Intensive Interdisciplinary Rehabilitation in the Pediatric Hematology/Oncology Setting: Feasibility and Perceived Benefit of the Acute Neurological Injury Service
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. ANI Service
2.2.1. ANI Service Development
2.2.2. Interdisciplinary Communication
2.2.3. Shared Goal Setting
2.2.4. Coordinated Transition Planning
2.3. Caregiver Interview
3. Results
3.1. ANI Service Participants
3.2. Caregiver Interview Participants
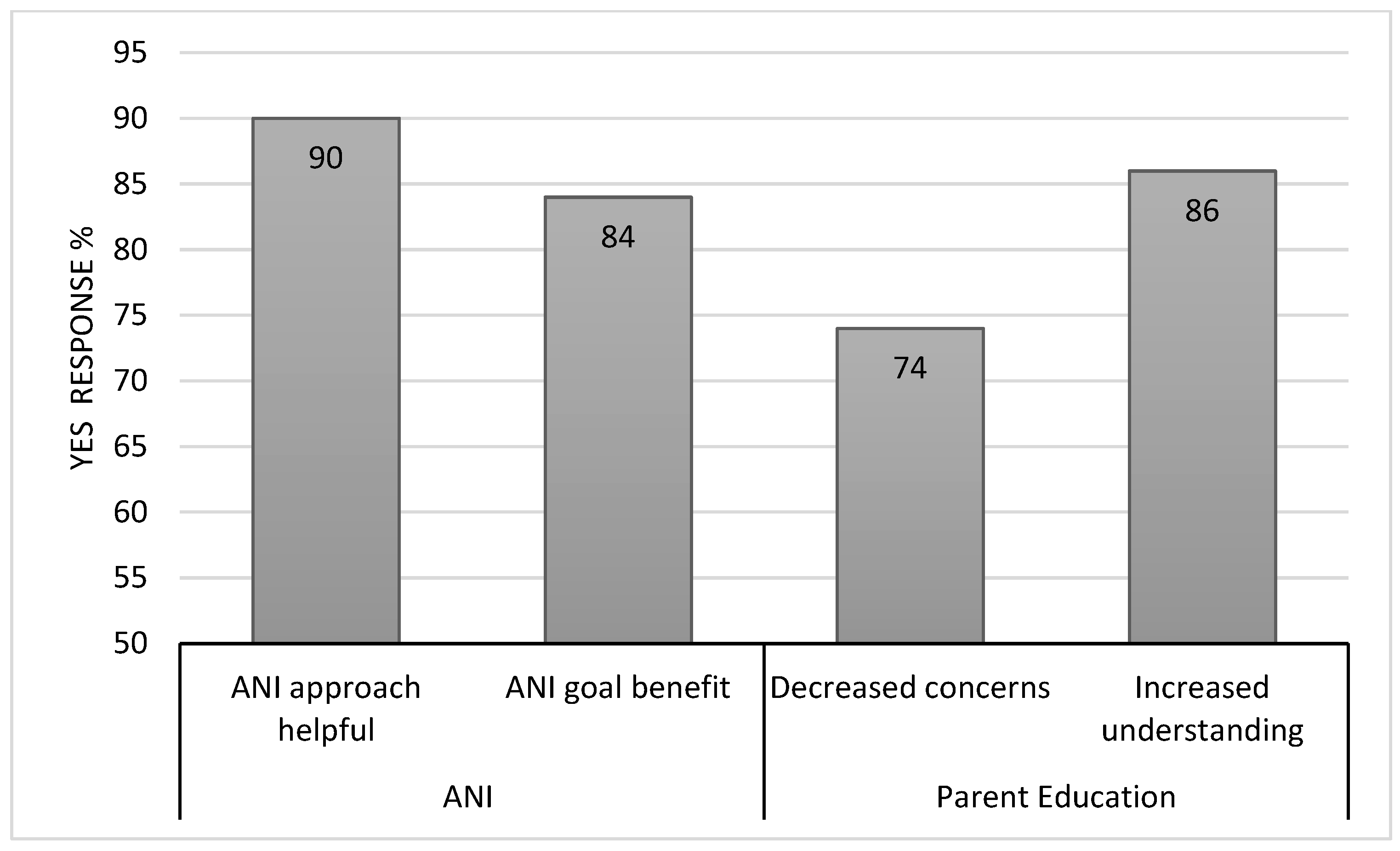
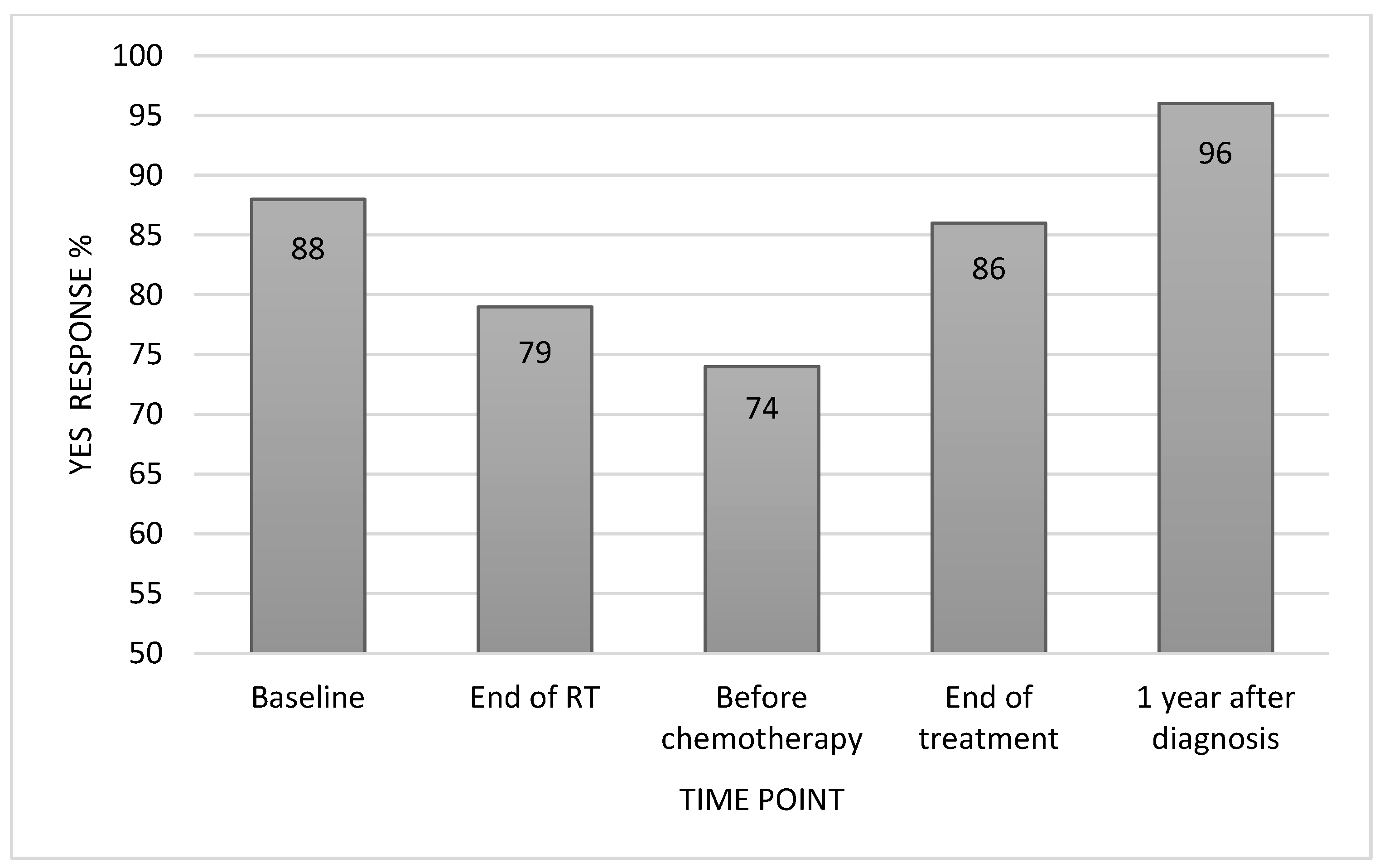
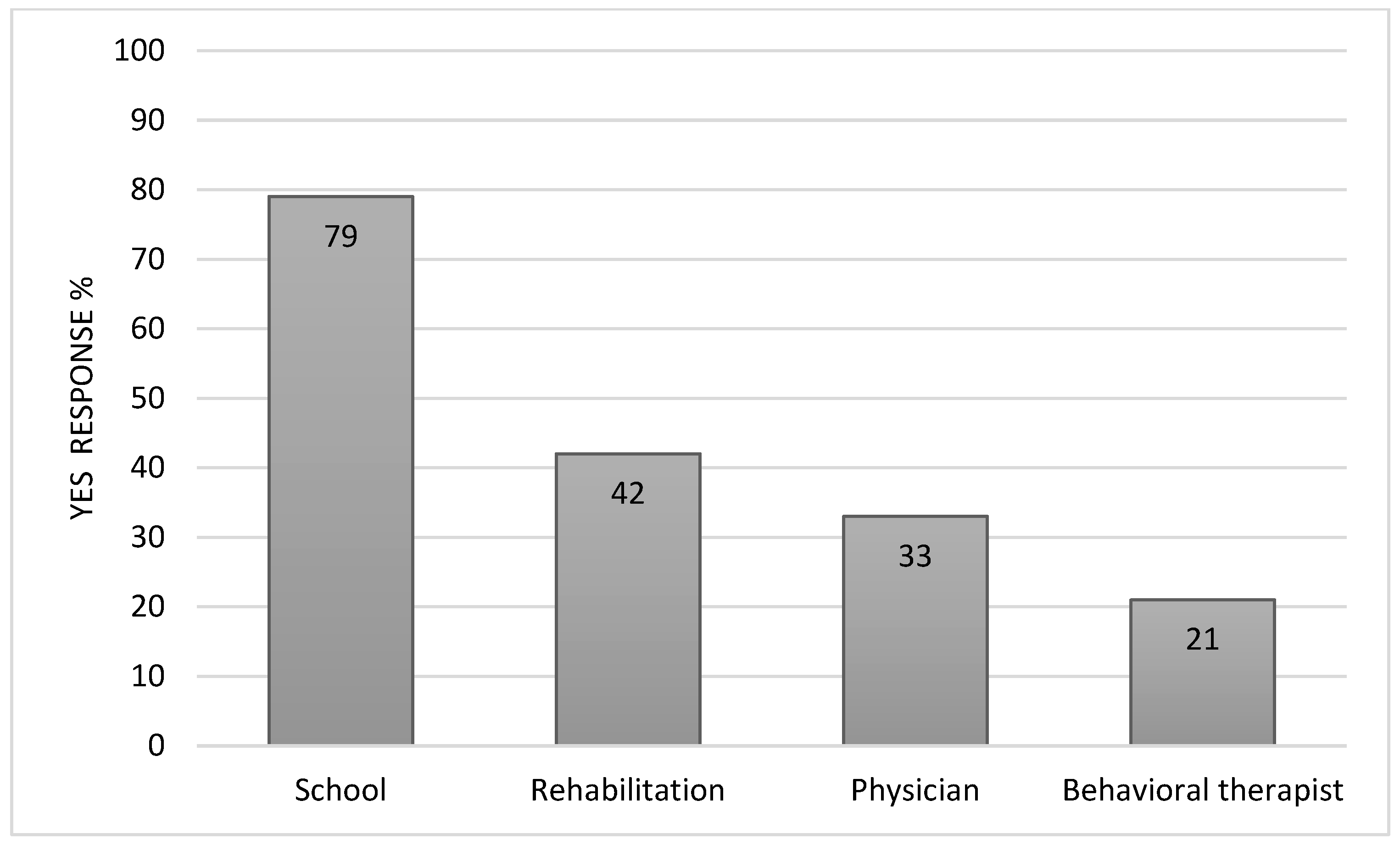
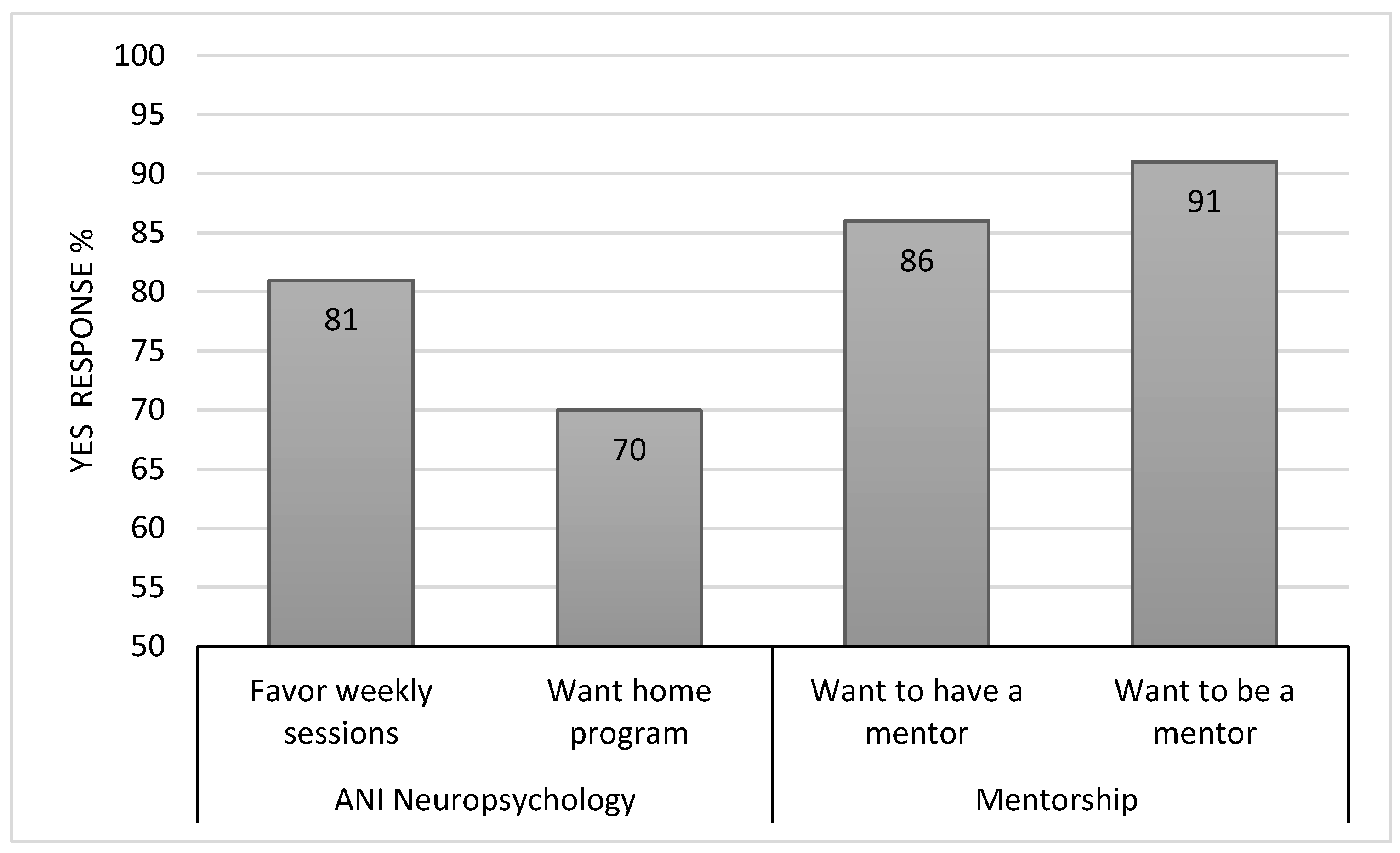
3.3. Caregiver-Perceived ANI Feasibility and Benefit
4. Discussion
Limitations and Future Directions:
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singh, R.; Kucukdeveci, A.A.; Grabljevec, K.; Gray, A. The role of Interdisciplinary Teams in Physical and Rehabilitation Medicine. J. Rehabil. Med. 2018, 50, 673–678. [Google Scholar] [CrossRef]
- High, W.M., Jr. Effectiveness of TBI Rehabilitation Programs. In Rehabilitation for Traumatic Brain Injury; High, W.M., Jr., Sander, A.M., Struchen, M.A., Hart, K.A., Eds.; Oxford University Press: New York, NY, USA, 2004; pp. 14–28. [Google Scholar]
- Bokhour, B.G. Communication in interdisciplinary team meetings: What are we talking about? J. Interprof. Care 2006, 20, 349–363. [Google Scholar] [CrossRef]
- Semlyen, J.K.; Summers, S.J.; Barnes, M.P. Traumatic brain injury: Efficacy of multidisciplinary rehabilitation. Arch. Phys. Med. Rehabil. 1998, 79, 678–683. [Google Scholar] [CrossRef]
- Korner, M. Interprofessional teamwork in medical rehabilitation: A comparison of multidisciplinary and interdisciplinary team approach. Clin. Rehabil. 2010, 24, 745–755. [Google Scholar] [CrossRef]
- Prigatano, G.P.; Klonoff, P.S.; O’Brien, K.P.; Altman, I.M.; Amin, K.; Chiapello, D.; Shepherd, J.; Cunningham, M.; Mora, M. Productivity after neuropsychologically oriented milieu rehabilitation. J. Head Trauma Rehabil. 1994, 9, 91–102. [Google Scholar] [CrossRef]
- Harman, J.L.; Molnar Jr, A.E.; Jacola, L.M.; Corr, A.; Scott, A.; Potter, B.; Schwartzberg, S.; Boyer, H.; Greear, J.; Willard, V.W. Establishing a hospital-based early intervention program for young children with cancer: A quality improvement initiative. Clin. Pract. Pediatr. Psychol. 2021, 9, 323. [Google Scholar] [CrossRef]
- Corr, A.; Thomas, K. Screening for Early Childhood Intervention in Oncology. Rehabil. Oncol. 2018, 37, 83–85. [Google Scholar] [CrossRef]
- L’Hotta, A.J.; Beam, I.A.; Thomas, K.M. Development of a comprehensive pediatric oncology rehabilitation program. Pediatr. Blood Cancer 2020, 67, e28083. [Google Scholar] [CrossRef]
- Miale, S.; Stimler, L.; Riedel, E.R. Using a simple screening tool to enhance awareness and utilization of rehabilitation services for pediatric oncology patients in the acute care setting. Rehabil. Oncol. 2013, 31, 6–10. [Google Scholar] [CrossRef]
- Tanner, L.R.; Sencer, S.; Gossai, N.; Watson, D.; Hooke, M.C. CREATE Childhood Cancer Rehabilitation Program development: Increase access through interprofessional collaboration. Pediatr. Blood Cancer 2022, 69, e29912. [Google Scholar] [CrossRef]
- Cordelli, D.M.; Masetti, R.; Zama, D.; Toni, F.; Castelli, I.; Ricci, E.; Franzoni, E.; Pession, A. Central Nervous System Complications in Children Receiving Chemotherapy or Hematopoietic Stem Cell Transplantation. Front. Pediatr. 2017, 5, 105. [Google Scholar] [CrossRef]
- Pizzo, P.A.; Robichaud, K.J.; Wesley, R.; Commers, J.R. Fever in the pediatric and young adult patient with cancer. A prospective study of 1001 episodes. Medicine 1982, 61, 153–165. [Google Scholar] [CrossRef]
- Noje, C.; Cohen, K.; Jordan, L.C. Hemorrhagic and ischemic stroke in children with cancer. Pediatr. Neurol. 2013, 49, 237–242. [Google Scholar] [CrossRef]
- Vagace, J.M.; de la Maya, M.D.; Caceres-Marzal, C.; Gonzalez de Murillo, S.; Gervasini, G. Central nervous system chemotoxicity during treatment of pediatric acute lymphoblastic leukemia/lymphoma. Crit. Rev. Oncol. Hematol. 2012, 84, 274–286. [Google Scholar] [CrossRef]
- De Smet, H.J.; Baillieux, H.; Catsman-Berrevoets, C.; De Deyn, P.P.; Marien, P.; Paquier, P.F. Postoperative motor speech production in children with the syndrome of ‘cerebellar’ mutism and subsequent dysarthria: A critical review of the literature. Eur. J. Paediatr. Neurol. 2007, 11, 193–207. [Google Scholar] [CrossRef]
- Korah, M.P.; Esiashvili, N.; Mazewski, C.M.; Hudgins, R.J.; Tighiouart, M.; Janss, A.J.; Schwaibold, F.P.; Crocker, I.R.; Curran, W.J., Jr.; Marcus, R.B., Jr. Incidence, risks, and sequelae of posterior fossa syndrome in pediatric medulloblastoma. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 106–112. [Google Scholar] [CrossRef]
- van Dun, K.; Overwalle, F.V.; Manto, M.; Marien, P. Cognitive Impact of Cerebellar Damage: Is There a Future for Cognitive Rehabilitation? CNS Neurol. Disord. Drug Targets 2018, 17, 199–206. [Google Scholar] [CrossRef]
- Palmer, S.L.; Hassall, T.; Evankovich, K.; Mabbott, D.J.; Bonner, M.; Deluca, C.; Cohn, R.; Fisher, M.J.; Morris, E.B.; Broniscer, A.; et al. Neurocognitive outcome 12 months following cerebellar mutism syndrome in pediatric patients with medulloblastoma. Neuro-oncology 2010, 12, 1311–1317. [Google Scholar] [CrossRef]
- Robertson, P.L.; Muraszko, K.M.; Holmes, E.J.; Sposto, R.; Packer, R.J.; Gajjar, A.; Dias, M.S.; Allen, J.C.; Children’s Oncology, G. Incidence and severity of postoperative cerebellar mutism syndrome in children with medulloblastoma: A prospective study by the Children’s Oncology Group. J. Neurosurg. 2006, 105, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, J.E.; Gurney, J.G.; Palmer, S.L.; Bass, J.K.; Wang, M.; Chen, S.; Zhang, H.; Swain, M.; Chapieski, M.L.; Bonner, M.J.; et al. Examination of risk factors for intellectual and academic outcomes following treatment for pediatric medulloblastoma. Neuro-oncology 2014, 16, 1129–1136. [Google Scholar] [CrossRef]
- Schreiber, J.E.; Palmer, S.L.; Conklin, H.M.; Mabbott, D.J.; Swain, M.A.; Bonner, M.J.; Chapieski, M.L.; Huang, L.; Zhang, H.; Gajjar, A. Posterior fossa syndrome and long-term neuropsychological outcomes among children treated for medulloblastoma on a multi-institutional, prospective study. Neuro-oncology 2017, 19, 1673–1682. [Google Scholar] [CrossRef]
- Khan, R.B.; Patay, Z.; Klimo, P.; Huang, J.; Kumar, R.; Boop, F.A.; Raches, D.; Conklin, H.M.; Sharma, R.; Simmons, A.; et al. Clinical features, neurologic recovery, and risk factors of postoperative posterior fossa syndrome and delayed recovery: A prospective study. Neuro-oncology 2021, 23, 1586–1596. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.; Wong, B. Central nervous system infections in immunocompromised hosts. Annu. Rev. Med. 1982, 33, 293–308. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Sheng, D. Analysis of the Factors Related to Intracranial Infection after Brain Tumor Surgery. Contrast Media Mol. Imaging 2022, 2022, 6988560. [Google Scholar] [CrossRef]
- Kralik, S.F.; Ho, C.Y.; Finke, W.; Buchsbaum, J.C.; Haskins, C.P.; Shih, C.S. Radiation Necrosis in Pediatric Patients with Brain Tumors Treated with Proton Radiotherapy. AJNR Am. J. Neuroradiol. 2015, 36, 1572–1578. [Google Scholar] [CrossRef]
- Plimpton, S.R.; Stence, N.; Hemenway, M.; Hankinson, T.C.; Foreman, N.; Liu, A.K. Cerebral radiation necrosis in pediatric patients. Pediatr. Hematol. Oncol. 2015, 32, 78–83. [Google Scholar] [CrossRef]
- King, V.K.A. The realities of a rehabilitation journey following posterior fossa syndrome. In Proceedings of the Posterior Fossa Society First Global Meeting, Liverpool, UK, 9–11 September 2022. [Google Scholar]
- McNeil, M.J.; Kiefer, A.; Woods, C.; Barnett, B.; Berry-Carter, K.; Clark, L.; Mandrell, B.N.; Snaman, J.; Kaye, E.C.; Baker, J.N. “You are not alone”: Connecting through a bereaved parent mentor program for parents whose child died of cancer. Cancer Med. 2022, 11, 3332–3341. [Google Scholar] [CrossRef] [PubMed]
- Rennke, S.; Ranji, S.R. Transitional care strategies from hospital to home: A review for the neurohospitalist. Neurohospitalist 2015, 5, 35–42. [Google Scholar] [CrossRef]
- Raches, D.; Conklin, H.M. Investigating severity of symptoms associated with Posterior Fossa Syndrome as predictors of long-term cognitive and functional outcomes: A case series. Brain Disord. 2023, 11, 100080. [Google Scholar] [CrossRef]
| Sex | |||
|---|---|---|---|
| Male (%) | 56 | ||
| Female | 44 | ||
| Age at diagnosis (years) | |||
| Mean (SD) | 8.84 (4.86) | ||
| Range | 2–21 | ||
| Distance from hospital (miles) | |||
| Mean (SD) | 577 (417) | ||
| Range | 11–2017 | ||
| Cancer diagnosis (%) | |||
| Brain tumor | 95 | ||
| Medulloblastoma | 74 | ||
| Ependymoma | 6 | ||
| Atypical teratoid rhabdoid tumor | 4 | ||
| Diffuse intrinsic pontine glioma | 2 | ||
| Other * | 9 | ||
| Leukemia | 2 | ||
| Lymphoma | 1 | ||
| Hemophagocytic lymphohistiocytosis | 1 | ||
| Neuroblastoma | 1 | ||
| ANI referral reason (%) | |||
| Posterior fossa/cerebellar mutism syndrome | 81 | ||
| Mental status change | 10 | ||
| Stroke | 4 | ||
| Other ** | 5 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raches, D.; Gajjar, A.; Robinson, G.W.; Ashford, J.M.; Bryndziar, M.; Huggins, A.; Lockett, S.; Harris, A.; Taylor, H.; Bursi, E.; et al. Intensive Interdisciplinary Rehabilitation in the Pediatric Hematology/Oncology Setting: Feasibility and Perceived Benefit of the Acute Neurological Injury Service. Cancers 2024, 16, 2999. https://doi.org/10.3390/cancers16172999
Raches D, Gajjar A, Robinson GW, Ashford JM, Bryndziar M, Huggins A, Lockett S, Harris A, Taylor H, Bursi E, et al. Intensive Interdisciplinary Rehabilitation in the Pediatric Hematology/Oncology Setting: Feasibility and Perceived Benefit of the Acute Neurological Injury Service. Cancers. 2024; 16(17):2999. https://doi.org/10.3390/cancers16172999
Chicago/Turabian StyleRaches, Darcy, Amar Gajjar, Giles W. Robinson, Jason M. Ashford, Martina Bryndziar, April Huggins, Sherry Lockett, Allison Harris, Hannah Taylor, Ellen Bursi, and et al. 2024. "Intensive Interdisciplinary Rehabilitation in the Pediatric Hematology/Oncology Setting: Feasibility and Perceived Benefit of the Acute Neurological Injury Service" Cancers 16, no. 17: 2999. https://doi.org/10.3390/cancers16172999
APA StyleRaches, D., Gajjar, A., Robinson, G. W., Ashford, J. M., Bryndziar, M., Huggins, A., Lockett, S., Harris, A., Taylor, H., Bursi, E., & Conklin, H. M. (2024). Intensive Interdisciplinary Rehabilitation in the Pediatric Hematology/Oncology Setting: Feasibility and Perceived Benefit of the Acute Neurological Injury Service. Cancers, 16(17), 2999. https://doi.org/10.3390/cancers16172999






