Single-Stage versus Multi-Stage Intramedullary Nailing for Multiple Synchronous Long Bone Impending and Pathologic Fractures in Metastatic Bone Disease and Multiple Myeloma
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
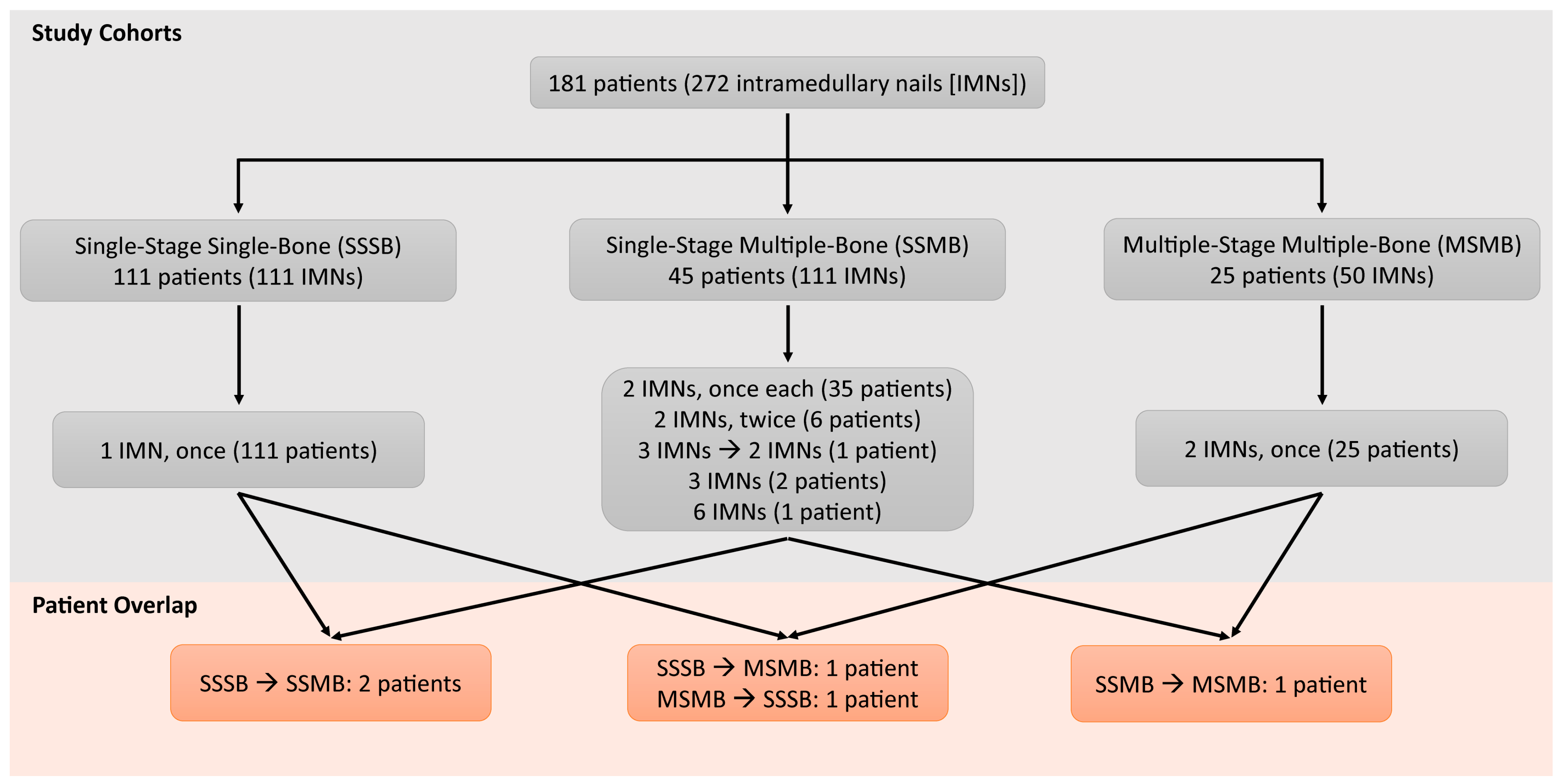
2.2. Group Stratification
2.3. Preoperative Optimization
2.4. Primary Demographics
2.5. Outcome Variables
2.6. Statistical Analysis
3. Results
3.1. Perioperative Outcomes
3.2. Postoperative Complications
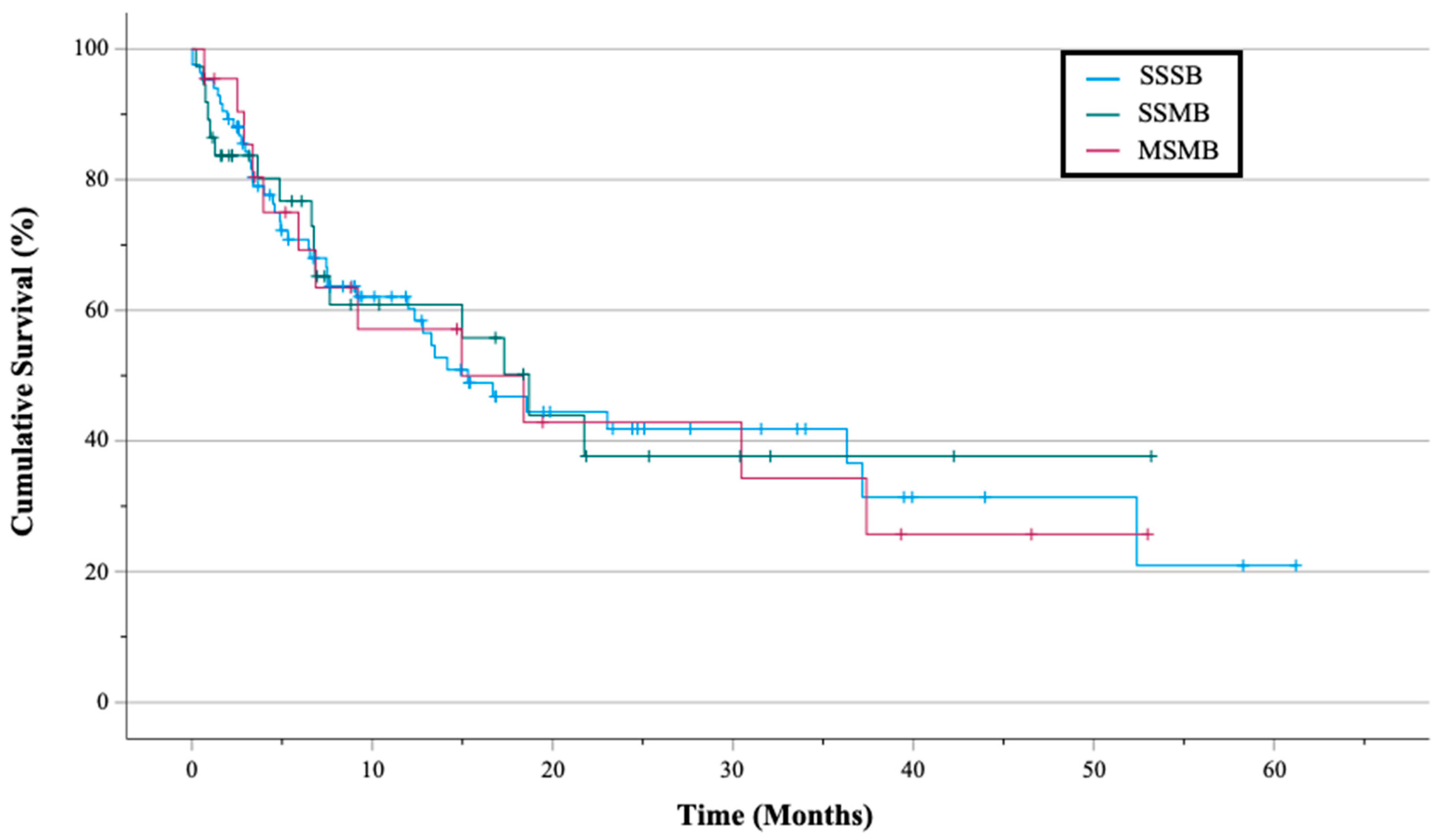
3.3. Survivorship and In-Hospital Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ma, K.L.S.; Kohles, J. Economic burden of metastatic bone disease in the U.S. Cancer 2007, 109, 2334–2342. [Google Scholar] [CrossRef]
- Biermann, J.S.; Holt, G.E.; Lewis, V.O.; Schwartz, H.S.; Yaszemski, M.J. Metastatic bone disease: Diagnosis, evaluation, and treatment. J. Bone Jt. Surg. 2009, 91, 1518–1530. [Google Scholar]
- Arneson, T.J.; Li, S.; Peng, Y.; Weinhandl, E.D.; Blaes, A.; Cetin, K.; Chia, V.M.; Stryker, S.; Pinzone, J.J.; Acquavella, J. Estimated number of prevalent cases of metastatic bone disease in the US adult population. Clin. Epidemiol. 2012, 4, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Harvey, N.; Ahlmann, E.R.; Allison, D.C.; Wang, L.; Menendez, L.R. Endoprostheses Last Longer Than Intramedullary Devices in Proximal Femur Metastases. Clin. Orthop. Relat. Res. 2012, 470, 684–691. [Google Scholar] [CrossRef]
- Piccioli, A.; Rossi, B.; Scaramuzzo, L.; Spinelli, M.S.; Yang, Z.; Maccauro, G. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury 2014, 45, 412–417. [Google Scholar] [CrossRef]
- Nooh, A.; Goulding, K.; Isler, M.H.; Mottard, S.; Arteau, A.; Dion, N.; Turcotte, R. Early Improvement in Pain and Functional Outcome but Not Quality of Life After Surgery for Metastatic Long Bone Disease. Clin. Orthop. Relat. Res. 2018, 476, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Bindels, B.J.J.; Thio, Q.C.B.S.; Raskin, K.A.; Ferrone, M.L.; Calderón, S.A.L.; Schwab, J.H. Thirty-day Postoperative Complications After Surgery For Metastatic Long Bone Disease Are Associated With Higher Mortality at 1 Year. Clin. Orthop. Relat. Res. 2020, 478, 306–318. [Google Scholar] [CrossRef] [PubMed]
- Cappellari, A.; Trovarelli, G.; Crimì, A.; Pala, E.; Angelini, A.; Berizzi, A.; Ruggieri, P. New concepts in the surgical treatment of actual and impending pathological fractures in metastatic disease. Injury 2020. [Google Scholar] [CrossRef]
- Ward, W.G.; Holsenbeck, S.; Dorey, F.J.; Spang, J.; Howe, D. Metastatic Disease of the Femur: Surgical Treatment. Clin. Orthop. Relat. Res. 2003, 415, S230–S244. [Google Scholar] [CrossRef] [PubMed]
- Ristevski, B.; Jenkinson, R.J.; Stephen, D.J.G.; Finkelstein, J.; Schemitsch, E.H.; McKee, M.D.; Kreder, H.J. Mortality and complications following stabilization of femoral metastatic lesions: A population-based study of regional variation and outcome. Can. J. Surg. 2009, 52, 302–308. [Google Scholar]
- Arvinius, C.; Parra, J.L.C.; Mateo, L.S.; Maroto, R.G.; Borrego, A.F.; Stern, L.L.-D. Benefits of early intramedullary nailing in femoral metastases. Int. Orthop. 2014, 38, 129–132. [Google Scholar] [CrossRef] [PubMed]
- El Abiad, J.M.; Raad, M.; Puvanesarajah, V.; Rao, S.S.; Morris, C.D.; Levin, A.S. Prophylactic Versus Postfracture Stabilization for Metastatic Lesions of the Long Bones. J. Am. Acad. Orthop. Surg. 2019, 27, e709–e716. [Google Scholar] [CrossRef]
- Barwood, S.A.; Wilson, J.L.; Molnar, R.R.; Choong, P.F.M. The incidence of acute cardiorespiratory and vascular dysfunction following intramedullary nail fixation of femoral metastasis. Acta Orthop. 2000, 71, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Choong, P.F. Cardiopulmonary Complications of Intramedullary Fixation of Long Bone Metastases. Clin. Orthop. Relat. Res. 2003, 415, S245–S253. [Google Scholar] [CrossRef]
- Roth, S.E.; Rebello, M.M.; Kreder, H.; Whyne, C.M. Pressurization of the Metastatic Femur During Prophylactic Intramedullary Nail Fixation. J. Trauma Inj. Infect. Crit. Care 2004, 57, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Sarahrudi, K.; Greitbauer, M.; Platzer, P.; Hausmann, J.-T.; Heinz, T.; Vécsei, V. Surgical Treatment of Metastatic Fractures of the Femur: A Retrospective Analysis of 142 Patients. J. Trauma Inj. Infect. Crit. Care 2009, 66, 1158–1163. [Google Scholar] [CrossRef]
- Shallop, B.; Starks, A.; Greenbaum, S.; Geller, D.S.; Lee, A.; Ready, J.; Merli, G.; Maltenfort, M.; Abraham, J.A. Thromboembolism After Intramedullary Nailing for Metastatic Bone Lesions. J. Bone Jt. Surg. 2015, 97, 1503–1511. [Google Scholar] [CrossRef]
- Tanaka, T.; Imanishi, J.; Charoenlap, C.; Choong, P.F.M. Intramedullary nailing has sufficient durability for metastatic femoral fractures. World J. Surg. Oncol. 2016, 14, 1–6. [Google Scholar] [CrossRef]
- Errani, C.; Mavrogenis, A.F.; Cevolani, L.; Spinelli, S.; Piccioli, A.; Maccauro, G.; Baldini, N.; Donati, D. Treatment for long bone metastases based on a systematic literature review. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 205–211. [Google Scholar] [CrossRef]
- Kotian, R.N.; Puvanesarajah, V.; Rao, S.; El Abiad, J.M.; Morris, C.D.; Levin, A.S. Predictors of survival after intramedullary nail fixation of completed or impending pathologic femur fractures from metastatic disease. Surg. Oncol. 2018, 27, 462–467. [Google Scholar] [CrossRef]
- Willeumier, J.J.; Kaynak, M.; van der Zwaal, P.; Meylaerts, S.A.G.; Mathijssen, N.M.C.; Jutte, P.C.; Tsagozis, P.; Wedin, R.; van de Sande, M.A.J.; Fiocco, M.; et al. What Factors Are Associated With Implant Breakage and Revision After Intramedullary Nailing for Femoral Metastases? Clin. Orthop. Relat. Res. 2018, 476, 1823–1833. [Google Scholar] [CrossRef] [PubMed]
- Janssen, S.J.; Van Der Heijden, A.S.; Van Dijke, M.; Ready, J.E.; Raskin, K.A.; Ferrone, M.L.; Hornicek, F.J.; Schwab, J.H. 2015 Marshall Urist Young Investigator Award: Prognostication in Patients With Long Bone Metastases: Does a Boosting Algorithm Improve Survival Estimates? Clin. Orthop. Relat. Res. 2015, 473, 3112–3121. [Google Scholar] [CrossRef]
- Kerr, P.; Jackson, M.; Atkins, R. Cardiac arrest during intramedullary nailing for femoral metastases. J. Bone Jt. Surg. 1993, 75, 972–973. [Google Scholar] [CrossRef]
- Charnley, G.; Coleman, N.P.; Hashemi-Nejad, A. Cardiac arrest during nailing. J. Bone Jt. Surg. 1994, 76, 506. [Google Scholar] [CrossRef]
- Roumen, R.M.; Lako, S.J.; Schoots, F.J. Acute lung damage after bilateral insertion of femoral intramedullary interlocking nails for metastatic bone disease. Br. J. Surg. 1995, 161, 451–453. [Google Scholar]
- Peter, R.E.; Schopfer, A.; Le Coultre, B.; Hoffmeyer, P. Fat Embolism and Death During Prophylactic Osteosynthesis of a Metastatic Femur Using an Unreamed Femoral Nail. J. Orthop. Trauma 1997, 11, 233–234. [Google Scholar] [CrossRef]
- Kontakis, G.M.; Tossounidis, T.; Weiss, K.; Pape, H.-C.; Giannoudis, P.V. Fat embolism: Special situations Bilateral femoral fractures and pathologic femoral fractures. Injury 2006, 37, S19–S24. [Google Scholar] [CrossRef] [PubMed]
- Moon, B.; Lin, P.; Satcher, R.; Lewis, V. Simultaneous Nailing of Skeletal Metastases: Is the Mortality Really that High? Clin. Orthop. Relat. Res. 2011, 469, 2367–2370. [Google Scholar] [CrossRef] [PubMed]
- Raasck, K.; Al Farii, H. The Effects of Simultaneous Versus Staged Bilateral Femoral Intramedullary Nailing for Metastatic Disease on Survival Time and Perioperative Complications: A Systematic Review. J. Orthop. Oncol. 2018, 4, 2. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Bastawrous, S.S.; Bunola, J.A.; Macdonald, D.A.; Smith, R.M. Unreamed intramedullary nailing for pathological femoral fractures: Good results in 30 cases. Acta Orthop. 1999, 70, 29–32. [Google Scholar] [CrossRef]
- Cole, A.; Hill, G.; Theologis, T.; Gibbons, C.; Willett, K. Femoral nailing for metastatic disease of the femur: A comparison of reamed and unreamed femoral nailing. Injury 2000, 31, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Mirels, H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin. Orthop. Relat. Res. 1989, 249, 256–264. [Google Scholar] [CrossRef]
- Hage, W.D.; Aboulafia, A.J.; Aboulafia, D.M. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop. Clin. N. Am. 2000, 31, 515–528. [Google Scholar] [CrossRef] [PubMed]
- Weber, K.L.; Lewis, V.O.; Randall, R.L.; Lee, A.K.; Springfield, D. An approach to the management of the patient with metastatic bone disease. Instr. Course Lect. 2004, 53, 663–676. [Google Scholar]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Rudloff, M.I.; Smith, W.R. Intramedullary Nailing of the Femur: Current Concepts Concerning Reaming. J. Orthop. Trauma 2009, 23, S12–S17. [Google Scholar] [CrossRef]
- Heineman, D.J.; Poolman, R.W.; Nork, S.E.; Ponsen, K.-J.; Bhandari, M. Plate fixation or intramedullary fixation of humeral shaft fractures. Acta Orthop. 2010, 81, 216–223. [Google Scholar] [CrossRef]
- Yoon, R.; Donegan, D.J.; Liporace, F.A. Reducing Subtrochanteric Femur Fractures. J. Orthop. Trauma 2015, 29, S28–S33. [Google Scholar] [CrossRef]
- Moura, D.L.; Alves, F.F.; Fonseca, R.; Freitas, J.; Casanova, J. Tratamento de fraturas patológicas tumorais diafisárias do úmero com haste intramedular rígida bloqueada estática—Experiência de 22 anos. Rev. Bras. Ortop. 2019, 54, 149–155. [Google Scholar] [CrossRef]
- Flagstad, I.R.; Tatman, L.M.; Heare, A.; Parikh, H.R.M.; Albersheim, M.; Atchison, J.B.; Breslin, M.M.; Davis, P.B.; Feinstein, S.; Hak, D.J.; et al. Single-Stage versus 2-Stage Bilateral Intramedullary Nail Fixation in Patients with Bilateral Femur Fractures: A Multicenter Retrospective Review. J. Orthop. Trauma 2021, 35, 499–504. [Google Scholar] [CrossRef]
| Total Patients (N = 181) IMN (N = 272) | SSSB Patients (N = 111) IMNs (N = 111) | SSMB Patients (N = 45) IMNs (N = 111) | MSMB Patients (N = 25) IMNs (N = 50) | p-Value | |
|---|---|---|---|---|---|
| Age (years) ‡ | 66.3 ± 12.1 [32–96] | 66.9 ± 12.4 [38–93] | 64.9 ± 12.3 [32–93] | 66.4 ± 10.6 [42–96] | 0.661 |
| Sex † | 0.320 | ||||
| Male | 100 (55.2%) | 66 (59.5%) | 21 (46.7%) | 13 (52.0%) | |
| Female | 81 (44.8%) | 45 (40.5%) | 24 (53.3%) | 12 (48.0%) | |
| BMI (kg/m2) ‡ | 27.1 ± 6.3 | 27.8 ± 7.1 | 26.4 ± 5.4 | 25.4 ± 4.31 | 0.160 |
| Fracture Type † | <0.001 | ||||
| Impending | 172 (63.2%) | 55 (49.6%) b,c | 76 (68.5%) a | 41 (82.0%) a | |
| Pathologic | 100 (36.8%) | 56 (50.4%) b,c | 35 (31.5%) a | 9 (18.0%) a | |
| Metastasis Location † | <0.001 | ||||
| Femur | 177 (65.1%) | 76 (68.7%) b,c | 55 (49.6%) a,c | 46 (92.0%) a,b | |
| Humerus | 79 (29.0%) | 32 (28.8%) c | 44 (39.6%) c | 3 (6.0%) a,b | |
| Tibia | 6 (2.2%) | 1 (0.9%) | 4 (3.6%) | 1 (2.0%) | |
| Fibula | 2 (0.7%) | 2 (1.8%) | 0 (0.0%) | 0 (0.0%) | |
| Radius | 6 (2.2%) | 0 (0.0%) b | 6 (5.4%) a | 0 (0.0%) | |
| Ulna | 2 (0.7%) | 0 (0.0%) | 2 (1.8%) | 0 (0.0%) | |
| Primary Diagnosis † | 0.497 | ||||
| Multiple Myeloma | 84 (46.4%) | 47 (42.3%) | 24 (53.3%) | 13 (52.0%) | |
| Breast | 26 (14.3%) | 13 (11.7%) | 10 (22.2%) | 3 (12.0%) | |
| Prostate | 22 (12.2%) | 14 (12.6%) | 4 (8.9%) | 4 (16.0%) | |
| Lung | 13 (7.2%) | 9 (8.1%) | 1 (2.2%) | 3 (12.0%) | |
| Renal | 10 (5.5%) | 8 (7.2%) | 2 (4.4%) | 0 (0.0%) | |
| Colon | 4 (2.2%) | 4 (3.6%) | 0 (0.0%) | 0 (0.0%) | |
| Lymphoma | 3 (1.7%) | 3 (2.7%) | 0 (0.0%) | 0 (0.0%) | |
| Hepatocellular | 3 (1.7%) | 1 (0.9%) | 2 (4.4%) | 0 (0.0%) | |
| Other | 16 (8.8%) | 12 (10.8%) | 2 (4.4%) | 2 (8.0%) |
| IMN Combination | SSMB Patients (N = 45) * | MSMB Patients (N = 25) |
|---|---|---|
| Femur and Humerus | 32 | 3 |
| Bilateral Femur | 7 | 21 |
| Bilateral Humerus | 3 | 0 |
| Femur and Tibia | 3 | 1 |
| Femur and Radius | 2 | 0 |
| Femur, Humerus, and Tibia | 1 | 0 |
| Femur, Humerus, and Radius | 1 | 0 |
| Humerus and Radius | 1 | 0 |
| Bilateral Humerus and Femur | 1 | 0 |
| Femur, Humerus, Bilateral Radius, and Bilateral Ulna | 1 | 0 |
| Total surgical/anesthesia settings | 52 * | 50 |
| Total nails placed | 111 * | 50 |
| SSSB Patients (N = 111) | SSMB Patients (N = 45) | MSMB Patients (N = 25) | p-Value | |
|---|---|---|---|---|
| EBL (mL) ‡ | 219 ± 134 b,c | 419 ± 197 a | 467 ± 238 a | <0.001 |
| PRBC (units) ‡ | 0.4 ± 0.9 b | 1.2 ± 1.3 a | 0.8 ± 1.3 | <0.001 |
| Length of Stay (days) ‡ | 8.5 ± 7.7 c | 11.7 ± 7.6 c | 24.3 ± 14.2 a,b | <0.001 |
| Survival (months) ‡ | 8.1 ± 8.6 | 7.1 ± 7.2 | 11.4 ± 11.8 | 0.424 |
| Adjuvant Therapy (days) ‡ | 25.5 ± 20.3 | 26.6 ± 23.1 | 27.4 ± 12.1 | 0.933 |
| Initiation of Rehabilitation (days) ‡ | 1.8 ± 1.6 c | 2.0 ± 1.6 c | 3.4 ± 2.5 a,b | 0.002 |
| Medical Complications † | 12 (10.8%) b,c | 14 (31.1%) a | 9 (36.0%) a | <0.001 |
| Surgical Complications † | 8 (7.2%) | 2 (4.4%) | 0 (0.0%) | 0.408 |
| Total Complications †,* | 20 (18.0%) b,c | 15 (33.3%) a | 9 (36.0%) a | 0.038 |
| Death † | 5 (4.5%) | 4 (8.9%) | 1 (4.0%) | 0.524 |
| Sex | Age | Group | Location | Primary Tumor | Complication | In-Hospital Mortality |
|---|---|---|---|---|---|---|
| Medical Complications a | ||||||
| Female | 46 | SSSB | Femur | Breast | Deep vein thrombosis and pulmonary embolism | |
| Male | 68 | SSSB | Femur | Multiple myeloma | Atrial fibrillation | |
| Female | 55 | SSSB | Humerus | Breast | Septic shock from urinary tract infection | 44 days postoperatively |
| Male | 85 | SSSB | Femur | Prostate | Urinary tract infection | |
| Male | 80 | SSSB | Femur | Colon | Urinary tract infection | |
| Male | 49 | SSSB | Femur | Pleomorphic sarcoma | Progression of existing deep vein thrombosis | |
| Female | 68 | SSSB | Femur | Multiple myeloma | Urinary tract infection | |
| Male | 67 | SSSB | Femur | Lung | Pulmonary embolism | |
| Female | 51 | SSSB | Femur | Breast | Intraoperative ST-elevation myocardial infarction | 8 h postoperatively * |
| Female | 57 | SSSB | Femur | Leiomyosarcoma | Pulmonary embolism | 1 day postoperatively |
| Male | 83 | SSSB | Femur | Renal | Intra-pelvic bleed requiring embolization | 17 days postoperatively due to respiratory failure |
| Male | 60 | SSSB | Femur | Prostate | Sepsis from urinary tract infection, cerebrovascular accident (CVA) | 79 days postoperatively due to CVA |
| Male | 71 | SSMB | Femur; Humerus | Multiple myeloma | Pneumonia requiring intubation | |
| Male | 81 | SSMB | Femur; BL Humerus | Prostate | Disseminated intravascular coagulation | |
| Female | 66 | SSMB | Femur; Humerus; BL Ulna; BL Radius | Multiple myeloma | Clostridium difficile infection | |
| Female | 60 | SSMB | Femur; Humerus | Multiple myeloma | Cervical spinal instability leading to cord compression with quadriparesis, requiring urgent neurosurgical decompression and fixation | |
| Female | 38 | SSMB | Femur; Humerus | Breast | Pulmonary embolism | |
| Female | 71 | SSMB | Femur; Humerus | Multiple myeloma | Pneumonia | |
| Male | 65 | SSMB | Femur; Humerus | Multiple myeloma | Disseminated intravascular coagulation | 7 days postoperatively |
| Male | 72 | SSMB | Femur; Radius | Multiple myeloma | Urinary tract infection | |
| Male | 68 | SSMB | Femur; Humerus | Liver | Sepsis from urinary tract infection, gastrointestinal (GI) bleed | 30 days postoperatively due to GI bleed |
| Male | 83 | SSMB | Femur; Humerus | Multiple myeloma | Multiorgan failure from progression of disease | 20 days postoperatively |
| Female | 52 | SSMB | Humerus; radius | Multiple myeloma | Multiorgan failure from progression of disease | 23 days postoperatively |
| Female | 64 | SSMB | BL Femur | Breast | Hypotension | |
| Female | 64 | SSMB | Femur; Tibia | Breast | Urinary tract infection | |
| Female † | 57 | SSMB | Femur; Humerus | Breast | Hypotension and bradycardia | |
| Female | 74 | MSMB | BL Femur | Breast | Bilateral pleural effusion | |
| Female | 52 | MSMB | Femur; Tibia | Thyroid | Thyroid storm | |
| Female | 78 | MSMB | BL Femur | Multiple myeloma | Hypotension | |
| Female | 74 | MSMB | BL Femur | Multiple myeloma | Respiratory distress | |
| Female | 68 | MSMB | BL Femur | Lung | Pulmonary embolism, multiorgan failure due progression of disease | 22 days postoperatively due to progression of disease |
| Male | 57 | MSMB | BL Femur | Multiple myeloma | Pneumonia | |
| Male | 70 | MSMB | BL Femur | Prostate | Urinary tract obstruction and infection | |
| Female | 56 | MSMB | BL Femur | Multiple myeloma | Acute kidney injury | |
| Male | 60 | MSMB | BL Femur | Lung | Urinary tract infection | |
| Surgical Complications b | ||||||
| Female | 77 | SSSB | Humerus | Breast | Proximal locking screw back-out, not needing further surgery (asymptomatic) | |
| Male | 70 | SSSB | Femur | Multiple myeloma | Progression of bisphosphonate induced subtrochanteric fracture; treated conservatively with vitamin D and calcium healed uneventfully at one year | |
| Female | 64 | SSSB | Humerus | Multiple myeloma | Intraoperative distal humerus periprosthetic fracture; requiring additional plating | |
| Male | 62 | SSSB | Humerus | Renal | Cement extrusion in the joint and the fracture site acting as large loose body requiring immediate arthrotomy and removal | |
| Male | 57 | SSSB | Humerus | Multiple myeloma | Painful locking screw back-out, requiring removal at 2 years | |
| Male | 70 | SSSB | Femur | Colon | Failed hardware and fracture non-union due to progression of disease requiring revision nailing with a distal plate combo and cementation at 2 years | |
| Male | 57 | SSSB | Humerus | Multiple myeloma | Nondisplaced distal humerus periprosthetic fracture after 10 weeks; treated conservatively with radiation and splint | |
| Male | 74 | SSSB | Femur | Multiple myeloma | Failed hardware with progression of fracture and disease; refused further treatment | |
| Female | 44 | SSMB | Femur; Humerus | Breast | Transient radial nerve palsy treated conservatively, recovered | |
| Female † | 57 | SSMB | Femur; Humerus | Breast | Cement extrusion in the adjacent joint requiring immediate arthrotomy and removal | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maheshwari, A.V.; Kobryn, A.; Alam, J.S.; Tretiakov, M. Single-Stage versus Multi-Stage Intramedullary Nailing for Multiple Synchronous Long Bone Impending and Pathologic Fractures in Metastatic Bone Disease and Multiple Myeloma. Cancers 2023, 15, 1227. https://doi.org/10.3390/cancers15041227
Maheshwari AV, Kobryn A, Alam JS, Tretiakov M. Single-Stage versus Multi-Stage Intramedullary Nailing for Multiple Synchronous Long Bone Impending and Pathologic Fractures in Metastatic Bone Disease and Multiple Myeloma. Cancers. 2023; 15(4):1227. https://doi.org/10.3390/cancers15041227
Chicago/Turabian StyleMaheshwari, Aditya V., Andriy Kobryn, Juhayer S. Alam, and Mikhail Tretiakov. 2023. "Single-Stage versus Multi-Stage Intramedullary Nailing for Multiple Synchronous Long Bone Impending and Pathologic Fractures in Metastatic Bone Disease and Multiple Myeloma" Cancers 15, no. 4: 1227. https://doi.org/10.3390/cancers15041227
APA StyleMaheshwari, A. V., Kobryn, A., Alam, J. S., & Tretiakov, M. (2023). Single-Stage versus Multi-Stage Intramedullary Nailing for Multiple Synchronous Long Bone Impending and Pathologic Fractures in Metastatic Bone Disease and Multiple Myeloma. Cancers, 15(4), 1227. https://doi.org/10.3390/cancers15041227





