Simple Summary
The myogenic differentiation 1 gene (MYOD1) p.L122R mutation was first discovered in a subset of clinically aggressive rhabdomyosarcomas in both adults and children. It occurs most frequently in spindle cell (Sp) or sclerosing (Sc) RMS, but also occasionally in ERMS, including 3% of all PAX fusion-negative RMS. The presence of the MYOD1L122R mutation seems to be associated with a very poor prognosis, especially when it occurs concomitantly with other mutations such as PIK3CA. In this review, we consider the known biological effects of MYOD1 mutations and present a review of published cases of RMS with MYOD1 mutations. Together, the reviewed biological characteristics and the clinical features focus attention on this specific subgroup of patients with poor outcome and highlight the need to identify an optimal therapeutic strategy.
Abstract
Major progress in recent decades has furthered our clinical and biological understanding of rhabdomyosarcoma (RMS) with improved stratification for treatment based on risk factors. Clinical risk factors alone were used to stratify patients for treatment in the European Pediatric Soft Tissue Sarcoma Study Group (EpSSG) RMS 2005 protocol. The current EpSSG overarching study for children and adults with frontline and relapsed rhabdomyosarcoma (FaR-RMS NCT04625907) includes FOXO1 fusion gene status in place of histology as a risk factor. Additional molecular features of significance have recently been recognized, including the MYOD1L122R gene mutation. Here, we review biological information showing that MYOD1L122R blocks cell differentiation and has a MYC-like activity that enhances tumorigenesis and is linked to an aggressive cellular phenotype. MYOD1L122R mutations can be found together with mutations in other genes, such as PIK3CA, as potentially cooperating events. Using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, ten publications in the clinical literature involving 72 cases were reviewed. MYOD1L122R mutation in RMS can occur in both adults and children and is frequent in sclerosing/spindle cell histology, although it is also significantly reported in a subset of embryonal RMS. MYOD1L122R mutated tumors most frequently arise in the head and neck and extremities and are associated with poor outcome, raising the issue of how to use MYOD1L122R in risk stratification and how to treat these patients most effectively.
1. Introduction
Rhabdomyosarcoma (RMS) is the most frequent soft tissue sarcoma in children and adolescents, accounting for 5% of all pediatric cancers [1]. Major progress has been made in recent decades to improve knowledge of the disease and its biology, with subsequent better stratification of treatment, based on risk factors. Accordingly, survival in recent years has improved, especially for patients with localized tumors, reaching a 5-year overall survival (OS) of 85% for high-risk disease [2]. This has been possible due to risk-adapted, multidisciplinary treatment, with the most recent advance being the introduction of maintenance treatment for high-risk patients [2]. Despite all these efforts, relapse still occurs in 24% of patients [3,4,5,6] and, additionally, RMS is refractory to frontline treatment in a small number of patients, including 2% of intermediate-risk patients [7,8].
Various clinical risk factors were used to stratify treatment in the European Pediatric Sarcoma Study Group (EpSSG) RMS 2005 protocol including histology, primary disease site, nodal involvement, age < or ≥10 years, size ≤5 or >5 cm and distant metastasis [7,9,10]. Moreover, since the introduction of the RMS 2005 protocol, alveolar histology has been better characterized as being associated with the presence of PAX3::FOXO1 or PAX7::FOXO1 fusion in 85–90% of alveolar tumors [11]. In addition, fusion status has been found to correlate better than histology with prognosis [12]. Thanks to the progress and the routine use of techniques of molecular characterization, new genetic abnormalities have been progressively identified in RMS, such as new fusion transcripts including PAX3::NCOA1, PAX3::NCOA2, VGLL2::NCOA2, FUS::TFCP2, EWSR::TFCP2 [13,14,15,16], as well as new somatic pathogenic mutations such as MYOD1 and TP53 mutations [17,18].
The discovery of myogenic differentiation 1 (MYOD1) mutations is closely related to the emerging evidence of spindle cell (SpRMS) and sclerosing (ScRMS) subtypes of RMS as separate entities from the other histologic subtypes. SpRMS was first described in children in a report by Cavazzana et al. in 1992 [19], followed by the sclerosing subtype (ScRMS), described between 2000 and 2004 by different authors, first in adult case series [20,21], then in the pediatric setting [22], with a variable outcome. While in previous classifications Sp/ScRMS was considered a subtype of ERMS, in 2013 Sp/ScRMS subtypes were defined as a stand-alone entity in the WHO classification [23]. Later on, in the 2020 WHO classification, Sp/ScRMS evolved further as it included three different groups: infantile subgroup with recurrent VGLL2::NCOA2 and other fusions; MYOD1 mutated subgroup; Sp and epithelioid RMS with TFCP fusions. However, spindle RMS outside this context is probably part of the ERMS group [24].
Since the first report from Memorial Sloan Kettering Center published in Nature Genetics in 2014 [25], the MYOD1L122R somatic mutation has been reported repeatedly in case series and case reports of adult and pediatric patients with Sp/ScRMS [17]. The biology of MYOD1 and the clinical features of the patients with MYOD1L122R mutated tumors have not been comprehensively characterized and little is known about its true prognostic role.
The aim of this review is to draw together understanding of the biology of MYOD1L122R mutation and its frequency in tumors from patients affected by RMS and to explore clinical features of such patients, the prognostic role of MYOD1L122R mutation and the possible implications for risk stratification and treatment.
Firstly, we reviewed the literature on MYOD1 biology to give an overview of the normal functioning of the protein and its altered mechanism of action when mutated in RMS to MYOD1L122R. Secondly, we focused on clinical aspects of patients with MYOD1L122R mutated RMS through a review of the clinical records reported in the literature. A search in PubMed identified case reports, cases series, reviews and articles including cases of patients (adults and children) with RMS bearing MYOD1L122R somatic mutations, from the first report of MYOD1L122R mutation published in 2014 to September 2022, according to PRISMA guidelines (Supplementary Materials Figure S1). To enlarge the search, we also looked for papers focused on Sp- and ScRMS. Used terms and words were: MYOD1, RMS, spindle cell RMS, sclerosing RMS, pediatric RMS, adult RMS. Contributions in English, French and Italian were considered. The minimum data required to include a case record in our analysis were age at diagnosis, sex, site of the primary tumor, histology and confirmation of MYOD1L122R mutation. Description of events and outcome criteria were looked for, but, since they were not described in detail for most of the cases, they were not mandatory to include the reference in our analysis. Papers with insufficient data for the purpose of our study were excluded. All the cases that were reported twice (or more) through the different reports have been carefully checked for, identified and presented just once. Events and outcome were taken into account only for patients with a minimal follow-up of 12 months.
2. Normal Role for MYOD1 in Myogenesis
Myogenic determination factor 1 (MYOD1) is one of the four originally described myogenic regulatory factors identified towards the end of the 1980s [26] (along with myogenin MYF4, MYF5 and MYF6 (also known as MRF4 or herculin) [27]). All of these proteins share the ability to convert non-myogenic cells such as fibroblasts to the muscle lineage upon transfection of their encoding cDNA alone. These four factors are highly conserved in vertebrates, including birds and amphibians [28]. They are expressed sequentially in embryogenesis beginning with MYF5 then MYOD1, MYF6 and MYF4. MYF5 and MYOD1 are responsible for the specification and determination of skeletal myoblasts, whereas MYF4 plays a role in the formation of myofibers (MYF4 null mice have normal numbers of myoblasts but lack muscle fibers) [29]. Expression of MYF5 and MYOD1 protein is absent in quiescent satellite stem cells [30,31,32]. Evidence from knockout mouse models suggests that there is a degree of functional redundancy between MYOD1 and MYF5, as single knockout models of either gene result in normal muscle development. Notably in MYOD1 null mice, MYF5 is significantly upregulated as a compensatory mechanism [33,34]. Double knockout mice for MYOD1 and MYF5, in contrast, are born immobile soon after birth with complete skeletal muscle aplasia [34]. Subsequently, it has been shown that attempting to rescue muscle formation in these mice by replacing the MYOD1 coding sequence with that of MYF5 is unsuccessful, showing that temporal and spatial expressions of these genes are distinct [35]. Additional evidence that these two genes cannot fully compensate for each other in all contexts comes from experimental models demonstrating that MYOD1 deficient mice were unable to regenerate muscle following injury due to myogenic precursor cells continuing to self-renew rather than enter the differentiation pathway following satellite cell activation [36].
The four primary myogenic factors also share homology at the proteomic level with a very large transcription factor superfamily, the basic helix–loop–helix (bHLH) family, which comprises hundreds of members. These proteins bind E-box motifs in the genome (CANNTG) following dimerization; in the case of MYOD1, heterodimerization occurs with a member of the E-protein bHLH family [37]. The MYOD1:E-protein heterodimer shows a preference for binding the VCASCTGT E-box site (where V indicates not T, and S indicates G or C). Transcriptional regulation of myogenesis by MYOD1 is multifaceted and complex, as E-box binding motifs occur very frequently in the genome, allowing MYOD1 to bind at thousands of different locations. The majority of loci bound by MYOD1 are therefore not muscle-specific genes and indeed MYOD1 has been found to affect regional transcription by causing widespread histone acetylation through recruiting histone acetyltransferases (HATs) and opening up chromatin to other transcription factors and machinery [38]. This indirect mode of regulation means that binding of MYOD1 to a gene promoter may not result in any direct expression of that gene. MYOD1 primarily drives progression of muscle differentiation by direct transactivation, via use of “feed-forward” circuits whereby MYOD1 activates transcription of muscle-specific transcription factors which later in the differentiation pathway activate a further set of genes by co-operatively binding with MYOD1 [39]. MYOD1 also participates in negative (termed incoherent) feed-forward circuits to achieve temporal co-ordination of myogenic differentiation where MYOD1 activates proteins that subsequently compete with it for promoter or enhancer binding at muscle gene loci [40].
3. MYOD1L122R Mutation Blocks Differentiation of the Cells and Has an MYC-like Activity
A very early study by Van Antwerp et al., published long before any MYOD1 mutations had been found in RMS, investigated the consequences of mutating various residues in the basic DNA-binding domain of MYOD1 to the analogous residue of MYC, the oncoprotein which is also a member of the bHLH transcription factor family [41]. This study identified one mutation which allowed MYOD1 to continue to bind MYOD1 binding sites but no longer transactivated target genes, and additionally was now also capable of binding MYC binding sites and repressing a reporter construct phenocopying the action of MYC. This mutation was the substitution of leucine with arginine (L122R), the recurrent mutation observed in RMS. The authors prophetically predicted that this mutation (achieved by a single base substitution in the coding sequence of MYOD1 DNA) could have a role in skeletal muscle oncogenesis. Following the first detection of the L122R mutation in RMS tumors, further functional work confirmed these initial findings. Kohsaka et al. introduced ectopic expression of MYOD1L122R into C2C12 mouse myoblasts and demonstrated that they were no longer able to be induced to differentiate and express muscle markers or undergo fusion to form myofibers in comparison to wild-type MYOD1 or controls [25]. This effect is seen in the presence of the normal wild-type MYOD1, suggesting that MYOD1L122R can act in a dominant negative manner. Gene expression profiling of the mouse myoblast models supported a shift in expression pattern towards a more MYC-like signature and, similarly, analysis of histone modification by ChIP sequencing showed a stronger deposition of activating histone marks (H3K4me3) at MYC target genes compared to wild-type MYOD1. The overall picture suggests that the binding site repertoire of mutant MYOD1 has expanded to include MYC-regulated genes while still retaining the ability to bind MYOD1 sites at myogenic gene loci, yet blocking expression of these genes by competing with normal MYOD1 and preventing differentiation. In comparison with normal myoblasts, RMS typically expresses both MYOD1 and myogenin yet fails to undergo terminal differentiation. MYOD1 was found to bind myogenic loci more poorly in the RD embryonal RMS cell line compared to primary human myoblasts, therefore it is unclear what the contribution of MYOD1L122R would be to an existing underlying defect in differentiation in embryonal RMS [42]. A schema for the functional behavior of MYOD1L122R is summarized in Figure 1.
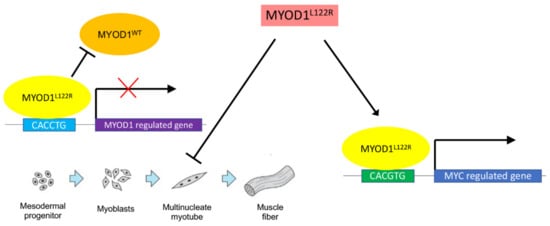
Figure 1.
How MYOD1L122R can contribute towards an aggressive phenotype in RMS. MYOD1L122R contributes to aggressive disease in RMS, leading to poor outcomes, in two potential ways. Firstly, MYOD1L122R can act in a dominant negative manner and bind MYOD1-responsive promoters, blocking normal MYOD1 from binding but failing to transactivate these myogenic genes, resulting in a failure of myoblasts to differentiate and keeping them in a proliferating state. Secondly, MYOD1L122R can additionally bind to MYC-responsive genes and activate an oncogenic program of transcription.
4. MYOD1L122R Affects Tumorigenesis and Causes an Aggressive Biological Phenotype
Evidence of the phenotypic behavior of cells harboring the MYOD1L122R mutation from the mouse myoblast model generated by Kohsaka et al. indicates more aggressive tumorigenic behavior [25]. MYOD1L122R-expressing cells do not proliferate any faster than controls but do form more colonies in the anchorage-independent soft agar assay (a tumorigenic property that predicts tumor formation in nude mice). C2C12 myoblast cells expressing exogenous MYOD1L122R exhibited tumor formation in in vivo xenograft models in comparison to the parental cell line which does not form tumors in mice, however, when the MYOD1L122R mutation was combined with an activating mutation in PIK3CA, a dramatic increase in tumor size was observed.
5. MYOD1L122R Mutation Frequently Occurs with Other Mutations
A large panel sequencing study of somatic mutations in RMS tumor samples, which identified 17 MYOD1L122R cases, illustrates the enrichment of other mutations found in mutant MYOD1 cohorts, particularly PIK3CA and other PI3K pathway genes which are involved in approximately half of mutant MYOD1 tumors, and the RAS pathway which accounts for at least another quarter [18]. Mutations in these pathways are not mutually exclusive, with some tumors containing RAS, PIK3CA and MYOD1 mutations. This suggests that MYOD1 may require these cooperating mutations to achieve its full spectrum of tumorigenic behavior. Interestingly, in the Kohsaka et al. study, an activating mutation in PIK3CA led to increased proliferation but not increased soft agar colony formation and therefore the mutations in MYOD1 and PIK3CA led to complementary but not overlapping phenotypes in mouse myoblasts [25]. Further understanding of the possible cooperative nature and dependencies on the different mutations associated with MYOD1L122R is required.
6. MYOD1L122R Mutation Can Occur Both in Adults and Children
This section describes the 72 cases of adult and pediatric RMS with somatic mutation of MYOD1 reported in 10 publications that fulfill our selection criteria, as summarized in Table 1 and Supplementary Materials Figure S1.

Table 1.
Cases of RMS bearing MYOD1L122R mutation described in literature. Summary of cases of RMS with MYOD1L122R mutation presented in literature. All patients had MYOD1L122R mutation. ERMS: embryonal RMS, ScRMS: sclerosing RMS, SCRMS: spindle cell RMS, LR: local relapse, DR: distant relapse, DOD: dead of disease, NED: no evidence of disease, AWD: alive with disease, na: not available. Please note that for other mutations, different methods were used by different authors to assess the co-occurrence of other molecular abnormalities (such as targeted Sanger sequencing, exome sequencing, RNA sequencing).
MYOD1 mutation has been described in both adults and children with RMS, although it appears more frequent in the adult population, particularly in the Sp/Sc subtypes [43]. In the summary of the cases described to date that are shown in Table 1, the majority of patients (43/72, 60%) are ≥18 years of age. Among 29 patients aged <18 years, the median age is 10 years (range 2 to 17 years). Patients aged <10 years represent only 17% (12/72) of all cases described. In pediatric cases, MYOD1L122R mutations seem to occur in older children and the mutation has not been described in children aged less than 1 year old, as reported previously by Alaggio et al. [13].
According to the observations by Agaram et al. [46], there is no sex preference, with no significant difference in the mutant cohort from the slight majority of affected males seen in pediatric RMS in general. However, among all the published cases, 30/72 (42%) patients are males and 42/72 are females (58%) (Table 1). Moreover, within the pediatric subgroup, 23/29 patients (78%) are female.
7. MYOD1L122R Is Frequent in Sc/Sp Cell Histology but also Present in a Subset of Embryonal RMS
The MYOD1L122R mutation was first reported in tumors with Sp/Sc histology, with a frequency ranging from 30 to 67% depending on the case series [25,45,46]. Moreover, different authors have pointed out that ERMS can also bear a MYOD1L122R mutation, in up to 10% of embryonal RMS, most often in adolescents or young adults, with a slightly higher predilection for the female sex and with tumors localized in the head and neck [22,25,45,46]. A recent genomic classification in a large cohort of pediatric RMS showed that MYOD1 mutations occur in 3% of fusion-negative patients (where “fusion negative” includes tumors without the canonical PAX3::FOXO1 or PAX7::FOXO1 fusion, pathognomonic of ARMS) [18]. Moreover, MYOD1L122R mutations have never been described in any case of PAX::FOXO1 fusion-positive RMS. Among cases with confirmed MYOD1 mutations reported in Table 1 which includes both adults and children, 26/72 (36%) of cases had Sp cell histology, 25/72 (35%) had Sc histology, 12/72 (17%) were ERMS and 9/72 (12%) tumors showed a combination of Sp/Sc areas. However, the retrospective character of the analysis and the absence of any centralized pathological review prevents us from drawing strong conclusions about the real MYOD1 L122R distribution among histotypes.
8. MYOD1L122R Mutated Tumors Most Frequently Arise at Head and Neck and Extremity Sites
Shern et al.’s genomic characterization of RMS at diagnosis in children included 641 patients from two separate cohorts in the UK and USA, including 515 fusion-negative RMS and 126 fusion-positive RMS [16]. Among the 17 cases of MYOD1L122R mutated tumors, 16 were located in the head and neck, (including 9/16 (56%) at parameningeal subsite), and in 1 case at the extremities [18]. Among the whole reported cohort of MYOD1L1222R cases, noting the limitation of the absence of a radiological centralized review, in 31/72 (43%) the primary site was the head and neck (and just 4/31 cases had parameningeal extension) and extremities in 27/72 (38%). In the pediatric subset, the primary site was in the head and neck in 14/28 tumors (50%) and the extremities in 7/28 (25%). Only 3/14 children with head and neck tumors showed parameningeal extension, similar to the low incidence of 1/3 in the series by Owosho et al. [28]. The information regarding nodal extension and distant metastasis at diagnosis is missing for all the cases.
9. MYOD1L122R Mutation Is Associated with a Poor Outcome
The first published report describing Sp- and ScRMS in pediatric and adult patients [43] included a small cohort of nine patients with MYOD1L122R mutated RMS. Follow-up of at least 12 months was available for 11 patients (including 8/9 MYOD1 L122R mutated patients), and among them 9 had an event (64%). In 7/9 patients who had an event, the tumor was MYOD1 L122R mutated and in all the cases the event included a distant relapse. Among the 8 MYOD1L122R mutated RMS patients with a follow-up > 12 months, 2/8 did not have evidence of disease (NED), 2/8 were alive with disease (AWD) and 4/8 were dead of the disease (DOD) [43]. The authors thus concluded that relapse is a frequent event in the subgroup of Sp- and ScRMS bearing MYOD1L122R mutation.
Moreover, in the report by Alaggio et al. describing only pediatric patients with Sp cell and ScRMS (n = 26), the authors underlined the striking differences between pathology in infants and older children [13]. In the infant setting, Sp and Sc histology had wild-type MYOD1 but showed typical fusion transcripts involving VGLL and NCOA2 as partners. All infantile patients were alive without event. In contrast, in the cohort of 10 older children with Sp or Sc histology and MYOD1L122R mutation, 7 had early events, with a median time interval of 1.5 years from diagnosis of whom all were dead of disease, 1 patient was alive with disease, 1 had no evidence of disease with a follow-up of 1 year and 1 case was still on treatment. Details of the events are not available, and there is insufficient information to distinguish relapse from primary refractory disease. A better characterization of the events can be found in the report by Agaram et al. published in 2019 [46]. In this cohort of 30 patients, (15 adults, 15 children), with MYOD1L122R mutated RMS, follow-up was available for 22 patients. Among 20 patients with at least 12 months of surveillance, 16/20 showed at least one event: in 5 cases the event was a local relapse, in 4 cases a distant relapse and in 7 cases a combined local and distant relapse.
The striking difference between the outcome of MYOD1 wild-type and MYOD1L122R mutated tumors can be appreciated in the survival analysis by Shern et al. [18]. MYOD1L122R mutated tumors have a worse event-free survival (EFS) independently of the risk group of classification (5-year EFS in MYOD1L122R mutated tumors <10% versus MYOD1 wild-type 75%, p < 0.0001), based on the known risk factors used in the Children’s Oncology Group (COG) and EpSSG RMS 2005 protocol.
In the cohort described in Table 1, 37/72 (52%) patients had follow-up of at least 12 months (range 12–134 months), including 18 pediatric patients. Information on events was available only for 33/37 (Table 2). Nine patients (24%) had no event. Events were recorded in 24/33 cases (72%) patients. In 8/24 (33%) the event was a local relapse, in 5/24 (21%) a distant relapse and in 11/24 (46%) a combined local and distant relapse. If we focus just on the 18 pediatric patients with follow-up, information on events was recorded for 15 of them: 3/15 (20%) had no event, 5/15 (33%) had a local relapse, 1/15 (7%) had a distant relapse and 6/15 (40%) had a combined local plus distant relapse. Unfortunately, the time interval from diagnosis to the event was not described. Among these 37 patients, 9/37 (24%) were reported as NED, 12/37 (33%) were AWD and 16/37 (43%) were DOD. NED patients had a median age of 34 years (range 8–44 years), AWD patients 24, 5 years (range 8–76), DOD patients 15 years (range 2–77).

Table 2.
Events and outcomes in children and adults. Summary of cases with a follow-up of at least 12 months with events and outcome, by age. na: not available, LR: local relapse, DR: distant relapse, NED: no evidence of disease, AWD: alive with disease, DOD: dead of the disease.
Considering only the 24 patients who had an event (local, distant or combined relapse), 2/24 (8%) were NED, 9/24 (37%) were AWD and 13/24 (54%) were DOD (for further detail, see Table 1).
In the DOD group, 6/16 (37%) MYOD1 mutations were associated with another concurrent molecular event (mutation or copy number variation) in contrast to the NED group in which just 2 out of 9 patients had a concurrent molecular event (22%). For the DOD group, in four cases the associated molecular event was a PIK3CA mutation (in one case with a further event being MDM2 copy number variation), in one an NRAS mutation and in one an MDM2 copy number variation. In 5/6 reports of concurrent molecular events, the patients were in the pediatric group.
10. Discussion
In this review, we highlight the importance of the MYOD1L122R mutation as a prognostic factor for patients with RMS. Our comprehensive analysis of the cases described in the literature confirms the aggressiveness of this specific subgroup of tumors and clarifies the clinical features of patients affected by MYOD1L122R mutated tumors. There is a lack of information regarding the events and in particular it is not clear if MYOD1L122R mutated tumors tend to relapse after initial response, or whether they present as primary refractory disease. Similar to the presence of the PAX::FOXO1 fusion, the presence of this genetic alteration may need to be considered as a factor in risk stratification. This reflection comes from the evidence of a striking difference in survival between MYOD1 wild-type (fusion negative) and MYOD1L122R mutated patients, irrespective of the risk group and age [24]. The poor prognosis associated with the presence of the MYOD1L122R mutation suggests that early identification soon after the diagnosis of these patients at higher risk could be important, particularly if treatment can be tailored accordingly. Although these findings are based on our analysis of cases reported in the literature, the evaluation of the outcome comes from a summary of reported case series that altogether represent a convenience cohort. This could generate potential bias due to non-random selection of samples, as already explained by authors from COG in the case of PAX::FOXO biomarker in RMS, and it explains the need to evaluate the role of MYOD1L122R prospectively in an unselected cohort [50].
Early detection of MYOD1L122R mutated tumors is facilitated by routine molecular profiling of newly diagnosed tumors, which is now available in some but not all countries. In addition, particular attention to histological features and immunohistochemistry markers is required to detect any possible suggestive constellation of features that could trigger suspicion of a MYOD1 L122R mutation and target a subpopulation for analysis of MYOD1 L122R mutation. This latter approach could be important for countries where access to molecular biology techniques is a challenge and there is a real need to identify the RMS sub-population most likely to have somatic mutation of MYOD1.
The early detection of these patients drives the question of the most adequate staging and treatment to propose once the mutation has been identified. We know that the prognosis seems to be poor when MYOD1 L122R mutation is present, but the analyzed reports lack details regarding the role of MYOD1 mutation as an independent risk factor, the invasiveness of the tumor (for instance, are the nodes more or less frequently involved when MYOD1 is mutated?), the administered treatment (especially concerning the quality of the local control, and details of radiotherapy) and the pattern of events (is it mostly relapse or are these tumors primary refractory; what is the pattern of relapse?). Better knowledge of these characteristics would shed light on which aspects of the treatment could be improved in this special subset of patients. These reflections ultimately relate to identifying the most adapted practical therapeutic approach when treating these patients within the currently ongoing EpSSG FaR-RMS trial (NCT04625907) in which MYOD1 is currently not used as prognostic factor in risk stratification.
A consensus of international working groups has recently agreed that molecular analyses of tumors, that include identification of MYOD1 mutations, should be performed in RMS clinical trials [51]. This will enable the detailed issues raised relating to age and sex predilection and clinical behavior to be comprehensively addressed. However, in light of the correlations with poor outcomes, Shern et al. suggested incorporating MYOD1L122R, in addition to mutations of TP53, into RMS risk stratification [24]. Additionally, a recent report by COG proposed that upstaging on this basis should lead to the intensification of treatment [52] and COG currently excludes cases with MYOD1L122R tumors from low-risk studies [24,52].
As treatment intensification may not be effective, new treatment strategies should also be sought. These may be derived from more comprehensive molecular knowledge of tumor biology driven by MYOD1L122R and the role of multiple mutations that are concomitant with MYOD1L122R. Together with drug screening and testing of patient-derived and other models representing the MYOD1L122R in RMS, this could open up new therapeutic approaches for this specific group of patients with poor prognosis. More must also be done to design promising innovative drugs and offer these patients the possibility to be included in clinical trials with them.
11. Conclusions
In conclusion, if we consider that the MYOD1 mutation has a similar adverse prognostic role to the presence of PAX3/7::FOXO1 fusion, which is prospectively assessed in every patient in the EpSSG FaR-RMS trial, MYOD1 status should be checked early in the course of the disease, to tailor treatment from the beginning, with the aim of improving the survival of these patients. Given the clinical features of the patients that most often have MYOD1 mutations, we propose to check for MYOD1 status in patients over the age of 1 year with a PAX fusion-negative Sp- or ScRMS localized in the head and neck or extremity site. Ideally, MYOD1 status should be checked in every pediatric patient with PAX fusion-negative histology, to avoid missing the less frequent cases that may have embryonal histology or are localized to other sites.
We propose to prospectively assess the clinical application of MYOD1L122R status in the FaR-RMS clinical trial as well as consider stratifying these patients based on adverse biology, as for fusion-positive patients, with careful attention to adequate local therapy. In addition, we are currently undertaking a detailed analysis of a cohort of MYOD1 mutated RMS tumors to help answer some of the detailed clinical and pathological questions raised in this review.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers15061644/s1, Figure S1: PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only [53].
Author Contributions
D.D.C.: Conceptualization; Data curation; Methodology; Writing—original draft; Writing—review. J.L.S.: Conceptualization; Data curation; Methodology; Writing—original draft. J.M.S.: Conceptualization; Supervision; Critical revision and approval of final version. G.B.: Conceptualization; Supervision; Critical revision and approval of final version. A.K.: Conceptualization; Supervision; Critical revision and approval of final version. R.A.: Conceptualization; Supervision; Critical revision and approval of final version. V.M.-C.: Conceptualization; Supervision; Critical revision and approval of final version. M.J.: Conceptualization; Supervision; Critical revision and approval of final version. R.D.F.: Conceptualization; Supervision; Critical revision and approval of final version. J.H.M.M.: Conceptualization; Supervision; Methodology; Writing—review and editing. J.C.: Conceptualization; Supervision; Methodology; Writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We are grateful to Anne-Sophie Defachelles, Susanne Gatz, Marie Karanian, Aisha Miah, Beat Schaefer, Angelica Zin and Lucia Tombolan who participated in the discussion and gave their contribution and ideas during the workshop on MYOD1 mutation in RMS, November 2021. We are grateful to Alice’s Arc Children’s Cancer Charity for supporting JS. JCC is supported by the Giant Pledge through the Royal Marsden Cancer Charity and this independent research is supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at the Royal Marsden NHS Foundation Trust and the Institute of Cancer Research, London. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Miller, R.W.; Young, J.L.; Novakovic, B. Childhood cancer. Cancer 1995, 75 (Suppl. 1), 395–405. [Google Scholar] [CrossRef]
- Bisogno, G.; De Salvo, G.L.; Bergeron, C.; Gallego Melcón, S.; Merks, J.H.; Kelsey, A.; Martelli, H.; Minard-Colin, V.; Orbach, D.; Glosli, H.; et al. Vinorelbine and continuous low-dose cyclophosphamide as maintenance chemotherapy in patients with high-risk rhabdomyosarcoma (RMS 2005): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2019, 20, 1566–1575. [Google Scholar] [CrossRef]
- Affinita, M.C.; Ferrari, A.; Chiaravalli, S.; Melchionda, F.; Quaglietta, L.; Casanova, M.; Zanetti, I.; Scarzello, G.; Di Pasquale, L.; Di Cataldo, A.; et al. Defining the impact of prognostic factors at the time of relapse for nonmetastatic rhabdomyosarcoma. Pediatr. Blood Cancer 2020, 67, e28674. [Google Scholar] [CrossRef]
- Chisholm, J.C.; Marandet, J.; Rey, A.; Scopinaro, M.; de Toledo, J.S.; Merks, J.H.M.; O’Meara, A.; Stevens, M.C.G.; Oberlin, O. Prognostic factors after relapse in nonmetastatic rhabdomyosarcoma: A nomogram to better define patients who can be salvaged with further therapy. J. Clin. Oncol. 2011, 29, 1319–1325. [Google Scholar] [CrossRef] [PubMed]
- Pappo, A.S.; Anderson, J.R.; Crist, W.M.; Wharam, M.D.; Breitfeld, P.P.; Hawkins, D.; Raney, R.B.; Womer, R.B.; Parham, D.M.; Qualman, S.J.; et al. Survival after Relapse in Children and Adolescents with Rhabdomyosarcoma: A Report from the Intergroup Rhabdomyosarcoma Study Group. J. Clin. Oncol. 1999, 17, 3487–3493. [Google Scholar] [CrossRef]
- Mazzoleni, S.; Bisogno, G.; Garaventa, A.; Cecchetto, G.; Ferrari, A.; Sotti, G.; Donfrancesco, A.; Madon, E.; Casula, L.; Carli, M.; et al. Outcomes and prognostic factors after recurrence in children and adolescents with nonmetastatic rhabdomyosarcoma. Cancer 2005, 104, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Minn, A.Y.; Lyden, E.R.; Anderson, J.R.; Million, L.; Arndt, C.A.; Brown, K.; Hawkins, D.S.; Donaldson, S.S. Early treatment failure in intermediate-risk rhabdomyosarcoma: Results from IRS-IV and D9803--a report from the Children’s Oncology Group. J. Clin. Oncol. 2010, 28, 4228–4232. [Google Scholar] [CrossRef] [PubMed]
- Vaarwerk, B.; Hol, M.L.F.; Schoot, R.A.; Breunis, W.B.; de Win, M.M.L.; Westerveld, H.; Fajardo, R.D.; Saeed, P.; van den Brekel, M.W.; Pieters, B.R.; et al. AMORE treatment as salvage treatment in children and young adults with relapsed head-neck rhabdomyosarcoma. Radiother. Oncol. 2019, 131, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Koscielniak, E.; Harms, D.; Henze, G.; Jürgens, H.; Gadner, H.; Herbst, M.; Klingebiel, T.; Schmidt, B.F.; Morgan, M.; Knietig, R.; et al. Results of treatment for soft tissue sarcoma in childhood and adolescence: A final report of the German Cooperative Soft Tissue Sarcoma Study CWS-86. J. Clin. Oncol. 1999, 17, 3706–3719. [Google Scholar] [CrossRef] [PubMed]
- Newton, W.A.; Gehan, E.A.; Webber, B.L.; Marsden, H.B.; van Unnik, A.J.; Hamoudi, A.B.; Tsokos, M.G.; Shimada, H.; Harms, D.; Schmidt, D. Classification of rhabdomyosarcomas and related sarcomas. Pathologic aspects and proposal for a new classification--an Intergroup Rhabdomyosarcoma Study. Cancer 1995, 76, 1073–1085. [Google Scholar] [CrossRef] [PubMed]
- Skapek, S.X.; Anderson, J.; Barr, F.G.; Bridge, J.A.; Gastier-Foster, J.M.; Parham, D.M.; Rudzinski, E.R.; Triche, T.; Hawkins, D.S. PAX-FOXO1 fusion status drives unfavorable outcome for children with rhabdomyosarcoma: A children’s oncology group report. Pediatr. Blood Cancer 2013, 60, 1411–1417. [Google Scholar] [CrossRef] [PubMed]
- Missiaglia, E.; Williamson, D.; Chisholm, J.; Wirapati, P.; Pierron, G.; Petel, F.; Concordet, J.-P.; Thway, K.; Oberlin, O.; Pritchard-Jones, K.; et al. PAX3/FOXO1 fusion gene status is the key prognostic molecular marker in rhabdomyosarcoma and significantly improves current risk stratification. J. Clin. Oncol. 2012, 30, 1670–1677. [Google Scholar] [CrossRef]
- Alaggio, R.; Zhang, L.; Sung, Y.-S.; Huang, S.-C.; Chen, C.-L.; Bisogno, G.; Zin, A.; Agaram, N.P.; LaQuaglia, M.P.; Wexler, L.H.; et al. A Molecular Study of Pediatric Spindle and Sclerosing Rhabdomyosarcoma: Identification of Novel and Recurrent VGLL2-related Fusions in Infantile Cases. Am. J. Surg. Pathol. 2016, 40, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Di Carlo, D.; Chargari, C.; Scoazec, J.-Y.; Cotteret, S.; Felix, A.; Moalla, S.; Temam, S.; Minard-Colin, V. PAX3-NCOA1 alveolar rhabdomyosarcoma of the tongue: A rare entity with challenging diagnosis and management. Pediatr. Blood Cancer 2021, 68, e29288. [Google Scholar] [CrossRef]
- Mosquera, J.M.; Sboner, A.; Zhang, L.; Kitabayashi, N.; Chen, C.-L.; Sung, Y.S.; Wexler, L.H.; LaQuaglia, M.P.; Edelman, M.; Sreekantaiah, C.; et al. Recurrent NCOA2 gene rearrangements in congenital/infantile spindle cell rhabdomyosarcoma. Genes Chromosomes Cancer 2013, 52, 538–550. [Google Scholar] [CrossRef]
- Chrisinger, J.S.A.; Wehrli, B.; Dickson, B.C.; Fasih, S.; Hirbe, A.C.; Shultz, D.B.; Zadeh, G.; Gupta, A.A.; Demicco, E.G. Epithelioid and spindle cell rhabdomyosarcoma with FUS-TFCP2 or EWSR1-TFCP2 fusion: Report of two cases. Virchows Arch. 2020, 477, 725–732. [Google Scholar] [CrossRef]
- Szuhai, K.; de Jong, D.; Leung, W.Y.; Fletcher, C.D.; Hogendoorn, P.C. Transactivating mutation of the MYOD1 gene is a frequent event in adult spindle cell rhabdomyosarcoma: MYOD1 mutation in adult spindle cell rhabdomyosarcoma. J. Pathol. 2014, 232, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Shern, J.F.; Selfe, J.; Izquierdo, E.; Patidar, R.; Chou, H.-C.; Song, Y.K.; Yohe, M.E.; Sindiri, S.; Wei, J.; Wen, X.; et al. Genomic Classification and Clinical Outcome in Rhabdomyosarcoma: A Report From an International Consortium. JCO 2021, 39, 2859–2871. [Google Scholar] [CrossRef] [PubMed]
- Cavazzana, A.O.; Schmidt, D.; Ninfo, V.; Harms, D.; Tollot, M.; Carli, M.; Treuner, J.; Betto, R.; Salviati, G. Spindle cell rhabdomyosarcoma. A prognostically favorable variant of rhabdomyosarcoma. Am. J. Surg. Pathol. 1992, 16, 229–235. [Google Scholar] [CrossRef]
- Folpe, A.L.; McKenney, J.K.; Bridge, J.A.; Weiss, S.W. Sclerosing rhabdomyosarcoma in adults: Report of four cases of a hyalinizing, matrix-rich variant of rhabdomyosarcoma that may be confused with osteosarcoma, chondrosarcoma, or angiosarcoma. Am. J. Surg. Pathol. 2002, 26, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Mentzel, T.; Katenkamp, D. Sclerosing, pseudovascular rhabdomyosarcoma in adults. Clinicopathological and immunohistochemical analysis of three cases. Virchows Arch. 2000, 436, 305–311. [Google Scholar] [CrossRef]
- Wang, Y.; Li, J.; Tian, Z.; Zhu, Y. Clinicopathologic features and molecular spectrum of spindle cell and sclerosing rhabdomyosarcomas in the head and neck region. Int. J. Clin. Exp. Pathol. 2018, 11, 3436. [Google Scholar]
- Jo, V.Y.; Fletcher, C.D.M. WHO classification of soft tissue tumours: An update based on the 2013 (4th) edition. Pathology 2014, 46, 95–104. [Google Scholar] [CrossRef]
- Choi, J.H.; Ro, J.Y. The 2020 WHO Classification of Tumors of Soft Tissue: Selected Changes and New Entities. Adv. Anat. Pathol. 2021, 28, 44–58. [Google Scholar] [CrossRef]
- Kohsaka, S.; Shukla, N.; Ameur, N.; Ito, T.; Ng, C.K.Y.; Wang, L.; Lim, D.; Marchetti, A.; Viale, A.; Pirun, M.; et al. A recurrent neomorphic mutation in MYOD1 defines a clinically aggressive subset of embryonal rhabdomyosarcoma associated with PI3K-AKT pathway mutations. Nat. Genet. 2014, 46, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.L.; Weintraub, H.; Lassar, A.B. Expression of a Single Transfected cDNA Converts Fibmblasts to Myoblasts. Cell 1987, 51, 987–1000. [Google Scholar] [CrossRef]
- Zammit, P.S. Function of the myogenic regulatory factors Myf5, MyoD, Myogenin and MRF4 in skeletal muscle, satellite cells and regenerative myogenesis. Semin. Cell Dev. Biol. 2017, 72, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Emerson, C.P. Skeletal myogenesis: Genetics and embryology to the fore. Curr. Opin. Genet. Dev. 1993, 3, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Hasty, P.; Bradley, A.; Morris, J.H.; Edmondson, D.G.; Venuti, J.M.; Olson, E.N.; Klein, W.H. Muscle deficiency and neonatal death in mice with a targeted mutation in the myogenin gene. Nature 1993, 364, 501–506. [Google Scholar] [CrossRef]
- Tajbakhsh, S.; Rocancourt, D.; Cossu, G.; Buckingham, M. Redefining the Genetic Hierarchies Controlling Skeletal Myogenesis: Pax-3 and Myf-5 Act Upstream of MyoD. Cell 1997, 89, 127–138. [Google Scholar] [CrossRef]
- Hausburg, M.A.; Doles, J.D.; Clement, S.L.; Cadwallader, A.B.; Hall, M.N.; Blackshear, P.J.; Lykke-Andersen, J.; Olwin, B.B. Post-transcriptional regulation of satellite cell quiescence by TTP-mediated mRNA decay. eLife 2015, 4, e03390. [Google Scholar] [CrossRef] [PubMed]
- Crist, C.G.; Montarras, D.; Buckingham, M. Muscle Satellite Cells Are Primed for Myogenesis but Maintain Quiescence with Sequestration of Myf5 mRNA Targeted by microRNA-31 in mRNP Granules. Cell Stem Cell 2012, 11, 118–126. [Google Scholar] [CrossRef]
- Rudnicki, M.A.; Braun, T.; Hinuma, S.; Jaenisch, R. Inactivation of MyoD in Mice Leads to Up-Regulation of the Myogenic HLH Gene Myf-5 and Results in Apparently Normal Muscle Development. Cell 1992, 71, 383–390. [Google Scholar] [CrossRef]
- Braun, T.; Rudnicki, M.A.; Arnold, H.-H.; Jaenisch, R. Targeted inactivation of the muscle regulatory gene Myf-5 results in abnormal rib development and perinatal death. Cell 1992, 71, 369–382. [Google Scholar] [CrossRef]
- Haldar, M.; Karan, G.; Watanabe, S.; Guenther, S.; Braun, T.; Capecchi, M.R. Response: Contributions of the Myf5-Independent Lineage to Myogenesis. Dev. Cell 2014, 31, 539–541. [Google Scholar] [CrossRef] [PubMed]
- Megeney, L.A.; Kablar, B.; Garrett, K.; Anderson, J.E.; Rudnicki, M.A. MyoD is required for myogenic stem cell function in adult skeletal muscle. Genes Dev. 1996, 10, 1173–1183. [Google Scholar] [CrossRef]
- Lassar, A.B.; Davis, R.L.; Wright, W.E.; Kadesch, T.; Murre, C.; Voronova, A.; Baltimore, D.; Weintraub, H. Functional activity of myogenic HLH proteins requires hetero-oligomerization with E12/E47-like proteins in vivo. Cell 1991, 66, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Yao, Z.; Sarkar, D.; Lawrence, M.; Sanchez, G.J.; Parker, M.H.; MacQuarrie, K.L.; Davison, J.; Morgan, M.T.; Ruzzo, W.L.; et al. Genome-wide MyoD Binding in Skeletal Muscle Cells: A Potential for Broad Cellular Reprogramming. Dev. Cell 2010, 18, 662–674. [Google Scholar] [CrossRef]
- Bergstrom, D.A.; Penn, B.H.; Strand, A.; Perry, R.L.S.; Rudnicki, M.A.; Tapscott, S.J. Promoter-Specific Regulation of MyoD Binding and Signal Transduction Cooperate to Pattern Gene Expression. Mol. Cell 2002, 9, 587–600. [Google Scholar] [CrossRef]
- Siles, L.; Sánchez-Tilló, E.; Lim, J.-W.; Darling, D.S.; Kroll, K.L.; Postigo, A. ZEB1 Imposes a Temporary Stage-Dependent Inhibition of Muscle Gene Expression and Differentiation via CtBP-Mediated Transcriptional Repression. Mol. Cell. Biol. 2013, 33, 1368–1382. [Google Scholar] [CrossRef]
- Van Antwerp, M.E.; Chen, D.G.; Chang, C.; Prochownik, E.V. A point mutation in the MyoD basic domain imparts c-Myc-like properties. Proc. Natl. Acad. Sci. USA 1992, 89, 9010–9014. [Google Scholar] [CrossRef]
- MacQuarrie, K.L.; Yao, Z.; Fong, A.P.; Diede, S.J.; Rudzinski, E.R.; Hawkins, D.S.; Tapscott, S.J. Comparison of Genome-Wide Binding of MyoD in Normal Human Myogenic Cells and Rhabdomyosarcomas Identifies Regional and Local Suppression of Promyogenic Transcription Factors. Mol. Cell. Biol. 2013, 33, 773–784. [Google Scholar] [CrossRef]
- Agaram, N.P.; Chen, C.-L.; Zhang, L.; LaQuaglia, M.P.; Wexler, L.; Antonescu, C.R. Recurrent MYOD1 mutations in pediatric and adult sclerosing and spindle cell rhabdomyosarcomas: Evidence for a common pathogenesis: MYOD1 Mutation in Rhabdomyosarcoma. Genes Chromosomes Cancer 2014, 53, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Rekhi, B.; Upadhyay, P.; Ramteke, M.P.; Dutt, A. MYOD1 (L122R) mutations are associated with spindle cell and sclerosing rhabdomyosarcomas with aggressive clinical outcomes. Mod. Pathol. 2016, 29, 1532–1540. [Google Scholar] [CrossRef]
- Owosho, A.A.; Chen, S.; Kashikar, S.; Zhang, L.; Chen, C.-L.; Wexler, L.H.; Estilo, C.L.; Huryn, J.M.; Antonescu, C.R. Clinical and molecular heterogeneity of head and neck spindle cell and sclerosing rhabdomyosarcoma. Oral Oncol. 2016, 58, e6–e11. [Google Scholar] [CrossRef] [PubMed]
- Agaram, N.P.; LaQuaglia, M.P.; Alaggio, R.; Zhang, L.; Fujisawa, Y.; Ladanyi, M.; Wexler, L.H.; Antonescu, C.R. MYOD1-mutant spindle cell and sclerosing rhabdomyosarcoma: An aggressive subtype irrespective of age. A reappraisal for molecular classification and risk stratification. Mod. Pathol. 2019, 32, 27–36. [Google Scholar] [CrossRef]
- Tsai, J.; ChangChien, Y.; Lee, J.; Kao, Y.; Li, W.; Liang, C.; Liao, I.; Chang, Y.; Wang, J.; Tsao, C.; et al. The expanding morphological and genetic spectrum of MYOD1-mutant spindle cell/sclerosing rhabdomyosarcomas: A clinicopathological and molecular comparison of mutated and non-mutated cases. Histopathology 2019, 74, 933–943. [Google Scholar] [CrossRef]
- Gorunova, L.; Bjerkehagen, B.; Micci, F.; Heim, S.; Panagopoulos, I. Cytogenetic and Molecular Study of an Adult Sclerosing Rhabdomyosarcoma of the Extremity: MYOD1-Mutation and Clonal Evolution. Cancer Genom. Proteom. 2020, 17, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Ting, M.A.; Reuther, J.; Chandramohan, R.; Voicu, H.; Gandhi, I.; Liu, M.; Cortes-Santiago, N.; Foster, J.H.; Hicks, J.; Nuchtern, J.; et al. Genomic analysis and preclinical xenograft model development identify potential therapeutic targets for MYOD1-mutant soft-tissue sarcoma of childhood. J. Pathol. 2021, 255, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, A.R.; Skapek, S.X.; Hawkins, D.S. The inconvenience of convenience cohorts: Rhabdomyosarcoma and the PAX-FOXO1 biomarker. Cancer Epidemiol. Biomark. Prev. 2012, 21, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Hettmer, S.; Linardic, C.M.; Kelsey, A.; Rudzinski, E.R.; Vokuhl, C.; Selfe, J.; Ruhen, O.; Shern, J.F.; Khan, J.; Kovach, A.R.; et al. Molecular testing of rhabdomyosarcoma in clinical trials to improve risk stratification and outcome: A consensus view from European paediatric Soft tissue sarcoma Study Group, Children’s Oncology Group and Cooperative Weichteilsarkom-Studiengruppe. Eur. J. Cancer 2022, 172, 367–386. [Google Scholar] [CrossRef] [PubMed]
- Haduong, J.H.; Heske, C.M.; Allen-Rhoades, W.; Xue, W.; Teot, L.A.; Rodeberg, D.A.; Donaldson, S.S.; Weiss, A.; Hawkins, D.S.; Venkatramani, R. An update on rhabdomyosarcoma risk stratification and the rationale for current and future Children’s Oncology Group clinical trials. Pediatr. Blood Cancer 2022, 69, e29511. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; Chou, R.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).