Real-World Treatment Outcomes and Safety of Afatinib in Advanced Squamous Cell Lung Cancer Progressed after Platinum-Based Doublet Chemotherapy and Immunotherapy (SPACE Study)
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Patients, and Data Collection
2.2. Treatment
2.3. Data Collection
2.4. Sample Collection and Preparation
2.5. Targeted NGS
2.6. Variant Calling
2.7. Outcomes and Statistical Analyses
3. Results
3.1. Clinicopathological Characteristics of Patients
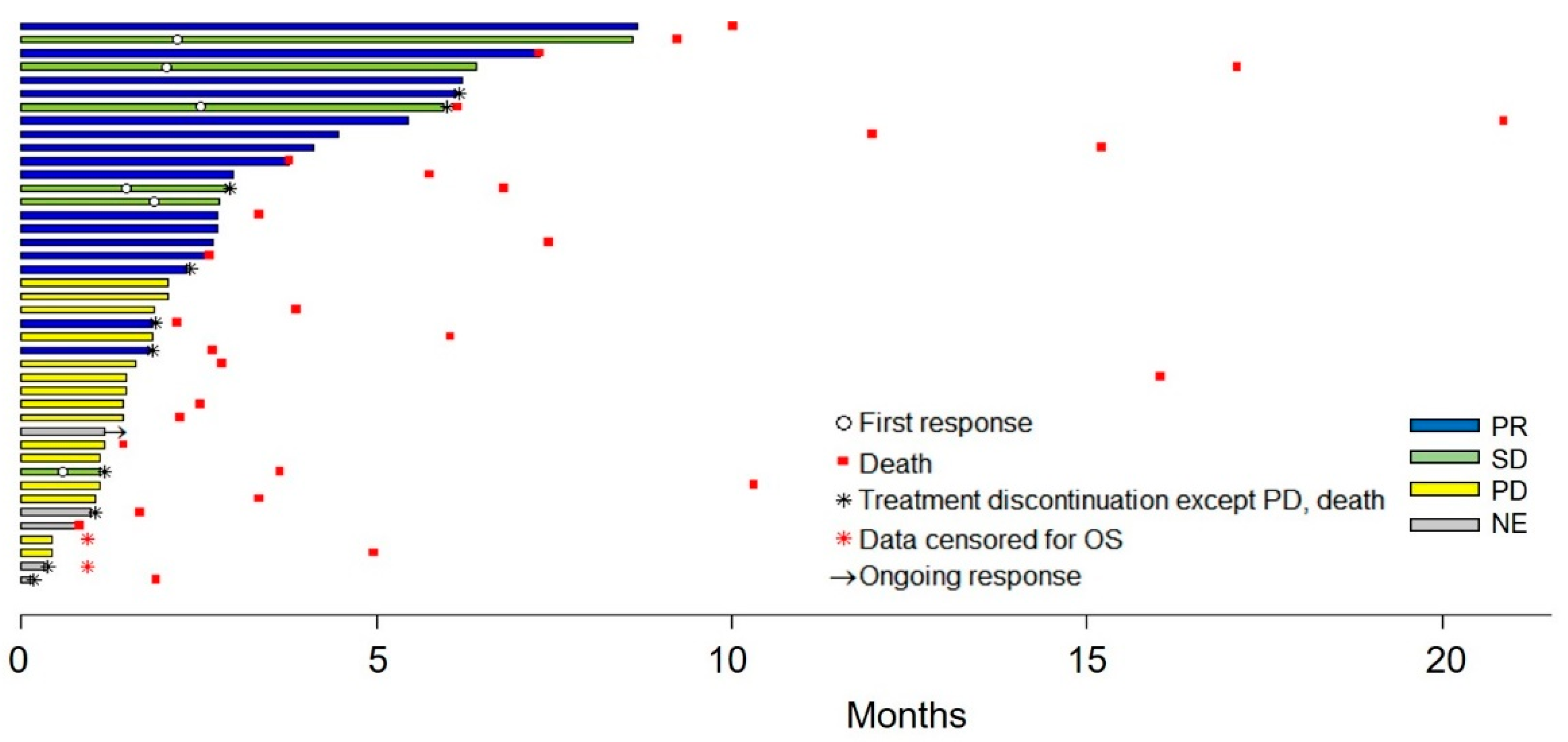
3.2. Treatment Outcomes
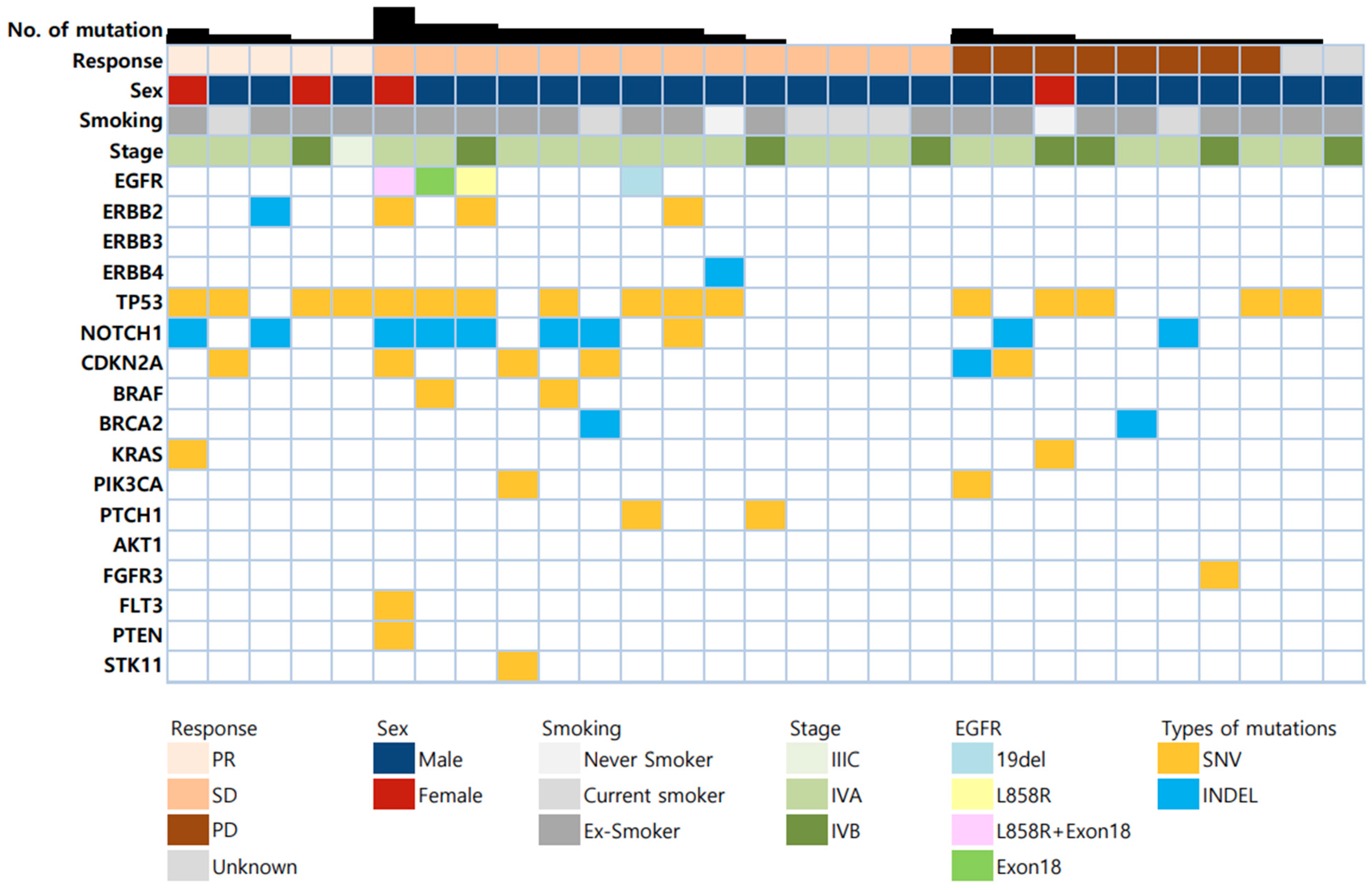
3.3. Explorative Biomarker Analysis
3.4. Safety
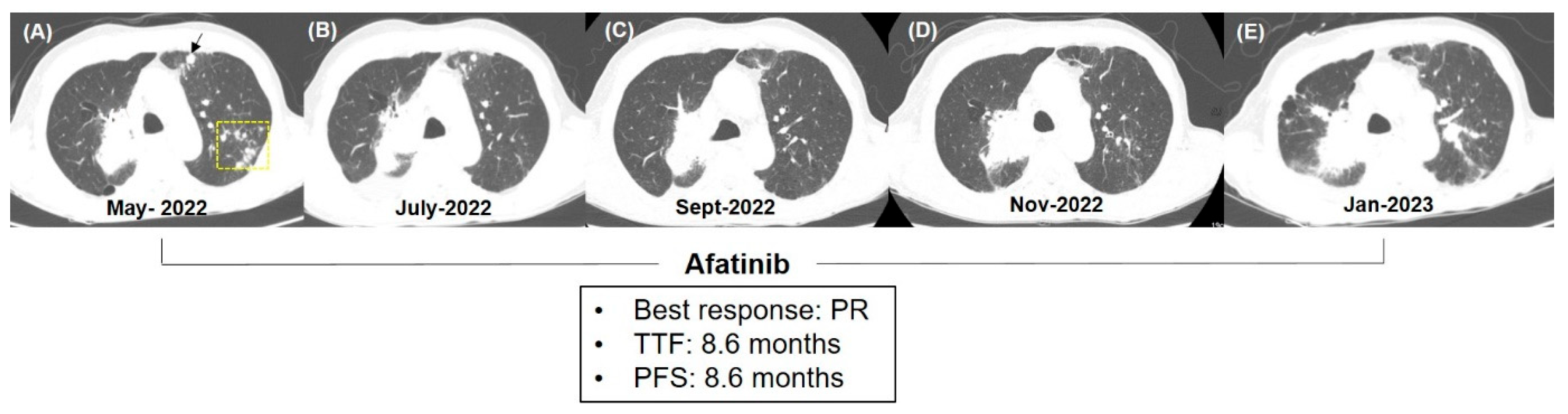
3.5. Clinical Case
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barta, J.A.; Powell, C.A.; Wisnivesky, J.P. Global Epidemiology of Lung Cancer. Ann. Glob. Health 2019, 85, 8. [Google Scholar] [CrossRef] [PubMed]
- Meza, R.; Meernik, C.; Jeon, J.; Cote, M.L. Lung cancer incidence trends by gender, race and histology in the United States, 1973–2010. PLoS ONE 2015, 10, e0121323. [Google Scholar] [CrossRef]
- Soldera, S.V.; Leighl, N.B. Update on the Treatment of Metastatic Squamous Non-Small Cell Lung Cancer in New Era of Personalized Medicine. Front. Oncol. 2017, 7, 50. [Google Scholar] [CrossRef] [PubMed]
- Park, C.K.; Kim, S.J. Trends and Updated Statistics of Lung Cancer in Korea. Tuberc. Respir. Dis. 2019, 82, 175–177. [Google Scholar] [CrossRef]
- Lau, S.C.M.; Pan, Y.; Velcheti, V.; Wong, K.K. Squamous cell lung cancer: Current landscape and future therapeutic options. Cancer Cell 2022, 40, 1279–1293. [Google Scholar] [CrossRef]
- Lahiri, A.; Maji, A.; Potdar, P.D.; Singh, N.; Parikh, P.; Bisht, B.; Mukherjee, A.; Paul, M.K. Lung cancer immunotherapy: Progress, pitfalls, and promises. Mol. Cancer 2023, 22, 40. [Google Scholar] [CrossRef]
- Paz-Ares, L.; Luft, A.; Vicente, D.; Tafreshi, A.; Gumus, M.; Mazieres, J.; Hermes, B.; Cay Senler, F.; Csoszi, T.; Fulop, A.; et al. Pembrolizumab plus Chemotherapy for Squamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 379, 2040–2051. [Google Scholar] [CrossRef]
- Paz-Ares, L.; Vicente, D.; Tafreshi, A.; Robinson, A.; Soto Parra, H.; Mazieres, J.; Hermes, B.; Cicin, I.; Medgyasszay, B.; Rodriguez-Cid, J.; et al. A Randomized, Placebo-Controlled Trial of Pembrolizumab Plus Chemotherapy in Patients With Metastatic Squamous NSCLC: Protocol-Specified Final Analysis of KEYNOTE-407. J. Thorac. Oncol. 2020, 15, 1657–1669. [Google Scholar] [CrossRef]
- Novello, S.; Kowalski, D.M.; Luft, A.; Gumus, M.; Vicente, D.; Mazieres, J.; Rodriguez-Cid, J.; Tafreshi, A.; Cheng, Y.; Lee, K.H.; et al. Pembrolizumab Plus Chemotherapy in Squamous Non-Small-Cell Lung Cancer: 5-Year Update of the Phase III KEYNOTE-407 Study. J. Clin. Oncol. 2023, 41, 1999–2006. [Google Scholar] [CrossRef]
- Friedlaender, A.; Banna, G.; Malapelle, U.; Pisapia, P.; Addeo, A. Next Generation Sequencing and Genetic Alterations in Squamous Cell Lung Carcinoma: Where Are We Today? Front. Oncol. 2019, 9, 166. [Google Scholar] [CrossRef]
- Dearden, S.; Stevens, J.; Wu, Y.L.; Blowers, D. Mutation incidence and coincidence in non small-cell lung cancer: Meta-analyses by ethnicity and histology (mutMap). Ann. Oncol. 2013, 24, 2371–2376. [Google Scholar] [CrossRef] [PubMed]
- Niu, Z.; Jin, R.; Zhang, Y.; Li, H. Signaling pathways and targeted therapies in lung squamous cell carcinoma: Mechanisms and clinical trials. Signal Transduct. Target Ther. 2022, 7, 353. [Google Scholar] [CrossRef] [PubMed]
- Solca, F.; Dahl, G.; Zoephel, A.; Bader, G.; Sanderson, M.; Klein, C.; Kraemer, O.; Himmelsbach, F.; Haaksma, E.; Adolf, G.R. Target binding properties and cellular activity of afatinib (BIBW 2992), an irreversible ErbB family blocker. J. Pharmacol. Exp. Ther. 2012, 343, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Soria, J.C.; Felip, E.; Cobo, M.; Lu, S.; Syrigos, K.; Lee, K.H.; Goker, E.; Georgoulias, V.; Li, W.; Isla, D.; et al. Afatinib versus erlotinib as second-line treatment of patients with advanced squamous cell carcinoma of the lung (LUX-Lung 8): An open-label randomised controlled phase 3 trial. Lancet Oncol. 2015, 16, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Chae, D.K.; Lee, S.H.; Lim, Y.; An, J.; Chae, C.H.; Kim, B.C.; Bhak, J.; Bolser, D.; Cho, D.H. Efficient mutation screening for cervical cancers from circulating tumor DNA in blood. BMC Cancer 2020, 20, 694. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Chae, D.K.; An, J.; Yoo, S.; Jung, S.; Chae, C.H.; Bhak, J.; Kim, B.C.; Cho, D.H. Combinatory Analysis of Cell-free and Circulating Tumor Cell DNAs Provides More Variants for Cancer Treatment. Anticancer. Res. 2019, 39, 6595–6602. [Google Scholar] [CrossRef]
- Chae, Y.K.; Davis, A.A.; Carneiro, B.A.; Chandra, S.; Mohindra, N.; Kalyan, A.; Kaplan, J.; Matsangou, M.; Pai, S.; Costa, R.; et al. Concordance between genomic alterations assessed by next-generation sequencing in tumor tissue or circulating cell-free DNA. Oncotarget 2016, 7, 65364–65373. [Google Scholar] [CrossRef]
- Kim, J.; Weber, J.A.; Jho, S.; Jang, J.; Jun, J.; Cho, Y.S.; Kim, H.M.; Kim, H.; Kim, Y.; Chung, O.; et al. KoVariome: Korean National Standard Reference Variome database of whole genomes with comprehensive SNV, indel, CNV, and SV analyses. Sci. Rep. 2018, 8, 5677. [Google Scholar] [CrossRef]
- Kim, E.S.; Kish, J.K.; Cseh, A.; Moehring, B.; Tang, W.; Terlizzi, E.; Subramanian, J. Second-line Afatinib or Chemotherapy Following Immunochemotherapy for the Treatment of Metastatic, Squamous Cell Carcinoma of the Lung: Real-world Effectiveness and Safety from a Multisite Retrospective Chart Review in the USA. Clin. Lung Cancer 2021, 22, 292–300.e291. [Google Scholar] [CrossRef]
- Borczuk, A.C. Uncommon Types of Lung Carcinoma with Mixed Histology: Sarcomatoid Carcinoma, Adenosquamous Carcinoma, and Mucoepidermoid Carcinoma. Arch. Pathol. Lab. Med. 2018, 142, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.Y.; Wu, Y.L. Effect of Dose Adjustments on the Safety and Efficacy of Afatinib in Chinese Patients with EGFR-Mutated Non-Small Cell Lung Cancer Who Participated in the LUX-Lung Clinical Trial Program. Oncol. Targets Ther. 2020, 13, 12539–12547. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Du, X.; Chen, K.; Li, S.; Yu, Z.; Wu, Z.; Yang, L.; Chen, D.; Liu, W. Impact of Dose Reduction of Afatinib Used in Patients with Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2021, 12, 781084. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, F.R.; Varella-Garcia, M.; Bunn, P.A., Jr.; Di Maria, M.V.; Veve, R.; Bremmes, R.M.; Baron, A.E.; Zeng, C.; Franklin, W.A. Epidermal growth factor receptor in non-small-cell lung carcinomas: Correlation between gene copy number and protein expression and impact on prognosis. J. Clin. Oncol. 2003, 21, 3798–3807. [Google Scholar] [CrossRef]
- Lopez-Malpartida, A.V.; Ludena, M.D.; Varela, G.; Garcia Pichel, J. Differential ErbB receptor expression and intracellular signaling activity in lung adenocarcinomas and squamous cell carcinomas. Lung Cancer 2009, 65, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Heinmoller, P.; Gross, C.; Beyser, K.; Schmidtgen, C.; Maass, G.; Pedrocchi, M.; Ruschoff, J. HER2 status in non-small cell lung cancer: Results from patient screening for enrollment to a phase II study of herceptin. Clin. Cancer Res. 2003, 9, 5238–5243. [Google Scholar] [CrossRef]
- Ugocsai, K.; Mandoky, L.; Tiszlavicz, L.; Molnar, J. Investigation of HER2 overexpression in non-small cell lung cancer. Anticancer. Res. 2005, 25, 3061–3066. [Google Scholar]
- Goss, G.D.; Felip, E.; Cobo, M.; Lu, S.; Syrigos, K.; Lee, K.H.; Goker, E.; Georgoulias, V.; Li, W.; Guclu, S.; et al. Association of ERBB Mutations with Clinical Outcomes of Afatinib- or Erlotinib-Treated Patients with Lung Squamous Cell Carcinoma: Secondary Analysis of the LUX-Lung 8 Randomized Clinical Trial. JAMA Oncol. 2018, 4, 1189–1197. [Google Scholar] [CrossRef]
- Joshi, A.; Zanwar, S.; Noronha, V.; Patil, V.M.; Chougule, A.; Kumar, R.; Janu, A.; Mahajan, A.; Kapoor, A.; Prabhash, K. EGFR mutation in squamous cell carcinoma of the lung: Does it carry the same connotation as in adenocarcinomas? Oncol. Targets Ther. 2017, 10, 1859–1863. [Google Scholar] [CrossRef]
- Sun, Y.; Yin, X.; Wen, M.M.; Zhang, J.; Wang, X.J.; Xia, J.H.; Zhang, Y.N.; Zhang, Z.P.; Li, X.F. EGFR mutations subset in Chinese lung squamous cell carcinoma patients. Mol. Med. Rep. 2018, 17, 7575–7584. [Google Scholar] [CrossRef]
- Suzawa, K.; Toyooka, S.; Sakaguchi, M.; Morita, M.; Yamamoto, H.; Tomida, S.; Ohtsuka, T.; Watanabe, M.; Hashida, S.; Maki, Y.; et al. Antitumor effect of afatinib, as a human epidermal growth factor receptor 2-targeted therapy, in lung cancers harboring HER2 oncogene alterations. Cancer Sci. 2016, 107, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Gow, C.H.; Liao, W.Y.; Liu, Y.N.; Shih, J.Y. Discordant HER2 Exon 20 Mutation Status Determines a Differential Sensitivity to Afatinib. J. Thorac. Oncol. 2015, 10, e58–e60. [Google Scholar] [CrossRef] [PubMed][Green Version]
- De Greve, J.; Teugels, E.; Geers, C.; Decoster, L.; Galdermans, D.; De Mey, J.; Everaert, H.; Umelo, I.; In’t Veld, P.; Schallier, D. Clinical activity of afatinib (BIBW 2992) in patients with lung adenocarcinoma with mutations in the kinase domain of HER2/neu. Lung Cancer 2012, 76, 123–127. [Google Scholar] [CrossRef]
- Santos, E.S.; Hart, L. Advanced Squamous Cell Carcinoma of the Lung: Current Treatment Approaches and the Role of Afatinib. Oncol. Targets Ther. 2020, 13, 9305–9321. [Google Scholar] [CrossRef]
- Tathineni, P.; Joshi, N.; Jelinek, M.J. Current State and Future Directions of EGFR-Directed Therapy in Head and Neck Cancer. Curr. Treat Options Oncol. 2023, 24, 680–692. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Cheng, B.; Chen, Z.; Li, J.; Liang, H.; Chen, Y.; Zhu, F.; Li, C.; Xu, K.; Xiong, S.; et al. Toxicity profile of epidermal growth factor receptor tyrosine kinase inhibitors for patients with lung cancer: A systematic review and network meta-analysis. Crit. Rev. Oncol. Hematol. 2021, 160, 103305. [Google Scholar] [CrossRef]
- Yang, J.C. Afatinib for the treatment of non-small-cell lung cancer with unusual EGFR mutations: A plain language summary. Future Oncol. 2023, 19, 291–297. [Google Scholar] [CrossRef]
- Lee, S.Y.; Choi, C.M.; Chang, Y.S.; Lee, K.Y.; Kim, S.J.; Yang, S.H.; Ryu, J.S.; Lee, J.E.; Lee, S.Y.; Park, J.Y.; et al. Real-world experience of afatinib as first-line therapy for advanced EGFR mutation-positive non-small cell lung cancer in Korea. Transl. Lung Cancer Res. 2021, 10, 4353–4367. [Google Scholar] [CrossRef]
- Nakamura, A.; Tanaka, H.; Saito, R.; Suzuki, A.; Harada, T.; Inoue, S.; Yamada, T.; Nakagawa, T.; Jingu, D.; Sugawara, S. Phase II Study of Low-Dose Afatinib Maintenance Treatment Among Patients with EGFR-Mutated Non-Small Cell Lung Cancer: North Japan Lung Cancer Study Group Trial 1601 (NJLCG1601). Oncologist 2020, 25, e1451–e1456. [Google Scholar] [CrossRef]
- Noro, R.; Igawa, S.; Bessho, A.; Hirose, T.; Shimokawa, T.; Nakashima, M.; Minato, K.; Seki, N.; Tokito, T.; Harada, T.; et al. A prospective, phase II trial of monotherapy with low-dose afatinib for patients with EGFR, mutation-positive, non-small cell lung cancer: Thoracic oncology research group 1632. Lung Cancer 2021, 161, 49–54. [Google Scholar] [CrossRef]
- Yokoyama, T.; Yoshioka, H.; Fujimoto, D.; Demura, Y.; Hirano, K.; Kawai, T.; Kagami, R.; Washio, Y.; Ishida, T.; Kogo, M.; et al. A phase II study of low starting dose of afatinib as first-line treatment in patients with EGFR mutation-positive non-small-cell lung cancer (KTORG1402). Lung Cancer 2019, 135, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Oxnard, G.R.; Yang, J.C.; Yu, H.; Kim, S.W.; Saka, H.; Horn, L.; Goto, K.; Ohe, Y.; Mann, H.; Thress, K.S.; et al. TATTON: A multi-arm, phase Ib trial of osimertinib combined with selumetinib, savolitinib, or durvalumab in EGFR-mutant lung cancer. Ann. Oncol. 2020, 31, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Oshima, Y.; Tanimoto, T.; Yuji, K.; Tojo, A. EGFR-TKI-Associated Interstitial Pneumonitis in Nivolumab-Treated Patients with Non-Small Cell Lung Cancer. JAMA Oncol. 2018, 4, 1112–1115. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, A.J.; Arbour, K.C.; Rizvi, H.; Iqbal, A.N.; Gadgeel, S.M.; Girshman, J.; Kris, M.G.; Riely, G.J.; Yu, H.A.; Hellmann, M.D. Severe immune-related adverse events are common with sequential PD-(L)1 blockade and osimertinib. Ann. Oncol. 2019, 30, 839–844. [Google Scholar] [CrossRef]

| No. of Patients (%) | |
|---|---|
| Age (Years) | |
| Median (range) | 69 (41–85) |
| <70 | 22 (52.4) |
| ≥70 | 20 (47.6) |
| Sex | |
| Male | 38 (90.5) |
| Female | 4 (9.5) |
| Smoking status | |
| Never | 2 (4.7) |
| Former | 7 (16.7) |
| Current | 33 (78.6) |
| Smoking intensity | |
| <30 pack-years | 12 (28.6) |
| ≥30 pack-years | 30 (71.4) |
| ECOG PS | |
| 0, 1 | 33 (78.6) |
| ≥2 | 9 (21.4) |
| Differentiation | |
| Well, moderate | 20 (47.6) |
| Poor | 7 (16.7) |
| Unknown | 15 (35.7) |
| Number of previous lines of systemic therapy before afatinib | |
| Median (range) | 3 (1–8) |
| 1 | 4 (9.5) |
| 2 | 13 (30.9) |
| 3 | 12 (28.6) |
| ≥4 | 13 (30.9) |
| Types of previous systemic therapy | |
| Platinum-doublet followed by immunotherapy | 35 (83.3) |
| Chemoimmunotherapy | 6 (14.3) |
| Immunotherapy followed by platinum-doublet | 1 (2.4) |
| Stage | |
| IIIC | 1 (2.4) |
| IVA | 29 (69.1) |
| IVB | 12 (28.6) |
| Metastasis sites | |
| Brain | 8 (19.1) |
| Lung | 21 (50.0) |
| Liver | 8 (19.1) |
| Bone | 14 (33.3) |
| Pleura | 17 (40.5) |
| Adrenal gland | 1 (2.4) |
| Extrathoracic lymph nodes | 22 (52.4) |
| Mediastinal lymph nodes | 13 (30.9) |
| Number of involved organs | |
| <3 | 24 (57.1) |
| ≥3 | 18 (42.9) |
| PD-L1 TPS | |
| <1% | 13 (30.9) |
| 1–49% | 14 (33.3) |
| ≥50% | 14 (33.3) |
| Unknown | 1 (2.4) |
| Afatinib starting dose | |
| 30 mg | 10 (23.8) |
| 40 mg | 32 (76.2) |
| Dose modification | |
| No | 24 (57.1) |
| Yes | 18 (42.9) |
| Variables | No. of Patients (%) |
|---|---|
| Ongoing Treatment | 1 |
| Reason for cessation of treatment | 41 |
| Progression | 27 |
| Adverse events | 5 |
| Withdrawal of consent | 2 |
| Death | 4 |
| Researchers’ decision | 3 |
| Best response | |
| CR | 0 (0) |
| PR | 6 (12.2) |
| SD | 16 (32.7) |
| PD | 15 (30.6) |
| NE | 5 (24.5) |
| Objective response rate, % | 16.2 |
| Disease control rate, % | 59.5 |
| Follow-up duration, months, median (95% CI) | 8.6 (1.0–21.0) |
| Duration of response, median (95% CI) | 4.0 (0.9–6.4) |
| TTF, months, median (95% CI) | 2.1 (1.5–2.8) |
| PFS, months, median (95% CI) | 2.6 (1.8–3.8) |
| OS, months, median (95% CI) | 6.1 (3.6–10.0) |
| Alive | 10 |
| Death | 30 |
| Lost to follow-up | 1 |
| Mutations | No. of Patients | Disease Control | TTF | PFS | OS | ||||
|---|---|---|---|---|---|---|---|---|---|
| DCR (%) | p-Value | Median (95% CI) | p-Value | Median (95% CI) | p-Value | Median (95% CI) | p-Value | ||
| EGFR | 0.286 | 0.306 | 0.199 | 0.249 | |||||
| Negative | 25 | 65.2 | 2.1 (1.6–3.0) | 2.6 (1.9–3.8) | 6.1 (2.8–10.0) | ||||
| Positive | 4 | 100 | 5.2 (2.3-7.3) | 5.9 (4.0-7.3) | 15.2 (7.3–NE) | ||||
| ERBB2 | 0.286 | 0.045 | 0.134 | 0.781 | |||||
| Negative | 25 | 65.2 | 2.1 (1.6–2.9) | 2.6 (1.9–4.0) | 6.8 (2.8–11.9) | ||||
| Positive | 4 | 100 | 6.8 (3.8–8.6) | 6.6 (3.8-8.6) | 8.7 (3.8–NE) | ||||
| ERBB4 | >0.999 | 0.868 | 0.483 | 0.167 | |||||
| Negative | 28 | 69.2 | 2.5 (1.8–3.8) | 3.5 (2.0–5.3) | 6.8 (3.7–10.3) | ||||
| Positive | 1 | 100 | 2.8 (NE–NE) | 2.6 (NE–NE) | NR | ||||
| Any ERBB | 0.068 | 0.101 | 0.113 | 0.156 | |||||
| Negative | 22 | 60.0 | 2.0 (1.5–2.9) | 2.4 (1.6–4.5) | 6.0 (2.7–10.3) | ||||
| Positive | 7 | 100 | 4.1 (2.3–7.3) | 5.9 (2.6–8.6) | 15.2 (3.8–NE) | ||||
| Patient No. | ERBB Mutations | Sex/Age | Stage | Prev Lines of Tx | Starting Dose of Afatinib (mg) | ORR | DoR | TTF | PFS | OS | Reason of Discontinuation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| S1P03 | EGFR exon 18 and L858R ERBB2 | F/69 | IVA | 8 | 40 | SD | - | 7.3 | 7.3 | 7.3 | Death |
| S1P07 | ERBB2 | M/68 | IVA | 3 | 40 | PR | 6.4 | 8.6 | 8.6 | 9.2 | PD |
| S1P12 | EGFR exon 18 | M/85 | IVA | 2 | 40 | SD | - | 2.3 | 4.9 | 4.9 | Death |
| S2R14 | ERBB4 | M/73 | IVA | 2 | 40 | SD | - | 2.8 | 2.6 | 17.4 | PD |
| S3P03 | EGFR exon 19del | M/54 | IVA | 5 | 40 | SD | - | 4.1 | 4.0 | 15.2 | PD |
| S3P06 | ERBB2 | M/75 | IVA | 5 | 40 | SD | - | 3.8 | 3.8 | 3.8 | Death |
| S4P03 | ERBB2 | M/67 | IVB | 2 | 40 | SD | - | 6.2 | 5.9 | 16.9 | PD |
| Any Grade | Grade 1 or 2 | Grade 3 | Grade 4 | Grade 5 | |
|---|---|---|---|---|---|
| No. of Patients (%) | |||||
| TRAEs * | 22 (52.4) | 19 (45.2) | 3 (7.1) | 0 | 0 |
| TRAEs leading to dose modification | 17 (40.5) | 14 (33.3) | 3 (7.1) | 0 | 0 |
| TRAEs leading to discontinuation of therapy | 4 (9.5) | 2 (4.8) | 2 (4.8) | 0 | 0 |
| Types of TRAEs | |||||
| Diarrhea | 16 (38.1) | 16 (38.1) | 0 | 0 | 0 |
| Stomatitis | 10 (23.8) | 9 (21.4) | 1 (2.4) | 0 | 0 |
| Paronychia | 5 (11.9) | 4 (9.5) | 1 (2.4) | 0 | 0 |
| Acneiform dermatitis | 4 (9.5) | 4 (9.5) | 0 | 0 | 0 |
| Pneumonia/pneumonitis | 2 (4.8) | 0 | 2 (4.8) | 0 | 0 |
| Elevated liver enzyme | 1 (2.4) | 1 (2.4) | 0 | 0 | 0 |
| Anorexia | 1 (2.4) | 1 (2.4) | 0 | 0 | 0 |
| Itching | 1 (2.4) | 1 (2.4) | 0 | 0 | 0 |
| Nausea | 1 (2.4) | 1 (2.4) | 0 | 0 | 0 |
| Epigastric pain | 1 (2.4) | 1 (2.4) | 0 | 0 | 0 |
| Fatigue | 1 (2.4) | 0 | 1 (2.4) | 0 | 0 |
| irAEs | 0 | 0 | 0 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ji, W.; Oh, I.-J.; Park, C.-K.; Lee, S.Y.; Choi, J.; Lee, J.C.; Kim, J.; Lee, S.H. Real-World Treatment Outcomes and Safety of Afatinib in Advanced Squamous Cell Lung Cancer Progressed after Platinum-Based Doublet Chemotherapy and Immunotherapy (SPACE Study). Cancers 2023, 15, 5568. https://doi.org/10.3390/cancers15235568
Ji W, Oh I-J, Park C-K, Lee SY, Choi J, Lee JC, Kim J, Lee SH. Real-World Treatment Outcomes and Safety of Afatinib in Advanced Squamous Cell Lung Cancer Progressed after Platinum-Based Doublet Chemotherapy and Immunotherapy (SPACE Study). Cancers. 2023; 15(23):5568. https://doi.org/10.3390/cancers15235568
Chicago/Turabian StyleJi, Wonjun, In-Jae Oh, Cheol-Kyu Park, Sung Yong Lee, Juwhan Choi, Jae Cheol Lee, Jiwon Kim, and Seung Hyeun Lee. 2023. "Real-World Treatment Outcomes and Safety of Afatinib in Advanced Squamous Cell Lung Cancer Progressed after Platinum-Based Doublet Chemotherapy and Immunotherapy (SPACE Study)" Cancers 15, no. 23: 5568. https://doi.org/10.3390/cancers15235568
APA StyleJi, W., Oh, I.-J., Park, C.-K., Lee, S. Y., Choi, J., Lee, J. C., Kim, J., & Lee, S. H. (2023). Real-World Treatment Outcomes and Safety of Afatinib in Advanced Squamous Cell Lung Cancer Progressed after Platinum-Based Doublet Chemotherapy and Immunotherapy (SPACE Study). Cancers, 15(23), 5568. https://doi.org/10.3390/cancers15235568









