852–865. [Google Scholar] [CrossRef]
- Stegmann, M.E.; Geerse, O.P.; van Zuylen, L.; Nekhlyudov, L.; Brandenbarg, D. Improving Care for Patients Living with Prolonged Incurable Cancer. Cancers 2021, 13, 2555. [Google Scholar] [CrossRef] [PubMed]
- van Elk, M.; Murphy, B.P.; Eufrásio-da-Silva, T.; O’Reilly, D.P.; Vermonden, T.; Hennink, W.E.; Duffy, G.P.; Ruiz-Hernández, E. Nanomedicines for Advanced Cancer Treatments: Transitioning towards Responsive Systems. Int. J. Pharm. 2016, 515, 132–164. [Google Scholar] [CrossRef]
- Diep, Y.N.; Kim, T.J.; Cho, H.; Lee, L.P. Nanomedicine for Advanced Cancer Immunotherapy. J. Control. Release 2022, 351, 1017–1037. [Google Scholar] [CrossRef]
- Johnson, P.C.; Jacobson, C.; Yi, A.; Saucier, A.; Dhawale, T.M.; Nelson, A.; Lavoie, M.W.; Reynolds, M.J.; Topping, C.E.W.; Frigault, M.J.; et al. Healthcare Utilization and End-of-Life Outcomes in Patients Receiving CAR T-Cell Therapy. J. Natl. Compr. Cancer Netw. 2021, 19, 928–934. [Google Scholar] [CrossRef]
- Miliotou, A.N.; Papadopoulou, L.C. CAR T-Cell Therapy: A New Era in Cancer Immunotherapy. Curr. Pharm. Biotechnol. 2018, 19, 5–18. [Google Scholar] [CrossRef]
- Maher, J.; Brentjens, R.J.; Gunset, G.; Rivière, I.; Sadelain, M. Human T-Lymphocyte Cytotoxicity and Proliferation Directed by a Single Chimeric TCRζ/CD28 Receptor. Nat. Biotechnol. 2002, 20, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.A.; Walsh, D.; Abdullah, O.; McDonnell, F.; Homsi, J.; Komurcu, S.; LeGrand, S.B.; Zhukovsky, D.S. Common Complications of Advanced Cancer. Semin. Oncol. 2000, 27, 34–44. [Google Scholar]
- Laird, B.J.; McMillan, D.C.; Fayers, P.; Fearon, K.; Kaasa, S.; Fallon, M.T.; Klepstad, P. The Systemic Inflammatory Response and Its Relationship to Pain and Other Symptoms in Advanced Cancer. Oncologist 2013, 18, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Aburub, A.S.; Gagnon, B.; Rodríguez, A.M.; Mayo, N.E. Agreement between Personally Generated Areas of Quality of Life Concern and Standard Outcome Measures in People with Advanced Cancer. Support. Care Cancer 2016, 24, 3831–3838. [Google Scholar] [CrossRef]
- von Haehling, S.; Anker, S.D. Prevalence, Incidence and Clinical Impact of Cachexia: Facts and Numbers-Update 2014. J. Cachexia Sarcopenia Muscle 2014, 5, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.F.; Rohm, M.; Herzig, S.; Berriel Diaz, M. Cancer Cachexia: More Than Skeletal Muscle Wasting. Trends Cancer 2018, 4, 849–860. [Google Scholar] [CrossRef]
- Evans, W.J.; Morley, J.E.; Argilés, J.; Bales, C.; Baracos, V.; Guttridge, D.; Jatoi, A.; Kalantar-Zadeh, K.; Lochs, H.; Mantovani, G.; et al. Cachexia: A New Definition. Clin. Nutr. 2008, 27, 793–799. [Google Scholar] [CrossRef]
- Zhang, Q.; Song, M.-M.; Zhang, X.; Ding, J.-S.; Ruan, G.-T.; Zhang, X.-W.; Liu, T.; Yang, M.; Ge, Y.-Z.; Tang, M.; et al. Association of Systemic Inflammation with Survival in Patients with Cancer Cachexia: Results from a Multicentre Cohort Study. J. Cachexia Sarcopenia Muscle 2021, 12, 1466–1476. [Google Scholar] [CrossRef]
- Cole, C.L.; Kleckner, I.R.; Jatoi, A.; Schwarz, E.M.; Dunne, R.F. The Role of Systemic Inflammation in Cancer-Associated Muscle Wasting and Rationale for Exercise as a Therapeutic Intervention. JCSM Clin. Rep. 2018, 3, e00065. [Google Scholar] [CrossRef]
- Wyart, E.; Bindels, L.B.; Mina, E.; Menga, A.; Stanga, S.; Porporato, P.E. Cachexia, a Systemic Disease beyond Muscle Atrophy. Int. J. Mol. Sci. 2020, 21, 8592. [Google Scholar] [CrossRef]
- Amano, K.; Baracos, V.E.; Morita, T.; Miura, T.; Mori, N.; Tatara, R.; Kessoku, T.; Tokoro, A.; Tagami, K.; Otani, H.; et al. The Impact of Cachexia on Dietary Intakes, Symptoms, and Quality of Life in Advanced Cancer. JCSM Rapid Commun. 2022, 5, 162–170. [Google Scholar] [CrossRef]
- LeBlanc, T.W.; Nipp, R.D.; Rushing, C.N.; Samsa, G.P.; Locke, S.C.; Kamal, A.H.; Cella, D.F.; Abernethy, A.P. Correlation Between the International Consensus Definition of the Cancer Anorexia-Cachexia Syndrome (CACS) and Patient-Centered Outcomes in Advanced Non-Small Cell Lung Cancer. J. Pain Symptom Manag. 2015, 49, 680–689. [Google Scholar] [CrossRef] [PubMed]
- Gale, N.; Wasley, D.; Roberts, S.; Backx, K.; Nelson, A.; van Deursen, R.; Byrne, A. A Longitudinal Study of Muscle Strength and Function in Patients with Cancer Cachexia. Support. Care Cancer 2019, 27, 131–137. [Google Scholar] [CrossRef]
- Crawford, J. What Are the Criteria for Response to Cachexia Treatment? Ann. Palliat. Med. 2019, 8, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Baracos, V.E.; Mazurak, V.C.; Bhullar, A.S. Cancer Cachexia Is Defined by an Ongoing Loss of Skeletal Muscle Mass. Ann. Palliat. Med. 2019, 8, 3–12. [Google Scholar] [CrossRef]
- Xie, H.; Ruan, G.; Wei, L.; Zhang, H.; Ge, Y.; Zhang, Q.; Lin, S.; Song, M.; Zhang, X.; Liu, X.; et al. Hand Grip Strength-Based Cachexia Index as a Predictor of Cancer Cachexia and Prognosis in Patients with Cancer. J. Cachexia Sarcopenia Muscle 2023, 14, 382–390. [Google Scholar] [CrossRef]
- Stephens, N.A.; Gray, C.; MacDonald, A.J.; Tan, B.H.; Gallagher, I.J.; Skipworth, R.J.E.; Ross, J.A.; Fearon, K.C.H.; Greig, C.A. Sexual Dimorphism Modulates the Impact of Cancer Cachexia on Lower Limb Muscle Mass and Function. Clin. Nutr. 2012, 31, 499–505. [Google Scholar] [CrossRef]
- Naito, T.; Okayama, T.; Aoyama, T.; Ohashi, T.; Masuda, Y.; Kimura, M.; Shiozaki, H.; Murakami, H.; Kenmotsu, H.; Taira, T.; et al. Skeletal Muscle Depletion during Chemotherapy Has a Large Impact on Physical Function in Elderly Japanese Patients with Advanced Non-Small-Cell Lung Cancer. BMC Cancer 2017, 17, 571. [Google Scholar] [CrossRef]
- Roy, I.; Huang, K.; Bhakta, A.; Marquez, E.; Spangenberg, J.; Jayabalan, P. Relationship Between Cachexia and the Functional Progress of Patients With Cancer in Inpatient Rehabilitation. Am. J. Phys. Med. Rehabil. 2023, 102, 99–104. [Google Scholar] [CrossRef]
- Muhandiramge, J.; Orchard, S.G.; Warner, E.T.; van Londen, G.J.; Zalcberg, J.R. Functional Decline in the Cancer Patient: A Review. Cancers 2022, 14, 1368. [Google Scholar] [CrossRef]
- Cheville, A. Rehabilitation of Patients with Advanced Cancer. Cancer 2001, 92, 1039–1048. [Google Scholar] [CrossRef]
- Viganó, A.; Bruera, E.; Jhangri, G.S.; Newman, S.C.; Fields, A.L.; Suarez-Almazor, M.E. Clinical Survival Predictors in Patients with Advanced Cancer. Arch. Intern. Med. 2000, 160, 861–868. [Google Scholar] [CrossRef]
- Ezzatvar, Y.; Ramírez-Vélez, R.; Sáez de Asteasu, M.L.; Martínez-Velilla, N.; Zambom-Ferraresi, F.; Izquierdo, M.; García-Hermoso, A. Physical Function and All-Cause Mortality in Older Adults Diagnosed With Cancer: A Systematic Review and Meta-Analysis. J. Gerontol. Ser. A 2021, 76, 1447–1453. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.W.; Hornsby, W.E.; Goetzinger, A.; Forbes, L.M.; Sherrard, E.L.; Quist, M.; Lane, A.T.; West, M.; Eves, N.D.; Gradison, M.; et al. Prognostic Significance of Functional Capacity and Exercise Behavior in Patients with Metastatic Non-Small Cell Lung Cancer. Lung Cancer 2012, 76, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Fram, J.; Vail, C.; Roy, I. Assessment of Cancer-Associated Cachexia—How to Approach Physical Function Evaluation. Curr. Oncol. Rep. 2022, 24, 751–761. [Google Scholar] [CrossRef] [PubMed]
- Cheville, A.L.; Yost, K.J.; Larson, D.R.; Dos Santos, K.; O’Byrne, M.M.; Chang, M.T.; Therneau, T.M.; Diehn, F.E.; Yang, P. Performance of an Item Response Theory-Based Computer Adaptive Test in Identifying Functional Decline. Arch. Phys. Med. Rehabil. 2012, 93, 1153–1160. [Google Scholar] [CrossRef]
- Bland, K.A.; Harrison, M.; Zopf, E.M.; Sousa, M.S.; Currow, D.C.; Ely, M.; Agar, M.; Butcher, B.E.; Vaughan, V.; Dowd, A.; et al. Quality of Life and Symptom Burden Improve in Patients Attending a Multidisciplinary Clinical Service for Cancer Cachexia: A Retrospective Observational Review. J. Pain Symptom Manag. 2021, 62, e164–e176. [Google Scholar] [CrossRef]
- Bland, K.A.; Zopf, E.M.; Harrison, M.; Ely, M.; Cormie, P.; Liu, E.; Dowd, A.; Martin, P. Prognostic Markers of Overall Survival in Cancer Patients Attending a Cachexia Support Service: An Evaluation of Clinically Assessed Physical Function, Malnutrition and Inflammatory Status. Nutr. Cancer 2021, 73, 1400–1410. [Google Scholar] [CrossRef]
- Kasymjanova, G.; Correa, J.A.; Kreisman, H.; Dajczman, E.; Pepe, C.; Dobson, S.; Lajeunesse, L.; Sharma, R.; Small, D. Prognostic Value of the Six-Minute Walk in Advanced Non-Small Cell Lung Cancer. J. Thorac. Oncol. 2009, 4, 602–607. [Google Scholar] [CrossRef]
- Rodríguez-Cañamero, S.; Cobo-Cuenca, A.I.; Carmona-Torres, J.M.; Pozuelo-Carrascosa, D.P.; Santacruz-Salas, E.; Rabanales-Sotos, J.A.; Cuesta-Mateos, T.; Laredo-Aguilera, J.A. Impact of Physical Exercise in Advanced-Stage Cancer Patients: Systematic Review and Meta-Analysis. Cancer Med. 2022, 11, 3714–3727. [Google Scholar] [CrossRef]
- Ester, M.; Culos-Reed, S.N.; Abdul-Razzak, A.; Daun, J.T.; Duchek, D.; Francis, G.; Bebb, G.; Black, J.; Arlain, A.; Gillis, C.; et al. Feasibility of a Multimodal Exercise, Nutrition, and Palliative Care Intervention in Advanced Lung Cancer. BMC Cancer 2021, 21, 159. [Google Scholar] [CrossRef] [PubMed]
- Cheville, A.L.; Moynihan, T.; Herrin, J.; Loprinzi, C.; Kroenke, K. Effect of Collaborative Telerehabilitation on Functional Impairment and Pain Among Patients With Advanced-Stage Cancer. JAMA Oncol. 2019, 5, 644. [Google Scholar] [CrossRef] [PubMed]
- De Craene, B.; Berx, G. Regulatory Networks Defining EMT during Cancer Initiation and Progression. Nat. Rev. Cancer 2013, 13, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Lamouille, S.; Xu, J.; Derynck, R. Molecular Mechanisms of Epithelial-Mesenchymal Transition. Nat. Rev. Mol. Cell Biol. 2014, 15, 178–196. [Google Scholar] [CrossRef]
- Bakhoum, S.F.; Ngo, B.; Laughney, A.M.; Cavallo, J.-A.; Murphy, C.J.; Ly, P.; Shah, P.; Sriram, R.K.; Watkins, T.B.K.; Taunk, N.K.; et al. Chromosomal Instability Drives Metastasis through a Cytosolic DNA Response. Nature 2018, 553, 467–472. [Google Scholar] [CrossRef]
- Gupta, P.B.; Kuperwasser, C.; Brunet, J.-P.; Ramaswamy, S.; Kuo, W.-L.; Gray, J.W.; Naber, S.P.; Weinberg, R.A. The Melanocyte Differentiation Program Predisposes to Metastasis after Neoplastic Transformation. Nat. Genet. 2005, 37, 1047–1054. [Google Scholar] [CrossRef]
- Anderson, R.L.; Balasas, T.; Callaghan, J.; Coombes, R.C.; Evans, J.; Hall, J.A.; Kinrade, S.; Jones, D.; Jones, P.S.; Jones, R.; et al. A Framework for the Development of Effective Anti-Metastatic Agents. Nat. Rev. Clin. Oncol. 2019, 16, 185–204. [Google Scholar] [CrossRef]
- Ganesh, K.; Massague, J. Targeting Metastatic Cancer. Nat. Med. 2021, 27, 34–44. [Google Scholar] [CrossRef]
- Roy, I.; McAllister, D.M.; Gorse, E.; Dixon, K.; Piper, C.T.; Zimmerman, N.P.; Getschman, A.E.; Tsai, S.; Engle, D.D.; Evans, D.B.; et al. Pancreatic Cancer Cell Migration and Metastasis Is Regulated by Chemokine-Biased Agonism and Bioenergetic Signaling. Cancer Res. 2015, 75, 3529–3542. [Google Scholar] [CrossRef]
- Gomes, A.P.; Ilter, D.; Low, V.; Drapela, S.; Schild, T.; Mullarky, E.; Han, J.; Elia, I.; Broekaert, D.; Rosenzweig, A.; et al. Altered Propionate Metabolism Contributes to Tumour Progression and Aggressiveness. Nat. Metab. 2022, 4, 435–443. [Google Scholar] [CrossRef]
- Bergers, G.; Fendt, S.-M. The Metabolism of Cancer Cells during Metastasis. Nat. Rev. Cancer 2021, 21, 162–180. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, A.; Given, C.W.; Given, B.; Sikorskii, A. Quality of Life among Patients with Primary, Metastatic and Recurrent Cancer. Eur. J. Cancer Care 2009, 18, 84–96. [Google Scholar] [CrossRef]
- Gupta, D.; Lis, C.G.; Granick, J.; Grutsch, J.F.; Vashi, P.G.; Lammersfeld, C.A. Malnutrition Was Associated with Poor Quality of Life in Colorectal Cancer: A Retrospective Analysis. J. Clin. Epidemiol. 2006, 59, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Segura, A.; Pardo, J.; Jara, C.; Zugazabeitia, L.; Carulla, J.; de Las Peñas, R.; García-Cabrera, E.; Luz Azuara, M.; Casadó, J.; Gómez-Candela, C. An Epidemiological Evaluation of the Prevalence of Malnutrition in Spanish Patients with Locally Advanced or Metastatic Cancer. Clin. Nutr. 2005, 24, 801–814. [Google Scholar] [CrossRef] [PubMed]
- Bossi, P.; Delrio, P.; Mascheroni, A.; Zanetti, M. The Spectrum of Malnutrition/Cachexia/Sarcopenia in Oncology According to Different Cancer Types and Settings: A Narrative Review. Nutrients 2021, 13, 1980. [Google Scholar] [CrossRef]
- Sánchez-Torralvo, F.J.; Contreras-Bolívar, V.; Ruiz-Vico, M.; Abuín-Fernández, J.; González-Almendros, I.; Barrios, M.; Olveira, G. Relationship between Malnutrition and the Presence of Symptoms of Anxiety and Depression in Hospitalized Cancer Patients. Support. Care Cancer 2022, 30, 1607–1613. [Google Scholar] [CrossRef] [PubMed]
- Trutschnigg, B.; Kilgour, R.D.; Morais, J.A.; Lucar, E.; Hornby, L.; Molla, H.; Vigano, A. Metabolic, Nutritional and Inflammatory Characteristics in Elderly Women with Advanced Cancer. J. Geriatr. Oncol. 2013, 4, 183–189. [Google Scholar] [CrossRef]
- Ferreira, V.; Lawson, C.; Gillis, C.; Scheede-Bergdahl, C.; Chevalier, S.; Carli, F. Malnourished Lung Cancer Patients Have Poor Baseline Functional Capacity but Show Greatest Improvements with Multimodal Prehabilitation. Nutr. Clin. Pract. 2021, 36, 1011–1019. [Google Scholar] [CrossRef]
- Song, M.; Zhang, Q.; Tang, M.; Zhang, X.; Ruan, G.; Zhang, X.; Zhang, K.; Ge, Y.; Yang, M.; Li, Q.; et al. Associations of Low Hand Grip Strength with 1 Year Mortality of Cancer Cachexia: A Multicentre Observational Study. J. Cachexia Sarcopenia Muscle 2021, 12, 1489–1500. [Google Scholar] [CrossRef]
- Hadzibegovic, S.; Porthun, J.; Lena, A.; Weinländer, P.; Lück, L.C.; Potthoff, S.K.; Rösnick, L.; Fröhlich, A.; Ramer, L.V.; Sonntag, F.; et al. Hand Grip Strength in Patients with Advanced Cancer: A Prospective Study. J. Cachexia Sarcopenia Muscle 2023, 14, 1682–1694. [Google Scholar] [CrossRef]
- Poisson, J.; Martinez-Tapia, C.; Heitz, D.; Geiss, R.; Albrand, G.; Falandry, C.; Gisselbrecht, M.; Couderc, A.-L.; Boulahssass, R.; Liuu, E.; et al. Prevalence and Prognostic Impact of Cachexia among Older Patients with Cancer: A Nationwide Cross-Sectional Survey (NutriAgeCancer). J. Cachexia Sarcopenia Muscle 2021, 12, 1477–1488. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.; Sayers, J.; Anker, S.D.; Arends, J.; Balstad, T.R.; Baracos, V.; Brown, L.; Bye, A.; Dajani, O.; Dolan, R.; et al. Physical Function Endpoints in Cancer Cachexia Clinical Trials: Systematic Review 1 of the Cachexia Endpoints Series. J. Cachexia Sarcopenia Muscle 2023, 14, 1932–1948. [Google Scholar] [CrossRef]
- Douglas, E.; McMillan, D.C. Towards a Simple Objective Framework for the Investigation and Treatment of Cancer Cachexia: The Glasgow Prognostic Score. Cancer Treat. Rev. 2014, 40, 685–691. [Google Scholar] [CrossRef]
- Martin, L.; Senesse, P.; Gioulbasanis, I.; Antoun, S.; Bozzetti, F.; Deans, C.; Strasser, F.; Thoresen, L.; Jagoe, R.T.; Chasen, M.; et al. Diagnostic Criteria for the Classification of Cancer-Associated Weight Loss. J. Clin. Oncol. 2015, 33, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Fearon, K.; Strasser, F.; Anker, S.D.; Bosaeus, I.; Bruera, E.; Fainsinger, R.L.; Jatoi, A.; Loprinzi, C.; MacDonald, N.; Mantovani, G.; et al. Definition and Classification of Cancer Cachexia: An International Consensus. Lancet Oncol. 2011, 12, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Wang, B.; Liu, H.; Yang, K.; Thapa, S.; Zhang, H.; Li, L.; Yu, S. Development and Validation of a Clinically Applicable Score to Classify Cachexia Stages in Advanced Cancer Patients. J. Cachexia Sarcopenia Muscle 2018, 9, 306–314. [Google Scholar] [CrossRef]
- Amano, K.; Hopkinson, J.; Baracos, V. Psychological Symptoms of Illness and Emotional Distress in Advanced Cancer Cachexia. Curr. Opin. Clin. Nutr. Metab. Care 2022, 25, 167–172. [Google Scholar] [CrossRef]
- Kir, S.; White, J.P.; Kleiner, S.; Kazak, L.; Cohen, P.; Baracos, V.E.; Spiegelman, B.M. Tumour-Derived PTH-Related Protein Triggers Adipose Tissue Browning and Cancer Cachexia. Nature 2014, 513, 100–104. [Google Scholar] [CrossRef]
- Argilés, J.M.; Busquets, S.; Stemmler, B.; López-Soriano, F.J. Cancer Cachexia: Understanding the Molecular Basis. Nat. Rev. Cancer 2014, 14, 754–762. [Google Scholar] [CrossRef]
- Mitnitski, A.B.; Mogilner, A.J.; MacKnight, C.; Rockwood, K. The Mortality Rate as a Function of Accumulated Deficits in a Frailty Index. Mech. Ageing Dev. 2002, 123, 1457–1460. [Google Scholar] [CrossRef]
- Ma, L.; Chan, P. Understanding the Physiological Links Between Physical Frailty and Cognitive Decline. Aging Dis. 2020, 11, 405–418. [Google Scholar] [CrossRef] [PubMed]
- Bortone, I.; Sardone, R.; Lampignano, L.; Castellana, F.; Zupo, R.; Lozupone, M.; Moretti, B.; Giannelli, G.; Panza, F. How Gait Influences Frailty Models and Health-Related Outcomes in Clinical-Based and Population-Based Studies: A Systematic Review. J. Cachexia Sarcopenia Muscle 2021, 12, 274–297. [Google Scholar] [CrossRef] [PubMed]
- Pamoukdjian, F.; Paillaud, E.; Zelek, L.; Laurent, M.; Lévy, V.; Landre, T.; Sebbane, G. Measurement of Gait Speed in Older Adults to Identify Complications Associated with Frailty: A Systematic Review. J. Geriatr. Oncol. 2015, 6, 484–496. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.A.; DuMontier, C.; Murillo, A.; Hshieh, T.T.; Bean, J.F.; Soiffer, R.J.; Stone, R.M.; Abel, G.A.; Driver, J.A. Gait Speed, Grip Strength, and Clinical Outcomes in Older Patients with Hematologic Malignancies. Blood 2019, 134, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Goede, V. Frailty and Cancer: Current Perspectives on Assessment and Monitoring. Clin. Interv. Aging 2023, 18, 505–521. [Google Scholar] [CrossRef] [PubMed]
- Morris, R.; Lewis, A. Falls and Cancer. Clin. Oncol. 2020, 32, 569–578. [Google Scholar] [CrossRef]
- Stone, C.A.; Lawlor, P.G.; Savva, G.M.; Bennett, K.; Kenny, R.A. Prospective Study of Falls and Risk Factors for Falls in Adults With Advanced Cancer. J. Clin. Oncol. 2012, 30, 2128–2133. [Google Scholar] [CrossRef]
- Toomey, A.; Friedman, L. Mortality in Cancer Patients after a Fall-Related Injury: The Impact of Cancer Spread and Type. Injury 2014, 45, 1710–1716. [Google Scholar] [CrossRef]
- Fabi, A.; Bhargava, R.; Fatigoni, S.; Guglielmo, M.; Horneber, M.; Roila, F.; Weis, J.; Jordan, K.; Ripamonti, C.I. Cancer-Related Fatigue: ESMO Clinical Practice Guidelines for Diagnosis and Treatment. Ann. Oncol. 2020, 31, 713–723. [Google Scholar] [CrossRef]
- Bower, J.E. Cancer-Related Fatigue--Mechanisms, Risk Factors, and Treatments. Nat. Rev. Clin. Oncol. 2014, 11, 597–609. [Google Scholar] [CrossRef]
- Feng, L.R.; Regan, J.; Shrader, J.A.; Liwang, J.; Ross, A.; Kumar, S.; Saligan, L.N. Cognitive and Motor Aspects of Cancer-Related Fatigue. Cancer Med. 2019, 8, 5840–5849. [Google Scholar] [CrossRef] [PubMed]
- Mo, J.; Darke, A.K.; Guthrie, K.A.; Sloan, J.A.; Unger, J.M.; Hershman, D.L.; O’Rourke, M.; Bakitas, M.; Krouse, R.S. Association of Fatigue and Outcomes in Advanced Cancer: An Analysis of Four SWOG Treatment Trials. JCO Oncol. Pract. 2021, 17, e1246–e1257. [Google Scholar] [CrossRef]
- Tornero-Aguilera, J.F.; Jimenez-Morcillo, J.; Rubio-Zarapuz, A.; Clemente-Suárez, V.J. Central and Peripheral Fatigue in Physical Exercise Explained: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 3909. [Google Scholar] [CrossRef] [PubMed]
- Yavuzsen, T.; Davis, M.P.; Ranganathan, V.K.; Walsh, D.; Siemionow, V.; Kirkova, J.; Khoshknabi, D.; Lagman, R.; LeGrand, S.; Yue, G.H. Cancer-Related Fatigue: Central or Peripheral? J. Pain Symptom Manag. 2009, 38, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Hendrix, C.C. Cancer-Related Cognitive Impairment in Breast Cancer Patients: Influences of Psychological Variables. Asia Pac. J. Oncol. Nurs. 2018, 5, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Lange, M.; Joly, F.; Vardy, J.; Ahles, T.; Dubois, M.; Tron, L.; Winocur, G.; De Ruiter, M.B.; Castel, H. Cancer-Related Cognitive Impairment: An Update on State of the Art, Detection, and Management Strategies in Cancer Survivors. Ann. Oncol. 2019, 30, 1925–1940. [Google Scholar] [CrossRef]
- Oh, P.-J. Predictors of Cognitive Decline in People with Cancer Undergoing Chemotherapy. Eur. J. Oncol. Nurs. 2017, 27, 53–59. [Google Scholar] [CrossRef]
- Molassiotis, A.; Wang, M. Care Needs of Older Patients with Advanced Cancer. Curr. Opin. Support. Palliat. Care 2023, 17, 31–36. [Google Scholar] [CrossRef]
- Argyriou, A.A.; Assimakopoulos, K.; Iconomou, G.; Giannakopoulou, F.; Kalofonos, H.P. Either Called “Chemobrain” or “Chemofog,” the Long-Term Chemotherapy-Induced Cognitive Decline in Cancer Survivors Is Real. J. Pain Symptom Manag. 2011, 41, 126–139. [Google Scholar] [CrossRef]
- Wefel, J.S.; Parsons, M.W.; Gondi, V.; Brown, P.D. Neurocognitive Aspects of Brain Metastasis. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2018; pp. 155–165. [Google Scholar]
- Biglia, N.; Bounous, V.E.; Malabaila, A.; Palmisano, D.; Torta, D.M.E.; D’alonzo, M.; Sismondi, P.; Torta, R. Objective and Self-Reported Cognitive Dysfunction in Breast Cancer Women Treated with Chemotherapy: A Prospective Study. Eur. J. Cancer Care 2012, 21, 485–492. [Google Scholar] [CrossRef]
- Versluis, M.A.J.; Raijmakers, N.J.H.; Baars, A.; van den Beuken-van Everdingen, M.H.J.; de Graeff, A.; Hendriks, M.P.; de Jong, W.K.; Kloover, J.S.; Kuip, E.J.M.; Mandigers, C.M.P.W.; et al. Trajectories of Health-Related Quality of Life and Symptom Burden in Patients with Advanced Cancer towards the End of Life: Longitudinal Results from the EQuiPe Study. Cancer 2023. [Google Scholar] [CrossRef] [PubMed]
- Murphy, K.T.; Chee, A.; Trieu, J.; Naim, T.; Lynch, G.S. Importance of Functional and Metabolic Impairments in the Characterization of the C-26 Murine Model of Cancer Cachexia. Dis. Models Mech. 2012, 5, 533–545. [Google Scholar] [CrossRef] [PubMed]
- van de Worp, W.R.P.H.; Theys, J.; González, A.S.; van der Heyden, B.; Verhaegen, F.; Hauser, D.; Caiment, F.; Smeets, H.J.M.; Schols, A.M.W.J.; van Helvoort, A.; et al. A Novel Orthotopic Mouse Model Replicates Human Lung Cancer Cachexia. J. Cachexia Sarcopenia Muscle 2023, 14, 1410–1423. [Google Scholar] [CrossRef] [PubMed]
- Michaelis, K.A.; Zhu, X.; Burfeind, K.G.; Krasnow, S.M.; Levasseur, P.R.; Morgan, T.K.; Marks, D.L. Establishment and Characterization of a Novel Murine Model of Pancreatic Cancer Cachexia. J. Cachexia Sarcopenia Muscle 2017, 8, 824–838. [Google Scholar] [CrossRef]
- Voltarelli, F.A.; Frajacomo, F.T.; de Padilha, C.S.; Testa, M.T.J.; Cella, P.S.; Ribeiro, D.F.; de Oliveira, D.X.; Veronez, L.C.; Bisson, G.S.; Moura, F.A.; et al. Syngeneic B16F10 Melanoma Causes Cachexia and Impaired Skeletal Muscle Strength and Locomotor Activity in Mice. Front. Physiol. 2017, 8, 715. [Google Scholar] [CrossRef] [PubMed]
- Olson, B.; Norgard, M.A.; Levasseur, P.R.; Zhu, X.; Marks, D.L. Physiologic and Molecular Characterization of a Novel Murine Model of Metastatic Head and Neck Cancer Cachexia. J. Cachexia Sarcopenia Muscle 2021, 12, 1312–1332. [Google Scholar] [CrossRef]
- Vanderveen, B.N.; Fix, D.K.; Counts, B.R.; Carson, J.A. The Effect of Wheel Exercise on Functional Indices of Cachexia in Tumor-Bearing Mice. Med. Sci. Sports Exerc. 2020, 52, 2320–2330. [Google Scholar] [CrossRef]
- VanderVeen, B.N.; Hardee, J.P.; Fix, D.K.; Carson, J.A. Skeletal Muscle Function during the Progression of Cancer Cachexia in the Male Apc Min/+ Mouse. J. Appl. Physiol. 2018, 124, 684–695. [Google Scholar] [CrossRef]
- Paval, D.R.; Patton, R.; McDonald, J.; Skipworth, R.J.E.; Gallagher, I.J.; Laird, B.J. A Systematic Review Examining the Relationship between Cytokines and Cachexia in Incurable Cancer. J. Cachexia Sarcopenia Muscle 2022, 13, 824–838. [Google Scholar] [CrossRef]
- Anderson, L.J.; Lee, J.; Mallen, M.C.; Migula, D.; Liu, H.; Wu, P.C.; Dash, A.; Garcia, J.M. Evaluation of Physical Function and Its Association with Body Composition, Quality of Life and Biomarkers in Cancer Cachexia Patients. Clin. Nutr. 2021, 40, 978–986. [Google Scholar] [CrossRef]
- Chen, J.L.; Walton, K.L.; Qian, H.; Colgan, T.D.; Hagg, A.; Watt, M.J.; Harrison, C.A.; Gregorevic, P. Differential Effects of IL6 and Activin A in the Development of Cancer-Associated Cachexia. Cancer Res. 2016, 76, 5372–5382. [Google Scholar] [CrossRef] [PubMed]
- Rausch, V.; Sala, V.; Penna, F.; Porporato, P.E.; Ghigo, A. Understanding the Common Mechanisms of Heart and Skeletal Muscle Wasting in Cancer Cachexia. Oncogenesis 2021, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Carson, J.A.; Baltgalvis, K.A. Interleukin 6 as a Key Regulator of Muscle Mass during Cachexia. Exerc. Sport Sci. Rev. 2010, 38, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Baltgalvis, K.A.; Berger, F.G.; Peña, M.M.O.; Mark Davis, J.; White, J.P.; Carson, J.A. Activity Level, Apoptosis, and Development of Cachexia in Apc(Min/+) Mice. J. Appl. Physiol. 2010, 109, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Yuan, L.; Han, J.; Meng, Q.; Xi, Q.; Zhuang, Q.; Jiang, Y.; Han, Y.; Zhang, B.; Fang, J.; Wu, G. Muscle-Specific E3 Ubiquitin Ligases Are Involved in Muscle Atrophy of Cancer Cachexia: An in Vitro and in Vivo Study. Oncol. Rep. 2015, 33, 2261–2268. [Google Scholar] [CrossRef]
- Neyroud, D.; Laitano, O.; Dasgupta, A.; Lopez, C.; Schmitt, R.E.; Schneider, J.Z.; Hammers, D.W.; Sweeney, H.L.; Walter, G.A.; Doles, J.; et al. Blocking Muscle Wasting via Deletion of the Muscle-Specific E3 Ligase MuRF1 Impedes Pancreatic Tumor Growth. Commun. Biol. 2023, 6, 519. [Google Scholar] [CrossRef] [PubMed]
- Scheede-Bergdahl, C.; Watt, H.L.; Trutschnigg, B.; Kilgour, R.D.; Haggarty, A.; Lucar, E.; Vigano, A. Is IL-6 the Best pro-Inflammatory Biomarker of Clinical Outcomes of Cancer Cachexia? Clin. Nutr. 2012, 31, 85–88. [Google Scholar] [CrossRef]
- Narasimhan, A.; Ghosh, S.; Stretch, C.; Greiner, R.; Bathe, O.F.; Baracos, V.; Damaraju, S. Small RNAome Profiling from Human Skeletal Muscle: Novel MiRNAs and Their Targets Associated with Cancer Cachexia. J. Cachexia Sarcopenia Muscle 2017, 8, 405–416. [Google Scholar] [CrossRef]
- Powrózek, T.; Mlak, R.; Brzozowska, A.; Mazurek, M.; Gołębiowski, P.; Małecka-Massalska, T. MiRNA-130a Significantly Improves Accuracy of SGA Nutritional Assessment Tool in Prediction of Malnutrition and Cachexia in Radiotherapy-Treated Head and Neck Cancer Patients. Cancers 2018, 10, 294. [Google Scholar] [CrossRef]
- Thibaut, M.M.; Sboarina, M.; Roumain, M.; Pötgens, S.A.; Neyrinck, A.M.; Destrée, F.; Gillard, J.; Leclercq, I.A.; Dachy, G.; Demoulin, J.-B.; et al. Inflammation-Induced Cholestasis in Cancer Cachexia. J. Cachexia Sarcopenia Muscle 2021, 12, 70–90. [Google Scholar] [CrossRef]
- Falconer, J.S.; Fearon, K.C.; Plester, C.E.; Ross, J.A.; Carter, D.C. Cytokines, the Acute-Phase Response, and Resting Energy Expenditure in Cachectic Patients with Pancreatic Cancer. Ann. Surg. 1994, 219, 325–331. [Google Scholar] [CrossRef] [PubMed]
- das Neves, R.X.; Yamashita, A.S.; Riccardi, D.M.R.; Köhn-Gaone, J.; Camargo, R.G.; Neto, N.I.; Caetano, D.; Gomes, S.P.; Santos, F.H.; Lima, J.D.C.C.; et al. Cachexia Causes Time-Dependent Activation of the Inflammasome in the Liver. J. Cachexia Sarcopenia Muscle 2023, 14, 1621–1630. [Google Scholar] [CrossRef] [PubMed]
- Biswas, A.K.; Acharyya, S. Understanding Cachexia in the Context of Metastatic Progression. Nat. Rev. Cancer 2020, 20, 274–284. [Google Scholar] [CrossRef]
- Braun, T.P.; Zhu, X.; Szumowski, M.; Scott, G.D.; Grossberg, A.J.; Levasseur, P.R.; Graham, K.; Khan, S.; Damaraju, S.; Colmers, W.F.; et al. Central Nervous System Inflammation Induces Muscle Atrophy via Activation of the Hypothalamic-Pituitary-Adrenal Axis. J. Exp. Med. 2011, 208, 2449–2463. [Google Scholar] [CrossRef]
- Chaves, F.M.; Mansano, N.S.; Frazão, R.; Donato, J. Tumor Necrosis Factor α and Interleukin-1β Acutely Inhibit AgRP Neurons in the Arcuate Nucleus of the Hypothalamus. Int. J. Mol. Sci. 2020, 21, 8928. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.H.; Hrupka, B.J.; Altreuther, G.; Arnold, M.; Langhans, W. Inhibition of TNF-Alpha Production Contributes to the Attenuation of LPS-Induced Hypophagia by Pentoxifylline. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000, 279, R2113–R2120. [Google Scholar] [CrossRef] [PubMed]
- Borner, T.; Shaulson, E.D.; Ghidewon, M.Y.; Barnett, A.B.; Horn, C.C.; Doyle, R.P.; Grill, H.J.; Hayes, M.R.; De Jonghe, B.C. GDF15 Induces Anorexia through Nausea and Emesis. Cell Metab. 2020, 31, 351–362.e5. [Google Scholar] [CrossRef]
- Olson, B.; Diba, P.; Korzun, T.; Marks, D.L. Neural Mechanisms of Cancer Cachexia. Cancers 2021, 13, 3990. [Google Scholar] [CrossRef]
- Olson, B.; Zhu, X.; Norgard, M.A.; Levasseur, P.R.; Butler, J.T.; Buenafe, A.; Burfeind, K.G.; Michaelis, K.A.; Pelz, K.R.; Mendez, H.; et al. Lipocalin 2 Mediates Appetite Suppression during Pancreatic Cancer Cachexia. Nat. Commun. 2021, 12, 2057. [Google Scholar] [CrossRef]
- Burfeind, K.G.; Zhu, X.; Norgard, M.A.; Levasseur, P.R.; Huisman, C.; Buenafe, A.C.; Olson, B.; Michaelis, K.A.; Torres, E.R.S.; Jeng, S.; et al. Circulating Myeloid Cells Invade the Central Nervous System to Mediate Cachexia during Pancreatic Cancer. eLife 2020, 9, e54095. [Google Scholar] [CrossRef]
- Olson, B.; Zhu, X.; Norgard, M.A.; Diba, P.; Levasseur, P.R.; Buenafe, A.C.; Huisman, C.; Burfeind, K.G.; Michaelis, K.A.; Kong, G.; et al. Chronic Cerebral Lipocalin 2 Exposure Elicits Hippocampal Neuronal Dysfunction and Cognitive Impairment. Brain Behav. Immun. 2021, 97, 102–118. [Google Scholar] [CrossRef]
- Coussens, L.M.; Fingleton, B.; Matrisian, L.M. Matrix Metalloproteinase Inhibitors and Cancer—Trials and Tribulations. Science 2002, 295, 2387–2392. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J. The Importance of Estimating the Therapeutic Index in the Development of Matrix Metalloproteinase Inhibitors. Cardiovasc. Res. 2006, 69, 677–687. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, S.A.; Yang, J.C.; Sherry, R.M.; Kammula, U.S.; Hughes, M.S.; Phan, G.Q.; Citrin, D.E.; Restifo, N.P.; Robbins, P.F.; Wunderlich, J.R.; et al. Durable Complete Responses in Heavily Pretreated Patients with Metastatic Melanoma Using T-Cell Transfer Immunotherapy. Clin. Cancer Res. 2011, 17, 4550–4557. [Google Scholar] [CrossRef] [PubMed]
- Vigano, A.; Del Fabbro, E.; Bruera, E.; Borod, M. The Cachexia Clinic: From Staging to Managing Nutritional and Functional Problems in Advanced Cancer Patients. Crit. Rev. Oncog. 2012, 17, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Del Fabbro, E.; Hui, D.; Dalal, S.; Dev, R.; Nooruddin, Z.I.; Bruera, E. Clinical Outcomes and Contributors to Weight Loss in a Cancer Cachexia Clinic. J. Palliat. Med. 2011, 14, 1004–1008. [Google Scholar] [CrossRef]
- Parmar, M.P.; Vanderbyl, B.L.; Kanbalian, M.; Windholz, T.Y.; Tran, A.-T.; Jagoe, R.T. A Multidisciplinary Rehabilitation Programme for Cancer Cachexia Improves Quality of Life. BMJ Support. Palliat. Care 2017, 7, 441–449. [Google Scholar] [CrossRef]
- Solheim, T.S.; Laird, B.J.A.; Balstad, T.R.; Bye, A.; Stene, G.; Baracos, V.; Strasser, F.; Griffiths, G.; Maddocks, M.; Fallon, M.; et al. Cancer Cachexia: Rationale for the MENAC (Multimodal—Exercise, Nutrition and Anti-Inflammatory Medication for Cachexia) Trial. BMJ Support. Palliat. Care 2018, 8, 258–265. [Google Scholar] [CrossRef]
- Lundholm, K.; Gelin, J.; Hyltander, A.; Lönnroth, C.; Sandström, R.; Svaninger, G.; Körner, U.; Gülich, M.; Kärrefors, I.; Norli, B. Anti-Inflammatory Treatment May Prolong Survival in Undernourished Patients with Metastatic Solid Tumors. Cancer Res. 1994, 54, 5602–5606. [Google Scholar]
- Bowers, M.; Cucchiaro, B.; Reid, J.; Slee, A. Non-steroidal Anti-inflammatory Drugs for Treatment of Cancer Cachexia: A Systematic Review. J. Cachexia Sarcopenia Muscle 2023, 14, 2473–2497. [Google Scholar] [CrossRef]
- Roeland, E.J.; Bohlke, K.; Baracos, V.E.; Bruera, E.; del Fabbro, E.; Dixon, S.; Fallon, M.; Herrstedt, J.; Lau, H.; Platek, M.; et al. Management of Cancer Cachexia: ASCO Guideline. J. Clin. Oncol. 2020, 38, 2438–2453. [Google Scholar] [CrossRef] [PubMed]
- Arends, J.; Strasser, F.; Gonella, S.; Solheim, T.S.; Madeddu, C.; Ravasco, P.; Buonaccorso, L.; de van der Schueren, M.A.E.; Baldwin, C.; Chasen, M.; et al. Cancer Cachexia in Adult Patients: ESMO Clinical Practice Guidelines☆. ESMO Open 2021, 6, 100092. [Google Scholar] [CrossRef] [PubMed]
- Hirata, H.; Tetsumoto, S.; Kijima, T.; Kida, H.; Kumagai, T.; Takahashi, R.; Otani, Y.; Inoue, K.; Kuhara, H.; Shimada, K.; et al. Favorable Responses to Tocilizumab in Two Patients With Cancer-Related Cachexia. J. Pain Symptom Manag. 2013, 46, e9–e13. [Google Scholar] [CrossRef] [PubMed]
- Rigas, J.R.; Schuster, M.; Orlov, S.V.; Milovanovic, B.; Prabhash, K.; Smith, J.T. Efect of ALD518, a Humanized Anti-IL-6 Antibody, on Lean Body Mass Loss and Symptoms in Patients with Advanced Non-Small Cell Lung Cancer (NSCLC): Results of a Phase II Randomized, Double-Blind Safety and Efficacy Trial. J. Clin. Oncol. 2010, 28, 7622. [Google Scholar] [CrossRef]
- Kotch, C.; Barrett, D.; Teachey, D.T. Tocilizumab for the Treatment of Chimeric Antigen Receptor T Cell-Induced Cytokine Release Syndrome. Expert Rev. Clin. Immunol. 2019, 15, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Si, S.; Teachey, D.T. Spotlight on Tocilizumab in the Treatment of CAR-T-Cell-Induced Cytokine Release Syndrome: Clinical Evidence to Date. Ther. Clin. Risk Manag. 2020, 16, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Advani, S.M.; Advani, P.G.; VonVille, H.M.; Jafri, S.H. Pharmacological Management of Cachexia in Adult Cancer Patients: A Systematic Review of Clinical Trials. BMC Cancer 2018, 18, 1174. [Google Scholar] [CrossRef]
- Garcia, J.M.; Boccia, R.V.; Graham, C.D.; Yan, Y.; Duus, E.M.; Allen, S.; Friend, J. Anamorelin for Patients with Cancer Cachexia: An Integrated Analysis of Two Phase 2, Randomised, Placebo-Controlled, Double-Blind Trials. Lancet Oncol. 2015, 16, 108–116. [Google Scholar] [CrossRef]
- Currow, D.; Temel, J.S.; Abernethy, A.; Milanowski, J.; Friend, J.; Fearon, K.C. ROMANA 3: A Phase 3 Safety Extension Study of Anamorelin in Advanced Non-Small-Cell Lung Cancer (NSCLC) Patients with Cachexia. Ann. Oncol. 2017, 28, 1949–1956. [Google Scholar] [CrossRef]
- Temel, J.S.; Abernethy, A.P.; Currow, D.C.; Friend, J.; Duus, E.M.; Yan, Y.; Fearon, K.C. Anamorelin in Patients with Non-Small-Cell Lung Cancer and Cachexia (ROMANA 1 and ROMANA 2): Results from Two Randomised, Double-Blind, Phase 3 Trials. Lancet Oncol. 2016, 17, 519–531. [Google Scholar] [CrossRef]
- Currow, D.; Maddocks, M.; Cella, D.; Muscaritoli, M. Efficacy of Anamorelin, a Novel Non-Peptide Ghrelin Analogue, in Patients with Advanced Non-Small Cell Lung Cancer (NSCLC) and Cachexia—Review and Expert Opinion. Int. J. Mol. Sci. 2018, 19, 3471. [Google Scholar] [CrossRef] [PubMed]
- Kim-Muller, J.Y.; Song, L.; LaCarubba Paulhus, B.; Pashos, E.; Li, X.; Rinaldi, A.; Joaquim, S.; Stansfield, J.C.; Zhang, J.; Robertson, A.; et al. GDF15 Neutralization Restores Muscle Function and Physical Performance in a Mouse Model of Cancer Cachexia. Cell Rep. 2023, 42, 111947. [Google Scholar] [CrossRef] [PubMed]
- Suriben, R.; Chen, M.; Higbee, J.; Oeffinger, J.; Ventura, R.; Li, B.; Mondal, K.; Gao, Z.; Ayupova, D.; Taskar, P.; et al. Antibody-Mediated Inhibition of GDF15-GFRAL Activity Reverses Cancer Cachexia in Mice. Nat. Med. 2020, 26, 1264–1270. [Google Scholar] [CrossRef] [PubMed]
- Breen, D.M.; Kim, H.; Bennett, D.; Calle, R.A.; Collins, S.; Esquejo, R.M.; He, T.; Joaquim, S.; Joyce, A.; Lambert, M.; et al. GDF-15 Neutralization Alleviates Platinum-Based Chemotherapy-Induced Emesis, Anorexia, and Weight Loss in Mice and Nonhuman Primates. Cell Metab. 2020, 32, 938–950.e6. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.; Calle, R.A.; Collins, S.M.; Weng, Y.; Lubaczewski, S.L.; Buckeridge, C.; Wang, E.Q.; Harrington, M.A.; Tarachandani, A.; Rossulek, M.I.; et al. Abstract CT108: First-in-Patient Study of the GDF-15 Inhibitor Ponsegromab in Patients with Cancer and Cachexia: Safety, Tolerability, and Exploratory Measures of Efficacy. Cancer Res. 2023, 83, CT108. [Google Scholar] [CrossRef]
- Zhu, X.; Callahan, M.F.; Gruber, K.A.; Szumowski, M.; Marks, D.L. Melanocortin-4 Receptor Antagonist TCMCB07 Ameliorates Cancer- and Chronic Kidney Disease-Associated Cachexia. J. Clin. Investig. 2020, 130, 4921–4934. [Google Scholar] [CrossRef]
- Zhu, X.; Roeland, E.J.; Norgard, M.A.; Gruber, K.; Potterfield, R.; Marks, D. Effect of Melanocortin-4 Receptor Antagonist TCMCB07 on Chemotherapy-Induced Anorexia and Weight Loss in Rats. J. Clin. Oncol. 2023, 41, e15196. [Google Scholar] [CrossRef]
- Axiak-Bechtel, S.M.; Leach, S.B.; Scholten, D.G.; Newton-Northup, J.R.; Johnson, B.J.; Durham, H.E.; Gruber, K.A.; Callahan, M.F. Pharmacokinetics and Safety of TCMCB07, a Melanocortin-4 Antagonist Peptide in Dogs. Pharmacol. Res. Perspect. 2021, 9, e00777. [Google Scholar] [CrossRef]
- Qi, L.K.; Zhu, X.; Gruber, K.; Roeland, E.J.; Potterfield, R.; Marks, D. Preliminary Data from the Phase I Study of TCMCB07, a Study to Assess the Safety, Tolerability and Pharmacokinetics of the Melanocortin Antagonist TCMCB07 in Healthy Subjects. J. Clin. Oncol. 2023, 41, e15195. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN Practical Guideline: Clinical Nutrition in Cancer. Clin. Nutr. 2021, 40, 2898–2913. [Google Scholar] [CrossRef]
- Ferrer, M.; Mourikis, N.; Davidson, E.E.; Kleeman, S.O.; Zaccaria, M.; Habel, J.; Rubino, R.; Gao, Q.; Flint, T.R.; Young, L.; et al. Ketogenic Diet Promotes Tumor Ferroptosis but Induces Relative Corticosterone Deficiency That Accelerates Cachexia. Cell Metab. 2023, 35, 1147–1162.e7. [Google Scholar] [CrossRef]
- Puetz, T.W.; Herring, M.P. Differential Effects of Exercise on Cancer-Related Fatigue During and Following Treatment. Am. J. Prev. Med. 2012, 43, e1–e24. [Google Scholar] [CrossRef]
- Tomlinson, D.; Diorio, C.; Beyene, J.; Sung, L. Effect of Exercise on Cancer-Related Fatigue. Am. J. Phys. Med. Rehabil. 2014, 93, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Meneses-Echávez, J.F.; González-Jiménez, E.; Ramírez-Vélez, R. Effects of Supervised Multimodal Exercise Interventions on Cancer-Related Fatigue: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Biomed. Res. Int. 2015, 2015, 328636. [Google Scholar] [CrossRef] [PubMed]
- van Vulpen, J.K.; Peeters, P.H.M.; Velthuis, M.J.; van der Wall, E.; May, A.M. Effects of Physical Exercise during Adjuvant Breast Cancer Treatment on Physical and Psychosocial Dimensions of Cancer-Related Fatigue: A Meta-Analysis. Maturitas 2016, 85, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.C.; Huedo-Medina, T.B.; Pescatello, L.S.; Pescatello, S.M.; Ferrer, R.A.; Johnson, B.T. Efficacy of Exercise Interventions in Modulating Cancer-Related Fatigue among Adult Cancer Survivors: A Meta-Analysis. Cancer Epidemiol. Biomark. Prev. 2011, 20, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Cramp, F.; Byron-Daniel, J. Exercise for the Management of Cancer-Related Fatigue in Adults. Cochrane Database Syst. Rev. 2012, 2021, CD006145. [Google Scholar] [CrossRef]
- Juvet, L.K.; Thune, I.; Elvsaas, I.K.Ø.; Fors, E.A.; Lundgren, S.; Bertheussen, G.; Leivseth, G.; Oldervoll, L.M. The Effect of Exercise on Fatigue and Physical Functioning in Breast Cancer Patients during and after Treatment and at 6 Months Follow-up: A Meta-Analysis. Breast 2017, 33, 166–177. [Google Scholar] [CrossRef]
- Keogh, J.W.L.; MacLeod, R.D. Body Composition, Physical Fitness, Functional Performance, Quality of Life, and Fatigue Benefits of Exercise for Prostate Cancer Patients: A Systematic Review. J. Pain Symptom Manag. 2012, 43, 96–110. [Google Scholar] [CrossRef]
- Mustian, K.M.; Alfano, C.M.; Heckler, C.; Kleckner, A.S.; Kleckner, I.R.; Leach, C.R.; Mohr, D.; Palesh, O.G.; Peppone, L.J.; Piper, B.F.; et al. Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue. JAMA Oncol. 2017, 3, 961. [Google Scholar] [CrossRef]
- Meneses-Echávez, J.F.; González-Jiménez, E.; Ramírez-Vélez, R. Supervised Exercise Reduces Cancer-Related Fatigue: A Systematic Review. J. Physiother. 2015, 61, 3–9. [Google Scholar] [CrossRef]
- McMillan, E.M.; Newhouse, I.J. Exercise Is an Effective Treatment Modality for Reducing Cancer-Related Fatigue and Improving Physical Capacity in Cancer Patients and Survivors: A Meta-Analysis. Appl. Physiol. Nutr. Metab. 2011, 36, 892–903. [Google Scholar] [CrossRef] [PubMed]
- Lahart, I.M.; Metsios, G.S.; Nevill, A.M.; Carmichael, A.R. Physical Activity for Women with Breast Cancer after Adjuvant Therapy. Cochrane Database Syst. Rev. 2018, 2018, CD011292. [Google Scholar] [CrossRef] [PubMed]
- Sweegers, M.G.; Altenburg, T.M.; Chinapaw, M.J.; Kalter, J.; Verdonck-de Leeuw, I.M.; Courneya, K.S.; Newton, R.U.; Aaronson, N.K.; Jacobsen, P.B.; Brug, J.; et al. Which Exercise Prescriptions Improve Quality of Life and Physical Function in Patients with Cancer during and Following Treatment? A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Br. J. Sports Med. 2018, 52, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Buffart, L.M.; Kalter, J.; Sweegers, M.G.; Courneya, K.S.; Newton, R.U.; Aaronson, N.K.; Jacobsen, P.B.; May, A.M.; Galvão, D.A.; Chinapaw, M.J.; et al. Effects and Moderators of Exercise on Quality of Life and Physical Function in Patients with Cancer: An Individual Patient Data Meta-Analysis of 34 RCTs. Cancer Treat. Rev. 2017, 52, 91–104. [Google Scholar] [CrossRef]
- Swartz, M.C.; Lewis, Z.H.; Lyons, E.J.; Jennings, K.; Middleton, A.; Deer, R.R.; Arnold, D.; Dresser, K.; Ottenbacher, K.J.; Goodwin, J.S. Effect of Home- and Community-Based Physical Activity Interventions on Physical Function Among Cancer Survivors: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2017, 98, 1652–1665. [Google Scholar] [CrossRef]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef]
- Grande, A.J.; Silva, V.; Sawaris Neto, L.; Teixeira Basmage, J.P.; Peccin, M.S.; Maddocks, M. Exercise for Cancer Cachexia in Adults. Cochrane Database Syst. Rev. 2021, 2021, CD010804. [Google Scholar] [CrossRef]
- Loughney, L.A.; West, M.A.; Kemp, G.J.; Grocott, M.P.; Jack, S. Exercise Interventions for People Undergoing Multimodal Cancer Treatment That Includes Surgery. Cochrane Database Syst. Rev. 2018, 2018, CD012280. [Google Scholar] [CrossRef]
- Trommer, M.; Marnitz, S.; Skoetz, N.; Rupp, R.; Niels, T.; Morgenthaler, J.; Theurich, S.; von Bergwelt-Baildon, M.; Baues, C.; Baumann, F.T. Exercise Interventions for Adults with Cancer Receiving Radiation Therapy Alone. Cochrane Database Syst. Rev. 2023, 2023, CD013448. [Google Scholar] [CrossRef]
- Peddle-McIntyre, C.J.; Singh, F.; Thomas, R.; Newton, R.U.; Galvão, D.A.; Cavalheri, V. Exercise Training for Advanced Lung Cancer. Cochrane Database Syst. Rev. 2019, CD012685. [Google Scholar] [CrossRef] [PubMed]
- Cheville, A.L.; Kollasch, J.; Vandenberg, J.; Shen, T.; Grothey, A.; Gamble, G.; Basford, J.R. A Home-Based Exercise Program to Improve Function, Fatigue, and Sleep Quality in Patients with Stage IV Lung and Colorectal Cancer: A Randomized Controlled Trial. J. Pain Symptom Manag. 2013, 45, 811–821. [Google Scholar] [CrossRef]
- Oldervoll, L.M.; Loge, J.H.; Lydersen, S.; Paltiel, H.; Asp, M.B.; Nygaard, U.V.; Oredalen, E.; Frantzen, T.L.; Lesteberg, I.; Amundsen, L.; et al. Physical Exercise for Cancer Patients with Advanced Disease: A Randomized Controlled Trial. Oncologist 2011, 16, 1649–1657. [Google Scholar] [CrossRef] [PubMed]
- Tsianakas, V.; Harris, J.; Ream, E.; Van Hemelrijck, M.; Purushotham, A.; Mucci, L.; Green, J.S.A.; Fewster, J.; Armes, J. CanWalk: A Feasibility Study with Embedded Randomised Controlled Trial Pilot of a Walking Intervention for People with Recurrent or Metastatic Cancer. BMJ Open 2017, 7, e013719. [Google Scholar] [CrossRef] [PubMed]
- Quist, M.; Adamsen, L.; Rørth, M.; Laursen, J.H.; Christensen, K.B.; Langer, S.W. The Impact of a Multidimensional Exercise Intervention on Physical and Functional Capacity, Anxiety, and Depression in Patients With Advanced-Stage Lung Cancer Undergoing Chemotherapy. Integr. Cancer Ther. 2015, 14, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Kuehr, L.; Wiskemann, J.; Abel, U.; Ulrich, C.M.; Hummler, S.; Thomas, M. Exercise in Patients with Non–Small Cell Lung Cancer. Med. Sci. Sports Exerc. 2014, 46, 656–663. [Google Scholar] [CrossRef] [PubMed]
- Quist, M.; Rørth, M.; Langer, S.; Jones, L.W.; Laursen, J.H.; Pappot, H.; Christensen, K.B.; Adamsen, L. Safety and Feasibility of a Combined Exercise Intervention for Inoperable Lung Cancer Patients Undergoing Chemotherapy: A Pilot Study. Lung Cancer 2012, 75, 203–208. [Google Scholar] [CrossRef]
- Headley, J.A.; Ownby, K.K.; John, L.D. The Effect of Seated Exercise on Fatigue and Quality of Life in Women with Advanced Breast Cancer. Oncol. Nurs. Forum 2004, 31, 977–983. [Google Scholar] [CrossRef]
- Oldervoll, L.M.; Loge, J.H.; Paltiel, H.; Asp, M.B.; Vidvei, U.; Wiken, A.N.; Hjermstad, M.J.; Kaasa, S. The Effect of a Physical Exercise Program in Palliative Care: A Phase II Study. J. Pain Symptom Manag. 2006, 31, 421–430. [Google Scholar] [CrossRef]
- Hansen, P.A.; Dechet, C.B.; Porucznik, C.A.; LaStayo, P.C. Comparing Eccentric Resistance Exercise in Prostate Cancer Survivors On and Off Hormone Therapy: A Pilot Study. PMR 2009, 1, 1019–1024. [Google Scholar] [CrossRef]
- Cheville, A.L.; Girardi, J.; Clark, M.M.; Rummans, T.A.; Pittelkow, T.; Brown, P.; Hanson, J.; Atherton, P.; Johnson, M.E.; Sloan, J.A.; et al. Therapeutic Exercise during Outpatient Radiation Therapy for Advanced Cancer. Am. J. Phys. Med. Rehabil. 2010, 89, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Henke, C.C.; Cabri, J.; Fricke, L.; Pankow, W.; Kandilakis, G.; Feyer, P.C.; de Wit, M. Strength and Endurance Training in the Treatment of Lung Cancer Patients in Stages IIIA/IIIB/IV. Support. Care Cancer 2014, 22, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Dittus, K.L.; Gramling, R.E.; Ades, P.A. Exercise Interventions for Individuals with Advanced Cancer: A Systematic Review. Prev. Med. 2017, 104, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Navigante, A.; Morgado, P.C. Does Physical Exercise Improve Quality of Life of Advanced Cancer Patients? Curr. Opin. Support. Palliat. Care 2016, 10, 306–309. [Google Scholar] [CrossRef] [PubMed]
- Progression Models in Resistance Training for Healthy Adults. Med. Sci. Sports Exerc. 2009, 41, 687–708. [CrossRef]
- Patel, H.; Alkhawam, H.; Madanieh, R.; Shah, N.; Kosmas, C.E.; Vittorio, T.J. Aerobic vs Anaerobic Exercise Training Effects on the Cardiovascular System. World J. Cardiol. 2017, 9, 134. [Google Scholar] [CrossRef]
- De Lazzari, N.; Niels, T.; Tewes, M.; Götte, M. A Systematic Review of the Safety, Feasibility and Benefits of Exercise for Patients with Advanced Cancer. Cancers 2021, 13, 4478. [Google Scholar] [CrossRef]
- Han, J.; Meng, Q.; Shen, L.; Wu, G. Interleukin-6 Induces Fat Loss in Cancer Cachexia by Promoting White Adipose Tissue Lipolysis and Browning. Lipids Health Dis. 2018, 17, 14. [Google Scholar] [CrossRef]
- He, W.A.; Berardi, E.; Cardillo, V.M.; Acharyya, S.; Aulino, P.; Thomas-Ahner, J.; Wang, J.; Bloomston, M.; Muscarella, P.; Nau, P.; et al. NF-κB–mediated Pax7 Dysregulation in the Muscle Microenvironment Promotes Cancer Cachexia. J. Clin. Investig. 2013, 123, 4821–4835. [Google Scholar] [CrossRef]
- Pryce, B.R.; Guttridge, D.C. NF-KB Signaling in the Macroenvironment of Cancer Cachexia. In The Systemic Effects of Advanced Cancer; Springer International Publishing: Cham, Switzerland, 2022; pp. 119–135. [Google Scholar]
- Vella, L.; Caldow, M.K.; Larsen, A.E.; Tassoni, D.; Della Gatta, P.A.; Gran, P.; Russell, A.P.; Cameron-Smith, D. Resistance Exercise Increases NF-ΚB Activity in Human Skeletal Muscle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2012, 302, R667–R673. [Google Scholar] [CrossRef]
- Tsitkanou, S.; Murach, K.A.; Washington, T.A.; Greene, N.P. Exercise Counteracts the Deleterious Effects of Cancer Cachexia. Cancers 2022, 14, 2512. [Google Scholar] [CrossRef] [PubMed]
- Petersen, A.M.W.; Pedersen, B.K. The Anti-Inflammatory Effect of Exercise. J. Appl. Physiol. 2005, 98, 1154–1162. [Google Scholar] [CrossRef] [PubMed]
- Rébé, C.; Ghiringhelli, F. Interleukin-1β and Cancer. Cancers 2020, 12, 1791. [Google Scholar] [CrossRef] [PubMed]
- Ben-Baruch, A. Tumor Necrosis Factor α: Taking a Personalized Road in Cancer Therapy. Front. Immunol. 2022, 13, 903679. [Google Scholar] [CrossRef]
- Cannataro, R.; Cione, E.; Bonilla, D.A.; Cerullo, G.; Angelini, F.; D’Antona, G. Strength Training in Elderly: An Useful Tool against Sarcopenia. Front. Sports Act. Living 2022, 4, 950949. [Google Scholar] [CrossRef]
| Cancer Type | Length of Time | Intervention Type (Exercise or Rehabilitation?) | Routine | Improved Outcome Measures | References |
|---|---|---|---|---|---|
| Stage IV lung (n = 34) and colorectal (n = 32) cancer | 8 weeks | Exercise | 4×/week incremental 20 min brisk walks REX: 5 exercises, 10–15 reps | Mobility, fatigue, and sleep | Cheville et al., 2013 [173] |
| Mixed incurable metastatic cancers with life expectancy < 2 years (n = 121) | 8 weeks | Exercise | 2×/week 50–60 min AEX: 10–15 min REX circuit: 6 stations, 2 min on, 1 min off | Shuttle walk test (SWT) and HGS | Oldervoll et al., 2011 [174] |
| Mixed recurrent advanced or metastatic cancer (n = 46) | 12 weeks | Exercise | 30 min walking on alternate days | None | Tsianakas et al., 2017 [175] |
| Stage IIIb or IV NSCLC or extensive small cell lung cancer (n = 114) | 6 weeks | Exercise | 2×/week supervised REX and AEX 3×/week home walking | Peak VO2, 6MWT, and 1 RM | Quist et al., 2015 [176] |
| Advanced NSCLC (n = 40) | 8 weeks | Exercise | 3 days/week supervised, 2 day/week independent REX and AEX | 6MWT and dynamometer muscle strength | Kuehr et al., 2014 [177] |
| Stage IIIb or IV NSCLC or extensive small cell lung cancer (n = 23) | 6 weeks | Exercise | 2×/week supervised AEX and REX 3×/week home walking | Peak VO2, 1 RM, and emotional QoL | Quist et al., 2012 [178] |
| Stage IV breast cancer (n = 38, 16 intervention) | 12 weeks | Exercise | 3×/week video-guided seated REX and stretching | Slower decline in total and physical well-being Less increase in fatigue | Headley et al., 2004 [179] |
| Mixed advanced cancers (n = 34) | 6 weeks | Exercise | 2×/week supervised REX circuit training | 6MWT, timed sit-to-stand, physical fatigue, and emotional QoL | Oldervoll et al., 2006 [180] |
| Prostate cancer (n = 16) | 12 weeks | Exercise | 3×/week 12–15 min eccentric resistance cycling | 6MWT and isometric knee extension strength | Hansen et al., 2009 [181] |
| Mixed advanced cancers (n = 115) | 8 sessions | Rehabilitation | 3×/week 90 min PT for trunk and lower extremity | Physical well-being | Cheville et al., 2010 [182] |
| Stages III and IV lung cancer (n = 46) | Duration of 3 chemotherapy cycles | Rehabilitation | 3–4×/week REX: 50% capacity 10 reps, 3 sets with resistance bands 5×/week AEX: 6 min walk moderate intensity 2 min staircase walking | Cognitive function, physical function, staircase walking, and 6MWT | Henke et al., 2014 [183] |
| Inpatient advanced cancer patients (n = 250) | Length of hospital stay | Rehabilitation | Minimum of 900 min of therapy/week, including PT, OT, and SLT | Motor and cognitive FIM scores | Roy et al., 2023 [29] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Willbanks, A.; Seals, M.; Karmali, R.; Roy, I. Harnessing the Systemic Biology of Functional Decline and Cachexia to Inform more Holistic Therapies for Incurable Cancers. Cancers 2024, 16, 360. https://doi.org/10.3390/cancers16020360
Willbanks A, Seals M, Karmali R, Roy I. Harnessing the Systemic Biology of Functional Decline and Cachexia to Inform more Holistic Therapies for Incurable Cancers. Cancers. 2024; 16(2):360. https://doi.org/10.3390/cancers16020360
Chicago/Turabian StyleWillbanks, Amber, Mina Seals, Reem Karmali, and Ishan Roy. 2024. "Harnessing the Systemic Biology of Functional Decline and Cachexia to Inform more Holistic Therapies for Incurable Cancers" Cancers 16, no. 2: 360. https://doi.org/10.3390/cancers16020360
APA StyleWillbanks, A., Seals, M., Karmali, R., & Roy, I. (2024). Harnessing the Systemic Biology of Functional Decline and Cachexia to Inform more Holistic Therapies for Incurable Cancers. Cancers, 16(2), 360. https://doi.org/10.3390/cancers16020360





