Outcomes of Robot-Assisted Surgery in Rectal Cancer Compared with Open and Laparoscopic Surgery
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Eligibility Criteria
2.3. Study Selection and Data Extraction
2.4. Definition of Extracted Data
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
3.1. Literature Search and Study Characteristics
3.2. Risk of Bias Assessment
3.3. Quantitative Analysis
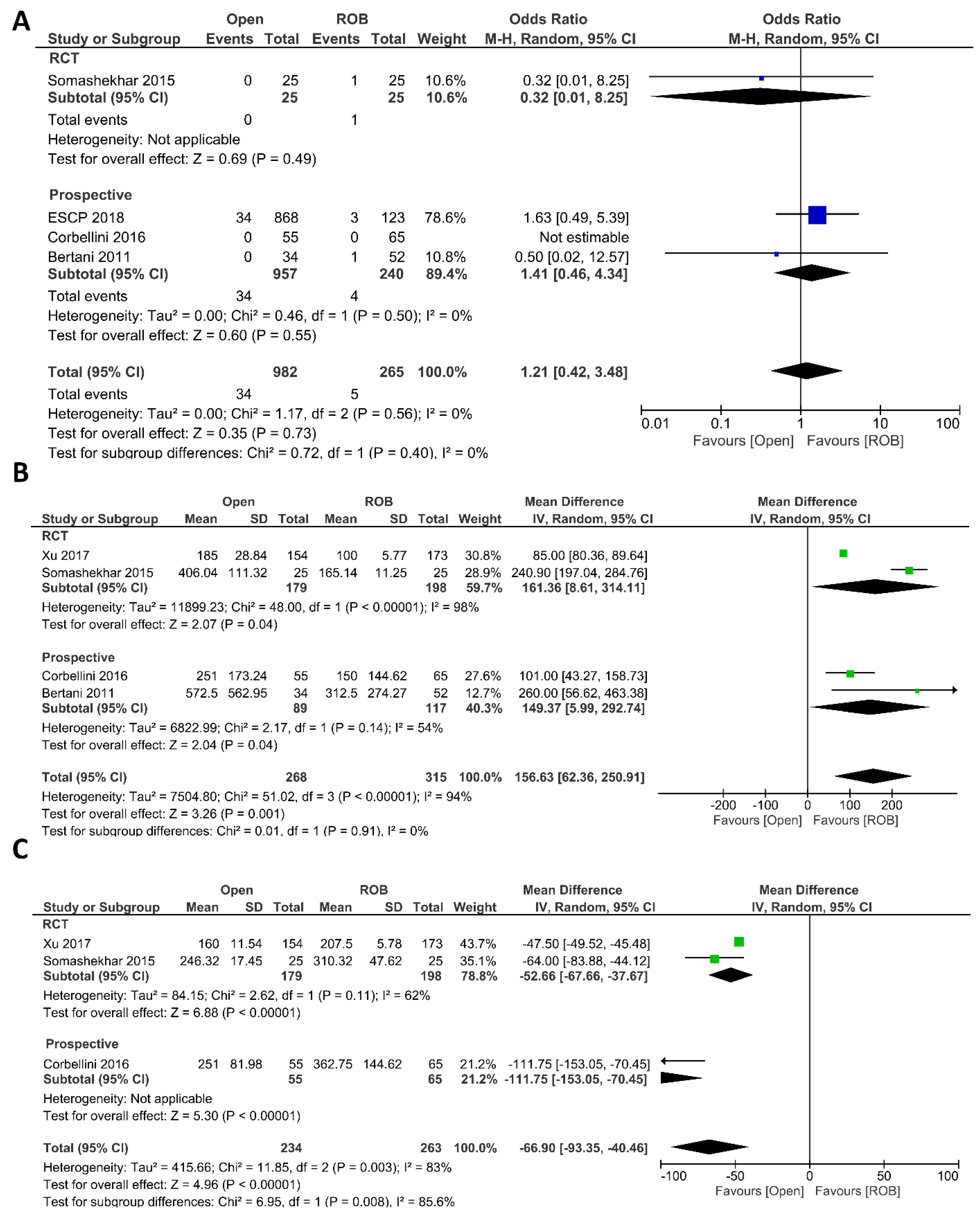
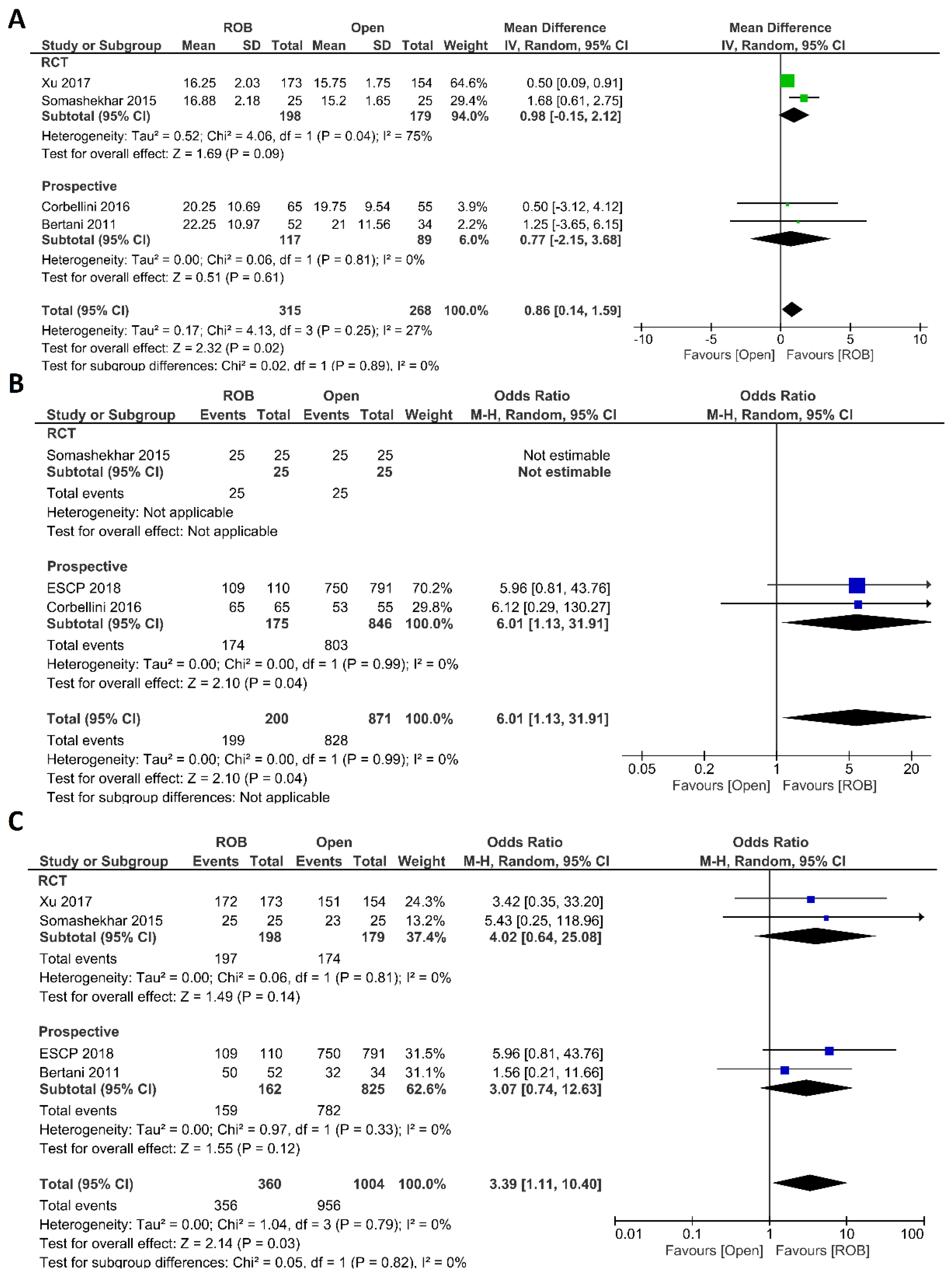
3.3.1. Meta-Analysis A: Robotic vs. Open Rectal Resection
Intraoperative Outcomes
Postoperative Outcomes
Histological Outcomes
Mortality and Survival Outcomes
Operative Costs
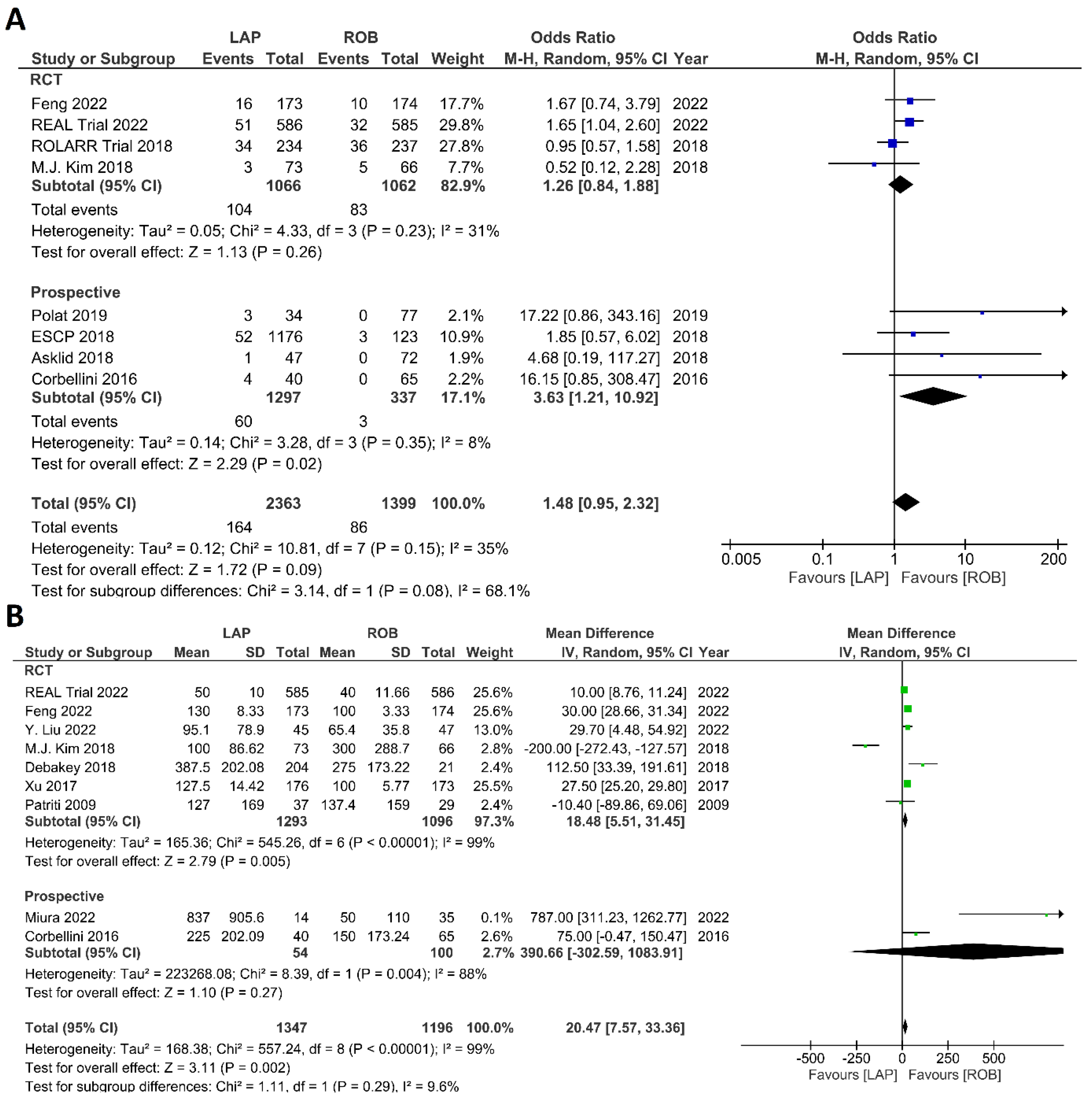
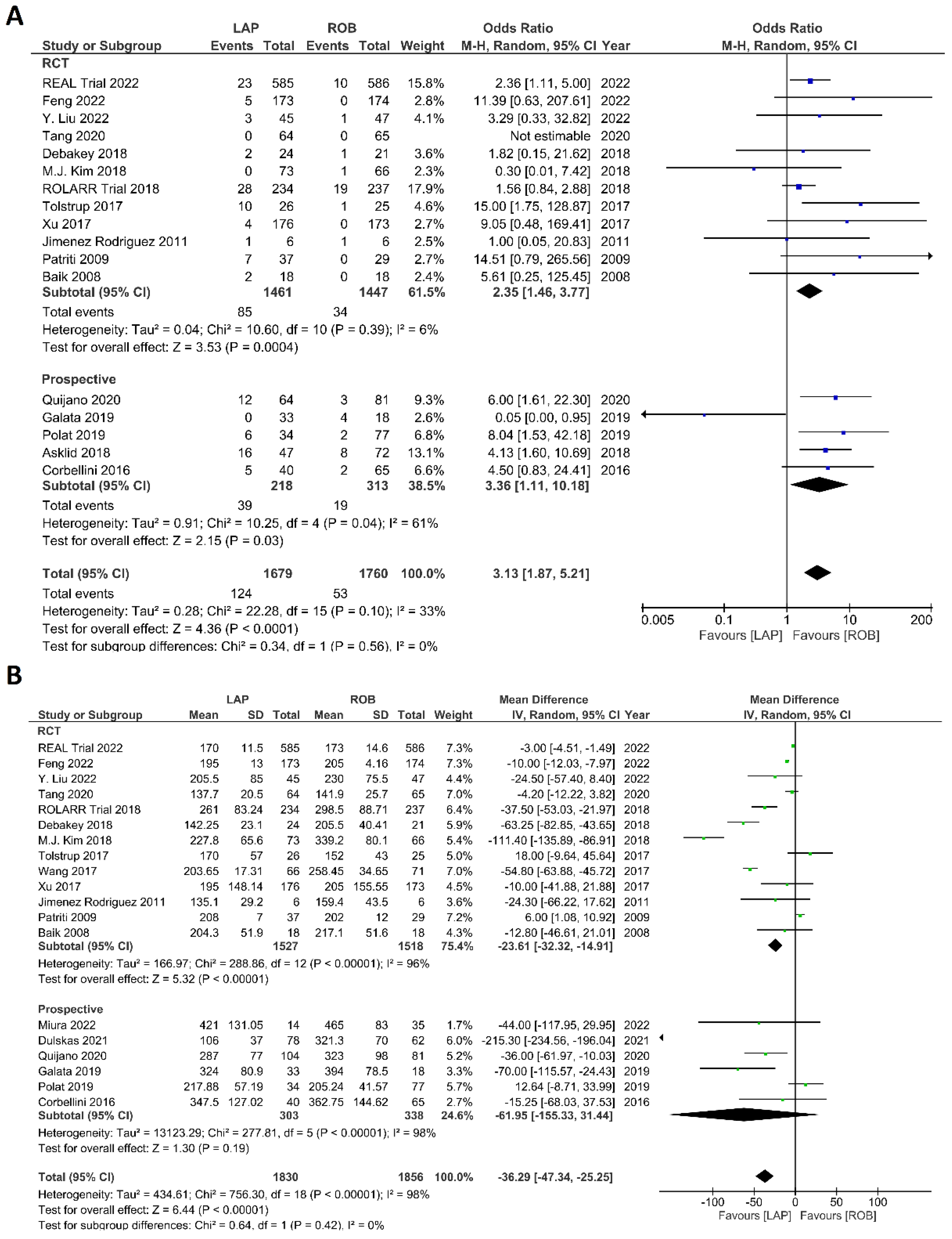
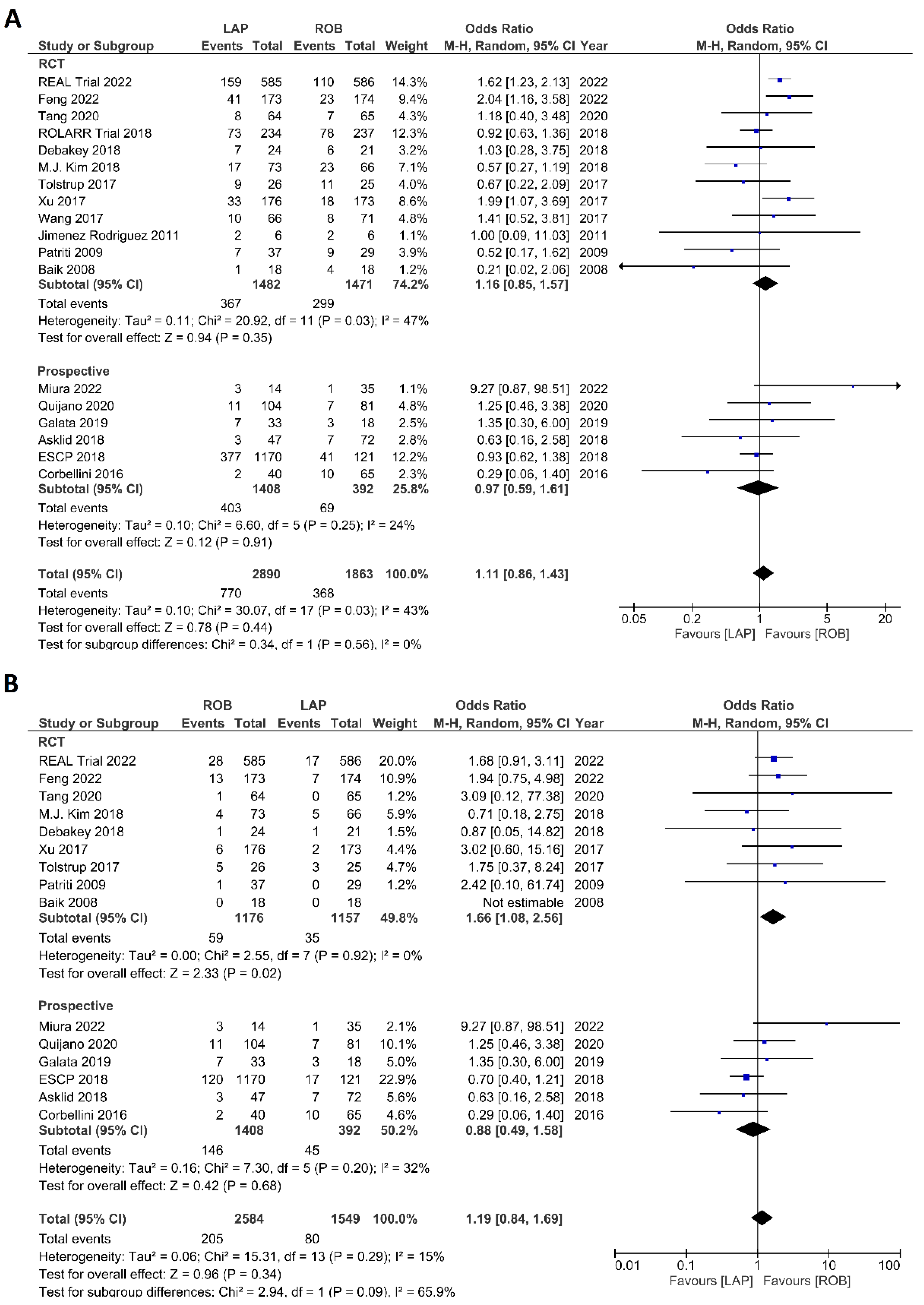
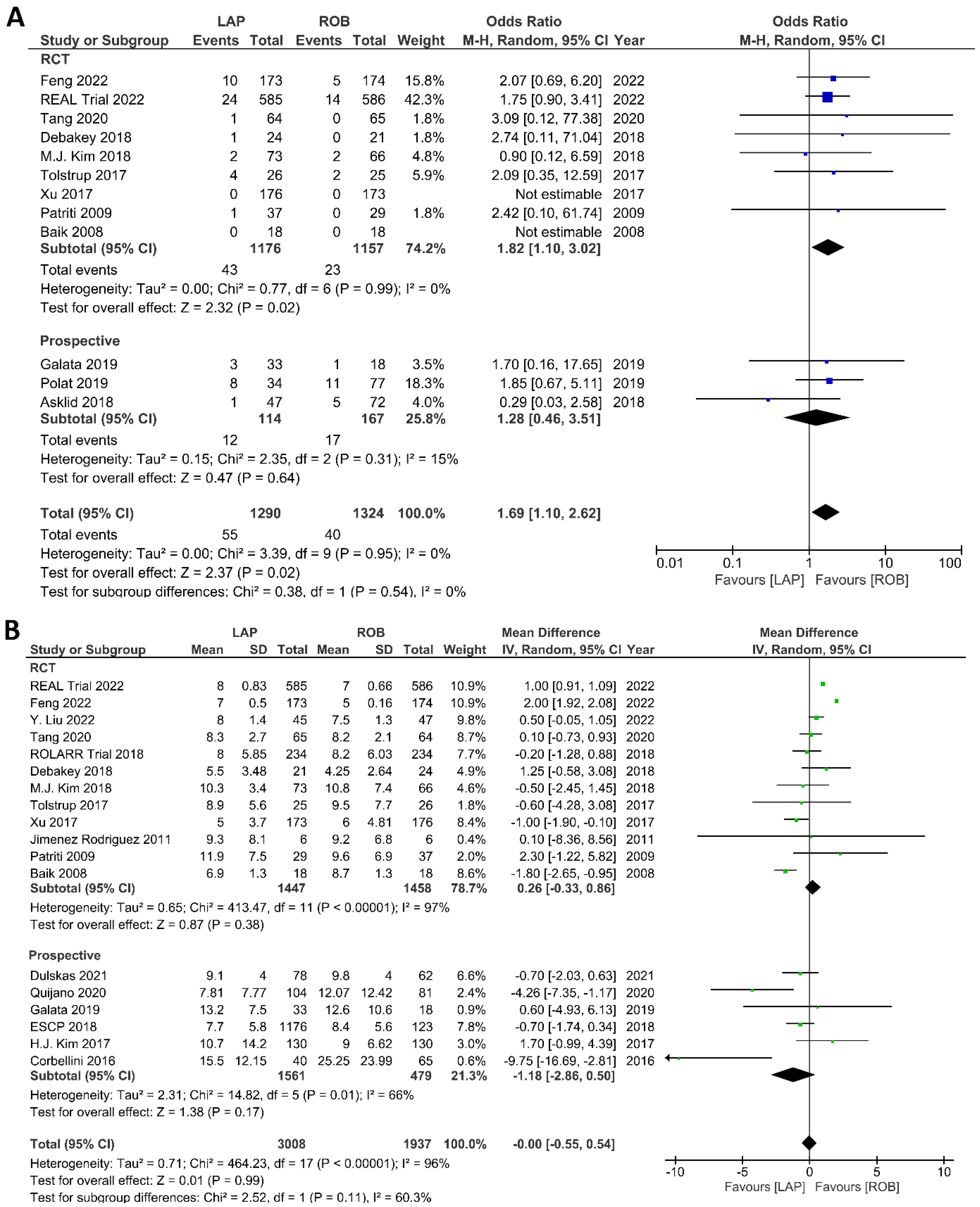
3.3.2. Meta-Analysis B: Robotic vs. Laparoscopic Rectal Resection
Intraoperative Outcomes
Postoperative Outcomes
Histological Outcomes
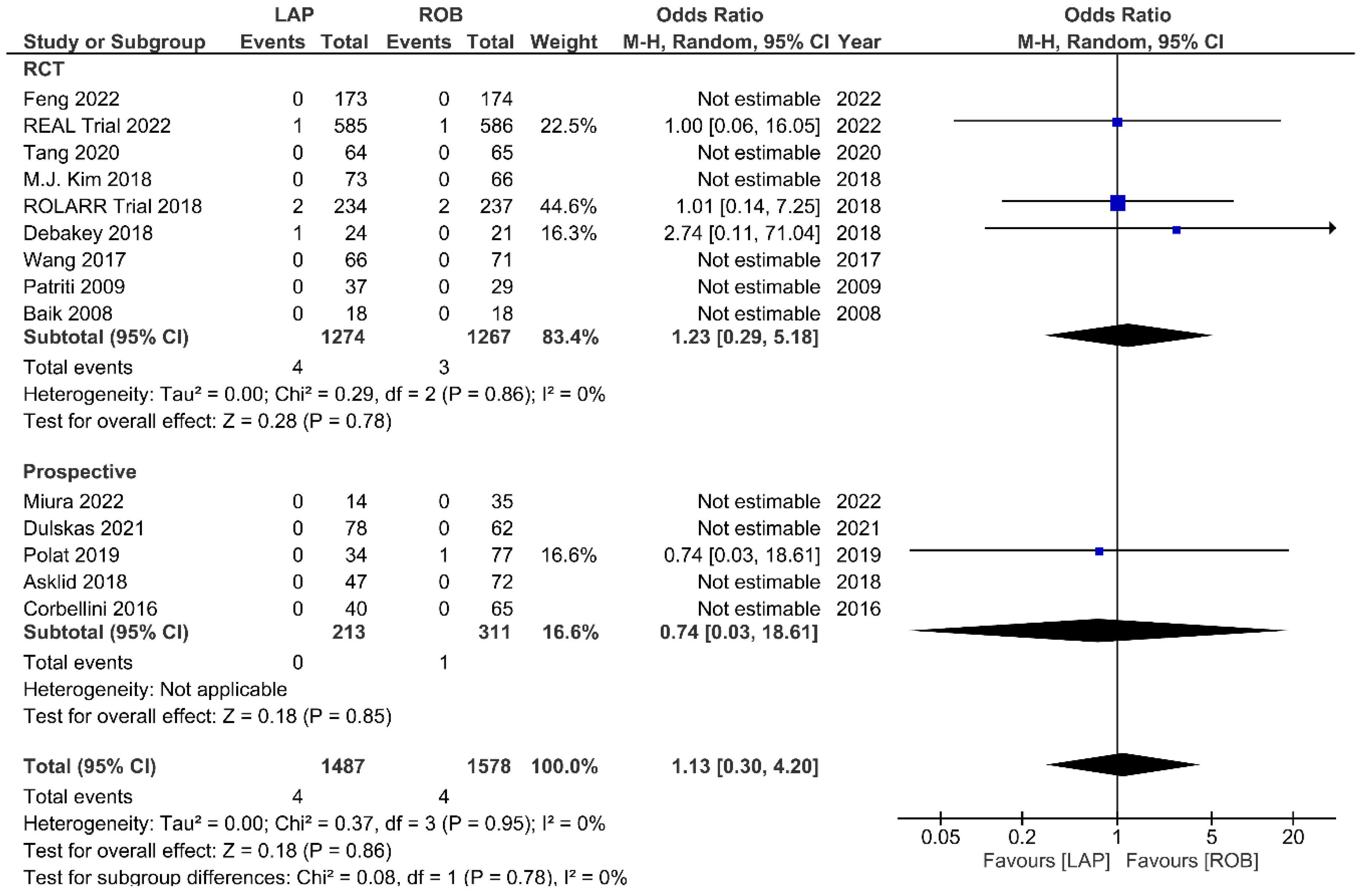
Mortality and Survival Outcomes
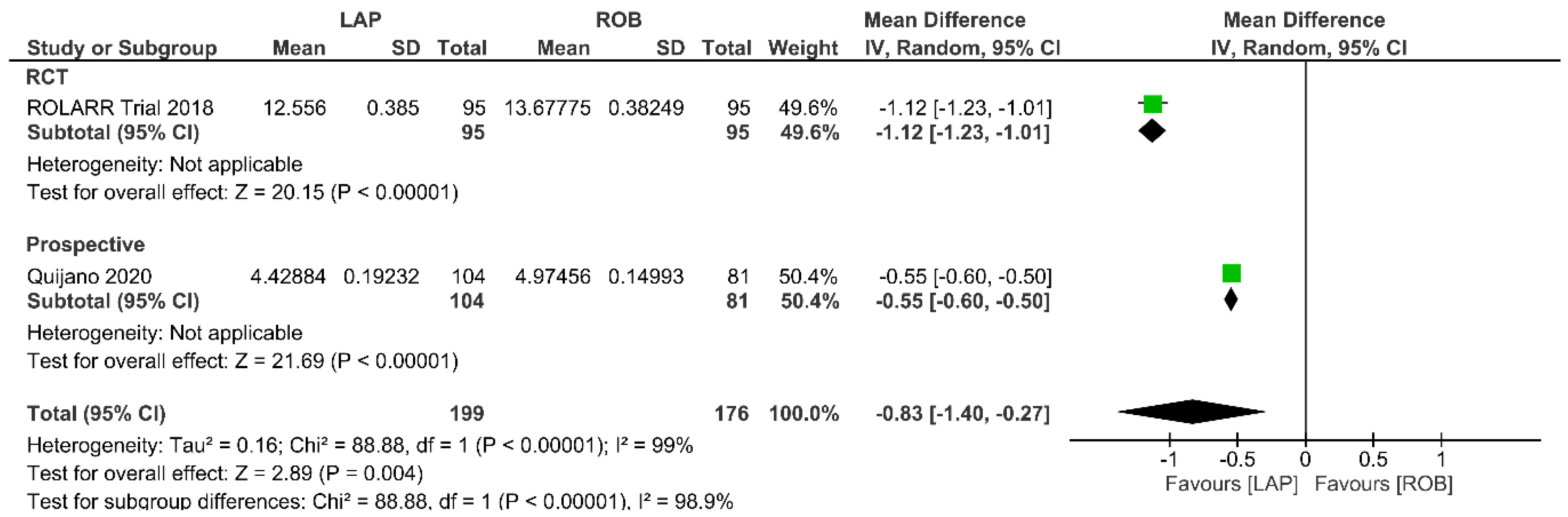
Operative Cost
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Hossain, M.S.; Karuniawati, H.; Jairoun, A.A.; Urbi, Z.; Ooi, J.; John, A.; Lim, Y.C.; Kibria, K.M.K.; Mohiuddin, A.K.M.; Ming, L.C.; et al. Colorectal Cancer: A Review of Carcinogenesis, Global Epidemiology, Current Challenges, Risk Factors, Preventive and Treatment Strategies. Cancers 2022, 14, 1732. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Fazeli, M.S.; Keramati, M.R. Rectal cancer: A review. Med. J. Islam. Repub. Iran 2015, 29, 171. [Google Scholar] [PubMed]
- Glynne-Jones, R.; Wyrwicz, L.; Tiret, E.; Brown, G.; Rödel, C.; Cervantes, A.; Arnold, D. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv22–iv40. [Google Scholar] [CrossRef] [PubMed]
- Senagore, A.J. Adoption of Laparoscopic Colorectal Surgery: It Was Quite a Journey. Clin. Colon Rectal Surg. 2015, 28, 131–134. [Google Scholar] [CrossRef]
- Baik, S.H.; Ko, Y.T.; Kang, C.M.; Lee, W.J.; Kim, N.K.; Sohn, S.K.; Chi, H.S.; Cho, C.H. Robotic tumor-specific mesorectal excision of rectal cancer: Short-term outcome of a pilot randomized trial. Surg. Endosc. 2008, 22, 1601–1608. [Google Scholar] [CrossRef]
- Denost, Q.; Adam, J.P.; Rullier, A.; Buscail, E.; Laurent, C.; Rullier, E. Perineal transanal approach: A new standard for laparoscopic sphincter-saving resection in low rectal cancer, a randomized trial. Ann. Surg. 2014, 260, 993–999. [Google Scholar] [CrossRef]
- Martel, G.; Boushey, R.P. Laparoscopic colon surgery: Past, present and future. Surg. Clin. N. Am. 2006, 86, 867–897. [Google Scholar] [CrossRef]
- Van der Pas, M.H.; Haglind, E.; Cuesta, M.A.; Fürst, A.; Lacy, A.M.; Hop, W.C.; Bonjer, H.J. Laparoscopic versus open surgery for rectal cancer (COLOR II): Short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013, 14, 210–218. [Google Scholar] [CrossRef]
- Jeong, S.Y.; Park, J.W.; Nam, B.H.; Kim, S.; Kang, S.B.; Lim, S.B.; Choi, H.S.; Kim, D.W.; Chang, H.J.; Kim, D.Y.; et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): Survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014, 15, 767–774. [Google Scholar] [CrossRef]
- Bege, T.; Lelong, B.; Esterni, B.; Turrini, O.; Guiramand, J.; Francon, D.; Mokart, D.; Houvenaeghel, G.; Giovannini, M.; Delpero, J.R. The learning curve for the laparoscopic approach to conservative mesorectal excision for rectal cancer: Lessons drawn from a single institution’s experience. Ann. Surg. 2010, 251, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Fleshman, J.; Branda, M.; Sargent, D.J.; Boller, A.M.; George, V.; Abbas, M.; Peters, W.R., Jr.; Maun, D.; Chang, G.; Herline, A.; et al. Effect of Laparoscopic-Assisted Resection vs. Open Resection of Stage II or III Rectal Cancer on Pathologic Outcomes: The ACOSOG Z6051 Randomized Clinical Trial. JAMA 2015, 314, 1346–1355. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, A.R.; Solomon, M.J.; Lumley, J.W.; Hewett, P.; Clouston, A.D.; Gebski, V.J.; Davies, L.; Wilson, K.; Hague, W.; Simes, J. Effect of Laparoscopic-Assisted Resection vs. Open Resection on Pathological Outcomes in Rectal Cancer: The ALaCaRT Randomized Clinical Trial. JAMA 2015, 314, 1356–1363. [Google Scholar] [CrossRef]
- Weber, P.A.; Merola, S.; Wasielewski, A.; Ballantyne, G.H. Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis. Colon Rectum 2002, 45, 1689–1694. [Google Scholar] [CrossRef] [PubMed]
- Stefanidis, D.; Wang, F.; Korndorffer, J.R., Jr.; Dunne, J.B.; Scott, D.J. Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg. Endosc. 2010, 24, 377–382. [Google Scholar] [CrossRef]
- Stefanidis, D.; Hope, W.W.; Scott, D.J. Robotic suturing on the FLS model possesses construct validity, is less physically demanding, and is favored by more surgeons compared with laparoscopy. Surg. Endosc. 2011, 25, 2141–2146. [Google Scholar] [CrossRef]
- Kim, M.J.; Park, S.C.; Park, J.W.; Chang, H.J.; Kim, D.Y.; Nam, B.H.; Sohn, D.K.; Oh, J.H. Robot-assisted Versus Laparoscopic Surgery for Rectal Cancer: A Phase II Open Label Prospective Randomized Controlled Trial. Ann. Surg. 2018, 267, 243–251. [Google Scholar] [CrossRef]
- Corbellini, C.; Biffi, R.; Luca, F.; Chiappa, A.; Costa, S.; Bertani, E.; Bona, S.; Lombardi, D.; Tamayo, D.; Botteri, E.; et al. Open, laparoscopic, and robotic surgery for rectal cancer: Medium-term comparative outcomes from a multicenter study. Tumori 2016, 102, 414–421. [Google Scholar] [CrossRef]
- Jayne, D.; Pigazzi, A.; Marshall, H.; Croft, J.; Corrigan, N.; Copeland, J.; Quirke, P.; West, N.; Rautio, T.; Thomassen, N.; et al. Effect of Robotic-Assisted vs. Conventional Laparoscopic Surgery on Risk of Conversion to Open Laparotomy Among Patients Undergoing Resection for Rectal Cancer: The ROLARR Randomized Clinical Trial. JAMA 2017, 318, 1569–1580. [Google Scholar] [CrossRef]
- Somashekhar, S.P.; Ashwin, K.R.; Rajashekhar, J.; Zaveri, S. Prospective Randomized Study Comparing Robotic-Assisted Surgery with Traditional Laparotomy for Rectal Cancer-Indian Study. Indian J. Surg. 2015, 77, 788–794. [Google Scholar] [CrossRef]
- Prete, F.P.; Pezzolla, A.; Prete, F.; Testini, M.; Marzaioli, R.; Patriti, A.; Jimenez-Rodriguez, R.M.; Gurrado, A.; Strippoli, G.F.M. Robotic Versus Laparoscopic Minimally Invasive Surgery for Rectal Cancer: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann. Surg. 2018, 267, 1034–1046. [Google Scholar] [CrossRef]
- Qiu, H.; Yu, D.; Ye, S.; Shan, R.; Ai, J.; Shi, J. Long-term oncological outcomes in robotic versus laparoscopic approach for rectal cancer: A systematic review and meta-analysis. Int. J. Surg. 2020, 80, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Lei, X.; Ai, J.; Huang, Z.; Shi, J.; Li, T. Comparison of robotic and laparoscopic rectal cancer surgery: A meta-analysis of randomized controlled trials. World J. Surg. Oncol. 2021, 19, 38. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Yan, P.; Jing, W.; Li, M.; Du, B.; Si, M.; Yang, J.; Yang, K.; Cai, H.; Guo, T. Clinical, pathological, and oncologic outcomes of robotic-assisted versus laparoscopic proctectomy for rectal cancer: A meta-analysis of randomized controlled studies. Asian J. Surg. 2020, 43, 880–890. [Google Scholar] [CrossRef] [PubMed]
- Ryan, O.K.; Ryan, É.J.; Creavin, B.; Rausa, E.; Kelly, M.E.; Petrelli, F.; Bonitta, G.; Kennelly, R.; Hanly, A.; Martin, S.T.; et al. Surgical approach for rectal cancer: A network meta-analysis comparing open, laparoscopic, robotic and transanal TME approaches. Eur. J. Surg. Oncol. 2021, 47, 285–295. [Google Scholar] [CrossRef]
- Simillis, C.; Lal, N.; Thoukididou, S.N.; Kontovounisios, C.; Smith, J.J.; Hompes, R.; Adamina, M.; Tekkis, P.P. Open Versus Laparoscopic Versus Robotic Versus Transanal Mesorectal Excision for Rectal Cancer: A Systematic Review and Network Meta-analysis. Ann. Surg. 2019, 270, 59–68. [Google Scholar] [CrossRef]
- Guo, Y.; Guo, Y.; Luo, Y.; Song, X.; Zhao, H.; Li, L. Comparison of pathologic outcomes of robotic and open resections for rectal cancer: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0245154. [Google Scholar] [CrossRef]
- Liao, G.; Li, Y.B.; Zhao, Z.; Li, X.; Deng, H.; Li, G. Robotic-assisted surgery versus open surgery in the treatment of rectal cancer: The current evidence. Sci. Rep. 2016, 6, 26981. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Kalkum, E.; Klotz, R.; Seide, S.; Hüttner, F.J.; Kowalewski, K.F.; Nickel, F.; Khajeh, E.; Knebel, P.; Diener, M.K.; Probst, P. Systematic reviews in surgery-recommendations from the Study Center of the German Society of Surgery. Langenbecks Arch. Surg. 2021, 406, 1723–1731. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, N.; Marshall, H.; Croft, J.; Copeland, J.; Jayne, D.; Brown, J. Exploring and adjusting for potential learning effects in ROLARR: A randomised controlled trial comparing robotic-assisted vs. standard laparoscopic surgery for rectal cancer resection. Trials 2018, 19, 339. [Google Scholar] [CrossRef]
- Debakey, Y.; Zaghloul, A.; Farag, A.; Mahmoud, A.; Elattar, I. Robotic-Assisted versus Conventional Laparoscopic Approach for Rectal Cancer Surgery, First Egyptian Academic Center Experience, RCT. Minim. Invasive Surg. 2018, 2018, 5836562. [Google Scholar] [CrossRef]
- Jiménez Rodríguez, R.M.; Díaz Pavón, J.M.; De La Portilla de Juan, F.; Prendes Sillero, E.; Hisnard Cadet Dussort, J.M.; Padillo, J. Prospective randomised study: Robotic-assisted versus conventional laparoscopic surgery in colorectal cancer resection. Cir. Esp. 2011, 89, 432–438. [Google Scholar] [CrossRef]
- Patriti, A.; Ceccarelli, G.; Bartoli, A.; Spaziani, A.; Biancafarina, A.; Casciola, L. Short- and medium-term outcome of robot-assisted and traditional laparoscopic rectal resection. J. Soc. Laparoendosc. Surg. 2009, 13, 176–183. [Google Scholar]
- Tolstrup, R.; Funder, J.A.; Lundbech, L.; Thomassen, N.; Iversen, L.H. Perioperative pain after robot-assisted versus laparoscopic rectal resection. Int. J. Colorectal. Dis. 2018, 33, 285–289. [Google Scholar] [CrossRef]
- Wang, G.; Wang, Z.; Jiang, Z.; Liu, J.; Zhao, J.; Li, J. Male urinary and sexual function after robotic pelvic autonomic nerve-preserving surgery for rectal cancer. Int. J. Med. Robot. Comput. Assist. Surg. 2017, 13, e1725. [Google Scholar] [CrossRef]
- Xu, J.; Wei, Y.; Ren, L.; Feng, Q.; Chen, J.; Zhu, D.; Chang, W.; Yi, T.; Yang, L.; Qin, X. Robot-assisted vs. laparoscopic vs open abdominoperineal resections for low rectal cancer: Short-term outcomes of a single-center prospective randomized controlled trial. Ann. Oncol. 2017, 28, v161–v162. [Google Scholar] [CrossRef]
- Feng, Q.; Yuan, W.; Li, T.; Tang, B.; Jia, B.; Zhou, Y.; Zhang, W.; Zhao, R.; Zhang, C.; Cheng, L.; et al. Robotic versus laparoscopic surgery for middle and low rectal cancer (REAL): Short-term outcomes of a multicentre randomised controlled trial. Lancet. Gastroenterol. Hepatol. 2022, 7, 991–1004. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; Tang, W.; Zhang, Z.; Wei, Y.; Ren, L.; Chang, W.; Zhu, D.; Liang, F.; He, G.; Xu, J. Robotic versus laparoscopic abdominoperineal resections for low rectal cancer: A single-center randomized controlled trial. J. Surg. Oncol. 2022, 126, 1481–1493. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Liu, M.; Lei, Y.; Zhang, H.; Xie, J.; Zhu, S.; Jiang, J.; Li, J.; Yi, B. Evaluation of effect of robotic versus laparoscopic surgical technology on genitourinary function after total mesorectal excision for rectal cancer. Int. J. Surg. 2022, 104, 106800. [Google Scholar] [CrossRef]
- European Society of Coloproctology collaborating group. An international multicentre prospective audit of elective rectal cancer surgery; operative approach versus outcome, including transanal total mesorectal excision (TaTME). Color. Dis. 2018, 20, 33–46. [Google Scholar] [CrossRef]
- Asklid, D.; Gerjy, R.; Hjern, F.; Pekkari, K.; Gustafsson, U.O. Robotic vs. laparoscopic rectal tumour surgery: A cohort study. Color. Dis. 2019, 21, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Bertani, E.; Chiappa, A.; Biffi, R.; Bianchi, P.P.; Radice, D.; Branchi, V.; Cenderelli, E.; Vetrano, I.; Cenciarelli, S.; Andreoni, B. Assessing appropriateness for elective colorectal cancer surgery: Clinical, oncological, and quality-of-life short-term outcomes employing different treatment approaches. Int. J. Color. Dis. 2011, 26, 1317–1327. [Google Scholar] [CrossRef]
- Dulskas, A.; Albandar, M.; Samalavicius, N.E.; Han, Y.D.; Kim, N.K. Laparoscopic and Robotic Surgery for Rectal Cancer—Comparative Study Between Two Centres. Indian J. Surg. 2021, 83, 48–54. [Google Scholar] [CrossRef]
- Galata, C.; Vassilev, G.; Haas, F.; Kienle, P.; Büttner, S.; Reißfelder, C.; Hardt, J. Clinical, oncological, and functional outcomes of Da Vinci (Xi)-assisted versus conventional laparoscopic resection for rectal cancer: A prospective, controlled cohort study of 51 consecutive cases. Int. J. Color. Dis. 2019, 34, 1907–1914. [Google Scholar] [CrossRef]
- Kim, H.J.; Choi, G.S.; Park, J.S.; Park, S.Y.; Yang, C.S.; Lee, H.J. The impact of robotic surgery on quality of life, urinary and sexual function following total mesorectal excision for rectal cancer: A propensity score-matched analysis with laparoscopic surgery. Color. Dis. 2018, 20, O103–O113. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kim, N.K.; Lee, K.Y.; Hur, H.; Min, B.S.; Kim, J.H. A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: Laparoscopic versus robotic surgery. Ann. Surg. Oncol. 2012, 19, 2485–2493. [Google Scholar] [CrossRef]
- Miura, T.; Sakamoto, Y.; Morohashi, H.; Suto, A.; Kubota, S.; Ichisawa, A.; Kuwata, D.; Yamada, T.; Tamba, H.; Matsumoto, S.; et al. Robotic surgery contributes to the preservation of bowel and urinary function after total mesorectal excision: Comparisons with transanal and conventional laparoscopic surgery. BMC Surg. 2022, 22, 147. [Google Scholar] [CrossRef] [PubMed]
- Polat, F.; Willems, L.H.; Dogan, K.; Rosman, C. The oncological and surgical safety of robot-assisted surgery in colorectal cancer: Outcomes of a longitudinal prospective cohort study. Surg. Endosc. 2019, 33, 3644–3655. [Google Scholar] [CrossRef]
- Quijano, Y.; Nuñez-Alfonsel, J.; Ielpo, B.; Ferri, V.; Caruso, R.; Durán, H.; Díaz, E.; Malavé, L.; Fabra, I.; Pinna, E.; et al. Robotic versus laparoscopic surgery for rectal cancer: A comparative cost-effectiveness study. Tech. Coloproctol. 2020, 24, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Choi, G.S.; Lim, K.H.; Jang, Y.S.; Jun, S.H. Robotic-assisted versus laparoscopic surgery for low rectal cancer: Case-matched analysis of short-term outcomes. Ann. Surg. Oncol. 2010, 17, 3195–3202. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Pérez, A.; Carra, M.C.; Brunetti, F.; De’Angelis, N. Pathologic Outcomes of Laparoscopic vs Open Mesorectal Excision for Rectal Cancer: A Systematic Review and Meta-analysis. JAMA Surg. 2017, 152, e165665. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, A.R.L.; Solomon, M.J.; Brown, C.S.B.; Lumley, J.W.; Hewett, P.; Clouston, A.D.; Gebski, V.J.; Wilson, K.; Hague, W.; Simes, J. Disease-free Survival and Local Recurrence After Laparoscopic-assisted Resection or Open Resection for Rectal Cancer: The Australasian Laparoscopic Cancer of the Rectum Randomized Clinical Trial. Ann. Surg. 2019, 269, 596–602. [Google Scholar] [CrossRef]
- Liu, G.; Zhang, S.; Zhang, Y.; Fu, X.; Liu, X. Robotic Surgery in Rectal Cancer: Potential, Challenges, and Opportunities. Curr. Treat. Options Oncol. 2022, 23, 961–979. [Google Scholar] [CrossRef]
- Wee, I.J.Y.; Kuo, L.J.; Ngu, J.C. Urological and sexual function after robotic and laparoscopic surgery for rectal cancer: A systematic review, meta-analysis and meta-regression. Int. J. Med. Robot. Comput. Assist. Surg. 2021, 17, 1–8. [Google Scholar] [CrossRef]
- Kowalewski, K.F.; Seifert, L.; Ali, S.; Schmidt, M.W.; Seide, S.; Haney, C.; Tapking, C.; Shamiyeh, A.; Kulu, Y.; Hackert, T.; et al. Functional outcomes after laparoscopic versus robotic-assisted rectal resection: A systematic review and meta-analysis. Surg. Endosc. 2021, 35, 81–95. [Google Scholar] [CrossRef]
- Clancy, C.; O’Leary, D.P.; Burke, J.P.; Redmond, H.P.; Coffey, J.C.; Kerin, M.J.; Myers, E. A meta-analysis to determine the oncological implications of conversion in laparoscopic colorectal cancer surgery. Color. Dis. 2015, 17, 482–490. [Google Scholar] [CrossRef]
- Guillou, P.J.; Quirke, P.; Thorpe, H.; Walker, J.; Jayne, D.G.; Smith, A.M.; Heath, R.M.; Brown, J.M. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): Multicentre, randomised controlled trial. Lancet 2005, 365, 1718–1726. [Google Scholar] [CrossRef] [PubMed]
- Rottoli, M.; Bona, S.; Rosati, R.; Elmore, U.; Bianchi, P.P.; Spinelli, A.; Bartolucci, C.; Montorsi, M. Laparoscopic rectal resection for cancer: Effects of conversion on short-term outcome and survival. Ann. Surg. Oncol. 2009, 16, 1279–1286. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, P.P.; Ceriani, C.; Locatelli, A.; Spinoglio, G.; Zampino, M.G.; Sonzogni, A.; Crosta, C.; Andreoni, B. Robotic versus laparoscopic total mesorectal excision for rectal cancer: A comparative analysis of oncological safety and short-term outcomes. Surg. Endosc. 2010, 24, 2888–2894. [Google Scholar] [CrossRef] [PubMed]
- Mörner, M.E.; Gunnarsson, U.; Jestin, P.; Svanfeldt, M. The importance of blood loss during colon cancer surgery for long-term survival: An epidemiological study based on a population based register. Ann. Surg. 2012, 255, 1126–1128. [Google Scholar] [CrossRef] [PubMed]
- Basilico, V.; Griffa, B.; Radaelli, F.; Zanardo, M.; Rossi, F.; Caizzone, A.; Vannelli, A. Anastomotic leakage following colorectal resection for cancer: How to define, manage and treat it. Minerva Chir. 2014, 69, 245–252. [Google Scholar] [PubMed]
- Memon, S.; Heriot, A.G.; Murphy, D.G.; Bressel, M.; Lynch, A.C. Robotic versus laparoscopic proctectomy for rectal cancer: A meta-analysis. Ann. Surg. Oncol. 2012, 19, 2095–2101. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Choi, G.S.; Lim, K.H.; Jang, Y.S.; Jun, S.H. S052: A comparison of robot-assisted, laparoscopic, and open surgery in the treatment of rectal cancer. Surg. Endosc. 2011, 25, 240–248. [Google Scholar] [CrossRef]
- Flynn, J.; Larach, J.T.; Kong, J.C.H.; Waters, P.S.; Warrier, S.K.; Heriot, A. The learning curve in robotic colorectal surgery compared with laparoscopic colorectal surgery: A systematic review. Color. Dis. 2021, 23, 2806–2820. [Google Scholar] [CrossRef]
- Brodie, A.; Vasdev, N. The future of robotic surgery. Ann. R. Coll. Surg. Engl. 2018, 100, 4–13. [Google Scholar] [CrossRef]
- Son, G.M.; Kim, J.G.; Lee, J.C.; Suh, Y.J.; Cho, H.M.; Lee, Y.S.; Lee, I.K.; Chun, C.S. Multidimensional analysis of the learning curve for laparoscopic rectal cancer surgery. J. Laparoendosc. Adv. Surg. Tech. Part A 2010, 20, 609–617. [Google Scholar] [CrossRef]
- Jiménez-Rodríguez, R.M.; Díaz-Pavón, J.M.; De la Portilla de Juan, F.; Prendes-Sillero, E.; Dussort, H.C.; Padillo, J. Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int. J. Color. Dis. 2013, 28, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Kinugasa, Y.; Shiomi, A.; Sato, S.; Yamakawa, Y.; Kagawa, H.; Tomioka, H.; Mori, K. Learning curve for robotic-assisted surgery for rectal cancer: Use of the cumulative sum method. Surg. Endosc. 2015, 29, 1679–1685. [Google Scholar] [CrossRef] [PubMed]






| Study (Year) | Study Design | Country | Group | Age (Mean ± SD) | Sex (M/F) | BMI (Mean ± SD) | ASA (I/II/III/IV) | Tumor Location from Anal Verge, cm (Mean ± SD) | Robotic Surgical Technique | Sphincter-Saving Procedures | Follow-Up Duration, Months (Mean) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Robotic vs. Open | |||||||||||
| Bertani et al. (2011) [46] | Prospective | Italy | ROB: 52 | 59.6 ± 11.6 | 31/21 | 24.8 ± 3.62 | 49 (I–II) 3 (III–V) | Median 8.4 (3–20) | Full-robotic | N/A | N/A |
| Open: 34 | 63.2 ± 10.5 | 20/14 | 25.6 ± 3.85 | 28 (I–II) 6 (III–V) | Median 9.7 (3–25) | N/A | N/A | ||||
| Somashekhar et al. (2015) [20] | RCT | India | ROB: 25 | 56.36 ± 8.21 | 17/8 | 31.51 ± 3.02 | N/A | N/A | N/A | N/A | Median 5 |
| Open: 25 | 59.56 ± 5.75 | 15/10 | 29.84 ± 2.75 | N/A | N/A | N/A | |||||
| Corbellini et al. (2016) [18] | Prospective | Italy | ROB: 65 | 64 (39–78) | 35/30 | 36 (<25) 23 (25–30) 6 (>30) | N/A | Median 8 (1–12) | Hybrid | N/A | 33 (1–57) |
| Open: 55 | 62 (40–80) | 36/19 | 33 (<25) 13 (25–30) 9 (>30) | N/A | Median 7 (1–12) | N/A | |||||
| Xu et al. (2017) [40] | RCT | China | ROB: 173 | N/A | N/A | N/A | N/A | 5 | N/A | N/A | N/A |
| Open: 154 | N/A | N/A | N/A | N/A | N/A | N/A | |||||
| ESCP (2018) [44] | Prospective | Denmark | ROB: 123 | N/A | 84/39 | 51 (<25) 45 (25–29.9) 26 (≥30) | 89 (I–II) 34 (III–V) | N/A | N/A | N/A | N/A |
| Open: 868 | N/A | 526/342 | 295 (<25) 357 (25–29.9) 201 (≥30) | 516 (I–II) 348 (III–V) | N/A | N/A | N/A | ||||
| Robotic vs. Laparoscopic | |||||||||||
| Bailk et al. (2008) [6] | RCT | South Korea | ROB: 18 | 57.3 ± 6.3 | 14/4 | 22.8 ± 1.8 | 12/6/0/0 | 11.3 ± 2.5 | Hybrid | 18 | N/A |
| LAP: 18 | 62.0 ± 9.0 | 14/4 | 24.0 ± 2.5 | 10/6/1/1 | 1.0 ± 2.5 | 18 | N/A | ||||
| Patriti et al. (2009) [37] | RCT | Italy | ROB:29 | 68 ± 10 | 11/18 | 24 ± 6.2 | 2/13/14/0 | 5.9 ± 4.2 | Hybrid | 24 | 29.2 |
| LAP: 37 | 69 ± 10 | 12/25 | 25.4 ± 6.44 | 2/14/21/0 | 11 ± 4.5 | 34 | 18.7 | ||||
| Jimenez Rodrıguez et al. (2011) [36] | RCT | Spain | ROB: 28 * | 68 ± 9.1 | 12/16 | 28.59 ± 2.5 | 14 (I–II) 14 (III) | 4.8 ± 1.6 | N/A | N/A | N/A |
| LAP: 28 * | 61.5 ± 15 | 17/11 | 26.75 ± 5.6 | 20 (I–II) 8 (III) | 3.8 ± 0.7 | N/A | N/A | ||||
| J.Y. Kim et al. (2012) [50] | Prospective | South Korea | ROB: 30 | 54.13 ± 8.52 | 18/12 | 24.36 ± 2.44 | 29/1 (I/II) | (10–15 cm): 8 (6–10 cm): 16 (<6 cm): 6 | Full-robotic | 29 | 12 |
| LAP: 39 | 56.85 ± 11.14 | 20/19 | 24.01 ± 2.19 | 39/0 (I/II) | (10–15 cm): 14 (6–10 cm): 17 (<6 cm): 6 | 38 | 12 | ||||
| Corbellini et al. (2016) [18] | Prospective | Italy | ROB: 65 | Median 64 (39–78) | 35/30 | 36 (<25) 23 (25–30) 6 (>30) | N/A | Median 8 (1–12) | Hybrid | N/A | 33 (1–57) |
| LAP: 40 | Median 64 (36–80) | 23/17 | 17 (<25) 14 (25–30) 9 (>30) | N/A | Median 8.5 (1.2–12) | N/A | |||||
| H. J. Kim et al. (2017) [49] | Prospective | South Korea | ROB:130 | 60.5 ± 10.1 | 95/35 | 23.7 ± 3.2 | 71/48/11 (I/II/III) | 5.9 ± 2.7 | Hybrid | N/A | N/A |
| LAP: 130 | 60 ± 9.3 | 95/35 | 23.3 ± 2.9 | 70/46/14 (I/II/III) | 6.3 ± 2.6 | N/A | N/A | ||||
| Tolstrup et al. (2017) [38] | RCT | Denmark | ROB: 25 | 63 ± 10.9 | 18/7 | 27 ± 4.5 | 11/7/0/0 | N/A | Full-robotic | 3/10/3/9 | N/A |
| LAP: 26 | 68 ± 9.9 | 20/6 | 28 ± 4.3 | 10/8/1/0 | N/A | 4/11/5/6 | N/A | ||||
| Xu et al. (2017) [40] | RCT | China | ROB: 173 | N/A | N/A | N/A | N/A | 5 | N/A | N/A | N/A |
| LAP: 176 | N/A | N/A | N/A | N/A | N/A | N/A | |||||
| Wang et al. (2017) [39] | RCT | China | ROB: 71 | Median 60.3 (36–68) | 71/0 | Median 22.9 (19.1–30.1) | N/A | 25 (7–12) 46 (≤7) | N/A | 69 | 12 |
| LAP: 66 | Median 58.7 (36–71) | 66/0 | Median 22.4 (18.3–30.6) | N/A | 26 (7–12 ) 40 (≤7) | 63 | 12 | ||||
| Jayne et al. (2017) [19] AND Corrigan et al. (2018) [34] (ROLLAR trial) | RCT | UK | ROB: 237 | 64.4 ± 10.98 | 161/76 | 93 (<25) 90 (25–29.9) 54 (≥30) | 39/150/46/0 | 71 (10–15) 107 (6–10) 57 (<6) | Hybrid+ Full- robotic | 184 | 6 |
| LAP: 234 | 65.5 ± 11.93 | 159/75 | 87 (< 25) 92 (25–29.9) 55 (≥30) | 52/124/52/1 | 69 (10–15) 99 (6–10) 61 (<6) | 185 | 6 | ||||
| Debakey et al. (2018) [35] | RCT | Egypt | ROB: 21 | Median 53.4 (32–67) | 11/10 | N/A | 18/3/0/0 | 9 (10–15) 10 (5–10) 5 (<5): | Full-robotic | 20 | N/A |
| LAP: 24 | Median 50.3 (36–64) | 13/11 | N/A | 18/6/0/0 | 13 (10–15) 8 (5–10) 3 (<5) | 21 | N/A | ||||
| M. J. Kim et al. (2018) [17] | RCT | South Korea | ROB: 66 | 60.4 ± 9.7 | 51/15 | 24.1 ± 3.3 | 20/46 (I/II) | 33 (>5) 33 (≤5) | Hybrid | 65 | N/A |
| LAP: 73 | 59.7 ± 11.7 | 52/21 | 23.6 ± 3.0 | 30/43 (I/II) | 38 (>5) 35 (≤5) | 70 | N/A | ||||
| Asklid et al. (2018) [45] | Prospective | Sweden | ROB: 72 | 65.5 ± 10.4 | 43/29 | 24.6 ± 0.4 | 16/43/13/0 | 8.5 ± 3.6 | N/A | N/A | N/A |
| LAP: 47 | 70.1 ± 12 | 21/26 | 25.3 ± 0.5 | 8/24/14/1 | 9.8 ± 3.9 | N/A | N/A | ||||
| ESCP (2018) [44] | Prospective | Denmark | ROB: 123 | N/A | 84/39 | 51 (<25) 45 (25–29.9) 26 (≥30) | 89 (I–II) 34 (III–V) | N/A | N/A | N/A | N/A |
| LAP: 1176 | N/A | 727/449 | 361 (0–24.9) 504 (25–29.9)) 281 (≥30) | 787 (I–II) 369 (III–V) | N/A | N/A | N/A | ||||
| Galata et al. (2019) [48] | Prospective | Germany | ROB: 18 | 60.0 ± 11.8 | 10/8 | 26.0 ± 4.0 | 15/3 (II/III) | 8.5 ± 4.0 | Hybrid | N/A | 12 |
| LAP: 33 | 62.3 ± 13.7 | 21/12 | 27.4 ± 5.5 | 21/12 (II/III) | 7.7 ± 3.3 | N/A | 12 | ||||
| Polat et al. (2019) [52] | Prospective | Netherlands | ROB: 77 | N/A | N/A | N/A | N/A | N/A | Full-robotic | N/A | N/A |
| LAP: 34 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||||
| Tang et al. (2020) [23] | RCT | China | ROB: 65 | 55.1 ± 12.1 | 36/29 | 22 ± 2.5 | 35/30/0/0 | 6 ± 2.4 | Full-robotic | 52 | 9–31 |
| LAP: 64 | 58.0 ± 9.7 | 36/28 | 22.1 ± 2.3 | 27/37/0/0 | 5.8 ± 2.6 | 44 | 9–31 | ||||
| Quijano et al. (2020) [53] | Prospective | Spain | ROB: 81 | 63.98 ± 9.68 | 54/37 | 25.98 ± 4.2 | 64 (I–II) 17 (III–V) | 7.1 | N/A | N/A | Median 12 (12–17) |
| LAP: 104 | 61.37 ± 10.7 | 85/55 | 25.23 ± 5.38 | 91 (I–II) 13 (III–V) | 7.3 | N/A | Median 12 (12–17 | ||||
| Dulskas et al. (2021) [47] | Prospective | Lithuania | ROB: 62 | Median 54 (35–74) | 42/20 | 22.9 ± 3.0 | N/A | 22 (≥10 cm) 40 (6–10 cm) | N/A | N/A | N/A |
| LAP: 78 | Median 64 (26–89) | 43/35 | 27.3 ± 3.3 | N/A | 74 (≥10 cm) 4 (6–10 cm) | N/A | N/A | ||||
| Miura et al. (2022) [51] | Prospective | Japan | ROB: 35 | Median 65 (37–75) | 28/7 | Median 22.9 (18.7–31.4) | 33 (I–II) 2 (III–V) | Median 5.5 (2.5–8) | N/A | N/A | Median 22 (9–47) |
| LAP: 14 | Median 66 (34–77) | 8/6 | Median 21.4 (18.6–28.8) | 13 (I–II) 1 (III–V) | Median 5.7 (3.5–8) | N/A | Median 33 (7–52) | ||||
| REAL Trial, (2022) [41] | RCT | China | ROB: 586 | 59.1 ± 11 | 356/230 | 23.5 ± 3.3 | 554 (I–II) 32 (III) | 5.9 ± 2.4 | Full-robotic | 444 | 30 (30–30) |
| LAP: 585 | 60.7 ± 9.8 | 354/231 | 23.5 ± 3.1 | 558 (I–II) 27 (III) | 5.8 ± 2.6 | 435 | 30 (30–30) | ||||
| Feng et al. (2022) [42] | RCT | China | ROB: 174 | 58.2 ± 9.6 | 108/66 | N/A | 170 (I–II) 4 (III) | 3.5 ± 0.7 | Full-robotic | N/A | 49 (38–62) |
| LAP: 173 | 59.5 ± 10.2 | 113/60 | N/A | 166 (I–II) 7 (III) | 3.6 ± 0.7 | N/A | 49 (38–62) | ||||
| Liu et al. (2022) [43] | RCT | China | ROB: 47 | 58.7 ± 7.63 | 27/20 | 22.50 ± 1.67 | 46 (I–II) 1 (III) | 5.15 ± 0.83 | Full-robotic | N/A | 12 |
| LAP: 45 | 58.53 ± 8.78 | 25/20 | 23.3 ± 2.37 | 45 (I–II) 0 (III) | 5.23 ± 0.92 | N/A | 12 | ||||
| Study and Year | Domain 1 | Domain 2 | Domain 3 | Domain 4 | Domain 5 | Domain 6 | Domain 7 | Overall |
|---|---|---|---|---|---|---|---|---|
| Bailk et al. (2008) [6] | Low | Low | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns |
| Patriti et al. (2009) [37] | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns |
| Jimenez Rodrıguez et al. (2011) [36] | Low | Some concerns | Some concerns | Some concerns | Low | Low | Low | Some concerns |
| Somashekhar et al. (2015) [20] | Some concerns | Some concerns | High | High | Some concerns | Some concerns | High | High |
| Jayne et al. (2017) [19] | Low | Some concerns | Some concerns | Low | Low | Low | Low | Some concerns |
| Xu et al. (2017) [40] | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Low | Some concerns | Some concerns |
| Wang et al. (2017) [39] | Low | Low | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns |
| Tolstrup et al. (2017) [38] | Low | Some concerns | High | High | Low | Some concerns | Low | High |
| Corrigan et al. (2018) [34] | Low | Some concerns | Some concerns | Low | Low | Low | Low | Some concerns |
| M. J. Kim et al. (2018) [17] | Low | Low | High | Low | Low | Low | Low | High |
| Debakey et al. (2018) [35] | Low | High | High | High | Low | Some concerns | Some concerns | High |
| Tang et al. (2020) [23] | Low | Low | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns |
| REAL Trial, (2022) [41] | Low | Low | High | Low | Low | Low | Low | High |
| Feng et al. (2022) [42] | Low | Some concerns | High | Low | Low | Low | Low | High |
| Liu et al. (2022) [43] | High | High | High | Some concerns | Some concerns | Low | Some concerns | High |
| Study and Year | Domain 1 | Domain 2 | Domain 3 | Domain 4 | Domain 5 | Domain 6 | Domain 7 | Overall |
|---|---|---|---|---|---|---|---|---|
| Bertani et al. (2011) [46] | Moderate | Low | Low | Low | Moderate | Low | Moderate | Moderate |
| J.Y. Kim et al. (2012) [50] | Serious | Moderate | Low | Low | Moderate | Low | Moderate | Serious |
| ESCP (2018) [44] | Moderate | Low | Low | Moderate | Moderate | Low | Low | Moderate |
| Corbellini et al. (2016) [18] | Moderate | Moderate | Moderate | Moderate | Moderate | Low | Moderate | Moderate |
| H. J. Kim et al. (2017) [49] | Moderate | Moderate | Low | Low | Serious | Moderate | Moderate | Serious |
| Asklid et al. (2018) [45] | Moderate | Moderate | Low | Low | Moderate | Low | Moderate | Moderate |
| Galata et al. (2019) [48] | Moderate | Moderate | Low | Low | Moderate | Low | Moderate | Moderate |
| Polat et al. (2019) [52] | Moderate | Moderate | Low | Low | Moderate | Low | Moderate | Moderate |
| Quijano et al. (2020) [53] | Moderate | Moderate | Moderate | Low | Moderate | Moderate | Low | Moderate |
| Dulskas et al. (2021) [47] | Serious | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Serious |
| Miura et al. (2022) [51] | Moderate | Moderate | Moderate | Moderate | Serious | Moderate | Serious | Serious |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khajeh, E.; Aminizadeh, E.; Dooghaie Moghadam, A.; Nikbakhsh, R.; Goncalves, G.; Carvalho, C.; Parvaiz, A.; Kulu, Y.; Mehrabi, A. Outcomes of Robot-Assisted Surgery in Rectal Cancer Compared with Open and Laparoscopic Surgery. Cancers 2023, 15, 839. https://doi.org/10.3390/cancers15030839
Khajeh E, Aminizadeh E, Dooghaie Moghadam A, Nikbakhsh R, Goncalves G, Carvalho C, Parvaiz A, Kulu Y, Mehrabi A. Outcomes of Robot-Assisted Surgery in Rectal Cancer Compared with Open and Laparoscopic Surgery. Cancers. 2023; 15(3):839. https://doi.org/10.3390/cancers15030839
Chicago/Turabian StyleKhajeh, Elias, Ehsan Aminizadeh, Arash Dooghaie Moghadam, Rajan Nikbakhsh, Gil Goncalves, Carlos Carvalho, Amjad Parvaiz, Yakup Kulu, and Arianeb Mehrabi. 2023. "Outcomes of Robot-Assisted Surgery in Rectal Cancer Compared with Open and Laparoscopic Surgery" Cancers 15, no. 3: 839. https://doi.org/10.3390/cancers15030839
APA StyleKhajeh, E., Aminizadeh, E., Dooghaie Moghadam, A., Nikbakhsh, R., Goncalves, G., Carvalho, C., Parvaiz, A., Kulu, Y., & Mehrabi, A. (2023). Outcomes of Robot-Assisted Surgery in Rectal Cancer Compared with Open and Laparoscopic Surgery. Cancers, 15(3), 839. https://doi.org/10.3390/cancers15030839







