The PedAL/EuPAL Project: A Global Initiative to Address the Unmet Medical Needs of Pediatric Patients with Relapsed or Refractory Acute Myeloid Leukemia
Abstract
:Simple Summary
Abstract
1. Introduction and Background
The Need to Establish a Standard of Care for Relapsed Patients
2. The PedAL/EuPAL Project
2.1. Screening Trial and Registry
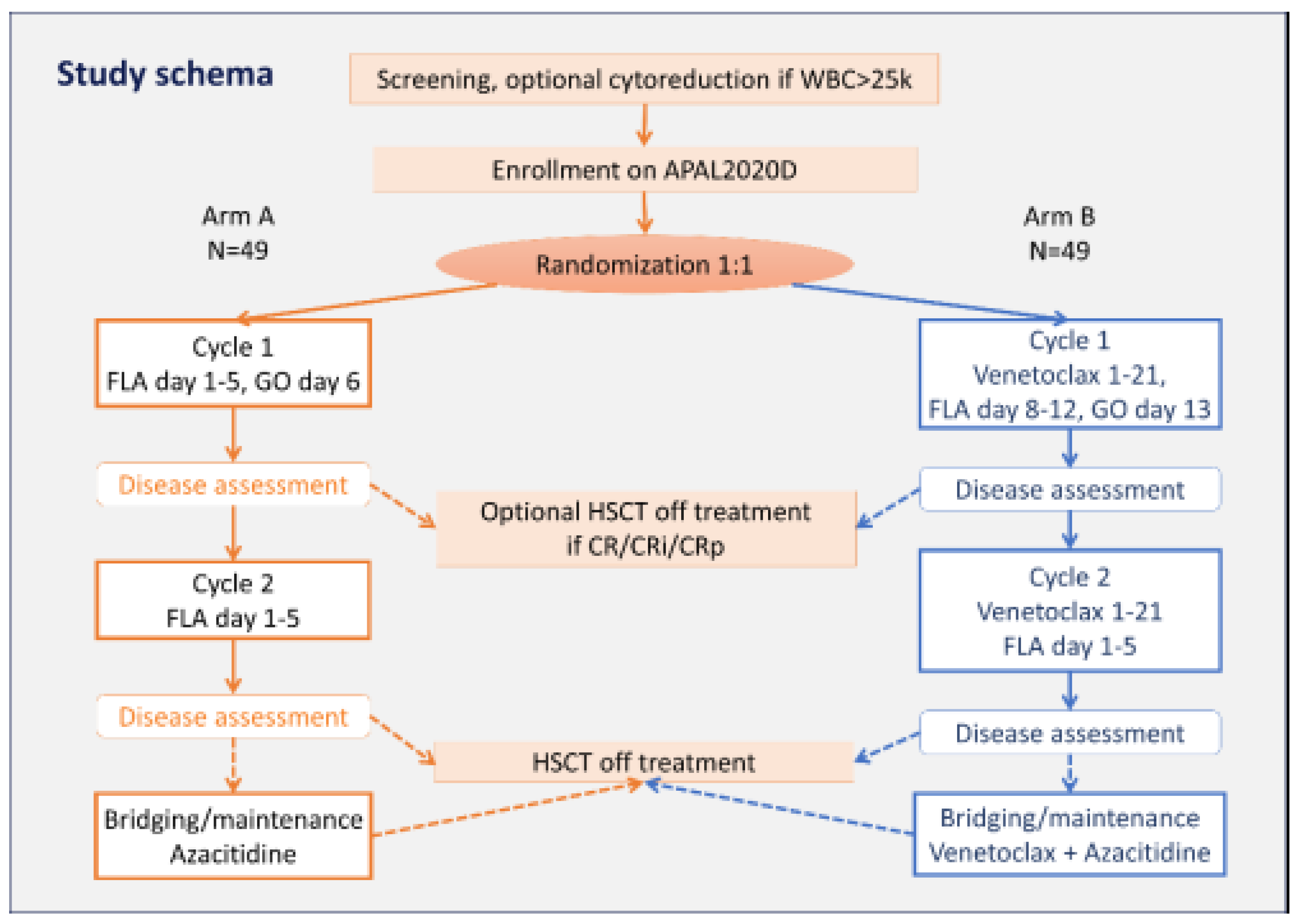
2.2. The First Sub-Trial Opened: APAL2020D
3. Potential Treatment Targets in Pediatric Acute Myeloid Leukemia
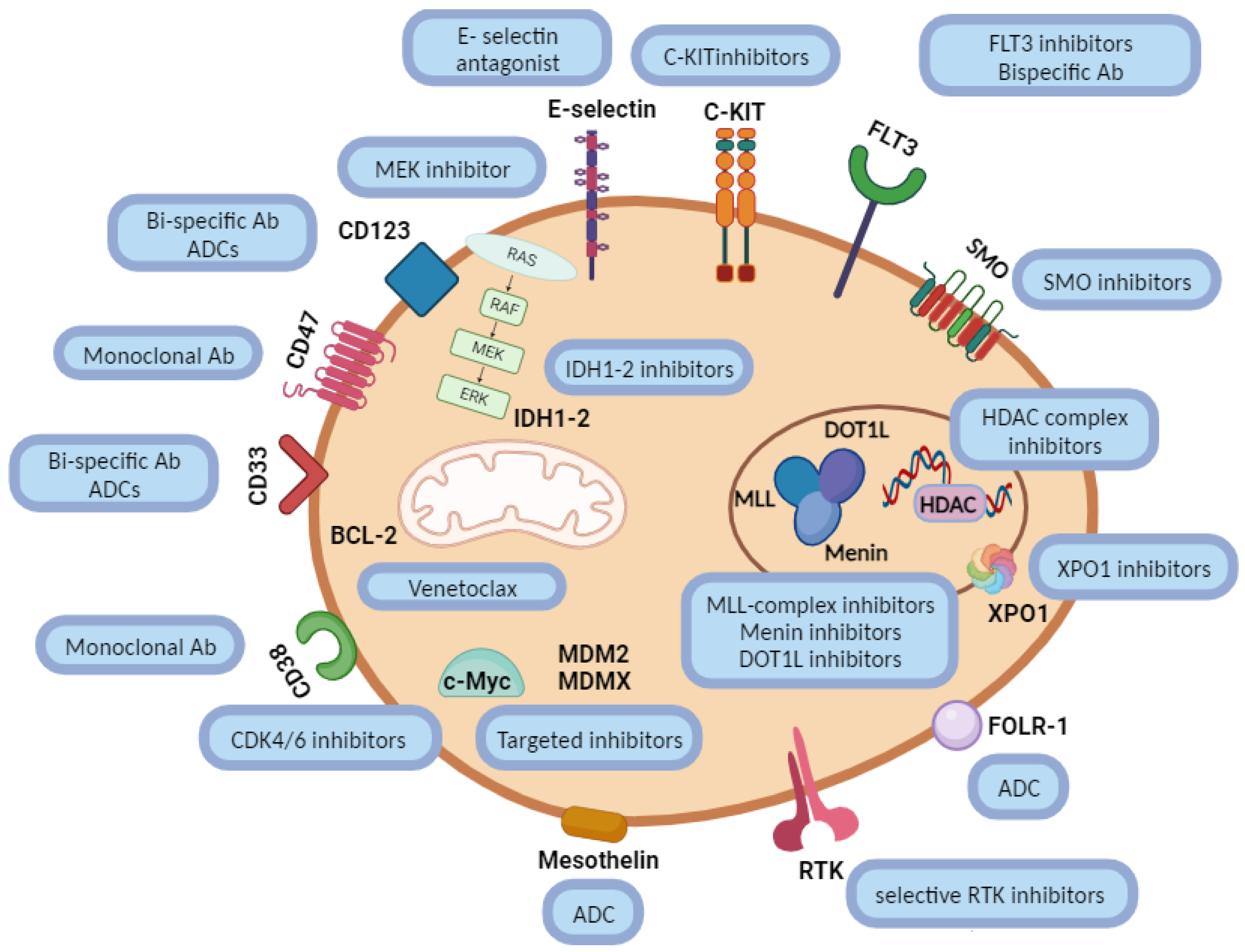
3.1. Novel Drugs in Pediatric AML
3.1.1. Gemtuzumab Ozogamicin
3.1.2. FLT3 Inhibitors
- -
- Midostaurin in combination with chemotherapy is being studied in newly diagnosed children in an ongoing company-sponsored study (NCT03591510);
- -
- Gilteritinib is currently investigated in children with both newly diagnosed and R/R FLT3-ITD and/or TKD mutated AML (NCT04293562; NCT04240002);
- -
- Quizartinib for newly diagnosed FLT3-ITD/NPM1-wild type AML will soon be open to enrolment (EudraCT: 2022-002886-14), based on data from the ongoing relapse study (NCT03793478).
3.2. Current High-Priority Pediatric AML Targets
3.2.1. BCL-2 Inhibitors
3.2.2. Menin Inhibitors
- -
- Revumenib (SNDX-5613) is being studied as a monotherapy in the company-sponsored AUGMENT-101 trial, a phase I/II trial that includes both adults and children with R/R KMT2A-rerarranged or NPM1-mutant acute leukemias (NCT04065399). Therapy with revumenib has been associated with a low frequency of Grade 3 or higher treatment-related adverse events and a 30% (18 of 60 evaluable patients) rate of complete remission (CR) or complete remission with incomplete hematologic recovery (CRi) [49]. Specific safety issues consist of QTc prolongation and an interaction with the cytochrome P450 3A4 inhibitor (CYP3A4), resulting in an RP2D with (Arm B) and without (Arm A) a strong CYP3A4 of 226 mg q12h and 276 mg q12h in Arm A and 113 mg q12h and 163 mg q12h in Arm B;
- -
- The AUGMENT-102 is a phase I, dose-escalation study also designed to evaluate the safety, tolerability, and preliminary anti-leukemic activity of revumenib (SNDX-5613) in combination with chemotherapy in patients with R/R leukemias harboring alterations in KMT2A/MLL, NPM1, and NUP98 genes (NCT05326516);
- -
- Revumenib (SNDX-5613) is also being investigated in a phase I/II trial with decitabine/cedazuridine (ASTX727) and venetoclax in R/R AML or mixed-phenotype acute leukemia (MPAL) with a myeloid phenotype;
- -
- Ziftomenib will be studied in the second sub-trial that will be soon opened under the ITCC-101 PedAL/EuPAL Master protocol (APAL2020K, EudraCT number: 2023-505262-28-00).
3.3. Other Targets
3.3.1. FOLR1-Targeted Agents
3.3.2. E-Selectin Inhibitors
3.3.3. IDH Inhibitors
3.3.4. XPO1 Inhibitors
3.3.5. CD123 Targeting
4. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rasche, M.; Zimmermann, M.; Borschel, L.; Bourquin, J.P.; Dworzak, M.; Klingebiel, T.; Lehrnbecher, T.; Creutzig, U.; Klusmann, J.H.; Reinhardt, D. Successes and challenges in the treatment of pediatric acute myeloid leukemia: A retrospective analysis of the AML-BFM trials from 1987 to 2012. Leukemia 2018, 32, 2167–2177. [Google Scholar] [CrossRef] [PubMed]
- Reedijk, A.M.J.; Klein, K.; Coebergh, J.W.W.; Kremer, L.C.; Dinmohamed, A.G.; de Haas, V.; Versluijs, A.B.; Ossenkoppele, G.J.; Beverloo, H.B.; Pieters, R.; et al. Improved survival for children and young adolescents with acute myeloid leukemia: A Dutch study on incidence, survival and mortality. Leukemia 2019, 33, 1349–1359. [Google Scholar] [CrossRef] [PubMed]
- De Moerloose, B.; Reedijk, A.; de Bock, G.H.; Lammens, T.; de Haas, V.; Denys, B.; Dedeken, L.; van den Heuvel-Eibrink, M.M.; Te Loo, M.; Uyttebroeck, A.; et al. Response-guided chemotherapy for pediatric acute myeloid leukemia without hematopoietic stem cell transplantation in first complete remission: Results from protocol DB AML-01. Pediatr. Blood Cancer 2019, 66, e27605. [Google Scholar] [CrossRef] [PubMed]
- Creutzig, U.; Zimmermann, M.; Bourquin, J.P.; Dworzak, M.N.; Kremens, B.; Lehrnbecher, T.; von Neuhoff, C.; Sander, A.; von Stackelberg, A.; Schmid, I.; et al. Favorable outcome in infants with AML after intensive first- and second-line treatment: An AML-BFM study group report. Leukemia 2012, 26, 654–661. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, A.E.; Schoonmade, L.J.; Kaspers, G.J. Pediatric relapsed acute myeloid leukemia: A systematic review. Expert Rev. Anticancer Ther. 2021, 21, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Rasche, M.; Zimmermann, M.; Steidel, E.; Alonzo, T.; Aplenc, R.; Bourquin, J.P.; Boztug, H.; Cooper, T.; Gamis, A.S.; Gerbing, R.B.; et al. Survival Following Relapse in Children with Acute Myeloid Leukemia: A Report from AML-BFM and COG. Cancers 2021, 13, 2336. [Google Scholar] [CrossRef] [PubMed]
- Rasche, M.; Zimmermann, M.; Steidel, E.; Alonzo, T.A.; Aplenc, R.; Bourquin, J.-P.; Boztug, H.; Gamis, A.S.; Gerbing, R.B.; Janotová, I.; et al. Failures and Successes in Pediatric Patients with Acute Myeloid Leukemia with First Relapse: A Large International Report on Current Treatment Strategies and Outcome. Blood 2020, 136, 6–7. [Google Scholar] [CrossRef]
- Aladjidi, N.; Auvrignon, A.; Leblanc, T.; Perel, Y.; Bénard, A.; Bordigoni, P.; Gandemer, V.; Thuret, I.; Dalle, J.H.; Piguet, C.; et al. Outcome in children with relapsed acute myeloid leukemia after initial treatment with the French Leucemie Aique Myeloide Enfant (LAME) 89/91 protocol of the French Society of Pediatric Hematology and Immunology. J. Clin. Oncol. 2003, 21, 4377–4385. [Google Scholar] [CrossRef]
- Karlsson, L.; Forestier, E.; Hasle, H.; Jahnukainen, K.; Jónsson, Ó.G.; Lausen, B.; Norén Nyström, U.; Palle, J.; Tierens, A.; Zeller, B.; et al. Outcome after intensive reinduction therapy and allogeneic stem cell transplant in paediatric relapsed acute myeloid leukaemia. Br. J. Haematol. 2017, 178, 592–602. [Google Scholar] [CrossRef]
- Nakayama, H.; Tabuchi, K.; Tawa, A.; Tsukimoto, I.; Tsuchida, M.; Morimoto, A.; Yabe, H.; Horibe, K.; Hanada, R.; Imaizumi, M.; et al. Outcome of children with relapsed acute myeloid leukemia following initial therapy under the AML99 protocol. Int. J. Hematol. 2014, 100, 171–179. [Google Scholar] [CrossRef]
- Niktoreh, N.; Lerius, B.; Zimmermann, M.; Gruhn, B.; Escherich, G.; Bourquin, J.P.; Dworzak, M.; Sramkova, L.; Rossig, C.; Creutzig, U.; et al. Gemtuzumab ozogamicin in children with relapsed or refractory acute myeloid leukemia: A report by Berlin-Frankfurt-Münster study group. Haematologica 2019, 104, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Kaspers, G.J.; Zimmermann, M.; Reinhardt, D.; Gibson, B.E.; Tamminga, R.Y.; Aleinikova, O.; Armendariz, H.; Dworzak, M.; Ha, S.Y.; Hasle, H.; et al. Improved outcome in pediatric relapsed acute myeloid leukemia: Results of a randomized trial on liposomal daunorubicin by the International BFM Study Group. J. Clin. Oncol. 2013, 31, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Zwaan, C.M.; Reinhardt, D.; Zimmerman, M.; Hasle, H.; Stary, J.; Stark, B.; Dworzak, M.; Creutzig, U.; Kaspers, G.J. Salvage treatment for children with refractory first or second relapse of acute myeloid leukaemia with gemtuzumab ozogamicin: Results of a phase II study. Br. J. Haematol. 2010, 148, 768–776. [Google Scholar] [CrossRef] [PubMed]
- White, T.; Kaspers, G.; Abrahamsson, J.; Arad-Cohen, N.; Cianci, D.; Fernandez, J.; Ha, S.Y.; Hasle, H.; De Moerloose, B.; Zwaan, C.M.; et al. Clinical outcomes of second relapsed and refractory first relapsed paediatric AML: A retrospective study within the NOPHO-DB SHIP consortium. Br. J. Haematol. 2022, 197, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Moritake, H.; Tanaka, S.; Miyamura, T.; Nakayama, H.; Shiba, N.; Shimada, A.; Terui, K.; Yuza, Y.; Koh, K.; Goto, H.; et al. The outcomes of relapsed acute myeloid leukemia in children: Results from the Japanese Pediatric Leukemia/Lymphoma Study Group AML-05R study. Pediatr. Blood Cancer 2021, 68, e28736. [Google Scholar] [CrossRef] [PubMed]
- Cooper, T.M.; Alonzo, T.A.; Gerbing, R.B.; Perentesis, J.P.; Whitlock, J.A.; Taub, J.W.; Horton, T.M.; Gamis, A.S.; Meshinchi, S.; Loken, M.R.; et al. AAML0523: A report from the Children’s Oncology Group on the efficacy of clofarabine in combination with cytarabine in pediatric patients with recurrent acute myeloid leukemia. Cancer 2014, 120, 2482–2489. [Google Scholar] [CrossRef] [PubMed]
- Niewerth, D.; Kaspers, G.J.; Jansen, G.; van Meerloo, J.; Zweegman, S.; Jenkins, G.; Whitlock, J.A.; Hunger, S.P.; Lu, X.; Alonzo, T.A.; et al. Proteasome subunit expression analysis and chemosensitivity in relapsed paediatric acute leukaemia patients receiving bortezomib-containing chemotherapy. J. Hematol. Oncol. 2016, 9, 82. [Google Scholar] [CrossRef]
- Horton, T.M.; Perentesis, J.P.; Gamis, A.S.; Alonzo, T.A.; Gerbing, R.B.; Ballard, J.; Adlard, K.; Howard, D.S.; Smith, F.O.; Jenkins, G.; et al. A Phase 2 study of bortezomib combined with either idarubicin/cytarabine or cytarabine/etoposide in children with relapsed, refractory or secondary acute myeloid leukemia: A report from the Children’s Oncology Group. Pediatr. Blood Cancer 2014, 61, 1754–1760. [Google Scholar] [CrossRef]
- Van Eijkelenburg, N.K.A.; Rasche, M.; Ghazaly, E.; Dworzak, M.N.; Klingebiel, T.; Rossig, C.; Leverger, G.; Stary, J.; De Bont, E.; Chitu, D.A.; et al. Clofarabine, high-dose cytarabine and liposomal daunorubicin in pediatric relapsed/refractory acute myeloid leukemia: A phase IB study. Haematologica 2018, 103, 1484–1492. [Google Scholar] [CrossRef]
- Cooper, T.M.; Absalon, M.J.; Alonzo, T.A.; Gerbing, R.B.; Leger, K.J.; Hirsch, B.A.; Pollard, J.; Razzouk, B.I.; Aplenc, R.; Kolb, E.A. Phase I/II Study of CPX-351 Followed by Fludarabine, Cytarabine, and Granulocyte-Colony Stimulating Factor for Children with Relapsed Acute Myeloid Leukemia: A Report from the Children’s Oncology Group. J. Clin. Oncol. 2020, 38, 2170–2177. [Google Scholar] [CrossRef]
- Karol, S.E.; Alexander, T.B.; Budhraja, A.; Pounds, S.B.; Canavera, K.; Wang, L.; Wolf, J.; Klco, J.M.; Mead, P.E.; Das Gupta, S.; et al. Venetoclax in combination with cytarabine with or without idarubicin in children with relapsed or refractory acute myeloid leukaemia: A phase 1, dose-escalation study. Lancet Oncol. 2020, 21, 551–560. [Google Scholar] [CrossRef] [PubMed]
- Rasche, M.; Steidel, E.; Zimmermann, M.; Bourquin, J.P.; Boztug, H.; Janotova, I.; Kolb, E.A.; Lehrnbecher, T.; von Neuhoff, N.; Niktoreh, N.; et al. Second Relapse of Pediatric Patients with Acute Myeloid Leukemia: A Report on Current Treatment Strategies and Outcome of the AML-BFM Study Group. Cancers 2021, 13, 789. [Google Scholar] [CrossRef] [PubMed]
- Pearson, A.D.J.; Zwaan, C.M.; Kolb, E.A.; Karres, D.; Guillot, J.; Kim, S.Y.; Marshall, L.; Tasian, S.K.; Smith, M.; Cooper, T.; et al. Paediatric Strategy Forum for medicinal product development for acute myeloid leukaemia in children and adolescents: ACCELERATE in collaboration with the European Medicines Agency with participation of the Food and Drug Administration. Eur. J. Cancer 2020, 136, 116–129. [Google Scholar] [CrossRef] [PubMed]
- Selim, A.; Alvaro, F.; Cole, C.H.; Fraser, C.J.; Mechinaud, F.; O’Brien, T.A.; Shaw, P.J.; Tapp, H.; Teague, L.; Nivison-Smith, I.; et al. Hematopoietic stem cell transplantation for children with acute myeloid leukemia in second remission: A report from the Australasian Bone Marrow Transplant Recipient Registry and the Australian and New Zealand Children’s Haematology Oncology Group. Pediatr. Blood Cancer 2019, 66, e27812. [Google Scholar] [CrossRef] [PubMed]
- Uy, G.L.; Aldoss, I.; Foster, M.C.; Sayre, P.H.; Wieduwilt, M.J.; Advani, A.S.; Godwin, J.E.; Arellano, M.L.; Sweet, K.L.; Emadi, A.; et al. Flotetuzumab as salvage immunotherapy for refractory acute myeloid leukemia. Blood 2021, 137, 751–762. [Google Scholar] [CrossRef] [PubMed]
- Rafiyath, S.M.; Rasul, M.; Lee, B.; Wei, G.; Lamba, G.; Liu, D. Comparison of safety and toxicity of liposomal doxorubicin vs. conventional anthracyclines: A meta-analysis. Exp. Hematol. Oncol. 2012, 1, 10. [Google Scholar] [CrossRef]
- Batist, G.; Ramakrishnan, G.; Rao, C.S.; Chandrasekharan, A.; Gutheil, J.; Guthrie, T.; Shah, P.; Khojasteh, A.; Nair, M.K.; Hoelzer, K.; et al. Reduced cardiotoxicity and preserved antitumor efficacy of liposome-encapsulated doxorubicin and cyclophosphamide compared with conventional doxorubicin and cyclophosphamide in a randomized, multicenter trial of metastatic breast cancer. J. Clin. Oncol. 2001, 19, 1444–1454. [Google Scholar] [CrossRef]
- Burd, A.; Levine, R.L.; Ruppert, A.S.; Mims, A.S.; Borate, U.; Stein, E.M.; Patel, P.; Baer, M.R.; Stock, W.; Deininger, M.; et al. Precision medicine treatment in acute myeloid leukemia using prospective genomic profiling: Feasibility and preliminary efficacy of the Beat AML Master Trial. Nat. Med. 2020, 26, 1852–1858. [Google Scholar] [CrossRef]
- De Rojas, T.; Kearns, P.; Blanc, P.; Skolnik, J.; Fox, E.; Knox, L.; Rousseau, R.; Doz, F.; Bird, N.; Pearson, A.J.; et al. Changing incentives to ACCELERATE drug development for paediatric cancer. Cancer Med. 2023, 12, 8825–8837. [Google Scholar] [CrossRef]
- Vassal, G.; Rousseau, R.; Blanc, P.; Moreno, L.; Bode, G.; Schwoch, S.; Schrappe, M.; Skolnik, J.; Bergman, L.; Bradley-Garelik, M.B.; et al. Creating a unique, multi-stakeholder Paediatric Oncology Platform to improve drug development for children and adolescents with cancer. Eur. J. Cancer 2015, 51, 218–224. [Google Scholar] [CrossRef]
- Ishimaru, S.; Gueguen, G.; Karol, S.E.; Bautista Sirvent, F.J.; Ceolin, V.; Goemans, B.F.; Bakker, M.; Laurenzio, L.D.; Lukin, J.; Van Tinteren, H.; et al. ITCC-101/APAL2020D: A Randomized Phase 3 Trial of Fludarabine/Cytarabine/Gemtuzumab Ozogamycin with or without Venetoclax in Children with Relapsed Acute Myeloid Leukemia. Blood 2022, 140, 3369–3370. [Google Scholar] [CrossRef]
- Egan, G.; Tasian, S.K. Relapsed pediatric acute myeloid leukaemia: State-of-the-art in 2023. Haematologica 2023, 108, 2275–2288. [Google Scholar] [CrossRef]
- Cooper, T.M.; Alonzo, T.A.; Tasian, S.K.; Kutny, M.A.; Hitzler, J.; Pollard, J.A.; Aplenc, R.; Meshinchi, S.; Kolb, E.A. Children’s Oncology Group’s 2023 blueprint for research: Myeloid neoplasms. Pediatr. Blood Cancer 2023, 70, e30584. [Google Scholar] [CrossRef] [PubMed]
- Brivio, E.; Baruchel, A.; Beishuizen, A.; Bourquin, J.P.; Brown, P.A.; Cooper, T.; Gore, L.; Kolb, E.A.; Locatelli, F.; Maude, S.L.; et al. Targeted inhibitors and antibody immunotherapies: Novel therapies for paediatric leukaemia and lymphoma. Eur. J. Cancer 2022, 164, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Gamis, A.S.; Alonzo, T.A.; Meshinchi, S.; Sung, L.; Gerbing, R.B.; Raimondi, S.C.; Hirsch, B.A.; Kahwash, S.B.; Heerema-McKenney, A.; Winter, L.; et al. Gemtuzumab ozogamicin in children and adolescents with de novo acute myeloid leukemia improves event-free survival by reducing relapse risk: Results from the randomized phase III Children’s Oncology Group trial AAML0531. J. Clin. Oncol. 2014, 32, 3021–3032. [Google Scholar] [CrossRef] [PubMed]
- Meshinchi, S.; Alonzo, T.A.; Stirewalt, D.L.; Zwaan, M.; Zimmerman, M.; Reinhardt, D.; Kaspers, G.J.; Heerema, N.A.; Gerbing, R.; Lange, B.J.; et al. Clinical implications of FLT3 mutations in pediatric AML. Blood 2006, 108, 3654–3661. [Google Scholar] [CrossRef] [PubMed]
- Zwaan, C.M.; Meshinchi, S.; Radich, J.P.; Veerman, A.J.; Huismans, D.R.; Munske, L.; Podleschny, M.; Hählen, K.; Pieters, R.; Zimmermann, M.; et al. FLT3 internal tandem duplication in 234 children with acute myeloid leukemia: Prognostic significance and relation to cellular drug resistance. Blood 2003, 102, 2387–2394. [Google Scholar] [CrossRef]
- Papaemmanuil, E.; Gerstung, M.; Bullinger, L.; Gaidzik, V.I.; Paschka, P.; Roberts, N.D.; Potter, N.E.; Heuser, M.; Thol, F.; Bolli, N.; et al. Genomic Classification and Prognosis in Acute Myeloid Leukemia. N. Engl. J. Med. 2016, 374, 2209–2221. [Google Scholar] [CrossRef]
- Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/midostaurin (accessed on 2 November 2023).
- Available online: https://www.fda.gov/drugs/fda-approves-gilteritinib-relapsed-or-refractory-acute-myeloid-leukemia-aml-flt3-mutation (accessed on 2 November 2023).
- Available online: https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-quizartinib-newly-diagnosed-acute-myeloid-leukemia (accessed on 2 November 2023).
- Pollard, J.A.; Alonzo, T.A.; Gerbing, R.; Brown, P.; Fox, E.; Choi, J.; Fisher, B.; Hirsch, B.; Kahwash, S.; Getz, K.; et al. Sorafenib in Combination with Standard Chemotherapy for Children with High Allelic Ratio FLT3/ITD+ Acute Myeloid Leukemia: A Report from the Children’s Oncology Group Protocol AAML1031. J. Clin. Oncol. 2022, 40, 2023–2035. [Google Scholar] [CrossRef]
- Schlenk, R.F.; Weber, D.; Fiedler, W.; Salih, H.R.; Wulf, G.; Salwender, H.; Schroeder, T.; Kindler, T.; Lübbert, M.; Wolf, D.; et al. Midostaurin added to chemotherapy and continued single-agent maintenance therapy in acute myeloid leukemia with FLT3-ITD. Blood 2019, 133, 840–851. [Google Scholar] [CrossRef]
- Levis, M. MT-CTN 1506 (MORPHO): A randomised trial of the FLT3 inhibitor gilteritinib as post-transplant maintenance for FLT3-ITD AML. EHA Libr. 2023. [Google Scholar]
- Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-regular-approval-venetoclax-combination-untreated-acute-myeloid-leukemia (accessed on 2 November 2023).
- Karol, S.E.; Bittencourt, H.; Morgenstern, D.A.; Macy, M.E.; Khaw, S.L.; Cooper, T.M.; Petit, A.; Ramsingh, G.; Tong, B.; Unnebrink, K.; et al. Venetoclax Alone or in Combination with Chemotherapy: Responses in Pediatric Patients with Relapsed/Refractory Acute Myeloid Leukemia with Heterogeneous Genomic Profiles. Blood 2020, 136, 30–31. [Google Scholar] [CrossRef]
- Place, A.E.; Goldsmith, K.; Bourquin, J.P.; Loh, M.L.; Gore, L.; Morgenstern, D.A.; Sanzgiri, Y.; Hoffman, D.; Zhou, Y.; Ross, J.A.; et al. Accelerating drug development in pediatric cancer: A novel Phase I study design of venetoclax in relapsed/refractory malignancies. Future Oncol. 2018, 14, 2115–2129. [Google Scholar] [CrossRef] [PubMed]
- Balgobind, B.V.; Raimondi, S.C.; Harbott, J.; Zimmermann, M.; Alonzo, T.A.; Auvrignon, A.; Beverloo, H.B.; Chang, M.; Creutzig, U.; Dworzak, M.N.; et al. Novel prognostic subgroups in childhood 11q23/MLL-rearranged acute myeloid leukemia: Results of an international retrospective study. Blood 2009, 114, 2489–2496. [Google Scholar] [CrossRef] [PubMed]
- Van Weelderen, R.E.; Klein, K.; Harrison, C.J.; Jiang, Y.; Abrahamsson, J.; Arad-Cohen, N.; Bart-Delabesse, E.; Buldini, B.; De Moerloose, B.; Dworzak, M.N.; et al. Measurable Residual Disease and Fusion Partner Independently Predict Survival and Relapse Risk in Childhood KMT2A-Rearranged Acute Myeloid Leukemia: A Study by the International Berlin-Frankfurt-Münster Study Group. J. Clin. Oncol. 2023, 41, 2963–2974. [Google Scholar] [CrossRef] [PubMed]
- Tasian, S.K.; Loh, M.L.; Hunger, S.P. Childhood acute lymphoblastic leukemia: Integrating genomics into therapy. Cancer 2015, 121, 3577–3590. [Google Scholar] [CrossRef] [PubMed]
- Kühn, M.W.; Song, E.; Feng, Z.; Sinha, A.; Chen, C.W.; Deshpande, A.J.; Cusan, M.; Farnoud, N.; Mupo, A.; Grove, C.; et al. Targeting Chromatin Regulators Inhibits Leukemogenic Gene Expression in NPM1 Mutant Leukemia. Cancer Discov. 2016, 6, 1166–1181. [Google Scholar] [CrossRef]
- Rasouli, M.; Blair, H.; Troester, S.; Szoltysek, K.; Cameron, R.; Ashtiani, M.; Krippner-Heidenreich, A.; Grebien, F.; McGeehan, G.; Zwaan, C.M.; et al. The MLL-Menin Interaction is a Therapeutic Vulnerability in NUP98-rearranged AML. Hemasphere 2023, 7, e935. [Google Scholar] [CrossRef]
- Klossowski, S.; Miao, H.; Kempinska, K.; Wu, T.; Purohit, T.; Kim, E.; Linhares, B.M.; Chen, D.; Jih, G.; Perkey, E.; et al. Menin inhibitor MI-3454 induces remission in MLL1-rearranged and NPM1-mutated models of leukemia. J. Clin. Invest. 2020, 130, 981–997. [Google Scholar] [CrossRef]
- Erba, H.P.; Fathi, A.T.; Issa, G.C.; Altman, J.K.; Montesinos, P.; Patnaik, M.M.; Foran, J.M.; De Botton, S.; Baer, M.R.; Schiller, G.J.; et al. Update on a Phase 1/2 First-in-Human Study of the Menin-KMT2A (MLL) Inhibitor Ziftomenib (KO-539) in Patients with Relapsed or Refractory Acute Myeloid Leukemia. Blood 2022, 140, 153–156. [Google Scholar] [CrossRef]
- Le, Q.; Leonti, A.R.; Tang, T.T.; Castro, S.; Nourigat-Mckay, C.; Perkins, L.; Ries, R.E.; Smith, J.L.; Hylkema, T.A.; Pardo, L.; et al. Therapeutic Targeting of CD74 with STRO-001 Antibody-Drug Conjugate in AML and ALL. Blood 2021, 138, 509. [Google Scholar] [CrossRef]
- Meshinchi, S.; Miller, L.; Massaro, S.; Williams, R.; Krieger, E.; Pauly, M.; Nelson, C.; Bhojwani, D.; Johnson, R.; Horton, T.M.; et al. Anti-Leukemic Activity of STRO-002 a Novel Folate Receptor-α (FR-α)-Targeting ADC in Relapsed/Refractory CBF2AT3-GLIS2 AML. Blood 2022, 140, 159–161. [Google Scholar] [CrossRef]
- Dafflon, C.; Craig, V.J.; Méreau, H.; Gräsel, J.; Schacher Engstler, B.; Hoffman, G.; Nigsch, F.; Gaulis, S.; Barys, L.; Ito, M.; et al. Complementary activities of DOT1L and Menin inhibitors in MLL-rearranged leukemia. Leukemia 2017, 31, 1269–1277. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://irp.cdn-website.com/c584cf91/files/uploaded/ACCELERATE%20Meeting%20on%20Menin%20Inhibitors_Summary.pdf (accessed on 15 March 2023).
- Hahn, C.K.; Berchuck, J.E.; Ross, K.N.; Kakoza, R.M.; Clauser, K.; Schinzel, A.C.; Ross, L.; Galinsky, I.; Davis, T.N.; Silver, S.J.; et al. Proteomic and genetic approaches identify Syk as an AML target. Cancer Cell 2009, 16, 281–294. [Google Scholar] [CrossRef] [PubMed]
- Issa, G.C.; DiNardo, C.D. Acute myeloid leukemia with IDH1 and IDH2 mutations: 2021 treatment algorithm. Blood Cancer J. 2021, 11, 107. [Google Scholar] [CrossRef] [PubMed]
- Alexander, T.B.; Lacayo, N.J.; Choi, J.K.; Ribeiro, R.C.; Pui, C.H.; Rubnitz, J.E. Phase I Study of Selinexor, a Selective Inhibitor of Nuclear Export, in Combination with Fludarabine and Cytarabine, in Pediatric Relapsed or Refractory Acute Leukemia. J. Clin. Oncol. 2016, 34, 4094–4101. [Google Scholar] [CrossRef]
- Testa, U.; Pelosi, E.; Frankel, A. CD 123 is a membrane biomarker and a therapeutic target in hematologic malignancies. Biomark. Res. 2014, 2, 4. [Google Scholar] [CrossRef]
- Bras, A.E.; de Haas, V.; van Stigt, A.; Jongen-Lavrencic, M.; Beverloo, H.B.; Te Marvelde, J.G.; Zwaan, C.M.; van Dongen, J.J.M.; Leusen, J.H.W.; van der Velden, V.H.J. CD123 expression levels in 846 acute leukemia patients based on standardized immunophenotyping. Cytom. B Clin. Cytom. 2019, 96, 134–142. [Google Scholar] [CrossRef]
- Lamble, A.J.; Liu, X.; Minard, C.; Militano, O.; Bernhardt, M.B.; Cooper, T.M.; Kolb, E.A.; Breese, E.H.; Fox, E.; Tasian, S.K.; et al. Safety and Activity of Flotetuzumab in Pediatric and Young Adult Patients with Relapsed/Refractory Acute Myeloid Leukemia: Results from the COG PEPN1812 Phase 1 Trial. Blood 2022, 140, 6209–6210. [Google Scholar] [CrossRef]
| Study Group | Countries | New Patients per Year |
|---|---|---|
| NOPHO-DB-SHIP 1 | Belgium, Denmark, Estonia, Finland, Hong-Kong, Israel, Iceland, Latvia, Lithuania, The Netherlands, Norway, Portugal, Spain, Sweden, Uruguay | ~150 |
| AIEOP-BFM 2 | Austria, Czech Republic, Germany, Italy, Poland, Slovenia, Slovakia | ~200 |
| MyeChild | Australia, France, Ireland, Switzerland, United Kingdom | ~180 |
| JCCG 3 | Japan | ~100 |
| COG 4 | United States, Canada | ~700 |
| St. Jude | United States | ~50 |
| All groups | ~1380 |
| Study | Years of Enrollment | Study Question | Relapse Status | Nr. Pts | CR (%) | EFS (%) and (Median FU) | OS (%) and (Median FU) | Ref. |
|---|---|---|---|---|---|---|---|---|
| LAME89/91 | 1988–1998 | Post-relapse survival | 1st relapse | 106 | 71 | DFS 45 (5-y) | 33 (5-y) | [8] |
| NOPHO | 1993–2012 | Various regimens | 1st relapse | 208 | 70 | 39 (5-y) | [9] | |
| Japanese AML Cooperative Study | 2000–2005 | Various regimens | 1st relapse after AML99 protocol | 71 | 50 | 37 (5-y) | [10] | |
| AML BFM-SG compassionate use series | 1995–2014 | GO+ cytarabine | Relapsed/refractory (mostly 2nd) | 76 | 18 (all pts) 27 (transplanted) (4-y) | [11] | ||
| I-BFM AML 2001/01 | 2001–2009 | FLAG vs. FLAG + DNX | 1st relapse | 394 | 59 vs. 69 | 34 (5-y) | [12] | |
| AML-BFM SG relapse registry | 2009–2017 | DNX+FLA(G) +/− FLA vs. other re-induction therapies | 1st relapse | 197 | 45 n = 156 DNX- FLA(G) +/− FLA | 30 (5-y) n = 156 DNX-FLA(G) +/− FLA | 42 (5-y) | [7] |
| I-BFM AML 2001/02 phase II | 2001–2009 | GO single agent | Relapsed/ refractory | 30 | ORR 37 | 27 (3-y, responders only) | [13] | |
| NOPHO-DB SHIP | 2004–2019 | Retrospective cohort review | Refractory 1st relapse/ 2nd relapse | 157 | 22 (1-y) 14 (5-y) | [14] | ||
| JPLSG | 2006–2010 | Retrospective cohort review | 1st relapse | 111 | 64 63 ECM 66 FLAG 36 others | 36 (5-y) | [15] | |
| COG AAML0523 phase I/II | 2007–2012 | Clofarabine/cytarabine | Relapsed/ refractory | 51 | ORR 48 | 46 (3-y, responders only) | [16] | |
| COG AAML-07P1 phase II | 2008–2011 | Cytarabine/ida/bortezomib vs. Cytarabine/etoposide/bortezomib | Relapsed/ refractory tAML | 37 | 57 vs. 48 | 39 (2-y) | [17,18] | |
| ITCC 020 phase Ib | 2010–2014 | Clofarabine with FLA + DNX | Relapsed/ refractory | 34 | ORR 68 | 35 (1-y) | 50 (1-y) | [19] |
| COG AAML1421 phase I/II | 2016–2018 | CPX351, followed by FLAG | Relapsed/ refractory | 37 | ORR 81 | [20] | ||
| Venetoclax phase I | 2017–2019 | Venetoclax/cytarabine | Relapsed/ refractory | 38 | ORR 69 | [21] |
| Drug | Mechanism of Action | Indication | Approval Status | Pediatric Studies | Pediatric Study Population |
|---|---|---|---|---|---|
| CPX-351 | Liposomal formulation cytarabine/daunorubicin | Newly diagnosed t-AML or AML-MRC | USA: approved for adult and pediatric patients aged 1 and older EU: approved for adult patients | EudraCT 2020-000142-34 [recruiting] NCT04915612 [recruiting] NCT04293562 [recruiting] | early 1st R or ≥2nd R AML 1–21 y relapsed AML ≤21 y newly diagnosed AML <21 y |
| Enasidenib mesylate | IDH2 inhibitor | R/R AML with IDH2 mutation | USA: approved for adult patients | NCT04203316 [recruiting] NCT02813135 [recruiting] | IDH2 mutated ≥2nd R/R AML 2–18 y R/R hematologic or solid tumor <18 y |
| Ivosidenib Olutasidenib | IDH1 inhibitor | Newly diagnosed IDH1 mutated patients with AML R/R AML with IDH1 mutation R/R AML with IDH1 mutation | USA: approved for adult patients EU: approved for adult patients | NCT03245424 [expanded access program] | R/R IDH1 mutated AML ≥12 y |
| Gemtuzumab Ozogamicine | Conjugated antibody against CD33 | Newly diagnosed CD33-positive AML in adults and R/R CD33-positive AML in adults and in pediatric patients 2 years and older | USA: approved for adult and pediatric patients aged 2 and older EU: approved for patients aged 15 years and above who have not tried other treatments. | NCT04293562 [recruiting] NCT02724163 [recruiting] | newly diagnosed AML ≤21 y AML/HR MDS /isolated MS <18 y |
| Gilteritinib | FLT3 inhibitor | R/R AML with FLT3 mutation as monotherapy | USA: approved for adult patients EU: approved for adult patients | NCT04293562 [recruiting] NCT04240002 [recruiting] | newly diagnosed AML ≤21 y FLT3-ITD R/R AML ≥6 m–21 y |
| Midostaurin | FLT3 inhibitor | Newly diagnosed AML with FLT3 mutation, combined with chemotherapy | USA: approved for adult patients EU: approved for adult patients | NCT03591510 [recruiting] | FLT3-mutant AML ≥3 m–17 y |
| Glasdegib | SMO inhibitor hedgehog pathway | Newly diagnosed AML in patients ≥ 75 years or ineligible for intensive chemotherapy | USA: approved for adult patients EU: approved for adult patients | Waiver for pediatric development | |
| Venetoclax | BCL2 inhibitor | Newly diagnosed AML in patients ≥ 75 years or ineligible for intensive chemotherapy, in combination with HMA/low dose Ara-c | USA: approved for adult patients EU: approved for adult patients | NCT05183035 [recruiting] | ≥2nd R AML or 1st R AML intolerant to anthracycline ≥ 29 d−≤ 21 y |
| Azacitidine | Hypomethylating agent | Maintenance and adult AML and MDS | USA: approved for adult patients and for children with JMML EU: approved for adult patients | NCT03825367 [closed early due to lack of activity] | R/R AML 1–30 y |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceolin, V.; Ishimaru, S.; Karol, S.E.; Bautista, F.; Goemans, B.F.; Gueguen, G.; Willemse, M.; Di Laurenzio, L.; Lukin, J.; van Tinteren, H.; et al. The PedAL/EuPAL Project: A Global Initiative to Address the Unmet Medical Needs of Pediatric Patients with Relapsed or Refractory Acute Myeloid Leukemia. Cancers 2024, 16, 78. https://doi.org/10.3390/cancers16010078
Ceolin V, Ishimaru S, Karol SE, Bautista F, Goemans BF, Gueguen G, Willemse M, Di Laurenzio L, Lukin J, van Tinteren H, et al. The PedAL/EuPAL Project: A Global Initiative to Address the Unmet Medical Needs of Pediatric Patients with Relapsed or Refractory Acute Myeloid Leukemia. Cancers. 2024; 16(1):78. https://doi.org/10.3390/cancers16010078
Chicago/Turabian StyleCeolin, Valeria, Sae Ishimaru, Seth E. Karol, Francisco Bautista, Bianca Frederika Goemans, Gwenaëlle Gueguen, Marieke Willemse, Laura Di Laurenzio, Jennifer Lukin, Harm van Tinteren, and et al. 2024. "The PedAL/EuPAL Project: A Global Initiative to Address the Unmet Medical Needs of Pediatric Patients with Relapsed or Refractory Acute Myeloid Leukemia" Cancers 16, no. 1: 78. https://doi.org/10.3390/cancers16010078
APA StyleCeolin, V., Ishimaru, S., Karol, S. E., Bautista, F., Goemans, B. F., Gueguen, G., Willemse, M., Di Laurenzio, L., Lukin, J., van Tinteren, H., Locatelli, F., Petit, A., Tomizawa, D., Norton, A., Kaspers, G., Reinhardt, D., Tasian, S. K., Nichols, G., Kolb, E. A., ... Cooper, T. M. (2024). The PedAL/EuPAL Project: A Global Initiative to Address the Unmet Medical Needs of Pediatric Patients with Relapsed or Refractory Acute Myeloid Leukemia. Cancers, 16(1), 78. https://doi.org/10.3390/cancers16010078








