Factors Associated with Poor Quality of Life in Breast Cancer Survivors: A 3-Year Follow-Up Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
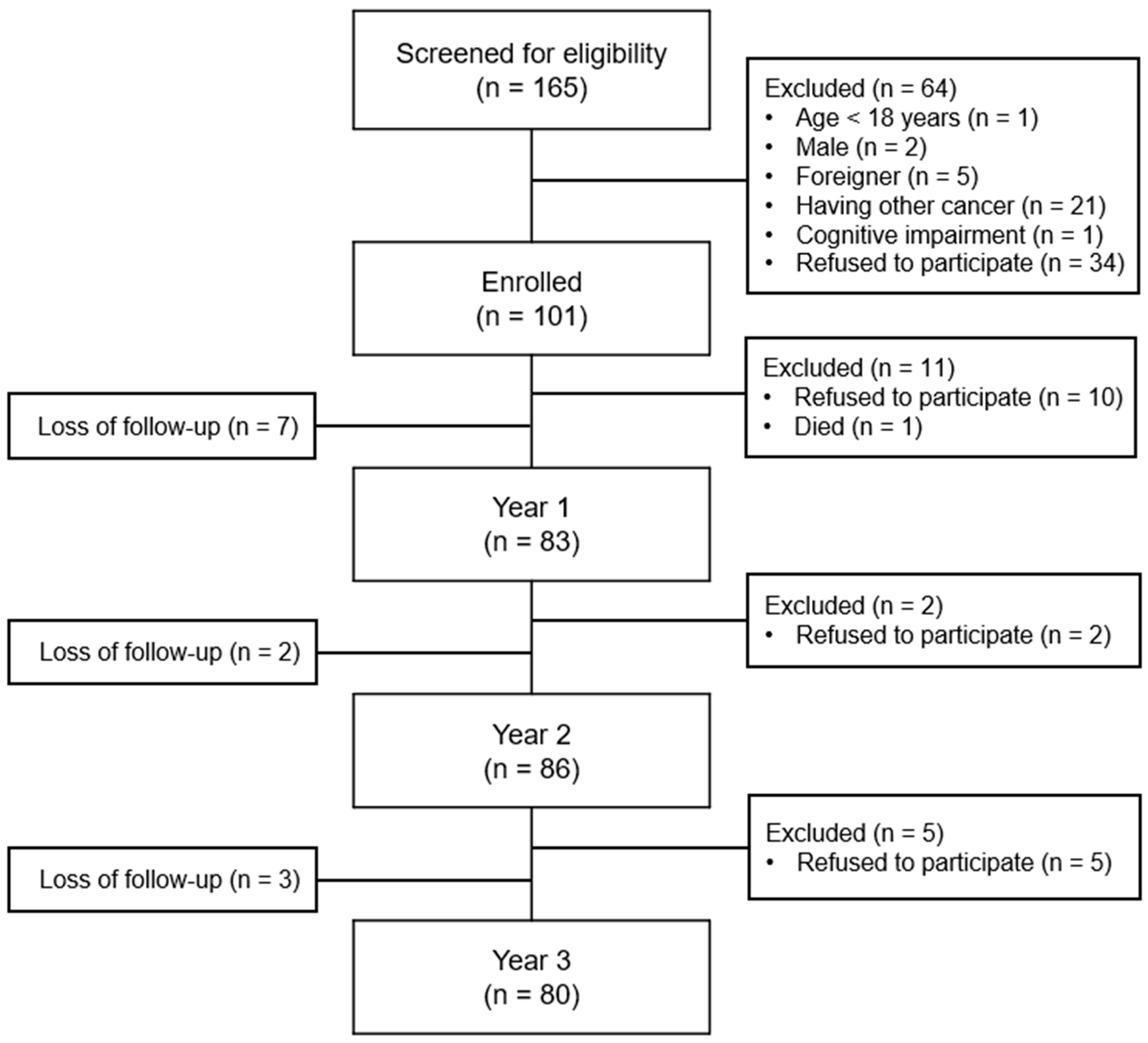
2.1. Study Design and Participants
2.2. Data Collection
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
3.2. Lifestyle and Symptoms Characteristics over Time
3.3. QOL Change Subgroups
3.4. Univariate Logistic Regression Analyses for Poor QOL
3.5. Multivariable Logistic Regression Analyses for Poor QOL
4. Discussion
4.1. Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kang, M.J.; Jung, K.W.; Bang, S.H.; Choi, S.H.; Park, E.H.; Yun, E.H.; Kim, H.J.; Kong, H.J.; Im, J.S.; Seo, H.G.; et al. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2020. Cancer Res. Treat. 2023, 55, 385–399. [Google Scholar]
- Global Breast Cancer Initiative. Available online: https://www.who.int/initiatives/global-breast-cancer-initiative (accessed on 9 May 2023).
- Skandarajah, A.R.; Lisy, K.; Ward, A.; Bishop, J.; Lacey, K.; Mann, B.; Jefford, M. Patient-reported outcomes in survivors of breast cancer one, three, and five years post-diagnosis: A cancer registry-based feasibility study. Qual. Life Res. 2021, 30, 385–394. [Google Scholar]
- Carreira, H.; Williams, R.; Dempsey, H.; Stanway, S.; Smeeth, L.; Bhaskaran, K. Quality of life and mental health in breast cancer survivors compared with non-cancer controls: A study of patient-reported outcomes in the United Kingdom. J. Cancer Surviv. 2021, 15, 564–575. [Google Scholar]
- Jeffe, D.B.; Perez, M.; Liu, Y.; Collins, K.K.; Aft, R.L.; Schootman, M. Quality of life over time in women diagnosed with ductal carcinoma in situ, early-stage invasive breast cancer, and age-matched controls. Breast Cancer Res. Treat. 2012, 134, 379–391. [Google Scholar]
- Ahn, S.H.; Park, B.W.; Noh, D.Y.; Nam, S.J.; Lee, E.S.; Lee, M.K.; Kim, S.H.; Lee, K.M.; Park, S.M.; Yun, Y.H. Health-related quality of life in disease-free survivors of breast cancer with the general population. Ann. Oncol. 2007, 18, 173–182. [Google Scholar]
- Doege, D.; Thong, M.S.Y.; Koch-Gallenkamp, L.; Bertram, H.; Eberle, A.; Holleczek, B.; Nennecke, A.; Pritzkuleit, R.; Waldmann, A.; Zeissig, S.R.; et al. Clinical and sociodemographic determinants of disease-specific health-related quality of life in long-term breast cancer survivors. J. Cancer Res. Clin. Oncol. 2022, 148, 3461–3473. [Google Scholar]
- Lee, E.S.; Lee, M.K.; Kim, S.H.; Ro, J.S.; Kang, H.S.; Kim, S.W.; Lee, K.S.; Yun, Y.H. Health-related quality of life in survivors with breast cancer 1 year after diagnosis compared with the general population: A prospective cohort study. Ann. Surg. 2011, 253, 101–108. [Google Scholar]
- Lei, Y.Y.; Ho, S.C.; Lau, T.K.H.; Kwok, C.; Cheng, A.; Cheung, K.L.; Lee, R.; Yeo, W. Longitudinal change of quality of life in the first five years of survival among disease-free Chinese breast cancer survivors. Qual. Life Res. 2021, 30, 1583–1594. [Google Scholar]
- Hsiao, F.H.; Kuo, W.H.; Jow, G.M.; Wang, M.Y.; Chang, K.J.; Lai, Y.M.; Chen, Y.T.; Huang, C.S. The changes of quality of life and their correlations with psychosocial factors following surgery among women with breast cancer from the post-surgery to post-treatment survivorship. Breast 2019, 44, 59–65. [Google Scholar]
- Tran, T.X.M.; Jung, S.Y.; Lee, E.G.; Cho, H.; Cho, J.; Lee, E.; Chang, Y.J.; Cho, H. Long-term trajectory of postoperative health-related quality of life in young breast cancer patients: A 15-year follow-up study. J. Cancer Surviv. 2023, 17, 1416–1426. [Google Scholar]
- Maurer, T.; Thone, K.; Obi, N.; Jung, A.Y.; Behrens, S.; Becher, H.; Chang-Claude, J. Health-Related Quality of Life in a Cohort of Breast Cancer Survivors over More than 10 Years Post-Diagnosis and in Comparison to a Control Cohort. Cancers 2021, 13, 1854. [Google Scholar]
- Jeffe, D.B.; Perez, M.; Cole, E.F.; Liu, Y.; Schootman, M. The Effects of Surgery Type and Chemotherapy on Early-Stage Breast Cancer Patients’ Quality of Life Over 2-Year Follow-up. Ann. Surg. Oncol. 2016, 23, 735–743. [Google Scholar]
- Koch, L.; Jansen, L.; Herrmann, A.; Stegmaier, C.; Holleczek, B.; Singer, S.; Brenner, H.; Arndt, V. Quality of life in long-term breast cancer survivors—A 10-year longitudinal population-based study. Acta. Oncol. 2013, 52, 1119–1128. [Google Scholar]
- Ganz, P.A.; Kwan, L.; Stanton, A.L.; Bower, J.E.; Belin, T.R. Physical and psychosocial recovery in the year after primary treatment of breast cancer. J. Clin. Oncol. 2011, 29, 1101–1109. [Google Scholar]
- Park, J.H.; Jung, Y.S.; Kim, J.Y.; Jo, Y.; Bae, S.H. Trajectories of health-related quality of life in breast cancer patients. Support Care Cancer 2020, 28, 3381–3389. [Google Scholar]
- Goyal, N.G.; Levine, B.J.; Van Zee, K.J.; Naftalis, E.; Avis, N.E. Trajectories of quality of life following breast cancer diagnosis. Breast Cancer Res. Treat. 2018, 169, 163–173. [Google Scholar]
- Di Meglio, A.; Havas, J.; Gbenou, A.S.; Martin, E.; El-Mouhebb, M.; Pistilli, B.; Menvielle, G.; Dumas, A.; Everhard, S.; Martin, A.L.; et al. Dynamics of Long-Term Patient-Reported Quality of Life and Health Behaviors After Adjuvant Breast Cancer Chemotherapy. J. Clin. Oncol. 2022, 40, 3190–3204. [Google Scholar]
- Cho, Y.U.; Lee, B.G.; Kim, S.H. Coping style at diagnosis and its association with subsequent health-related quality of life in women with breast cancer: A 3-year follow-up study. Eur. J. Oncol. Nurs. 2020, 45, 101726. [Google Scholar]
- Fayers, P.; Aaronson, N.; Bjordal, K. The EORTC QLQ-C30 Scoring Manual, 3rd ed.; European Organization for Research and Treatment of Cancer: Brussels, Belgium, 2001. [Google Scholar]
- Yun, Y.H.; Park, Y.S.; Lee, E.S.; Bang, S.M.; Heo, D.S.; Park, S.Y.; You, C.H.; Wet, K. Validation of the Korean version of the EORTC QLQ-C30. Qual. Life Res. 2004, 13, 863–868. [Google Scholar]
- Giesinger, J.M.; Loth, F.L.C.; Aaronson, N.K.; Arraras, J.I.; Caocci, G.; Efficace, F.; Groenvold, M.; van Leeuwen, M.; Petersen, M.A.; Ramage, J.; et al. Thresholds for clinical importance were established to improve interpretation of the EORTC QLQ-C30 in clinical practice and research. J. Clin. Epidemiol. 2020, 118, 1–8. [Google Scholar]
- Yun, Y.H.; Kim, S.H.; Lee, K.M.; Park, S.M.; Kim, Y.M. Age, sex, and comorbidities were considered in comparing reference data for health-related quality of life in the general and cancer populations. J. Clin. Epidemiol. 2007, 60, 1164–1175. [Google Scholar]
- Osoba, D.; Rodrigues, G.; Myles, J.; Zee, B.; Pater, J. Interpreting the significance of changes in health-related quality-of-life scores. J. Clin. Oncol. 1998, 16, 139–144. [Google Scholar]
- King, M.T. The interpretation of scores from the EORTC quality of life questionnaire QLQ-C30. Qual. Life Res. 1996, 5, 555–567. [Google Scholar]
- Oh, S.; Min, K.; Park, D. A study on the standardization of the Hospital Anxiety and Depression Scale for Koreans: A comparison of normal, depressed and anxious groups. J. Korean Neuropsychiatr. Assoc. 1999, 38, 289–296. [Google Scholar]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom. Res. 2002, 52, 69–77. [Google Scholar]
- Otte, J.L.; Davis, L.; Carpenter, J.S.; Krier, C.; Skaar, T.C.; Rand, K.L.; Weaver, M.; Landis, C.; Chernyak, Y.; Manchanda, S. Sleep disorders in breast cancer survivors. Support Care Cancer 2016, 24, 4197–4205. [Google Scholar]
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Survivorship. Available online: https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1466 (accessed on 2 March 2023).
- Reinertsen, K.V.; Cvancarova, M.; Loge, J.H.; Edvardsen, H.; Wist, E.; Fossa, S.D. Predictors and course of chronic fatigue in long-term breast cancer survivors. J. Cancer Surviv. 2010, 4, 405–414. [Google Scholar]
- Park, S.C.; Oh, H.S.; Oh, D.H.; Jung, S.A.; Na, K.S.; Lee, H.Y.; Kang, R.H.; Choi, Y.K.; Lee, M.S.; Park, Y.C. Evidence-based, non-pharmacological treatment guideline for depression in Korea. J. Korean Med. Sci. 2014, 29, 12–22. [Google Scholar]
- Lengacher, C.A.; Shelton, M.M.; Reich, R.R.; Barta, M.K.; Johnson-Mallard, V.; Moscoso, M.S.; Paterson, C.; Ramesar, S.; Budhrani, P.; Carranza, I.; et al. Mindfulness based stress reduction (MBSR(BC)) in breast cancer: Evaluating fear of recurrence (FOR) as a mediator of psychological and physical symptoms in a randomized control trial (RCT). J. Behav. Med. 2014, 37, 185–195. [Google Scholar]
- Hewitt, M.; Greenfield, S.; Stovall, E. From Cancer Patient to Cancer Survivor: Lost in Transition: An American Society of Clinical Oncology and Institute of Medicine Symposium; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Chu, W.O.; Dialla, P.O.; Roignot, P.; Bone-Lepinoy, M.C.; Poillot, M.L.; Coutant, C.; Arveux, P.; Dabakuyo-Yonli, T.S. Determinants of quality of life among long-term breast cancer survivors. Qual. Life Res. 2016, 25, 1981–1990. [Google Scholar]
- Schoormans, D.; Czene, K.; Hall, P.; Brandberg, Y. The impact of co-morbidity on health-related quality of life in breast cancer survivors and controls. Acta. Oncol. 2015, 54, 727–734. [Google Scholar]
| Characteristics | Category | n (%) |
|---|---|---|
| Age (years) | <40 | 3 (3.8) |
| 40–49 | 22 (27.5) | |
| 50–59 | 35 (43.7) | |
| ≥60 | 20 (25.0) | |
| Marital status | Married | 65 (81.3) |
| Single | 3 (3.7) | |
| Divorced/widowed | 12 (15.0) | |
| Education (n = 79) | Elementary school | 9 (11.3) |
| Middle school | 17 (21.3) | |
| High school | 42 (52.5) | |
| College or university | 11 (13.8) | |
| Religion | No | 32 (40.0) |
| Yes | 48 (60.0) | |
| Employment status | No | 46 (58.2) |
| Yes | 33 (41.8) | |
| Monthly income (n = 78) | <$2000 | 28 (35.9) |
| ≥$2000 | 50 (64.1) | |
| Menopause (n = 77) | No | 12 (15.6) |
| Yes | 65 (84.4) | |
| Comorbidity 1 | No | 50 (62.5) |
| Yes | 30 (37.5) | |
| Hypertension | 13 (16.3) | |
| Diabetes | 3 (3.8) | |
| Cardiovascular | 4 (5.0) | |
| Musculoskeletal | 5 (6.3) | |
| Thyroid disease | 2 (2.5) | |
| Liver disease | 2 (2.5) | |
| Pulmonary disease | 1 (1.3) | |
| Others | 4 (5.0) | |
| Cancer stage at diagnosis | 0 | 7 (8.7) |
| 1 | 29 (36.3) | |
| 2 | 36 (45.0) | |
| 3 | 8 (10.0) | |
| Type of surgery | Mastectomy | 21 (26.3) |
| Breast-conserving surgery | 59 (73.8) | |
| Chemotherapy | No | 22 (27.5) |
| Yes | 58 (72.5) | |
| Radiation therapy | No | 23 (28.7) |
| Yes | 57 (71.3) | |
| Anti-hormone therapy | No | 18 (22.5) |
| Yes | 62 (77.5) |
| Variables | Year 1 | Year 2 | Year 3 |
|---|---|---|---|
| n (%) | |||
| Lifestyle | |||
| Regular exercise | 50 (62.5) | 51 (63.7) | 51 (63.7) |
| Tobacco use | 8 (10.0) | 3 (3.8) | 1 (1.3) |
| Alcohol consumption | 11 (13.8) | 13 (16.3) | 16 (20.0) |
| Symptoms | |||
| EORTC QLQ-C30 | |||
| Fatigue | 17 (21.3) | 23 (28.7) | 18 (22.5) |
| Nausea/vomiting | 20 (25.0) | 16 (20.0) | 20 (25.0) |
| Pain | 26 (32.5) | 24 (30.0) | 26 (32.5) |
| Dyspnea | 26 (32.5) | 28 (35.0) | 24 (30.0) |
| Insomnia | 18 (22.5) | 16 (20.0) | 14 (17.5) |
| Appetite loss | 3 (3.8) | 5 (6.3) | 4 (5.0) |
| Constipation | 5 (6.3) | 8 (10.0) | 2 (2.5) |
| Diarrhea | 16 (20.0) | 15 (18.8) | 16 (20.0) |
| Financial difficulties | 40 (50.0) | 38 (47.5) | 33 (41.3) |
| HADS | |||
| Anxiety | 26 (32.5) | 19 (23.8) | 22 (27.5) |
| Depression | 23 (28.7) | 22 (27.5) | 19 (23.8) |
| n (%) | |
|---|---|
| Cases with low QOL | |
| Baseline (n = 101) | 57 (56.4) |
| Year 1 (n = 83) | 28 (33.7) |
| Year 2 (n = 86) | 20 (23.3) |
| Year 3 (n = 80) | 18 (22.6) |
| QOL change subgroups | |
| Improved | 38 (47.4) |
| Stable | 24 (30.0) |
| Continuously low | 7 (8.8) |
| Deteriorated | 11 (13.8) |
| Variables | OR | 95% CI | p | |
|---|---|---|---|---|
| Sociodemographic | ||||
| Age ≥ 50 years | 1.263 | 0.418–3.815 | 0.679 | |
| No spouse | 0.968 | 0.272–3.446 | 0.960 | |
| Education < high school | 1.584 | 0.524–4.790 | 0.415 | |
| No religion | 1.062 | 0.362–3.111 | 0.913 | |
| Not employed | 1.152 | 0.399–3.327 | 0.794 | |
| Monthly income < $2000 | 2.065 | 0.713–5.986 | 0.182 | |
| Menopausal | 3.896 | 0.467–32.374 | 0.209 | |
| Having comorbidity | 4.889 | 1.590–15.028 | 0.006 | |
| Clinical | ||||
| Stage 2–3 (ref. stage 0–1) | 1.875 | 0.625–5.629 | 0.262 | |
| MRM (ref. BCS) | 3.015 | 0.991–9.175 | 0.052 | |
| Receiving chemotherapy | 2.209 | 0.572–8.540 | 0.251 | |
| Receiving radiation therapy | 0.547 | 0.181–1.651 | 0.284 | |
| Receiving anti-hormone therapy | 1.021 | 0.289–3.601 | 0.974 | |
| Lifestyle | ||||
| Year 1 | Exercises regularly | 1.015 | 0.037–3.356 | 0.980 |
| Smokes | 1.167 | 0.214–6.348 | 0.858 | |
| Drinks | 0.313 | 0.037–2.653 | 0.287 | |
| Year 2 | Exercises regularly | 1.128 | 0.372–3.425 | 0.831 |
| Smokes | 7.600 | 0.645–89.574 | 0.107 | |
| Drinks | 0.557 | 0.111–2.782 | 0.476 | |
| Year 3 | Exercises regularly | 0.871 | 0.280–2.709 | 0.811 |
| Drinks | 0.677 | 0.169–2.705 | 0.581 | |
| Symptoms | ||||
| Year 1 | Fatigue | 1.603 | 0.479–5.367 | 0.444 |
| Nausea/vomiting | 2.399 | 0.777–7.409 | 0.128 | |
| Pain | 2.647 | 0.900–7.790 | 0.077 | |
| Dyspnea | 3.594 | 1.208–10.688 | 0.021 | |
| Insomnia | 5.889 | 1.840–18.845 | 0.003 | |
| Appetite loss | 1.765 | 0.151–20.658 | 0.651 | |
| Diarrhea | 1.783 | 0.526–6.040 | 0.353 | |
| Financial difficulties | 1.000 | 0.350–2.586 | >0.999 | |
| Anxiety | 3.594 | 1.208–10.688 | 0.021 | |
| Depression | 2.507 | 0.837–7.504 | 0.100 | |
| Year 2 | Fatigue | 13.520 | 3.938–46.423 | <0.001 |
| Nausea/vomiting | 2.600 | 0.790–8.555 | 0.116 | |
| Pain | 5.923 | 1.918–18.295 | 0.002 | |
| Dyspnea | 2.263 | 0.776–6.599 | 0.135 | |
| Insomnia | 3.747 | 1.149–12.221 | 0.028 | |
| Appetite loss | 6.000 | 0.919–39.185 | 0.061 | |
| Diarrhea | 2.000 | 0.582–6.867 | 0.271 | |
| Financial difficulties | 2.037 | 0.697–5.953 | 0.193 | |
| Anxiety | 7.361 | 2.290–23.664 | 0.001 | |
| Depression | 7.286 | 2.307–23.010 | 0.001 | |
| Year 3 | Fatigue | 8.281 | 2.518–27.231 | 0.001 |
| Nausea/vomiting | 4.636 | 1.497–14.361 | 0.008 | |
| Pain | 4.924 | 1.620–14.996 | 0.005 | |
| Dyspnea | 5.923 | 1.918–18.275 | 0.002 | |
| Insomnia | 7.467 | 2.130–26.172 | 0.002 | |
| Appetite loss | 12.200 | 1.184–125.717 | 0.036 | |
| Diarrhea | 1.190 | 0.332–4.271 | 0.789 | |
| Financial difficulties | 2.120 | 0.732–6.136 | 0.166 | |
| Anxiety | 3.769 | 1.245–11.414 | 0.019 | |
| Depression | 7.361 | 2.290–23.664 | 0.001 | |
| Time Points | Variable | aOR | 95% CI | p |
|---|---|---|---|---|
| Year 1 | Insomnia | 5.889 | 1.840–18.845 | 0.003 |
| Year 2 | Fatigue | 22.783 | 4.493–115.515 | <0.001 |
| Anxiety | 13.985 | 2.627–74.461 | 0.002 | |
| Year 3 | Comorbidity | 5.056 | 1.275–20.051 | 0.021 |
| Fatigue | 9.070 | 2.167–37.954 | 0.003 | |
| Depression | 6.540 | 1.641–26.069 | 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-H.; Jo, H.-Y. Factors Associated with Poor Quality of Life in Breast Cancer Survivors: A 3-Year Follow-Up Study. Cancers 2023, 15, 5809. https://doi.org/10.3390/cancers15245809
Kim S-H, Jo H-Y. Factors Associated with Poor Quality of Life in Breast Cancer Survivors: A 3-Year Follow-Up Study. Cancers. 2023; 15(24):5809. https://doi.org/10.3390/cancers15245809
Chicago/Turabian StyleKim, Soo-Hyun, and Ha-Yeon Jo. 2023. "Factors Associated with Poor Quality of Life in Breast Cancer Survivors: A 3-Year Follow-Up Study" Cancers 15, no. 24: 5809. https://doi.org/10.3390/cancers15245809
APA StyleKim, S.-H., & Jo, H.-Y. (2023). Factors Associated with Poor Quality of Life in Breast Cancer Survivors: A 3-Year Follow-Up Study. Cancers, 15(24), 5809. https://doi.org/10.3390/cancers15245809






