Simple Summary
Cancer often causes long-term physical and psychological impairments. Lifestyle modification and nature-based interventions (NBIs) can have a positive impact on patients’ quality of life (QOL). However, there is sparse scientific research on the effects of natural environments in the treatment of cancer patients. Therefore, we integrated intensified nature experiences into the scientifically substantiated therapy approach of an oncology day care clinic program. This study aimed to compare the effects of a nature-based oncology day care clinic intervention to conventional oncology day care clinic intervention. A positive impact of the day care clinic program on QOL, fatigue, and psychological parameters in cancer patients was shown. In addition, NBIs seem to have more pronounced effects, which need to be further proven.
Abstract
Cancer often causes long-term physical and psychological impairments. Lifestyle modification and nature-based interventions (NBIs) can have a positive impact on patients’ quality of life (QOL). This participants-blinded, non-randomized controlled study assessed parameters at weeks 0, 12, and 24, including, as a primary endpoint, QOL in cancer patients on the Functional Assessment of Cancer Therapy—General (FACT-G) at week 12. QOL in breast cancer patients, fatigue, well-being, stress, anxiety/depression, socio-psychological well-being, benefits of nature interaction, insomnia, self-efficacy, mindfulness, and self-compassion were assessed as secondary endpoints. N = 107 cancer patients (96.3% women; 52.5 ± 9.3 years, 80.4% breast cancer) were assigned to either a 12-week nature-based (NDC; n = 56) or conventional (DC; n = 51) oncology day care clinic program, whereby the assignment group was not known to the participants. There was no significant group difference for the primary endpoint. At week 24, QOL, fatigue, mindfulness and self-compassion scores were significantly higher, and at weeks 12 and 24, the insomnia score was significantly lower in NDC compared to DC. In conclusion, this study indicates positive and clinically relevant effects of the program on QOL, fatigue, and psychological parameters. NBIs seem to have a more pronounced effect.
Keywords:
cancer; day care; integrative medicine; lifestyle; MICOM; Mind–body Medicine; mindfulness; meditation; nature; oncology 1. Introduction
Cancer is one of the most common causes of morbidity and mortality in industrialized societies [1]. In addition to disease- and treatment-related symptoms, cancer patients often suffer from psychological and physical complaints, even after completion of primary therapy. Fatigue, depression, and anxiety, as well as disturbed sleep, may lead to impaired quality of life and mood [2].
Complementary and integrative medicine (CIM) practices are widely used by cancer patients, mainly to reduce treatment-related side effects, e.g., to relieve pain and to strengthen their immune system [3,4,5]. In view of rising survival rates [6], the need for treatment options that improve disease-related symptoms such as pain or fatigue is growing and gaining importance in oncology. Therefore, “integrative” oncology, which combines “conventional” cancer therapy with evidence-based CIM methods, is an emerging field [7,8].
Mind–body medicine (MBM) is an important method within CIM, where “practices […] focus on the interactions between the brain, mind, body, and behavior” [9]. In a broader sense, MBM also comprises health-related lifestyle issues to improve patients’ self-care and self-efficacy [9].
MBM practices have been studied in cancer patients in randomized, controlled clinical trials, which have showed positive effects on quality of life, pain intensity and pain coping, fatigue, and psychological well-being, including depression and anxiety [10,11].
It should be noted that the above studies evaluated unimodal interventions in clinical trials and usually recruited highly selected populations. We combined these MBM methods in an oncology day care clinic program and made it available for a general population of cancer patients. Cohort studies conducted at our department [12] and at the Department of Integrative Medicine, Evangelische Kliniken Essen-Mitte [13,14,15] have already evaluated this treatment approach. Improvements in quality of life, fatigue, and psychological parameters, especially anxiety and depression were shown [12,13,14,15]. Several compulsory health insurance funds cover the costs of this integrative oncology day care clinic program in Germany.
Furthermore, in recent years increasing amounts of evidence have been found for the health benefits of nature experiences and nature-based interventions (NBIs); among other things, positive effects on general well-being, autonomic nervous system functions, blood pressure, endocrine activity, and immune activity have been demonstrated [16,17,18]. Early findings from an intervention study on psychotherapy for depressive patients indicate that conducting therapy in nature (a forest environment) is more effective than conducting it in hospital [19]. However, there is sparse scientific research on the effects of natural environments in the treatment of cancer patients.
Therefore, we integrated intensified nature experiences into the scientifically substantiated therapy approach of an MICOM (Mind–body Medicine in Integrative and Complementary Medicine) based oncology day care clinic program. This study aimed to assess the effects of a nature-based oncology day care clinic intervention for cancer patients on patient-reported outcomes (PROs), compared to a conventional oncology day care clinic intervention.
2. Materials and Methods
2.1. Design
This participants-blinded, non-randomized controlled study was approved by the ethics committees of the Charité—Universitätsmedizin Berlin (EA4/026/20). After registration at ClinicalTrials.gov (NCT04411251), reporting was performed according to the CONSORT (Consolidated Standards of Reporting Trials) extension for pilot and feasibility trials [20].
2.2. Participants
Patients were recruited in the study department, checked for eligibility and assessed by a study physician. If all inclusion criteria and no exclusion criteria were met and informed consent was signed, patients were enrolled in the study. The participants were assigned to the group with the next possible start date of the day care clinic program, as there is usually a waiting time of several weeks for these clinics, due to high demand. The group they were assigned to was not known to the participants.
Adult patients between the ages of 18 and 85 years, diagnosed with any type of cancer were included. Exclusion criteria included (1) cognitive impairment that would interfere with answering questionnaires or the intervention, (2) pre-existing severe mental disorders, (3) pregnancy or breastfeeding, or (4) participation in another study.
2.3. Nature-Based Oncology Day Care Clinic Program (NDC)
Participants took part in a 12-week nature-based day care clinic program with weekly 6-h sessions, of which 1.5 h were in nature. A semi-residential format was chosen to improve group cohesion and the patient–therapist relationship. The day care clinic program was based on the mindfulness-based stress reduction (MBSR) program and the Mindbody medicine cancer program of the Benson–Henry Institute for Mind–Body Medicine, which was further developed according to the MICOM model [9]. The focus was on relaxation techniques, rooted in psychoneuroendocrinology, and used meditation, gentle yoga, breathing exercises, muscle relaxation, physical exercise, cognitive restructuring, and social support. In addition, CIM methods of self-care were incorporated, such as nutrition, self-massage, and hydrotherapy. Patients were strongly encouraged to use self-help techniques to enhance self-empowerment. The aim of the program was to reduce disease and treatment induced stress, to improve health-related lifestyles, coping skills, and acceptance of illness. MSc- or Ph.D.-level health professionals specially trained in MBM and psychosocial counseling held the day care clinic program. Moreover, weekly rounds were made by physicians, in which patients received individual recommendations for support. Therapists were trained to instruct with a mindful attitude during the entire program.
NBI training took place in an area close to nature, especially in the hospital park of the Immanuel Hospital Berlin, Berlin, Germany. These included relaxation techniques guided directly in nature, gentle movement exercises such as yoga and Qigong in nature as well as nature awareness and nature meditation exercises. Furthermore, participants were asked to spend at least 60 min a day in nature and to practice the exercises taught in the day care clinic close to nature.
2.4. Conventional Oncology Day Care Clinic Program (DC)
This intervention was the same as that of the NDC group, but took place mainly in the hospital building. Participants were asked to practice the above-mentioned exercises, taught in the day clinic, at home for at least 60 min a day.
2.5. Outcome Measures
Assessment of the following PROs took place at baseline and at 12 and 24 weeks after enrollment.
- The primary endpoint was the difference between changes from baseline to week 12 in the quality of life in cancer patients on the Functional Assessment of Cancer Therapy—General (FACT-G) scale, including 4 domains of health-related quality of life: physical (7 items), social (7 items), emotional (6 items), and functional (7 items) well-being [21].
- Quality of life assessment in breast cancer patients on the Functional Assessment of Cancer Therapy—Breast Cancer (FACT-B) consisted of the 27-item FACT-G and the 10-item breast cancer subscale (BCS) that addressed additional concerns associated with breast cancer and its treatment [22].
- Fatigue assessment on the Functional Assessment of Chronic Illness Therapy—Fatigue (FACIT-F) consisted of the 27-item FACT-G and the 13-item fatigue subscale, (FS) [23], measuring self-reported fatigue and its impact upon daily activities and function is.
- Well-being on the 5-item WHO-Five Well-Being Index (WHO-5) [24].
- Stress on the 10-item Perceived Stress Scale (PSS-10) for measuring perceived stress within the last month [25].
- Anxiety and depression on the 14-item Hospital Anxiety and Depression Scale (HADS-D) for assessing anxiety and depression symptoms [26].
- Socio-psychological well-being on the 8-item Flourishing Scale (FS-D) [27]. Flourishing of the personality refers to the self-assessment of one’s own perspective,, potential and resources [27].
- Perceived benefits of interacting with nature on the 11-item Perceived Benefits of Nature Questionnaire (PBNQ) [28].
- Insomnia on the 7-item Insomnia Severity Index (ISI) for assessing the nature, severity, and impact of insomnia [29].
- Self-efficacy on the 3-item Self-Efficacy Scale—Short Form (ASKU) [30]. Self-efficacy reflects “individual competence expectations to be able to deal with difficulties and obstacles in daily life“ [30].
- Mindfulness on the 14-item Freiburg Mindfulness Inventory (FMI) [31].
- Self-compassion on the 26-item Self-Compassion Scale (SCS-D) [32].
Evaluation, adherence to relaxation exercises and lifestyle (diet, Kneipp hydrotherapy, phytotherapy, relaxation exercises, cigarette/alcohol consumption, and sick leave) were assessed by questionnaires designed by the authors. A 5-point Likert scale was used to evaluate the day care clinic program and nominal/ordinal scales and duration in minutes were allocated as free text for the assessment of lifestyle-related issues. Participants completed a weekly review during the day care clinic program, in which they reflected on their exercise practice at home. Unfortunately, there were too many pieces of missing data, making analysis of this component impossible. Adverse effects were recorded using standardized forms.
2.6. Sample Size Calculation and Statistical Analysis
Based on a pre-study, it was determined that a total of 30 patients per group were required to detect a difference between groups at alpha = 0.05 and a statistical power of 80% (beta = 0.20) [12]. Accounting for a potential dropout rate of 15%, at least 72 participants needed to be included. However, due to good recruitment despite the Covid-19 pandemic, and since the program was part of the hospital’s regular care, we decided to enroll more patients. All analyses were conducted according to the intention-to-treat method, i.e., all participants were analyzed in the group to which they were originally assigned. Missing data were multiply imputed by Markov Chain Monte Carlo (MICE) methods [33,34], resulting in a total of 101 complete data sets.
For data analysis, differences between test results for V1 and V0, and for V2 and V0, were calculated. Test statistics are given as means ± standard deviations (M ± SD). Within-group differences were analyzed by paired t-tests and group differences by independent t-tests. Only the between-group test for the primary endpoint was tested in a confirmatory way, against an alpha = 0.05. All other comparisons within and between groups were conducted on an exploratory level only. Thus, no alpha adjustment (Bonferroni correction) was applied. ANCOVAs were used to test whether sociodemographic parameters such as sex, age, marital status, highest level of education, employment status, and self-reported monthly income, as well as the self-reported stress level (PSS at visit V0), had an impact on the primary endpoint. All analyses were performed using Statistical Package for Social Sciences software (IBM SPSS Statistics for Windows, Version 28.0. IBM Corp, Armonk, NY, USA).
3. Results
3.1. Participants
A total of 107 patients were screened, enrolled after giving informed consent, and allocated to either the NDC (n = 56) or DC group (n = 51). Eleven participants (four in the NDC group and seven in the DC group) dropped out of the study before the primary endpoint in week 12. Another seven (four in the NDC group and three in the DC group) were missing at the follow-up in week 24 (Figure 1). Patients were recruited between July 2020 (first patient in) and October 2021. The last follow-up assessment was completed in May 2022 (last patient out). Participants’ characteristics are shown in Table 1. Of the total of 107 participants (mean age 52.5 ± 9.3 years), almost all (96.3%) were female, while about two-thirds had a university degree. Participants had a BMI of 23.9 ± 4.1 kg/m2. Eighty percent were diagnosed with breast cancer. More than half reported sleep disturbances and fatigue, and polyneuropathy was mentioned by 29% of the participants. Co-morbidities are listed in Table S1 in the Supplementary Material.
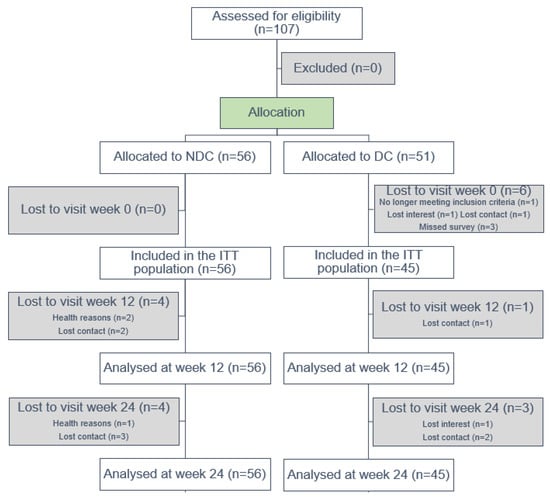
Figure 1.
Study flow chart. Abbreviations: NDC, nature-based oncology day care clinic program; DC, conventional oncology day care clinic program; ITT, intention-to-treat.

Table 1.
Sociodemographic and clinical characteristics at baseline.
3.2. Primary Endpoint
In respect of the primary endpoint, the FACT-G score, patients in both groups improved between the baseline measure and their visit at week 12 (NDC Δ = 11.0 ± 9.5, p < 0.0001; DC Δ = 8.7 ± 10.6, p < 0.0001). However, the hypothesized difference between groups did not become significant (Δ = 2.3 ± 2.0, p = 0.2573), and only the follow-up testing in week 24 yielded an (exploratively) significant group difference (Δ = 5.3 ± 2.2; p = 0.0161) (Table 2 and Figure 2).

Table 2.
Outcome measures (mean ± standard deviation). Bold p-values indicate significant group differences (p < 0.05).
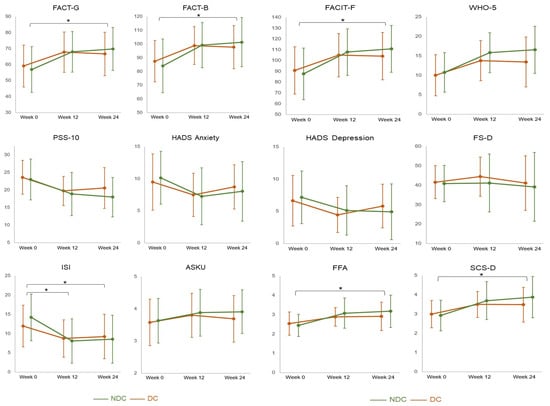
Figure 2.
Multiplot on patient-reported outcomes. Legend: ASKU, Self-Efficacy Scale—Short Form; FACIT-F, Functional Assessment of Chronic Illness Therapy—Fatigue; FACT-B, Functional Assessment of Cancer Therapy—Breast Cancer; FACT-G, Functional Assessment of Cancer Therapy—General; FMI, Freiburg Mindfulness Inventory; FS-D, Flourishing Scale; HADS-D, Hospital Anxiety and Depression Scale; ISI, Insomnia Severity Index; NDC, nature-based oncology day care clinic program; DC, conventional oncology day care clinic program; PSS-10, Perceived Stress Scale; SCS-D, Self-Compassion Scale; WHO-5, WHO-Five Well-Being Index; * = p < 0.05. The error bars indicate standard deviations.
3.3. Secondary Endpoints
From week 0 to week 12, within-group improvements in the range of moderate to large effects were obtained for most self-reported outcomes, i.e., quality of life (FACT-G and FACT-B), fatigue (FACIT-F), well-being (WHO-5), perceived stress (PSS-10), anxiety and depression (HADS), insomnia (ISI), self-efficacy (ASKU), mindfulness (FMI), and self-compassion (SCS-D). However, regarding between-group comparisons after 12 weeks, only the ISI score was significantly lower in NDC than in DC (Δ = 2.9 ± 1.1; p = 0.0116).
Positive within-group effects found after 12 weeks also persisted to week 24. In contrast to the comparisons for week 12, at week 24, more between-group comparisons became significant, with results indicating a better quality of life (FACT-G: Δ = 5.3 ± 2.2; p = 0.161 and FACT-B: Δ = 7.0 ± 2.8; p = 0.0129), less fatigue (FACT-F: Δ = 10.0 ± 4.1; p = 0.0162), higher mindfulness (FMI: Δ = 0.4 ± 0.2; p = 0.0298) and self-compassion (SCS-D: Δ = 0.5 ± 0.2; p = 0.0223), and less insomnia (Δ = 2.9 ± 1.1; p = 0.0108) in the NDC than in the DC group at the follow-up (Table 2 and Figure 2).
3.4. Covariates
The initial self-reported stress level (PSS at V0) was revealed to be a significant covariate for the primary endpoint. Higher initial stress levels (as indicated by higher values in the PSS) were significantly positively correlated with higher gains (differences) in the FACT-G for both comparisons, V1 vs. V0 (p < 0.001) and V2 vs. V0 (p < 0.001), indicating that patients with a higher initial stress level gained more from the intervention.
Apart from that, none of the other tested parameters (sex, age, marital status, highest level of education, employment status, and self-reported monthly income, as well as the self-reported stress level) had a significant impact on the FACT-G (primary endpoint).
3.5. Lifestyle
Results for lifestyle measures are listed in Table S2 (Supplementary Material). Patients’ diets changed slightly toward a plant-based diet during the study period. At baseline, participants used Kneipp hydrotherapy on average on one day, compared to three days at the follow-ups. The percentage of participants using phytotherapy increased from about 80% at baseline to nearly 100% post-intervention. Relaxation exercises were already practiced by about half of the participants at the beginning of the study, by almost all after 12 weeks and by about three quarters after 24 weeks. At baseline, participants in the NDC group exercised on average for 13.3 ± 34.5 and in the DC group for 7.6 ± 11.2 min per day, compared to 22.1 ± 20.9 and 20.2 ± 17.8 min per day after the intervention. Cigarette and alcohol consumption decreased overall after the intervention. The same applies to the number of sick days.
3.6. Evaluation
In all assessments, participants rated the effectiveness of the day care clinic program as strong. Most of them reported concerns about the implementation of the program before the start, but these negative expectations were not confirmed in the follow-ups (Table S3 in the Supplementary Material).
3.7. Adverse Events
No serious adverse events occurred that could be associated with the intervention. In the DC group, two patients suffered from a form of breast cancer recurrence during the course of the study and had to undergo surgery. Single participants reported restlessness and tension during certain exercises. Overall, 29 minor adverse events occurred in 19 patients in the DC group, and 18 in 13 patients in the NDC group (Table S4 in the Supplementary Material).
4. Discussion
This study aimed to assess the effects of a nature-based day care clinic intervention, compared to a conventional day care clinic intervention, on self-reported outcomes in cancer patients. Although the primary endpoint did not reach statistical difference between the groups, after the day care clinic intervention, we found (exploratively significant) improvements in both groups for almost all outcome measures, namely quality of life, fatigue, well-being, stress, anxiety, depression, insomnia, self-efficacy, mindfulness, and self-compassion. At week 12, the insomnia score (ISI) was significantly lower, and at week 24, quality of life (FACT-G, FACT-B), fatigue (FACIT-F), mindfulness (FMI) and self-compassion (SCS-D) were significantly higher and insomnia (ISI) significantly lower in the nature-based group.
With more than 90% women and about 80% breast cancer patients, the groups were similar regarding gender and cancer types. In total, a larger proportion had a higher level of education. At the start of the study, the entire population had lower levels of quality of life and increased stress, anxiety and insomnia levels.
The day care clinic intervention reduced stress and anxiety in both groups. Furthermore, participants had a higher level of quality of life at the end of intervention as well as at the 24-week follow-up. This is in line with the pre-study [12] and other findings that showed improvements in stress, anxiety, and depression through MBSR intervention [35,36,37]. Also, yoga has been shown in meta-analyses to improve quality of life and reduce anxiety, depression, stress, and fatigue, especially in patients with breast cancer [38,39]. In addition meta-analyses on psychosocial interventions found positive effects on health-related quality of life, mental health, and possibly survival in patients with prostate cancer [40] or breast cancer [41,42], but not in patients with head and neck cancer [43]. Psychosocial factors also have a major impact on the quality of life of patients with ovarian cancer [44]. Furthermore, for cancer patients of reproductive age, fertility preservation and family planning are important issues that affect quality of life [45,46,47].
The 24-week follow-up indicated that NDC significantly improved quality of life and fatigue in the between-group comparison. Recent studies have shown that NBIs can enhance health-related quality of life and mental health, particularly depressed mood, anxiety, and affect [48,49,50]. A natural environment is also associated with lower levels of stress hormones and higher levels of serotonin and endogenous opioids, which also contribute to better vitality and mood [51].
For several parameters, cut off values for clinically relevant effects have previously been reported. The minimum clinically important difference (MCID) for the FACT-G is defined as a value of 5, for the FACT-B as a value of 7, and for the FS as a value of 3. In our study the increases were greater than 7 points, 10 points, and 5 points, respectively [52,53]. With more than 6 points’ difference, the NDC group achieved the MCID for ISI at the 12-week visit [54]. Our study population experienced improvements in self-efficacy, mindfulness, and self-compassion through the MBM intervention. These parameters could interact with each other. In addition, a meta-analysis showed overall positive effects of mindfulness in natural environments, suggesting the important role of setting in the benefits of mindfulness-based interventions [55].
Study Limitations
Our study has several limitations. First, we could not randomize the participants, because the study was conducted in the framework of a regular care setting at the day care clinic. Therefore, the clinic personnel were not blinded either. The participants were assigned to the group with the next possible start date of the day care clinic program, as these usually have a waiting time of several weeks, due to high demand. Because of the non-randomized design, group comparisons are limited. However, participants did not know whether they were assigned to the NDC or the DC group, so that non-specific effects, e.g., due to disappointment effects, were minimized.
Second, the DC group was smaller and the clinical characteristics of the groups were not completely balanced. Another limiting fact is that our study population consisted of predominantly female participants with a higher level of education. We aimed to include more men and patients with other types of cancer, but only a limited number of these patients were referred during the recruitment phase.
The fact that the majority of participants were diagnosed with breast cancer also limits the generalizability of the study results. Future studies in the field should focus on single cancer types to capture the impact of the interventions more accurately.
Another limitation is the mix of patients undergoing chemotherapy, radiotherapy, hormone therapy and surgery. Patients’ concerns may vary significantly in these different oncology settings. However, the physicians gave the patients individual recommendations to support them.
Another limiting factor is that the interventions were a mixture of different techniques that could not all be applied to participants in the same way and were not used in the same way by the participants. The sample size should have been larger than calculated, to account for variability in interventions, cancer types, and cancer treatments.
Also, adherence to each intervention component (e.g., mindfulness, nature interventions, diet, hydrotherapy, phytotherapy) could be assessed in more detail.
5. Conclusions
In summary, the results of this study indicate positive and clinically relevant effects of the day care clinic program on quality of life, fatigue, and psychological parameters. In addition, nature-based interventions seem to have more pronounced effects, which need to be further proven in randomized trials.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers15184595/s1, Table S1: Secondary diagnoses; Table S2: Lifestyle. If not otherwise denoted values are reported as mean ± standard deviation; Table S3: Evaluation; Table S4: Type and number of adverse events.
Author Contributions
Conceptualization, L.K., C.S.K., C.v.S., B.K., A.M. and M.J.; Methodology, F.I.K. and M.W.; Formal analysis, L.K. and F.I.K.; Investigation, L.K. and M.J.; Resources, C.S.K., C.v.S., B.K. and M.J.; Data curation, L.K. and F.I.K.; Writing—original draft, L.K.; Writing—review & editing, C.S.K., F.I.K., C.v.S., M.M., B.K., A.M. and M.J.; Supervision, C.S.K., C.v.S., A.M. and M.J.; Project administration, C.S.K., C.v.S., A.M. and M.J.; Funding acquisition, C.S.K., A.M. and M.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Berg foundation.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Charité—Universitätsmedizin Berlin (EA4/026/20) according to the vote of 27 February 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
We acknowledge financial support from Berg Foundation and the Open Access Publication Fund of Charité—Universitätsmedizin Berlin and the German Research Foundation (DFG).
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CIM | Complementary and integrative medicine |
| MBM | Mind–body medicine |
| MICOM | Mind–body Medicine in integrative and complementary Medicine |
| NBI | Nature-based intervention |
| PRO | Patient-reported outcome |
| CONSORT | Consolidated Standards of Reporting Trials |
| NDC | Nature-based oncology day care clinic program |
| MBSR | Mindfulness-based stress reduction |
| DC | Conventional oncology day care clinic program |
| MICE | Markov Chain Monte Carlo |
| MCID | Minimum clinical important difference |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.K.; Yeung, R.M. Impact of mood disturbance, sleep disturbance, fatigue and pain among patients receiving cancer therapy. Eur. J. Cancer Care 2013, 22, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Fouladbakhsh, J.M.; Stommel, M. Gender, symptom experience, and use of complementary and alternative medicine practices among cancer survivors in the U.S. cancer population. Oncol. Nurs. Forum 2010, 37, E7–E15. [Google Scholar] [CrossRef] [PubMed]
- Molassiotis, A.; Fernández-Ortega, P.; Pud, D.; Ozden, G.; Scott, J.A.; Panteli, V.; Margulies, A.; Browall, M.; Magri, M.; Selvekerova, S.; et al. Use of complementary and alternative medicine in cancer patients: A European survey. Ann. Oncol. 2005, 16, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Verhoef, M.J.; Balneaves, L.G.; Boon, H.S.; Vroegindewey, A. Reasons for and characteristics associated with complementary and alternative medicine use among adult cancer patients: A systematic review. Integr. Cancer Ther. 2005, 4, 274–286. [Google Scholar] [CrossRef]
- Berry, D.A.; Cronin, K.A.; Plevritis, S.K.; Fryback, D.G.; Clarke, L.; Zelen, M.; Mandelblatt, J.S.; Yakovlev, A.Y.; Habbema, J.D.; Feuer, E.J. Effect of screening and adjuvant therapy on mortality from breast cancer. N. Engl. J. Med. 2005, 353, 1784–1792. [Google Scholar] [CrossRef]
- Cramer, H.; Cohen, L.; Dobos, G.; Witt, C.M. Integrative oncology: Best of both worlds-theoretical, practical, and research issues. Evid.-Based Complement. Alternat Med. 2013, 2013, 383142. [Google Scholar] [CrossRef]
- Dobos, G.; Cramer, H.; Anant, S.; Witt, C.M.; Cohen, L. Integrative oncology. Evid.-Based Complement. Alternat Med. 2013, 2013, 124032. [Google Scholar] [CrossRef]
- Dobos, G.; Paul, A.; Hübner, H. Mind-Body-Medizin: Integrative Konzepte zur Ressourcenstärkung und Lebensstilveränderung; Elsevier Health Sciences: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Sharma, M.; Lingam, V.C.; Nahar, V.K. A systematic review of yoga interventions as integrative treatment in breast cancer. J. Cancer Res. Clin. Oncol. 2016, 142, 2523–2540. [Google Scholar] [CrossRef]
- Zeng, Y.; Luo, T.; Xie, H.; Huang, M.; Cheng, A.S. Health benefits of qigong or tai chi for cancer patients: A systematic review and meta-analyses. Complement. Ther. Med. 2014, 22, 173–186. [Google Scholar] [CrossRef]
- Jeitler, M.; Jaspers, J.; von Scheidt, C.; Koch, B.; Michalsen, A.; Steckhan, N.; Kessler, C.S. Mind-body medicine and lifestyle modification in supportive cancer care: A cohort study on a day care clinic program for cancer patients. Psychooncology 2017, 26, 2127–2134. [Google Scholar] [CrossRef] [PubMed]
- Dobos, G.; Overhamm, T.; Bussing, A.; Ostermann, T.; Langhorst, J.; Kummel, S.; Paul, A.; Cramer, H. Integrating mindfulness in supportive cancer care: A cohort study on a mindfulness-based day care clinic for cancer survivors. Support. Care Cancer 2015, 23, 2945–2955. [Google Scholar] [CrossRef] [PubMed]
- Spahn, G.; Choi, K.E.; Kennemann, C.; Ludtke, R.; Franken, U.; Langhorst, J.; Paul, A.; Dobos, G.J. Can a multimodal mind-body program enhance the treatment effects of physical activity in breast cancer survivors with chronic tumor-associated fatigue? A randomized controlled trial. Integr. Cancer Ther. 2013, 12, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Paul, A.; Cramer, H.; Lauche, R.; Altner, N.; Langhorst, J.; Dobos, G.J. An oncology mind-body medicine day care clinic: Concept and case presentation. Integr. Cancer Ther. 2013, 12, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Ikei, H.; Miyazaki, Y. Physiological Effects of Visual Stimulation with Forest Imagery. Int. J. Environ. Res. Public. Health 2018, 15, 213. [Google Scholar] [CrossRef]
- Ideno, Y.; Hayashi, K.; Abe, Y.; Ueda, K.; Iso, H.; Noda, M.; Lee, J.S.; Suzuki, S. Blood pressure-lowering effect of Shinrin-yoku (Forest bathing): A systematic review and meta-analysis. BMC Complement. Altern. Med. 2017, 17, 409. [Google Scholar] [CrossRef]
- Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. Int. J. Environ. Res. Public. Health 2017, 14, 851. [Google Scholar] [CrossRef]
- Kim, W.; Lim, S.K.; Chung, E.J.; Woo, J.M. The effect of cognitive behavior therapy-based psychotherapy applied in a forest environment on physiological changes and remission of major depressive disorder. Psychiatry Investig. 2009, 6, 245–254. [Google Scholar] [CrossRef]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A.; Altman, D.; Bretz, F.; Campbell, M.; et al. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016, 2, 64. [Google Scholar] [CrossRef]
- Cella, D.F.; Tulsky, D.S.; Gray, G.; Sarafian, B.; Linn, E.; Bonomi, A.; Silberman, M.; Yellen, S.B.; Winicour, P.; Brannon, J.; et al. The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. J. Clin. Oncol. 1993, 11, 570–579. [Google Scholar] [CrossRef]
- Brady, M.J.; Cella, D.F.; Mo, F.; Bonomi, A.E.; Tulsky, D.S.; Lloyd, S.R.; Deasy, S.; Cobleigh, M.; Shiomoto, G. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J. Clin. Oncol. 1997, 15, 974–986. [Google Scholar] [CrossRef] [PubMed]
- Yellen, S.B.; Cella, D.F.; Webster, K.; Blendowski, C.; Kaplan, E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J. Pain. Symptom Manag. 1997, 13, 63–74. [Google Scholar] [CrossRef]
- Bonsignore, M.; Barkow, K.; Jessen, F.; Heun, R. Validity of the five-item WHO Well-Being Index (WHO-5) in an elderly population. Eur. Arch. Psychiatry Clin. Neurosci. 2001, 251 (Suppl. S2), 27–31. [Google Scholar] [CrossRef]
- Schneider, E.E.; Schönfelder, S.; Domke-Wolf, M.; Wessa, M. Measuring stress in clinical and nonclinical subjects using a German adaptation of the Perceived Stress Scale. Int. J. Clin. Health Psychol. 2020, 20, 173–181. [Google Scholar] [CrossRef]
- Herrmann-Lingen, C.B.U.; Snaith, R. HADS-D Hospital Anxiety and Depression Scale—Deutsche Version; Hans Huber: Bern, Germany, 2011. [Google Scholar]
- Esch, T.; Jose, G.; Gimpel, C.; von Scheidt, C.; Michalsen, A. The Flourishing Scale (FS) by Diener et al. is now available in an authorized German version (FS-D): Application in mind-body medicine. Forsch. Komplementmed. 2013, 20, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Dzhambov, A.M. Perceived Benefits of Nature Questionnaire: Preliminary Results. Ecopsychology 2014, 6, 109–115. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Beierlein, C.; Kovaleva, A.; Kemper, C.J.; Rammstedt, B. Allgemeine Selbstwirksamkeit Kurzskala (ASKU). In Zusammenstellung Sozialwissenschaftlicher Items und Skalen (ZIS); Leibniz Institute for Psychology: Trier, Germany, 2014. [Google Scholar]
- Walach, H.; Buchheld, N.; Buttenmüller, V.; Kleinknecht, N.; Schmidt, S. Measuring mindfulness—The Freiburg Mindfulness Inventory (FMI). Personal. Individ. Differ. 2006, 40, 1543–1555. [Google Scholar] [CrossRef]
- Hupfeld, J.; Ruffieux, N. Validierung einer deutschen Version der Self-Compassion Scale (SCS-D). Z. Klin. Psychol. Psychother. 2011, 40, 115–123. [Google Scholar] [CrossRef]
- Schafer, J.L. Analysis of Incomplete Multivariate Data; Chapman and Hall: New York, NY, USA, 1997. [Google Scholar]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: New York, NY, USA, 1987. [Google Scholar]
- Wu, H.; Li, F.; Zhang, F. The efficacy of mindfulness-based stress reduction vs. standard or usual care in patients with breast cancer: A systematic review and meta-analysis of randomized controlled trials. Transl. Cancer Res. 2022, 11, 4148–4158. [Google Scholar] [CrossRef]
- Zainal, N.Z.; Booth, S.; Huppert, F.A. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: A meta-analysis. Psychooncology 2013, 22, 1457–1465. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Lauche, R.; Paul, A.; Dobos, G. Mindfulness-based stress reduction for breast cancer-a systematic review and meta-analysis. Curr. Oncol. 2012, 19, e343–e352. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Lange, S.; Klose, P.; Paul, A.; Dobos, G. Yoga for breast cancer patients and survivors: A systematic review and meta-analysis. BMC Cancer 2012, 12, 412. [Google Scholar] [CrossRef] [PubMed]
- Buffart, L.M.; van Uffelen, J.G.; Riphagen, I.I.; Brug, J.; van Mechelen, W.; Brown, W.J.; Chinapaw, M.J. Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer 2012, 12, 559. [Google Scholar] [CrossRef]
- Parahoo, K.; McDonough, S.; McCaughan, E.; Noyes, J.; Semple, C.; Halstead, E.J.; Neuberger, M.M.; Dahm, P. Psychosocial interventions for men with prostate cancer: A Cochrane systematic review. BJU Int. 2015, 116, 174–183. [Google Scholar] [CrossRef]
- Jassim, G.A.; Whitford, D.L.; Hickey, A.; Carter, B. Psychological interventions for women with non-metastatic breast cancer. Cochrane Database Syst. Rev. 2015, CD008729. [Google Scholar] [CrossRef]
- Mustafa, M.; Carson-Stevens, A.; Gillespie, D.; Edwards, A.G. Psychological interventions for women with metastatic breast cancer. Cochrane Database Syst. Rev. 2013, CD004253. [Google Scholar] [CrossRef]
- Stern, C.; Kennedy, C. Psychosocial interventions for patients with head and neck cancer. Int. J. Evid.-Based Healthc. 2015, 13, 37–38. [Google Scholar] [CrossRef]
- Lutgendorf, S.K.; Slavich, G.M.; Degeest, K.; Goodheart, M.; Bender, D.; Thaker, P.H.; Penedo, F.; Zimmerman, B.; Lucci, J., 3rd; Mendez, L.; et al. Non-cancer life stressors contribute to impaired quality of life in ovarian cancer patients. Gynecol. Oncol. 2013, 131, 667–673. [Google Scholar] [CrossRef]
- Zaami, S.; Stark, M.; Signore, F.; Gullo, G.; Marinelli, E. Fertility preservation in female cancer sufferers: (only) a moral obligation? Eur. J. Contracept. Reprod. Health Care 2022, 27, 335–340. [Google Scholar] [CrossRef]
- Zaami, S.; Melcarne, R.; Patrone, R.; Gullo, G.; Negro, F.; Napoletano, G.; Monti, M.; Aceti, V.; Panarese, A.; Borcea, M.C.; et al. Oncofertility and Reproductive Counseling in Patients with Breast Cancer: A Retrospective Study. J. Clin. Med. 2022, 11, 1311. [Google Scholar] [CrossRef] [PubMed]
- Burgio, S.; Polizzi, C.; Buzzaccarini, G.; Laganà, A.S.; Gullo, G.; Perricone, G.; Perino, A.; Cucinella, G.; Alesi, M. Psychological variables in medically assisted reproduction: A systematic review. Prz. Menopauzalny 2022, 21, 47–63. [Google Scholar] [CrossRef] [PubMed]
- Coventry, P.A.; Brown, J.E.; Pervin, J.; Brabyn, S.; Pateman, R.; Breedvelt, J.; Gilbody, S.; Stancliffe, R.; McEachan, R.; White, P.L. Nature-based outdoor activities for mental and physical health: Systematic review and meta-analysis. SSM Popul. Health 2021, 16, 100934. [Google Scholar] [CrossRef] [PubMed]
- Brito, H.S.; Carraça, E.V.; Palmeira, A.L.; Ferreira, J.P.; Vleck, V.; Araújo, D. Benefits to Performance and Well-Being of Nature-Based Exercise: A Critical Systematic Review and Meta-Analysis. Environ. Sci. Technol. 2022, 56, 62–77. [Google Scholar] [CrossRef]
- Joschko, L.; Pálsdóttir, A.M.; Grahn, P.; Hinse, M. Nature-Based Therapy in Individuals with Mental Health Disorders, with a Focus on Mental Well-Being and Connectedness to Nature-A Pilot Study. Int. J. Environ. Res. Public. Health 2023, 20, 2167. [Google Scholar] [CrossRef]
- Morita, E.; Fukuda, S.; Nagano, J.; Hamajima, N.; Yamamoto, H.; Iwai, Y.; Nakashima, T.; Ohira, H.; Shirakawa, T. Psychological effects of forest environments on healthy adults: Shinrin-yoku (forest-air bathing, walking) as a possible method of stress reduction. Public. Health 2007, 121, 54–63. [Google Scholar] [CrossRef]
- Eton, D.T.; Cella, D.; Yost, K.J.; Yount, S.E.; Peterman, A.H.; Neuberg, D.S.; Sledge, G.W.; Wood, W.C. A combination of distribution- and anchor-based approaches determined minimally important differences (MIDs) for four endpoints in a breast cancer scale. J. Clin. Epidemiol. 2004, 57, 898–910. [Google Scholar] [CrossRef]
- Cella, D.; Eton, D.T.; Lai, J.S.; Peterman, A.H.; Merkel, D.E. Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J. Pain. Symptom Manag. 2002, 24, 547–561. [Google Scholar] [CrossRef]
- Yang, M.; Morin, C.M.; Schaefer, K.; Wallenstein, G.V. Interpreting score differences in the Insomnia Severity Index: Using health-related outcomes to define the minimally important difference. Curr. Med. Res. Opin. 2009, 25, 2487–2494. [Google Scholar] [CrossRef]
- Djernis, D.; Lerstrup, I.; Poulsen, D.; Stigsdotter, U.; Dahlgaard, J.; O’Toole, M. A Systematic Review and Meta-Analysis of Nature-Based Mindfulness: Effects of Moving Mindfulness Training into an Outdoor Natural Setting. Int. J. Environ. Res. Public. Health 2019, 16, 3202. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).