A Deep Learning Approach for Automatic Segmentation during Daily MRI-Linac Radiotherapy of Glioblastoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Patients and MRI-Linac Treatment
2.2. Imaging Acquisition and Tumor Delineation
2.3. Deep Learning Network for Auto-Segmentation of Tumor and Resection Cavity
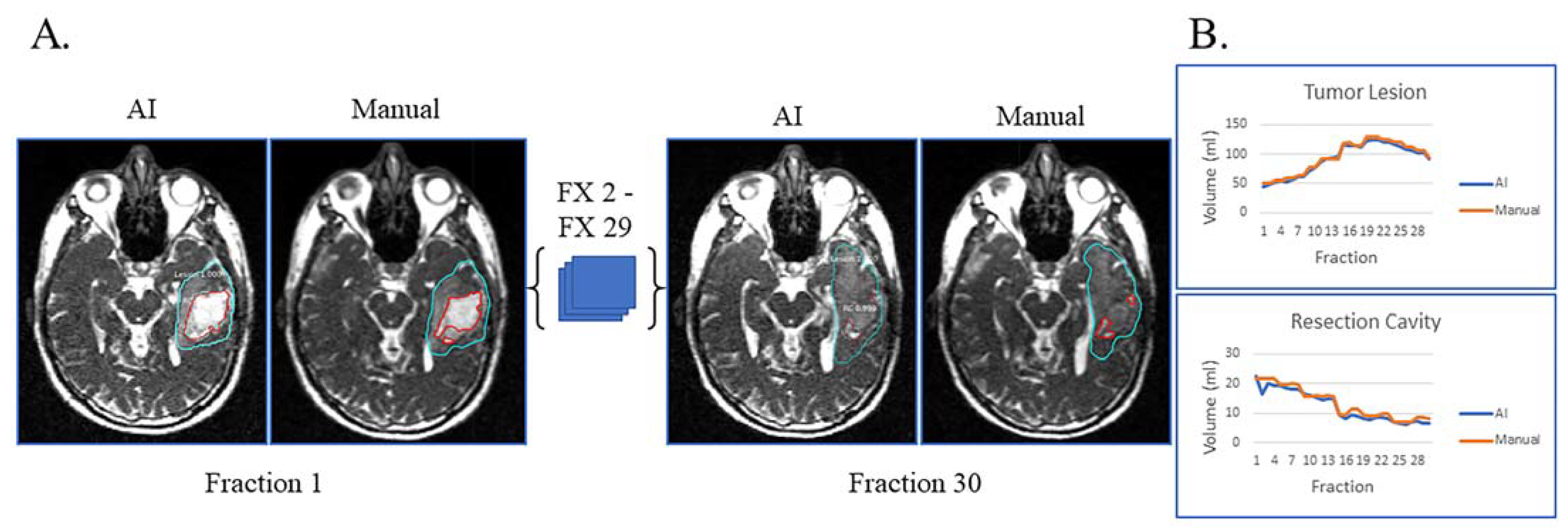
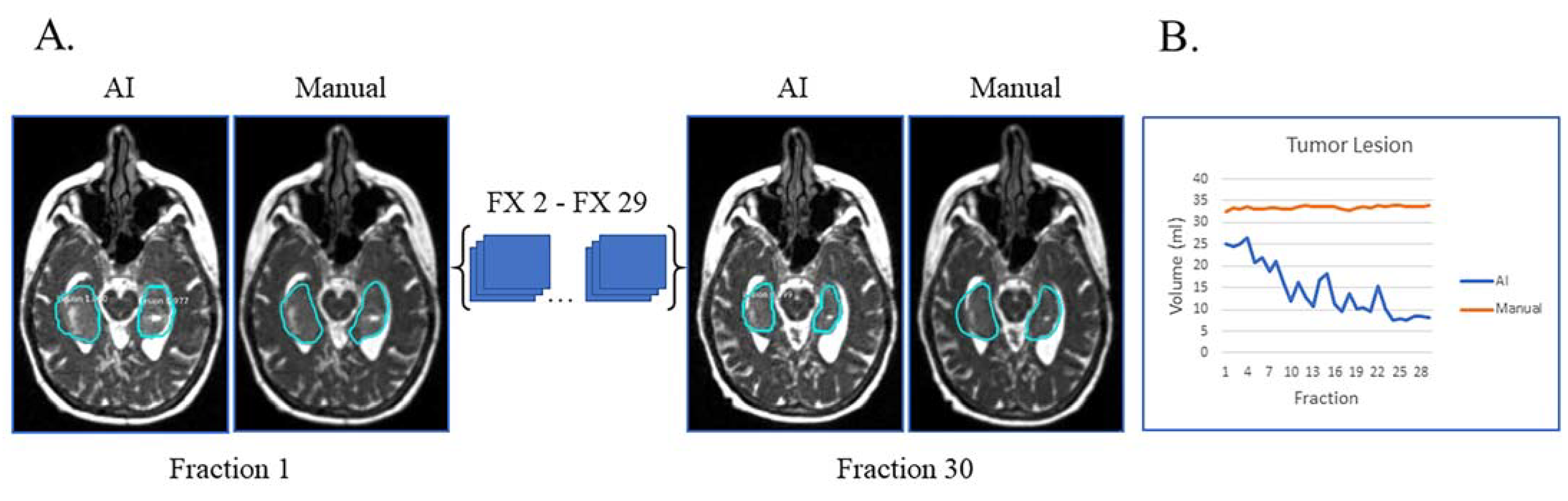
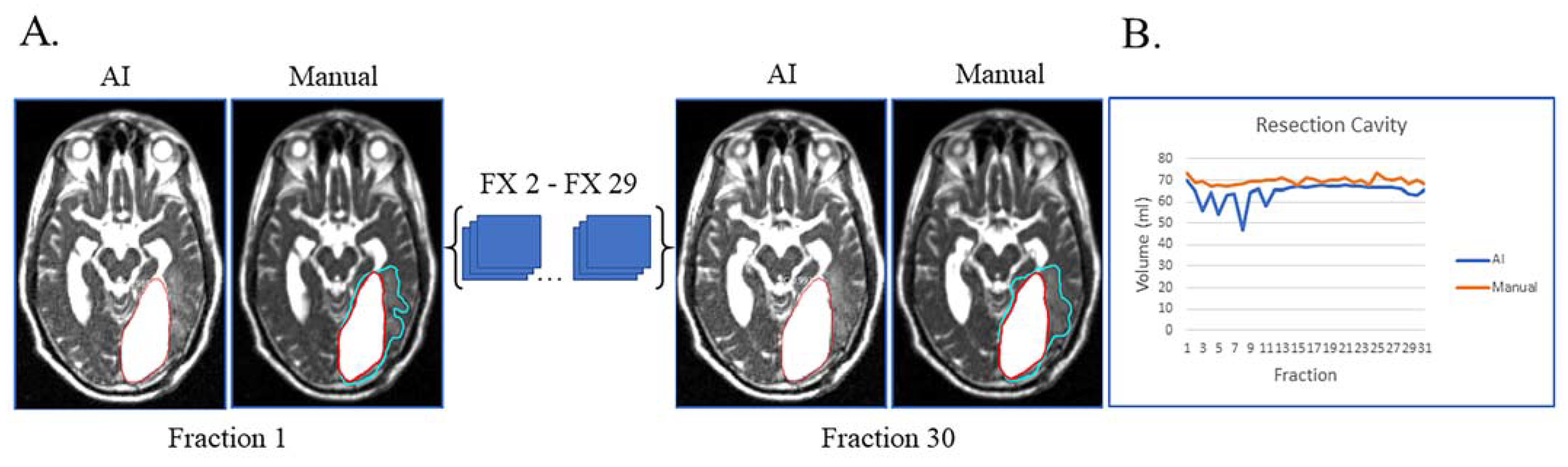
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hanif, F.; Muzaffar, K.; Perveen, K.; Malhi, S.M.; Simjee Sh, U. Glioblastoma Multiforme: A Review of its Epidemiology and Pathogenesis through Clinical Presentation and Treatment. Asian Pac. J. Cancer Prev. 2017, 18, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Ohka, F.; Natsume, A.; Wakabayashi, T. Current trends in targeted therapies for glioblastoma multiforme. Neurol. Res. Int. 2012, 2012, 878425. [Google Scholar] [CrossRef] [PubMed]
- Brandes, A.A.; Franceschi, E.; Tosoni, A.; Blatt, V.; Pession, A.; Tallini, G.; Bertorelle, R.; Bartolini, S.; Calbucci, F.; Andreoli, A.; et al. MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J. Clin. Oncol. 2008, 26, 2192–2197. [Google Scholar] [CrossRef] [PubMed]
- Wallner, K.E.; Galicich, J.H.; Krol, G.; Arbit, E.; Malkin, M.G. Patterns of failure following treatment for glioblastoma multiforme and anaplastic astrocytoma. Int. J. Radiat. Oncol. Biol. Phys. 1989, 16, 1405–1409. [Google Scholar] [CrossRef]
- Gaspar, L.E.; Fisher, B.J.; Macdonald, D.R.; LeBer, D.V.; Halperin, E.C.; Schold, S.C., Jr.; Cairncross, J.G. Supratentorial malignant glioma: Patterns of recurrence and implications for external beam local treatment. Int. J. Radiat. Oncol. Biol. Phys. 1992, 24, 55–57. [Google Scholar] [CrossRef]
- Farjam, R.; Tsien, C.I.; Feng, F.Y.; Gomez-Hassan, D.; Hayman, J.A.; Lawrence, T.S.; Cao, Y. Physiological imaging-defined, response-driven subvolumes of a tumor. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 1383–1390. [Google Scholar] [CrossRef]
- Farjam, R.; Tsien, C.I.; Feng, F.Y.; Gomez-Hassan, D.; Hayman, J.A.; Lawrence, T.S.; Cao, Y. Investigation of the diffusion abnormality index as a new imaging biomarker for early assessment of brain tumor response to radiation therapy. Neuro Oncol. 2014, 16, 131–139. [Google Scholar] [CrossRef]
- Stewart, J.; Sahgal, A.; Lee, Y.; Soliman, H.; Tseng, C.L.; Detsky, J.; Husain, Z.; Ho, L.; Das, S.; Maralani, P.J.; et al. Quantitating Interfraction Target Dynamics During Concurrent Chemoradiation for Glioblastoma: A Prospective Serial Imaging Study. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 736–746. [Google Scholar] [CrossRef]
- Mehta, S.; Gajjar, S.R.; Padgett, K.R.; Asher, D.; Stoyanova, R.; Ford, J.C.; Mellon, E.A. Daily Tracking of Glioblastoma Resection Cavity, Cerebral Edema, and Tumor Volume with MRI-Guided Radiation Therapy. Cureus 2018, 10, e2346. [Google Scholar] [CrossRef]
- Guevara, B.; Cullison, K.; Maziero, D.; Azzam, G.A.; De La Fuente, M.I.; Brown, K.; Valderrama, A.; Meshman, J.; Breto, A.; Ford, J.C.; et al. Simulated Adaptive Radiotherapy for Shrinking Glioblastoma Resection Cavities on a Hybrid MRI-Linear Accelerator. Cancers 2023, 15, 1555. [Google Scholar] [CrossRef]
- Singh, M.; Singh, T.; Soni, S. Pre-operative Assessment of Ablation Margins for Variable Blood Perfusion Metrics in a Magnetic Resonance Imaging Based Complex Breast Tumour Anatomy: Simulation Paradigms in Thermal Therapies. Comput. Methods Programs Biomed. 2021, 198, 105781. [Google Scholar] [CrossRef] [PubMed]
- Brandes, A.A.; Tosoni, A.; Spagnolli, F.; Frezza, G.; Leonardi, M.; Calbucci, F.; Franceschi, E. Disease progression or pseudoprogression after concomitant radiochemotherapy treatment: Pitfalls in neurooncology. Neuro Oncol. 2008, 10, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Chaskis, C.; Neyns, B.; Michotte, A.; De Ridder, M.; Everaert, H. Pseudoprogression after radiotherapy with concurrent temozolomide for high-grade glioma: Clinical observations and working recommendations. Surg. Neurol. 2009, 72, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Fabi, A.; Russillo, M.; Metro, G.; Vidiri, A.; Di Giovanni, S.; Cognetti, F. Pseudoprogression and MGMT status in glioblastoma patients: Implications in clinical practice. Anticancer Res. 2009, 29, 2607–2610. [Google Scholar]
- Leao, D.J.; Craig, P.G.; Godoy, L.F.; Leite, C.C.; Policeni, B. Response Assessment in Neuro-Oncology Criteria for Gliomas: Practical Approach Using Conventional and Advanced Techniques. AJNR Am. J. Neuroradiol. 2020, 41, 10–20. [Google Scholar] [CrossRef]
- Singh, G.; Manjila, S.; Sakla, N.; True, A.; Wardeh, A.H.; Beig, N.; Vaysberg, A.; Matthews, J.; Prasanna, P.; Spektor, V. Radiomics and radiogenomics in gliomas: A contemporary update. Br. J. Cancer 2021, 125, 641–657. [Google Scholar] [CrossRef]
- Maziero, D.; Straza, M.W.; Ford, J.C.; Bovi, J.A.; Diwanji, T.; Stoyanova, R.; Paulson, E.S.; Mellon, E.A. MR-Guided Radiotherapy for Brain and Spine Tumors. Front. Oncol. 2021, 11, 626100. [Google Scholar] [CrossRef]
- Styner, M.; Lee, J.; Chin, B.; Chin, M.S.; Commowick, O.; Tran, H.-H.; Markovic-Plese, S.; Jewells, V.; Warfield, S. 3D Segmentation in the Clinic: A Grand Challenge II: MS lesion segmentation. MIDAS J. 2008, 2008, 1–6. [Google Scholar] [CrossRef]
- Menze, B.H.; Jakab, A.; Bauer, S.; Kalpathy-Cramer, J.; Farahani, K.; Kirby, J.; Burren, Y.; Porz, N.; Slotboom, J.; Wiest, R.; et al. The Multimodal Brain Tumor Image Segmentation Benchmark (BRATS). IEEE Trans. Med. Imaging 2015, 34, 1993–2024. [Google Scholar] [CrossRef]
- Maier, O.; Menze, B.H.; von der Gablentz, J.; Hani, L.; Heinrich, M.P.; Liebrand, M.; Winzeck, S.; Basit, A.; Bentley, P.; Chen, L.; et al. ISLES 2015—A public evaluation benchmark for ischemic stroke lesion segmentation from multispectral MRI. Med. Image Anal. 2017, 35, 250–269. [Google Scholar] [CrossRef]
- Gazit, M.H.; Faran, R.; Stepovoy, K.; Peles, O.; Shamir, R.R. Post-operative glioblastoma multiforme segmentation with uncertainty estimation. Front. Hum. Neurosci. 2022, 16, 932441. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Li, M.; Gou, S.; Zhang, X.; Jiang, K. Automated Segmentation Method for Low Field 3D Stomach MRI Using Transferred Learning Image Enhancement Network. BioMed Res. Int. 2021, 2021, 6679603. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Ma, T.M.; Savjani, R.; Pham, J.; Cao, M.; Yang, Y.; Kishan, A.U.; Scalzo, F.; Sheng, K. Fully automated segmentation of prostatic urethra for MR-guided radiation therapy. Med. Phys. 2023, 50, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Breto, A.L.; Spieler, B.; Zavala-Romero, O.; Alhusseini, M.; Patel, N.V.; Asher, D.A.; Xu, I.R.; Baikovitz, J.B.; Mellon, E.A.; Ford, J.C.; et al. Deep Learning for Per-Fraction Automatic Segmentation of Gross Tumor Volume (GTV) and Organs at Risk (OARs) in Adaptive Radiotherapy of Cervical Cancer. Front. Oncol. 2022, 12, 854349. [Google Scholar] [CrossRef] [PubMed]
- Cullison, K.; Simpson, G.; Valderrama, A.; Maziero, D.; Jones, K.; De La Fuente, M.; Meshman, J.J.; Azzam, G.; Stoyanova, R.; Ford, J.; et al. Prognostic Value of Weekly Delta-Radiomics during MR-Linac Radiotherapy of Glioblastoma. Int. J. Radiat. Oncol. Biol. Phys. 2023, 117, S155–S156. [Google Scholar] [CrossRef]
- Brat, D.J.; Aldape, K.; Colman, H.; Holland, E.C.; Louis, D.N.; Jenkins, R.B.; Kleinschmidt-DeMasters, B.K.; Perry, A.; Reifenberger, G.; Stupp, R.; et al. cIMPACT-NOW update 3: Recommended diagnostic criteria for “Diffuse astrocytic glioma, IDH-wildtype, with molecular features of glioblastoma, WHO grade IV”. Acta Neuropathol. 2018, 136, 805–810. [Google Scholar] [CrossRef]
- Bieri, O.; Scheffler, K. Fundamentals of balanced steady state free precession MRI. J. Magn. Reson. Imaging 2013, 38, 2–11. [Google Scholar] [CrossRef]
- Chavhan, G.B.; Babyn, P.S.; Jankharia, B.G.; Cheng, H.L.; Shroff, M.M. Steady-state MR imaging sequences: Physics, classification, and clinical applications. Radiographics 2008, 28, 1147–1160. [Google Scholar] [CrossRef]
- Park, S.-H.; Han, P.K.; Choi, S.H. Physiological and Functional Magnetic Resonance Imaging Using Balanced Steady-state Free Precession. Korean J. Radiol. 2015, 16, 550–559. [Google Scholar] [CrossRef]
- Mutic, S.; Dempsey, J.F. The ViewRay system: Magnetic resonance-guided and controlled radiotherapy. Semin. Radiat. Oncol. 2014, 24, 196–199. [Google Scholar] [CrossRef]
- He, K.; Gkioxari, G.; Dollár, P.; Girshick, R. Mask R-CNN. In Proceedings of the IEEE International Conference on Computer Vision (ICCV), Venice, Italy, 22–29 Octobre2017; pp. 2980–2988. [Google Scholar]
- Abadi, M.; Barham, P.; Chen, J.; Chen, Z.; Davis, A.; Dean, J.; Devin, M.; Ghemawat, S.; Irving, G.; Isard, M.; et al. Tensorflow: A system for large-scale machine learning. In Proceedings of the 12th USENIX Symposium on Operating Systems Design and Implementation, Savannah, GA, USA, 2–4 November 2016. [Google Scholar]
- Cholett, F. Keras 3: A New Multi-Backend Keras. Available online: https://github.com/fchollet/keras (accessed on 29 May 2023).
- Russakovsky, O.; Deng, J.; Su, H.; Krause, J.; Satheesh, S.; Ma, S.; Huang, Z.H.; Karpathy, A.; Khosla, A.; Bernstein, M.; et al. ImageNet Large Scale Visual Recognition Challenge. Int. J. Comput. Vis. 2015, 115, 211–252. [Google Scholar] [CrossRef]
- Johnson, J.W. Adapting Mask-RCNN for Automatic Nucleus Segmentation. arXiv 2018, arXiv:1805.00500v1. [Google Scholar]
- Dice, L.R. Measures of the Amount of Ecologic Association between Species. Ecology 1945, 26, 297–302. [Google Scholar] [CrossRef]
- Waqar, M.; Roncaroli, F.; Lehrer, E.J.; Palmer, J.D.; Villanueva-Meyer, J.; Braunstein, S.; Hall, E.; Aznar, M.; De Witt Hamer, P.C.; D’Urso, P.I.; et al. Rapid early progression (REP) of glioblastoma is an independent negative prognostic factor: Results from a systematic review and meta-analysis. Neurooncol. Adv. 2022, 4, vdac075. [Google Scholar] [CrossRef] [PubMed]
- Luu, H.M.; Park, S.-H. (Eds.) Extending nn-UNet for Brain Tumor Segmentation; Springer International Publishing: Cham, Switzerland, 2022; pp. 173–186. [Google Scholar]
- Kim, H.E.; Cosa-Linan, A.; Santhanam, N.; Jannesari, M.; Maros, M.E.; Ganslandt, T. Transfer learning for medical image classification: A literature review. BMC Med. Imaging 2022, 22, 69. [Google Scholar] [CrossRef]
- Gibson, E.; Hu, Y.P.; Ghavami, N.; Ahmed, H.U.; Moore, C.; Emberton, M.; Huisman, H.J.; Barratt, D.C. Inter-site Variability in Prostate Segmentation Accuracy Using Deep Learning. Lect. Notes Comput. Sc. 2018, 11073, 506–514. [Google Scholar] [CrossRef]
- Zavala-Romero, O.; Breto, A.L.; Xu, I.S.R.; Chang, Y.C.C.; Gautney, N.; Pra, A.D.; Abramowitz, M.C.; Pollack, A.; Stoyanova, R. Segmentation of prostate and prostate zones using deep learning A multi-MRI vendor analysis. Strahlenther. Onkol. 2020, 196, 932–942. [Google Scholar] [CrossRef]
- Ridder, M.; Raaijmakers, C.P.J.; Pameijer, F.A.; Bree, R.; Reinders, F.C.J.; Doornaert, P.A.H.; Terhaard, C.H.J.; Philippens, M.E.P. Target Definition in MR-Guided Adaptive Radiotherapy for Head and Neck Cancer. Cancers 2022, 14, 3027. [Google Scholar] [CrossRef]
- Wen, P.Y.; Macdonald, D.R.; Reardon, D.A.; Cloughesy, T.F.; Sorensen, A.G.; Galanis, E.; Degroot, J.; Wick, W.; Gilbert, M.R.; Lassman, A.B.; et al. Updated response assessment criteria for high-grade gliomas: Response assessment in neuro-oncology working group. J. Clin. Oncol. 2010, 28, 1963–1972. [Google Scholar] [CrossRef]
- Singh, M.; Dalal, M.; Sodhi, G.S. Estimation of clinical size of breast tumour lesions using contrast enhanced magnetic resonance imaging: Delineation of tumour boundaries. In Proceedings of the Summer Biomechanics, Bioengineering and Biotransport Conference, Virtual, 14–18 June 2021. [Google Scholar]
- U.S. Food & Drugs Administration. FDA Drug Safety Communication: FDA Warns that Gadolinium-Based Contrast Agents (GBCAs) are Retained in the Body; Requires New Class Warnings. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-gadolinium-based-contrast-agents-gbcas-are-retained-body (accessed on 4 January 2023).
- Malikova, H.; Holesta, M. Gadolinium contrast agents—Are they really safe? J. Vasc. Access 2017, 18, 1–7. [Google Scholar] [CrossRef]
- Maziero, D.; Stoyanova, R.; Chang, Y.; Breto, A.; Ford, J.; Mellon, E. (Eds.) Feasibility of Dynamic Contrast Enhanced MR Perfusion for Glioblastoma on a Low-Field MRI-Linac System; Medical Physics; Wiley: Hoboken, NJ, USA, 2021. [Google Scholar]
- Cullison, K.; Maziero, D.; Spieler, B.; Mellon, E.A. Central nervous system tumors. MR Linac Radiotherapy—A New Personalized Treatment Approach. In Advances in Magnetic Resonance Technology and Applications; Elsevier: Amsterdam, The Netherlands, 2022; pp. 211–235. [Google Scholar]
- Rizzo, S.; Botta, F.; Raimondi, S.; Origgi, D.; Fanciullo, C.; Morganti, A.G.; Bellomi, M. Radiomics: The facts and the challenges of image analysis. Eur. Radiol. Exp. 2018, 2, 36. [Google Scholar] [CrossRef] [PubMed]
- Nejad-Davarani, S.P.; Zakariaei, N.; Chen, Y.; Haacke, E.M.; Hurst, N.J., Jr.; Salim Siddiqui, M.; Schultz, L.R.; Snyder, J.M.; Walbert, T.; Glide-Hurst, C.K. Rapid multicontrast brain imaging on a 0.35T MR-linac. Med. Phys. 2020, 47, 4064–4076. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Zhang, W.; Li, B.; Zhu, J.; Peng, Y.; Li, C.; Zhu, J.; Zhou, Q.; Yin, Y. Patient-specific daily updated deep learning auto-segmentation for MRI-guided adaptive radiotherapy. Radiother. Oncol. 2022, 177, 222–230. [Google Scholar] [CrossRef] [PubMed]

| Variable | N (%) |
|---|---|
| Age, Median (Range) | 60 (22–77) |
| Sex | |
| Female | 12 (33%) |
| Male | 24 (67%) |
| Resection type | |
| Gross total | 12 (33%) |
| Sub-total | 14 (39%) |
| Biopsy | 10 (28%) |
| O6-Methylguanine-DNA Methyl-Transferase (MGMT) Status | |
| Hypermethylated | 15 (42%) |
| Non-Hypermethylated | 17 (47%) |
| Unknown | 4 (11%) |
| Isocitrate Dehydrogenase I (IDH) Status | |
| Mutant | 6 (17%) |
| Wild Type | 30 (83%) |
| Global | TL | RC | Mixed (Both RC and TL) | |||||
|---|---|---|---|---|---|---|---|---|
| n | DSC (Mean ± σ) | n | DSC (Mean ± σ) | n | DSC (Mean ± σ) | n | DSC (Mean ± σ) | |
| Tumor Lesion (TL) | 20 | 0.67 ± 0.2 | 15 | 0.67 ± 0.17 | 0 | 5 | 0.67 ± 0.24 | |
| Resection Cavity (RC) | 12 | 0.84 ± 0.18 | 0 | 7 | 0.89 ± 0.06 | 5 | 0.81 ± 0.14 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Breto, A.L.; Cullison, K.; Zacharaki, E.I.; Wallaengen, V.; Maziero, D.; Jones, K.; Valderrama, A.; de la Fuente, M.I.; Meshman, J.; Azzam, G.A.; et al. A Deep Learning Approach for Automatic Segmentation during Daily MRI-Linac Radiotherapy of Glioblastoma. Cancers 2023, 15, 5241. https://doi.org/10.3390/cancers15215241
Breto AL, Cullison K, Zacharaki EI, Wallaengen V, Maziero D, Jones K, Valderrama A, de la Fuente MI, Meshman J, Azzam GA, et al. A Deep Learning Approach for Automatic Segmentation during Daily MRI-Linac Radiotherapy of Glioblastoma. Cancers. 2023; 15(21):5241. https://doi.org/10.3390/cancers15215241
Chicago/Turabian StyleBreto, Adrian L., Kaylie Cullison, Evangelia I. Zacharaki, Veronica Wallaengen, Danilo Maziero, Kolton Jones, Alessandro Valderrama, Macarena I. de la Fuente, Jessica Meshman, Gregory A. Azzam, and et al. 2023. "A Deep Learning Approach for Automatic Segmentation during Daily MRI-Linac Radiotherapy of Glioblastoma" Cancers 15, no. 21: 5241. https://doi.org/10.3390/cancers15215241
APA StyleBreto, A. L., Cullison, K., Zacharaki, E. I., Wallaengen, V., Maziero, D., Jones, K., Valderrama, A., de la Fuente, M. I., Meshman, J., Azzam, G. A., Ford, J. C., Stoyanova, R., & Mellon, E. A. (2023). A Deep Learning Approach for Automatic Segmentation during Daily MRI-Linac Radiotherapy of Glioblastoma. Cancers, 15(21), 5241. https://doi.org/10.3390/cancers15215241







