Evolution of the Management of Brain Metastases: A Bibliometric Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methodology
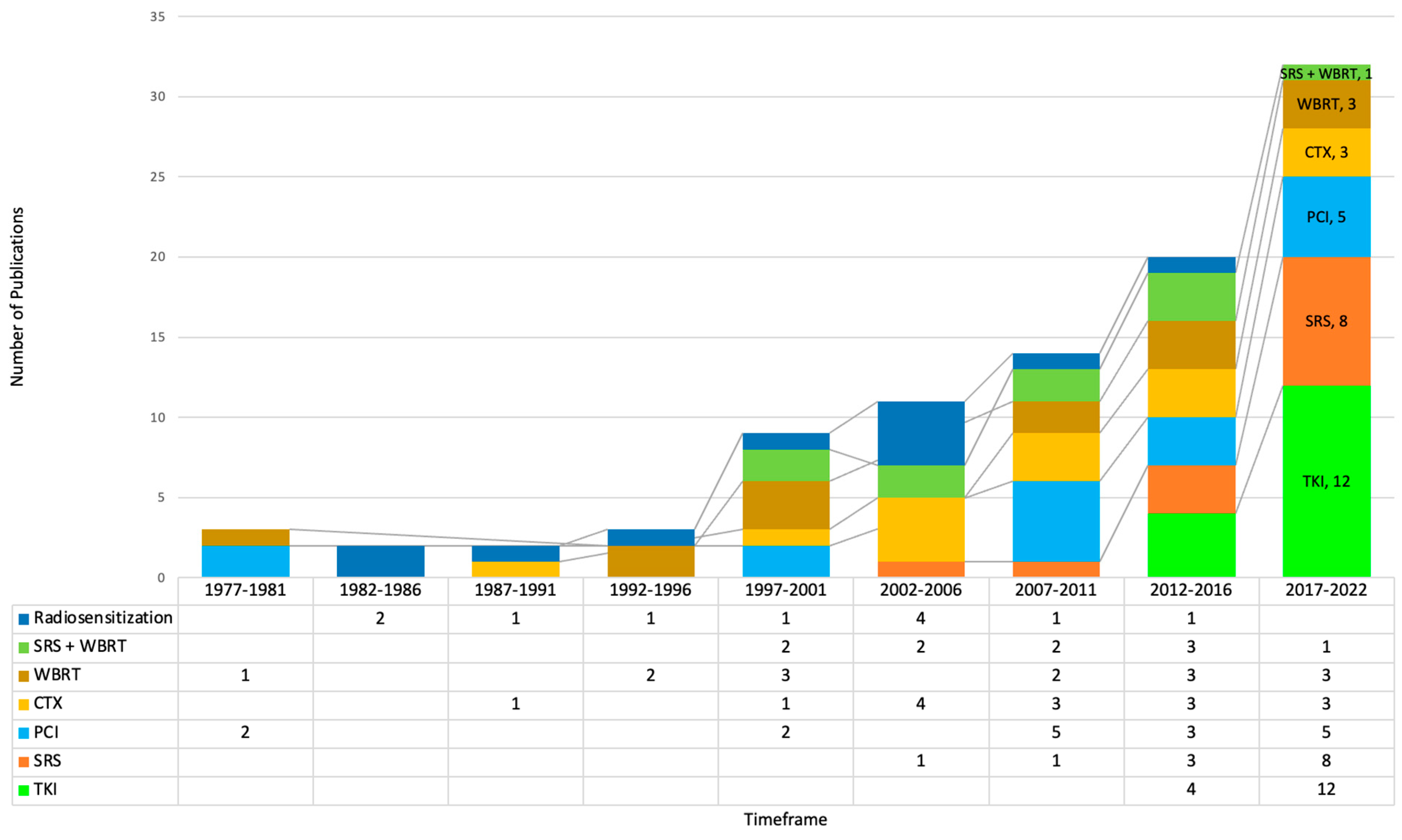
3. Results
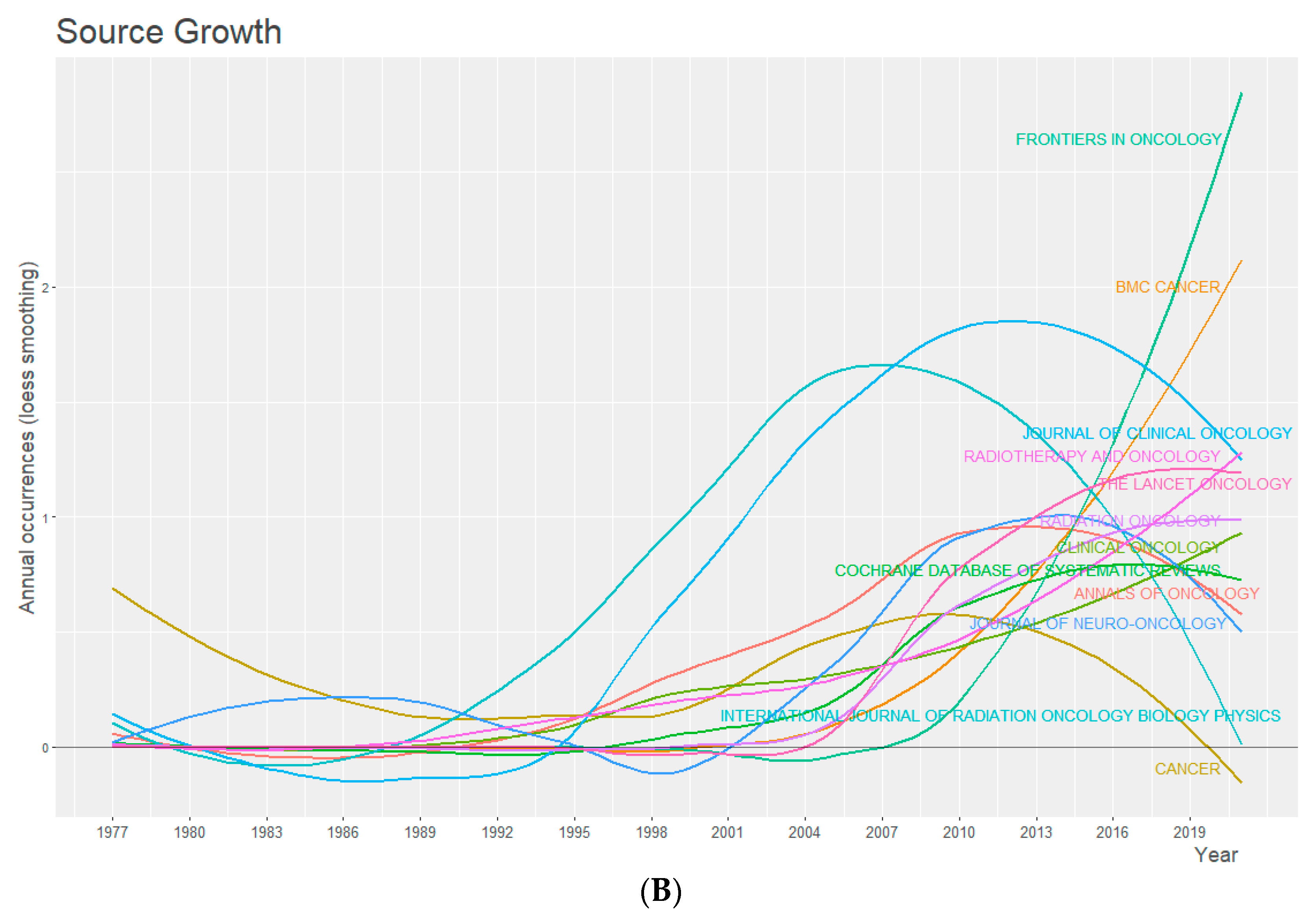
| Journal | Number of Publications | Total Citations | h-Index | Publication Start Year |
|---|---|---|---|---|
| Journal of Clinical Oncology | 37 | 8802 | 33 | 2000 |
| International Journal of Radiation Oncology Biology Physics | 32 | 5781 | 28 | 1997 |
| Frontiers in Oncology | 23 | 152 | 9 | 2012 |
| Annals of Oncology | 19 | 1474 | 15 | 1998 |
| The Lancet Oncology | 17 | 6336 | 16 | 2009 |
| Journal of Neuro-Oncology | 17 | 1110 | 15 | 1984 |
| BMC Cancer | 17 | 521 | 11 | 2007 |
| Cancer | 14 | 1515 | 13 | 1978 |
| Radiotherapy and Oncology | 14 | 470 | 12 | 1997 |
| Radiation Oncology | 13 | 348 | 10 | 2006 |
| Clinical Oncology | 12 | 418 | 9 | 1996 |
| Journal of Neurosurgery | 12 | 518 | 9 | 2006 |
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Vogelbaum, M.A.; Brown, P.D.; Messersmith, H.; Brastianos, P.K.; Burri, S.; Cahill, D.; Dunn, I.F.; Gaspar, L.E.; Gatson, N.T.N.; Gondi, V.; et al. Treatment for Brain Metastases: ASCO-SNO-ASTRO Guideline. Neuro Oncol. 2022, 24, 331–357. [Google Scholar] [CrossRef]
- Cagney, D.N.; Martin, A.M.; Catalano, P.J.; Redig, A.J.; Lin, N.U.; Lee, E.Q.; Wen, P.Y.; Dunn, I.F.; Bi, W.L.; Weiss, S.E. Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: A population-based study. Neuro Oncol. 2017, 19, 1511–1521. [Google Scholar]
- Davis, F.G.; Dolecek, T.A.; McCarthy, B.J.; Villano, J.L. Toward determining the lifetime occurrence of metastatic brain tumors estimated from 2007 United States cancer incidence data. Neuro Oncol. 2012, 14, 1171–1177. [Google Scholar]
- McTyre, E.; Scott, J.; Chinnaiyan, P. Whole brain radiotherapy for brain metastasis. Surg. Neurol. Int. 2013, 4 (Suppl. S4), S236. [Google Scholar]
- Black, P. Brain metastasis: Current status and recommended guidelines for management. Neurosurgery 1979, 5, 617–631. [Google Scholar]
- Sperduto, P.W.; Mesko, S.; Li, J.; Cagney, D.; Aizer, A.; Lin, N.U.; Nesbit, E.; Kruser, T.J.; Chan, J.; Braunstein, S. Survival in patients with brain metastases: Summary report on the updated diagnosis-specific graded prognostic assessment and definition of the eligibility quotient. J. Clin. Oncol. 2020, 38, 3773. [Google Scholar]
- Schimmel, W.C.M.; Gehring, K.; Eekers, D.B.P.; Hanssens, P.E.J.; Sitskoorn, M.M. Cognitive effects of stereotactic radiosurgery in adult patients with brain metastases: A systematic review. Adv. Radiat. Oncol. 2018, 3, 568–581. [Google Scholar]
- Kazda, T.; Jancalek, R.; Pospisil, P.; Sevela, O.; Prochazka, T.; Vrzal, M.; Burkon, P.; Slavik, M.; Hynkova, L.; Slampa, P.; et al. Why and how to spare the hippocampus during brain radiotherapy: The developing role of hippocampal avoidance in cranial radiotherapy. Radiat. Oncol. 2014, 9, 139. [Google Scholar] [CrossRef]
- Katano, A.; Yamashita, H. Brain metastasis: Recent treatment modalities and future-perspectives. Oncol. Lett. 2022, 23, 191. [Google Scholar]
- Sperduto, P.W.; Kased, N.; Roberge, D.; Xu, Z.; Shanley, R.; Luo, X.; Sneed, P.K.; Chao, S.T.; Weil, R.J.; Suh, J. Effect of tumor subtype on survival and the graded prognostic assessment for patients with breast cancer and brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 2111–2117. [Google Scholar]
- Khan, M.; Arooj, S.; Li, R.; Tian, Y.; Zhang, J.; Lin, J.; Liang, Y.; Xu, A.; Zheng, R.; Liu, M.; et al. Tumor Primary Site and Histology Subtypes Role in Radiotherapeutic Management of Brain Metastases. Front. Oncol. 2020, 10, 781. [Google Scholar] [CrossRef]
- Hackshaw, M.D.; Danysh, H.E.; Henderson, M.; Wang, E.; Tu, N.; Islam, Z.; Ladner, A.; Ritchey, M.E.; Salas, M. Prognostic factors of brain metastasis and survival among HER2-positive metastatic breast cancer patients: A systematic literature review. BMC Cancer 2021, 21, 967. [Google Scholar] [CrossRef]
- Brosnan, E.M.; Anders, C. Understanding patterns of brain metastasis in breast cancer and designing rational therapeutic strategies. Ann. Transl. Med. 2018, 6, 163. [Google Scholar] [CrossRef]
- Vaz-Luis, I.; Ottesen, R.; Hughes, M.E.; Marcom, P.K.; Moy, B.; Rugo, H.S.; Theriault, R.L.; Wilson, J.; Niland, J.C.; Weeks, J.C.; et al. Impact of hormone receptor status on patterns of recurrence and clinical outcomes among patients with human epidermal growth factor-2-positive breast cancer in the National Comprehensive Cancer Network: A prospective cohort study. Breast Cancer Res. 2012, 14, R129. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, J.S.; Kim, I.A. Molecular subtype predicts incidence and prognosis of brain metastasis from breast cancer in SEER database. J. Cancer Res. Clin. Oncol. 2018, 144, 1803–1816. [Google Scholar] [CrossRef]
- Sperduto, P.W. A review of stereotactic radiosurgery in the management of brain metastases. Technol. Cancer Res. Treat. 2003, 2, 105–109. [Google Scholar] [CrossRef]
- Huang, R.S.; Harries, L.; Decker, B.; Hiemenz, M.C.; Murugesan, K.; Creeden, J.; Tolba, K.; Stabile, L.P.; Ramkissoon, S.H.; Burns, T.F. Clinicopathologic and Genomic Landscape of Non-Small Cell Lung Cancer Brain Metastases. Oncologist 2022, 27, 839–848. [Google Scholar] [CrossRef]
- Thomsen, B.J.; Soliman, H. The modern management of untreated large (>2 cm) brain metastases: A narrative review. Chin. Clin. Oncol. 2022, 11, 16. [Google Scholar] [CrossRef]
- Bolem, N.; Soon, Y.; Ravi, S.; Dinesh, N.; Teo, K.; Nga, V.D.W.; Lwin, S.; Yeo, T.T.; Vellayappan, B. Is there any survival benefit from post-operative radiation in brain metastases? A systematic review and meta-analysis of randomized controlled trials. J. Clin. Neurosci. 2022, 99, 327–335. [Google Scholar] [CrossRef]
- Tan, X.L.; Le, A.; Lam, F.C.; Scherrer, E.; Kerr, R.G.; Lau, A.C.; Han, J.; Jiang, R.; Diede, S.J.; Shui, I.M. Current Treatment Approaches and Global Consensus Guidelines for Brain Metastases in Melanoma. Front. Oncol. 2022, 12, 885472. [Google Scholar] [CrossRef]
- Nader-Marta, G.; Martins-Branco, D.; de Azambuja, E. How we treat patients with metastatic HER2-positive breast cancer. ESMO Open 2022, 7, 100343. [Google Scholar] [CrossRef]
- Zeng, Q.; Zhang, X.; He, S.; Zhou, Z.; Xia, L.; Zhang, W.; Zeng, L. Crizotinib versus Alectinib for the Treatment of ALK-Positive Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Chemotherapy 2022, 67, 67–80. [Google Scholar] [CrossRef]
- Tosoni, A.; Ermani, M.; Brandes, A.A. The pathogenesis and treatment of brain metastases: A comprehensive review. Crit. Rev. Oncol. Hematol. 2004, 52, 199–215. [Google Scholar] [CrossRef]
- Mok, T.S.; Wu, Y.L.; Ahn, M.J.; Garassino, M.C.; Kim, H.R.; Ramalingam, S.S.; Shepherd, F.A.; He, Y.; Akamatsu, H.; Theelen, W.S.M.E.; et al. Osimertinib or platinum-pemetrexed in EGFR T790M-Positive lung cancer. N. Engl. J. Med. 2017, 376, 629–640. [Google Scholar] [CrossRef]
- Murthy, R.K.; Loi, S.; Okines, A.; Paplomata, E.; Hamilton, E.; Hurvitz, S.A.; Lin, N.U.; Borges, V.; Abramson, V.; Anders, C.; et al. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N. Engl. J. Med. 2020, 382, 597–609. [Google Scholar] [CrossRef]
- Brown, P.D.; Jaeckle, K.; Ballman, K.V.; Farace, E.; Cerhan, J.H.; Keith Anderson, S.; Carrero, X.W.; Barker, F.G.; Deming, R.; Burri, S.H.; et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases a randomized clinical trial. JAMA 2016, 316, 401–409. [Google Scholar] [CrossRef]
- Chang, G.; Shi, L.; Ye, Y.; Shi, H.; Zeng, L.; Tiwary, S.; Huse, J.T.; Huo, L.; Ma, L.; Ma, Y. YTHDF3 induces the translation of m6A-enriched gene transcripts to promote breast cancer brain metastasis. Cancer Cell 2020, 38, 857–871.e7. [Google Scholar] [CrossRef]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. J. Informetr. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Lotka, A.J. The frequency distribution of scientific productivity. J. Wash. Acad. Sci. 1926, 16, 317–323. [Google Scholar]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Bradford, S.C. Sources of information on specific subjects. Engineering 1934, 137, 85–86. [Google Scholar]
- Youngblood, M.; Lahti, D. A bibliometric analysis of the interdisciplinary field of cultural evolution. Palgrave Commun. 2018, 4, 120. [Google Scholar] [CrossRef]
- Abdallah, S.; Wong, A. Brain metastases in non-small-cell lung cancer: Are tyrosine kinase inhibitors and checkpoint inhibitors now viable options? Curr. Oncol. 2018, 25, 103–114. [Google Scholar] [CrossRef]
- Tabouret, E.; Chinot, O.; Metellus, P.; Tallet, A.; Viens, P.; Gonçalves, A. Recent trends in epidemiology of brain metastases: An overview. Anticancer Res. 2012, 32, 4655–4662. [Google Scholar]
- Quan, A.L.; Videtic, G.; Suh, J.H. Brain metastases in small cell lung cancer. Oncology 2004, 18, 961–987. [Google Scholar]
- Della Cuna Robustelli, G.; Pavesi, L.; Knerich, R.; Pretil, P.; Paoletti, P. Radio-chemo-immunotherapy (CCNU plus Levamisole) for treatment of metastatic brain tumors—A pilot study. J Neuro Oncol. 1984, 2, 237–240. [Google Scholar] [CrossRef]
- Eyre, H.J.; Ohlsen, J.D.; Frank, J.; LoBuglio, A.F.; McCracken, J.D.; Weatherall, T.; Mansfield, C. Randomized trial of radiotherapy versus radiotherapy plus metronidazole for the treatment metastatic cancer to brain: A Southwest Oncology Group study. J. Neuro Oncol. 1984, 2, 325–330. [Google Scholar] [CrossRef]
- Mehta, M.P.; Rodrigus, P.; Terhaard, C.; Rao, A.; Suh, J.; Roa, W.; Souhami, L.; Bezjak, A.; Leibenhaut, M.; Komaki, R. Survival and neurologic outcomes in a randomized trial of motexafin gadolinium and whole-brain radiation therapy in brain metastases. J. Clin. Oncol. 2003, 21, 2529–2536. [Google Scholar] [CrossRef]
- Meyers, C.A.; Smith, J.A.; Bezjak, A.; Mehta, M.P.; Liebmann, J.; Illidge, T.; Kunkler, I.; Caudrelier, J.M.; Eisenberg, P.D.; Meerwaldt, J.; et al. Neurocognitive function and progression in patients with brain metastases treated with whole-brain radiation and motexafin gadolinium: Results of a randomized phase III trial. J. Clin. Oncol. 2004, 22, 157–165. [Google Scholar] [CrossRef]
- Mehta, M.P.; Shapiro, W.R.; Phan, S.C.; Gervais, R.; Carrie, C.; Chabot, P.; Patchell, R.A.; Glantz, M.J.; Recht, L.; Langer, C.; et al. Motexafin Gadolinium Combined with Prompt Whole Brain Radiotherapy Prolongs Time to Neurologic Progression in Non-Small-Cell Lung Cancer Patients with Brain Metastases: Results of a Phase III Trial. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 1069–1076. [Google Scholar] [CrossRef]
- Stea, B.; Suh, J.H.; Boyd, A.P.; Cagnoni, P.J.; Shaw, E. Whole-brain radiotherapy with or without efaproxiral for the treatment of brain metastases: Determinants of response and its prognostic value for subsequent survival. Int. J. Radiat. Oncol. Biol. Phys. 2006, 64, 1023–1030. [Google Scholar] [CrossRef]
- Suh, J.H.; Stea, B.; Nabid, A.; Kresl, J.J.; Fortin, A.; Mercier, J.P.; Senzer, N.; Chang, E.L.; Boyd, A.P.; Cagnoni, P.J.; et al. Phase III study of efaproxiral as an adjunct to whole-brain radiation therapy for brain metastases. J. Clin. Oncol. 2006, 24, 106–114. [Google Scholar] [CrossRef]
- Rojas-Puentes, L.L.; Gonzalez-Pinedo, M.; Crismatt, A.; Ortega-Gomez, A.; Gamboa-Vignolle, C.; Nuñez-Gomez, R.; Dorantes-Gallareta, Y.; Arce-Salinas, C.; Arrieta, O. Phase II randomized, double-blind, placebo-controlled study of whole-brain irradiation with concomitant chloroquine for brain metastases. Radiat. Oncol. 2013, 8, 209. [Google Scholar] [CrossRef]
- Brown, P.D.; Gondi, V.; Pugh, S.; Tome, W.A.; Wefel, J.S.; Armstrong, T.S.; Bovi, J.A.; Robinson, C.; Konski, A.; Khuntia, D.; et al. Hippocampal avoidance during whole-brain radiotherapy plus memantine for patients with brain metastases: Phase III trial NRG oncology CC001. J. Clin. Oncol. 2020, 38, 1019–1029. [Google Scholar] [CrossRef]
- De Dios, N.R.; Couñago, F.; Murcia-Mejía, M.; Rico-Oses, M.; Calvo-Crespo, P.; Samper, P.; Vallejo, C.; Luna, J.; Trueba, I.; Sotoca, A.; et al. Randomized Phase III Trial of Prophylactic Cranial Irradiation with or Without Hippocampal Avoidance for Small-Cell Lung Cancer (PREMER): A GICOR-GOECP-SEOR Study. J. Clin. Oncol. 2021, 39, 3118–3127. [Google Scholar] [CrossRef]
- Zindler, J.D.; Bruynzeel, A.M.E.; Eekers, D.B.P.; Hurkmans, C.W.; Swinnen, A.; Lambin, P. Whole brain radiotherapy versus stereotactic radiosurgery for 4-10 brain metastases: A phase III randomised multicentre trial. BMC Cancer 2017, 17, 500. [Google Scholar] [CrossRef]
- Mahajan, A.; Ahmed, S.; McAleer, M.F.; Weinberg, J.S.; Li, J.; Brown, P.; Settle, S.; Prabhu, S.S.; Lang, F.F.; Levine, N.; et al. Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: A single-centre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017, 18, 1040–1048. [Google Scholar] [CrossRef]
- Brown, P.D.; Ballman, K.V.; Cerhan, J.H.; Anderson, S.K.; Carrero, X.W.; Whitton, A.C.; Greenspoon, J.; Parney, I.F.; Laack, N.N.I.; Ashman, J.B.; et al. Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC·3): A multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017, 18, 1049–1060. [Google Scholar] [CrossRef]
- Kayama, T.; Sato, S.; Sakurada, K.; Mizusawa, J.; Nishikawa, R.; Narita, Y.; Sumi, M.; Miyakita, Y.; Kumabe, T.; Sonoda, Y.; et al. Effects of surgery with salvage stereotactic radiosurgery versus surgery with whole-brain radiation therapy in patients with one to four brain metastases (JCOG0504): A Phase III, noninferiority, randomized controlled trial. J. Clin. Oncol. 2018, 36, 3282–3289. [Google Scholar] [CrossRef]
- Raman, S.; Mou, B.; Hsu, F.; Valev, B.; Cheung, A.; Vallières, I.; Ma, R.; McKenzie, M.; Beaton, L.; Rackley, T.; et al. Whole Brain Radiotherapy Versus Stereotactic Radiosurgery in Poor-Prognosis Patients with One to 10 Brain Metastases: A Randomised Feasibility Study. Clin. Oncol. 2020, 32, 442–451. [Google Scholar] [CrossRef]
- Hartgerink, D.; Bruynzeel, A.; Eekers, D.; Swinnen, A.; Hurkmans, C.; Wiggenraad, R.; Swaak-Kragten, A.; Dieleman, E.; Van Der Toorn, P.P.; Oei, B.; et al. A Dutch phase III randomized multicenter trial: Whole brain radiotherapy versus stereotactic radiotherapy for 4-10 brain metastases. Neuro Oncol. Adv. 2021, 3, vdab021. [Google Scholar] [CrossRef]
- Antonadou, D.; Paraskevaidis, M.; Sarris, G.; Coliarakis, N.; Economou, I.; Karageorgis, P.; Throuvalas, N. Phase II randomized trial of temozolomide and concurrent radiotherapy in patients with brain metastases. J. Clin. Oncol. 2002, 20, 3644–3650. [Google Scholar] [CrossRef]
- Verger, E.; Gil, M.; Yaya, R.; Viñolas, N.; Villà, S.; Pujol, T.; Quintó, L.; Graus, F. Temozolomide and concomitant whole brain radiotherapy in patients with brain metastases: A phase II randomized trial. Int. J. Radiat. Oncol. Biol. Phys. 2005, 61, 185–191. [Google Scholar] [CrossRef]
- Chua, D.; Krzakowski, M.; Chouaid, C.; Pallotta, M.G.; Martinez, J.I.; Gottfried, M.; Curran, W.; Throuvalas, N. Whole-brain radiation therapy plus concomitant temozolomide for the treatment of brain metastases from non-small-cell lung cancer: A randomized, open-label phase II study. Clin. Lung Cancer 2010, 11, 176–181. [Google Scholar] [CrossRef]
- Gamboa-Vignolle, C.; Ferrari-Carballo, T.; Arrieta, O.; Mohar, A. Whole-brain irradiation with concomitant daily fixed-dose Temozolomide for brain metastases treatment: A randomised phase II trial. Radiother. Oncol. 2012, 102, 187–191. [Google Scholar] [CrossRef]
- Cortés, J.; Rugo, H.S.; Awada, A.; Twelves, C.; Perez, E.A.; Im, S.; Gómez-Pardo, P.; Schwartzberg, L.S.; Diéras, V.; Yardley, D.A.; et al. Prolonged survival in patients with breast cancer and a history of brain metastases: Results of a preplanned subgroup analysis from the randomized phase III BEACON trial. Breast Cancer Res. Treat. 2017, 165, 329–341. [Google Scholar] [CrossRef]
- Tripathy, D.; Tolaney, S.M.; Seidman, A.D.; Anders, C.K.; Ibrahim, N.; Rugo, H.S.; Twelves, C.; Dieras, V.; Müller, V.; Tagliaferri, M.; et al. ATTAIN: Phase III study of etirinotecan pegol versus treatment of physician’s choice in patients with metastatic breast cancer and brain metastases. Future Oncol. 2019, 15, 2211–2225. [Google Scholar] [CrossRef]
- Tripathy, D.; Tolaney, S.M.; Seidman, A.D.; Anders, C.K.; Ibrahim, N.; Rugo, H.S.; Twelves, C.; Diéras, V.; Müller, V.; Du, Y.; et al. Treatment with Etirinotecan Pegol for Patients with Metastatic Breast Cancer and Brain Metastases: Final Results from the Phase 3 ATTAIN Randomized Clinical Trial. JAMA Oncol. 2022, 8, 1047–1052. [Google Scholar] [CrossRef]
- Long, G.V.; Atkinson, V.; Lo, S.; Sandhu, S.; Guminski, A.D.; Brown, M.P.; Wilmott, J.S.; Edwards, J.; Gonzalez, M.; Scolyer, R.A.; et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: A multicentre randomised phase 2 study. Lancet Oncol. 2018, 19, 672–681. [Google Scholar] [CrossRef]
- Gadgeel, S.M.; Lukas, R.V.; Goldschmidt, J.; Conkling, P.; Park, K.; Cortinovis, D.; de Marinis, F.; Rittmeyer, A.; Patel, J.D.; von Pawel, J.; et al. Atezolizumab in patients with advanced non-small cell lung cancer and history of asymptomatic, treated brain metastases: Exploratory analyses of the phase III OAK study. Lung Cancer 2019, 128, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Di Giacomo, A.M.; Chiarion-Sileni, V.; Del Vecchio, M.; Ferrucci, P.F.; Guida, M.; Quaglino, P.; Guidoboni, M.; Marchetti, P.; Cutaia, O.; Amato, G.; et al. Primary analysis and 4-year follow-up of the phase III NIBIT-M2 trial in melanoma patients with brain metastases. Clin. Cancer Res. 2021, 27, 4737–4745. [Google Scholar] [CrossRef] [PubMed]
- Solomon, B.J.; Bauer, T.M.; Ignatius Ou, S.H.; Liu, G.; Hayashi, H.; Bearz, A.; Penkov, K.; Wu, Y.L.; Arrieta, O.; Jassem, J.; et al. Post Hoc Analysis of Lorlatinib Intracranial Efficacy and Safety in Patients with ALK -Positive Advanced Non-Small-Cell Lung Cancer from the Phase III CROWN Study. J. Clin. Oncol. 2022, 40, 3593. [Google Scholar] [CrossRef] [PubMed]
- Horn, L.; Wang, Z.; Wu, G.; Poddubskaya, E.; Mok, T.; Reck, M.; Wakelee, H.; Chiappori, A.A.; Lee, D.H.; Breder, V.; et al. Ensartinib vs Crizotinib for Patients with Anaplastic Lymphoma Kinase-Positive Non-Small Cell Lung Cancer: A Randomized Clinical Trial. JAMA Oncol. 2021, 7, 1617–1625. [Google Scholar] [CrossRef] [PubMed]
- Camidge, D.R.; Kim, H.R.; Ahn, M.J.; Yang, J.C.H.; Han, J.Y.; Hochmair, M.J.; Lee, K.H.; Delmonte, A.; Garcia Campelo, M.R.; Kim, D.W.; et al. Brigatinib Versus Crizotinib in ALK Inhibitor–Naive Advanced ALK-Positive NSCLC: Final Results of Phase 3 ALTA-1L Trial. J. Thorac. Oncol. 2021, 16, 2091–2108. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Bauer, T.M.; De Marinis, F.; Felip, E.; Goto, Y.; Liu, G.; Mazieres, J.; Kim, D.W.; Mok, T.; Polli, A.; et al. First-line lorlatinib or crizotinib in advanced alk-positive lung cancer. N. Engl. J. Med. 2020, 383, 2018–2029. [Google Scholar] [CrossRef]
- Jiang, S.; Liang, H.; Liu, Z.; Zhao, S.; Liu, J.; Xie, Z.; Wang, W.; Zhang, Y.; Han, B.; He, J.; et al. The Impact of Anlotinib on Brain Metastases of Non-Small Cell Lung Cancer: Post Hoc Analysis of a Phase III Randomized Control Trial (ALTER0303). Oncologist 2020, 25, e870–e874. [Google Scholar] [CrossRef]
- Curigliano, G.; Mueller, V.; Borges, V.; Hamilton, E.; Hurvitz, S.; Loi, S.; Murthy, R.; Okines, A.; Paplomata, E.; Cameron, D.; et al. Tucatinib versus placebo added to trastuzumab and capecitabine for patients with pretreated HER2+ metastatic breast cancer with and without brain metastases (HER2CLIMB): Final overall survival analysis. Ann. Oncol. 2022, 33, 321–329. [Google Scholar] [CrossRef]
- Seligmann, J.F.; Wright-Hughes, A.; Pottinger, A.; Velikova, G.; Oughton, J.B.; Murden, G.; Rizwanullah, M.; Price, C.; Passant, H.; Heudtlass, P.; et al. Lapatinib plus Capecitabine versus Trastuzumab plus Capecitabine in the Treatment of Human Epidermal Growth Factor Receptor 2-positive Metastatic Breast Cancer with Central Nervous System Metastases for Patients Currently or Previously Treated with Trastuzumab (LANTERN): A Phase II Randomised Trial. Clin. Oncol. 2020, 32, 656–664. [Google Scholar] [CrossRef]
- Nishio, M.; Nakagawa, K.; Mitsudomi, T.; Yamamoto, N.; Tanaka, T.; Kuriki, H.; Zeaiter, A.; Tamura, T. Analysis of central nervous system efficacy in the J-ALEX study of alectinib versus crizotinib in ALK-positive non-small-cell lung cancer. Lung Cancer 2018, 121, 37–40. [Google Scholar] [CrossRef]
- Huber, R.M.; Hansen, K.H.; Paz-Ares Rodríguez, L.; West, H.L.; Reckamp, K.L.; Leighl, N.B.; Tiseo, M.; Smit, E.F.; Kim, D.W.; Gettinger, S.N.; et al. Brigatinib in Crizotinib-Refractory ALK+ NSCLC: 2-Year Follow-up on Systemic and Intracranial Outcomes in the Phase 2 ALTA Trial. J. Thorac. Oncol. 2020, 15, 404–415. [Google Scholar] [CrossRef] [PubMed]
- Sainaghi, R.; Köseoglu, M.A.; d’Angella, F.; Mehraliyev, F. Sharing economy: A co-citation analysis. Curr. Issues Tour. 2020, 23, 929–937. [Google Scholar] [CrossRef]
- Ahmad, N.; Naveed, A.; Ahmad, S.; Butt, I. Banking sector performance, profitability, and efficiency: A citation-based systematic literature review. J. Econ. Surv. 2020, 34, 185–218. [Google Scholar] [CrossRef]
- Geetha, N.; Kothainayaki, S. Research Output of Anna University: A Bibliometric Study Based on Scopus Database. Asian J. Inf. Sci. Technol. AJIST 2019, 9, 84–91. [Google Scholar] [CrossRef]
- Ahmad, N.; Aghdam, R.F.; Butt, I.; Naveed, A. Citation-based systematic literature review of energy-growth nexus: An overview of the field and content analysis of the top 50 influential papers. Energy Econ. 2020, 86, 104642. [Google Scholar] [CrossRef]
- Ahmad, N.; Menegaki, A.N.; Al-Muharrami, S. Systematic literature review of tourism growth nexus: An overview of the literature and a content analysis of 100 most influential papers. J. Econ. Surv. 2020, 34, 1068–1110. [Google Scholar] [CrossRef]
- Corbet, S.; Dowling, M.; Gao, X.; Huang, S.; Lucey, B.; Vigne, S.A. An analysis of the intellectual structure of research on the financial economics of precious metals. Resour. Policy 2019, 63, 101416. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burney, I.A.; Aal Hamad, A.H.; Hashmi, S.F.A.; Ahmad, N.; Pervez, N. Evolution of the Management of Brain Metastases: A Bibliometric Analysis. Cancers 2023, 15, 5570. https://doi.org/10.3390/cancers15235570
Burney IA, Aal Hamad AH, Hashmi SFA, Ahmad N, Pervez N. Evolution of the Management of Brain Metastases: A Bibliometric Analysis. Cancers. 2023; 15(23):5570. https://doi.org/10.3390/cancers15235570
Chicago/Turabian StyleBurney, Ikram A., Aya H. Aal Hamad, Syed F. A. Hashmi, Nisar Ahmad, and Nadeem Pervez. 2023. "Evolution of the Management of Brain Metastases: A Bibliometric Analysis" Cancers 15, no. 23: 5570. https://doi.org/10.3390/cancers15235570
APA StyleBurney, I. A., Aal Hamad, A. H., Hashmi, S. F. A., Ahmad, N., & Pervez, N. (2023). Evolution of the Management of Brain Metastases: A Bibliometric Analysis. Cancers, 15(23), 5570. https://doi.org/10.3390/cancers15235570







